Precepting Across A Spectrum of Student Abilities Becky
Precepting Across A Spectrum of Student Abilities Becky Brady, Pharm. D, Associate Professor of Pharmacy Practice Chelsea Sanchez, Pharm. D, Assistant Professor of Pharmacy Practice University of the Incarnate Word, Feik School of Pharmacy October 2016 Preceptor CE
Disclosure • Rebecca Brady and Chelsea Sanchez have no conflict of interest or financial disclosures to make in relation to this presentation. 2
Objectives 1) Integrate Rx. Preceptor into the student experience to improve efficiency with preceptor responsibilities. 2) Identify strategies to improve student performance during the pharmacy practice experience. 3) Identify strategies to enhance the pharmacy practice experience for high-performing students. 3
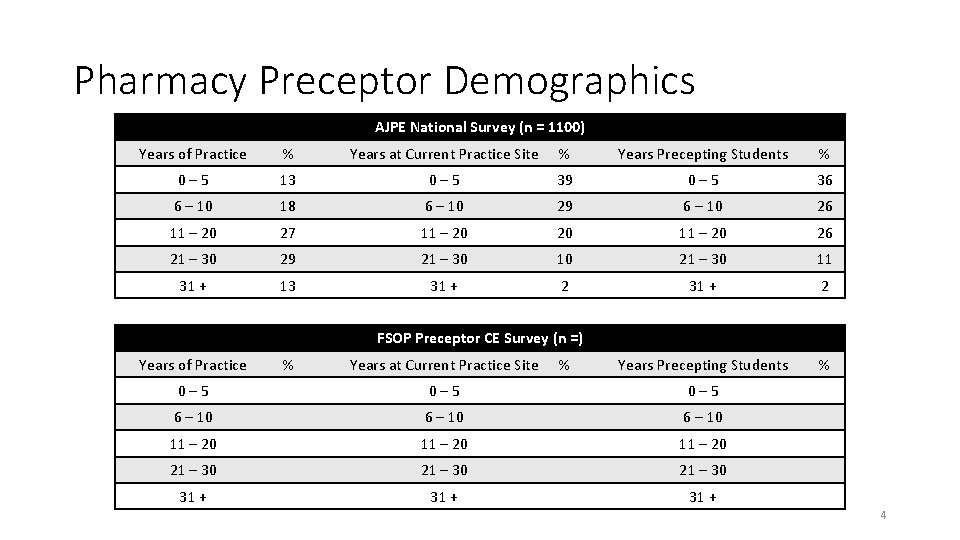
Pharmacy Preceptor Demographics AJPE National Survey (n = 1100) Years of Practice % Years at Current Practice Site % Years Precepting Students % 0 – 5 13 0 – 5 39 0 – 5 36 6 – 10 18 6 – 10 29 6 – 10 26 11 – 20 27 11 – 20 26 21 – 30 29 21 – 30 10 21 – 30 11 31 + 13 31 + 2 Years Precepting Students % FSOP Preceptor CE Survey (n =) Years of Practice % Years at Current Practice Site % 0 – 5 6 – 10 11 – 20 21 – 30 31 + 4

Preceptor Site Features AJPE National Survey (n = 1100) Practice Site FSOP Preceptor Pre-CE Survey (n = ) % Institution Practice Site % Institution Public 60 Public Private 40 Private Pharmacy Practice Setting Teaching Hospital 24 Teaching Hospital 27 Hospital Clinic 9 Clinic Community Chain 15 Community Chain Community Independent 10 Community Independent Nursing Home 2 Nursing Home Industry 2 Industry Other 13 Other 5
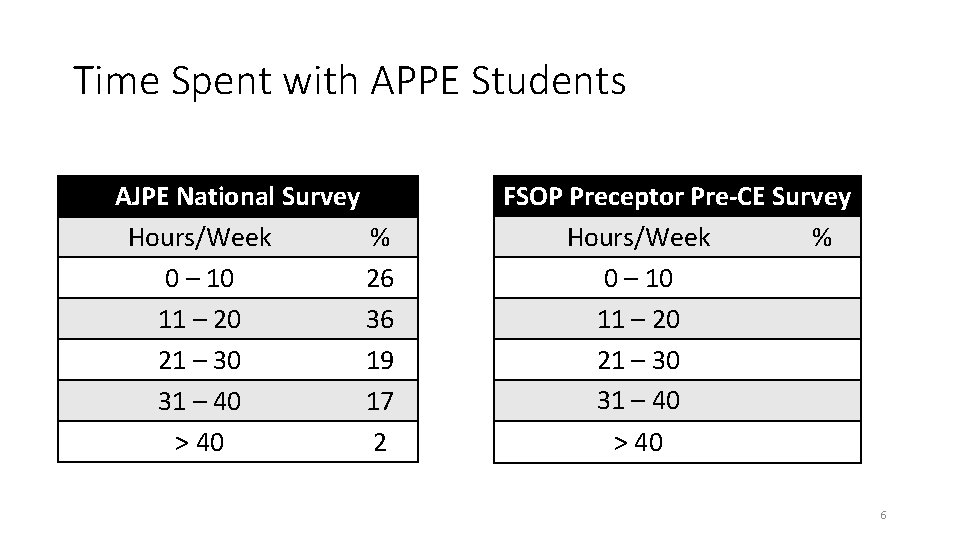
