Precancer diseases of the female sexual organs Female














- Slides: 59
Precancer diseases of the female sexual organs. Female cancer. O. Stelmakh
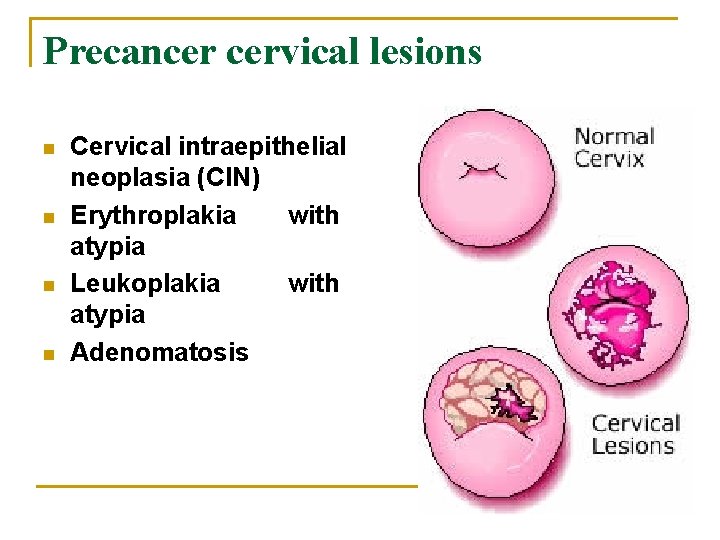
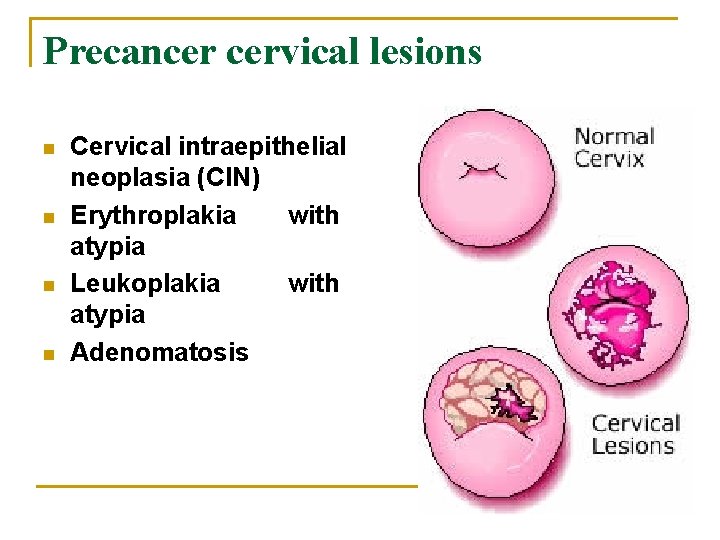
Precancer cervical lesions n n Cervical intraepithelial neoplasia (CIN) Erythroplakia with atypia Leukoplakia with atypia Adenomatosis
Risk factors for cervical dysplasia n Human papillomavirus is a common virus that most women will be infected with at some time in their life. smoking n multiple sexual partners n pregnancy before the age of 20 n suffering from conditions that affect the immune system, like HIV n

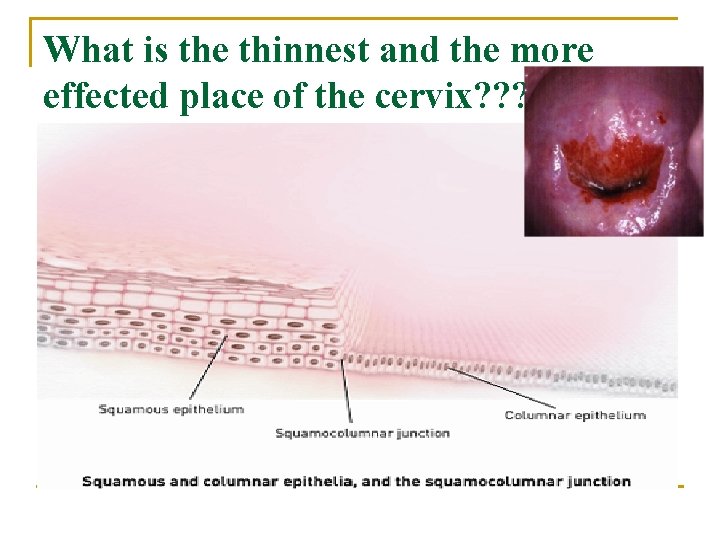
Layers of squamosus epithelium of cervix
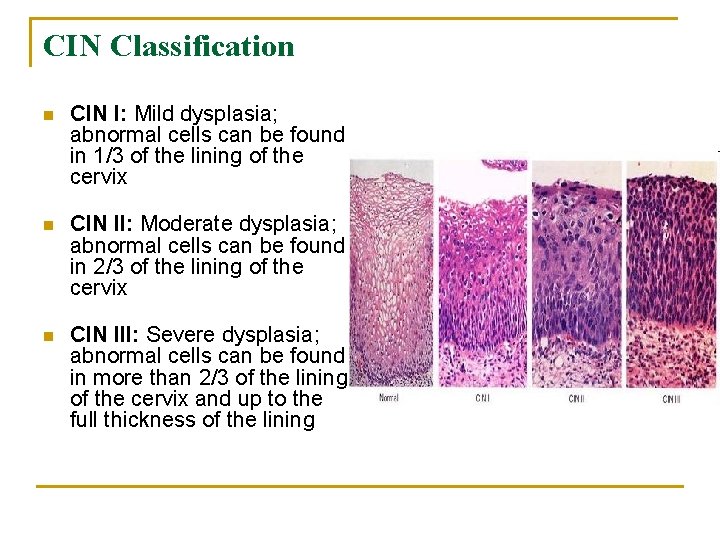
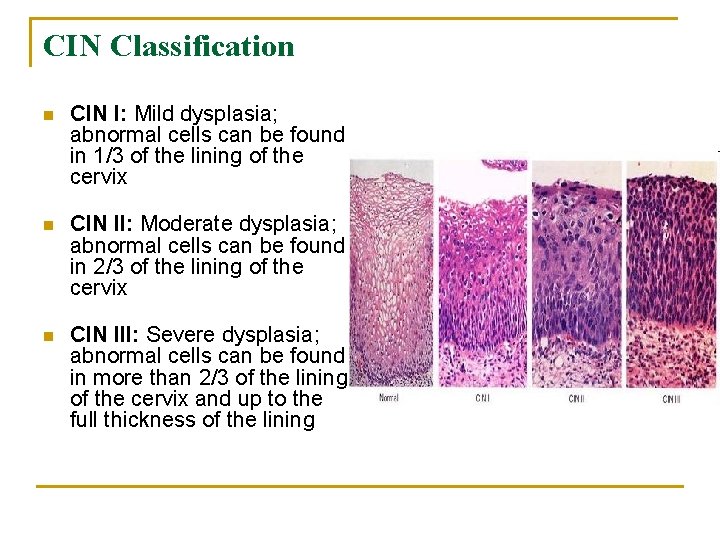
