PRECEDENTSETTING LEGAL CASES AND THEIR IMPACT ON CREDENTIALING


- Slides: 23
PRECEDENT-SETTING LEGAL CASES AND THEIR IMPACT ON CREDENTIALING & PRIVILEGING
Healthcare Organization Liability The primary purpose of credentialing is to protect health care organizations from the legal liability that could result from the actions of unqualified providers. Medical centers have a duty to credential carefully because they are ultimately responsible for arranging and coordinating the health care for their patients.
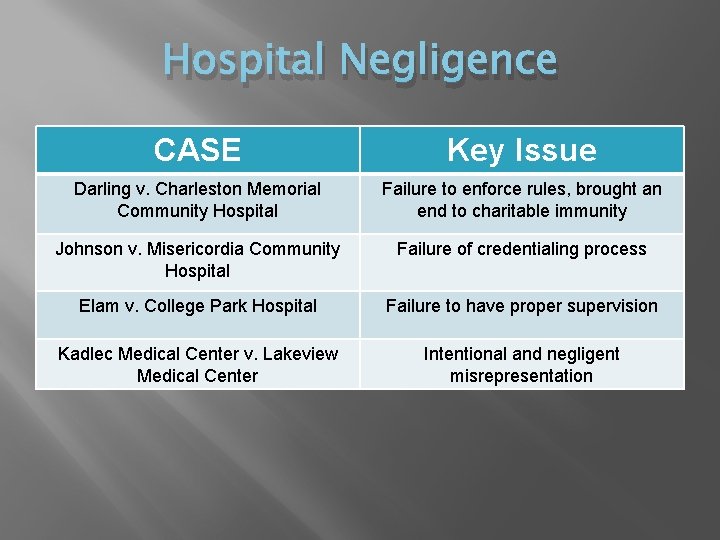
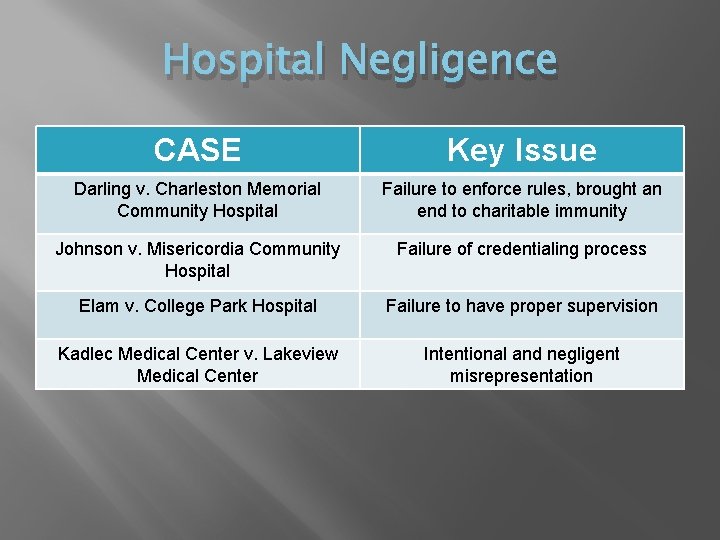
Hospital Negligence CASE Key Issue Darling v. Charleston Memorial Community Hospital Failure to enforce rules, brought an end to