Precancerous Lesions Oral Cancer Dr Sheetal Rai Asst






















- Slides: 49

Precancerous Lesions & Oral Cancer Dr Sheetal Rai Asst Prof Dept of ENT Yenepoya Medical College
Contents • Introduction • Classification of precancerous lesions & conditions • Leukoplakia • Erythroplakia • Carcinoma in Situ • Oral lichen planus • Oral submucous fibrosis

Introduction • Precancerous lesion • “Morphologically altered tissue in which cancer is more likely to occur, than in its apparently normal counterpart” • Precancerous condition • “Generalized state of the body, which is associated with a significantly increased risk of cancer”
PREMALIGNANT LESIONS • Leukoplakia • Erythroplakia • Carcinoma in situ • Bowens disease • Actinic keratosis & chelitis • Dyskeratosis follicularis
PREMALIGNANT CONDITIONS • Oral submucous fibrosis • Oral lichen planus • Syphilitic glossitis • Sideropenic dysphagia • Dyskeratosis congenita
Leukoplakia • The term LEUKOPLAKIA was first coined by a Hungarian Dermatologist SCHWIMMER in 1877 • Originates from Greek words – “leucos” - white and “plakia” - patch • WHO 1978 • “A white patch or plaque in the oral cavity which cannot be scrapped off or stripped off easily & more over, which cannot be characterized clinically or pathologically as

Epidemiology 1. Prevalence • Represents 85% of all oral precancers 2. Incidence 3 – 4 % of adult population 3. Age Usually in the 4 th – 6 th decades of life 4. Sex Males have the highest incidence, with the trend changing gradually

Classification of leukoplakia (Axell & Pindborg et al 1983) • Based on CLINICAL TYPE: Ø Homogenous Ø Non homogenous • Based on ETIOLOGY: Ø Tobacco associated Ø Idiopathic • Based on EXTENT: Ø Localized Ø Diffuse

• Based on risk of MALIGNANT TRANSFORMATION Ø High risk sites Floor of mouth Lateral/ventral surface of tongue Soft palate Ø Low risk sites Dorsum of tongue Hard palate • Based on HISTOLOGY: Ø Dysplastic Ø Non dysplastic

Etiopathogenesis • Tobacco – most imp offending agent • Alcohol • Chronic irritation • Syphilis • Nutritional deficiency • Actinic radiation • Galvanism
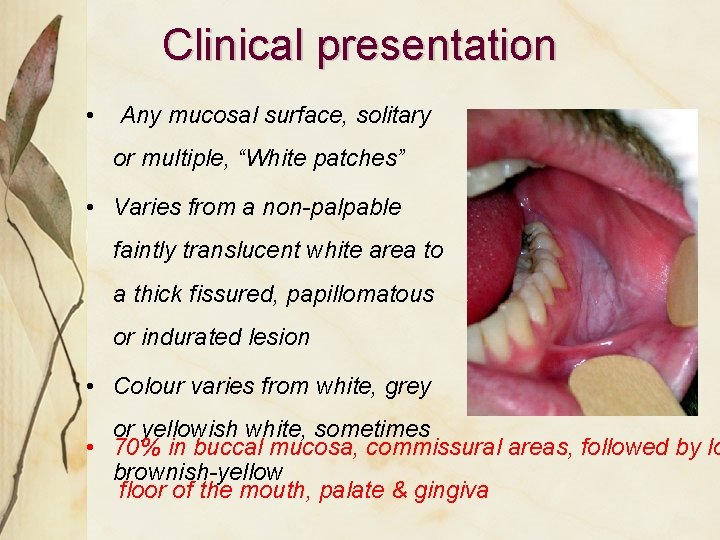
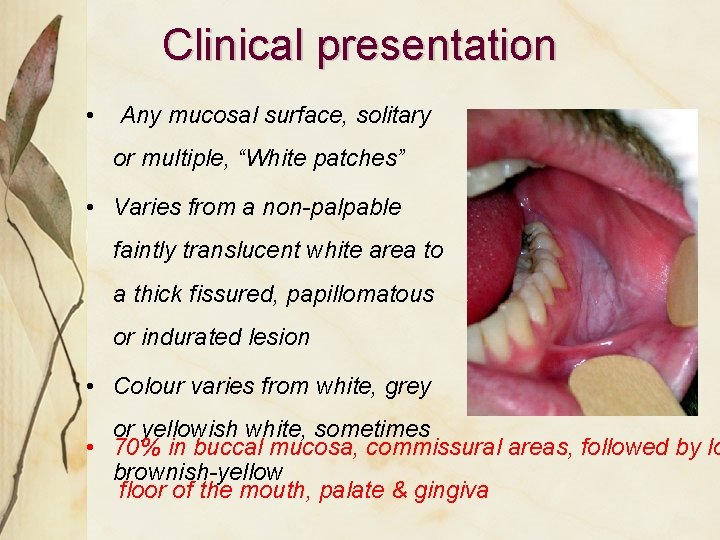
Clinical presentation • Any mucosal surface, solitary or multiple, “White patches” • Varies from a non-palpable faintly translucent white area to a thick fissured, papillomatous or indurated lesion • Colour varies from white, grey or yellowish white, sometimes • 70% in buccal mucosa, commissural areas, followed by lo brownish-yellow floor of the mouth, palate & gingiva
SYMPTOMS • Patients may report with a feeling of increased thickness of mucosa • Those with ulcerated or nodular type may complain of burning sensation • Enlarged cervical lymph nodes may signal occurrence of metastasis