CIN Classification n CIN I: Mild dysplasia; abnormal cells can be found in 1/3 of the lining of the cervix n CIN II: Moderate dysplasia; abnormal cells can be found in 2/3 of the lining of the cervix n CIN III: Severe dysplasia; abnormal cells can be found in more than 2/3 of the lining of the cervix and up to the full thickness of the lining

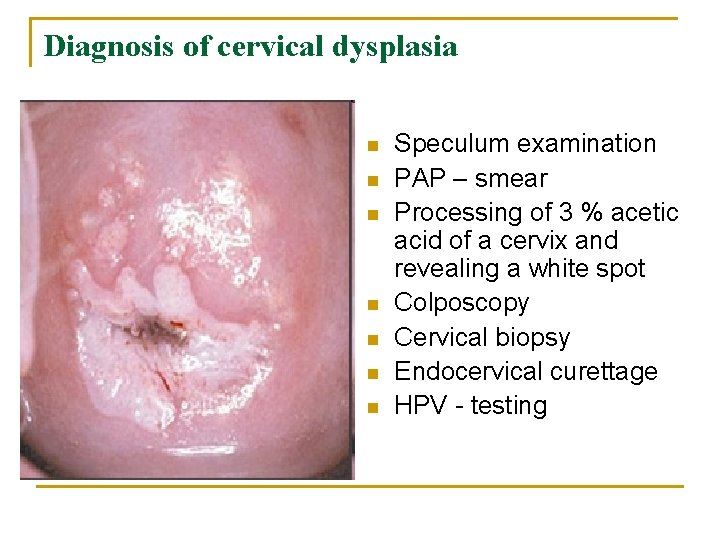
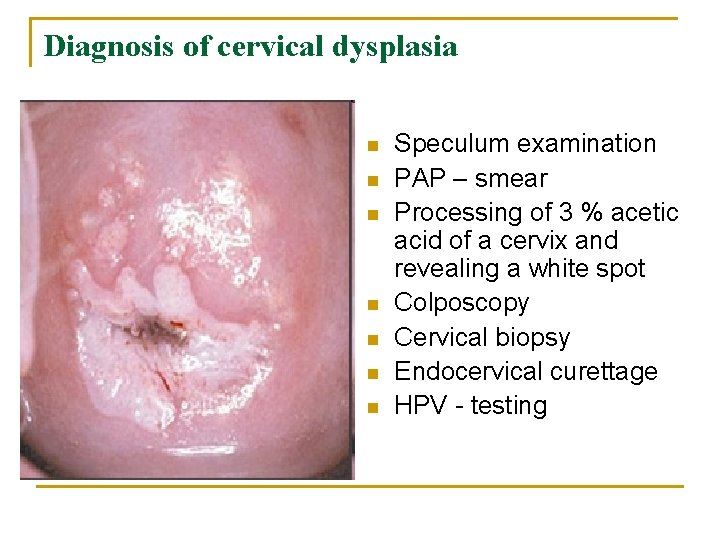
Diagnosis of cervical dysplasia n n n n Speculum examination PAP – smear Processing of 3 % acetic acid of a cervix and revealing a white spot Colposcopy Cervical biopsy Endocervical curettage HPV - testing
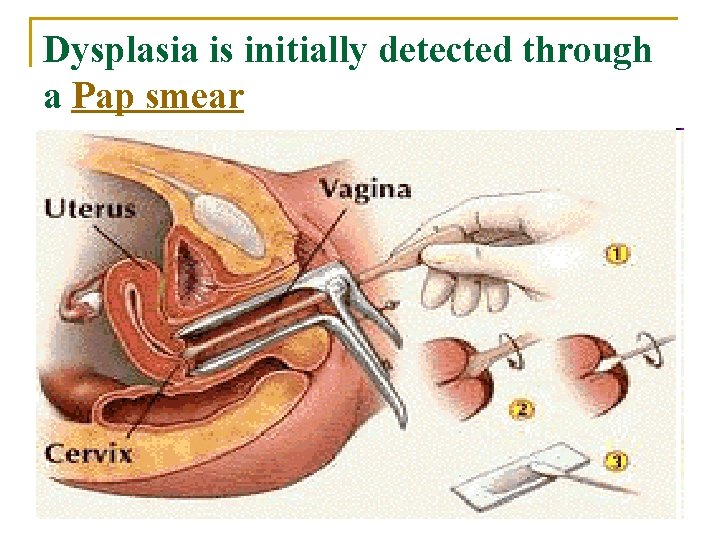
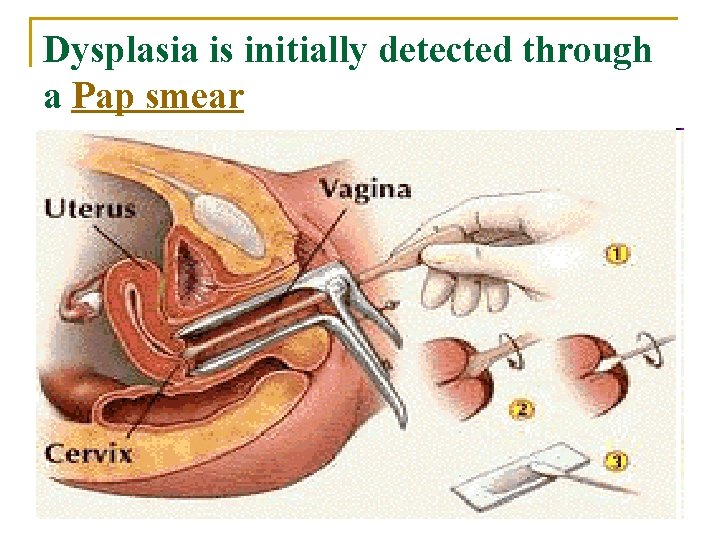
Dysplasia is initially detected through a Pap smear
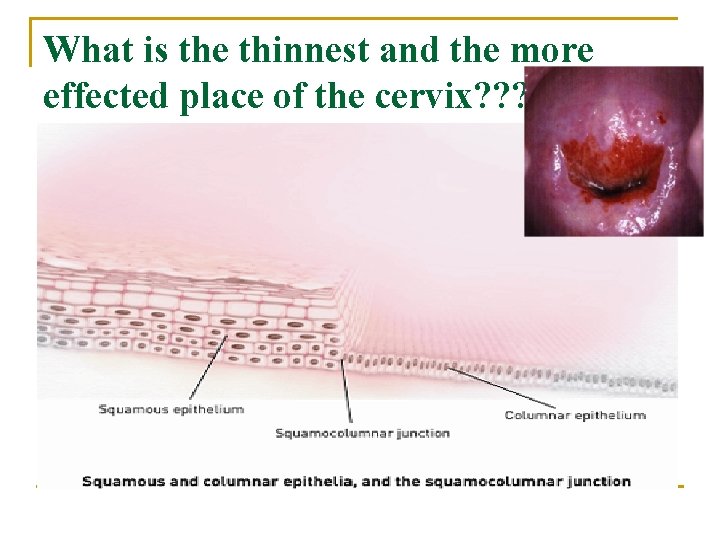
What is the thinnest and the more effected place of the cervix? ? ?
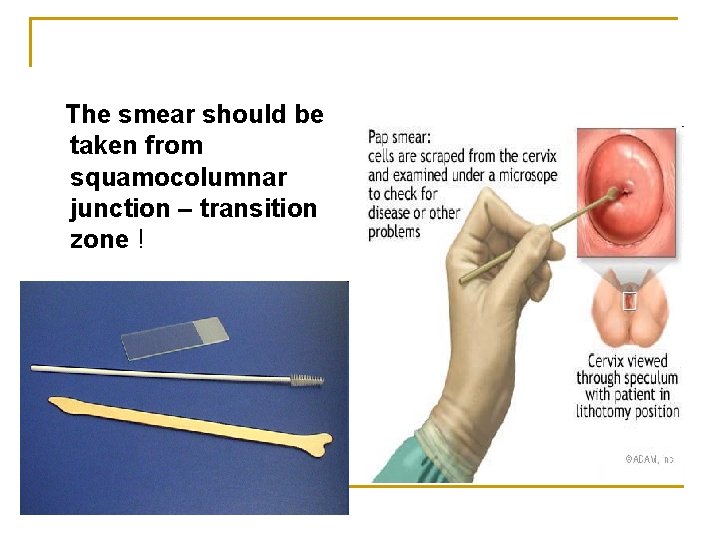
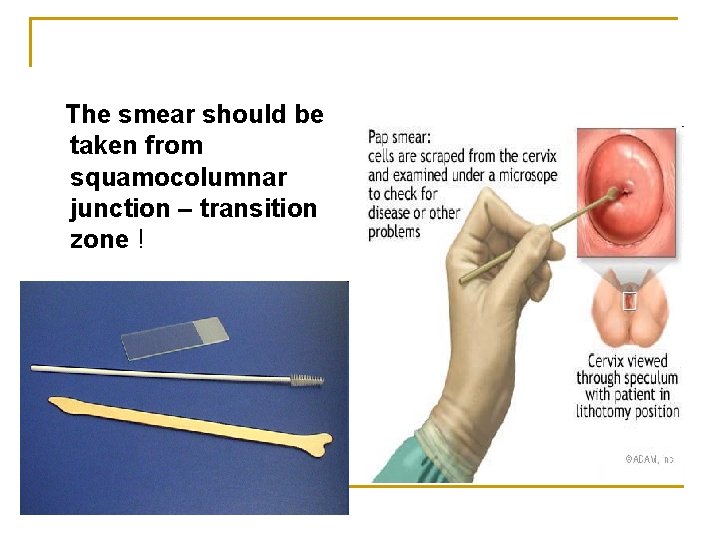
The smear should be taken from squamocolumnar junction – transition zone !

