Precise Nutrition with Precision ISCCM Day Precise Nutrition
- Slides: 26
Precise Nutrition with Precision ISCCM Day
Precise Nutrition with Precision Assessment:
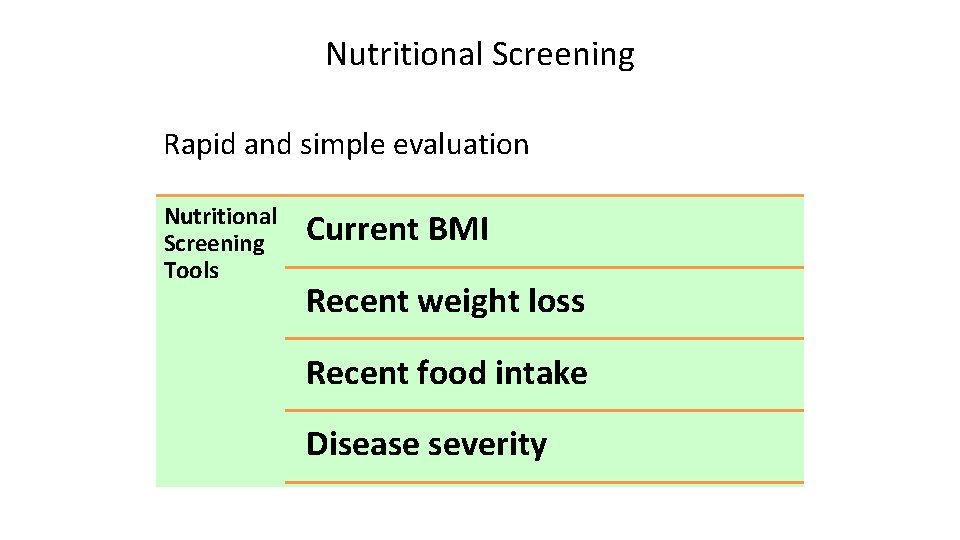
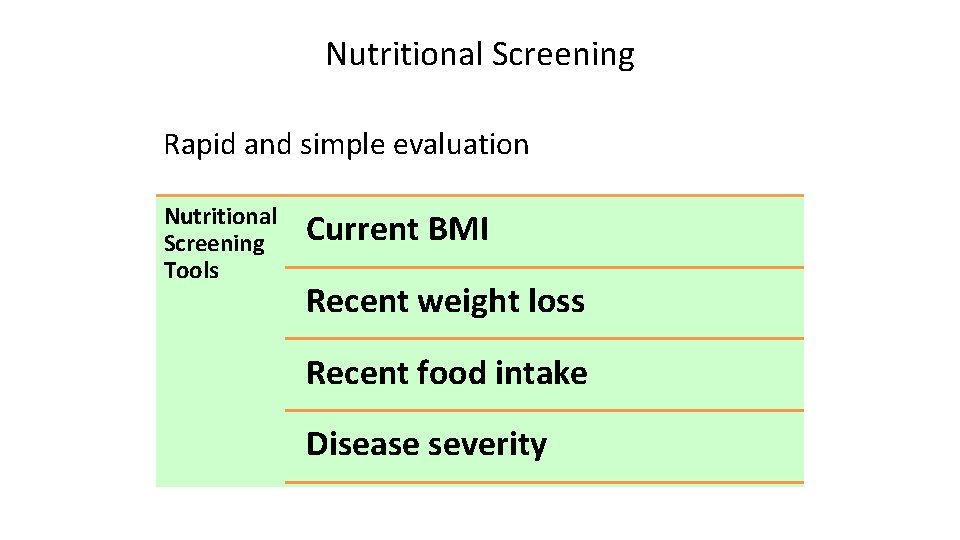
Nutritional Screening Rapid and simple evaluation Nutritional Screening Tools Current BMI Recent weight loss Recent food intake Disease severity
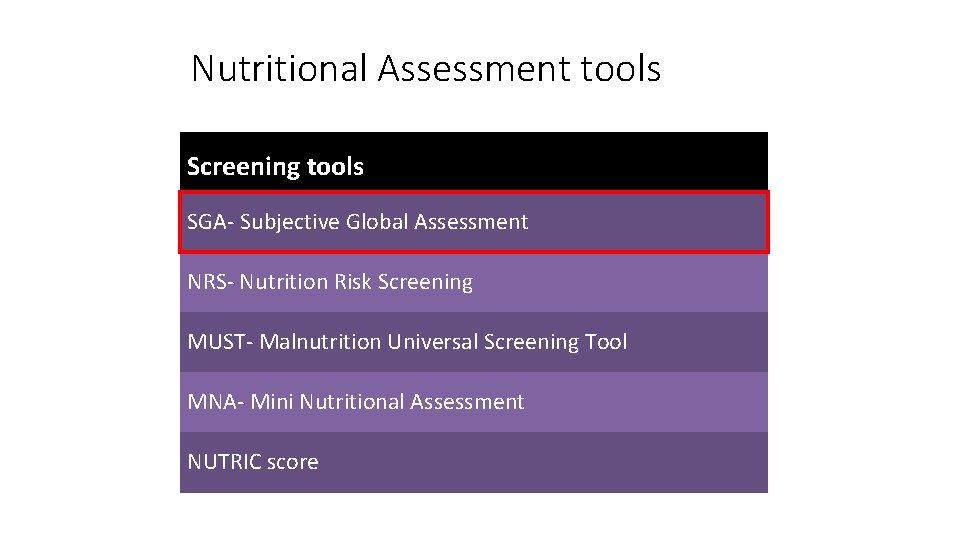
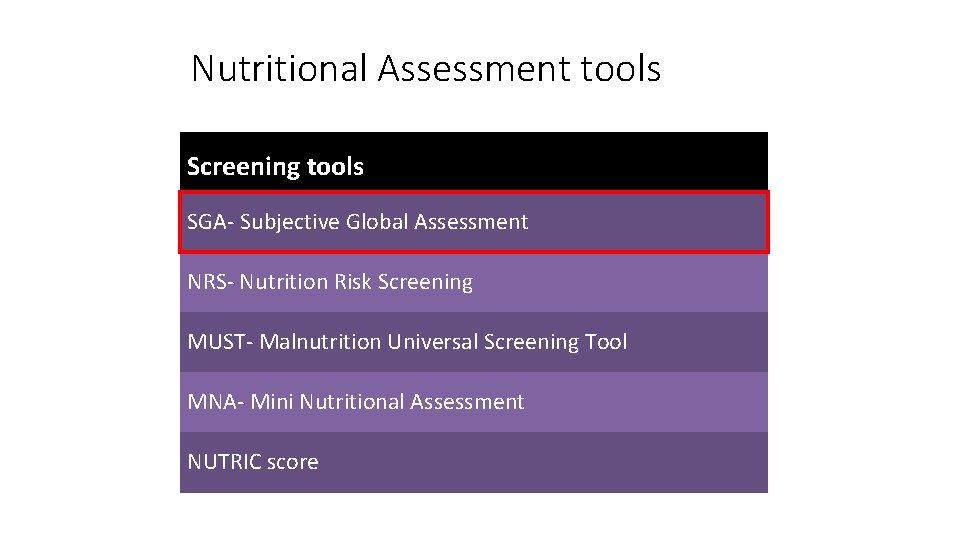
Nutritional Assessment tools Screening tools SGA- Subjective Global Assessment NRS- Nutrition Risk Screening MUST- Malnutrition Universal Screening Tool MNA- Mini Nutritional Assessment NUTRIC score
Precise Nutrition with Precision Diagnosis:
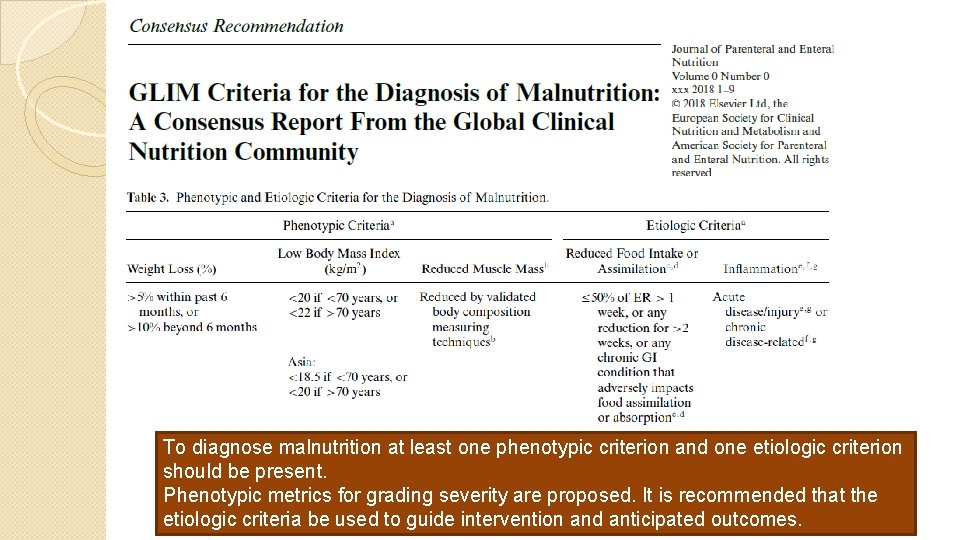
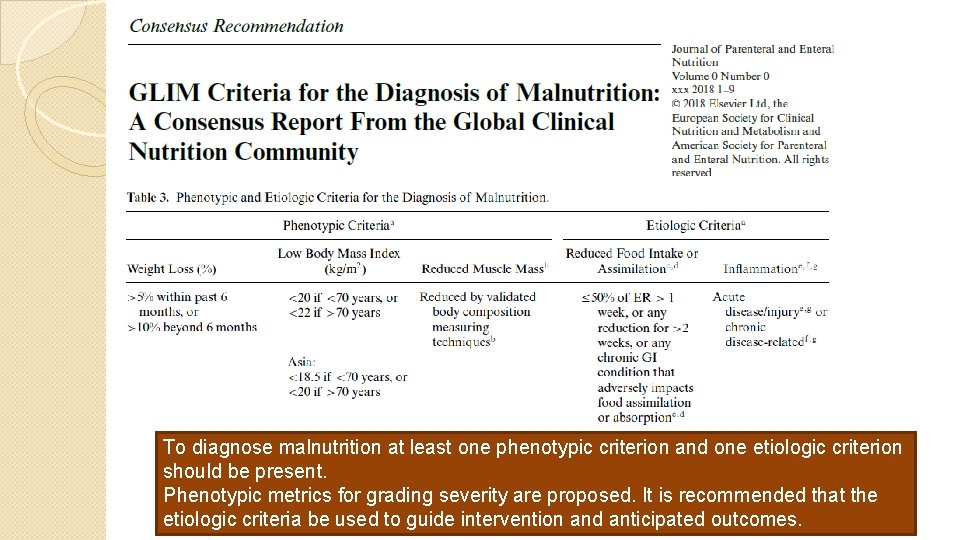
GLIM criteria To diagnose malnutrition at least one phenotypic criterion and one etiologic criterion should be present. Phenotypic metrics for grading severity are proposed. It is recommended that the etiologic criteria be used to guide intervention and anticipated outcomes.