Clinical variants of leukoplakia Homogeneous/ Leukoplakia Simplex Ulcerative Speckled/Nodular
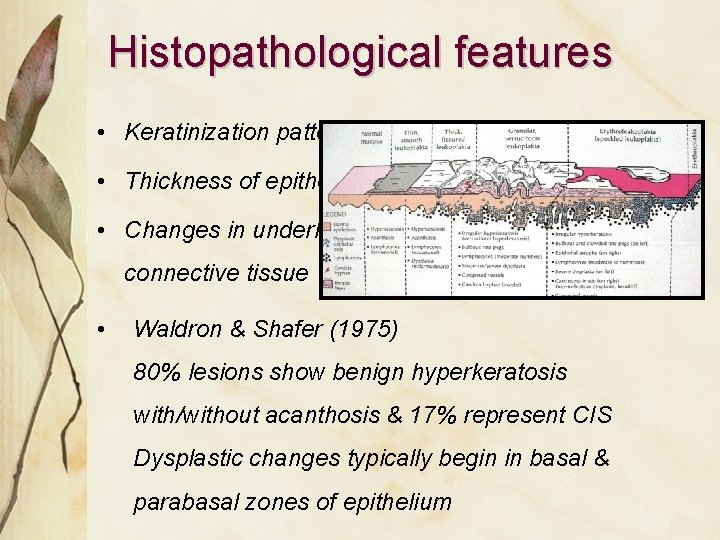
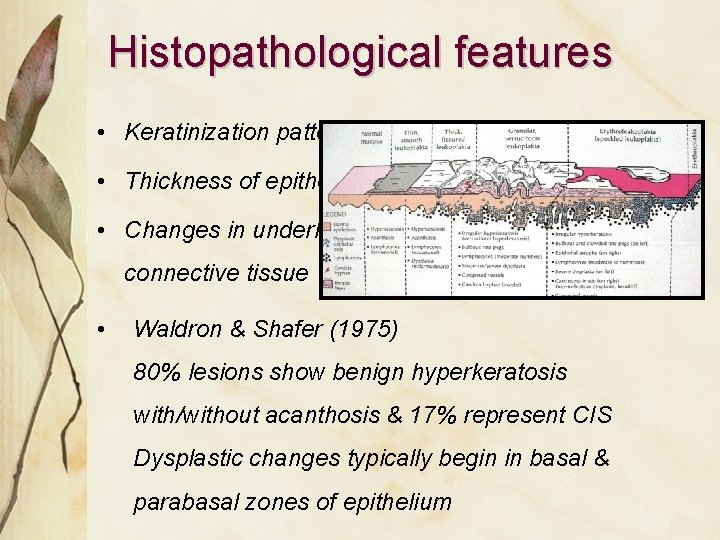
Histopathological features • Keratinization pattern • Thickness of epithelium • Changes in underlying connective tissue • Waldron & Shafer (1975) 80% lesions show benign hyperkeratosis with/without acanthosis & 17% represent CIS Dysplastic changes typically begin in basal & parabasal zones of epithelium