charitable immunity Johnson v. Misericordia Community Hospital Failure of credentialing process Elam v. College Park Hospital Failure to have proper supervision Kadlec Medical Center v. Lakeview Medical Center Intentional and negligent misrepresentation
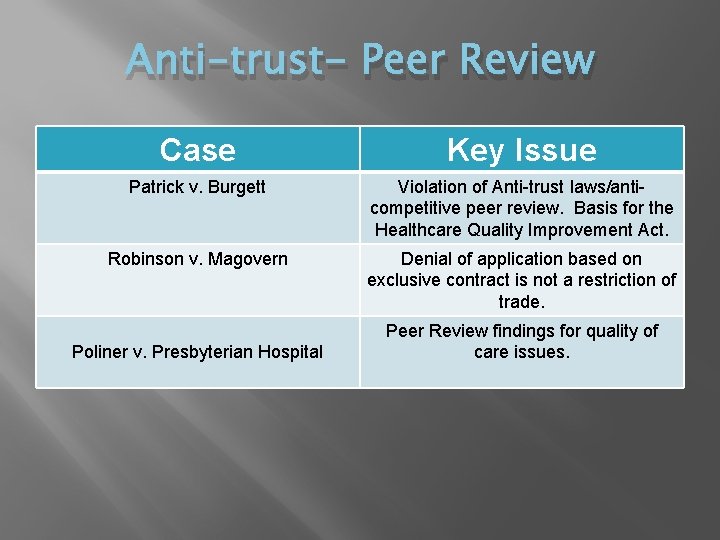
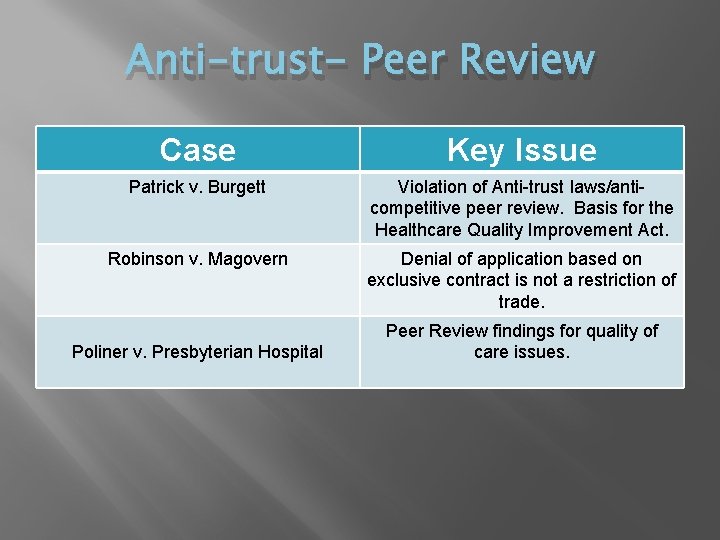
Anti-trust- Peer Review Case Key Issue Patrick v. Burgett Violation of Anti-trust laws/anticompetitive peer review. Basis for the Healthcare Quality Improvement Act. Robinson v. Magovern Denial of application based on exclusive contract is not a restriction of trade. Poliner v. Presbyterian Hospital Peer Review findings for quality of care issues.
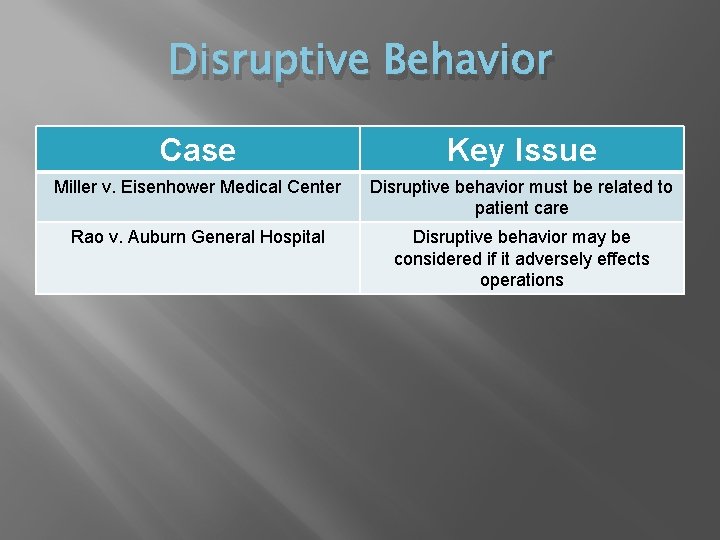