Time Spent with APPE Students AJPE National Survey Hours/Week % 0 – 10 26 11 – 20 36 21 – 30 19 31 – 40 17 > 40 2 FSOP Preceptor Pre-CE Survey Hours/Week % 0 – 10 11 – 20 21 – 30 31 – 40 > 40 6
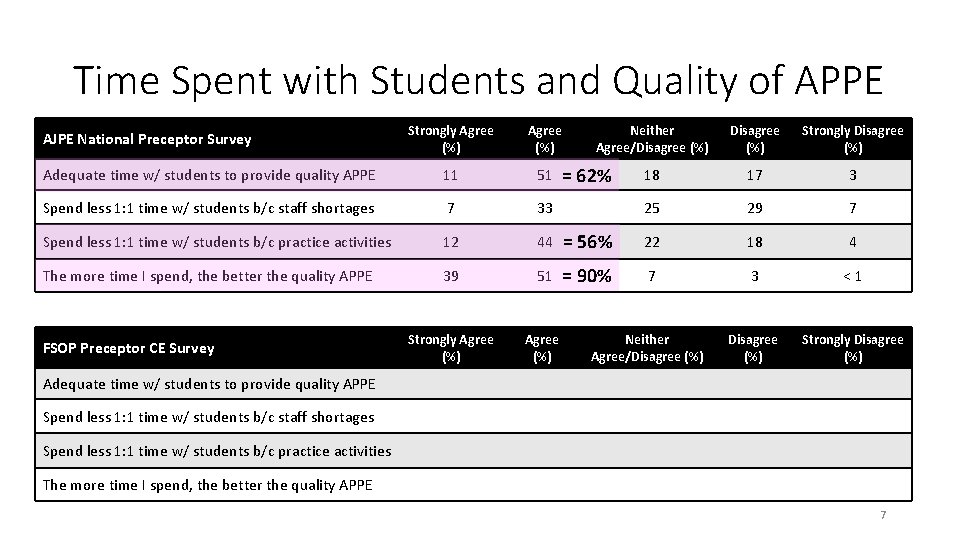
Time Spent with Students and Quality of APPE Strongly Agree (%) Adequate time w/ students to provide quality APPE 11 51 Spend less 1: 1 time w/ students b/c staff shortages 7 33 Spend less 1: 1 time w/ students b/c practice activities 12 44 The more time I spend, the better the quality APPE 39 51 Strongly Agree (%) AJPE National Preceptor Survey FSOP Preceptor CE Survey Neither Agree/Disagree (%) Strongly Disagree (%) 18 17 3 25 29 7 = 56% 22 18 4 = 90% 7 3 < 1 Disagree (%) Strongly Disagree (%) = 62% Neither Agree/Disagree (%) Adequate time w/ students to provide quality APPE Spend less 1: 1 time w/ students b/c staff shortages Spend less 1: 1 time w/ students b/c practice activities The more time I spend, the better the quality APPE 7
Take-Away • Time spent with students improves quality of experience • Work responsibilities can limit the amount of time with students • Solution • Increase efficiency • Maximize time with students • Student play active role in recognizing their learning opportunities 8
Become an Efficient and Effective Preceptor • Get organized • Communicate clearly and quickly • Students should have active role in documenting their activities 9
Get Organized: Set-up Rx. Preceptor Profile • Rotation description • Rotation expectations and requirements • Calendar • Pre-APPE Questionnaire • Supporting documents • Assigned readings • Rubrics • Etc. 10
Rotation Description: Match Student Interest with Rotation • Patient population description • Hours of attendance • Typical daily activities • Homework • Presentation requirements 11