• Five clinical criteria for high risk of malignant change – The nodular type – Erosion or ulceration within lesion – Presence of a nodule indicates malignant potential – A lesion that is hard in its periphery – Lesion of anterior floor of mouth & undersurface of tongue • In all cases, relative risk of malignant potential
Conservative management • Elimination of etiological factor • Restraining from smoking or chewing tobacco • To remove sharp broken down teeth • Correction & replacement of overhanging or faulty metal restorations with a metal bridge
CHEMOPREVENTION 1) Isotrenitoin / 13 - cis- retinoic acid – 2) Beta carotene -30 mg TID 3) Topical Bleomycin – 0. 5 -1% solution/2 wks 4) 5 -Fluorouracil & Cisplatin
• Surgical Excision: entire lesion excised if it is >1 cm in size, following modalities used: a) Scalpel – surgical stripping b) Cryosurgery – with liquid nitrogen c) Electrocautery d) Laser ablation

Erythroplakia WHO DEFINITION: “Any lesion of the oral mucosa that presents as a bright red velvety patch or plaque, which cannot be characterized clinically or pathologically as any other recognizable condition” Reported by Querat in 1911

CLASSIFICATION • Clinical variants 1. Homogenous erythroplakia 2. Erythroplakia interspersed with patches of leukoplakia 3. Granular or Speckled erythroplakia

• Etiology : Same as oral leukoplakia • Age : Mainly middle age, peak 65 -74 years • Gender : Predilection for men • Location/size - Soft palate, floor of the mouth & buccal mucosa & tongue - Typical lesion < 1. 5 cm in diameter but >4 cm also observed
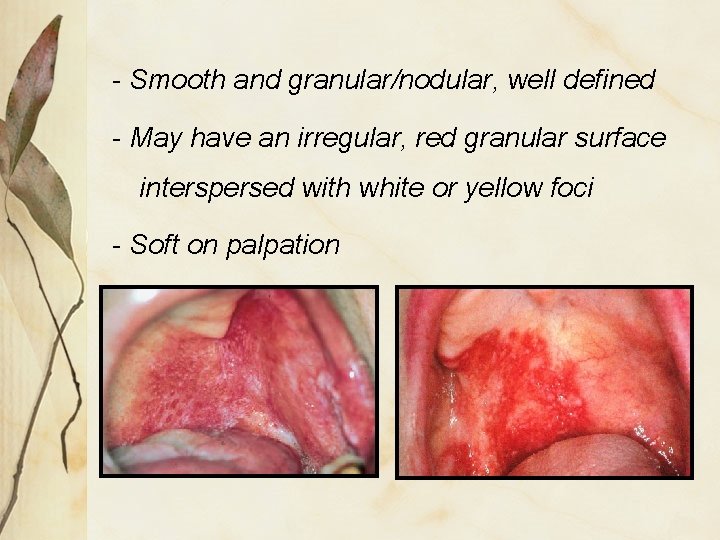
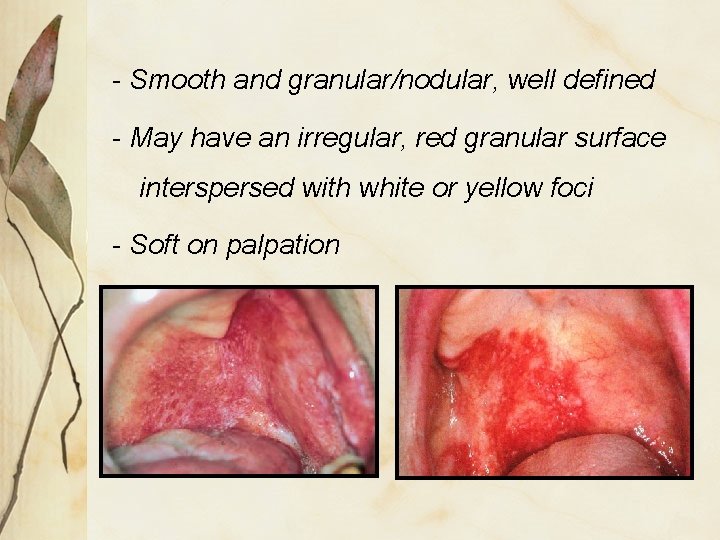
- Smooth and granular/nodular, well defined - May have an irregular, red granular surface interspersed with white or yellow foci - Soft on palpation