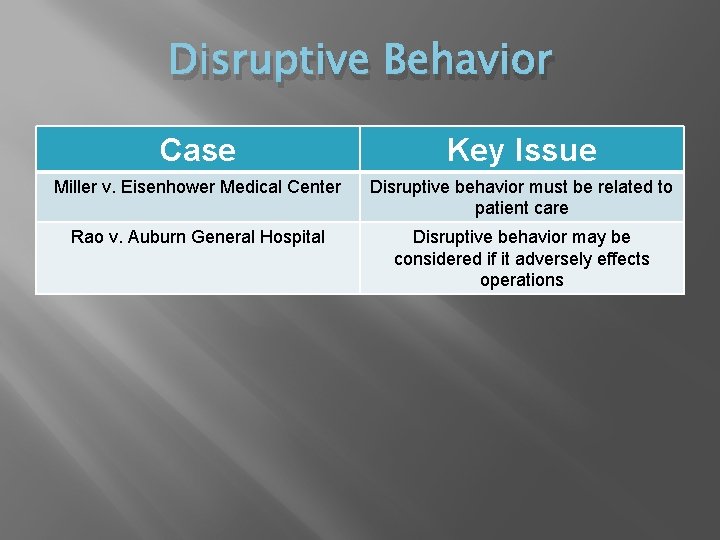
Disruptive Behavior Case Key Issue Miller v. Eisenhower Medical Center Disruptive behavior must be related to patient care Rao v. Auburn General Hospital Disruptive behavior may be considered if it adversely effects operations
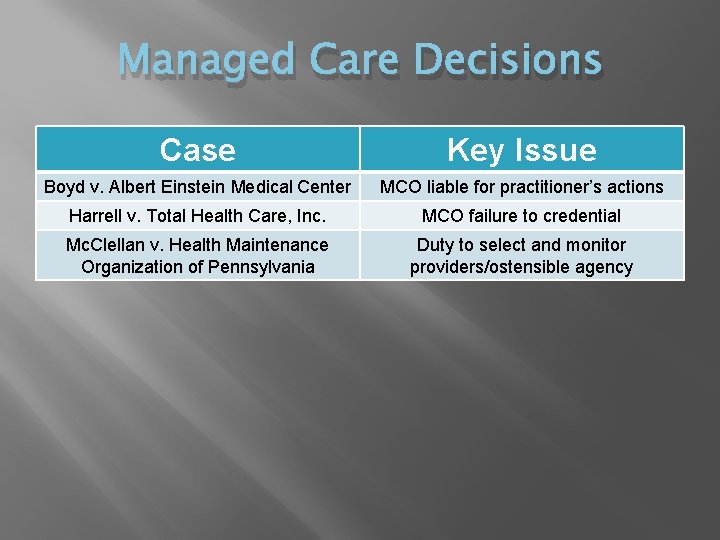
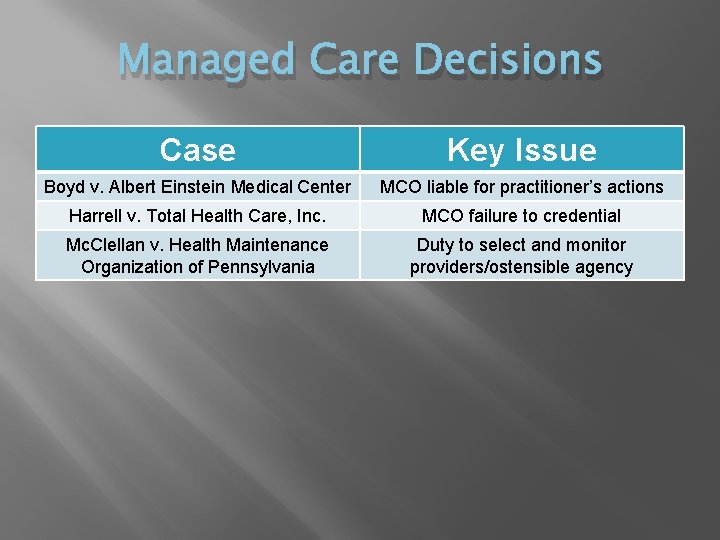
Managed Care Decisions Case Key Issue Boyd v. Albert Einstein Medical Center MCO liable for practitioner’s actions Harrell v. Total Health Care, Inc. MCO failure to credential Mc. Clellan v. Health Maintenance Organization of Pennsylvania Duty to select and monitor providers/ostensible agency
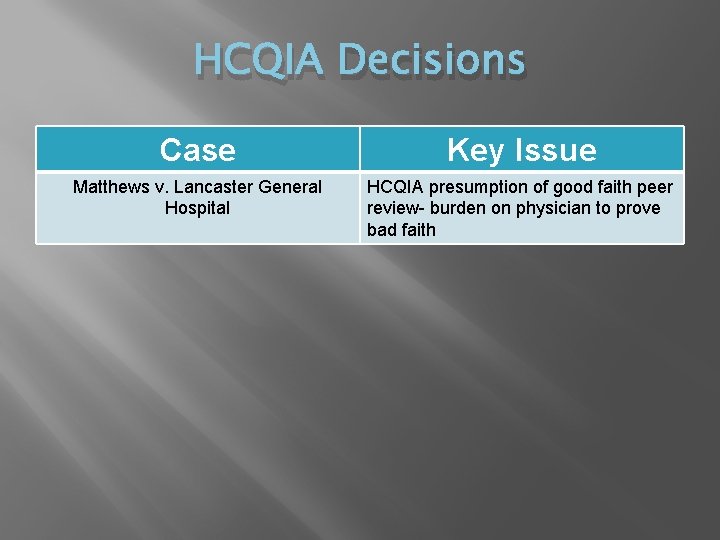
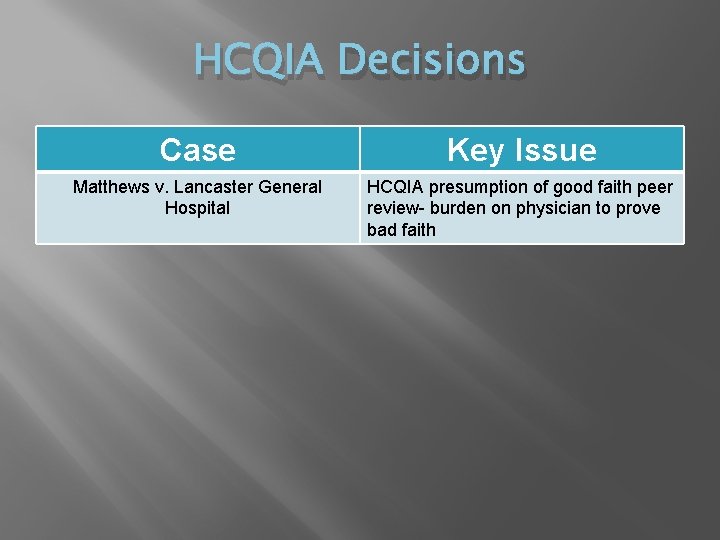