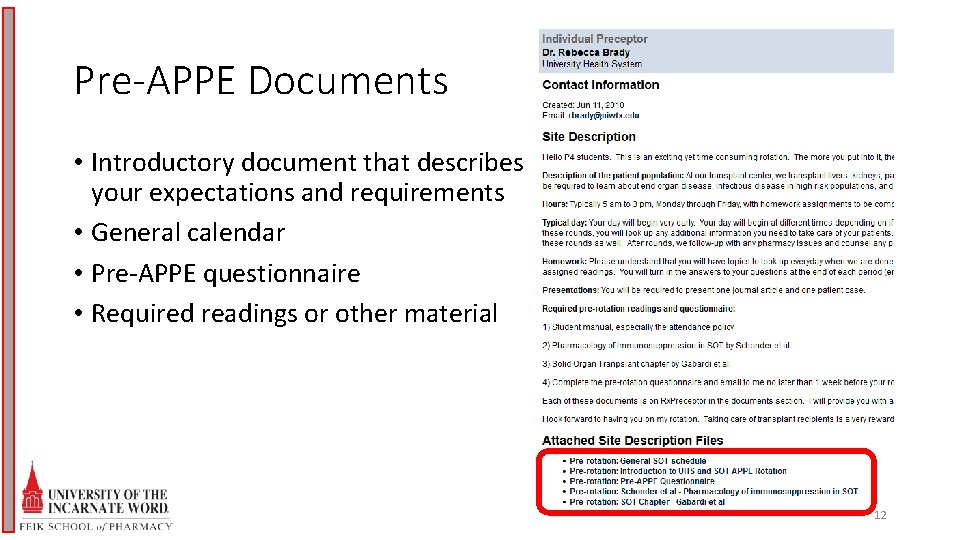
Pre-APPE Documents • Introductory document that describes your expectations and requirements • General calendar • Pre-APPE questionnaire • Required readings or other material 12
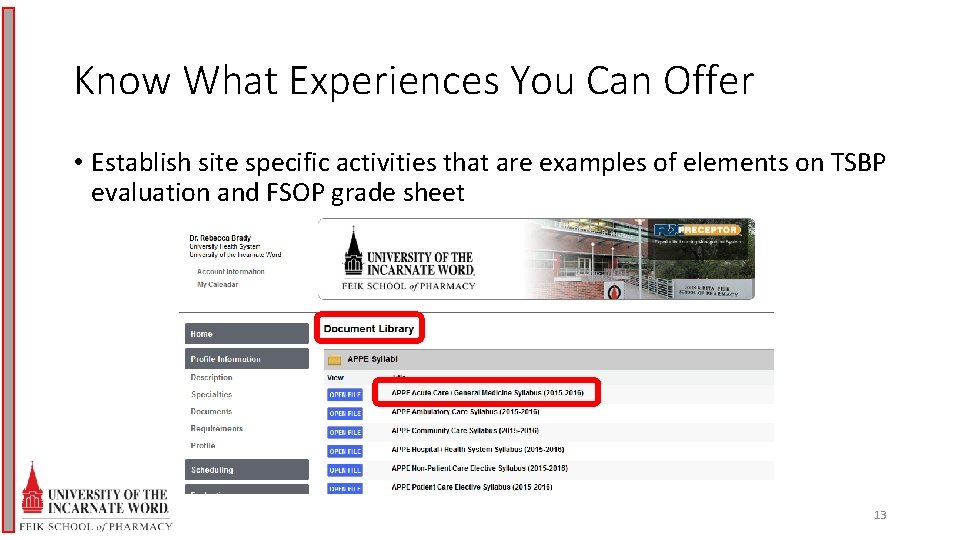
Know What Experiences You Can Offer • Establish site specific activities that are examples of elements on TSBP evaluation and FSOP grade sheet 13
Group Work (5 – 10 mins) • Use APPE syllabus to write specific examples of activities that will meet TSBP elements • Consider what performance would be • Minimum competency: all students should perform by end of rotation • Average: most students should perform by end of rotation • High-performance: above average students activities for those that exceed your expectations 14
Discussion (10 mins) MONITORS AND EVALUATES DRUG THERAPY: INITIAL AND ONGOING • Establishes and interprets data bases • Includes active problems, PMH, pertinent PE, lab data and hospital course in data base • Performs and completes patient medication history • Completes and updates medication profiles • Determines pharmacokinetic parameters • Uses sunrise (electronic medical record) to identify pertinent labs and exams in ‘results tab’ and vitals in ‘flowsheet tab’ • Uses sunrise antimicrobial filter to determine current antibiotic duration when treating infections • Able to list current problems for de-novo transplant recipients that includes transplant, current inpatient problems, and comorbidities to help assess patient’s readiness for discharge • Performs medication reconciliation on all de-novo transplant recipients • Updates ‘Med. Action. Plan’ and preceptor checks without requiring major intervention • Recommends vancomycin dosing based on trough levels 15