• Highest risk for malignant transformation - 14 -50% • Based on the fact that on histology 8090% of cases present as - Carcinoma In Situ - Severe epithelial dysplasia - Microinvasive carcinoma
Management • Biopsy should be performed • Treatment guided by histopathologic diagnosis • Recurrence , multifocality common • Careful long term follow up
Intraepthelial carcinoma (Ca in Situ) • Arises frequently on the skin, but also on mucous membranes, including oral cavity • Most severe stage of epithelial dysplasia • Striking feature – dysplastic epithelial cells do not invade into connective tissue • Common among elderly, with a male prediliction • Present as white plaques or ulcerated, & reddened areas • Site – floor of the mouth, tongue, lips

• Histopathology • Keratin may or may not be present on the surface, but if present it is usually parakeratin • Individual cell keratinization or keratin pearl formation are rare • Consistent finding – loss of orientation & normal polarity of cells • Treatment • No accepted treatment • Surgical excision, irradiation & cauterization
Precancerous conditions

Oral lichen planus • Named by E Wilson ( British physician) 1896 Lichen – latin for primitive plants (symbiotic algae & fungi) Planus – latin for flat • Definition • “A common chronic immunologic inflammatory mucocutaneous disorder that varies in appearance from keratotic (reticular or plaque like) to erythematous and ulcerative, affecting

• Affects 0. 5% to 1% of world's population • Approx half patients with cutaneous LP have oral involvement • Mucosal involvement, sole manifestation in up to 25% cases • Peak incidence - middle age, F: M- 2: 1 • Characteristically associated with persistent clinical course & resistance to most conventional treatments

