PREGNANCY AND HUMAN DEVELOPMENT Pregnancy and Human Development























- Slides: 124
PREGNANCY AND HUMAN DEVELOPMENT
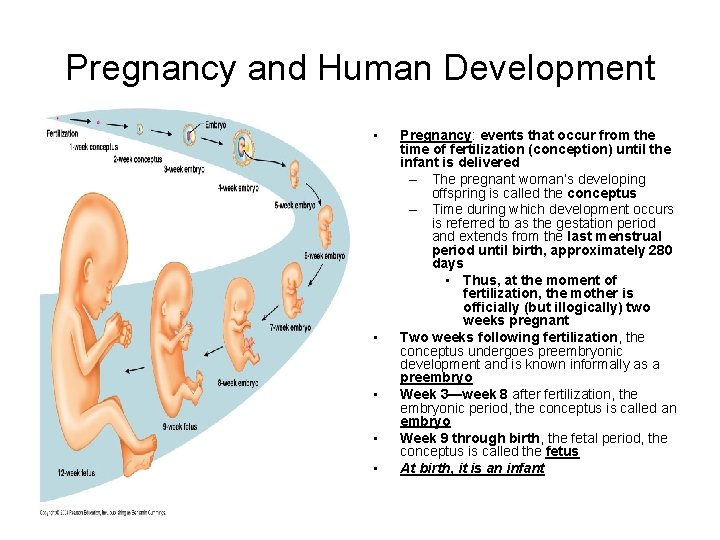
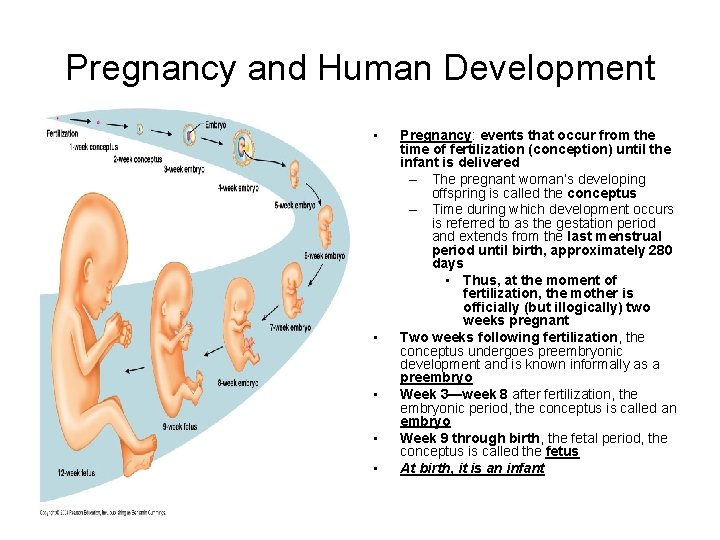
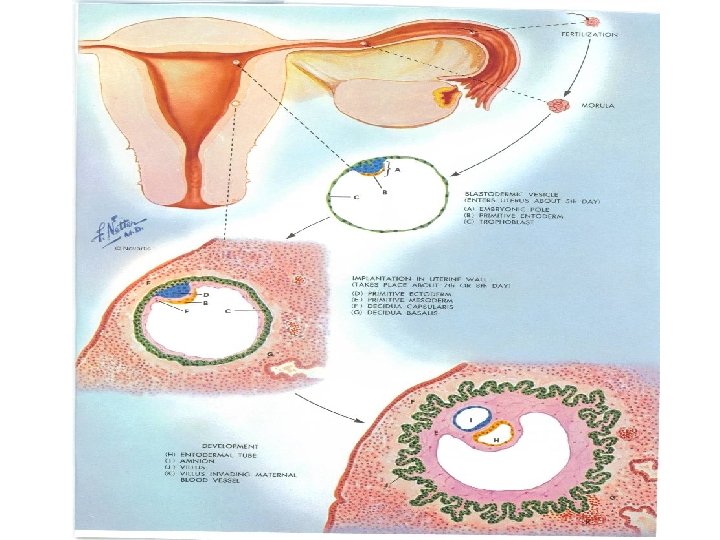
Pregnancy and Human Development • • • Pregnancy: events that occur from the time of fertilization (conception) until the infant is delivered – The pregnant woman’s developing offspring is called the conceptus – Time during which development occurs is referred to as the gestation period and extends from the last menstrual period until birth, approximately 280 days • Thus, at the moment of fertilization, the mother is officially (but illogically) two weeks pregnant Two weeks following fertilization, the conceptus undergoes preembryonic development and is known informally as a preembryo Week 3—week 8 after fertilization, the embryonic period, the conceptus is called an embryo Week 9 through birth, the fetal period, the conceptus is called the fetus At birth, it is an infant
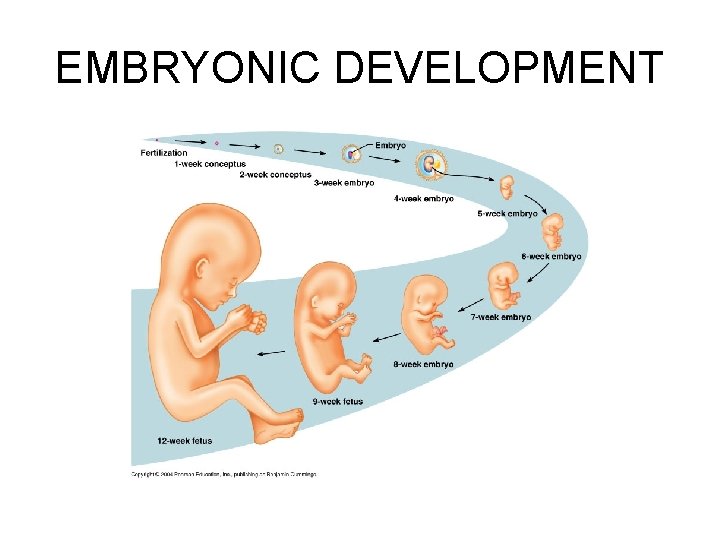
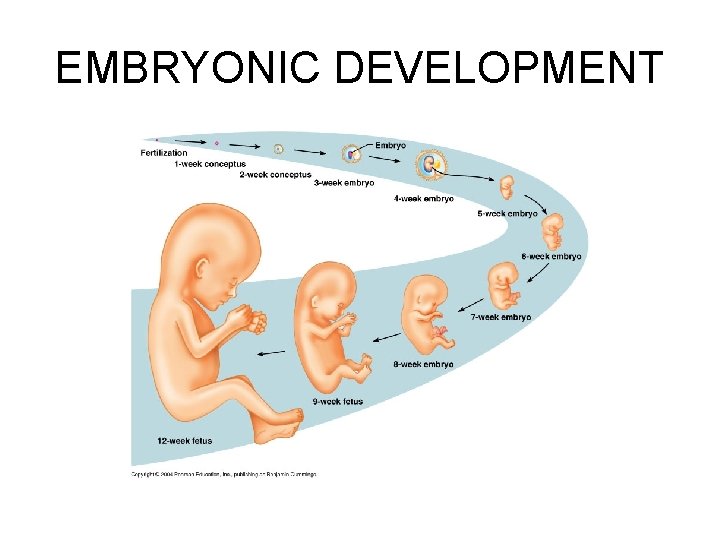
EMBRYONIC DEVELOPMENT
From Egg to Embryo Accomplishing Fertilization • Oocyte is viable for 12 to 24 hours after it is cast out of the ovary – Chance of pregnancy drops to almost zero the next day • Sperm retain their fertilizing power for 24 to 72 hours after ejaculation • For fertilization to occur, coitus must occur no more than three days (72 hours) before ovulation and no later than one day (24 hours) after ovulation, at which point the oocyte is approximately one-third of the way down the length of the uterine tube • Fertilization occurs when a sperm fuses with an egg to form a fertilized egg, or zygote, the first cell of the new individual
From Egg to Embryo Accomplishing Fertilization • Fertilization occurs when a sperm fuses with an egg to form a zygote • During copulation, millions of sperm ejaculated into the female reproductive tract are lost due to leakage from the vaginal canal, destruction by the acidic environment of the vagina, inability to pass the cervical mucus, or destruction by defense cells of the uterus – Those that do reach the uterus are subjected to forceful uterine contractions that act to disperse them throughout the uterine cavity, where thousands are destroyed by resident phagocytes • Only a few thousand (and sometimes fewer than 200 sperm), out of the millions in the male ejaculate, finally enter the uterine tubes, where the oocyte may be moving leisurely toward the uterus
From Egg to Embryo Accomplishing Fertilization • In order to fertilize an egg, sperm must be capacitated, a process involving weakening of the sperm cell membrane in order to allow release of acrosomal hydrolytic enzymes • As sperm swim through the cervical mucus, uterus, and uterine tubes, membrane proteins are removed and the cholesterol that keeps the acrosomal membranes tough and stable is depleted – The sperm undergo a gradual capacitation over the next 6 -8 hours • Thus, even though the sperm may reach the oocyte within a few minutes, they must wait around for capacitation to occur
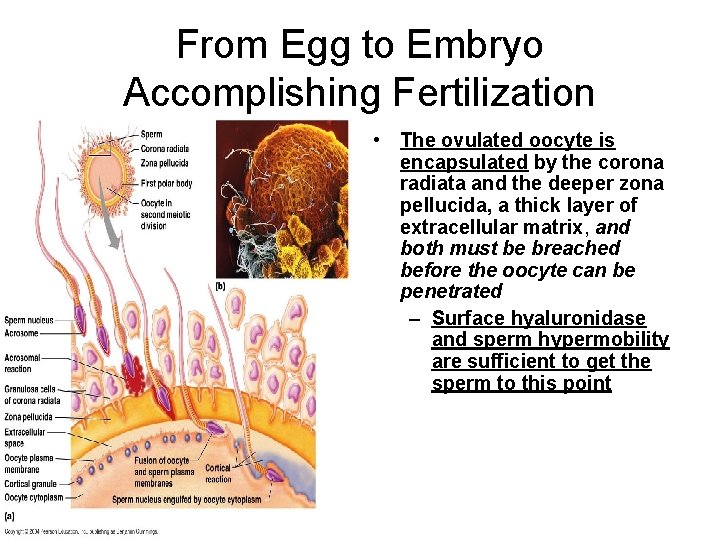
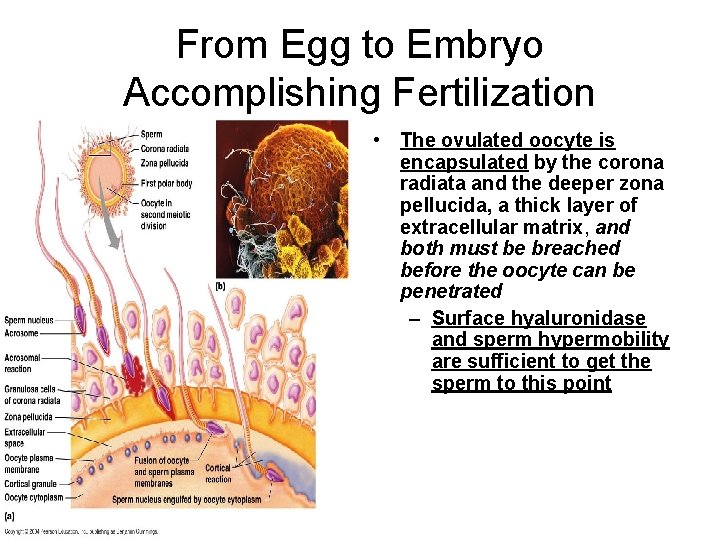
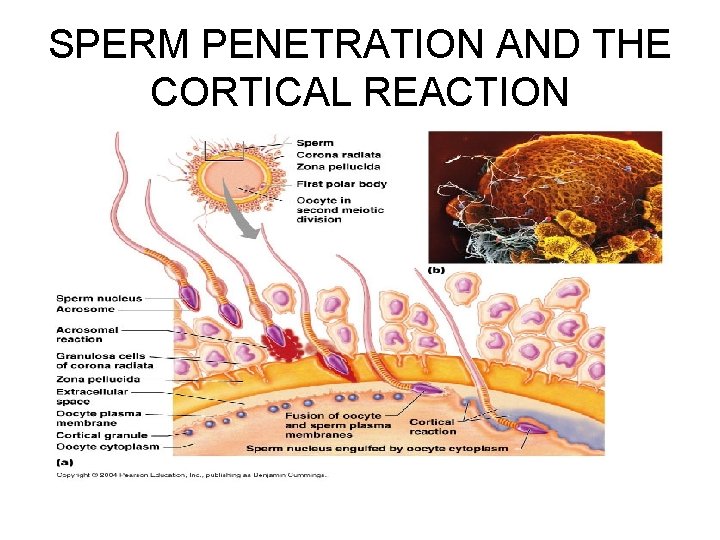
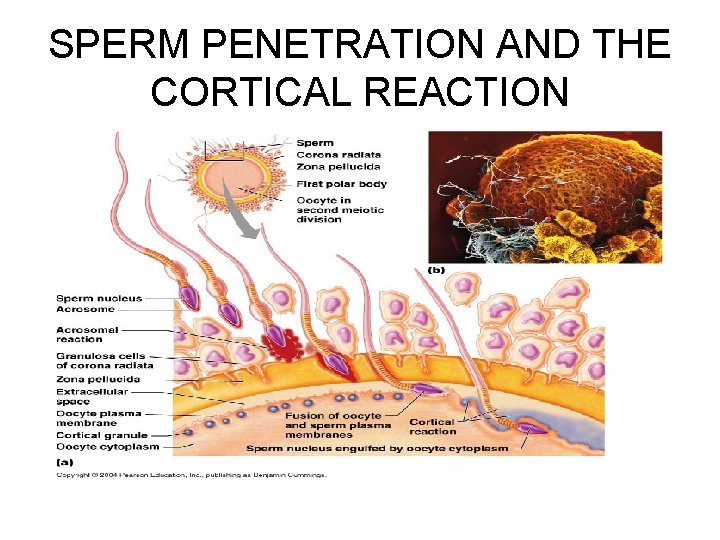
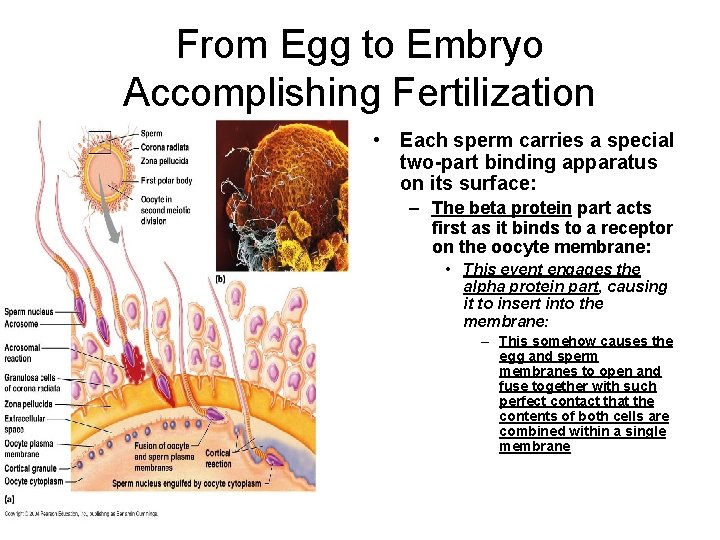
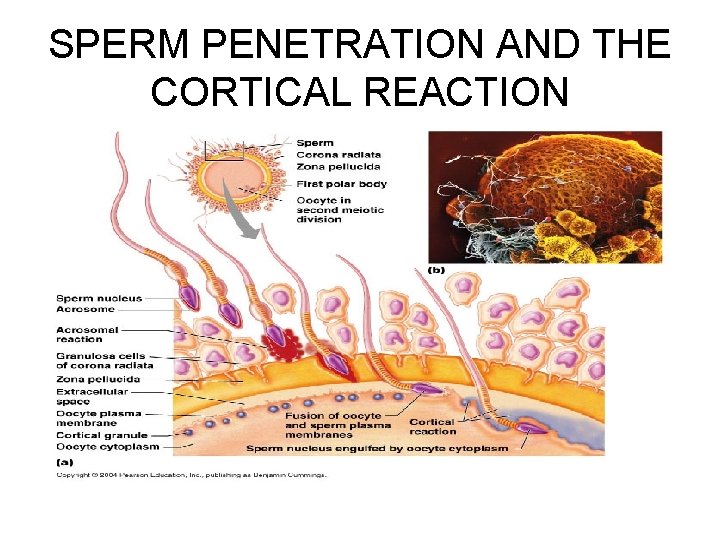
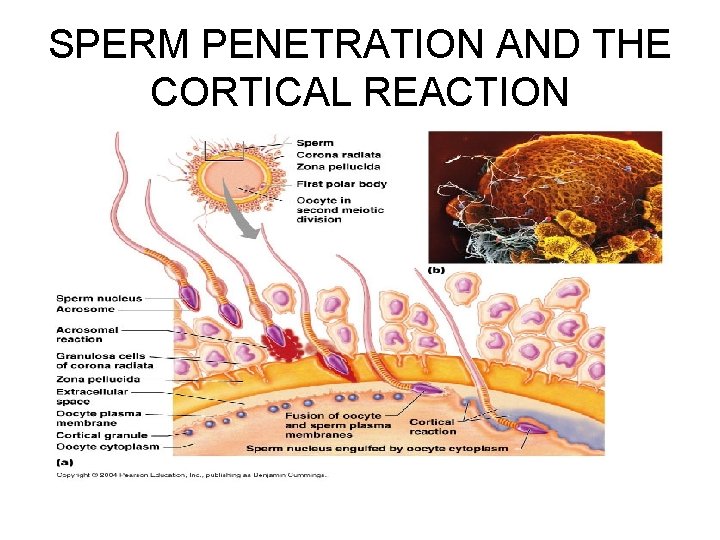
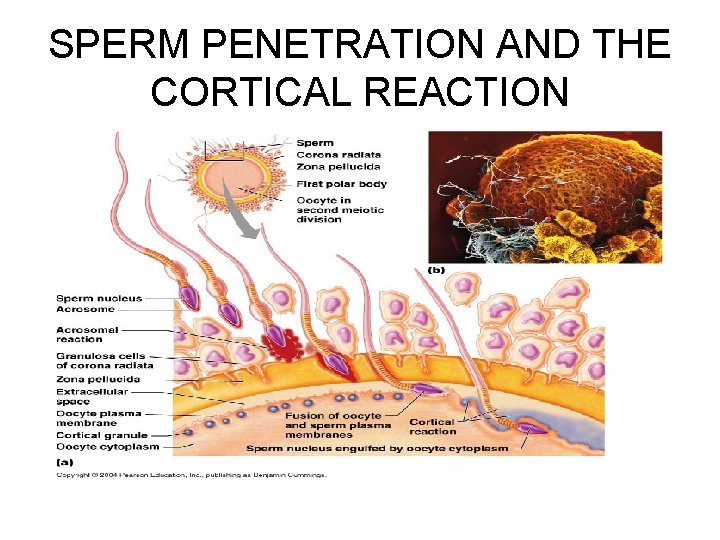
From Egg to Embryo Accomplishing Fertilization • The ovulated oocyte is encapsulated by the corona radiata and the deeper zona pellucida, a thick layer of extracellular matrix, and both must be breached before the oocyte can be penetrated – Surface hyaluronidase and sperm hypermobility are sufficient to get the sperm to this point
SPERM PENETRATION AND THE CORTICAL REACTION
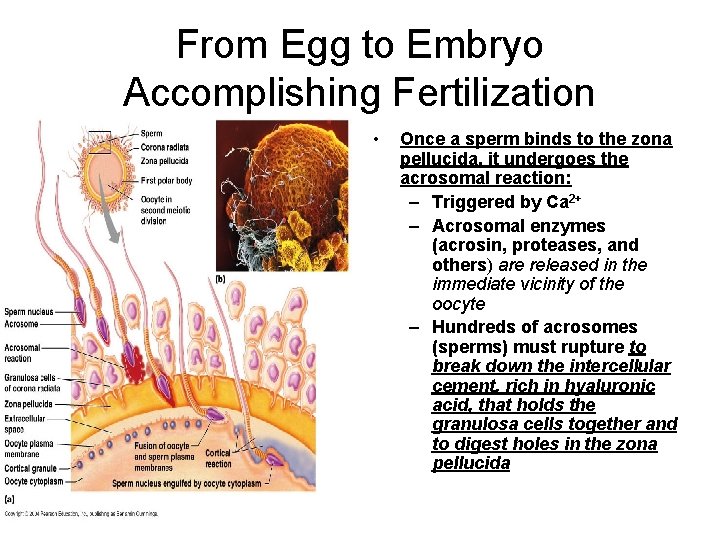
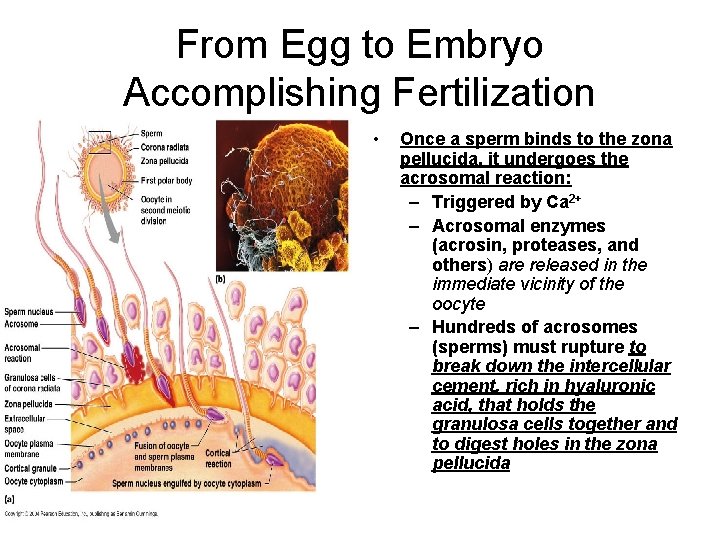
From Egg to Embryo Accomplishing Fertilization • Once a sperm binds to the zona pellucida, it undergoes the acrosomal reaction: – Triggered by Ca 2+ – Acrosomal enzymes (acrosin, proteases, and others) are released in the immediate vicinity of the oocyte – Hundreds of acrosomes (sperms) must rupture to break down the intercellular cement, rich in hyaluronic acid, that holds the granulosa cells together and to digest holes in the zona pellucida
SPERM PENETRATION AND THE CORTICAL REACTION
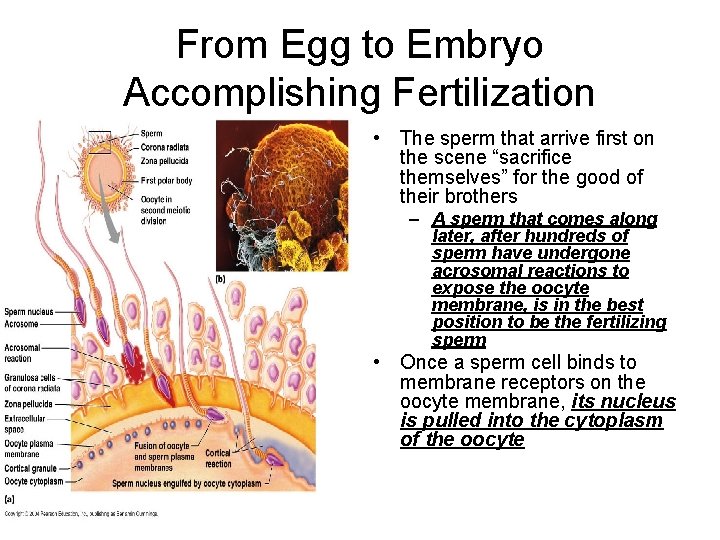
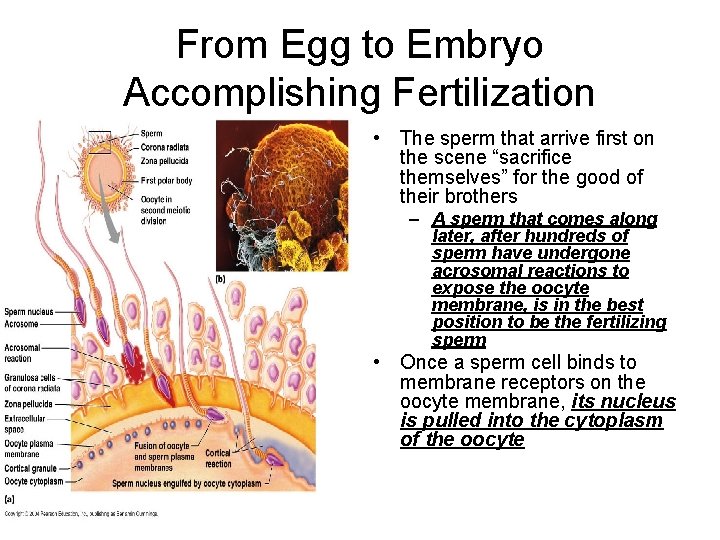
From Egg to Embryo Accomplishing Fertilization • The sperm that arrive first on the scene “sacrifice themselves” for the good of their brothers – A sperm that comes along later, after hundreds of sperm have undergone acrosomal reactions to expose the oocyte membrane, is in the best position to be the fertilizing sperm • Once a sperm cell binds to membrane receptors on the oocyte membrane, its nucleus is pulled into the cytoplasm of the oocyte