Day 1 Orientation • Have a checklist! • Go over all the rules • Attendance, dress-code, professionalism • Review activities that will meet elements • Review TSBP grading criteria • Explain end-of-day, end-of-week expectations • Find out student’s specific goals • If none, then identifying goals should be an objective on mid-point evaluation 16
The Importance of the Mid-Point • If they are documenting in Rx. Preceptor, then they should know how they are performing • Identify areas not successfully passing • Set-up goals for remaining three weeks 17
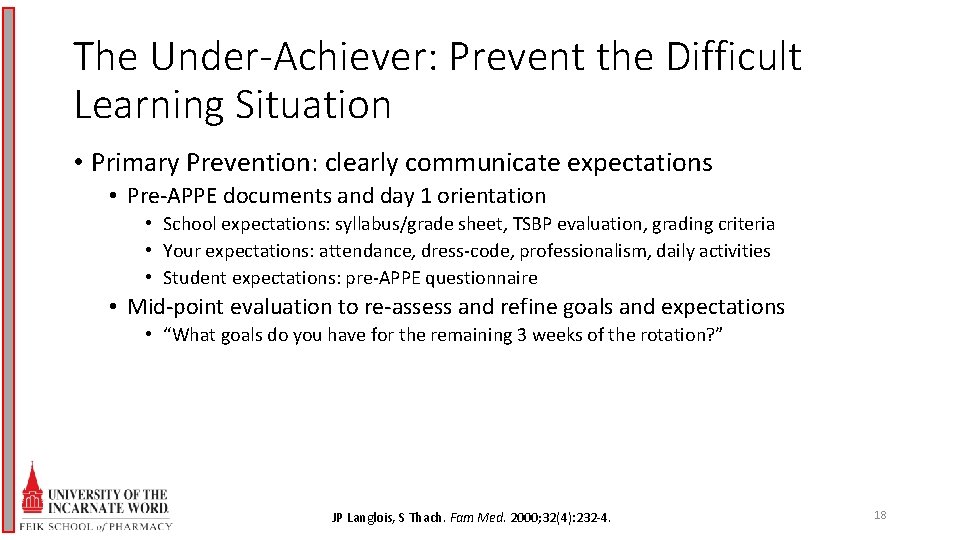
The Under-Achiever: Prevent the Difficult Learning Situation • Primary Prevention: clearly communicate expectations • Pre-APPE documents and day 1 orientation • School expectations: syllabus/grade sheet, TSBP evaluation, grading criteria • Your expectations: attendance, dress-code, professionalism, daily activities • Student expectations: pre-APPE questionnaire • Mid-point evaluation to re-assess and refine goals and expectations • “What goals do you have for the remaining 3 weeks of the rotation? ” JP Langlois, S Thach. Fam Med. 2000; 32(4): 232 -4. 18
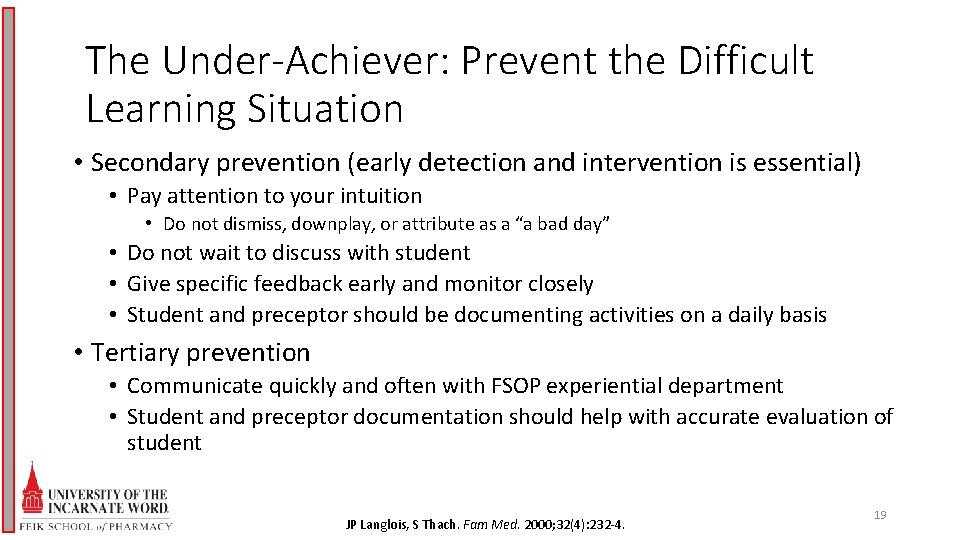
The Under-Achiever: Prevent the Difficult Learning Situation • Secondary prevention (early detection and intervention is essential) • Pay attention to your intuition • Do not dismiss, downplay, or attribute as a “a bad day” • Do not wait to discuss with student • Give specific feedback early and monitor closely • Student and preceptor should be documenting activities on a daily basis • Tertiary prevention • Communicate quickly and often with FSOP experiential department • Student and preceptor documentation should help with accurate evaluation of student JP Langlois, S Thach. Fam Med. 2000; 32(4): 232 -4. 19