• On skin- • Flat-topped purple polygonal & pruritic papular rash • Koebner phenomenon – appearance of lesions along a site of injury
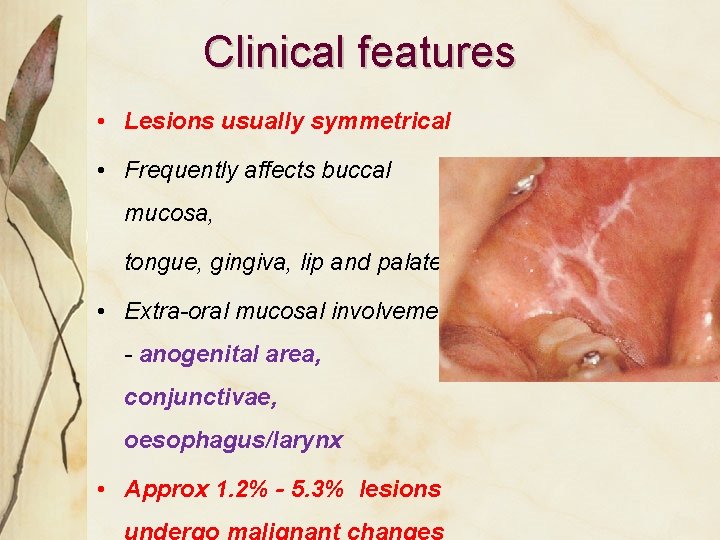
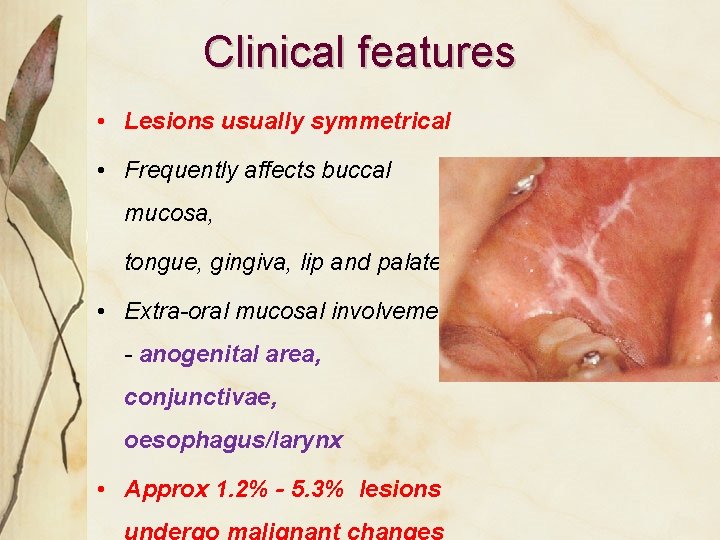
Clinical features • Lesions usually symmetrical • Frequently affects buccal mucosa, tongue, gingiva, lip and palate • Extra-oral mucosal involvements - anogenital area, conjunctivae, oesophagus/larynx • Approx 1. 2% - 5. 3% lesions
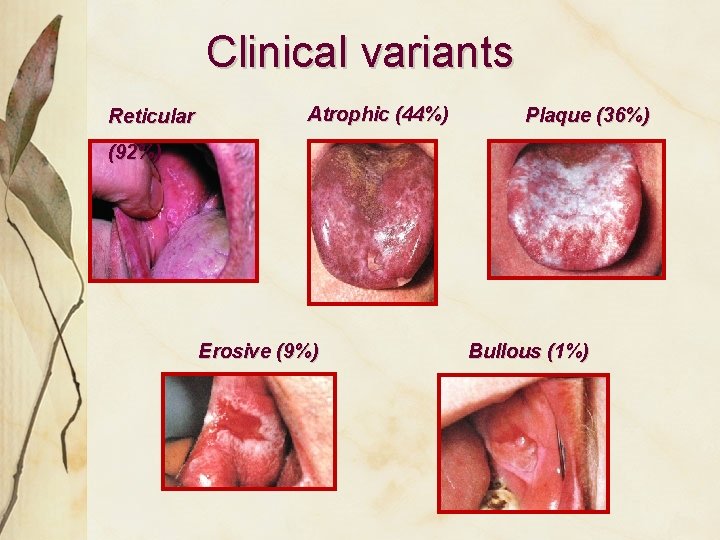
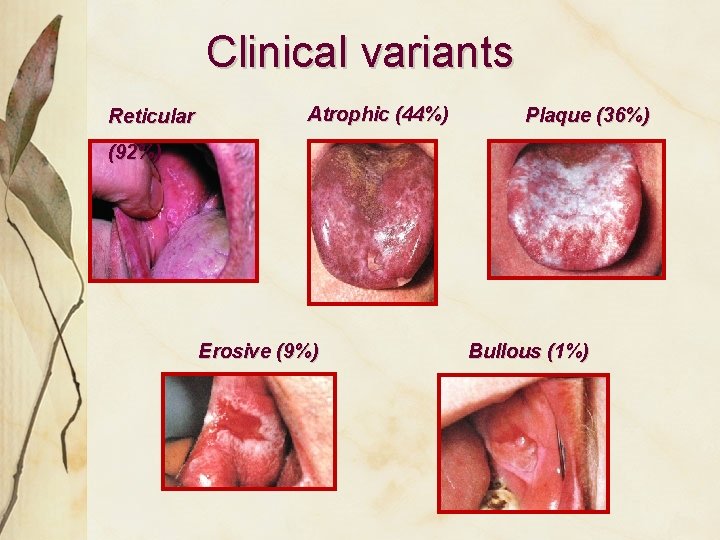
Clinical variants Reticular Atrophic (44%) Plaque (36%) (92%) Erosive (9%) Bullous (1%)