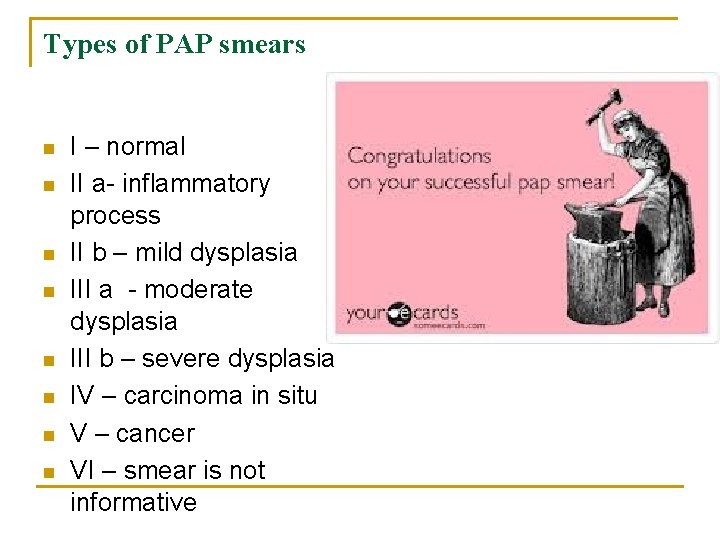
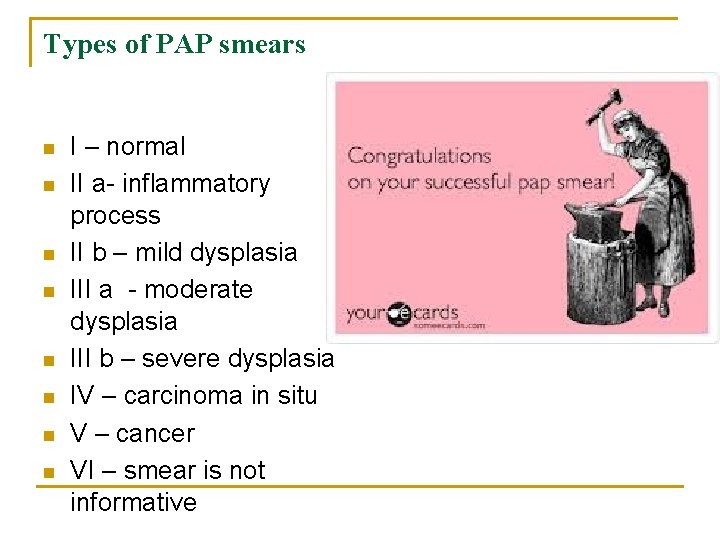
Types of PAP smears n n n n I – normal II a- inflammatory process II b – mild dysplasia III a - moderate dysplasia III b – severe dysplasia IV – carcinoma in situ V – cancer VI – smear is not informative

Frequency of Pap Smears n n n Begin no later than age 21. If patient is sexually active <21. Once initiated, screening should be performed annually After 30, for women who have had 3 consecutive, normal Pap smears, screening frequency may be reduced to every 3 years. Screening may stop after total hysterectomy, >70 if the patient is at low risk, and has had three consecutive normal Pap smears within the last 10 years.
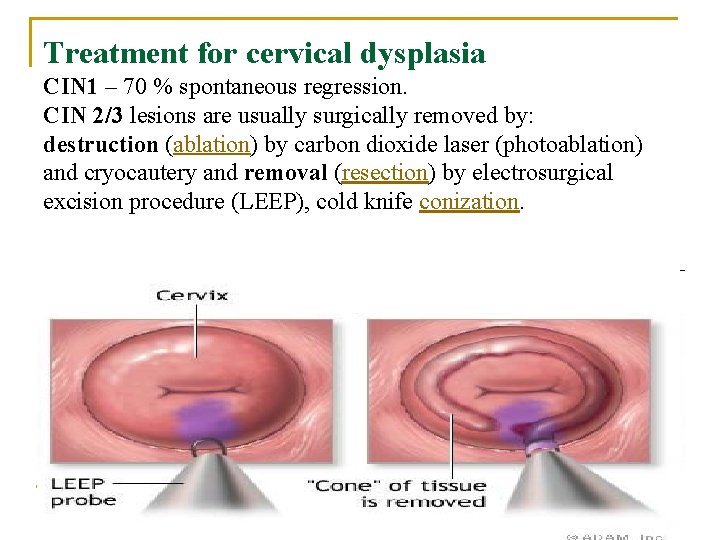
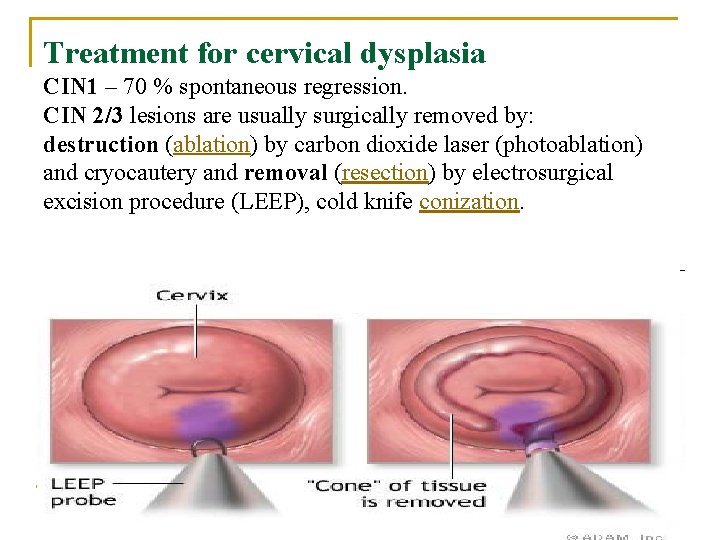
Treatment for cervical dysplasia CIN 1 – 70 % spontaneous regression. CIN 2/3 lesions are usually surgically removed by: destruction (ablation) by carbon dioxide laser (photoablation) and cryocautery and removal (resection) by electrosurgical excision procedure (LEEP), cold knife conization.
