PreConference Workshop EvidenceBased Stroke Rehabilitation Resourc e Persons
Pre-Conference Workshop Evidence-Based Stroke Rehabilitation Resourc e Persons Emmanuel B. John, PT, Ph. D Associate Professor & Director, Motor Control & Neuromuscular Performance Laboratory, Department of Physical Therapy, Radford University, Roanoke, VA, USA; Chair Stroke Interest Group, Neurology Section of the American Physical Therapy Association Abiodun E. Akinwuntan, Ph. D, MPH, DRS Associate Professor & Director, Driving Simulation Lab, Department of Physical Therapy; Interim Associate Dean for Research, College of Allied Health Sciences, Georgia Regents University,
Resource Persons Abiodun E. Akinwuntan, Ph. D, MPH, DRS Emmanuel B. John, PT, Ph. D

Pre-Workshop Quiz List one reliable and valid outcome measures for Physical functioning Neurological Status Gait Velocity Cardiovascular endurance Name the two (2) broad ICF classifications List three (3) common models of neurophysiotherapy interventions
Stroke Toolbox and Gentile’s taxonomy
Break
Interactive Case Study Session 1 A 53 year old surgeon with memory problems, slight weakness of the right arm, profound right leg weakness and impaired sensation of the right side of the body. History Patient woke up from sleep to discover that she could not move her right leg and difficulty using her right hand. She immediately called her physician who told her to call the EMS. Patient was immediately taken to the hospital. Patient has just been recently transferred to a rehabilitation hospital and requires PT. Things to know Patient has previous history of cigarette smoking, anxiety, peripheral vascular disease and hypertension. Patient is currently alert and oriented, but hardly comprehends or follows simple commands. Patient has difficulties remembering events or encounters that recently occurred but can relate old events with ease (always telling stories of the past). Muscle power of the right upper extremity is now 3. 5/5 and 1 for the lower extremity. Patient’s response to pin prick is inconsistent on the right side of the body, more evident in the lower extremity. Patient can sit and ambulate independently in a wheel chair. Patient wants to be discharged home as soon as possible and possibly return to his career.
Debrief for Case Study 1
Theories and Concepts
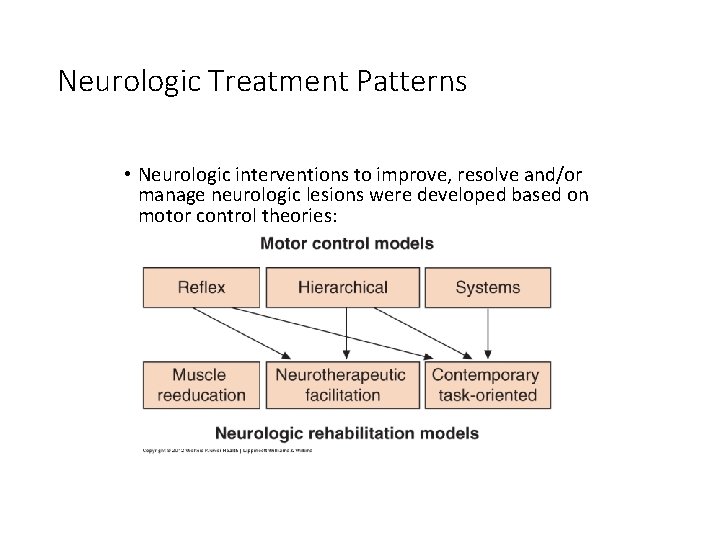
Neurologic Treatment Patterns • Neurologic interventions to improve, resolve and/or manage neurologic lesions were developed based on motor control theories:
Conventional Therapeutic Exercise Approach • Range Of Motion (ROM) Exercises • Muscle Strengthening Exercises • Mobilization Activities • Fitness training • Compensatory Techniques