Clinical features Asymptomatic • Reticular – Wickham’s striae + discrete erythematous border • Plaque-like – Resemble leukoplakia, common in smokers Symptomatic • Atrophic – Diffuse red patch, peripheral radiating white striae • Erosive – Irregular erosion covered with a
Diagnosis • The characteristic clinical aspects of OLP - sufficient for correct diagnosis • An oral biopsy - to confirm clinical diagnosis (exclude dysplasia & malignancy) • Gingival LP more difficult to diagnose, direct immunofluorescence of perilesional
Management • Reticular type is asymptomatic & treatment often unnecessary • Erosive type presents significant management problems • All patients should optimize oral hygiene • Oral candidiasis should be excluded/treated • Cortico steroids, is the treatment of choice eg – Fluocinonide or Clobetasol gel for 2 weeks, with 3 mnths follow-up
• In symptomatic patients with apparent contact dental factor, patch test with replacement of amalgam • In those with no apparent contact factor, topical or intralesional steroid - first line treatment. A short course of systemic steroid for more rapid control
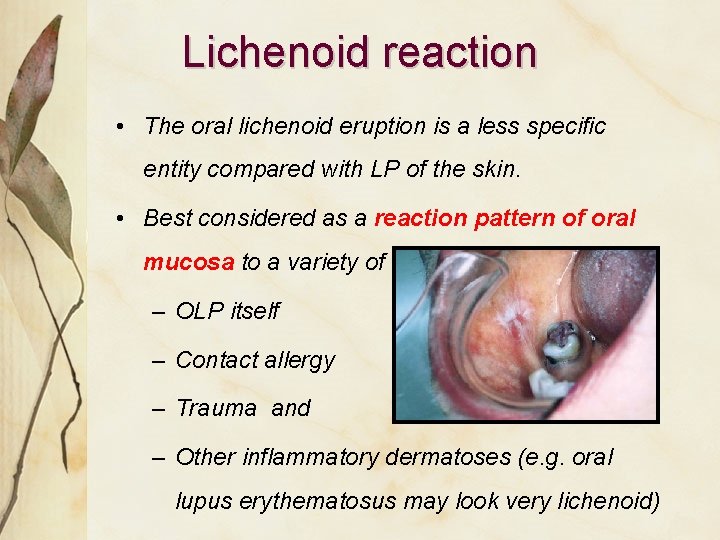
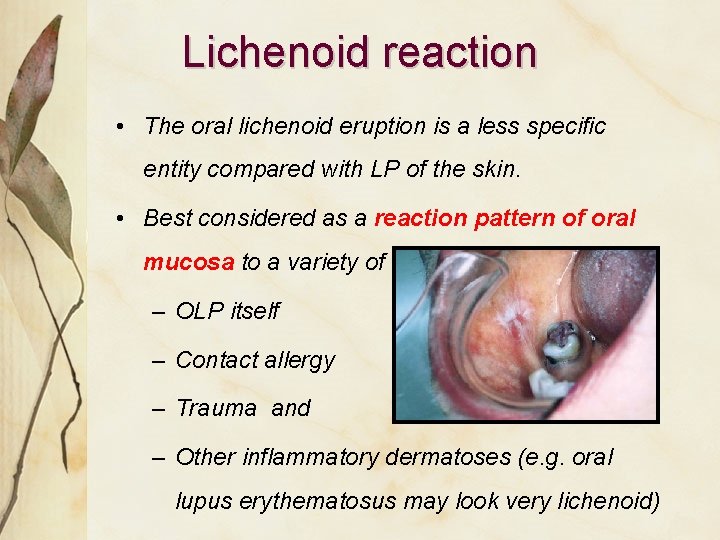
Lichenoid reaction • The oral lichenoid eruption is a less specific entity compared with LP of the skin. • Best considered as a reaction pattern of oral mucosa to a variety of insults, including – OLP itself – Contact allergy – Trauma and – Other inflammatory dermatoses (e. g. oral lupus erythematosus may look very lichenoid)
Oral submucous fibrosis DEFINITION “It is a slowly progressing chronic fibrotic disease of the oral cavity & oropharynx, characterized by fibroelastic change and inflammation leading to a progressive inability to open the mouth, swallow or speak”
Clinical features Age • Range wide & regional; even prevalent among teenagers in India Ranges from 11 -60 years Sex • From 0. 2 - 2. 3% in males to 1. 2 - 4. 5% in females in Indian communities Race • South-East Asian countries, in Indian immigrants to other countries

Mortality/morbidity • High rate of morbidity - progressive inability to open mouth, resulting in difficulty eating & consequent nutritional deficiencies • Significant mortality rate - can transform into oral cancer, particularly Squamous cell
Etiology • Initially classified as idiopathic, now • Betel quid & it’s components (Arecoline, an active alkaloid found in betel nuts, stimulates fibroblasts to increase production of collagen by 150%) • Capsaicin – Chillies (hypersensitivity reaction) • Nutritional factors
Clinical presentation • Common site – buccal mucosa, retromolar area, uvula, palate, etc • Initially, pain and a burning sensation upon consumption of hot & spicy foods • Vesicle & ulcers • Excessive or reduced salivation & defective gustation • Hearing loss