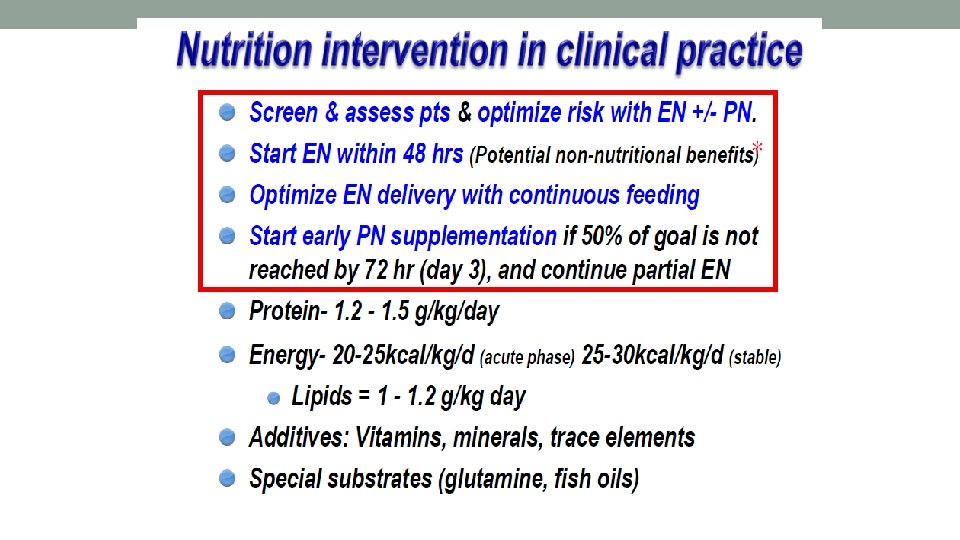
Precise Nutrition with Precision Intervention:
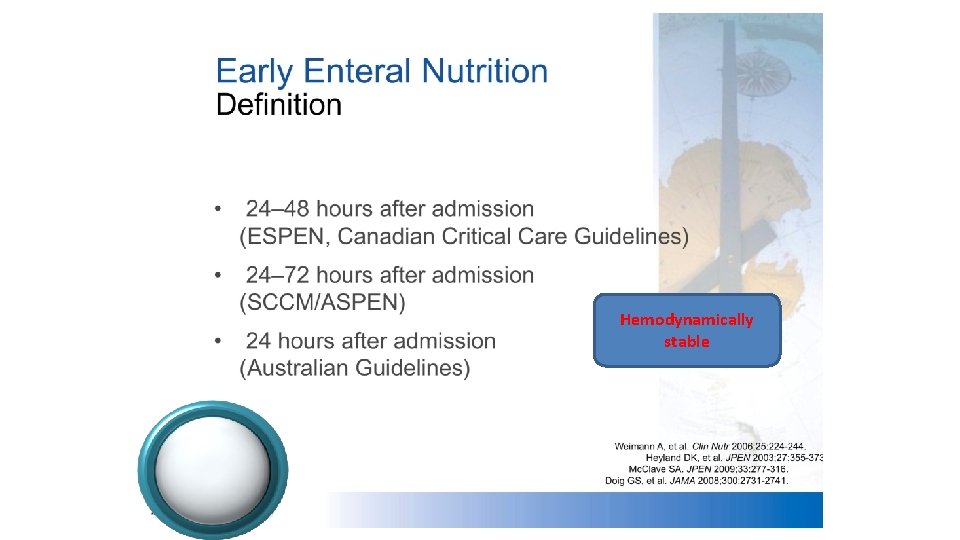
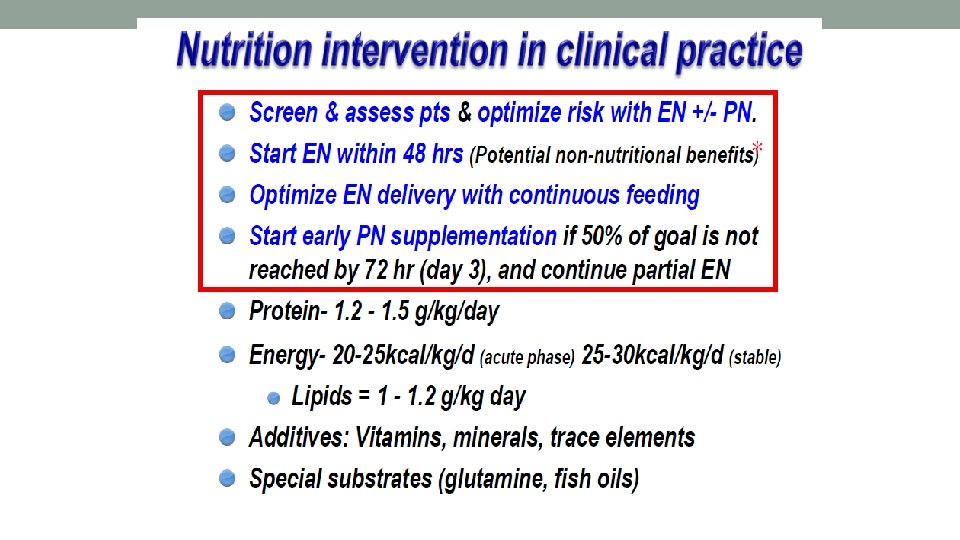
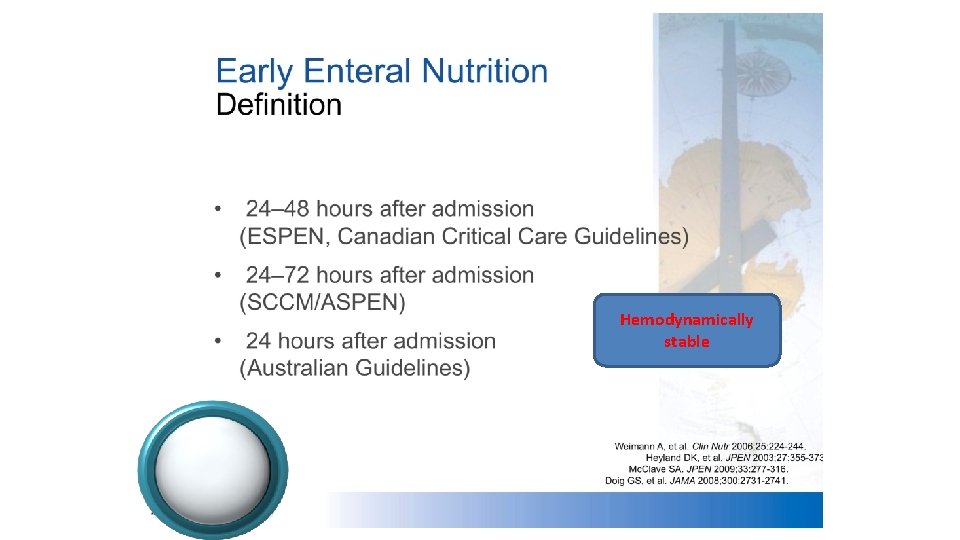
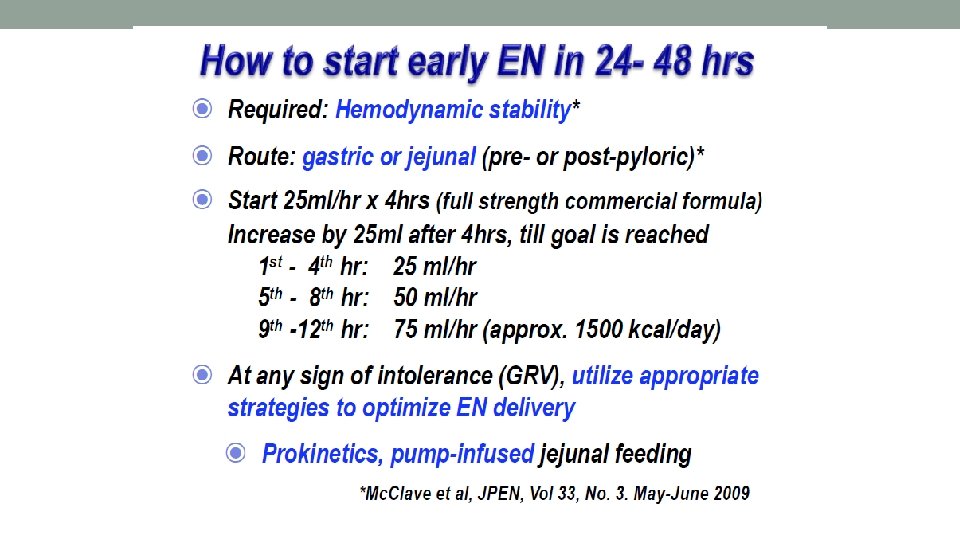
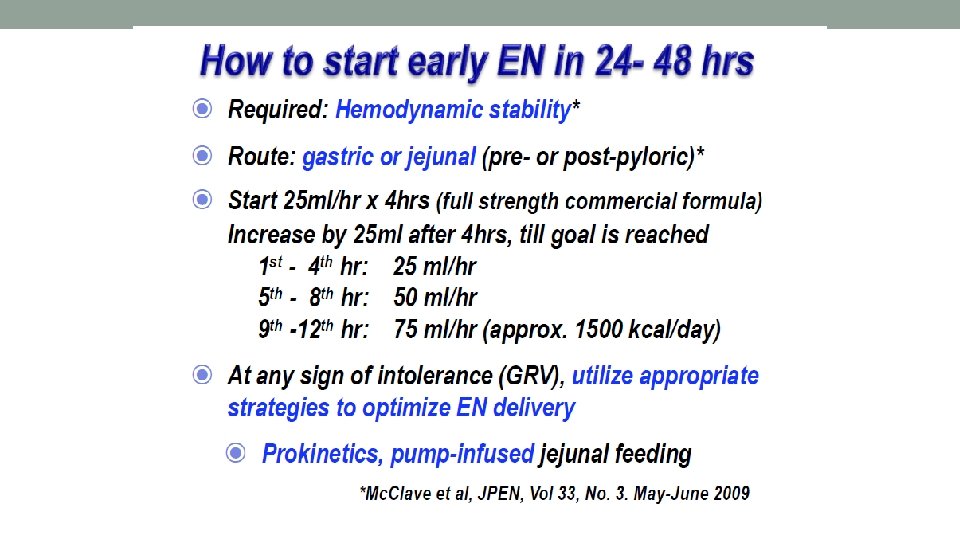
Hemodynamically stable
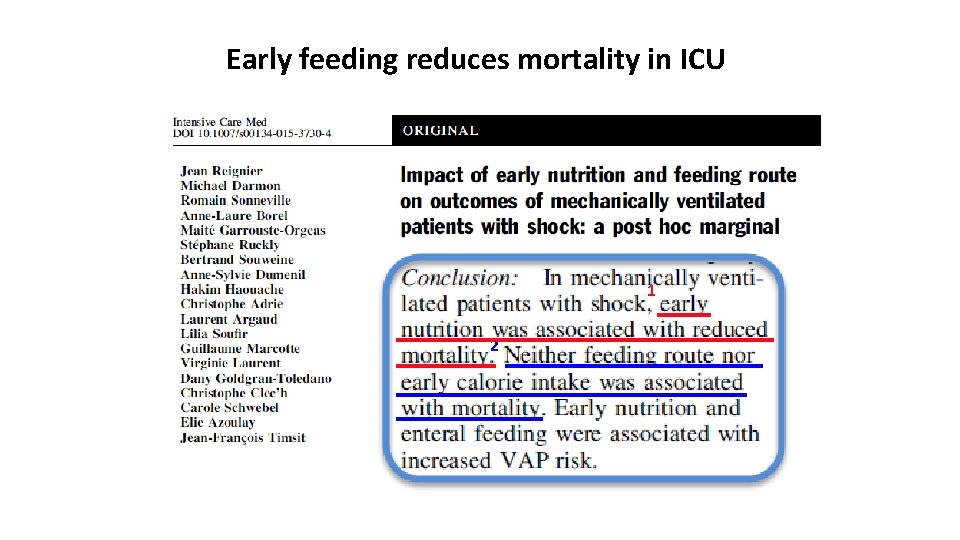
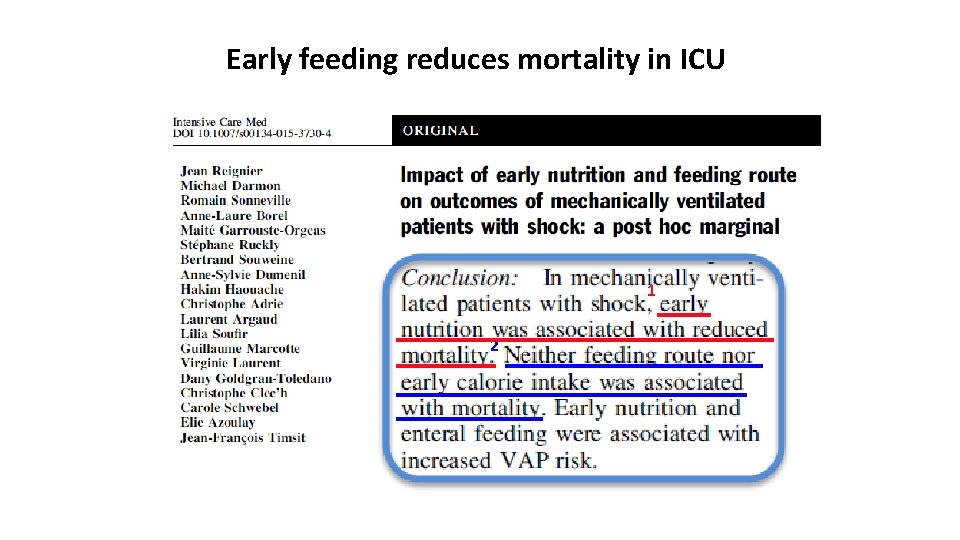
Early feeding reduces mortality in ICU 1 2
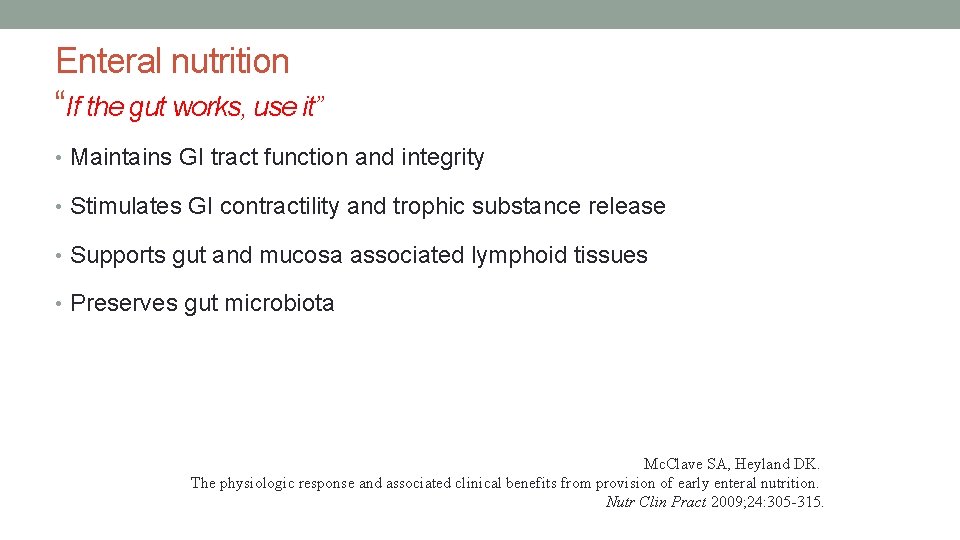
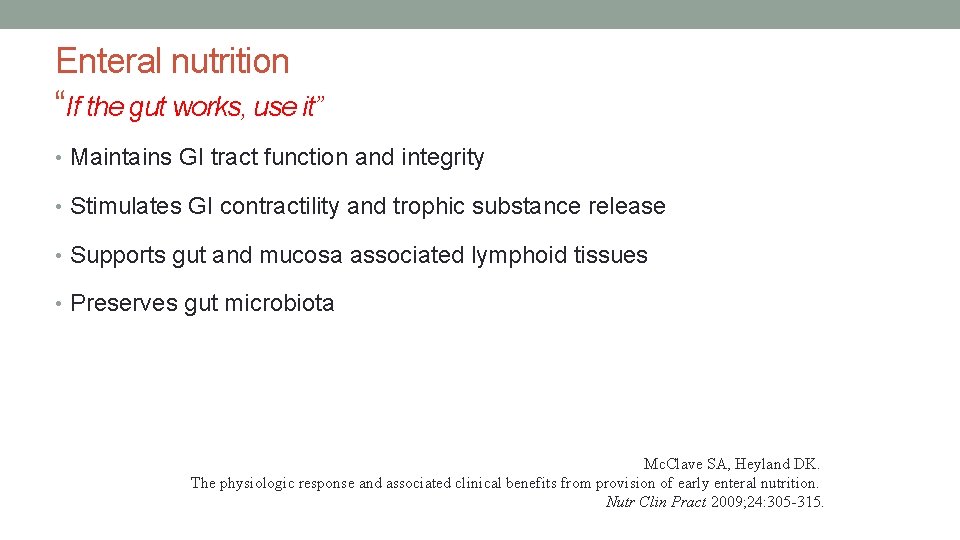
Enteral nutrition “If the gut works, use it” • Maintains GI tract function and integrity • Stimulates GI contractility and trophic substance release • Supports gut and mucosa associated lymphoid tissues • Preserves gut microbiota