SPERM PENETRATION AND THE CORTICAL REACTION
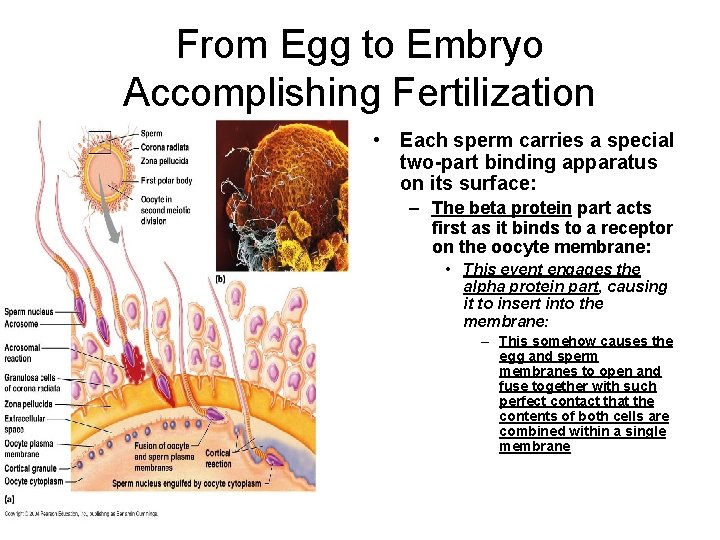
From Egg to Embryo Accomplishing Fertilization • Each sperm carries a special two-part binding apparatus on its surface: – The beta protein part acts first as it binds to a receptor on the oocyte membrane: • This event engages the alpha protein part, causing it to insert into the membrane: – This somehow causes the egg and sperm membranes to open and fuse together with such perfect contact that the contents of both cells are combined within a single membrane
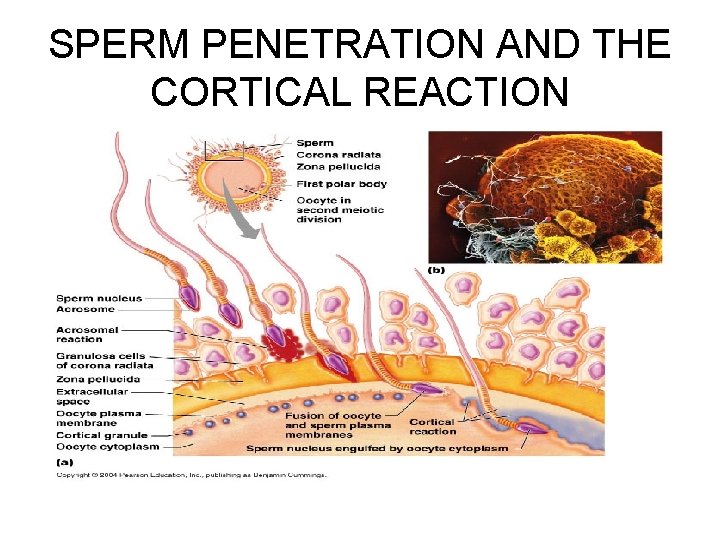
SPERM PENETRATION AND THE CORTICAL REACTION
Blocks to Polyspermy • Polyspermy, or fertilization by more than one sperm cell, leads to a lethal number of chromosomes, and must be prevented
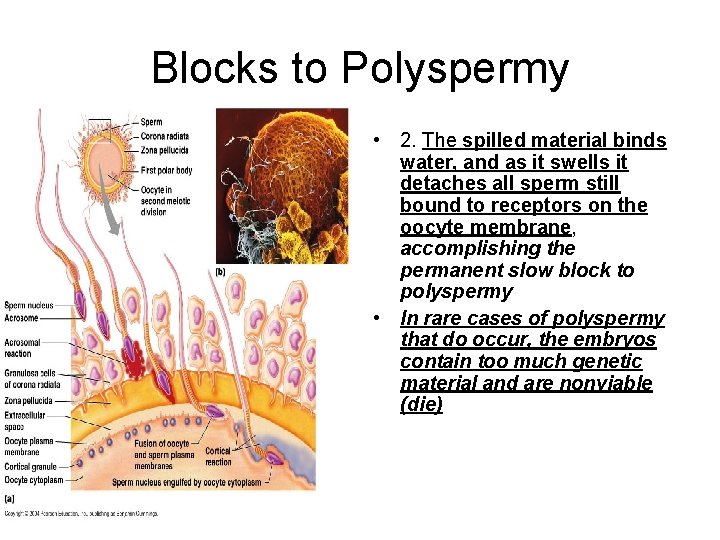
Blocks to Polyspermy • Two mechanisms ensure monospermy: the one sperm condition: – 1. When the plasma membrane of one sperm contacts the oocyte membrane, sodium channels open and Na+ diffuses into the oocyte from the extracellular space, causing its membrane to depolarize: • This electrical event, called the fast block to polyspermy, prevents other sperm from fusing with the oocyte membrane • Once the sperm has entered, Ca 2+ is released by the oocyte’s endoplasmic reticulum into its cytoplasm, which activates the oocyte to prepare for cell division – It also causes the cortical reaction, in which granules located just deep to the plasma membrane spill their enzymes into the extracellular space beneath the zona pellucida » These enzymes, called zonal inhibiting proteins (ZIPS), destroy the sperm receptors, preventing further sperm entry
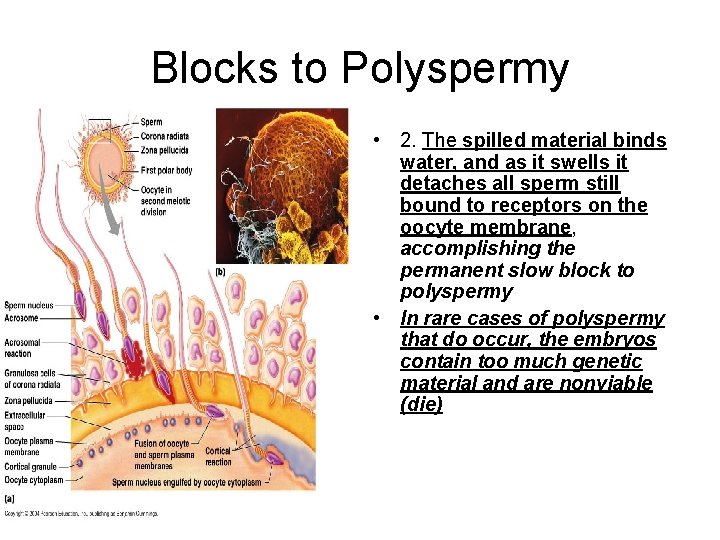
Blocks to Polyspermy • 2. The spilled material binds water, and as it swells it detaches all sperm still bound to receptors on the oocyte membrane, accomplishing the permanent slow block to polyspermy • In rare cases of polyspermy that do occur, the embryos contain too much genetic material and are nonviable (die)
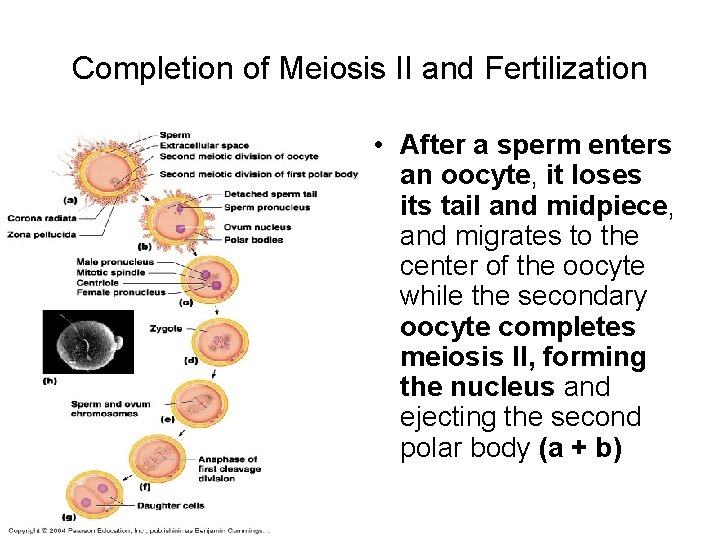
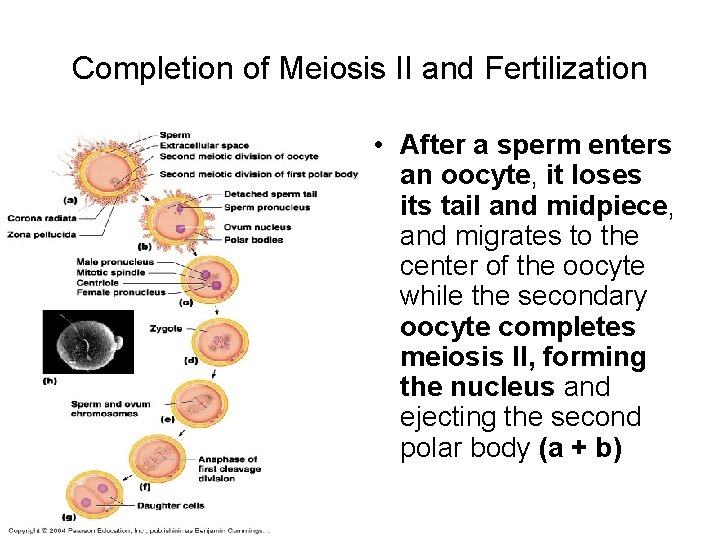
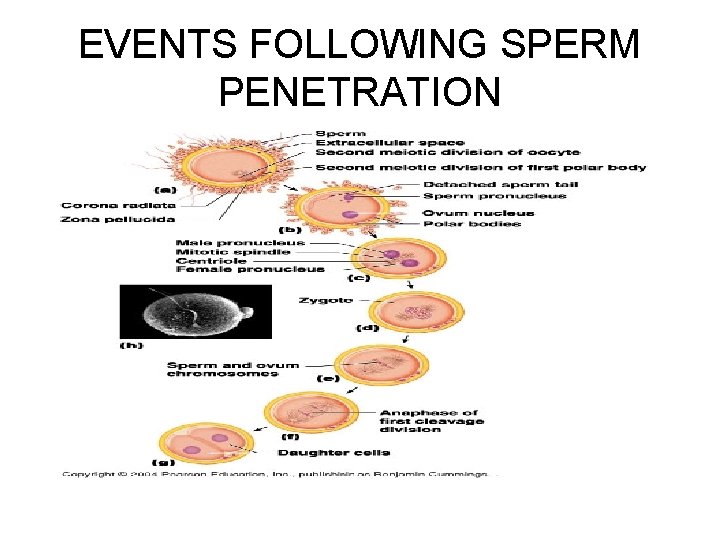
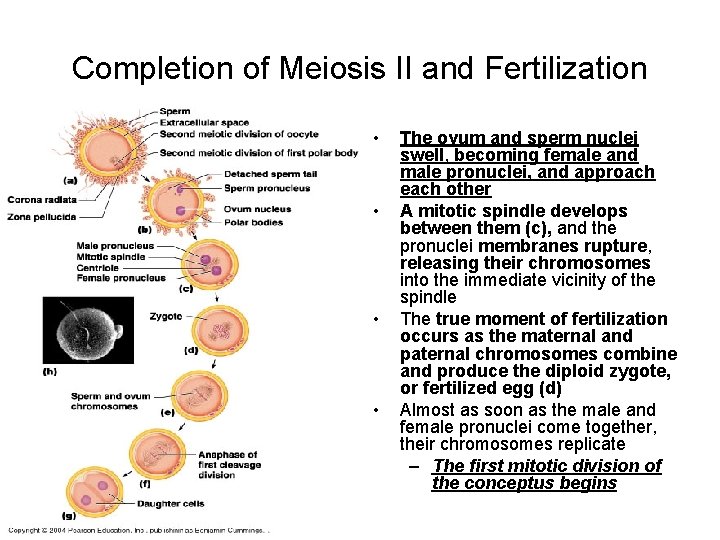
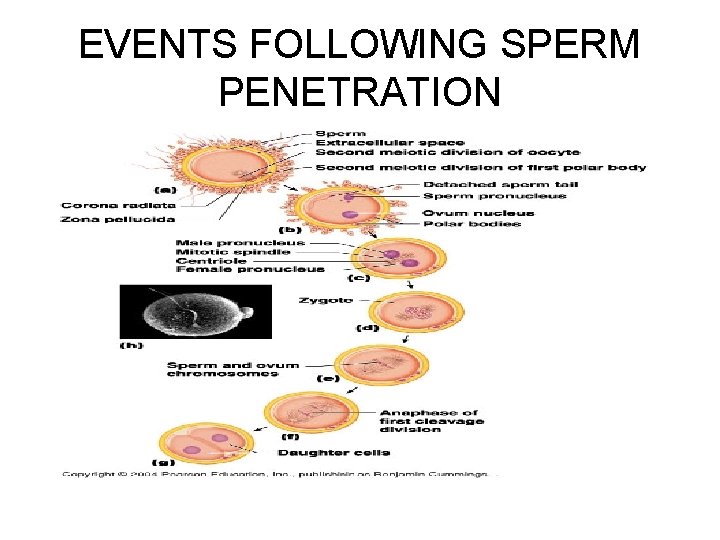
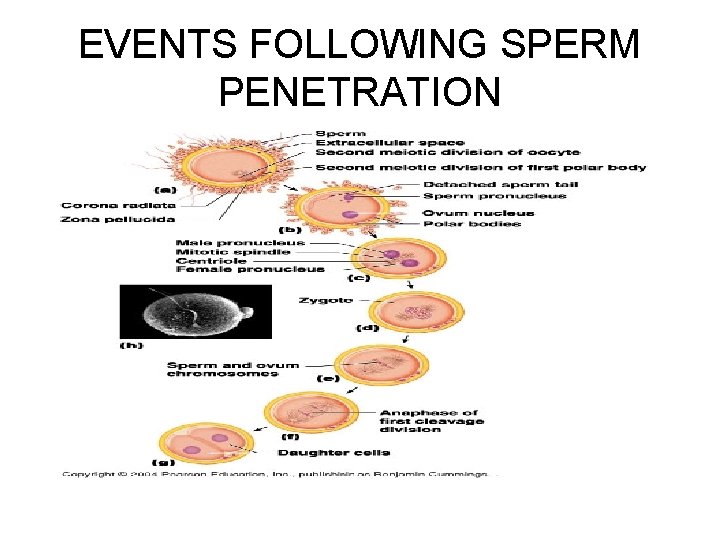
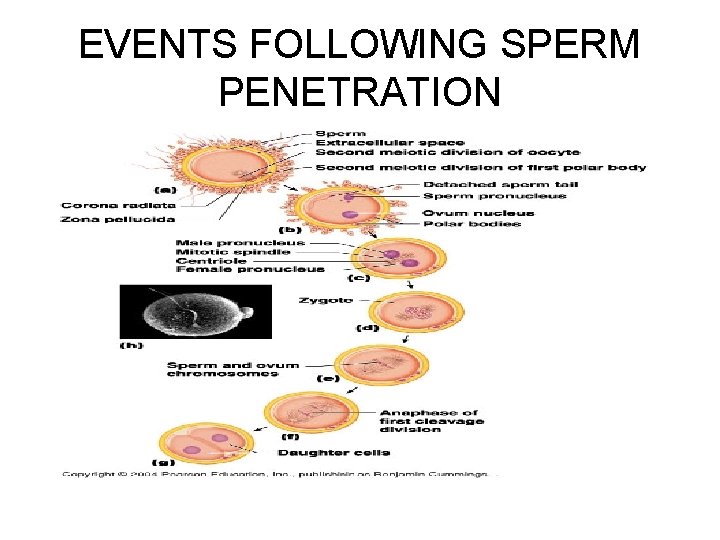
Completion of Meiosis II and Fertilization • After a sperm enters an oocyte, it loses its tail and midpiece, and migrates to the center of the oocyte while the secondary oocyte completes meiosis II, forming the nucleus and ejecting the second polar body (a + b)
EVENTS FOLLOWING SPERM PENETRATION
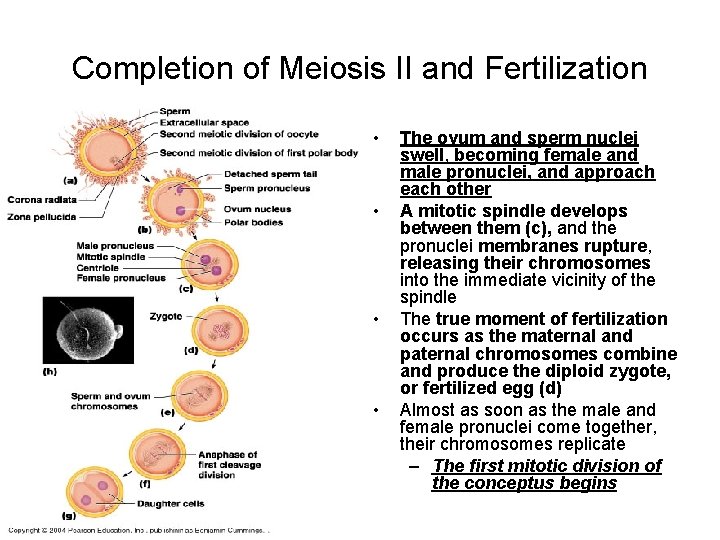
Completion of Meiosis II and Fertilization • • The ovum and sperm nuclei swell, becoming female and male pronuclei, and approach each other A mitotic spindle develops between them (c), and the pronuclei membranes rupture, releasing their chromosomes into the immediate vicinity of the spindle The true moment of fertilization occurs as the maternal and paternal chromosomes combine and produce the diploid zygote, or fertilized egg (d) Almost as soon as the male and female pronuclei come together, their chromosomes replicate – The first mitotic division of the conceptus begins
EVENTS FOLLOWING SPERM PENETRATION
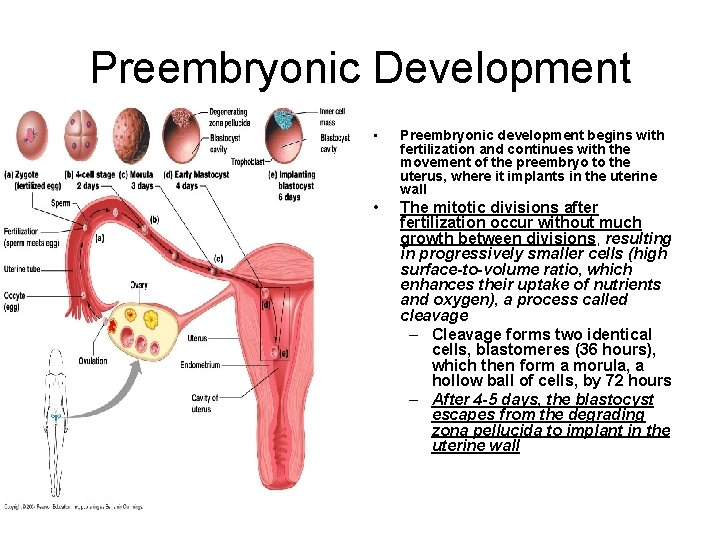
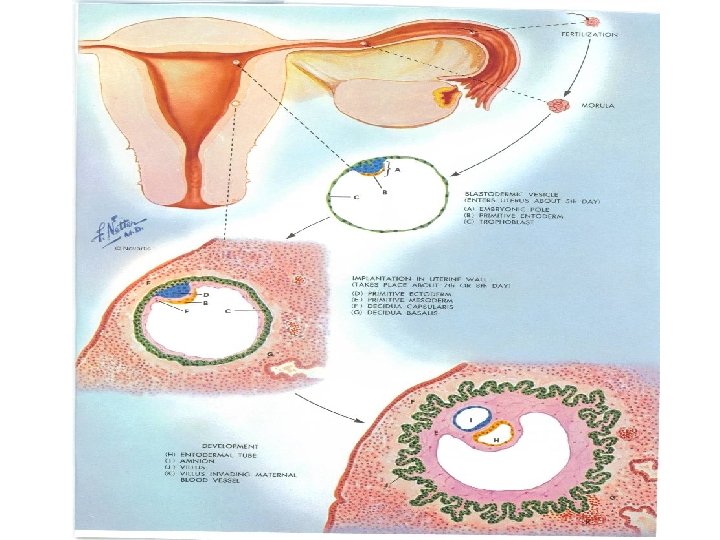
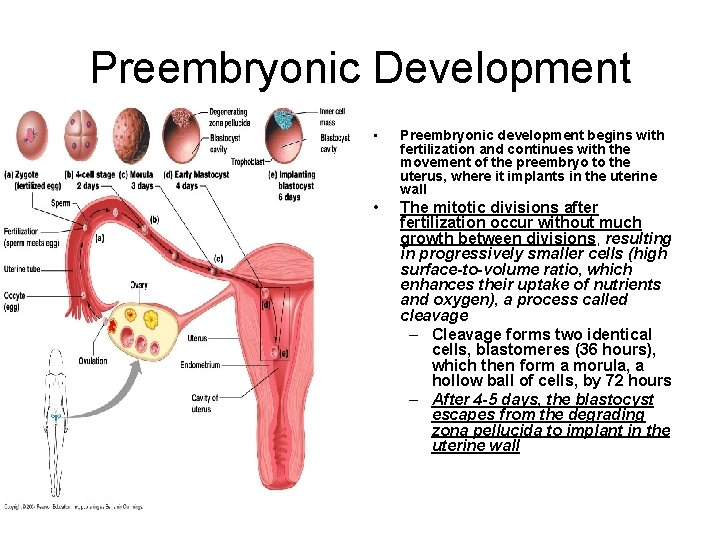
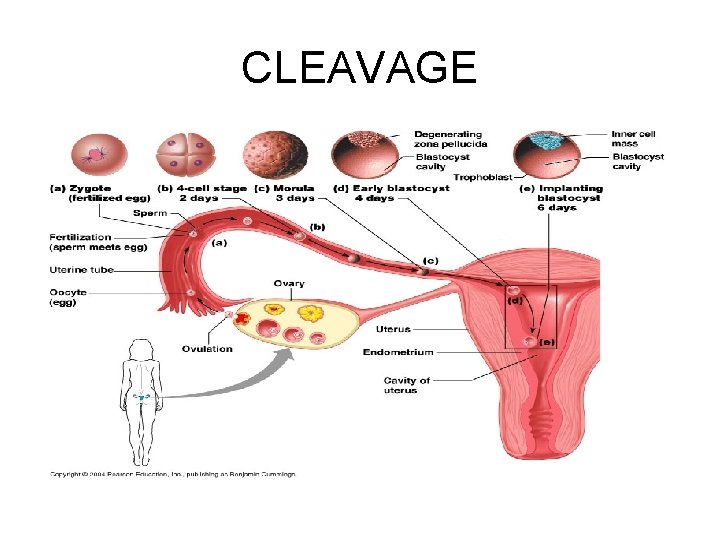
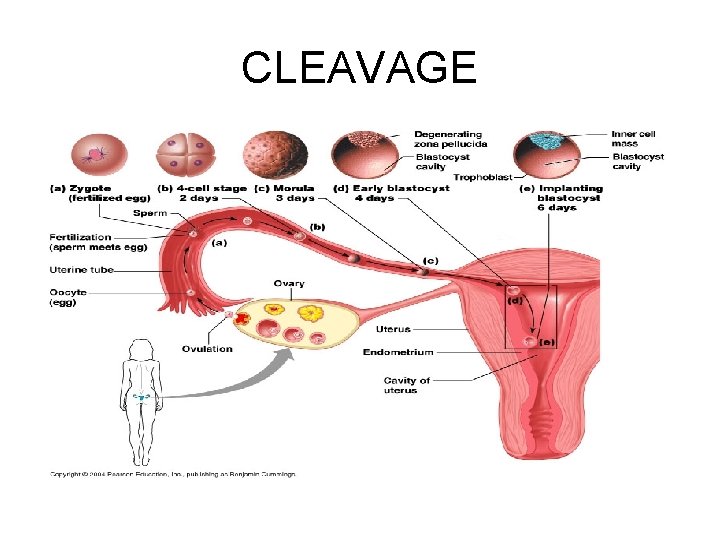
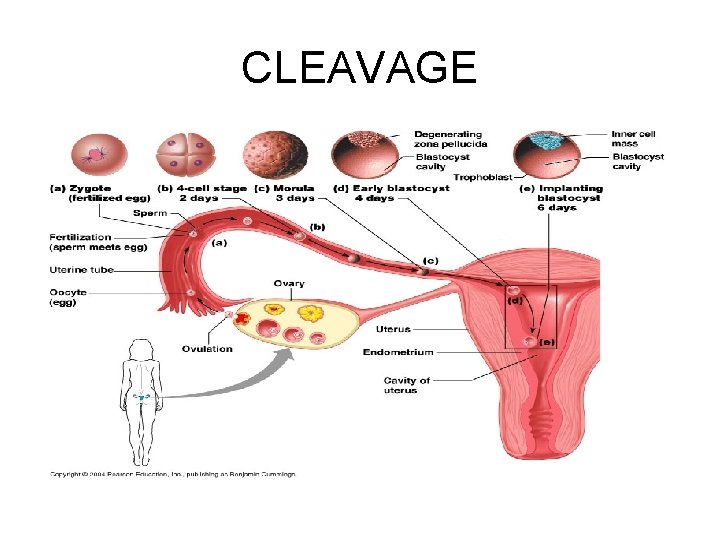
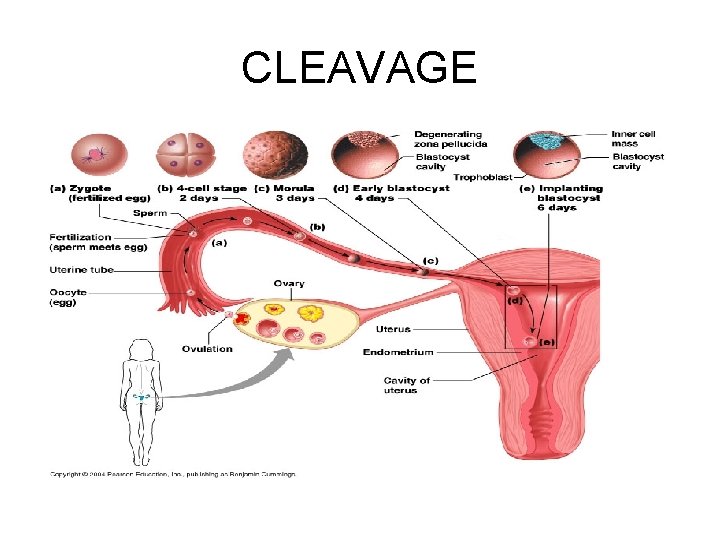
Preembryonic Development • Preembryonic development begins with fertilization and continues with the movement of the preembryo to the uterus, where it implants in the uterine wall • The mitotic divisions after fertilization occur without much growth between divisions, resulting in progressively smaller cells (high surface-to-volume ratio, which enhances their uptake of nutrients and oxygen), a process called cleavage – Cleavage forms two identical cells, blastomeres (36 hours), which then form a morula, a hollow ball of cells, by 72 hours – After 4 -5 days, the blastocyst escapes from the degrading zona pellucida to implant in the uterine wall
CLEAVAGE
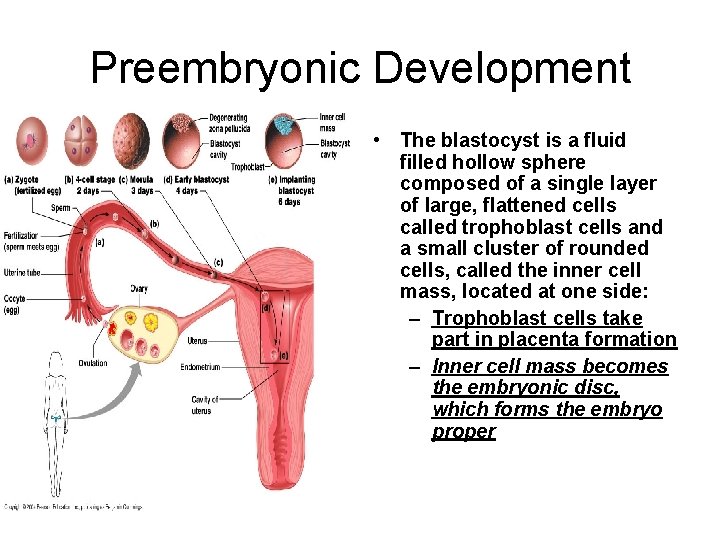
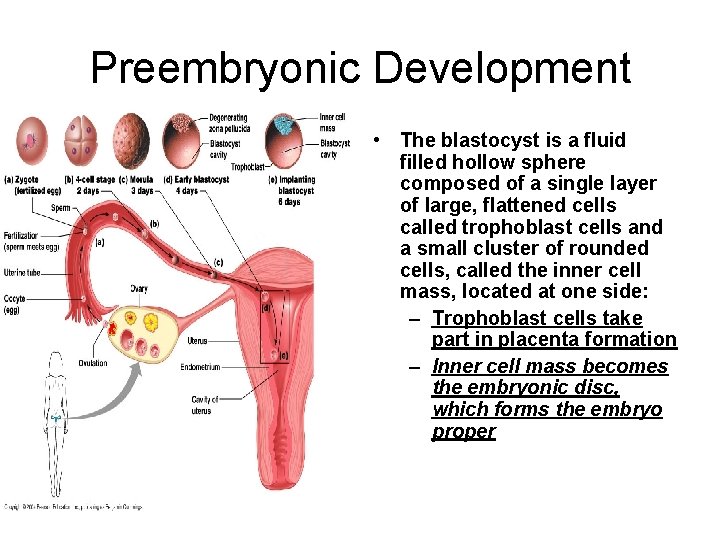
Preembryonic Development • The blastocyst is a fluid filled hollow sphere composed of a single layer of large, flattened cells called trophoblast cells and a small cluster of rounded cells, called the inner cell mass, located at one side: – Trophoblast cells take part in placenta formation – Inner cell mass becomes the embryonic disc, which forms the embryo proper
CLEAVAGE