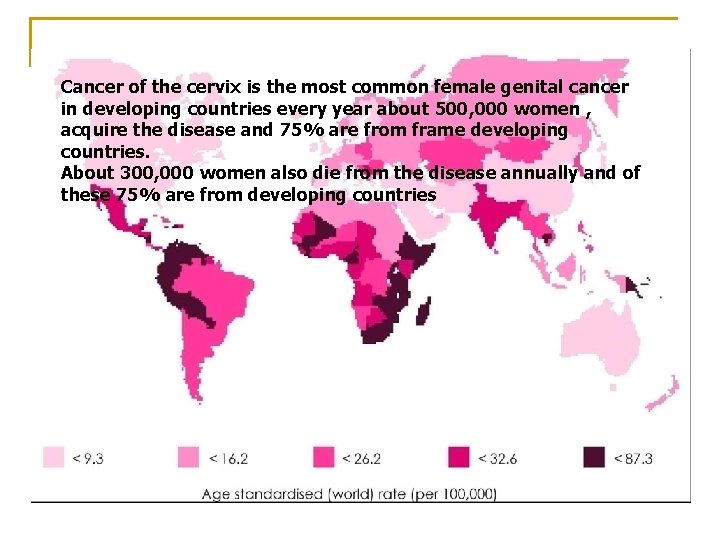
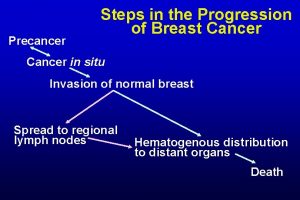
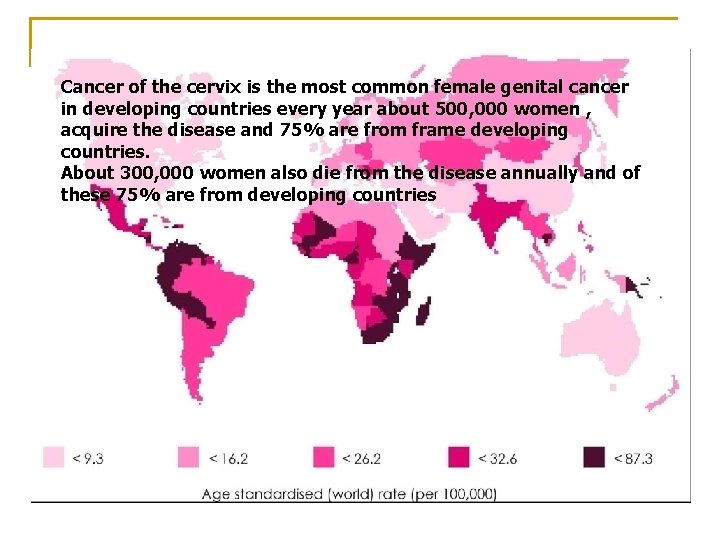
Cancer of the cervix is the most common female genital cancer in developing countries every year about 500, 000 women , acquire the disease and 75% are from frame developing countries. About 300, 000 women also die from the disease annually and of these 75% are from developing countries
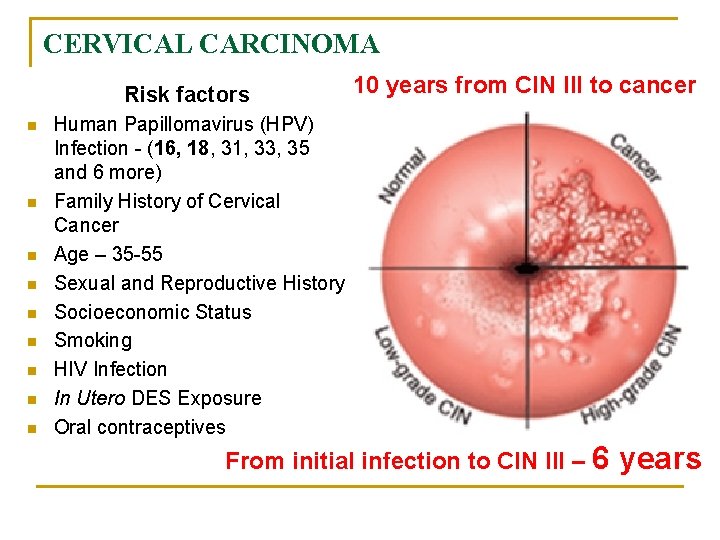
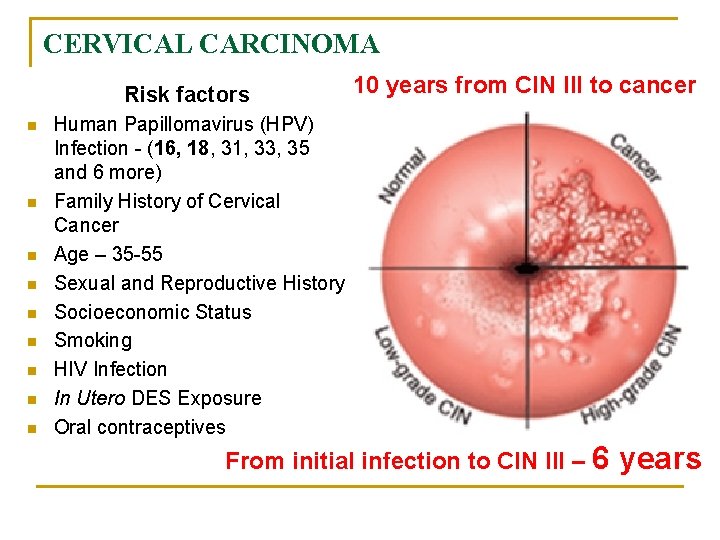
CERVICAL CARCINOMA Risk factors n n n n n 10 years from CIN III to cancer Human Papillomavirus (HPV) Infection - (16, 18, 31, 33, 35 and 6 more) Family History of Cervical Cancer Age – 35 -55 Sexual and Reproductive History Socioeconomic Status Smoking HIV Infection In Utero DES Exposure Oral contraceptives From initial infection to CIN III – 6 years
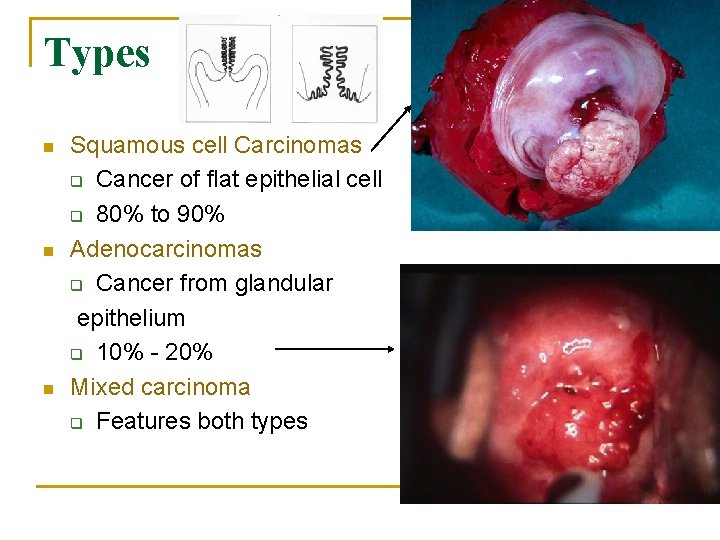