Mc. Clave SA, Heyland DK. The physiologic response and associated clinical benefits from provision of early enteral nutrition. Nutr Clin Pract 2009; 24: 305 -315.
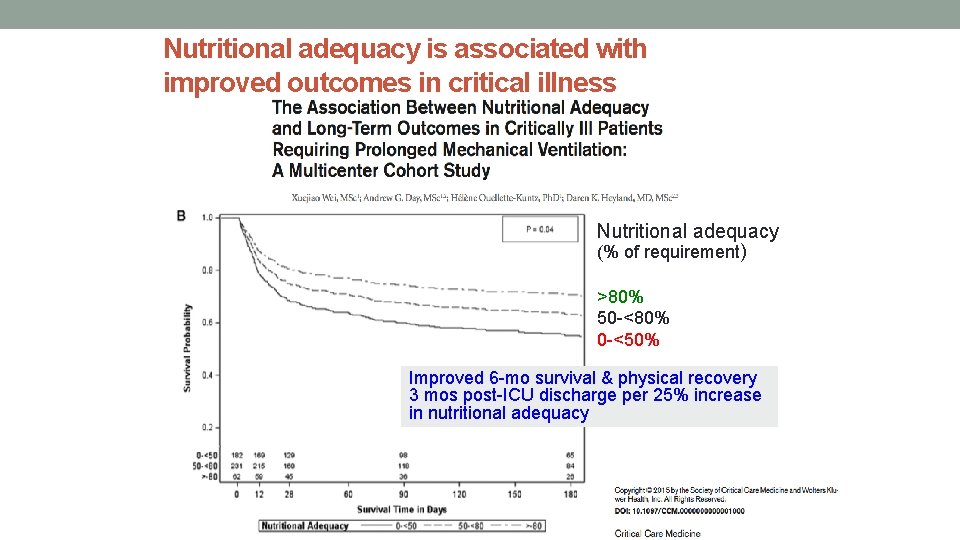
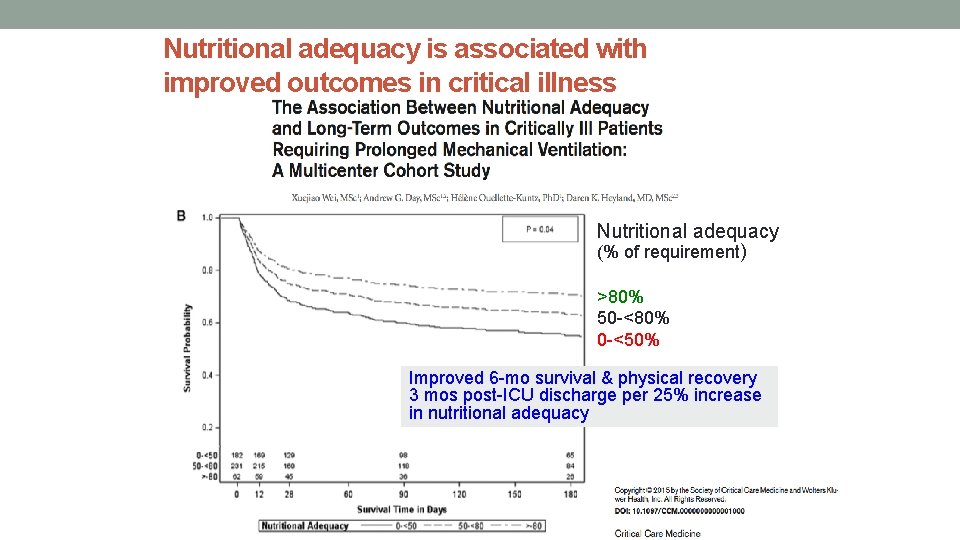
Nutritional adequacy is associated with improved outcomes in critical illness Nutritional adequacy (% of requirement) >80% 50 -<80% 0 -<50% Improved 6 -mo survival & physical recovery 3 mos post-ICU discharge per 25% increase in nutritional adequacy
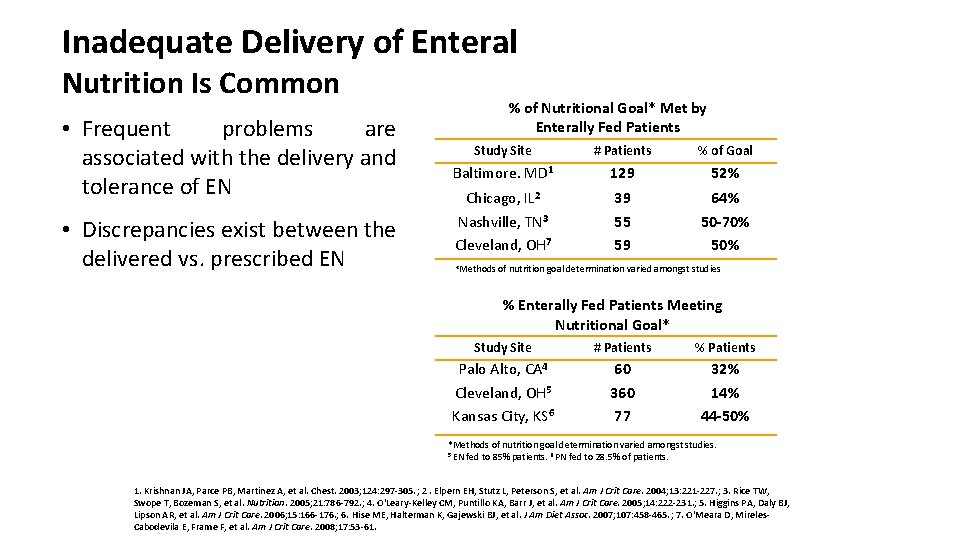
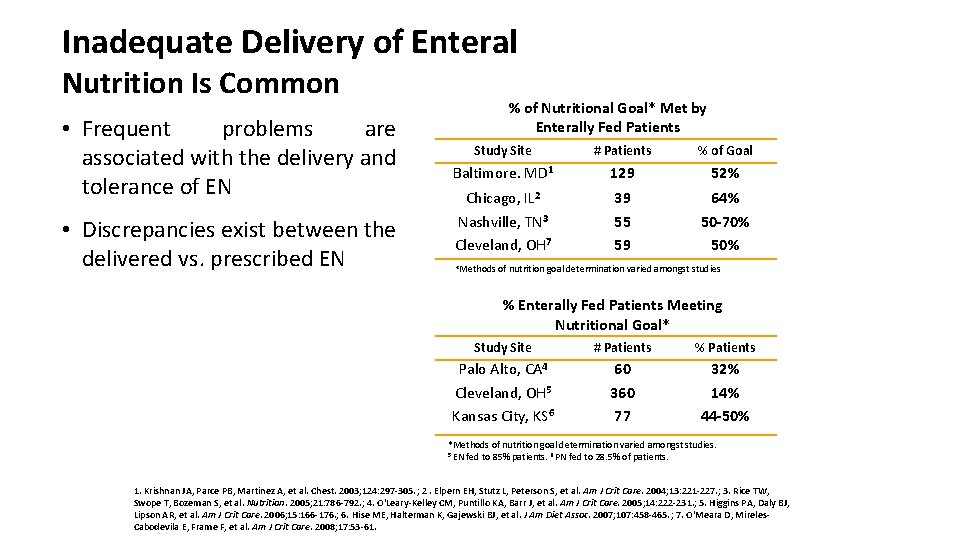
Inadequate Delivery of Enteral Nutrition Is Common • Frequent problems are associated with the delivery and tolerance of EN • Discrepancies exist between the delivered vs. prescribed