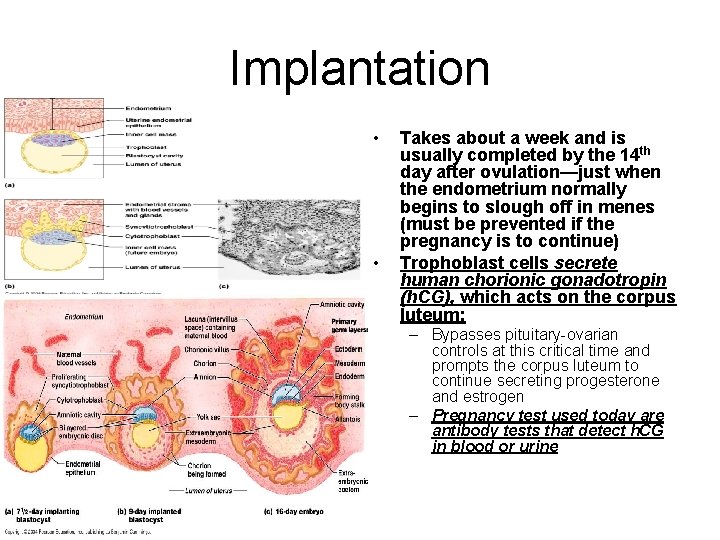
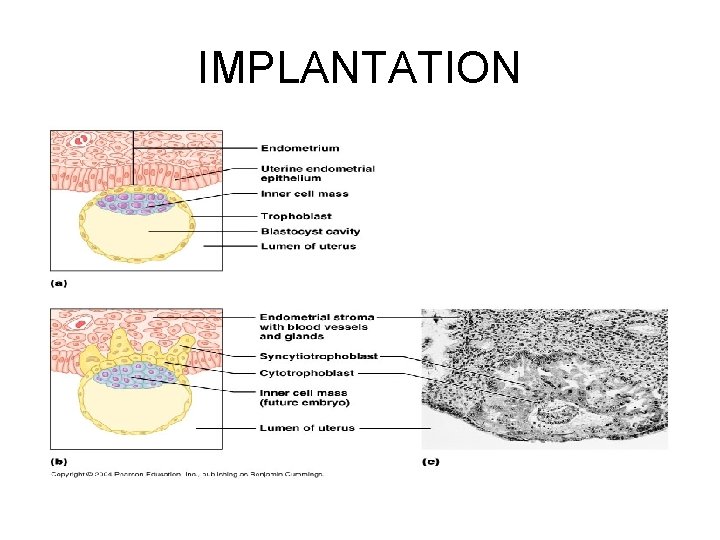
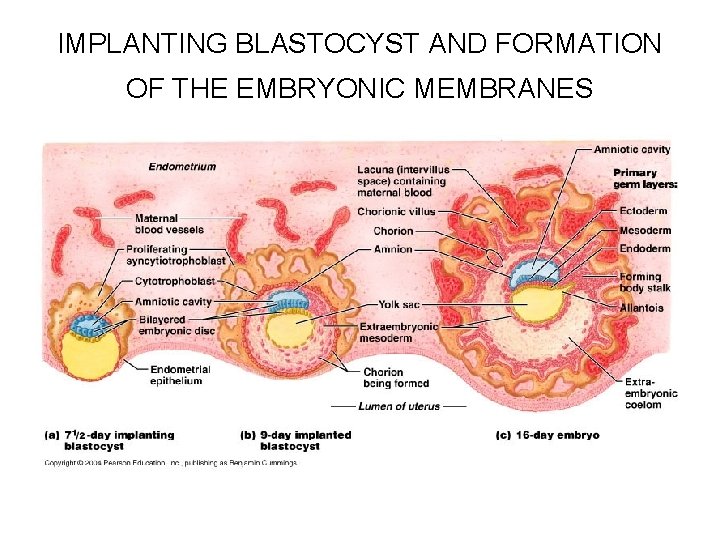
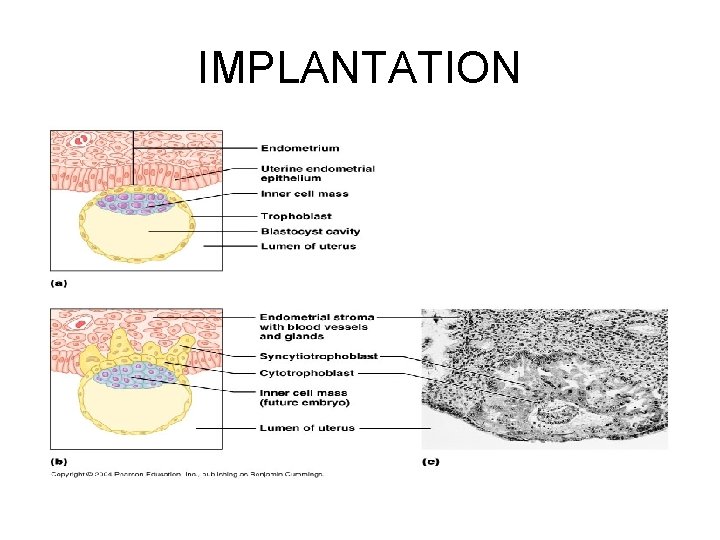
Implantation • Occurs after 6 -7 days; the trophoblast adheres to the endometrium, and produces enzymes that irritate (takes on the characteristics of an inflammation site) the endometrium – Uterine capillaries become permeable and leaky, and inflammatory cells including lymphocytes, natural killer cells, and macrohages invade the area – The trophoblast proliferates, forming two distinct layers; • Inner cytotrophoblast: cells retain their cell boundaries • Outer syncytiotrophoblast: cells that lose their plasma membranes and form a multinuclear cytoplasmic mass – Invade the endometrium and rapidly digests the uterine cells it contacts – Implanted blastocyst is covered over and sealed off from the uterine cavity by proliferation of the endometrical cells
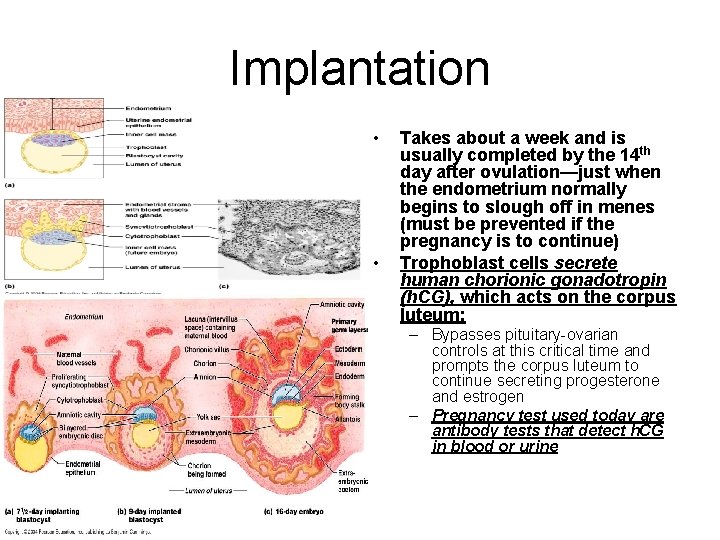
Implantation • • Takes about a week and is usually completed by the 14 th day after ovulation—just when the endometrium normally begins to slough off in menes (must be prevented if the pregnancy is to continue) Trophoblast cells secrete human chorionic gonadotropin (h. CG), which acts on the corpus luteum: – Bypasses pituitary-ovarian controls at this critical time and prompts the corpus luteum to continue secreting progesterone and estrogen – Pregnancy test used today are antibody tests that detect h. CG in blood or urine
IMPLANTATION

IMPLANTING BLASTOCYST AND FORMATION OF THE EMBRYONIC MEMBRANES
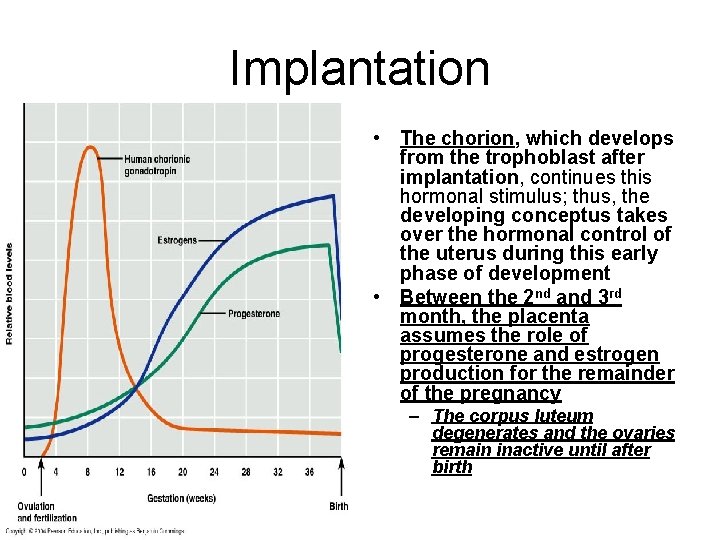
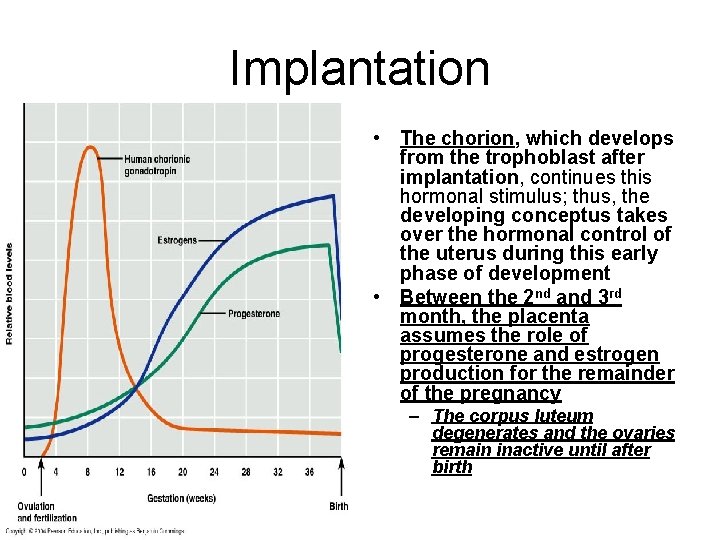
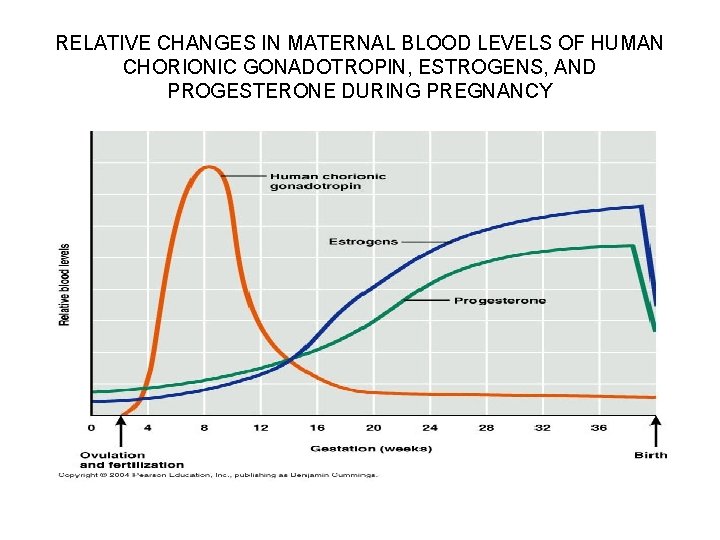
Implantation • The chorion, which develops from the trophoblast after implantation, continues this hormonal stimulus; thus, the developing conceptus takes over the hormonal control of the uterus during this early phase of development • Between the 2 nd and 3 rd month, the placenta assumes the role of progesterone and estrogen production for the remainder of the pregnancy – The corpus luteum degenerates and the ovaries remain inactive until after birth
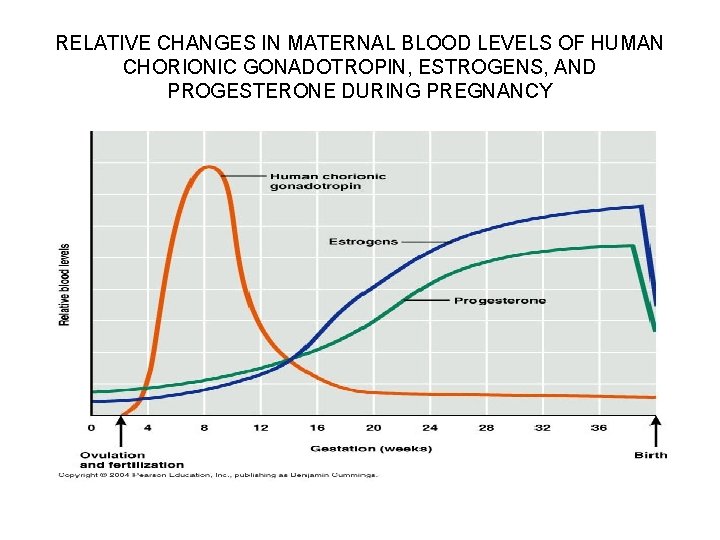
RELATIVE CHANGES IN MATERNAL BLOOD LEVELS OF HUMAN CHORIONIC GONADOTROPIN, ESTROGENS, AND PROGESTERONE DURING PREGNANCY
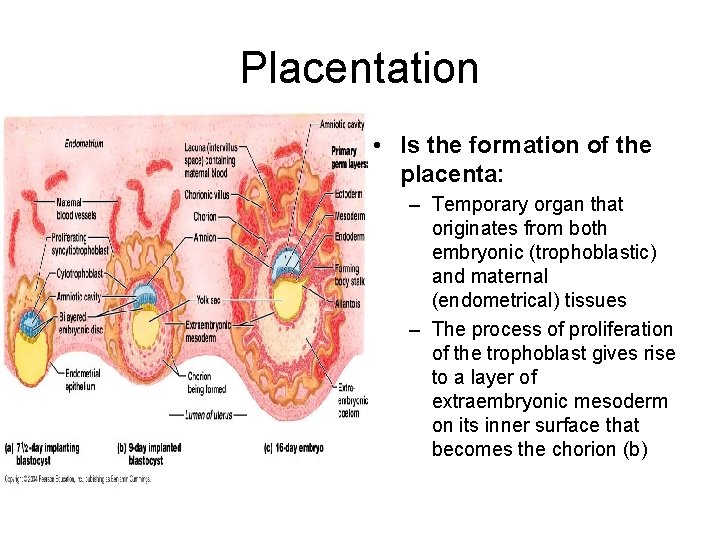
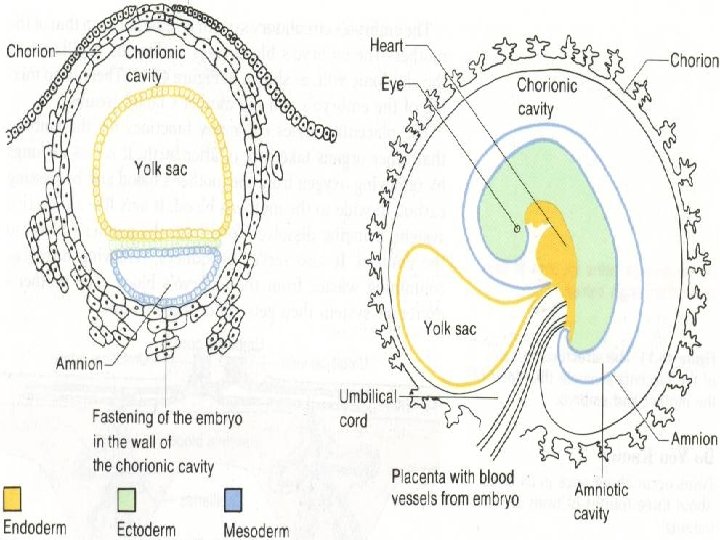
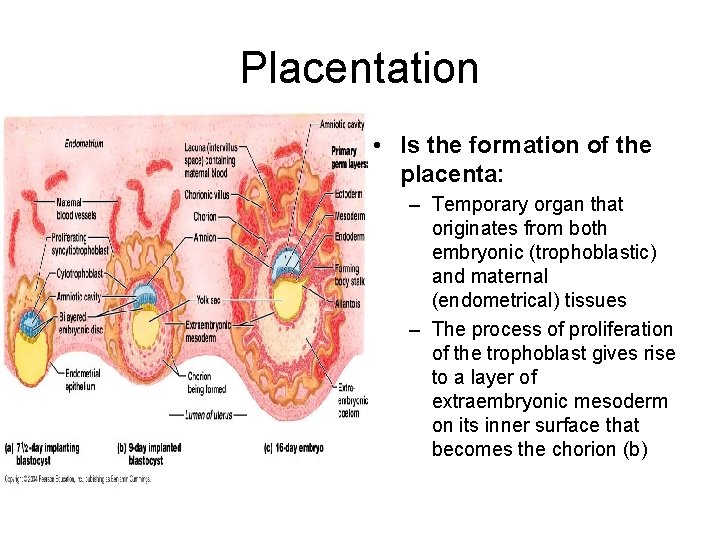
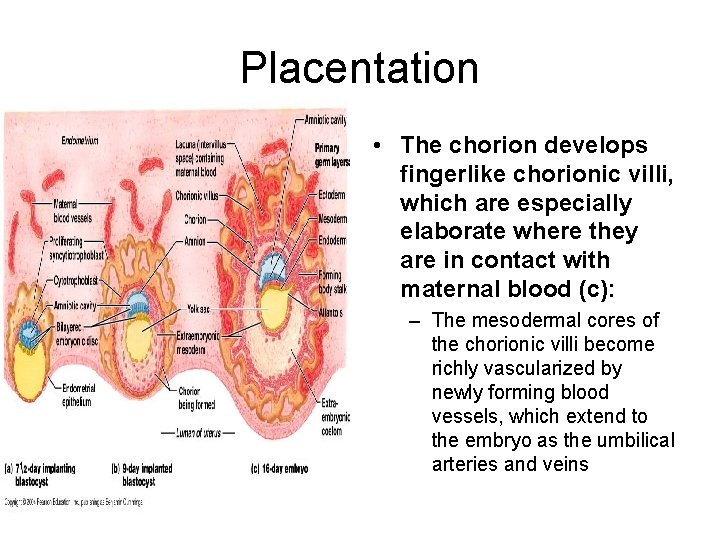
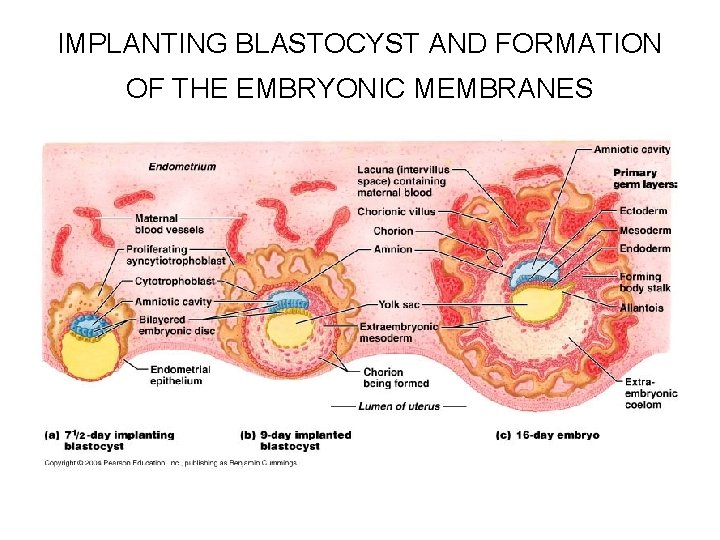
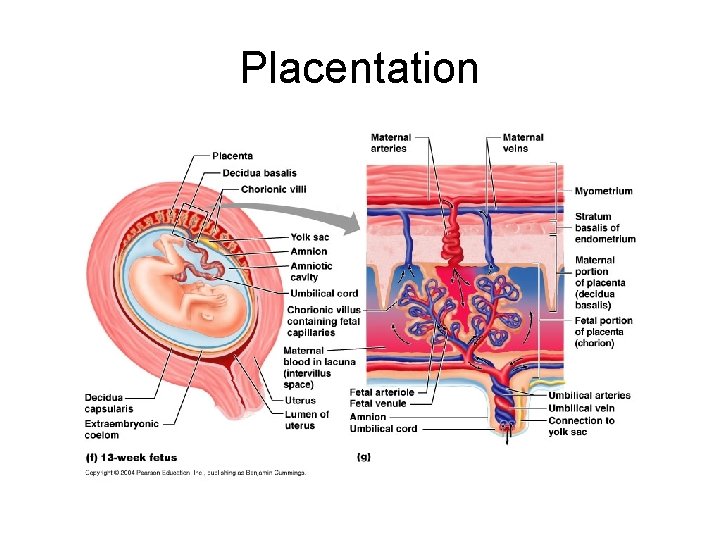
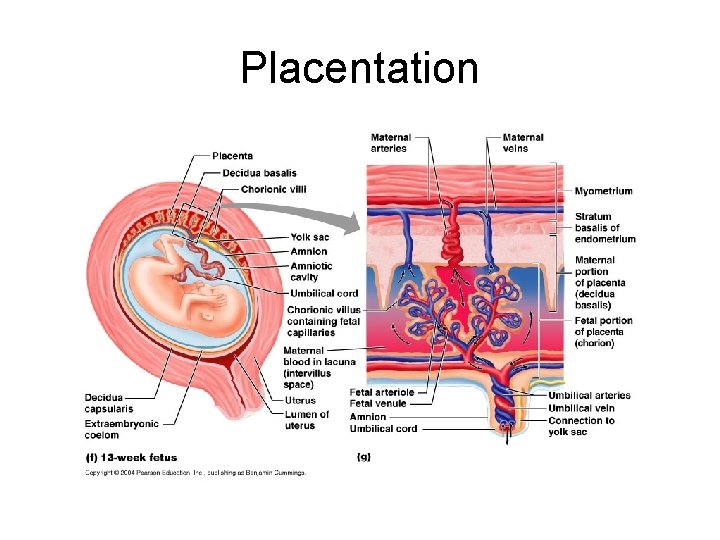
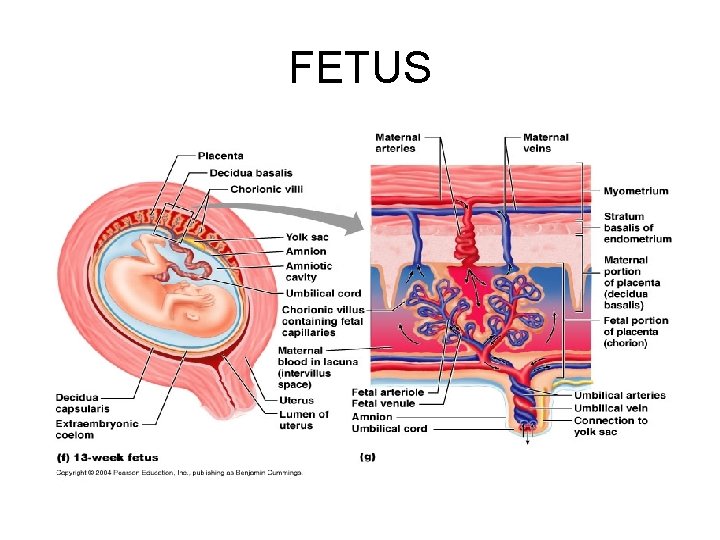
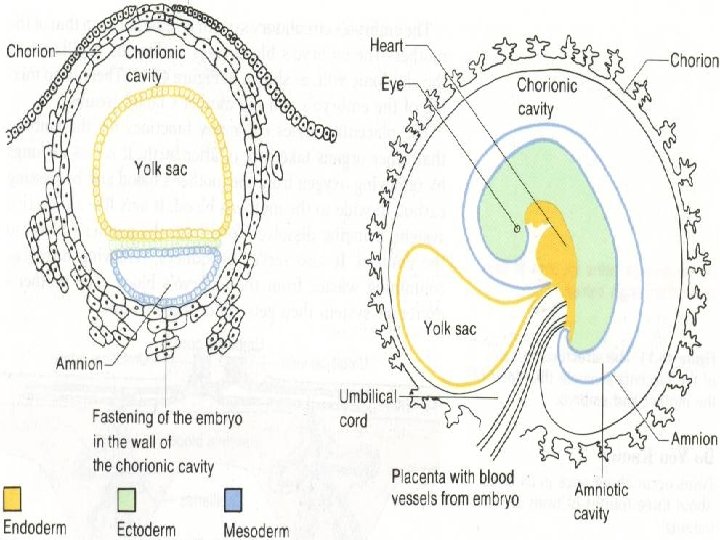
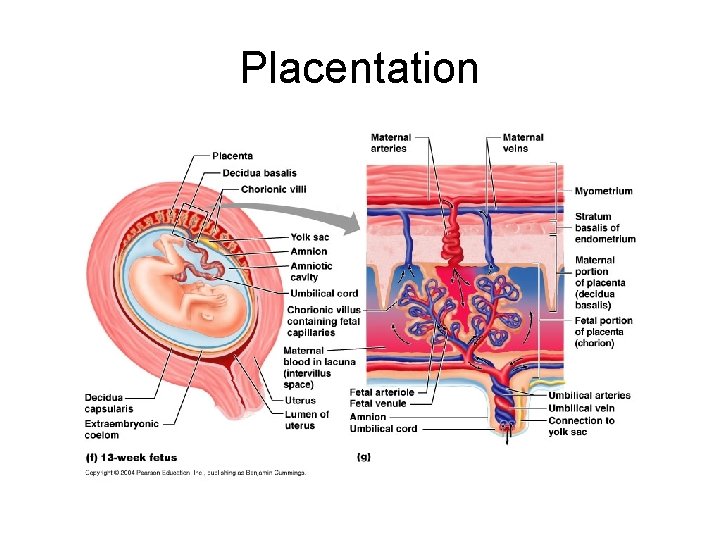
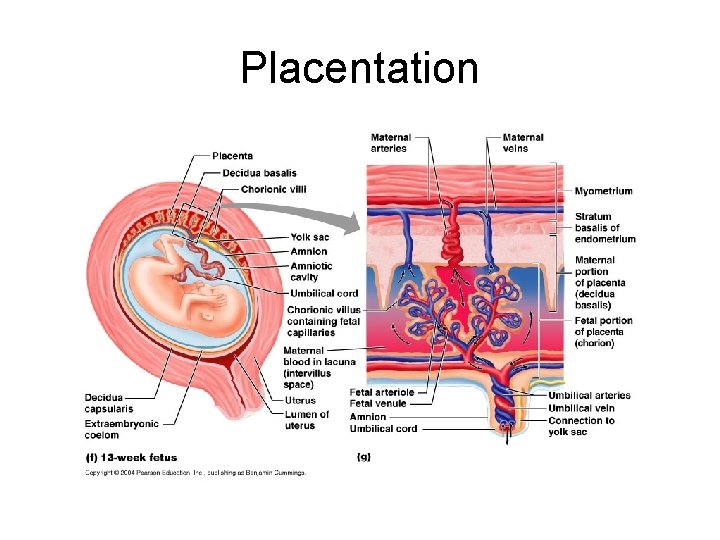
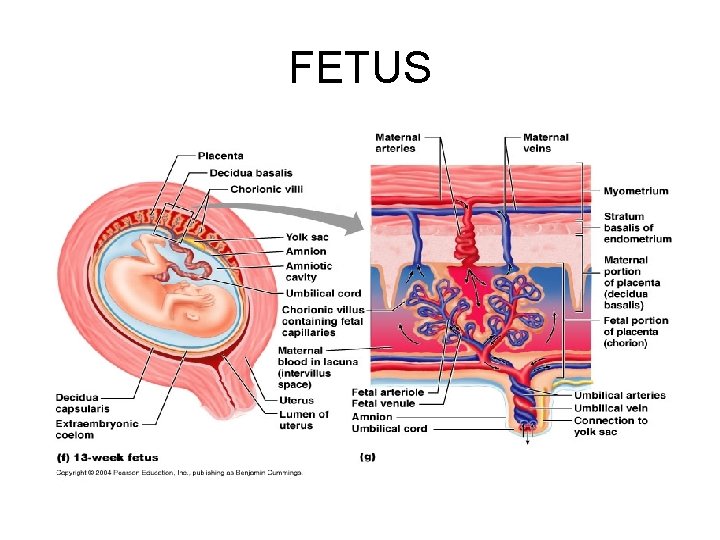
Placentation • Is the formation of the placenta: – Temporary organ that originates from both embryonic (trophoblastic) and maternal (endometrical) tissues – The process of proliferation of the trophoblast gives rise to a layer of extraembryonic mesoderm on its inner surface that becomes the chorion (b)
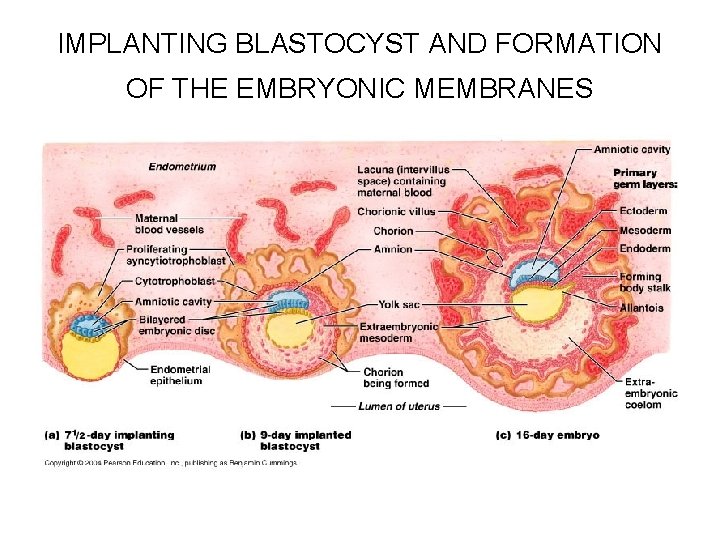
IMPLANTING BLASTOCYST AND FORMATION OF THE EMBRYONIC MEMBRANES
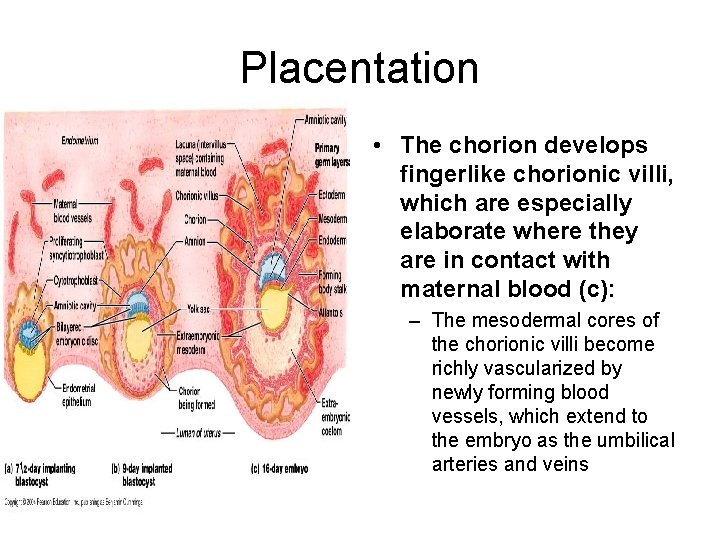
Placentation • The chorion develops fingerlike chorionic villi, which are especially elaborate where they are in contact with maternal blood (c): – The mesodermal cores of the chorionic villi become richly vascularized by newly forming blood vessels, which extend to the embryo as the umbilical arteries and veins
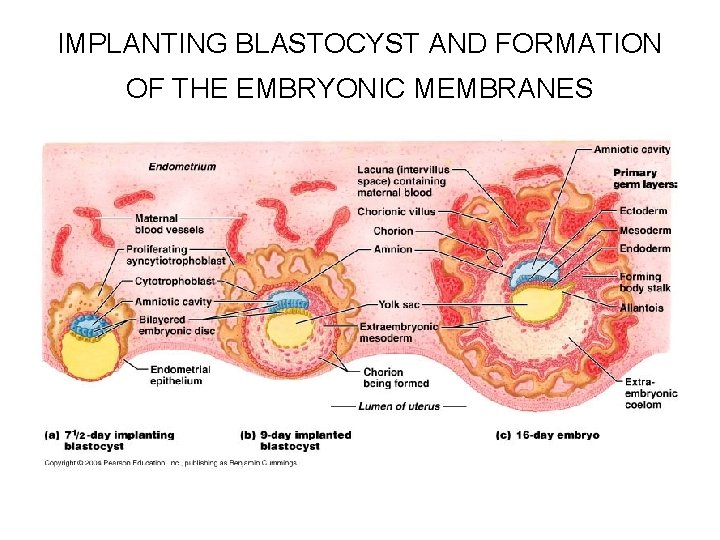
IMPLANTING BLASTOCYST AND FORMATION OF THE EMBRYONIC MEMBRANES
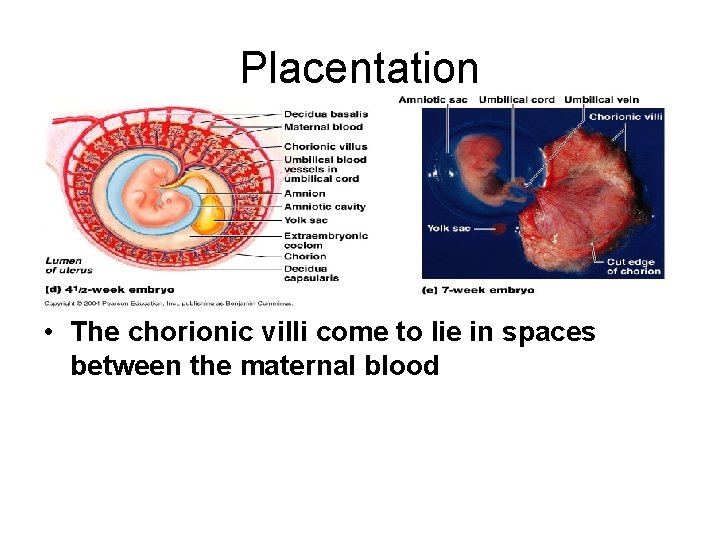
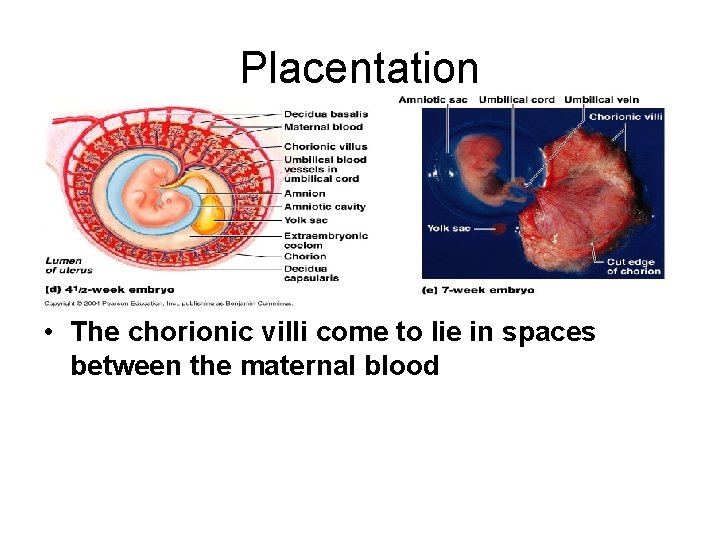
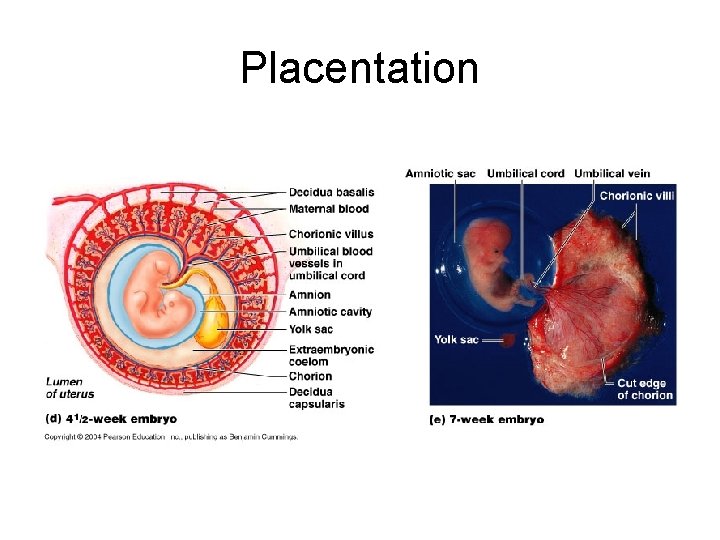
Placentation • The chorionic villi come to lie in spaces between the maternal blood
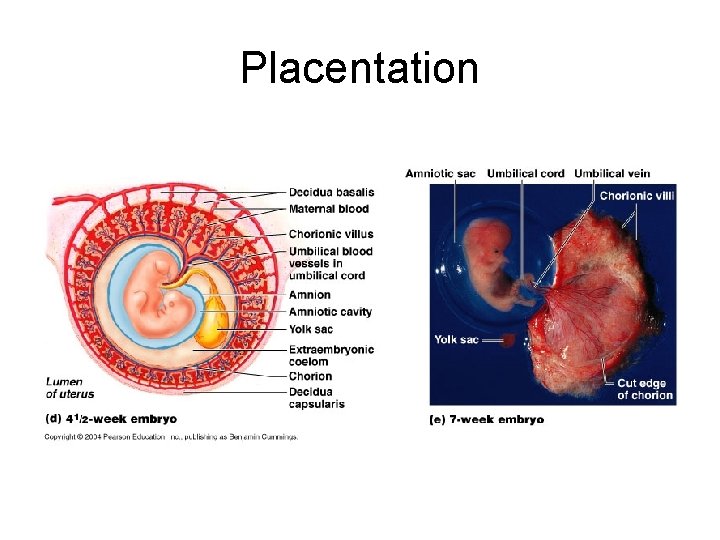
Placentation
Placentation