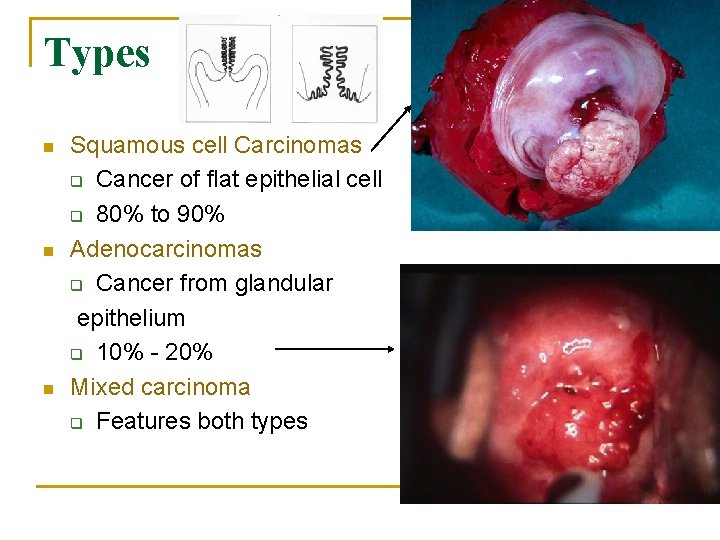
Types n n n Squamous cell Carcinomas q Cancer of flat epithelial cell q 80% to 90% Adenocarcinomas q Cancer from glandular epithelium q 10% - 20% Mixed carcinoma q Features both types
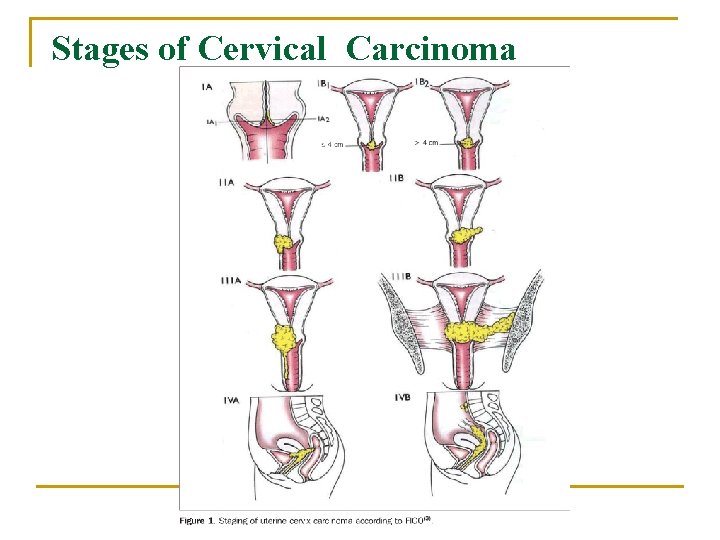
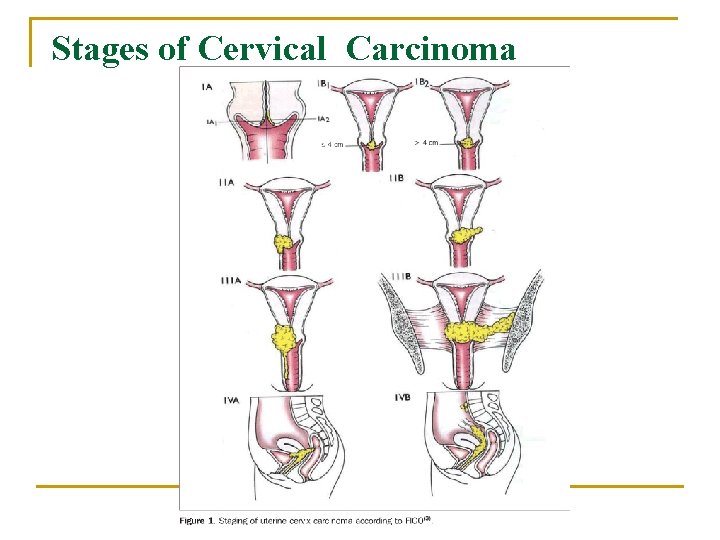
Stages of Cervical Carcinoma
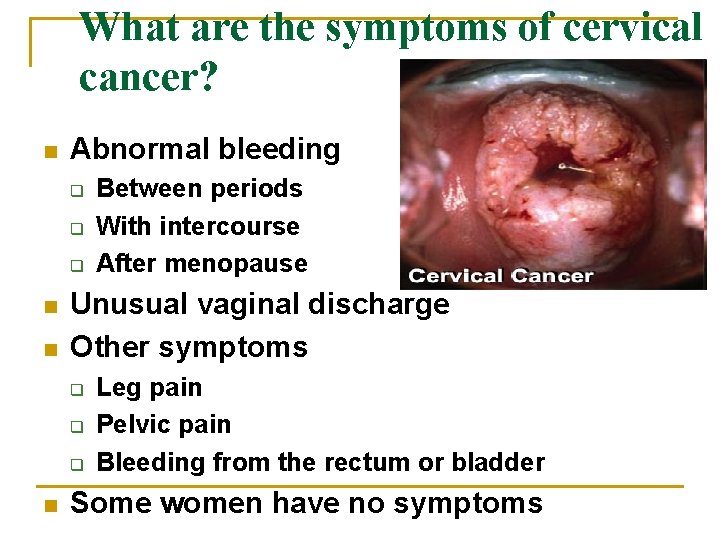
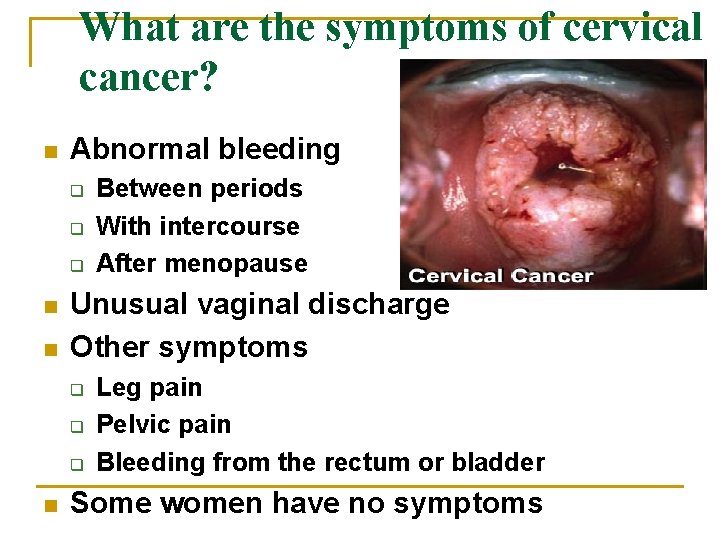
What are the symptoms of cervical cancer? n Abnormal bleeding q q q n n Unusual vaginal discharge Other symptoms q q q n Between periods With intercourse After menopause Leg pain Pelvic pain Bleeding from the rectum or bladder Some women have no symptoms
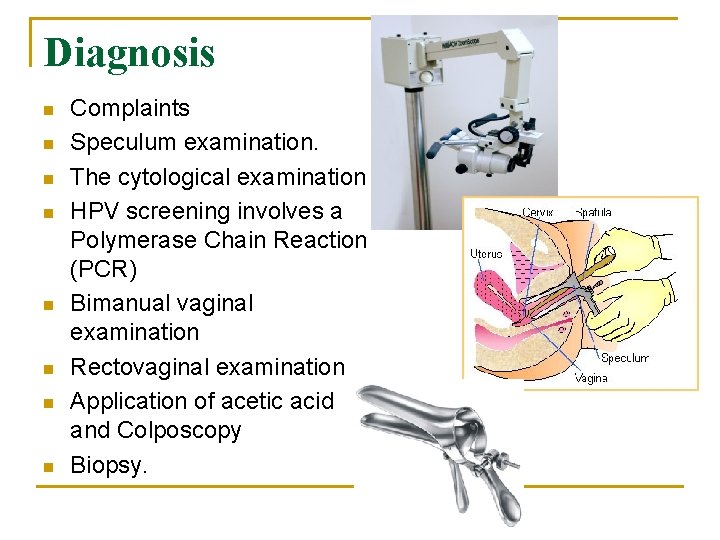
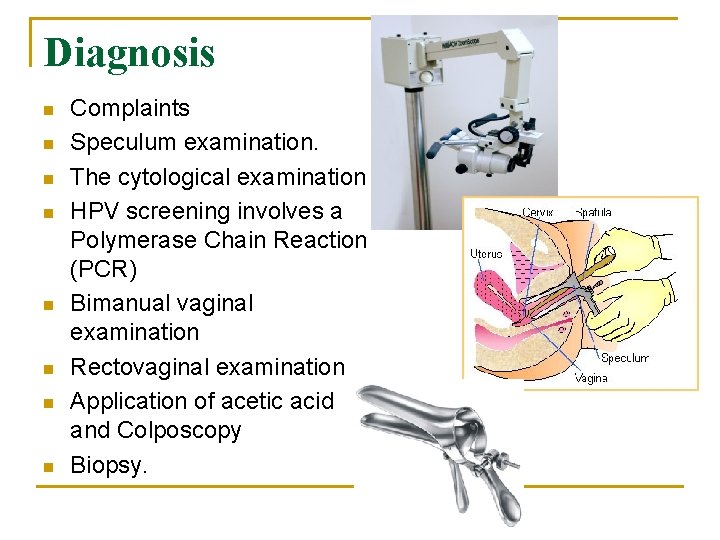
Diagnosis n n n n Complaints Speculum examination. The cytological examination HPV screening involves a Polymerase Chain Reaction (PCR) Bimanual vaginal examination Rectovaginal examination Application of acetic acid and Colposcopy Biopsy.