HCQIA Decisions Case Key Issue Matthews v. Lancaster General Hospital HCQIA presumption of good faith peer review- burden on physician to prove bad faith
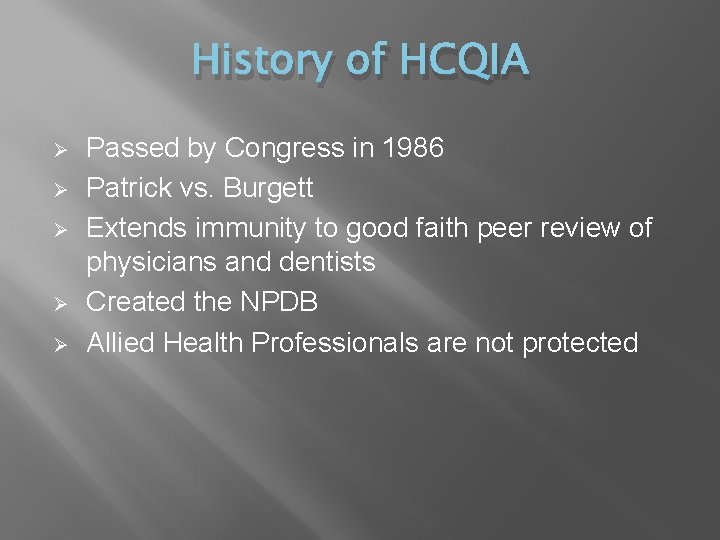
History of HCQIA Ø Ø Ø Passed by Congress in 1986 Patrick vs. Burgett Extends immunity to good faith peer review of physicians and dentists Created the NPDB Allied Health Professionals are not protected
Coverage Ø Ø Ø Professional review bodies Members and/or staff of those bodies Those under contract with those bodies Anyone who participates or assists the bodies with respect to action Those who provide information regarding competence/conduct unless the information is false and the person giving the information knew it was false.