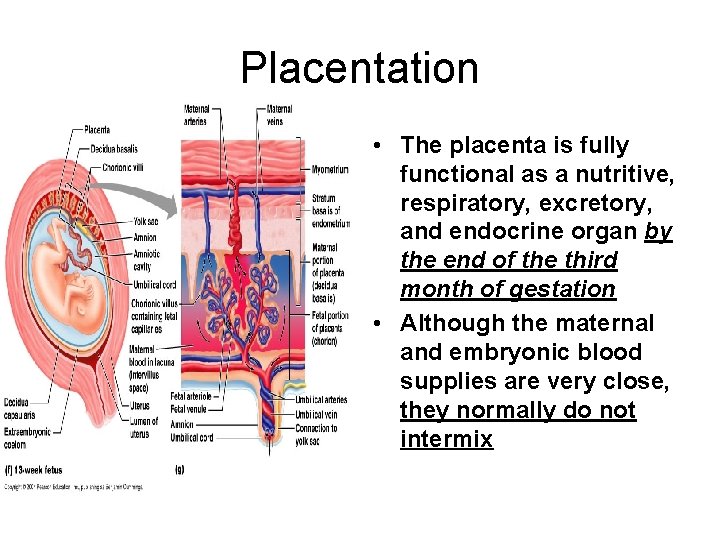
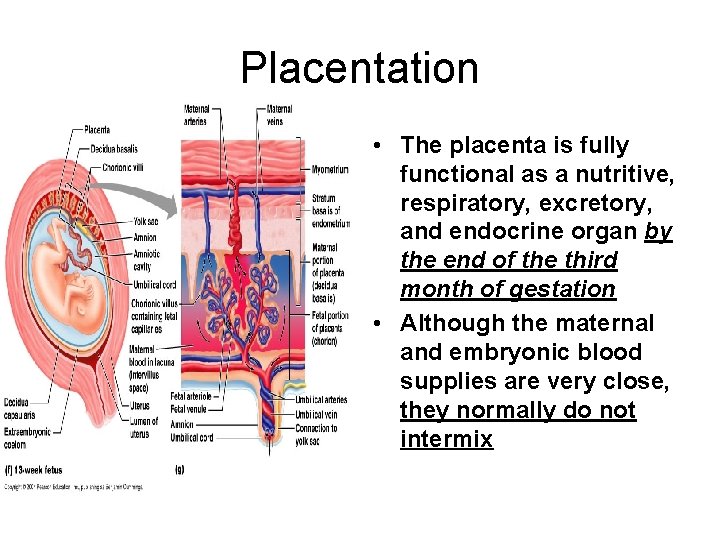
Placentation • The placenta is fully functional as a nutritive, respiratory, excretory, and endocrine organ by the end of the third month of gestation • Although the maternal and embryonic blood supplies are very close, they normally do not intermix

Placentation • Throughout pregnancy, blood levels of estrogens and progesterone continue to increase, encouraging growth and further differentiation of the mammary glands and readying them for lactation • The placenta also produces other hormones, such as human placental lactogen, human chorionic thyrotropin, and relaxin
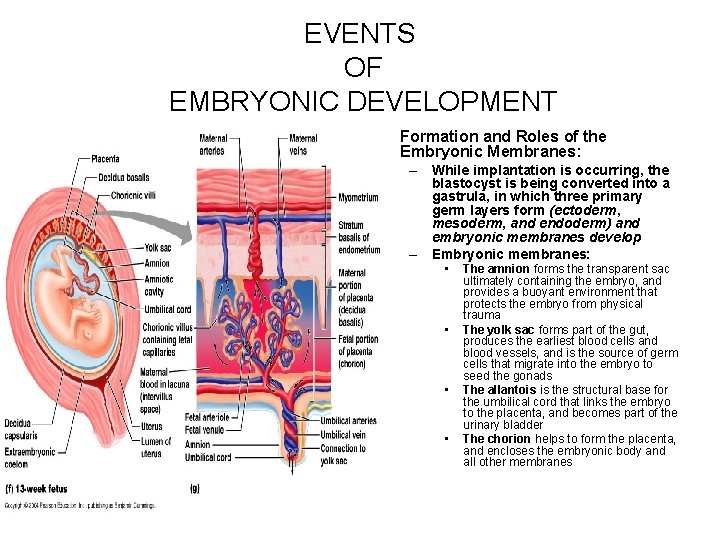
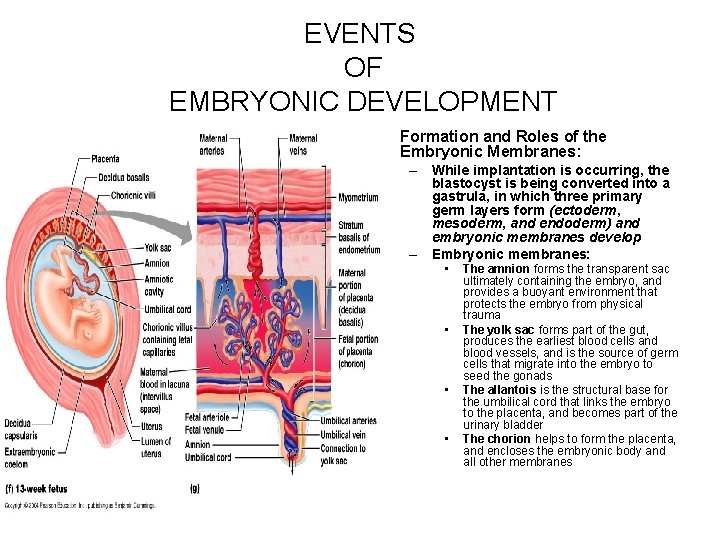
EVENTS OF EMBRYONIC DEVELOPMENT • Formation and Roles of the Embryonic Membranes: – While implantation is occurring, the blastocyst is being converted into a gastrula, in which three primary germ layers form (ectoderm, mesoderm, and endoderm) and embryonic membranes develop – Embryonic membranes: • • The amnion forms the transparent sac ultimately containing the embryo, and provides a buoyant environment that protects the embryo from physical trauma The yolk sac forms part of the gut, produces the earliest blood cells and blood vessels, and is the source of germ cells that migrate into the embryo to seed the gonads The allantois is the structural base for the umbilical cord that links the embryo to the placenta, and becomes part of the urinary bladder The chorion helps to form the placenta, and encloses the embryonic body and all other membranes
Placentation

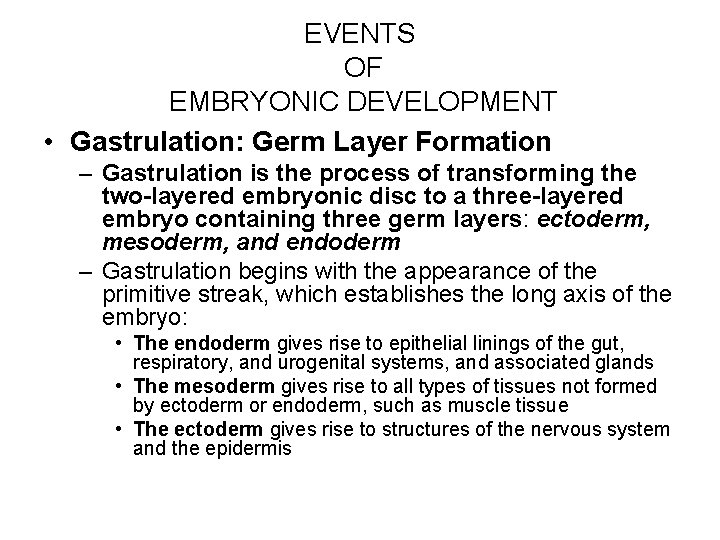
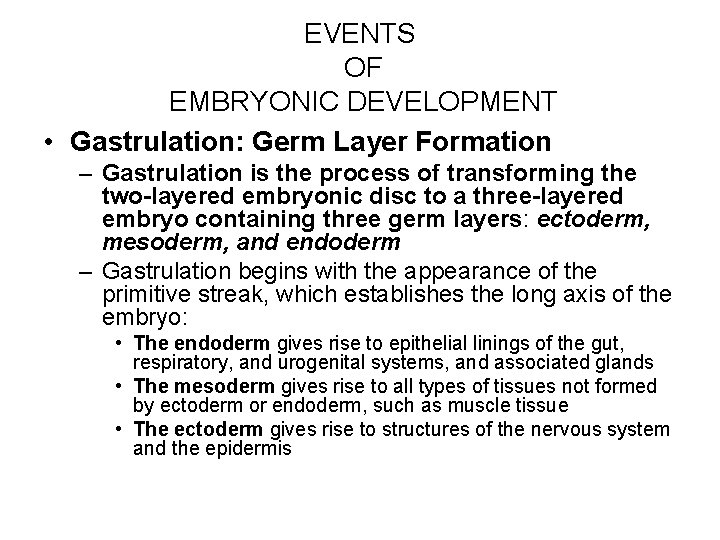
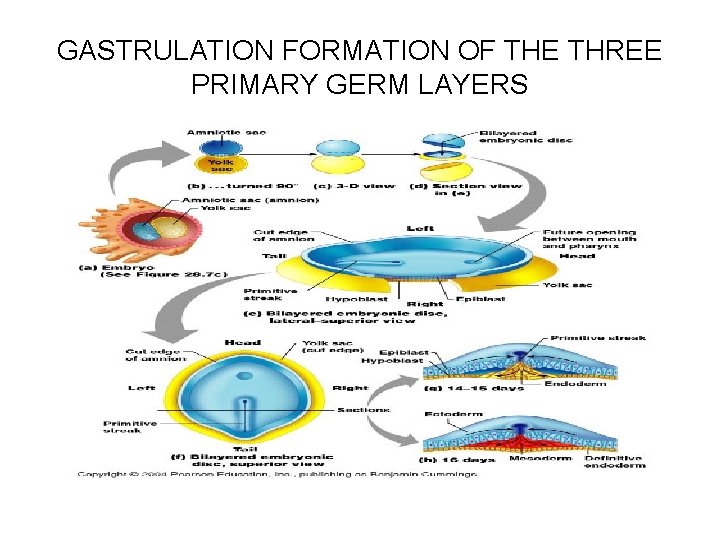
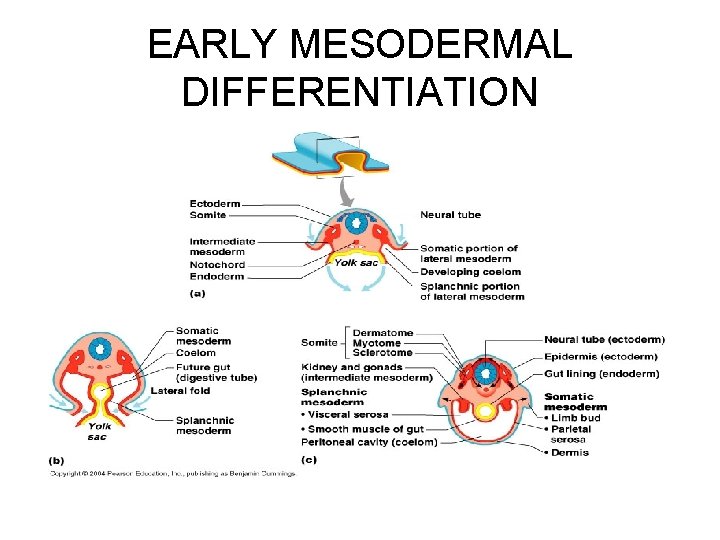
EVENTS OF EMBRYONIC DEVELOPMENT • Gastrulation: Germ Layer Formation – Gastrulation is the process of transforming the two-layered embryonic disc to a three-layered embryo containing three germ layers: ectoderm, mesoderm, and endoderm – Gastrulation begins with the appearance of the primitive streak, which establishes the long axis of the embryo: • The endoderm gives rise to epithelial linings of the gut, respiratory, and urogenital systems, and associated glands • The mesoderm gives rise to all types of tissues not formed by ectoderm or endoderm, such as muscle tissue • The ectoderm gives rise to structures of the nervous system and the epidermis
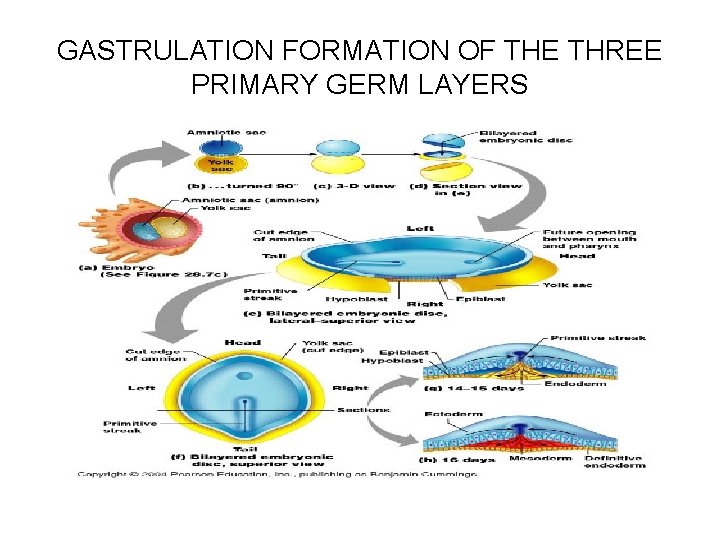
GASTRULATION FORMATION OF THE THREE PRIMARY GERM LAYERS