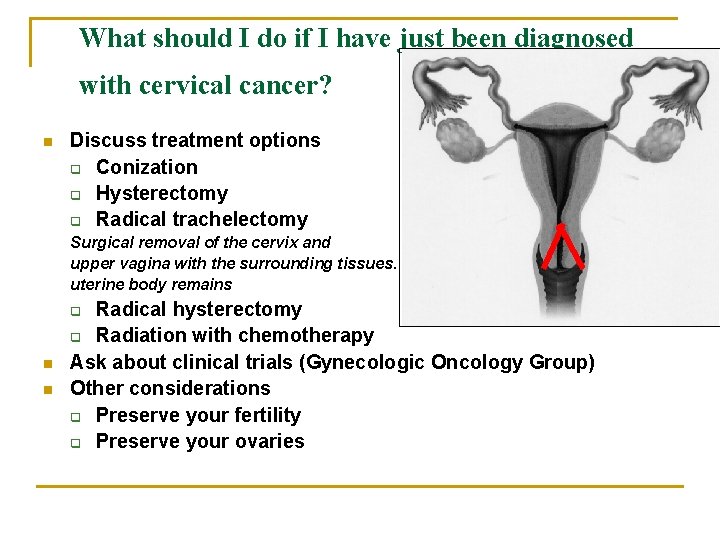
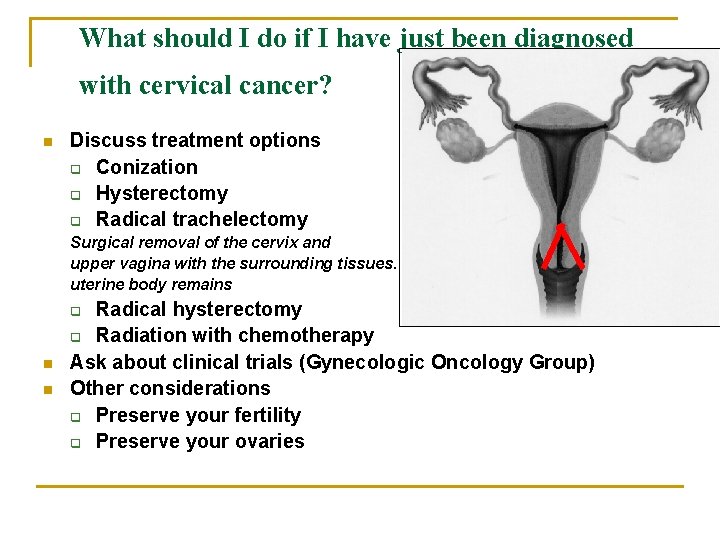
What should I do if I have just been diagnosed with cervical cancer? n Discuss treatment options q Conization q Hysterectomy q Radical trachelectomy Surgical removal of the cervix and upper vagina with the surrounding tissues. uterine body remains Radical hysterectomy q Radiation with chemotherapy Ask about clinical trials (Gynecologic Oncology Group) Other considerations q Preserve your fertility q Preserve your ovaries q n n

Cervical cancer: What is the chance of survival after treatment? FIGO Stage 5 -Year Survival Stage I 81 -96% Stage II 65 -87% Stage III 35 -50% Stage IVA 15 -20%

Vaccines
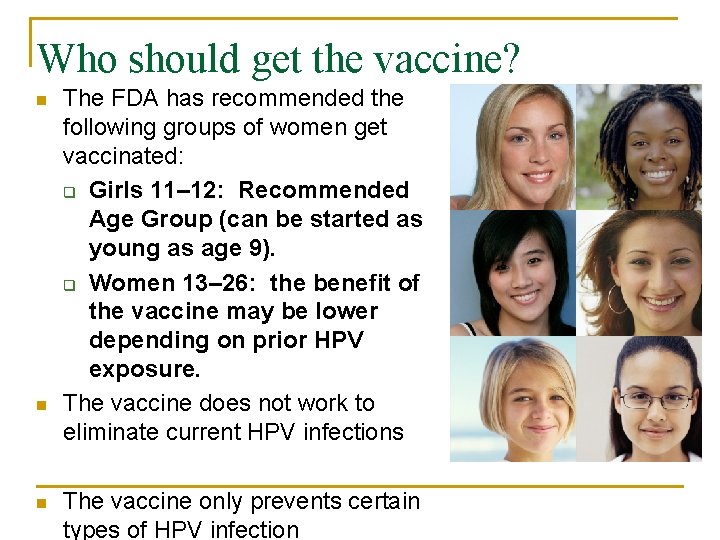
Who should get the vaccine? n n n The FDA has recommended the following groups of women get vaccinated: q Girls 11– 12: Recommended Age Group (can be started as young as age 9). q Women 13– 26: the benefit of the vaccine may be lower depending on prior HPV exposure. The vaccine does not work to eliminate current HPV infections The vaccine only prevents certain types of HPV infection

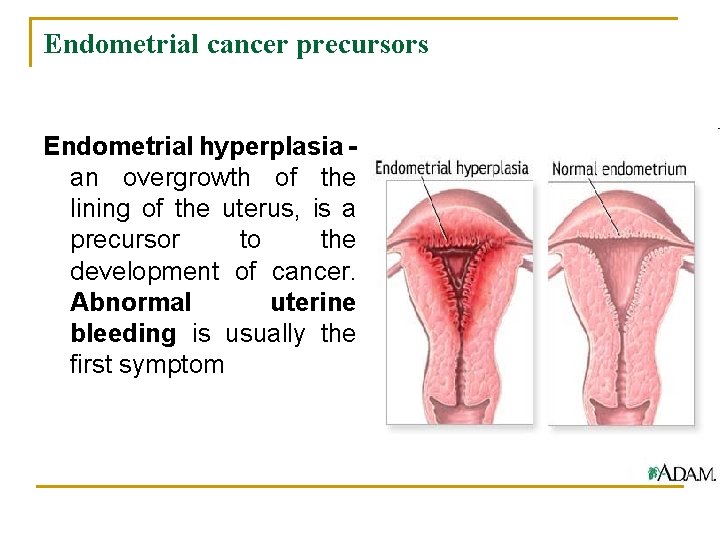
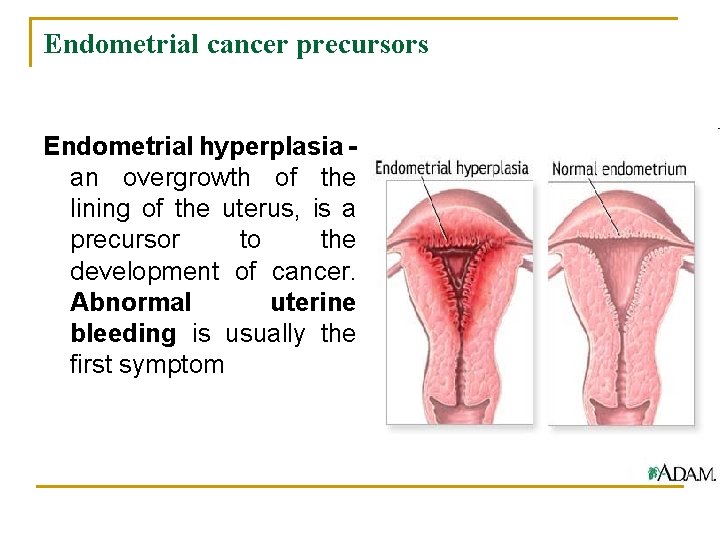
Endometrial cancer precursors Endometrial hyperplasia an overgrowth of the lining of the uterus, is a precursor to the development of cancer. Abnormal uterine bleeding is usually the first symptom