EN % of Nutritional Goal* Met by Enterally Fed Patients Study Site # Patients % of Goal Baltimore. MD 1 129 52% Chicago, IL 2 Nashville, TN 3 Cleveland, OH 7 39 55 59 64% 50 -70% 50% *Methods of nutrition goal determination varied amongst studies % Enterally Fed Patients Meeting Nutritional Goal* Study Site # Patients % Patients Palo Alto, CA 4 Cleveland, OH 5 Kansas City, KS 6 60 360 77 32% 14% 44 -50% *Methods of nutrition goal determination varied amongst studies. 5 EN fed to 85% patients. 6 PN fed to 28. 5% of patients. 1. Krishnan JA, Parce PB, Martinez A, et al. Chest. 2003; 124: 297 -305. ; 2. Elpern EH, Stutz L, Peterson S, et al. Am J Crit Care. 2004; 13: 221 -227. ; 3. Rice TW, Swope T, Bozeman S, et al. Nutrition. 2005; 21: 786 -792. ; 4. O'Leary-Kelley CM, Puntillo KA, Barr J, et al. Am J Crit Care. 2005; 14: 222 -231. ; 5. Higgins PA, Daly BJ, Lipson AR, et al. Am J Crit Care. 2006; 15: 166 -176. ; 6. Hise ME, Halterman K, Gajewski BJ, et al. J Am Diet Assoc. 2007; 107: 458 -465. ; 7. O'Meara D, Mireles. Cabodevila E, Frame F, et al. Am J Crit Care. 2008; 17: 53 -61.
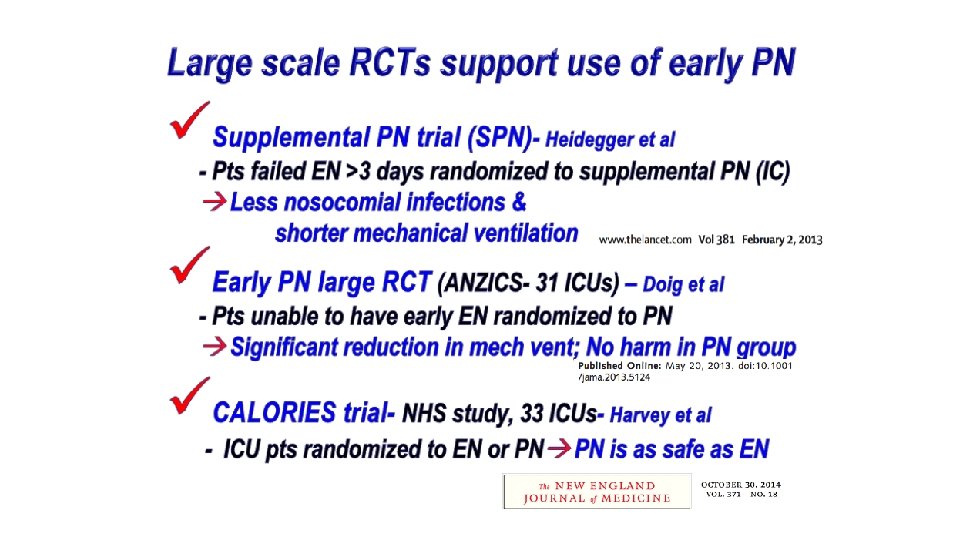
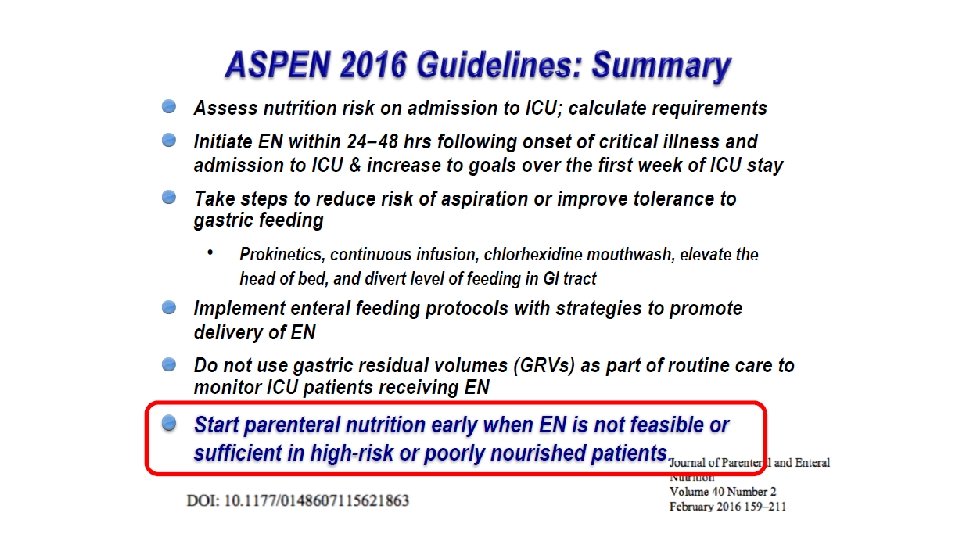
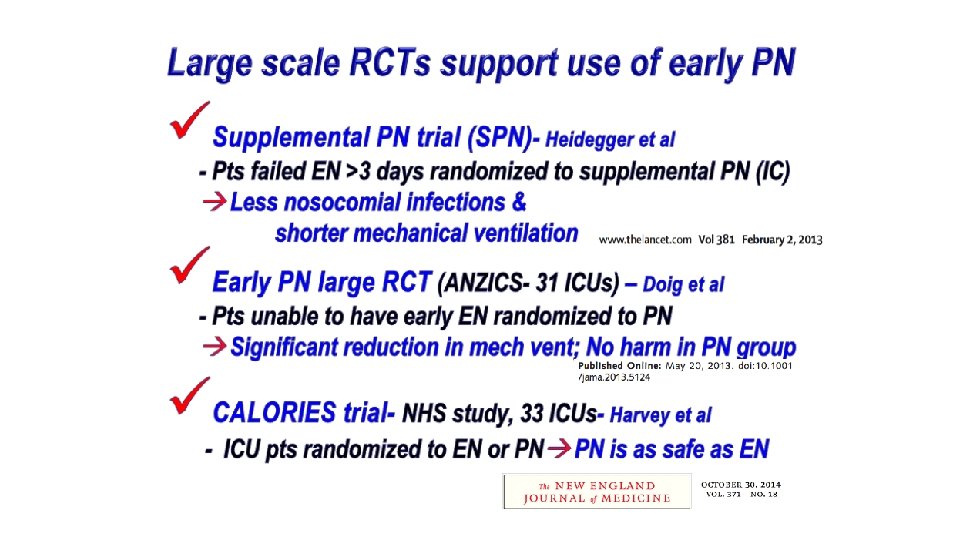
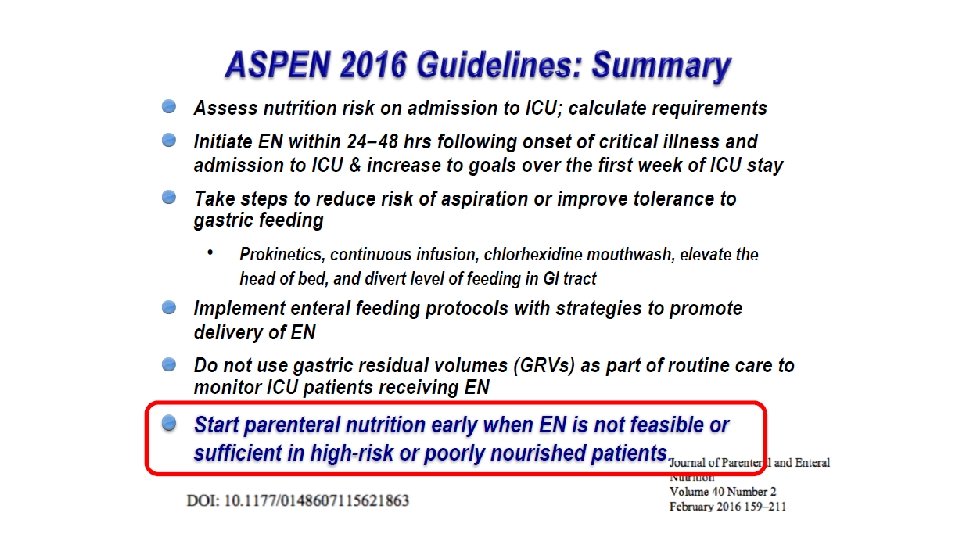
Early EN is the preferred route, but is often poorly tolerated in ICU patients with GI dysfunction. Therefore, early supplemental PN must be promptly initiated, so as to prevent underfeeding and the resulting energy-protein gap associated complications.