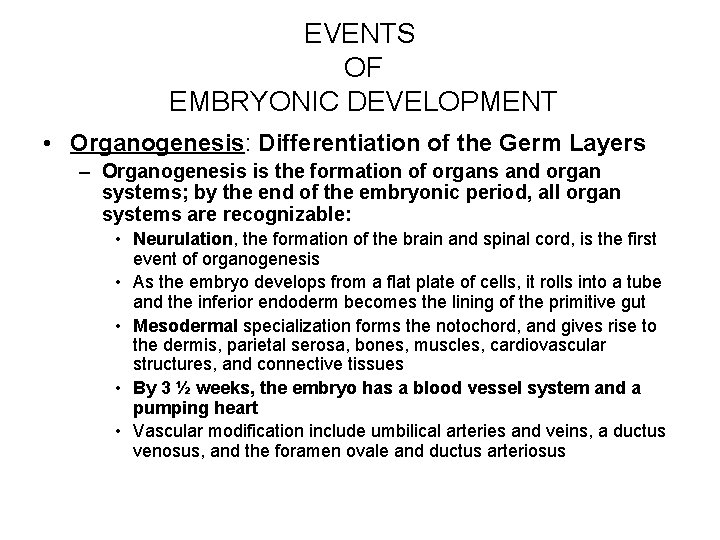
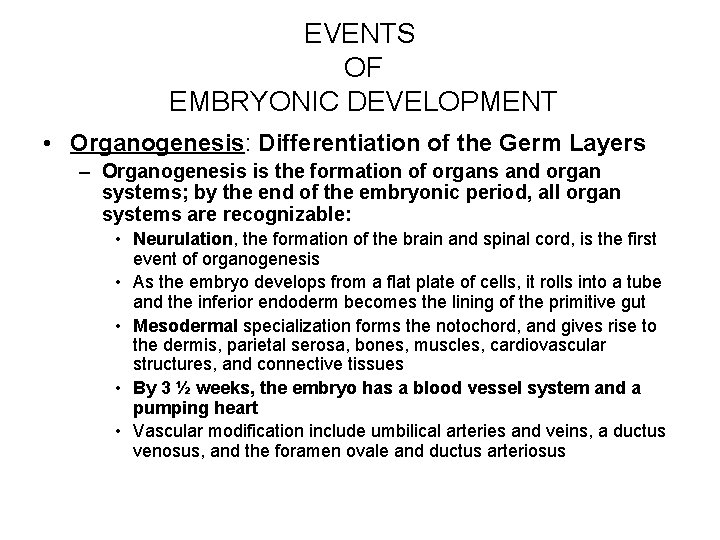
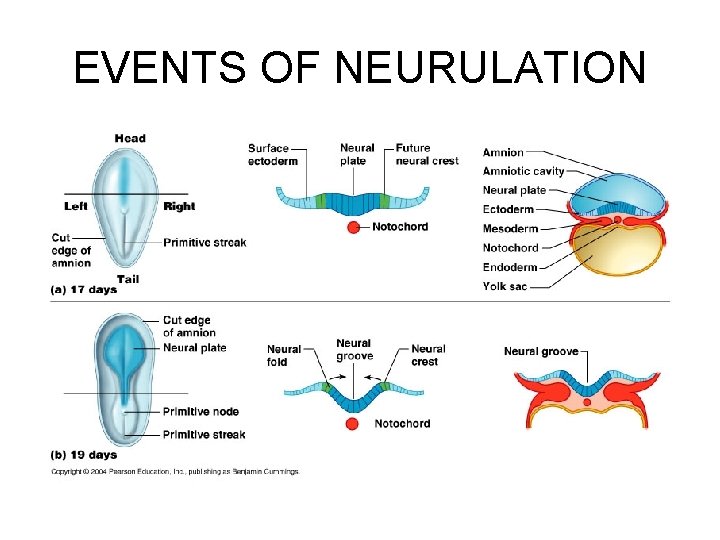
EVENTS OF EMBRYONIC DEVELOPMENT • Organogenesis: Differentiation of the Germ Layers – Organogenesis is the formation of organs and organ systems; by the end of the embryonic period, all organ systems are recognizable: • Neurulation, the formation of the brain and spinal cord, is the first event of organogenesis • As the embryo develops from a flat plate of cells, it rolls into a tube and the inferior endoderm becomes the lining of the primitive gut • Mesodermal specialization forms the notochord, and gives rise to the dermis, parietal serosa, bones, muscles, cardiovascular structures, and connective tissues • By 3 ½ weeks, the embryo has a blood vessel system and a pumping heart • Vascular modification include umbilical arteries and veins, a ductus venosus, and the foramen ovale and ductus arteriosus
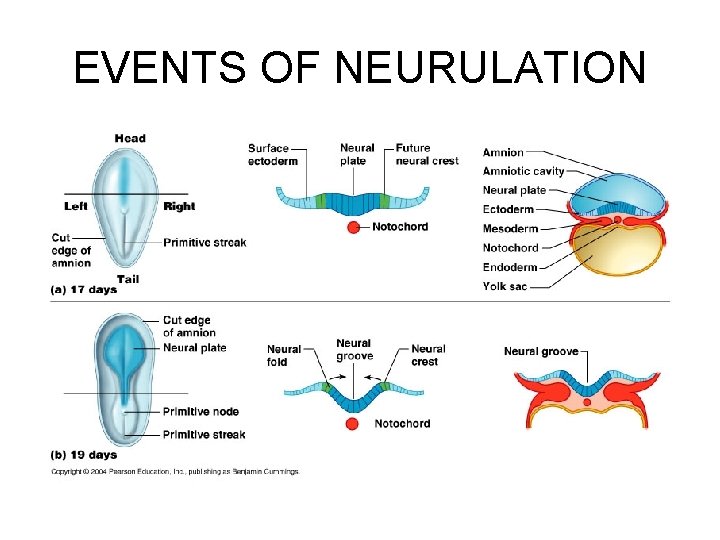
EVENTS OF NEURULATION

EVENTS OF NEURULATION

FOLDING OF THE EMBRYONIC BODY
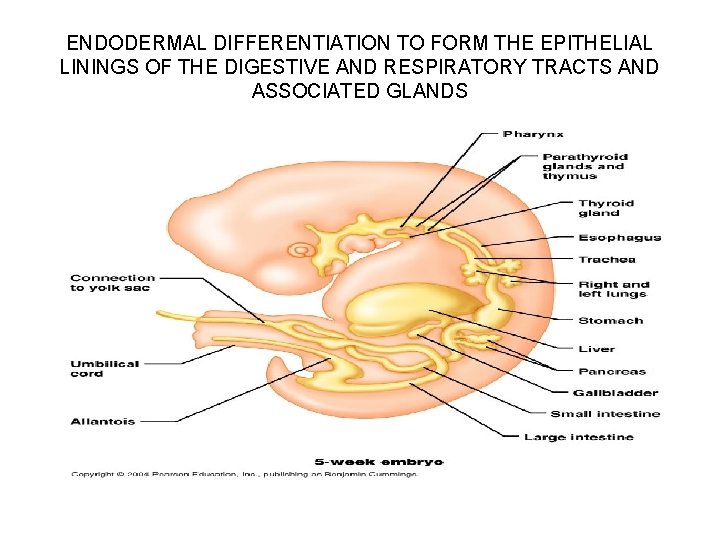
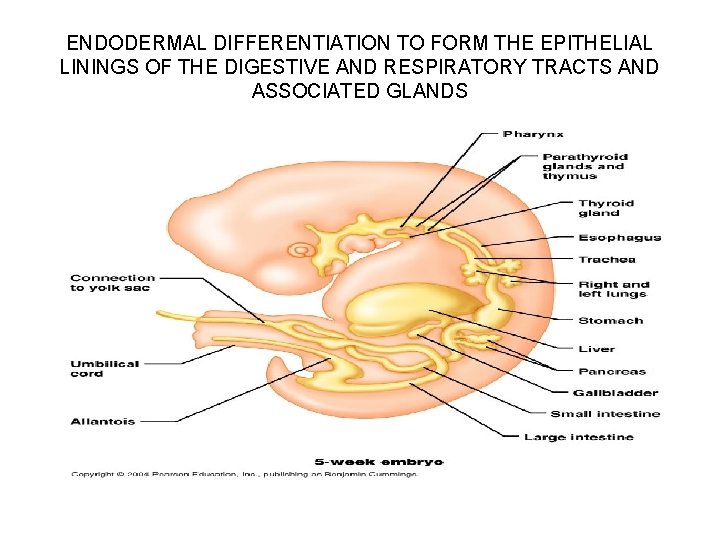
ENDODERMAL DIFFERENTIATION TO FORM THE EPITHELIAL LININGS OF THE DIGESTIVE AND RESPIRATORY TRACTS AND ASSOCIATED GLANDS
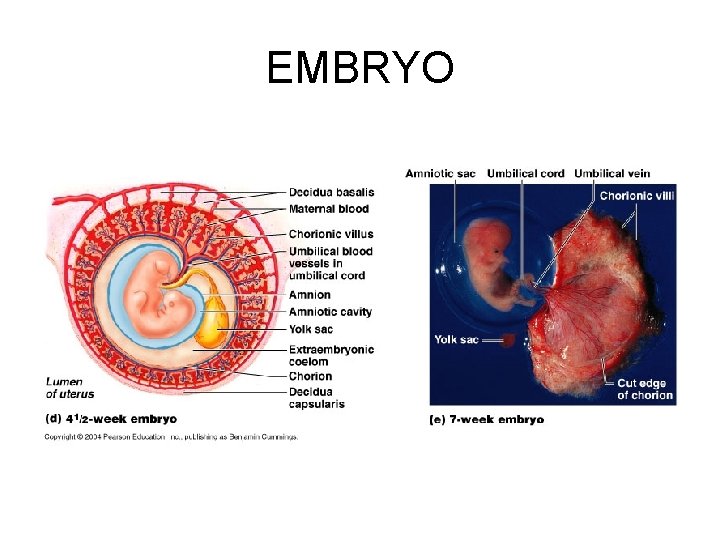
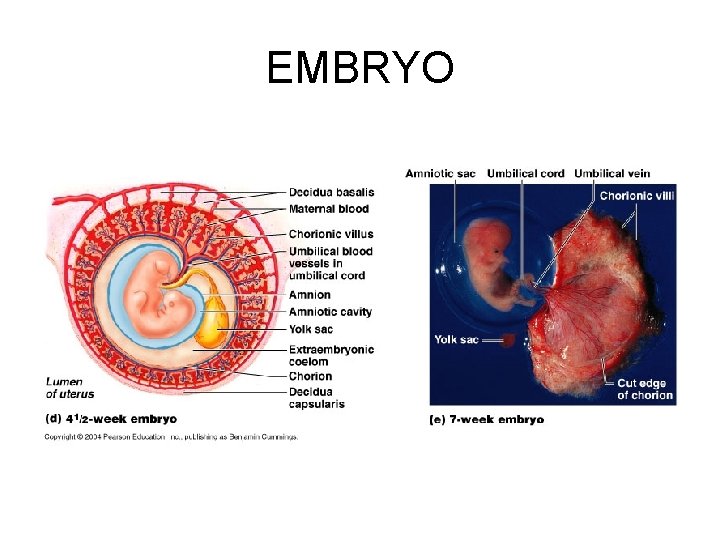
EMBRYO
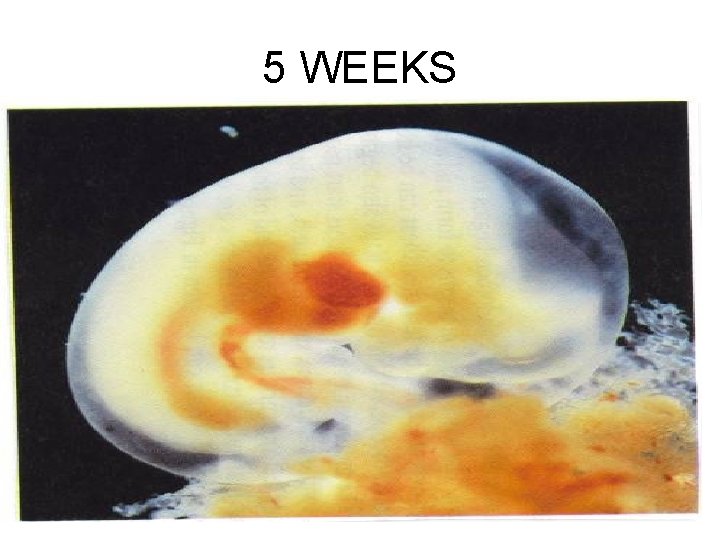
5 WEEKS
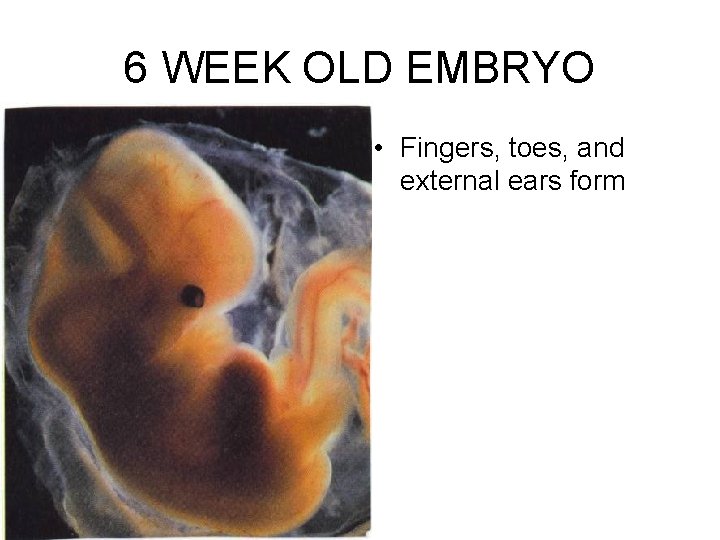
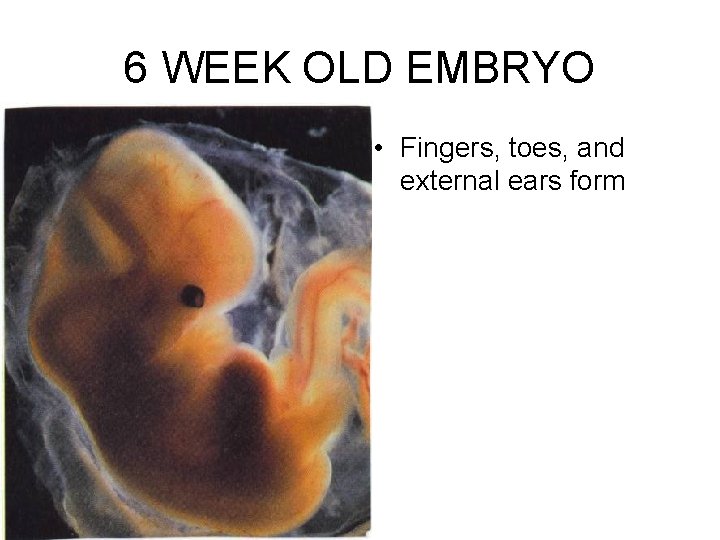
6 WEEK OLD EMBRYO • Fingers, toes, and external ears form

7 WEEK OLD EMBRYO • HANDS AND FEET

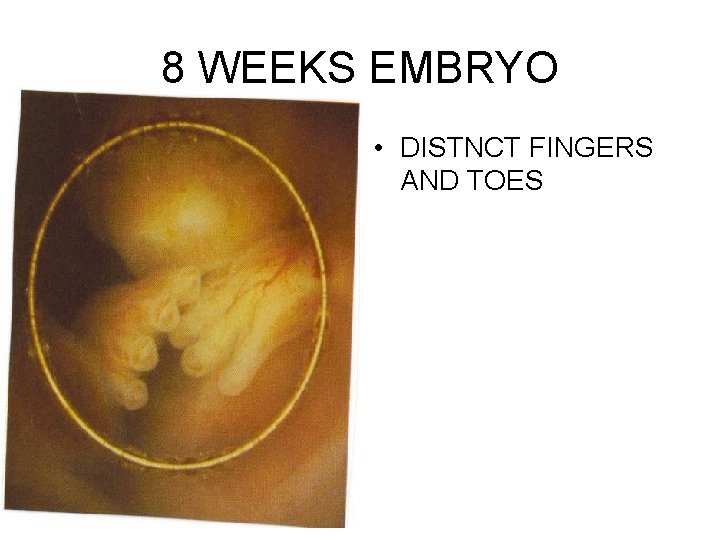
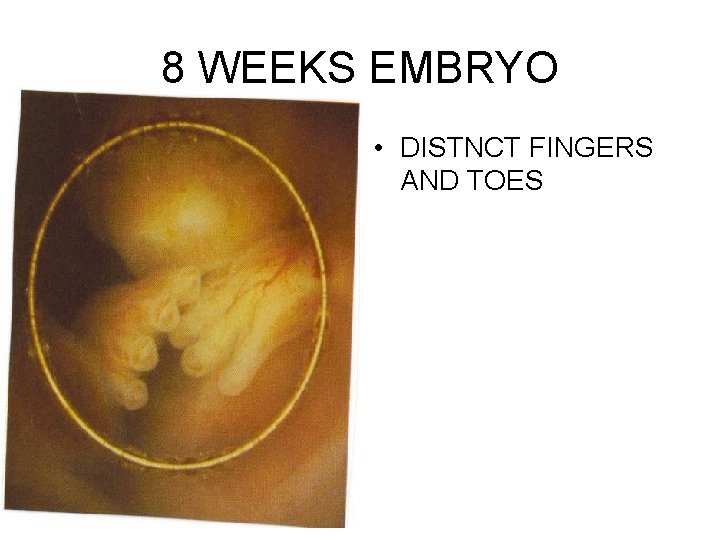
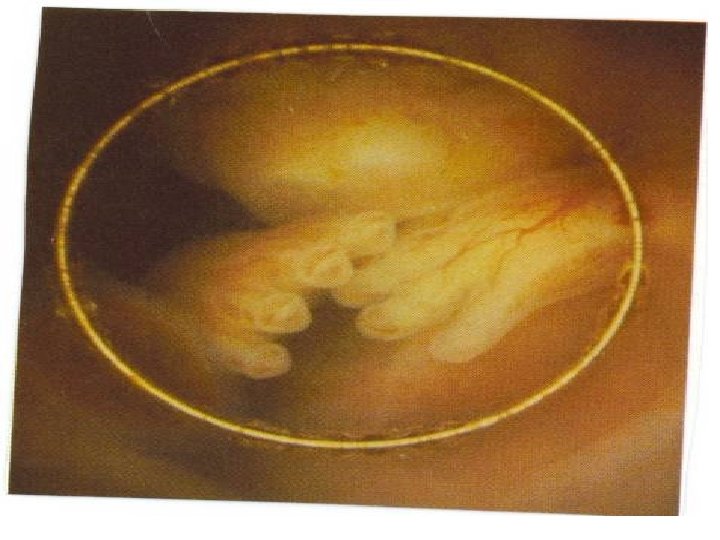
8 WEEKS EMBRYO • DISTNCT FINGERS AND TOES
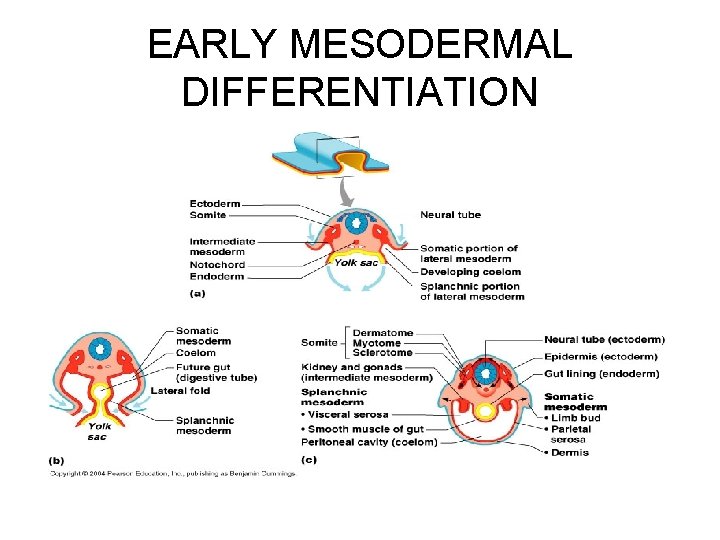
EARLY MESODERMAL DIFFERENTIATION
EVENTS OF FETAL DEVELOPMENT • The fetal period extends from weeks 938, and is a time of rapid growth of body structures established in the embryo • During the first half of the fetal period, cells are still differentiating into specific cell types to form the body’s distinctive tissues • TABLE 28. 2 page 1128
SECOND TRIMESTER • • Middle 3 months of pregnancy After 8 th week In beginning 5 cm Called Fetus Skeleton formed Soft hair grows over the skin Eyes open At end is 32 cm
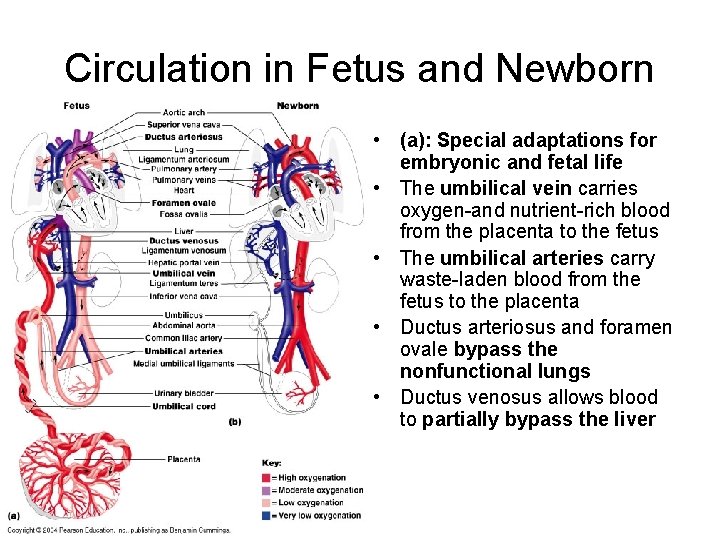
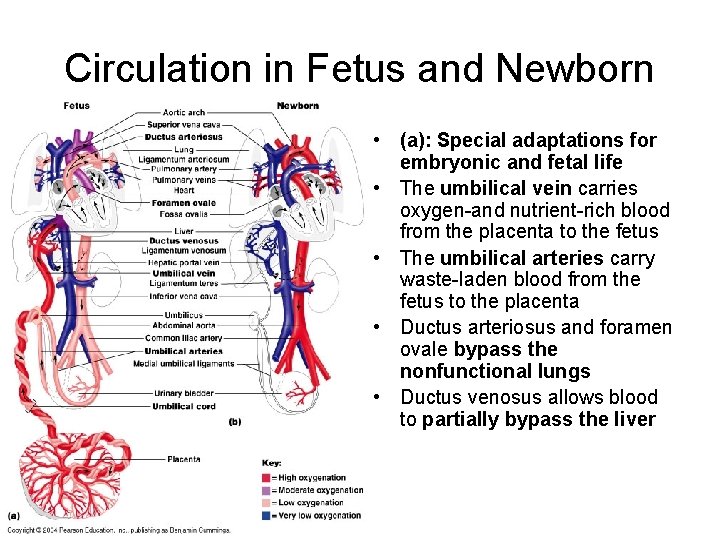
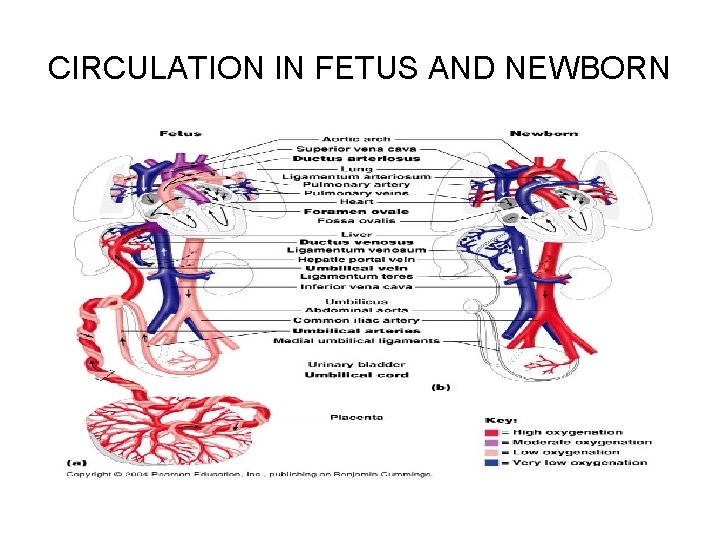
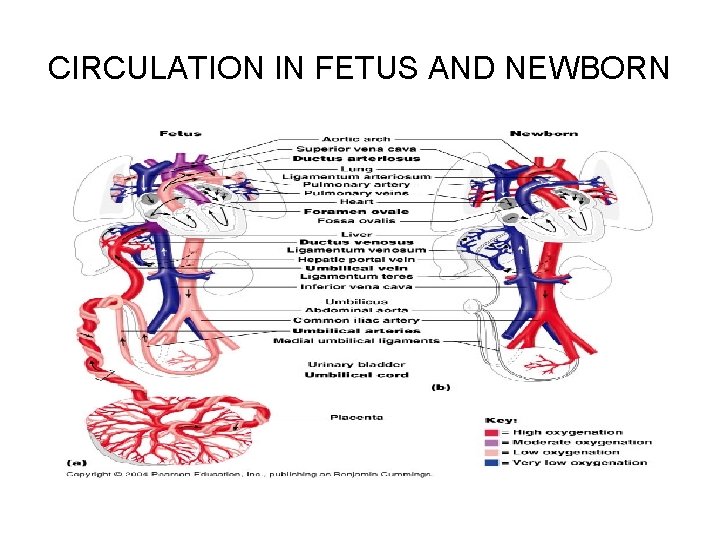
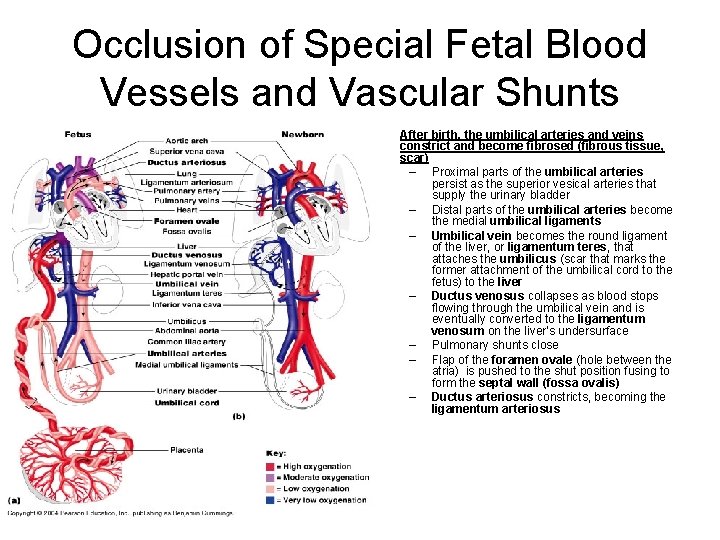
Circulation in Fetus and Newborn • (a): Special adaptations for embryonic and fetal life • The umbilical vein carries oxygen-and nutrient-rich blood from the placenta to the fetus • The umbilical arteries carry waste-laden blood from the fetus to the placenta • Ductus arteriosus and foramen ovale bypass the nonfunctional lungs • Ductus venosus allows blood to partially bypass the liver
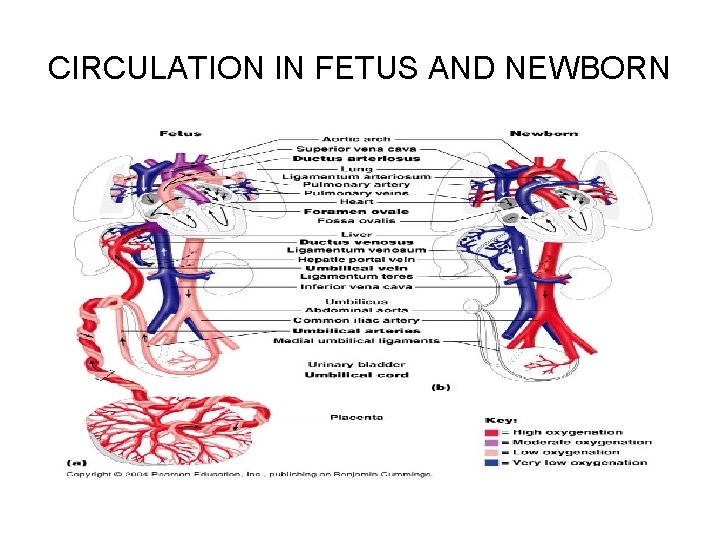
CIRCULATION IN FETUS AND NEWBORN
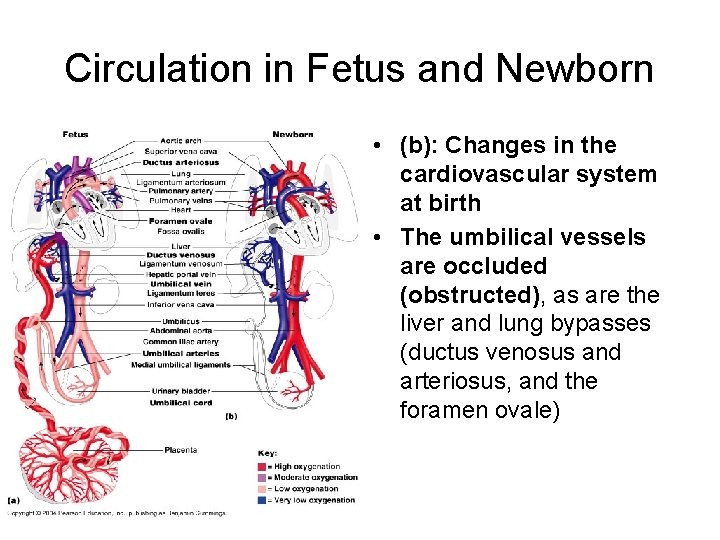
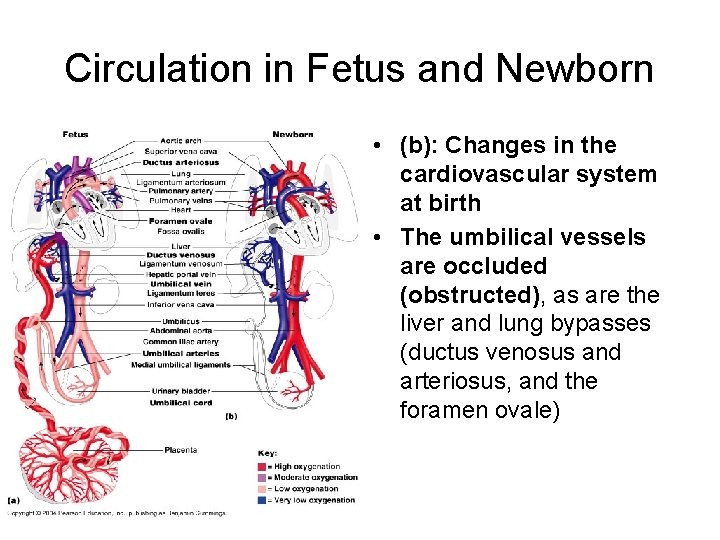
Circulation in Fetus and Newborn • (b): Changes in the cardiovascular system at birth • The umbilical vessels are occluded (obstructed), as are the liver and lung bypasses (ductus venosus and arteriosus, and the foramen ovale)
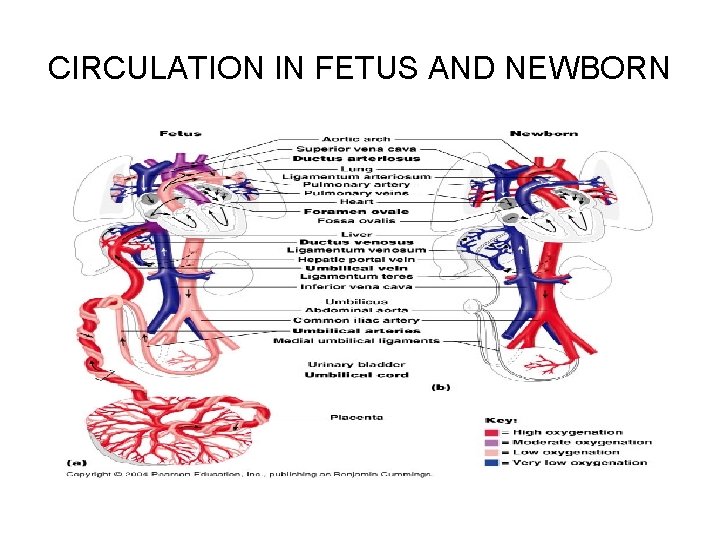
CIRCULATION IN FETUS AND NEWBORN