• Depapillation & atrophy of tongue and uvula • Depigmented & loss of stippling over gingiva • Nasal tone in the voice • Difficulty in deglutition • Impaired mouth movements (eg, eating, whistling, blowing, sucking)
Clinical stages Three stages (Pindborg, 1989) based on physical findings: • Stage 1: Stomatitis includes erythematous mucosa, vesicles, mucosal ulcers, melanotic mucosal pigmentation & mucosal petechiae • Stage 2: Fibrosis occurs in ruptured vesicles & ulcers when they heal, hallmark of this stage

• Stage 3: Sequelae of OSF – Leukoplakia is found in more than 25% of individuals with OSF – Speech and hearing deficits may occur because of involvement of the tongue and the eustachian tubes

Histopathology • Hyperkeratinized, atrophic epithelium with flattening & shortening of rete pegs • Nuclear pleomorphism & severe intercellular edema • Finely fibrilar collagen & increased fibroblastic activity in early stage showing dilated & congested blood vessels with areas of hemorrhage

• Advanced stage shows “homogenization” and “hyalinization” of collagen fibers (important feature) • Degeneration of muscle fibers and chronic inflammatory cell infiltration in the connective tissue
Management 1. Behavioral therapy - Patient counseling, stoppage of habit 2. Medicinal therapy -Hyaluronidase: Topically, shown to improve symptoms more quickly than steroids alone - Mild cases – intralesional inj Dexamethasone 4 mg to reduce symptoms & surgical splitting / excision of fibrous bands - Recent study – intralesional inj of gamma interferon 3 times a week, improves mouth
Thank You
 Sheetal rai
Sheetal rai Classification of white lesions of oral cavity
Classification of white lesions of oral cavity Cluster computing definition
Cluster computing definition Dr sheetal kale
Dr sheetal kale Hpv oral cancer
Hpv oral cancer Daughter mother grandmother pancreatic lesions
Daughter mother grandmother pancreatic lesions Pyramidal and extrapyramidal tracts
Pyramidal and extrapyramidal tracts White lesions
White lesions Name the five lesions associated with hiv/aids chapter 17
Name the five lesions associated with hiv/aids chapter 17 Epidermoid carcinoma
Epidermoid carcinoma Periradicular tissue
Periradicular tissue Gj mount classification
Gj mount classification Lésions
Lésions Pie on the floor visual field defect
Pie on the floor visual field defect Pr��ca it projektov�� mana����r
Pr��ca it projektov�� mana����r Pustule
Pustule Monocular visual field
Monocular visual field Nature lésions
Nature lésions Vesiculobullous lesions
Vesiculobullous lesions Extrapyramidal vs pyramidal
Extrapyramidal vs pyramidal Scattered white matter lesions
Scattered white matter lesions Olneys lesions
Olneys lesions Convergence insufficiency athens
Convergence insufficiency athens Vagus nerve lesion
Vagus nerve lesion Don't touch lesion
Don't touch lesion Describing skin lesions
Describing skin lesions Clinical features of burns
Clinical features of burns Smart business process
Smart business process Vertailukehittäminen
Vertailukehittäminen Rai inter
Rai inter Copiii sunt mainile cu care ne prindem de rai
Copiii sunt mainile cu care ne prindem de rai Naomi rai
Naomi rai J v k rao committee
J v k rao committee Rai cereal
Rai cereal Lady rai mummy
Lady rai mummy Richa rai
Richa rai Rai
Rai Aishwarya weight loss
Aishwarya weight loss Rai diagnostic
Rai diagnostic Haagen dazs slogan
Haagen dazs slogan Arushi rai
Arushi rai Rai oyau
Rai oyau Peran letnan kolonel i gusti ngurah rai
Peran letnan kolonel i gusti ngurah rai Kamalzar
Kamalzar Rai narita
Rai narita Arka rai choudhuri
Arka rai choudhuri El rai de la medusa comentario
El rai de la medusa comentario Rai kamaluddin
Rai kamaluddin Naomi rai
Naomi rai Rapporto aeroilluminante calcolo
Rapporto aeroilluminante calcolo