Preliminary discussion from SPN study Early EN within 24 hours in ICU patients on mechanical ventilation reduces energy deficit & maintains gut function However, poor EN tolerance indicates gut dysfunction– this sign of a “sick gut” is an important warning signal Persistent GI intolerance on day 3 automatically selects patients who will require supplemental PN Early EN with early supplemental PN improves outcomes:
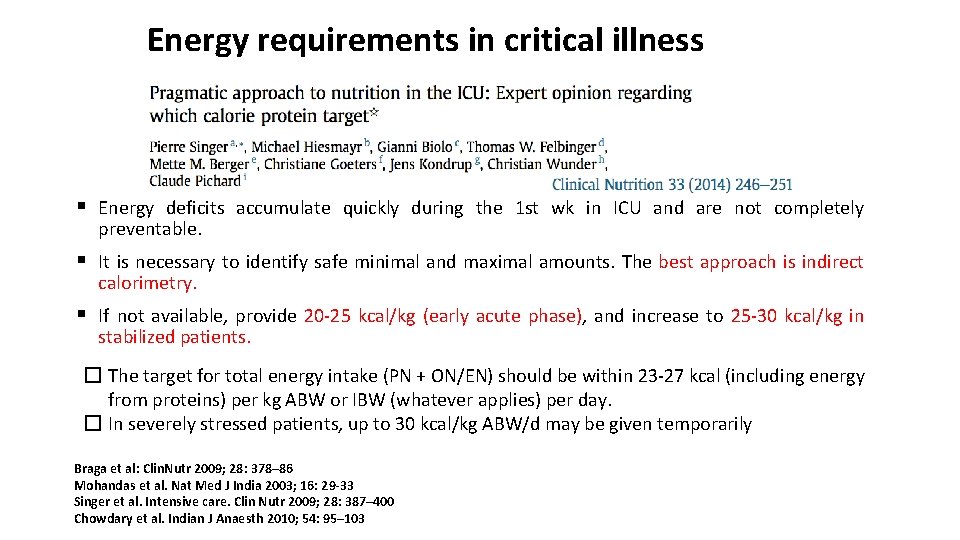
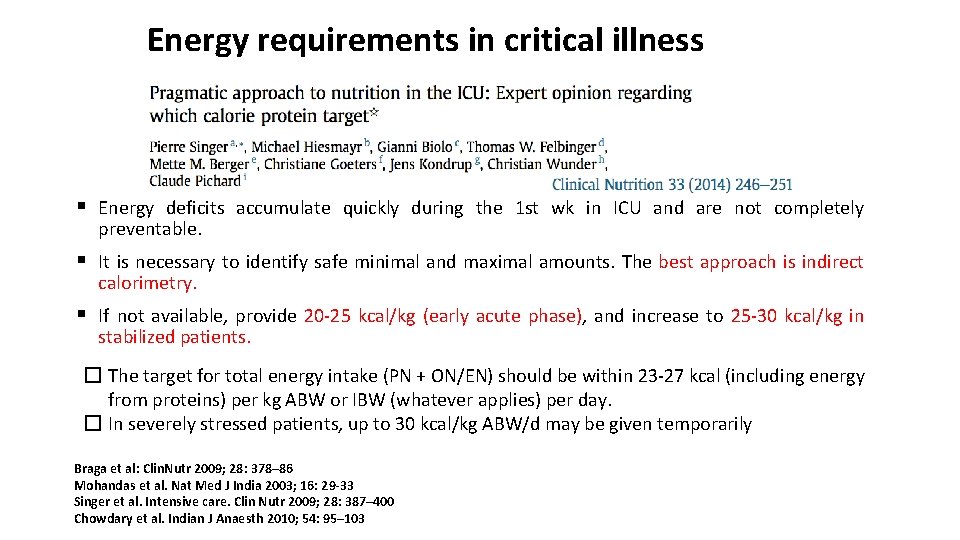
Energy requirements in critical illness § Energy deficits accumulate quickly during the 1 st wk in ICU and are not completely preventable. § It is necessary to identify safe minimal and maximal amounts. The best approach is indirect calorimetry. § If not available, provide 20 -25 kcal/kg (early acute phase), and increase to 25 -30 kcal/kg in stabilized patients. � The target for total energy intake (PN + ON/EN) should be within 23 -27 kcal (including energy from proteins) per kg ABW or IBW (whatever applies) per day. � In severely stressed patients, up to 30 kcal/kg ABW/d may be given temporarily Braga et al: Clin. Nutr 2009; 28: 378– 86 Mohandas et al. Nat Med J India 2003; 16: 29 -33 Singer et al. Intensive care. Clin Nutr 2009; 28: 387– 400 Chowdary et al. Indian J Anaesth 2010; 54: 95– 103
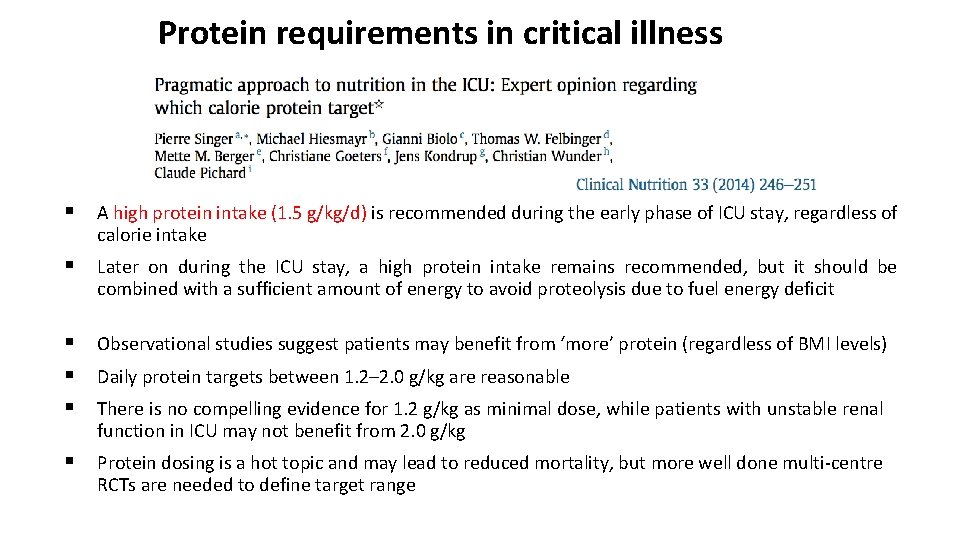
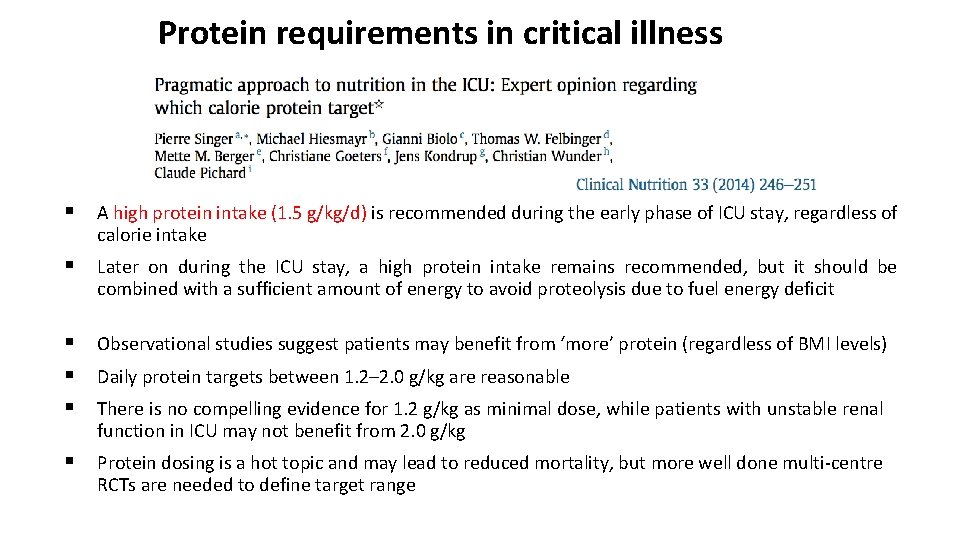