Events of Fetal Development • The main events of the fetal period—weeks 9 through 38—are listed in TABLE 28. 2 • Time of rapid growth of the body structures that were established in the embryo • First half of this period, differentiation is still continuing • Length (crown to rump): 30 mm (1 inch) to 360 mm (14 inches) – Total body length at birth is approximately 550 mm (22 inches) • Weight of approximately: 2 g (0. 06 ounce) to 2. 74. 1 Kg (6 -10 ponds)
FETUS
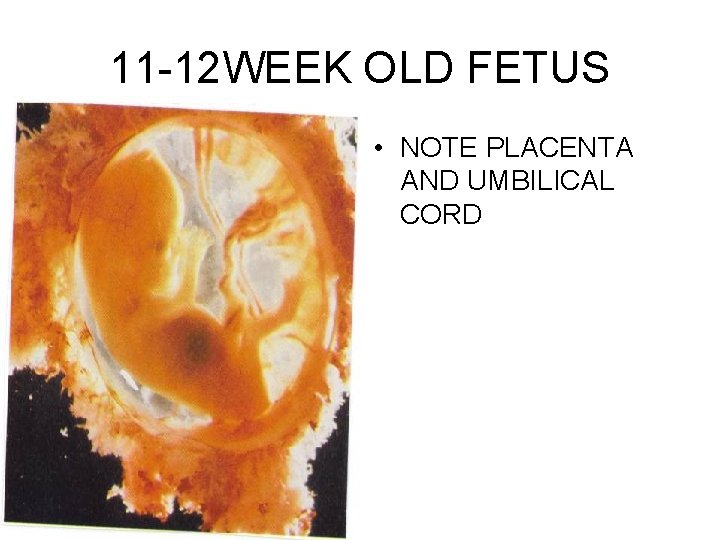
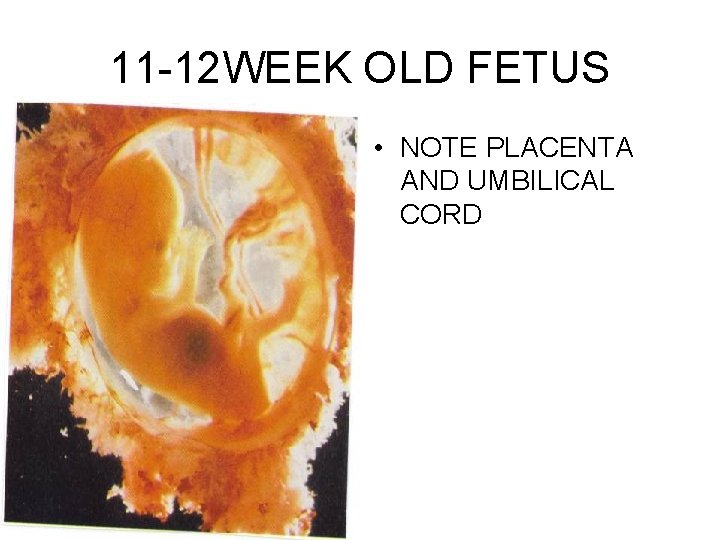
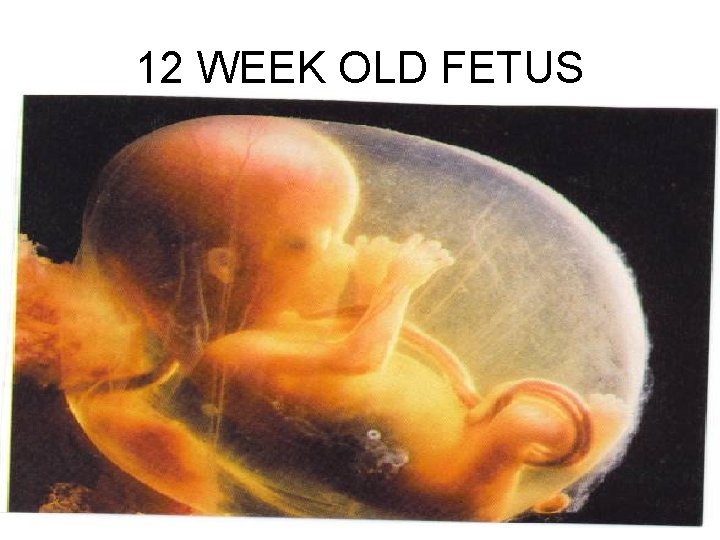
11 -12 WEEK OLD FETUS • NOTE PLACENTA AND UMBILICAL CORD

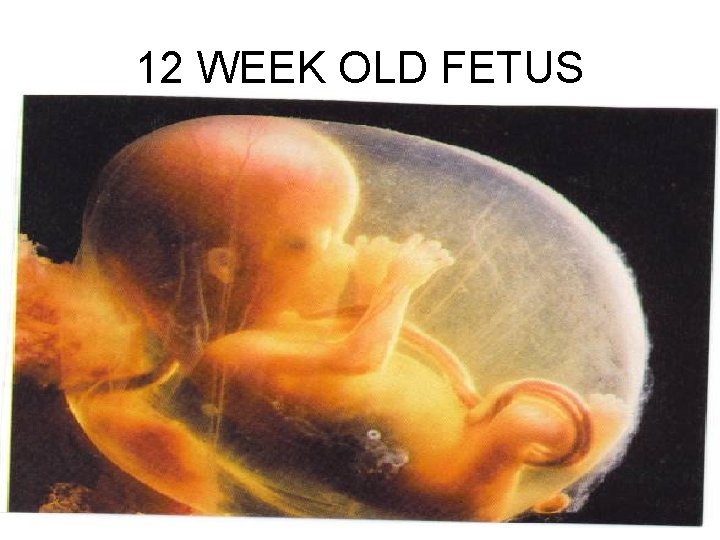
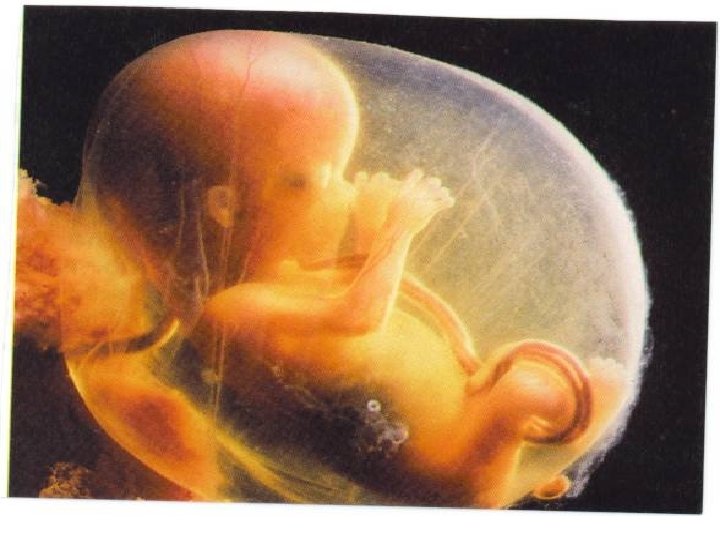
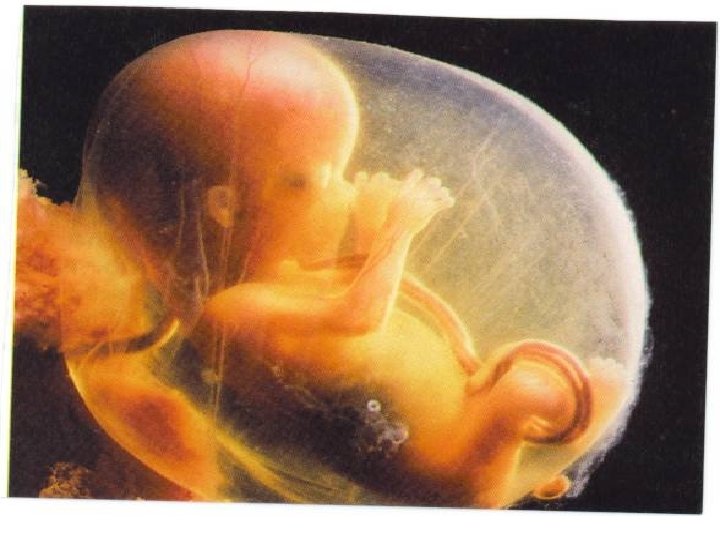
12 WEEK OLD FETUS
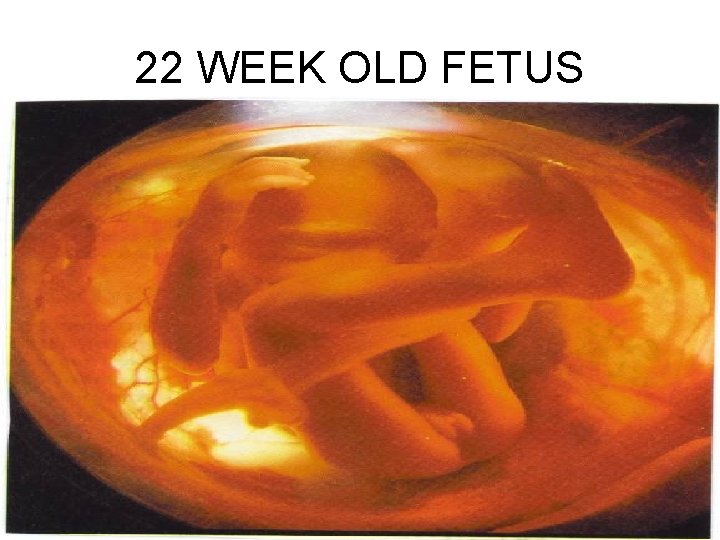
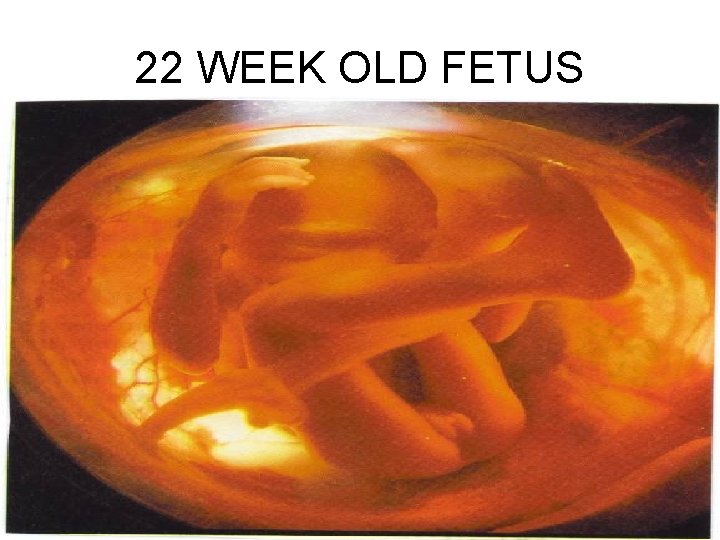
22 WEEK OLD FETUS

THIRD TRIMESTER • Final 3 months of pregnancy • Fetus becoming modified to survive in the outside world • Grows in size and weight

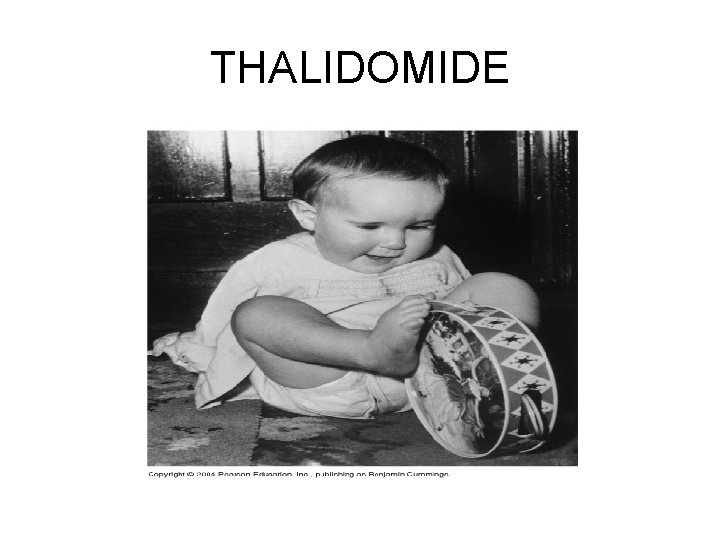
HOMEOSTATIC IMBALANCE • Because many potentially harmful substances can cross placental barriers and enter the fetal blood, a pregnant woman should be aware of what she is taking into her body, particularly during the embryonic period when the body’s foundations are laid down • Teratogens: factors that may cause severe congenital abnormalities or even fetal death include: – Alcohol: fetal alcohol syndrome (FAS) • Mental retardation, abnormal growth – Nicotine: hinders oxygen delivery to the fetus • Impairs normal growth and development – Anticoagulants – Sedatives: thalidomide (alleviated morning sickness) • If taken during days 26 -56 – Deformed infants with short flipperlike limbs – Antihypertensives – Some antibiotics – Maternal infections (German Measles)
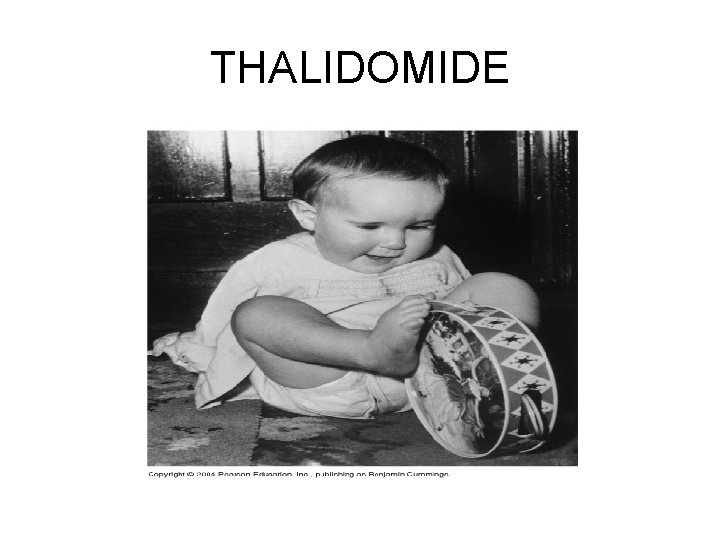
THALIDOMIDE
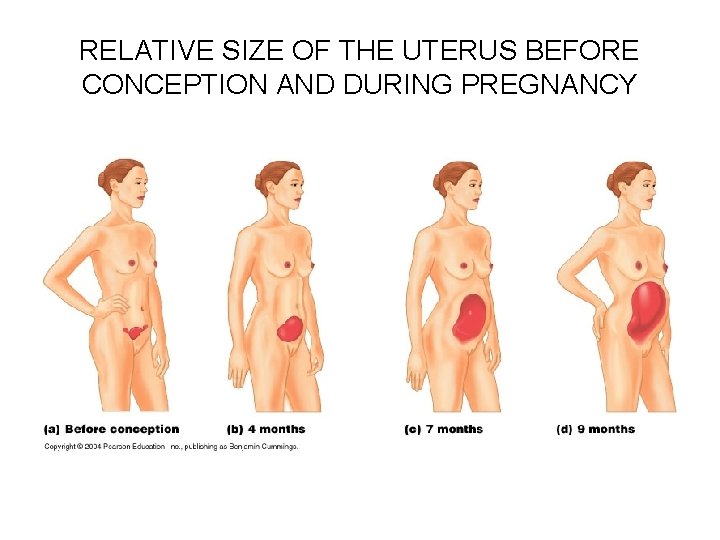
EFFECTS OF PREGNANCY ON THE MOTHER • Anatomical Changes: – The female reproductive organs and breasts become increasingly vascular and engorged with blood – The uterus enlarges dramatically, causing a shift in the woman’s center of gravity and an accentuated lumbar curvature (lordosis) – Placental production of the hormone relaxin causes pelvic ligaments and the pubic symphysis to soften and relax • This increases motility for easier birth passage – There is a normal weight gain of around 28 pounds, due to growth of the fetus, maternal reproductive organs, and breasts, and increased blood volume
EFFECTS OF PREGNANCY ON THE MOTHER • Good nutrition is necessary all through pregnancy if the developing fetus is to have all the building materials (especially proteins, calcium, and iron) needed to form its tissues • Multivitamins containing folic acid seem to reduce the risk of having babies with neurological problems, including such birth defects as spina bifida and anencephaly (absence of brain and cranial vault with cerebral hemisphere missing or reduced in size)
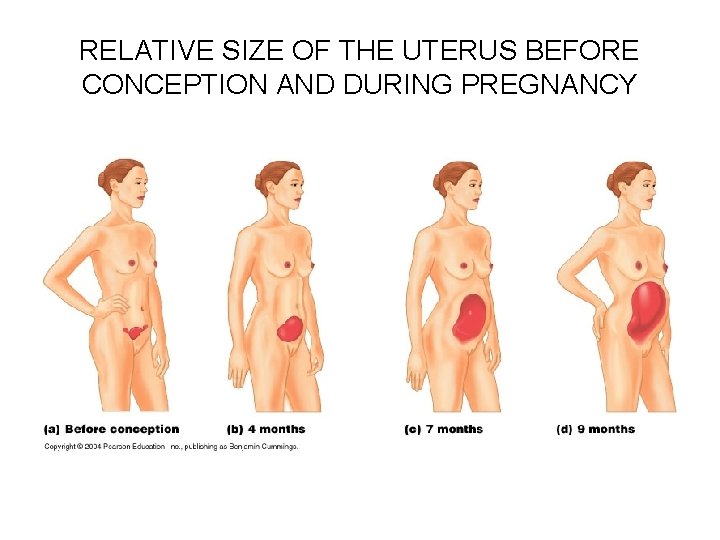
RELATIVE SIZE OF THE UTERUS BEFORE CONCEPTION AND DURING PREGNANCY
EFFECTS OF PREGNANCY ON THE MOTHER • Metabolic Changes: – As the placenta enlarges, it produces human placental lactogen, which works with estrogen and progesterone to promote maturation of the breasts for lactation – Human placental lactogen (h. PL) also promotes the growth of the fetus, and exerts a glucose-sparing effect on maternal metabolism • Consequently, maternal cells metabolize more fatty acids and less glucose than usual, sparing glucose for use by the fetus – Human chorionic thyrotropin from the placenta increases maternal metabolic rate
EFFECTS OF PREGNANCY ON THE MOTHER • Physiological Changes: – Many women suffer morning sickness during the first few months of pregnancy, until their systems adapt to elevated levels of estrogen and progesterone – Heartburn often results from the displacement of the esophagus (uterus pushing on body organs), and constipation may result due to the decreased motility of the digestive tract – The kidneys produce more urine, since there is additional fetal metabolic waste • Increased urination frequency due to uterus pressing on urinary bladder – Vital capacity and respiratory rate increases, but there is a decrease in residual volume, and many women suffer from difficult breathing, or dyspnea – Blood volume increases to accommodate the needs of the fetus, so blood pressure and heart rate rise, increasing cardiac output