Neurophysiological Therapeutic Exercise Approaches • Muscle Re-education Approach (1920 s) • Neurodevelopmental Approaches (1940 -70 s) • • • Sensorimotor Approach (Rood, 1940 s) Movement Therapy Approach (Brunnstrom, 1950 s) NDT Approach (Bobath, 1960 -70 s) PNF Approach (Knot and Voss, 1960 -70 s) Other Neurophysiological Approaches • Motor Control & Relearning (1980 s) • Contemporary Task-Oriented Approach (1990 s)
Contemporary Task-Oriented Approach • Based on systems model of motor control and contemporary motor learning theories • Emphasizes that effective therapeutic intervention depends on identification of the system that is critical to controlling the occupational performance at a specific time
Motor Control/Relearning Approaches • Incorporates functional training for key motor tasks such as sitting, standing up, or walking. • The therapist analyses each task, determines which component of the task cannot be performed, • trains the patient in those components of the task, and • ensures carryover of this training during daily activities
Interventions in Stroke
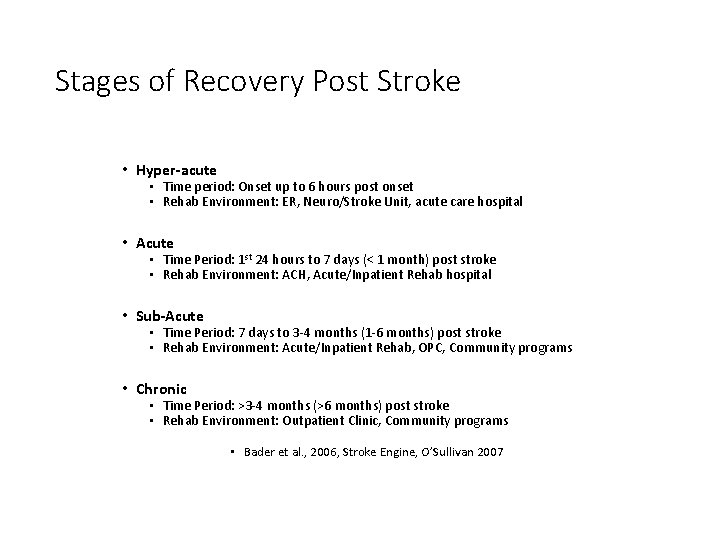
Stages of Recovery Post Stroke • Hyper-acute • Time period: Onset up to 6 hours post onset • Rehab Environment: ER, Neuro/Stroke Unit, acute care hospital • Acute • Time Period: 1 st 24 hours to 7 days (< 1 month) post stroke • Rehab Environment: ACH, Acute/Inpatient Rehab hospital • Sub-Acute • Time Period: 7 days to 3 -4 months (1 -6 months) post stroke • Rehab Environment: Acute/Inpatient Rehab, OPC, Community programs • Chronic • Time Period: >3 -4 months (>6 months) post stroke • Rehab Environment: Outpatient Clinic, Community programs • Bader et al. , 2006, Stroke Engine, O’Sullivan 2007
Drivers of Neuroplasticity Changes Post Stroke • • • Task-specific Training Aerobics Use it or Lose it; Use it and Improve it Specificity Repetition Intensity Age Sleep Timing of Rehabilitation Imagery and Mental Practice (Remember mirror neurons? ) •

Constraint-induced Movement Therapy

Body weight–supported treadmill training
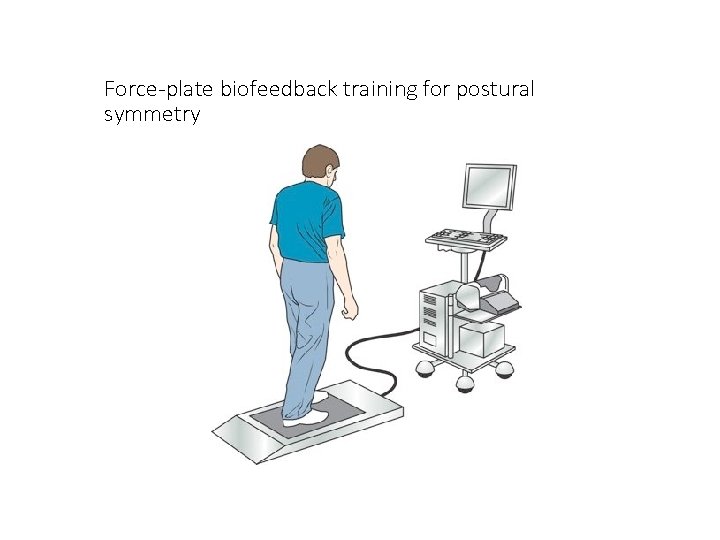
Force-plate biofeedback training for postural symmetry