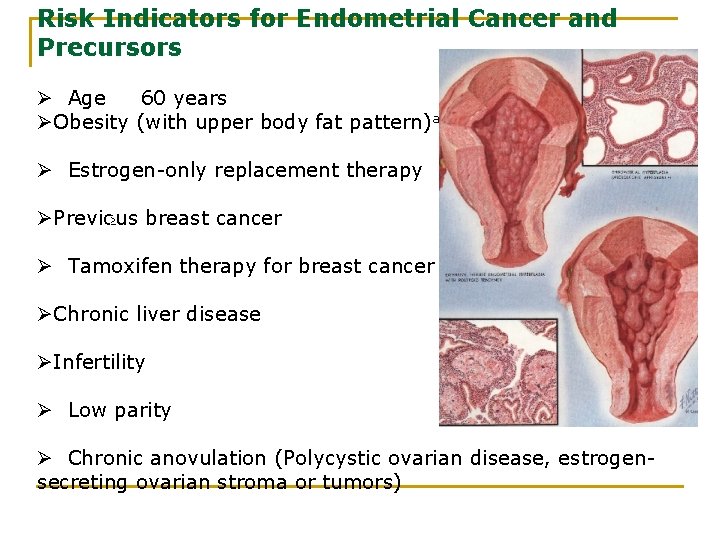
Risk Indicators for Endometrial Cancer and Precursors Ø Age 60 years ØObesity (with upper body fat pattern)a Ø Estrogen-only replacement therapy ØPrevious breast cancer Ø Tamoxifen therapy for breast cancer ØChronic liver disease ØInfertility Ø Low parity Ø Chronic anovulation (Polycystic ovarian disease, estrogensecreting ovarian stroma or tumors)
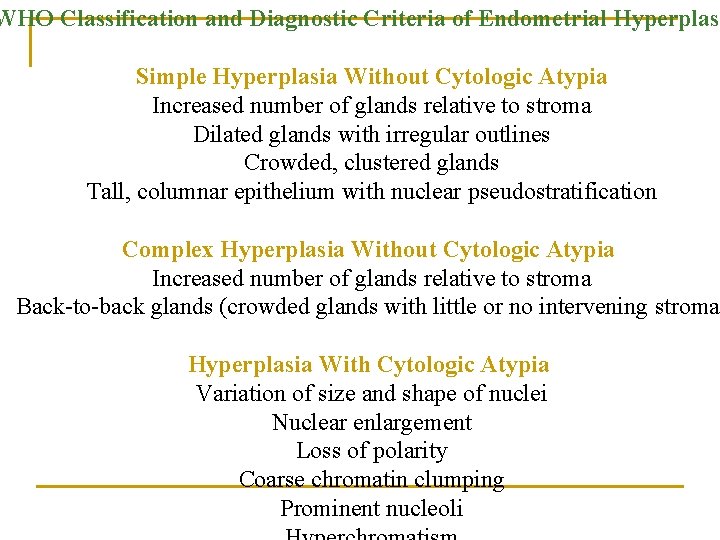
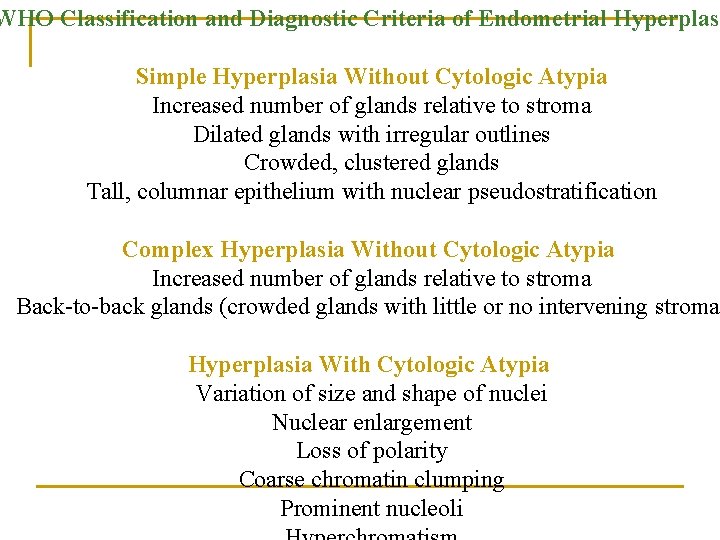
WHO Classification and Diagnostic Criteria of Endometrial Hyperplasi Simple Hyperplasia Without Cytologic Atypia Increased number of glands relative to stroma Dilated glands with irregular outlines Crowded, clustered glands Tall, columnar epithelium with nuclear pseudostratification Complex Hyperplasia Without Cytologic Atypia Increased number of glands relative to stroma Back-to-back glands (crowded glands with little or no intervening stroma Hyperplasia With Cytologic Atypia Variation of size and shape of nuclei Nuclear enlargement Loss of polarity Coarse chromatin clumping Prominent nucleoli
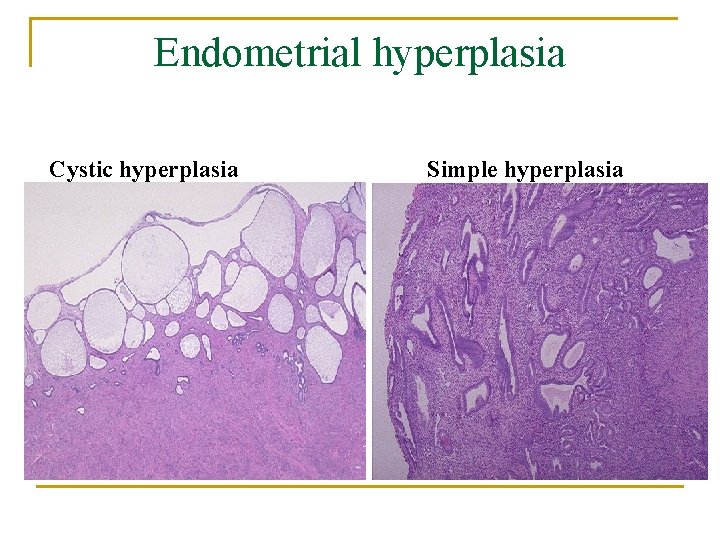
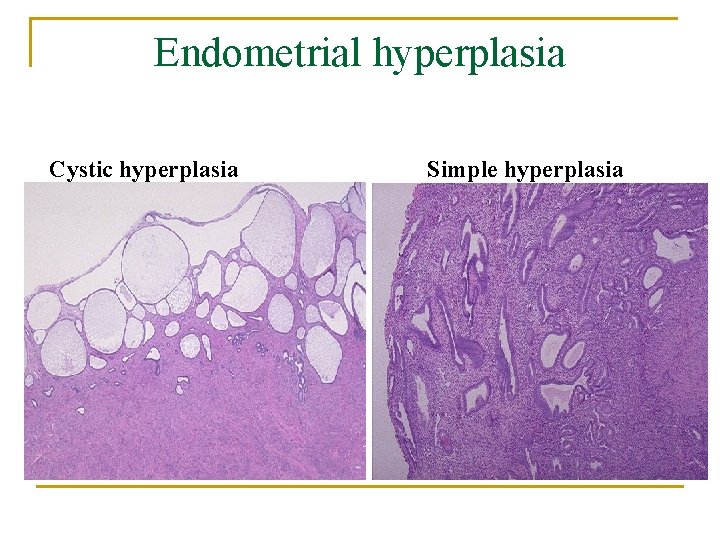
Endometrial hyperplasia Cystic hyperplasia Simple hyperplasia
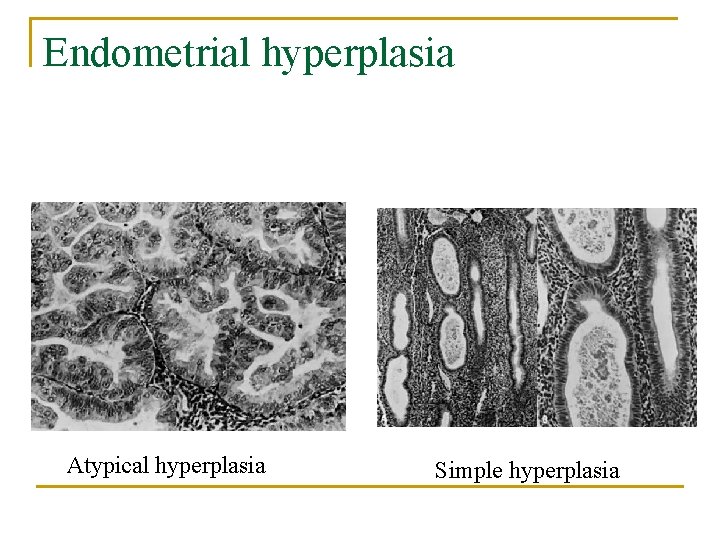
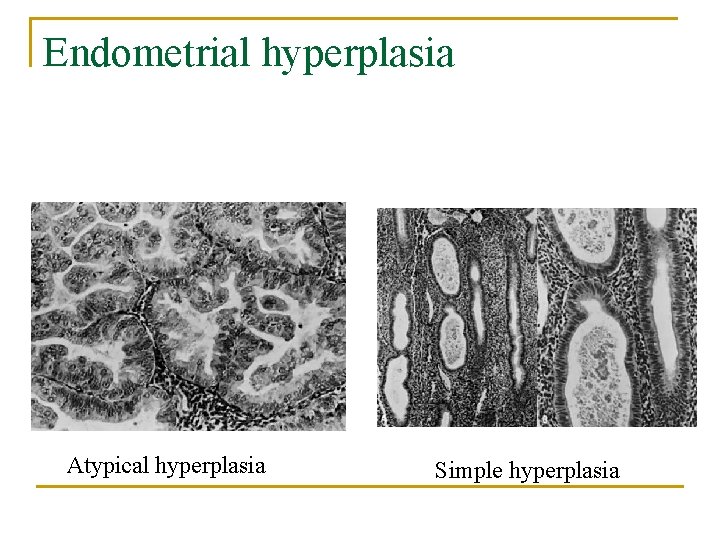
Endometrial hyperplasia Atypical hyperplasia Simple hyperplasia