PARTURITION (BIRTH) • Parturition is the process of giving birth, and usually occurs within 15 days of the calculated due date, which is 280 days from the last menstrual period
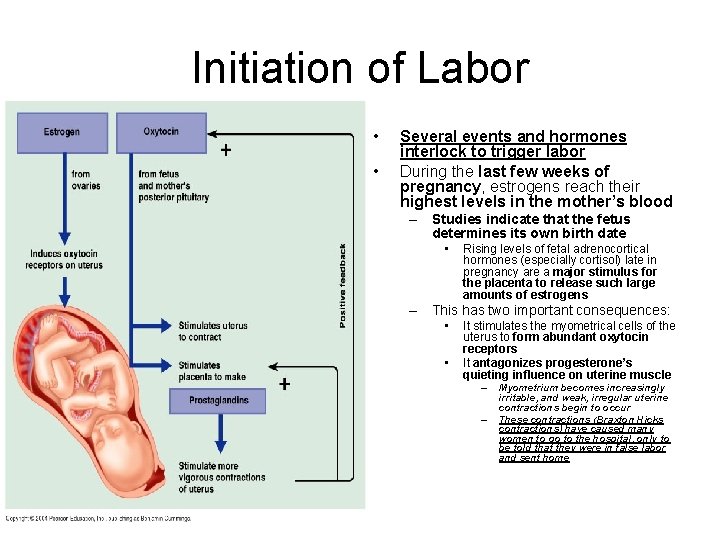
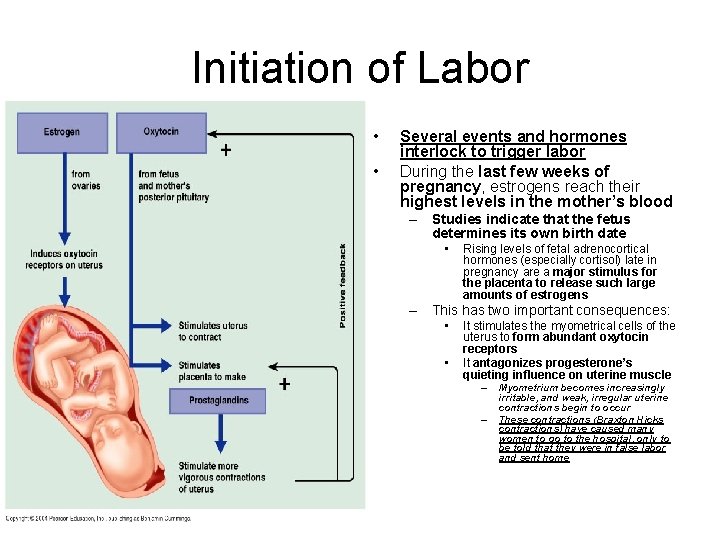
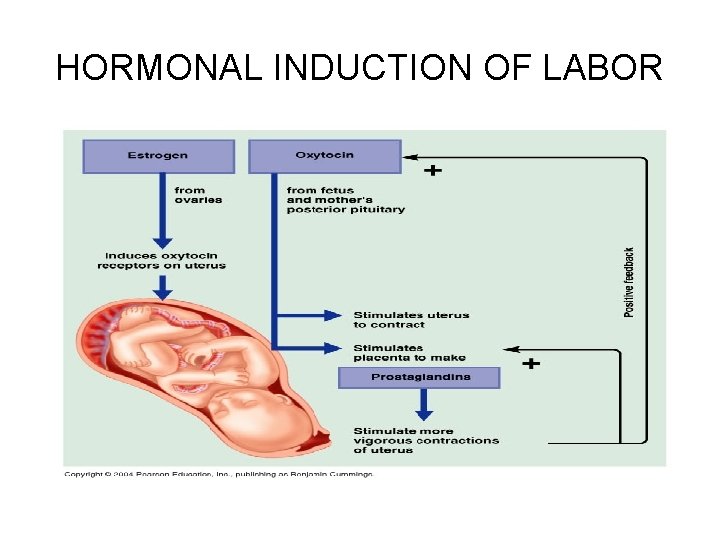
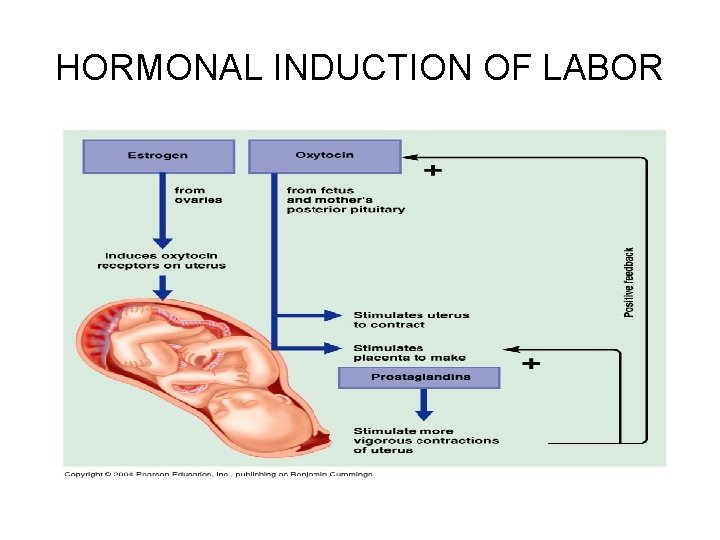
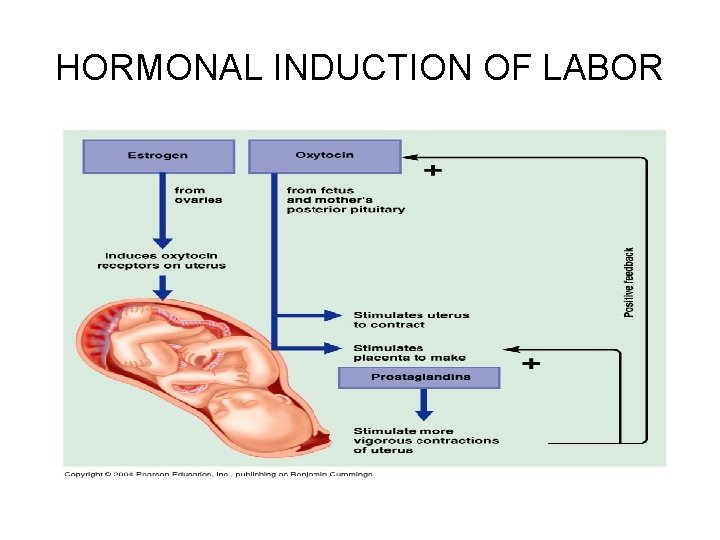
Initiation of Labor • • Several events and hormones interlock to trigger labor During the last few weeks of pregnancy, estrogens reach their highest levels in the mother’s blood – Studies indicate that the fetus determines its own birth date • Rising levels of fetal adrenocortical hormones (especially cortisol) late in pregnancy are a major stimulus for the placenta to release such large amounts of estrogens – This has two important consequences: • • It stimulates the myometrical cells of the uterus to form abundant oxytocin receptors It antagonizes progesterone’s quieting influence on uterine muscle – – Myometrium becomes increasingly irritable, and weak, irregular uterine contractions begin to occur These contractions (Braxton Hicks contractions) have caused many women to go to the hospital, only to be told that they were in false labor and sent home
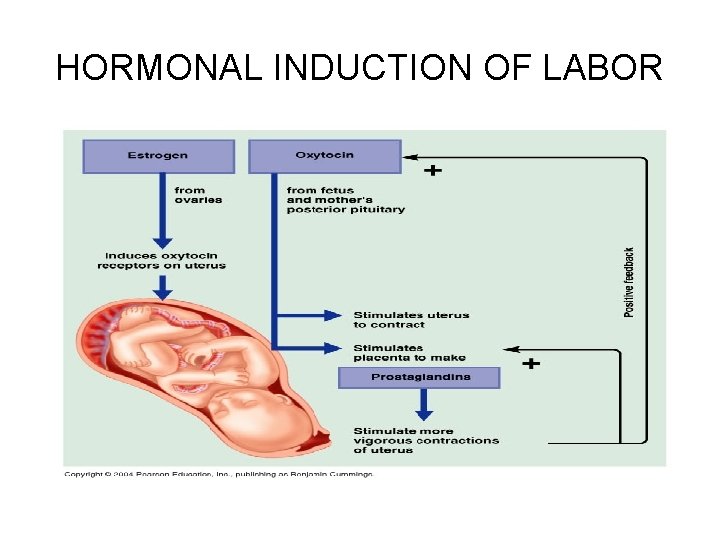
HORMONAL INDUCTION OF LABOR
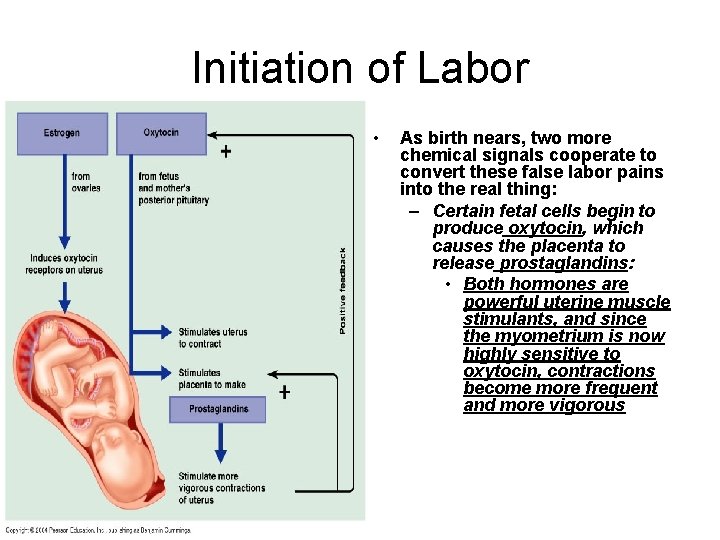
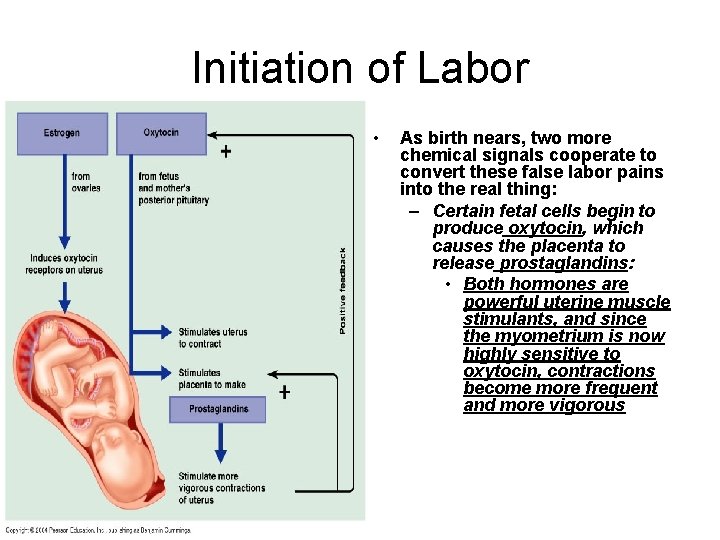
Initiation of Labor • As birth nears, two more chemical signals cooperate to convert these false labor pains into the real thing: – Certain fetal cells begin to produce oxytocin, which causes the placenta to release prostaglandins: • Both hormones are powerful uterine muscle stimulants, and since the myometrium is now highly sensitive to oxytocin, contractions become more frequent and more vigorous
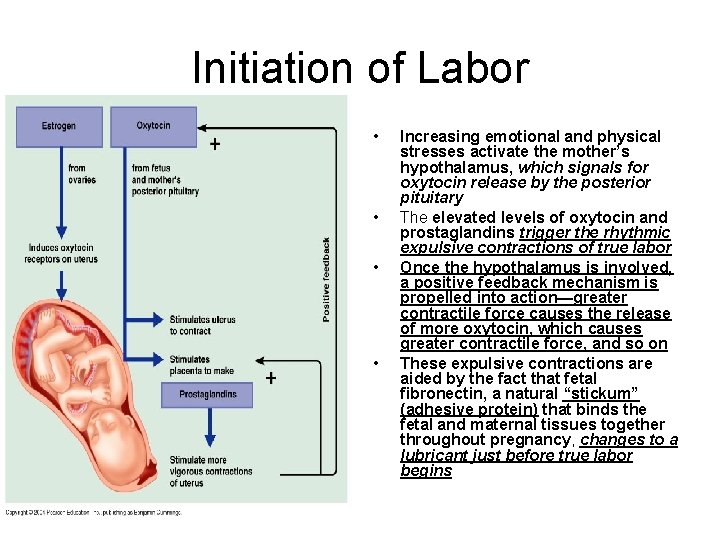
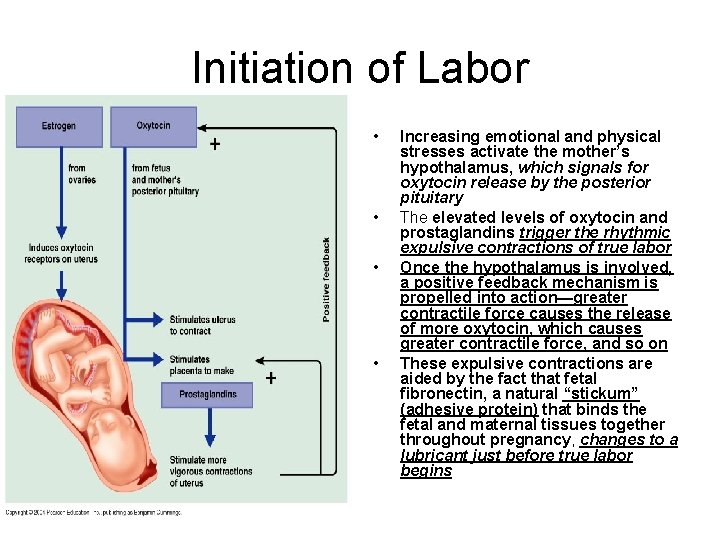
Initiation of Labor • • Increasing emotional and physical stresses activate the mother’s hypothalamus, which signals for oxytocin release by the posterior pituitary The elevated levels of oxytocin and prostaglandins trigger the rhythmic expulsive contractions of true labor Once the hypothalamus is involved, a positive feedback mechanism is propelled into action—greater contractile force causes the release of more oxytocin, which causes greater contractile force, and so on These expulsive contractions are aided by the fact that fetal fibronectin, a natural “stickum” (adhesive protein) that binds the fetal and maternal tissues together throughout pregnancy, changes to a lubricant just before true labor begins

HORMONAL INDUCTION OF LABOR
Initiation of Labor • Both oxytocin and prostaglandins are essential for initiating labor in humans • Untimely spurts of oxytocin may provoke some instances of premature birth, and interfering with production of either of these hormones will hinder onset of labor – Example: • Antiprostaglandin drugs such as ibuprofen (antiinflammatory) can inhibit the early stages of labor and such drugs are used occasionally to prevent preterm births
HORMONAL INDUCTION OF LABOR
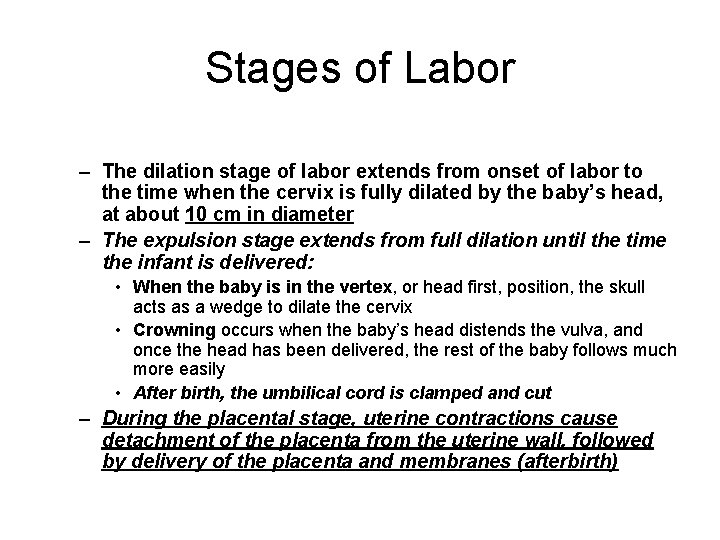
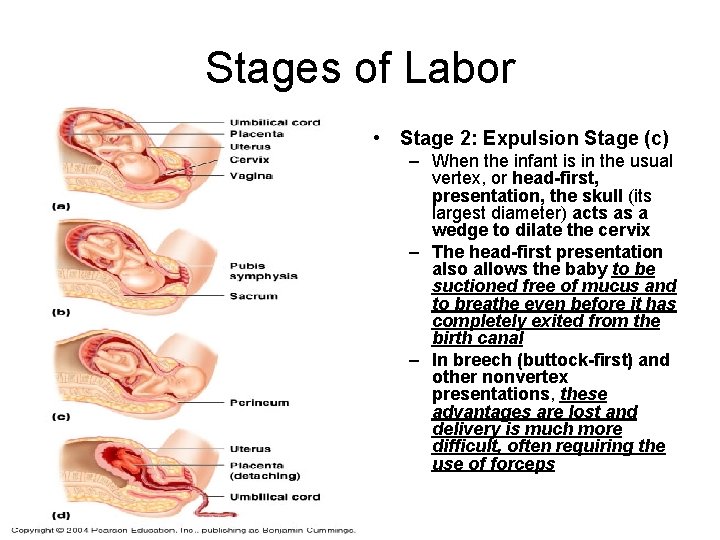
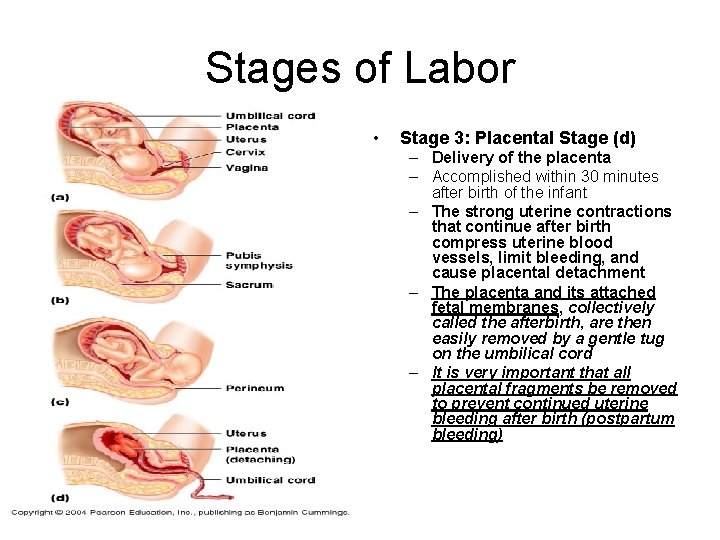
Stages of Labor – The dilation stage of labor extends from onset of labor to the time when the cervix is fully dilated by the baby’s head, at about 10 cm in diameter – The expulsion stage extends from full dilation until the time the infant is delivered: • When the baby is in the vertex, or head first, position, the skull acts as a wedge to dilate the cervix • Crowning occurs when the baby’s head distends the vulva, and once the head has been delivered, the rest of the baby follows much more easily • After birth, the umbilical cord is clamped and cut – During the placental stage, uterine contractions cause detachment of the placenta from the uterine wall, followed by delivery of the placenta and membranes (afterbirth)
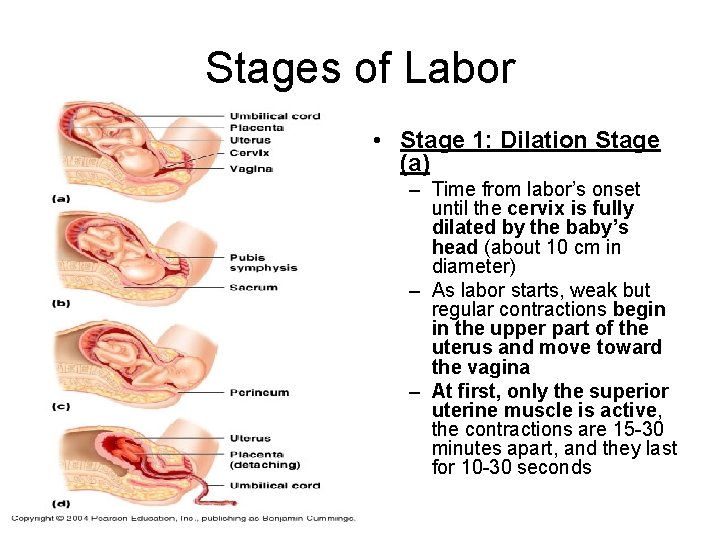
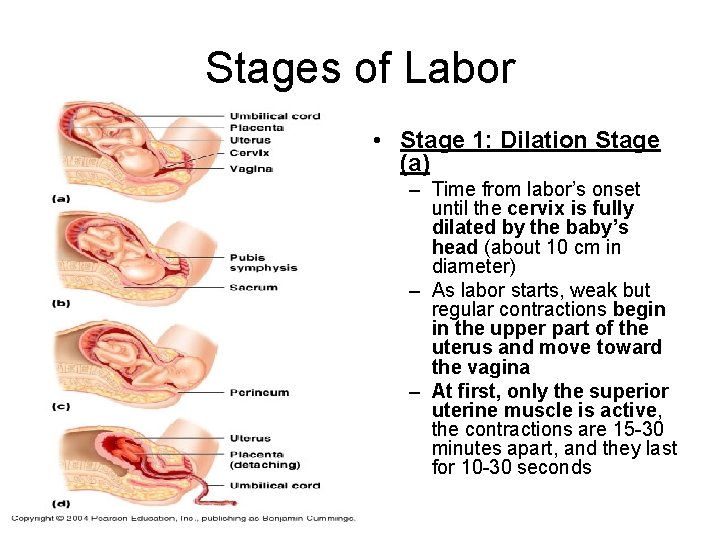
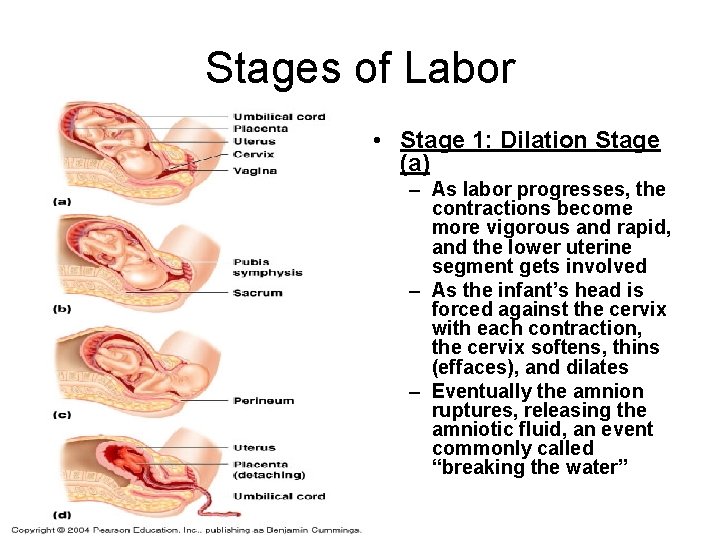
Stages of Labor • Stage 1: Dilation Stage (a) – Time from labor’s onset until the cervix is fully dilated by the baby’s head (about 10 cm in diameter) – As labor starts, weak but regular contractions begin in the upper part of the uterus and move toward the vagina – At first, only the superior uterine muscle is active, the contractions are 15 -30 minutes apart, and they last for 10 -30 seconds
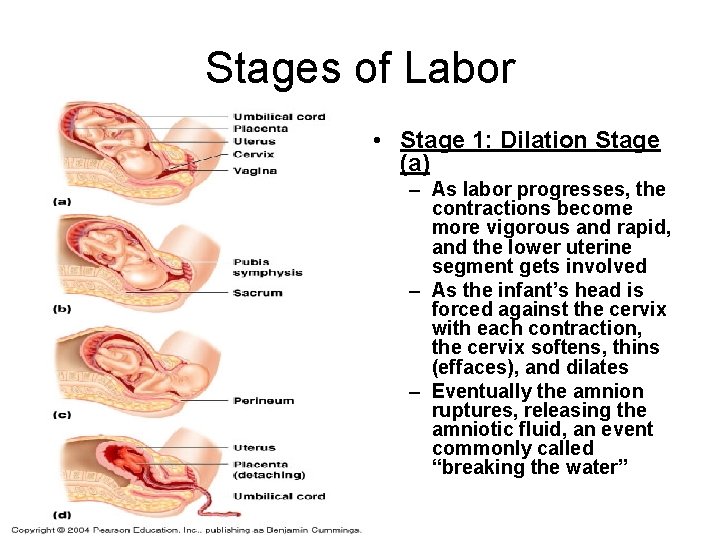
Stages of Labor • Stage 1: Dilation Stage (a) – As labor progresses, the contractions become more vigorous and rapid, and the lower uterine segment gets involved – As the infant’s head is forced against the cervix with each contraction, the cervix softens, thins (effaces), and dilates – Eventually the amnion ruptures, releasing the amniotic fluid, an event commonly called “breaking the water”
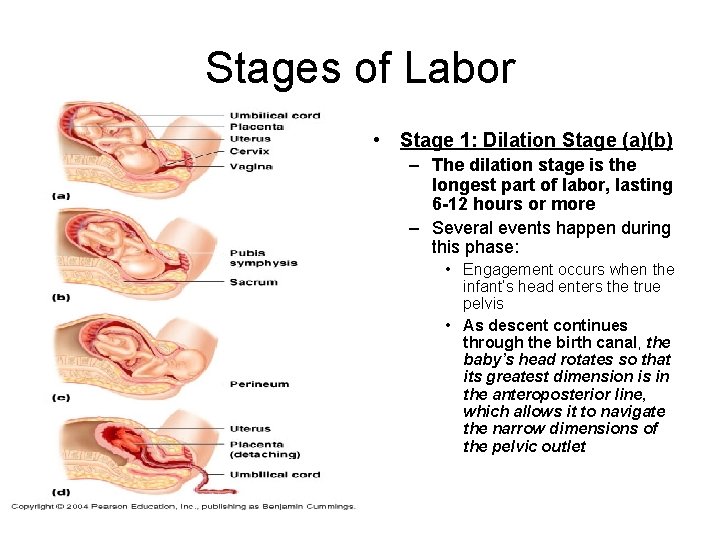
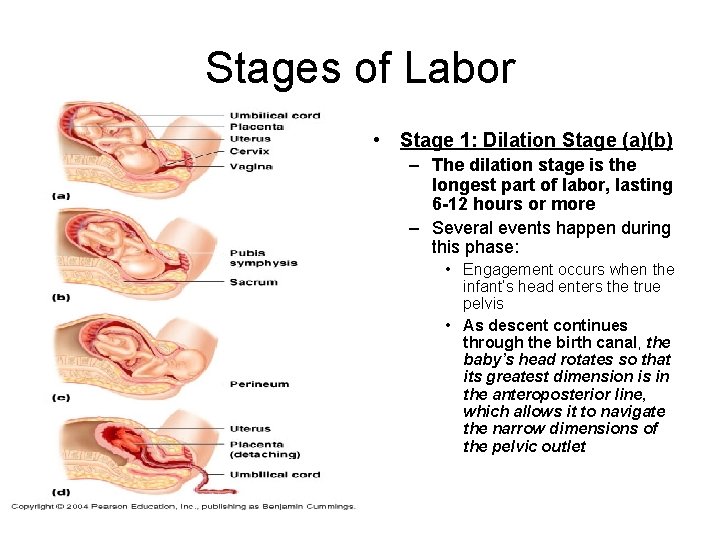
Stages of Labor • Stage 1: Dilation Stage (a)(b) – The dilation stage is the longest part of labor, lasting 6 -12 hours or more – Several events happen during this phase: • Engagement occurs when the infant’s head enters the true pelvis • As descent continues through the birth canal, the baby’s head rotates so that its greatest dimension is in the anteroposterior line, which allows it to navigate the narrow dimensions of the pelvic outlet
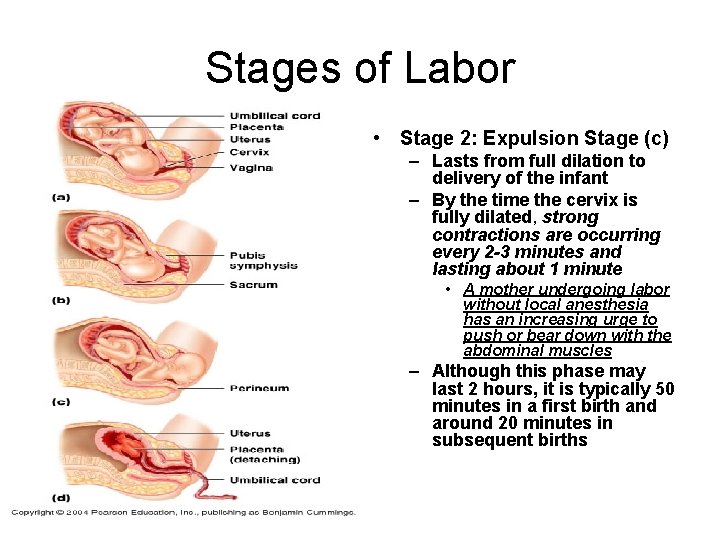
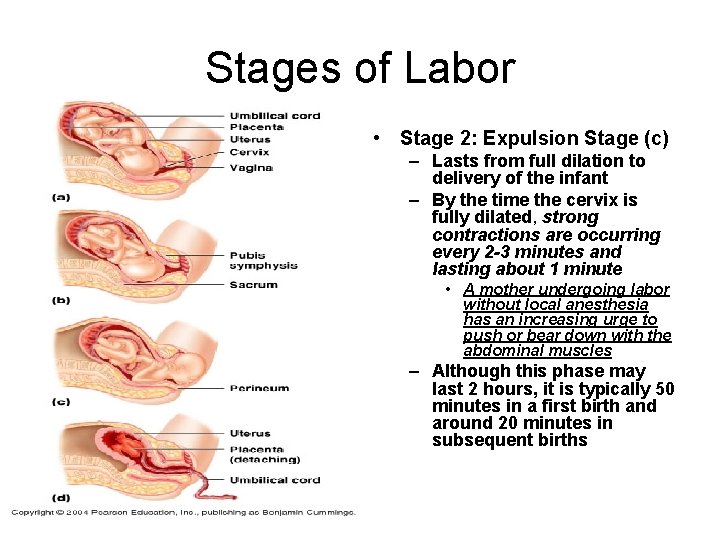
Stages of Labor • Stage 2: Expulsion Stage (c) – Lasts from full dilation to delivery of the infant – By the time the cervix is fully dilated, strong contractions are occurring every 2 -3 minutes and lasting about 1 minute • A mother undergoing labor without local anesthesia has an increasing urge to push or bear down with the abdominal muscles – Although this phase may last 2 hours, it is typically 50 minutes in a first birth and around 20 minutes in subsequent births
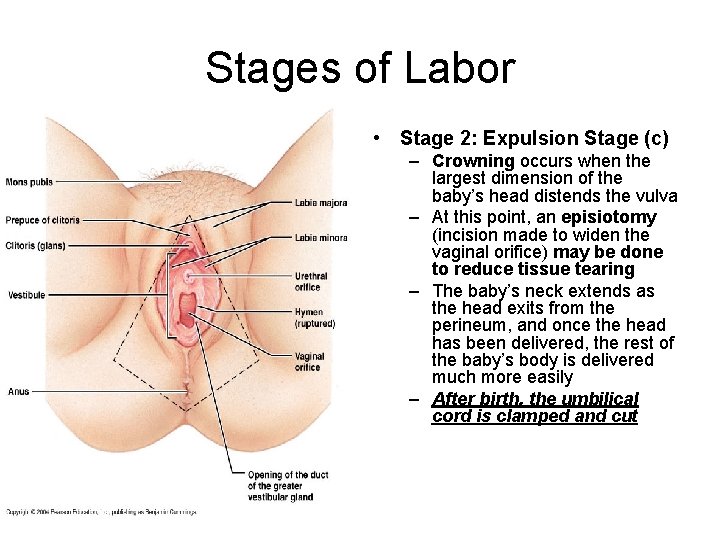
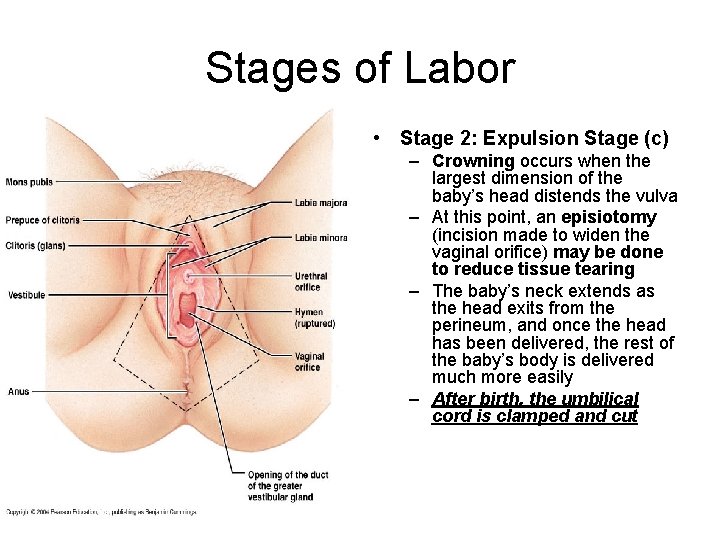
Stages of Labor • Stage 2: Expulsion Stage (c) – Crowning occurs when the largest dimension of the baby’s head distends the vulva – At this point, an episiotomy (incision made to widen the vaginal orifice) may be done to reduce tissue tearing – The baby’s neck extends as the head exits from the perineum, and once the head has been delivered, the rest of the baby’s body is delivered much more easily – After birth, the umbilical cord is clamped and cut
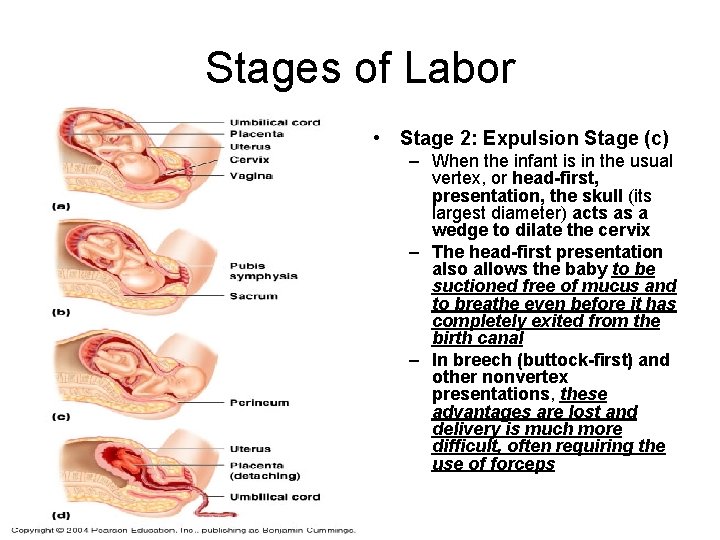
Stages of Labor • Stage 2: Expulsion Stage (c) – When the infant is in the usual vertex, or head-first, presentation, the skull (its largest diameter) acts as a wedge to dilate the cervix – The head-first presentation also allows the baby to be suctioned free of mucus and to breathe even before it has completely exited from the birth canal – In breech (buttock-first) and other nonvertex presentations, these advantages are lost and delivery is much more difficult, often requiring the use of forceps
HOMEOSTATIC IMBALANCE • If a women has a deformed or malelike pelvis, labor may be prolonged and difficult (dystocia) – Besides extreme maternal fatigue, another consequence is fetal brain damage – To prevent these outcomes, a cesarean (Csection) is performed in many such cases – A C-section is delivery of the infant through n incision made through the abdominal and uterine walls
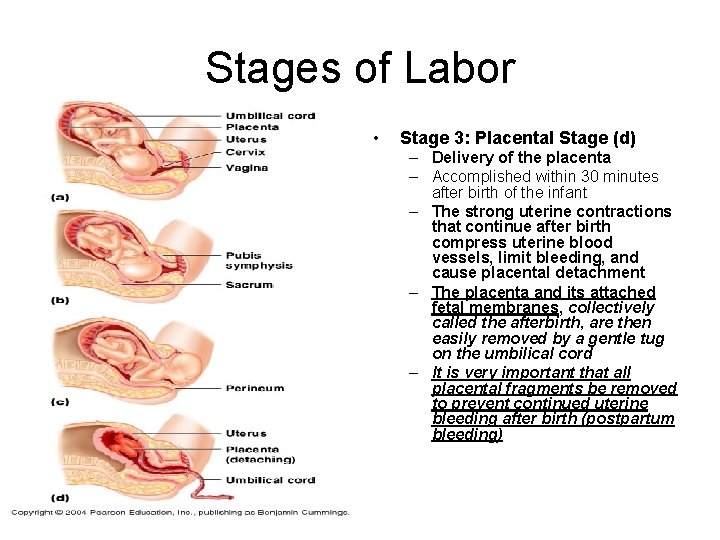
Stages of Labor • Stage 3: Placental Stage (d) – Delivery of the placenta – Accomplished within 30 minutes after birth of the infant – The strong uterine contractions that continue after birth compress uterine blood vessels, limit bleeding, and cause placental detachment – The placenta and its attached fetal membranes, collectively called the afterbirth, are then easily removed by a gentle tug on the umbilical cord – It is very important that all placental fragments be removed to prevent continued uterine bleeding after birth (postpartum bleeding)