Protein requirements in critical illness § A high protein intake (1. 5 g/kg/d) is recommended during the early phase of ICU stay, regardless of calorie intake § Later on during the ICU stay, a high protein intake remains recommended, but it should be combined with a sufficient amount of energy to avoid proteolysis due to fuel energy deficit § § § Observational studies suggest patients may benefit from ‘more’ protein (regardless of BMI levels) § Protein dosing is a hot topic and may lead to reduced mortality, but more well done multi-centre RCTs are needed to define target range Daily protein targets between 1. 2– 2. 0 g/kg are reasonable There is no compelling evidence for 1. 2 g/kg as minimal dose, while patients with unstable renal function in ICU may not benefit from 2. 0 g/kg
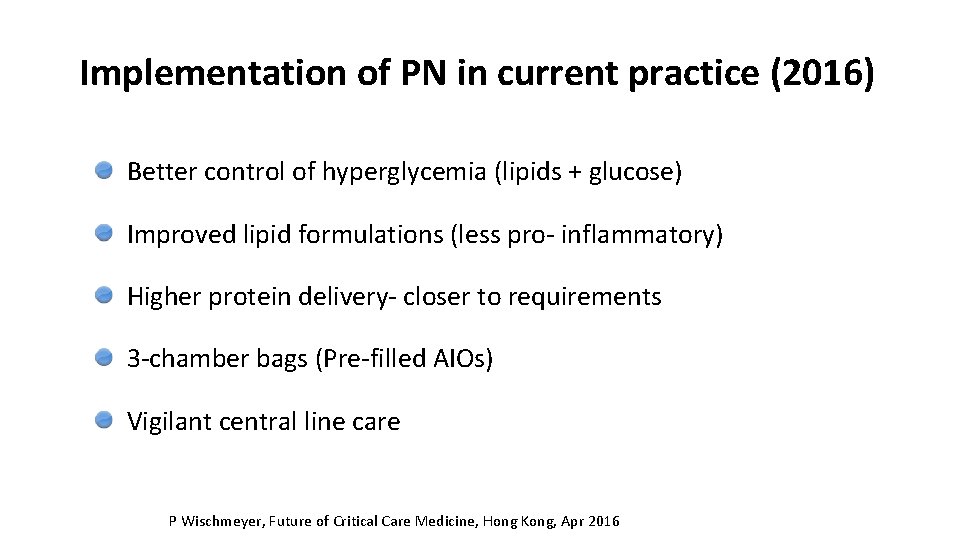
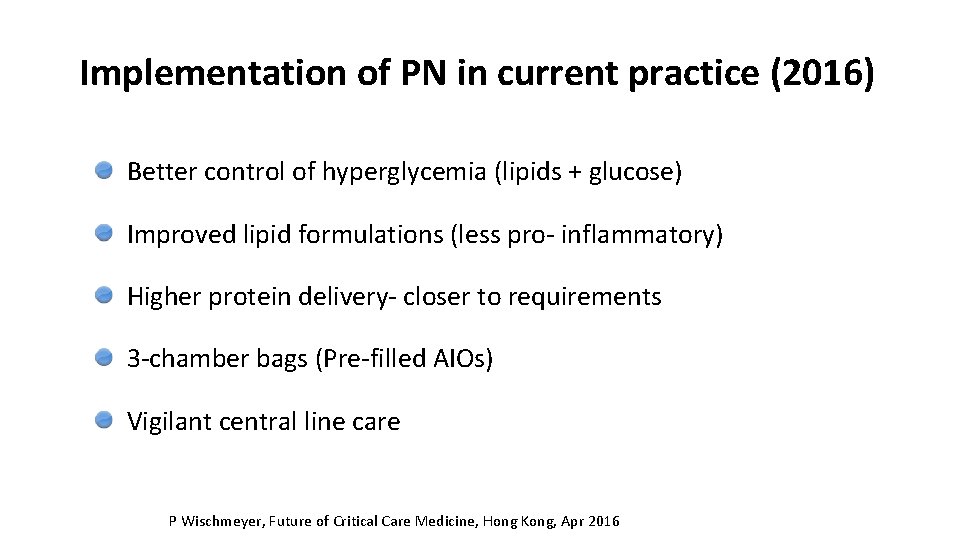
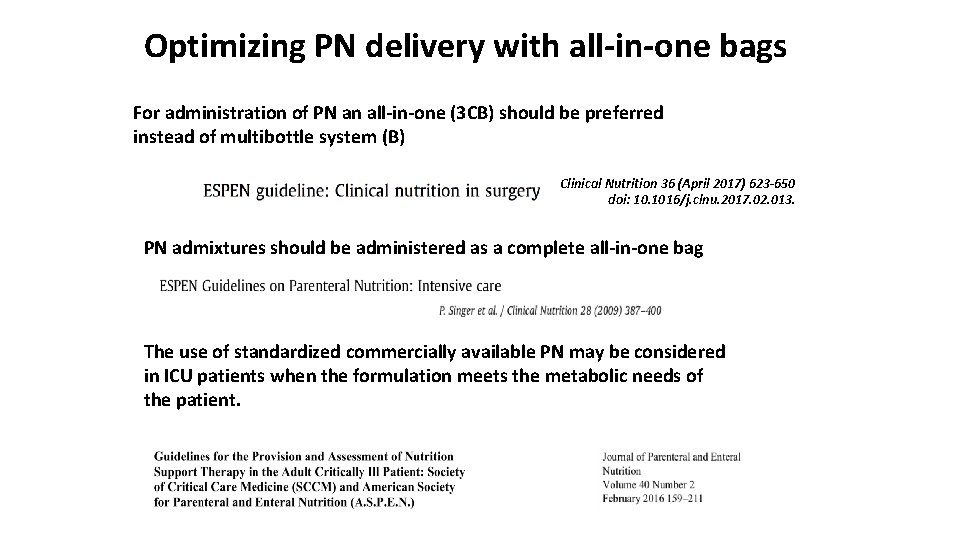
Implementation of PN in current practice (2016) Better control of hyperglycemia (lipids + glucose) Improved lipid formulations (less pro- inflammatory) Higher protein delivery- closer to requirements 3 -chamber bags (Pre-filled AIOs) Vigilant central line care P Wischmeyer, Future of Critical Care Medicine, Hong Kong, Apr 2016
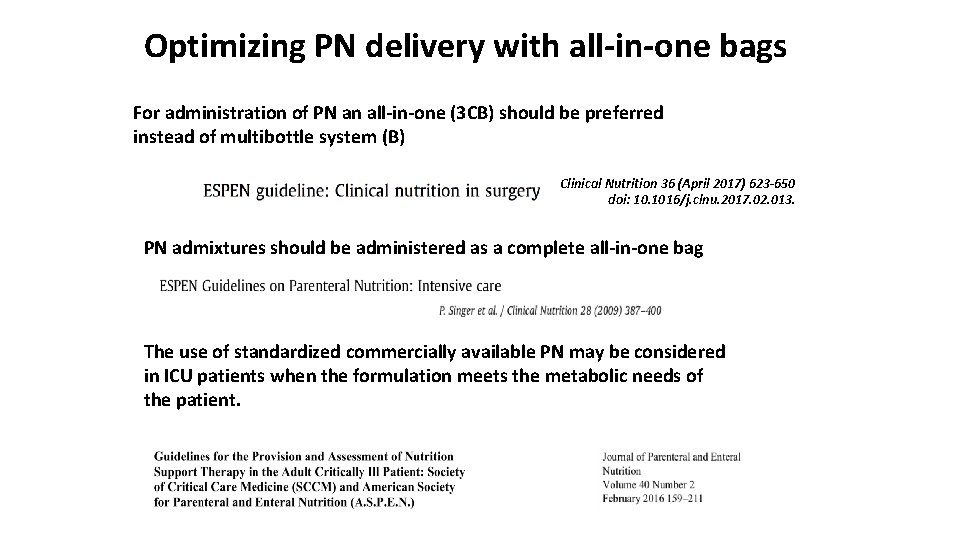
Optimizing PN delivery with all-in-one bags For administration of PN an all-in-one (3 CB) should be preferred instead of multibottle system (B) Clinical Nutrition 36 (April 2017) 623 -650 doi: 10. 1016/j. clnu. 2017. 02. 013. PN admixtures should be administered as a complete all-in-one bag The use of standardized commercially available PN may be considered in ICU patients when the formulation meets the metabolic needs of the patient.