The Under-Achiever: Manage the Difficult Learning Situation • Think of using “SOAP” format • Subjective • Chief-complaint and HPI • Clearly state what you have noticed • Ask what other staff have noticed • Establish pattern of behavior • Objective • Document evidence! JP Langlois, S Thach. Fam Med. 2000; 32(5): 307 -309. 20
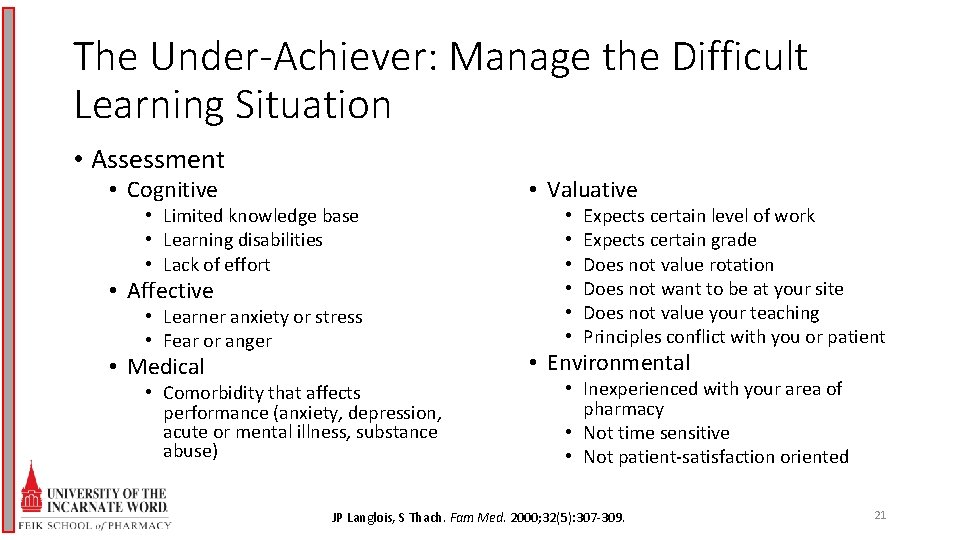
The Under-Achiever: Manage the Difficult Learning Situation • Assessment • Cognitive • Limited knowledge base • Learning disabilities • Lack of effort • Affective • Learner anxiety or stress • Fear or anger • Medical • Comorbidity that affects performance (anxiety, depression, acute or mental illness, substance abuse) • Valuative • • • Expects certain level of work Expects certain grade Does not value rotation Does not want to be at your site Does not value your teaching Principles conflict with you or patient • Environmental • Inexperienced with your area of pharmacy • Not time sensitive • Not patient-satisfaction oriented JP Langlois, S Thach. Fam Med. 2000; 32(5): 307 -309. 21
The Under-Achiever: Manage the Difficult Learning Situation • Plan • • • Discuss with student your assessment Gather information as to why the problem is occurring Identify strategies to improve student performance Identify monitoring plan for follow-up Document student performance after intervention JP Langlois, S Thach. Fam Med. 2000; 32(5): 307 -309. 22