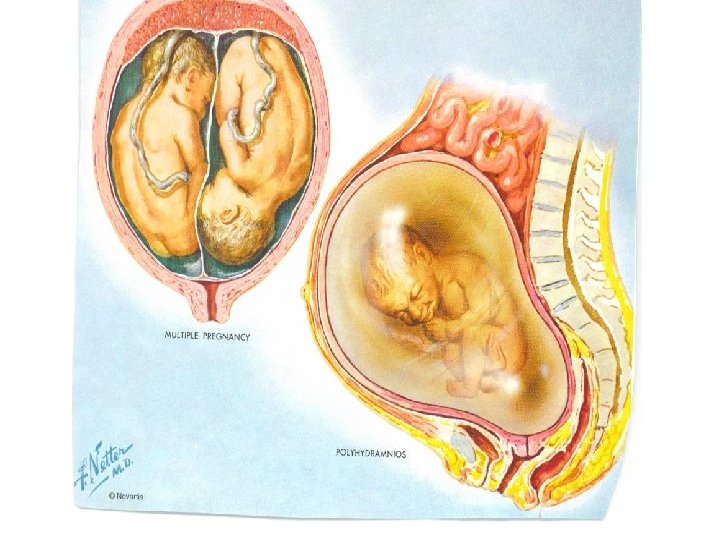
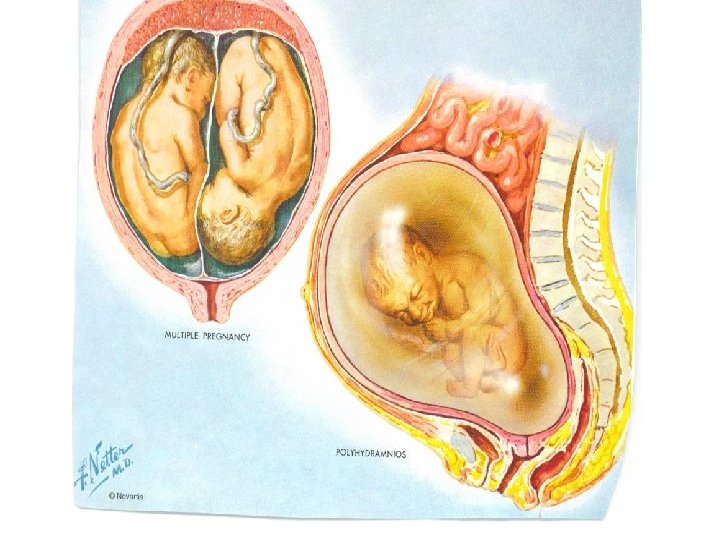
TWINS • Identical: – One embryo splits into two separate embryos • Probably during the blastocyst stage • Fraternal: – Two eggs are fertilized by different sperm


AFTERBIRTH • Baby still attached to the placenta by means of the umbilical cord: – Once tied and cut, the baby no longer obtains food and oxygen from the mother – Navel is the spot where your umbilical cord was attached to your body • Lung filled with amniotic fluid: – First cries rid the lungs of fluid and fill them with air – Newborn begins to breathe on its own • In the uterus most of the blood bypassed the lungs: – Right ventricle through a duct into the systemic system – Duct closes at birth – Right ventricle begins pumping to the lungs • Before birth, an opening exists between the right and left atria: – Normally this opening closes shortly after birth preventing oxygenated and deoxygenated blood from mixing • The remains of the placenta and amnion are then expelled from the mother’s body about 10 minutes after the birth of the baby (afterbirth)

ADJUSTMENTS OF THE INFANT TO EXTRAUTERINE LIFE • Neonatal period is the four-week period immediately after birth • Birth represents quite a shock to the infant – – Exposed to physical trauma during the birth process Suddenly cast out of its watery, warm environment Its placental life supports are severed NOW must do for itself
ADJUSTMENTS OF THE INFANT TO EXTRAUTERINE LIFE • At 1 and 5 minutes after birth, the infant’s physical status is assessed based on five signs: – Each observation is given a score of 0 to 2 • • • Heart rate Respiration Color Muscle tone Reflexes (tested by slaps on the feet) – Total is called the Apgar score • Score of 8 to 10 indicates a healthy baby • Lower scores reveal problems in one or more of the physiological functions assessed
ADJUSTMENTS OF THE INFANT TO EXTRAUTERINE LIFE • Taking the First Breath: – Once carbon dioxide is no longer removed by the placenta, it accumulates in the baby’s blood, causing central acidosis – This excites respiratory control centers in the baby’s brain and triggers the first inspiration – The first breathe requires a tremendous effort • The airways are tiny, and the lungs are collapsed • Once the lungs have been inflated in full-term babies, surfactant in alveolar fluid reduces surface tension in the alveoli, and breathing is easier – The rate of respiration is rapid (about 45 respirations/min) during the first two weeks and then gradually declines to normal levels
ADJUSTMENTS OF THE INFANT TO EXTRAUTERINE LIFE • Keeping the lungs inflated is much more difficult for premature infants (those weighing less than 2500 g, or about 5. 5 pounds, at birth) because surfactant production occurs during the last months of prenatal life – Consequently, preemies are usually put on respiratory assistance (a ventilator) until their lungs are mature enough to function on their own
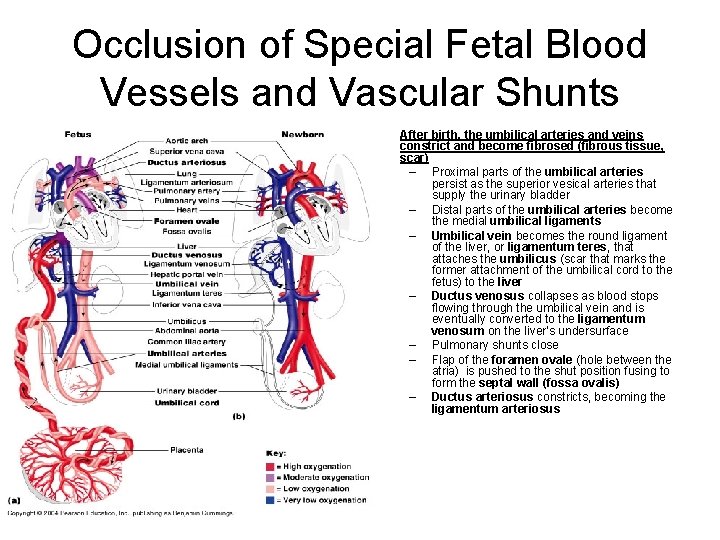
Occlusion of Special Fetal Blood Vessels and Vascular Shunts • After birth, the umbilical arteries and veins constrict and become fibrosed (fibrous tissue, scar) – Proximal parts of the umbilical arteries persist as the superior vesical arteries that supply the urinary bladder – Distal parts of the umbilical arteries become the medial umbilical ligaments – Umbilical vein becomes the round ligament of the liver, or ligamentum teres, that attaches the umbilicus (scar that marks the former attachment of the umbilical cord to the fetus) to the liver – Ductus venosus collapses as blood stops flowing through the umbilical vein and is eventually converted to the ligamentum venosum on the liver’s undersurface – Pulmonary shunts close – Flap of the foramen ovale (hole between the atria) is pushed to the shut position fusing to form the septal wall (fossa ovalis) – Ductus arteriosus constricts, becoming the ligamentum arteriosus

The Transitional Period • Infants pass through an unstable transitional period: – 6 -8 hours after birth – Characterized by intermittent waking periods in which the infant’s heart rate, respiratory behavior, and body temperature fluctuate

LACTATION • Lactation is the production of milk by the hormone-prepared mammary glands: – Rising levels of placental estrogens, progesterone, and lactogen toward the end of pregnancy stimulate the hypothalamus to produce prolactin-releasing hormone (PRH), which promotes secretion of prolactin by the anterior pituitary – After a delay of two to three days, true milk production begins
LACTATION • During the delay of milk production, a yellowish fluid called colostrum is secreted: – Comparison to milk: • • • Has less lactose than milk Almost no fat Higher in protein Higher in Vitamin C Higher in minerals – Like milk, colostrum is rich in Ig. A antibodies: • Since these antibodies are resistant to digestion in the stomach, they may help to protect the infant’s digestive tract against bacterial infection • These antibodies are absorbed by endocytosis and subsequently enter the bloodstream to provide even broader immunity
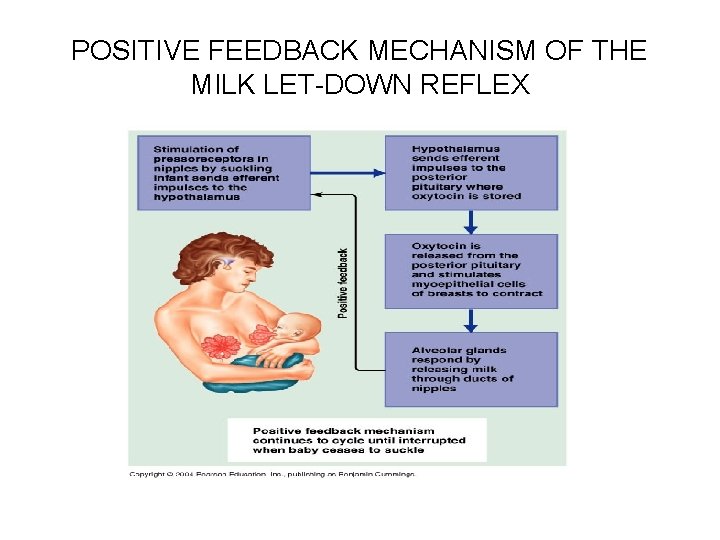
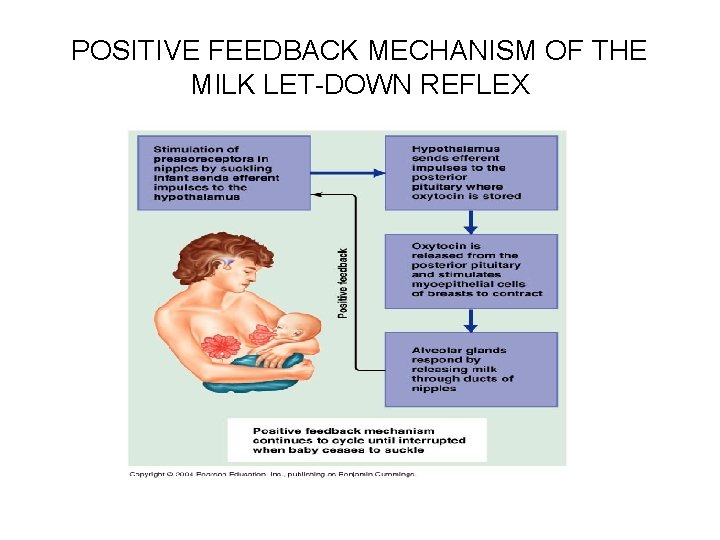
LACTATION • After birth, prolactin (placenta) release gradually wanes, and continual milk production depends on mechanical stimulation of the nipples, normally provided by the sucking infant: – Mechanoreceptors in the nipples send afferent nerve impulses to the hypothalamus, stimulating secretion of Prolactin releasing hormone (PRH) • Which stimulates the anterior pituitary to secrete prolactin – Nipple stimulation during nursing sends neural signals to the hypothalamus, resulting in production of PRH and a burst of prolactin from the anterior pituitary resulting in the stimulation of milk production for the next feeding
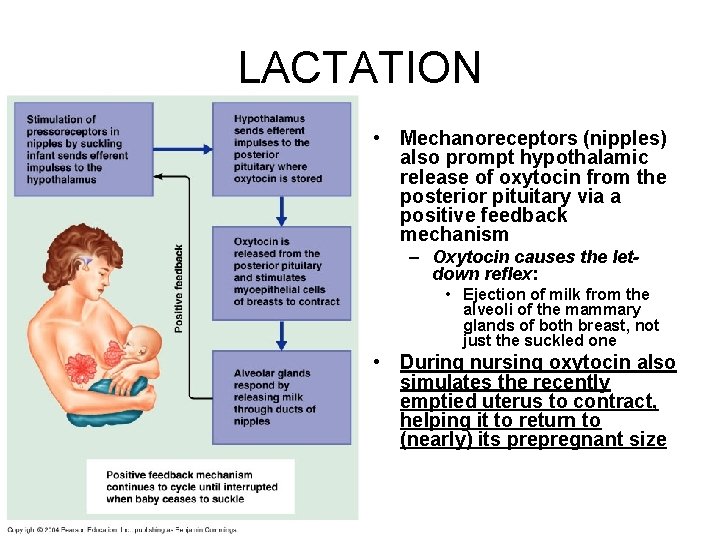
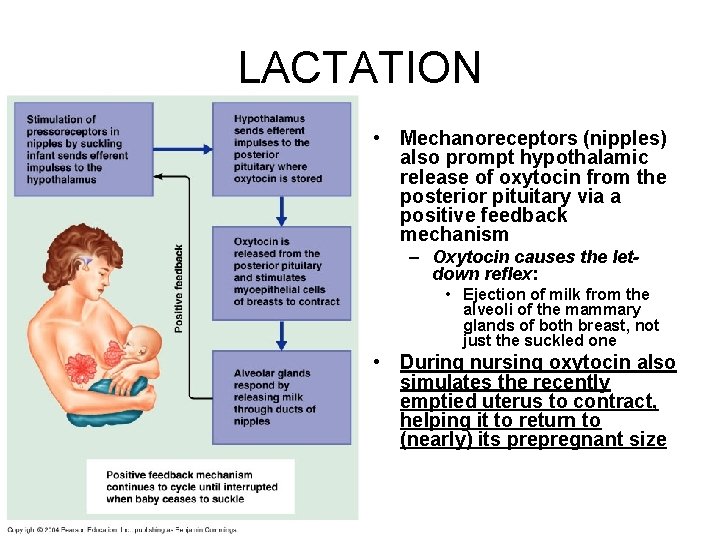
LACTATION • Mechanoreceptors (nipples) also prompt hypothalamic release of oxytocin from the posterior pituitary via a positive feedback mechanism – Oxytocin causes the letdown reflex: • Ejection of milk from the alveoli of the mammary glands of both breast, not just the suckled one • During nursing oxytocin also simulates the recently emptied uterus to contract, helping it to return to (nearly) its prepregnant size
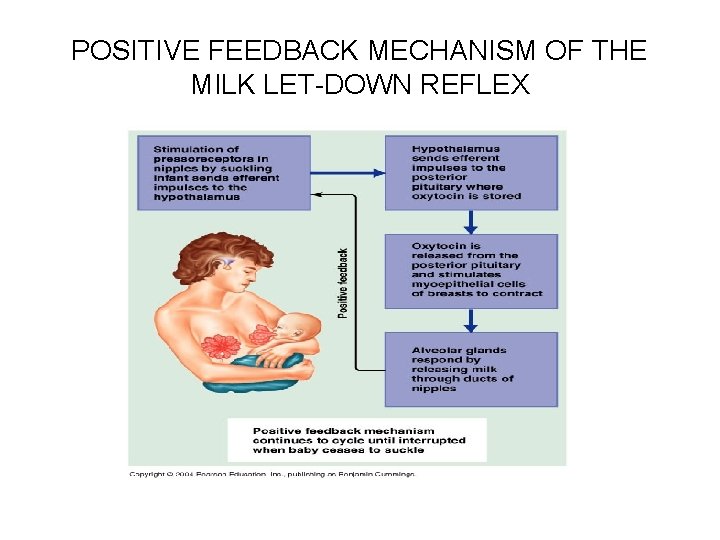
POSITIVE FEEDBACK MECHANISM OF THE MILK LET-DOWN REFLEX
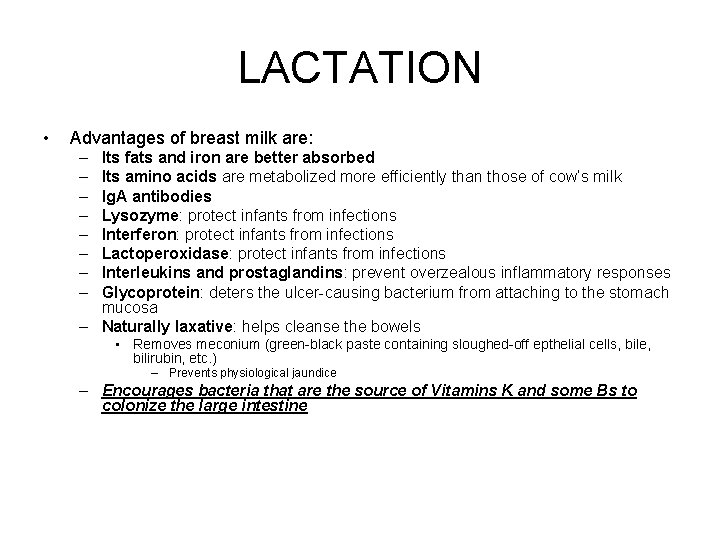
LACTATION • Advantages of breast milk are: – – – – Its fats and iron are better absorbed Its amino acids are metabolized more efficiently than those of cow’s milk Ig. A antibodies Lysozyme: protect infants from infections Interferon: protect infants from infections Lactoperoxidase: protect infants from infections Interleukins and prostaglandins: prevent overzealous inflammatory responses Glycoprotein: deters the ulcer-causing bacterium from attaching to the stomach mucosa – Naturally laxative: helps cleanse the bowels • Removes meconium (green-black paste containing sloughed-off epthelial cells, bile, bilirubin, etc. ) – Prevents physiological jaundice – Encourages bacteria that are the source of Vitamins K and some Bs to colonize the large intestine
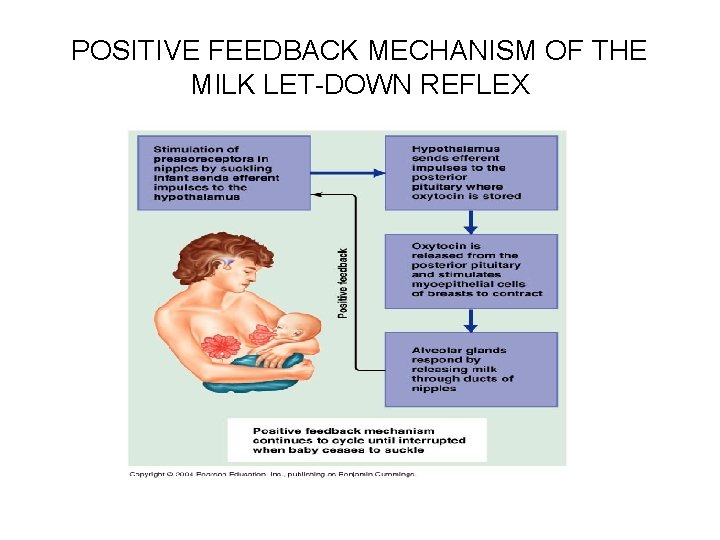
POSITIVE FEEDBACK MECHANISM OF THE MILK LET-DOWN REFLEX
LACTATION • When nursing is discontinued, the stimulus for prolactin release and milk production ends, and the mammary glands stop producing milk
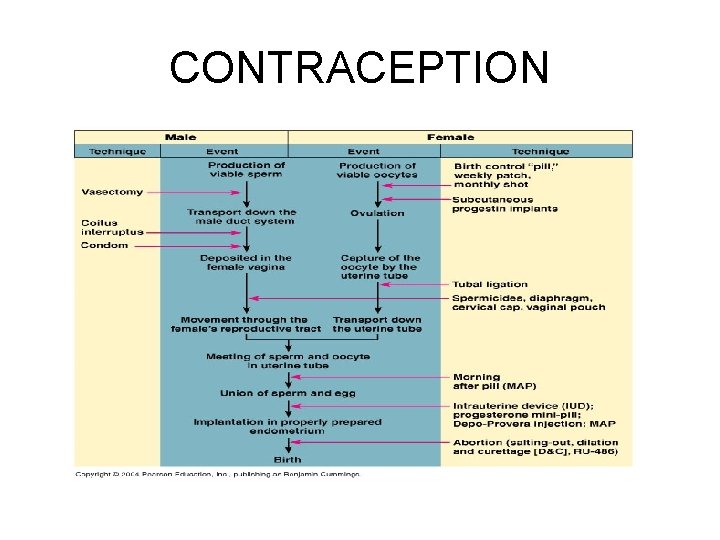
CONTRACEPTION