Precise Nutrition with Precision Monitoring/Evaluation:
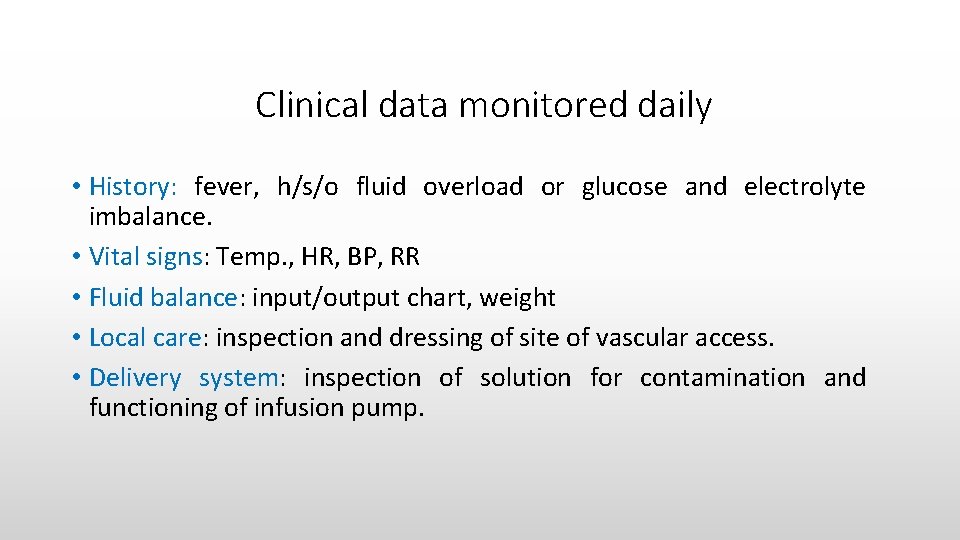
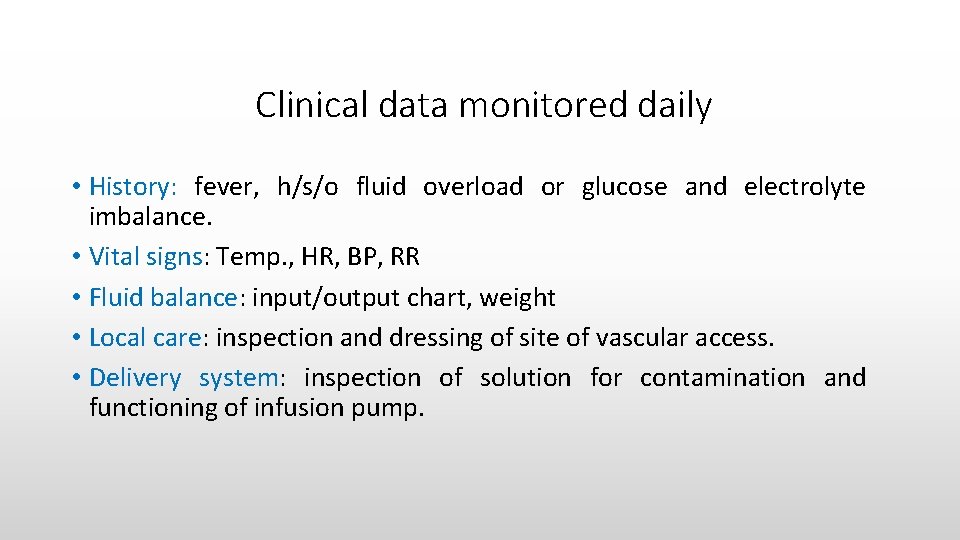
Clinical data monitored daily • History: fever, h/s/o fluid overload or glucose and electrolyte imbalance. • Vital signs: Temp. , HR, BP, RR • Fluid balance: input/output chart, weight • Local care: inspection and dressing of site of vascular access. • Delivery system: inspection of solution for contamination and functioning of infusion pump.
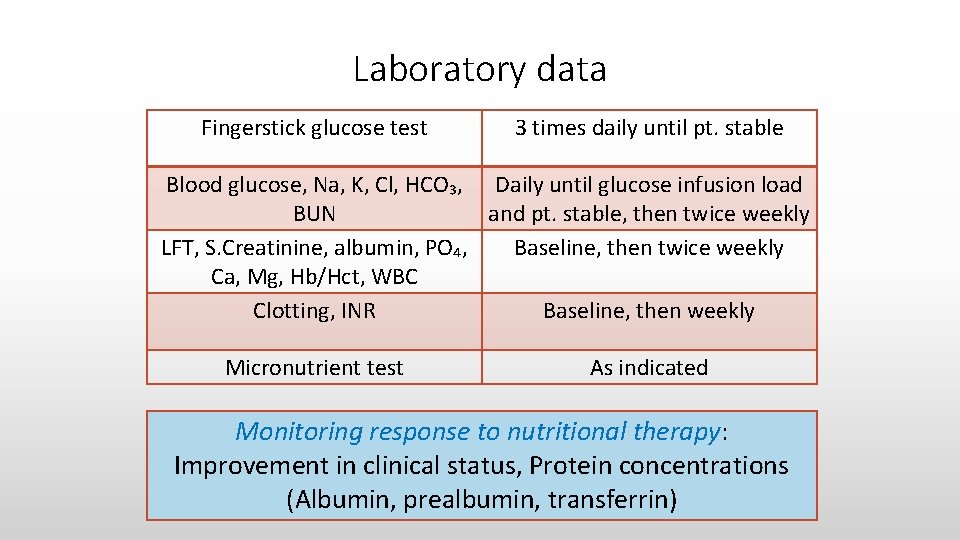
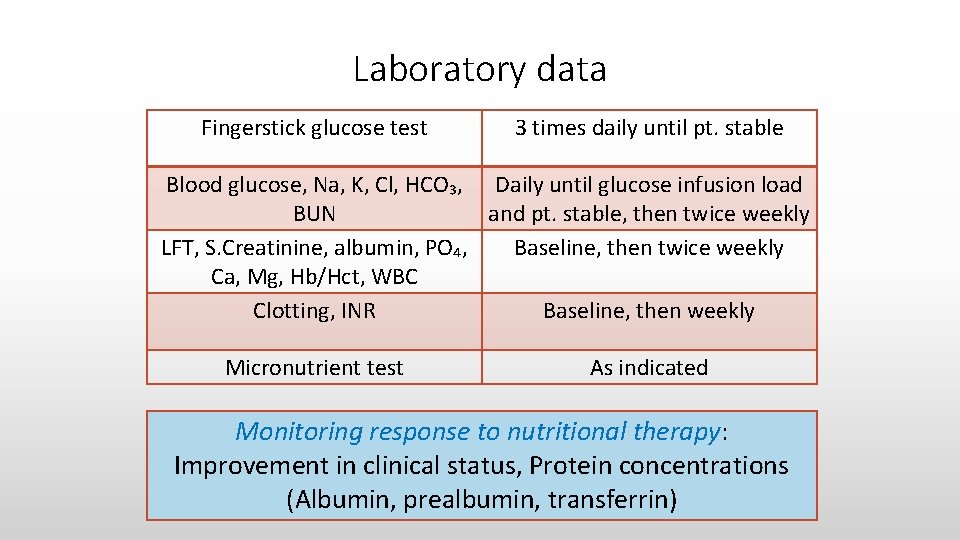
Laboratory data Fingerstick glucose test 3 times daily until pt. stable Blood glucose, Na, K, Cl, HCO₃, Daily until glucose infusion load BUN and pt. stable, then twice weekly LFT, S. Creatinine, albumin, PO₄, Baseline, then twice weekly Ca, Mg, Hb/Hct, WBC Clotting, INR Baseline, then weekly Micronutrient test As indicated Monitoring response to nutritional therapy: Improvement in clinical status, Protein concentrations (Albumin, prealbumin, transferrin)
To summarize nutrition therapy…. • Patients admitted in ICU should be screened for pre-existing malnutrition or nutrition risk (for nutrition related complications). • When nutrition risk is identified, it should be optimized by provision of appropriate nutrition therapy. • Early EN provides both nutritional benefits as well as non-nutritional benefits, but may be associated with poor tolerance due to the gut dysfunction associated with critical illness. • Early supplemental PN assures adequate delivery of energy, protein & nutrients to minimize risk and improve clinical outcomes. Enhance nutrition with specialized substrates like Immunonutrients