Exceptions Ø Ø Ø Health care entities failing to meet the standards for immunity Health care entities failing to report information to the NPDB Once the determination is made that the entity failed to report, immunity protection can be taken away for up to three years
Standards for Immunity Ø Ø Ø Be carried out with the reasonable belief that the action was taken to further quality health care Follow a reasonable effort, through investigations and review, to obtain the facts Meet adequate notice and fair hearing procedures afforded to the physician or dentist
National Practitioner Data Bank Ø Health care professionals covered: Physicians and Dentists must be reported if required under the reporting standards Ø Hospitals and health care entities may report professional review actions against other licensed health care practitioners (such as podiatrists or psychologists) but they are not required to even if the practitioners are medical staff members. Ø
NPDB Reporting ØMedical Malpractice Payments ØReported by the entity ØPayments made by individuals not reportable ØUp to $10, 000 fine to entities who fail to report ØLicensure Actions ØAction based on professional competence or conduct ØDenial of initial licensure not reportable ØFailure to report may result in the state licensing board losing its reporting responsibility
NPDB Reporting (continued) ØClinical Privilege Actions ØAdverse actions against clinical privileges or membership based on professional competence or conduct and lasting longer than 30 days, and any surrender or restriction of clinical privileges by a physician or dentist while under investigation or to avoid investigation or corrective action ØFailure to report could lead to loss of eligibility for HCQIA immunity for up to three years ØMay report other health care practitioners (but are not required to) ØReport must be sent to current state licensing boards within 15 days of effective date of adverse action. State licensing board has 15 days to respond to the NPDB
NPDB Reporting (continued) ØSociety Membership Actions ØAdverse actions taken against membership when the action is reached through a formal peer review process and when the action is based on the practitioner’s professional competence and conduct ØFailure to report may lead to loss of HCQIA immunity protection for up to three years
Querying the NPDB Ø Ø Ø Ø Hospitals for practitioners with privileges at initial granting and at least every two years thereafter Hospitals when considering new or additional clinical privileges Hospitals may query at other times when they deem necessary State licensing boards may query Other health care entities may query when entering into employment arrangements Plaintiff’s attorneys may query under specific circumstances Self query
Who’s Reported? Ø Ø Licensed health care practitioners Providers (hospital and other health care entities that provide health care services and follow formal peer review processes for the purposes of furthering quality health care and any other health care entity that directly or through contract provide health care services

What is Reported? Ø Ø Ø Ø Ø Medical malpractice payments (all health care practitioners) Any adverse licensure actions (all practitioners or entities) --revocation, reprimand, censure, suspension, probation --any dismissal or closure of the proceedings by reason of the practitioner or entity surrendering the license or leaving the State or jurisdiction --Any other loss of license Final Adjudicated adverse clinical privileging actions Adverse professional society membership actions Any negative action or finding by a State licensing or certification authority Peer review organization negative actions or findings against health care practitioners Private accreditation organization negative actions or findings against health entities Adverse Actions against DEA Certification Medicare/Medicaid Exclusions
Who Reports? Ø Ø Ø Ø Ø Medical malpractice payers State health care practitioner licensing and certification authorities (including medical and dental boards) Hospitals Other health care entities with formal peer review (HMOs, group practices, managed care organizations) Professional societies with formal peer review State entity licensing and certification authorities Peer review organizations Private accreditation organizations DEA HHS OIG

Who Queries? Ø Ø Ø Ø Hospitals Other health care entities, with formal peer review Professional societies with formal peer review State health care practitioner licensing and certification authorities (including medical and dental boards) State entity licensing and certification authorities* Agencies or contractors administering Federal health care programs* State agencies administering State health care programs* State Medicaid Fraud Units* U. S. Comptroller General* U. S. Attorney General and other law enforcement* Health care practitioners (self query) Plaintiff’s attorney/pro se plaintiffs (under limited circumstances)** Quality Improvement Organizations* Researchers (statistical data only) * Eligible to receive only those reports authorized by section 1921. ** Eligible to receive only those reports authorized by HCQIA
Case Study Dr. Harris resigned at the time of reappointment based on questions raised about compliance with record keeping requirements. This was discovered through a medical record audit which revealed a continuous pattern of not seeing patients within 24 hours of their admission and not completing histories and physicals within 48 hours of discharge (which failures led to adverse patient consequences, including one patient death)
Case Study Challenges? ? What if an investigation, corrective action or medical staff due process is never triggered? Ø Ø Ø Employment agreements Exclusive contracts Other arrangements
Questions? ?