Provide Effective Feedback • Ongoing process • Nonjudgmental information to help student build on foundation of skills and behaviors • Should be frequent, face-to-face, and brief (“small doses”) • Environment: neutral, private setting • Timing: as soon as possible after the interaction • Interaction can be brief and specific ST Wilkinson, R Couldry, H Phillips et al. Hosp Pharm. 2013; 48(1): 26 -32 23
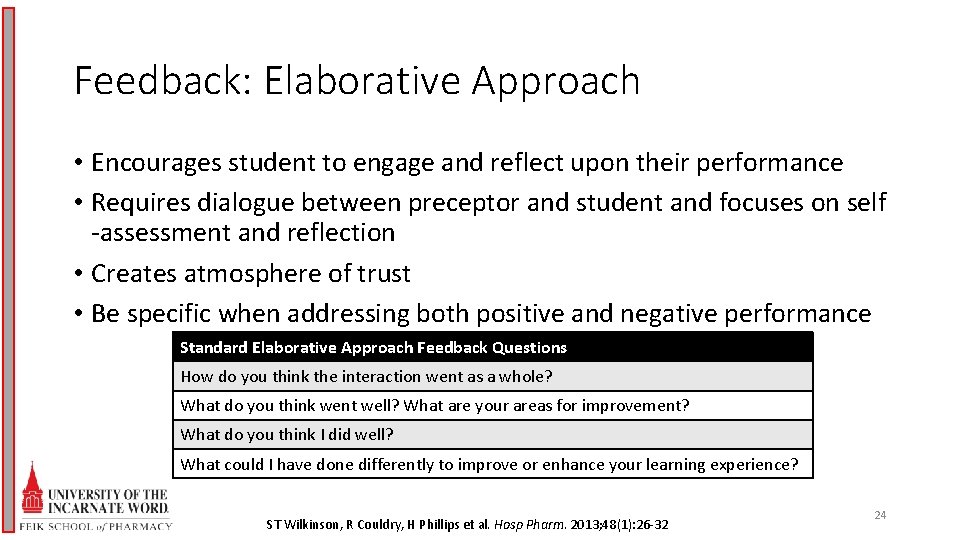
Feedback: Elaborative Approach • Encourages student to engage and reflect upon their performance • Requires dialogue between preceptor and student and focuses on self -assessment and reflection • Creates atmosphere of trust • Be specific when addressing both positive and negative performance Standard Elaborative Approach Feedback Questions How do you think the interaction went as a whole? What do you think went well? What are your areas for improvement? What do you think I did well? What could I have done differently to improve or enhance your learning experience? ST Wilkinson, R Couldry, H Phillips et al. Hosp Pharm. 2013; 48(1): 26 -32 24
Challenges for Effective Feedback • Interpersonal factors between student and preceptor • Have to provide negative feedback • Use “feedback sandwich” • Positive comment, negative comment, positive comment • Provide suggestion on how to improve instead of just stating what was wrong • Similar to conflict resolution skills ST Wilkinson, R Couldry, H Phillips et al. Hosp Pharm. 2013; 48(1): 26 -32 A Dohrenwend. Fam Pract Management. Nov/Dec 2002. Available at: www. aafp. org/fpm. Accessed on: 10/10/16 25
Conflict Resolution • Listen • Give clear feedback • Document • Write down the key points and details • Be consistent • Set consequences • Adhere to FSOP’s process • Manage your self-talk • Be courageous E Anderson. Ways to deal with difficult employees. Available at: http: //www. forbes. com; Accessed on 10/10/16. 26