Virtual Reality and Robotics Rehabilitation
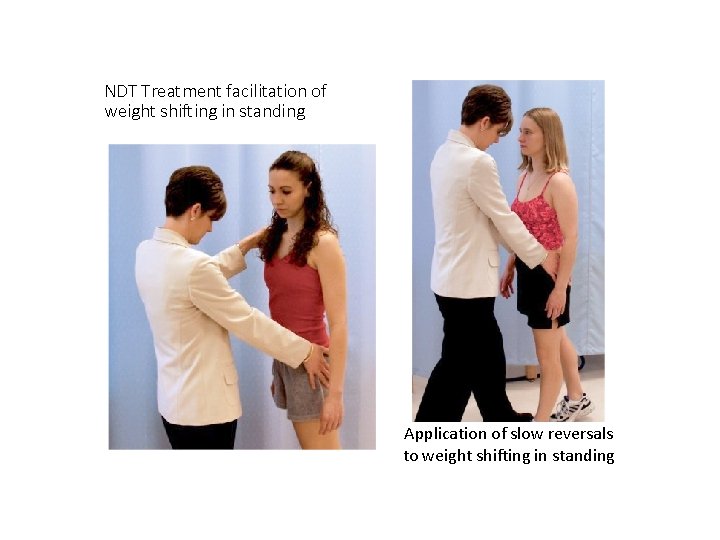
NDT Treatment facilitation of weight shifting in standing Application of slow reversals to weight shifting in standing
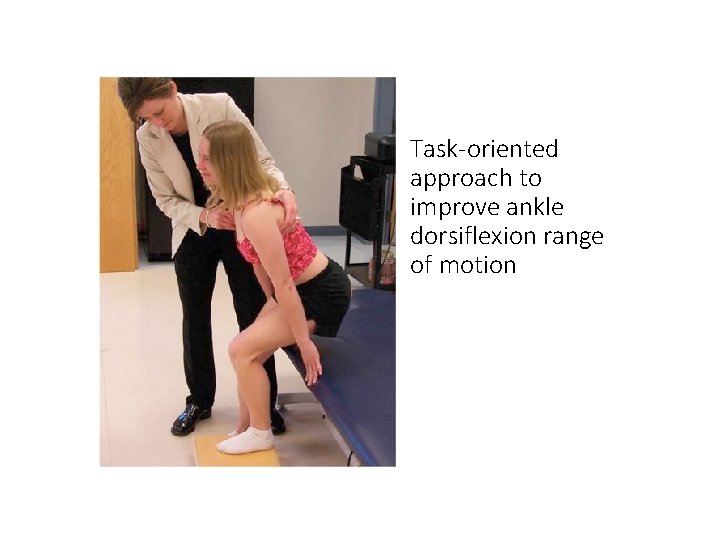
Task-oriented approach to improve ankle dorsiflexion range of motion

NDT treatment facilitation of bridging with key points of control on the distal femurs
Summary • Review causes of stroke • Description of Ischemic and Hemorrhagic strokes • Description of deficits and postural control problems • Stages of recovery • Assessment tools • Acute Care Intervensions
Lunch Break
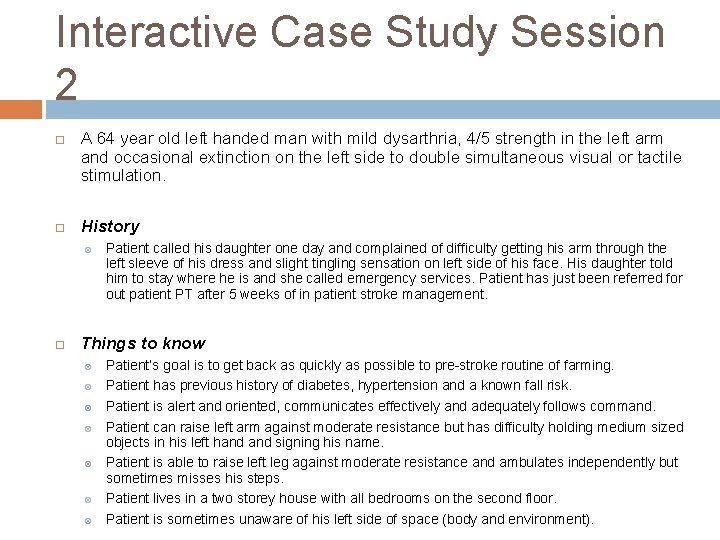
Interactive Case Study Session 2 A 64 year old left handed man with mild dysarthria, 4/5 strength in the left arm and occasional extinction on the left side to double simultaneous visual or tactile stimulation. History Patient called his daughter one day and complained of difficulty getting his arm through the left sleeve of his dress and slight tingling sensation on left side of his face. His daughter told him to stay where he is and she called emergency services. Patient has just been referred for out patient PT after 5 weeks of in patient stroke management. Things to know Patient’s goal is to get back as quickly as possible to pre-stroke routine of farming. Patient has previous history of diabetes, hypertension and a known fall risk. Patient is alert and oriented, communicates effectively and adequately follows command. Patient can raise left arm against moderate resistance but has difficulty holding medium sized objects in his left hand signing his name. Patient is able to raise left leg against moderate resistance and ambulates independently but sometimes misses his steps. Patient lives in a two storey house with all bedrooms on the second floor. Patient is sometimes unaware of his left side of space (body and environment).
Debrief for Case Study 2
Break
Theories and Concepts
Post-Workshop Quiz List one reliable and valid outcome measures for Physical functioning Neurological Status Gait Velocity Cardiovascular endurance Name the two (2) broad ICF classifications List three (3) common models of neurophysiotherapy interventions
Discussions: Current and Future Workshops
- Slides: 32