Student Cases (5 – 10 mins) • Discuss each case in your group • Answer the questions • Add your own experiences and thoughts 27
The Over-Achiever • What is your definition of an ‘over-achiever? ’ • Student goals important • Think “outside the box” for extra projects that will enhance student experience • Clinical rotation • present topic to the team, nurse education, participate in DUE, submit patient case as abstract to a meeting • Community practice • OTC counseling, HTN monitoring, topic presentation to staff, participate in community education presentation 28
Conclusions • To improve efficiency as a preceptor • Organizing your rotation at the beginning of the academic year • Student involvement in documenting competency achievement • Improving student performance • Immediate discussion with the student • Practice listening and communication skills • Develop plan for improvement with monitoring • Enhancing the rotation for high-performing students • Identify the student’s goals • Have list of ‘high-performing’ activities ready to go 29
References for Pharmacists • LM Cuellar, DB Ginsburg. Preceptor’s Handbook for Pharmacists. 3 rd ed. American Society of Health-System Pharmacists, Inc. 2016. • MM Soric. Maximize Your Rotations: ASHP’s Student Guide to IPPEs, APPEs, and Beyond. American Society of Health-System Pharmacists, Inc. 2013. • ASHP’s – Preceptor Skills. • Available at: http: //www. ashp. org/preceptorskills • Membership required to access most articles • Pharmacist’s Letter – Preceptor Toolbox. • Available at: pharmacistsletter. com • Membership required 30
- Slides: 30