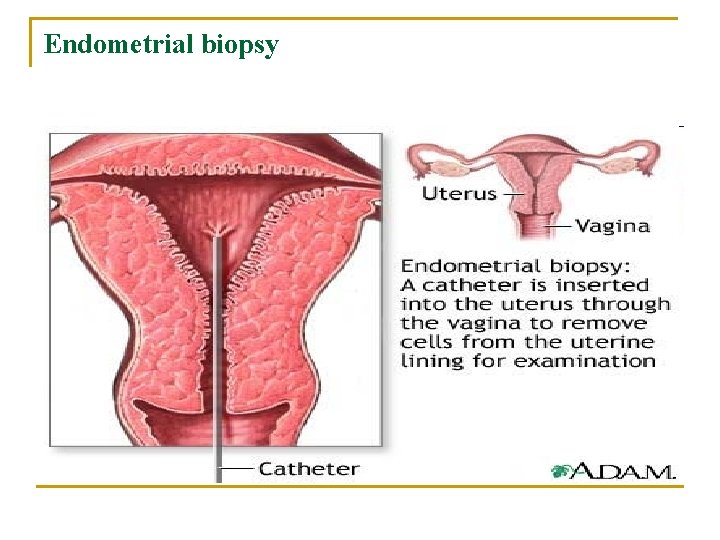
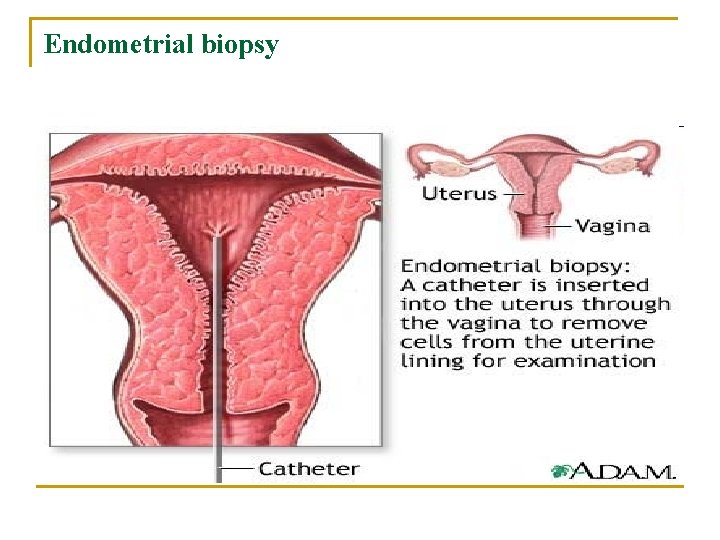
Endometrial biopsy
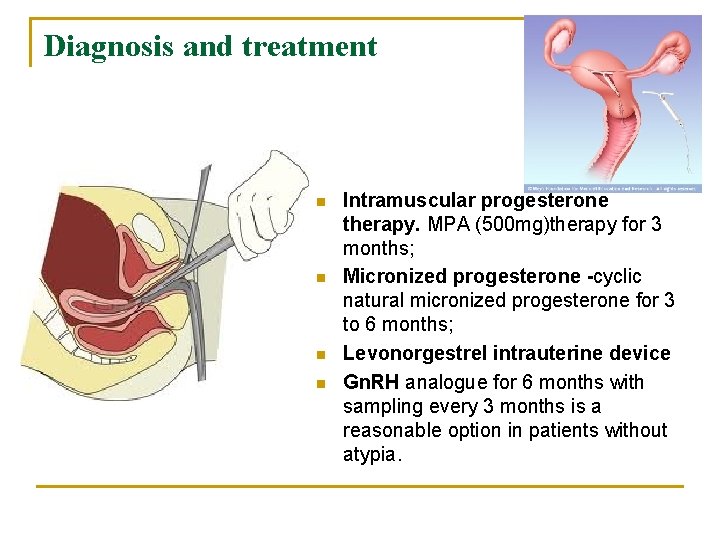
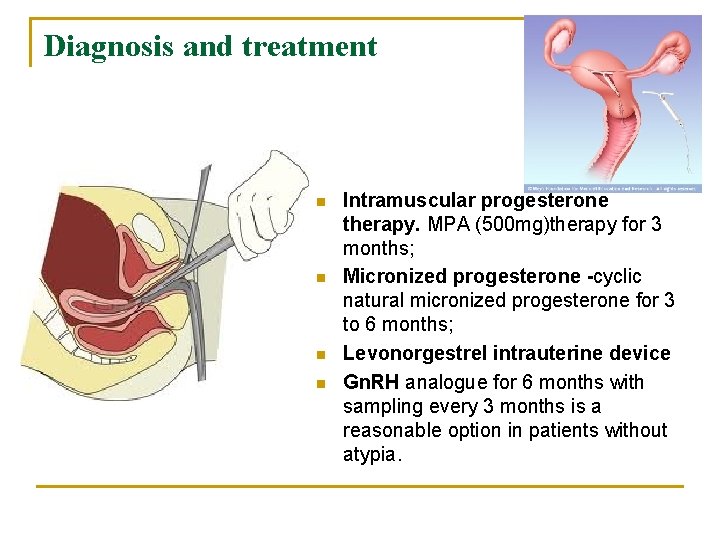
Diagnosis and treatment n n Intramuscular progesterone therapy. MPA (500 mg)therapy for 3 months; Micronized progesterone -cyclic natural micronized progesterone for 3 to 6 months; Levonorgestrel intrauterine device Gn. RH analogue for 6 months with sampling every 3 months is a reasonable option in patients without atypia.

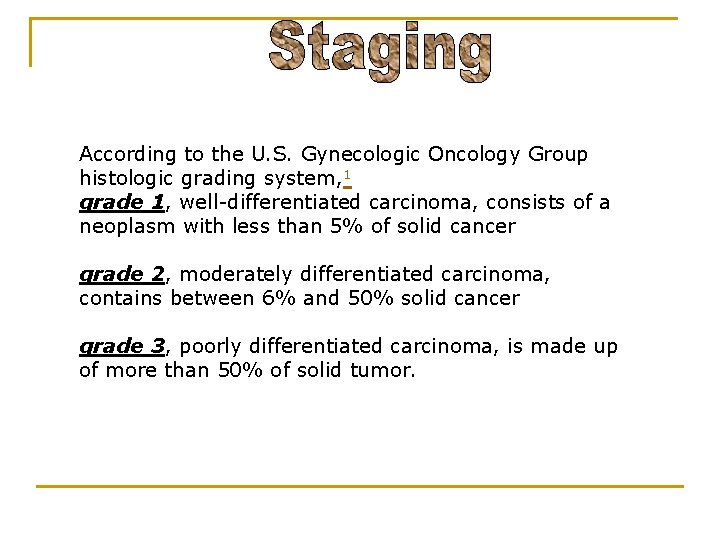
According to the U. S. Gynecologic Oncology Group histologic grading system, 1 grade 1, well-differentiated carcinoma, consists of a neoplasm with less than 5% of solid cancer grade 2, moderately differentiated carcinoma, contains between 6% and 50% solid cancer grade 3, poorly differentiated carcinoma, is made up of more than 50% of solid tumor.
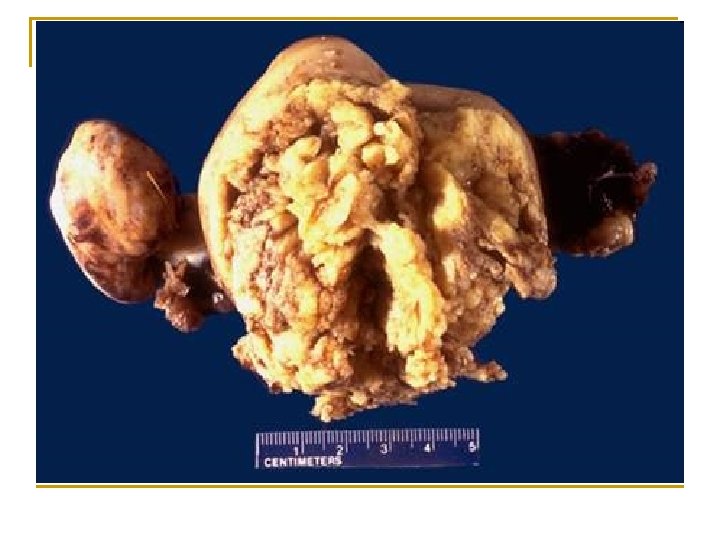
Modified WHO classification n n n endometrioid adenocarcinoma serous carcinoma clear cell carcinoma mucinous carcinoma serous carcinoma mixed types of carcinoma undifferentiated carcinoma

Clinical signs n Irregular vaginal bleeding, intermenstrual or post menopausal n Watery vaginal discharge may be present in postmenopausal women n Mass in late stages
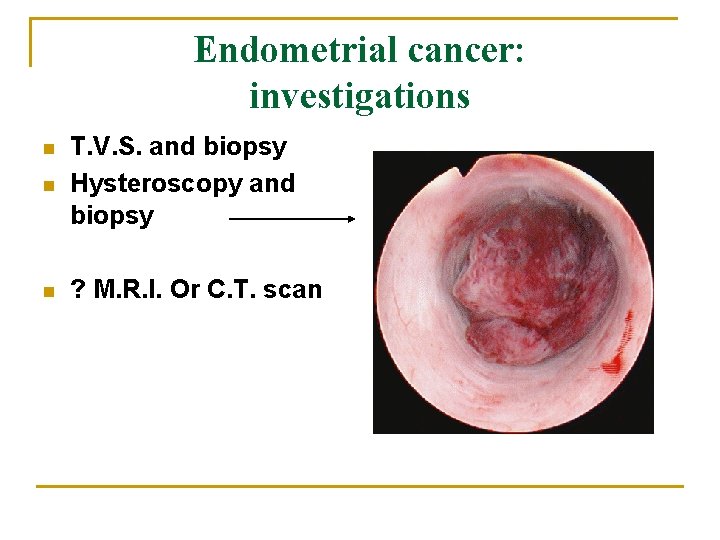
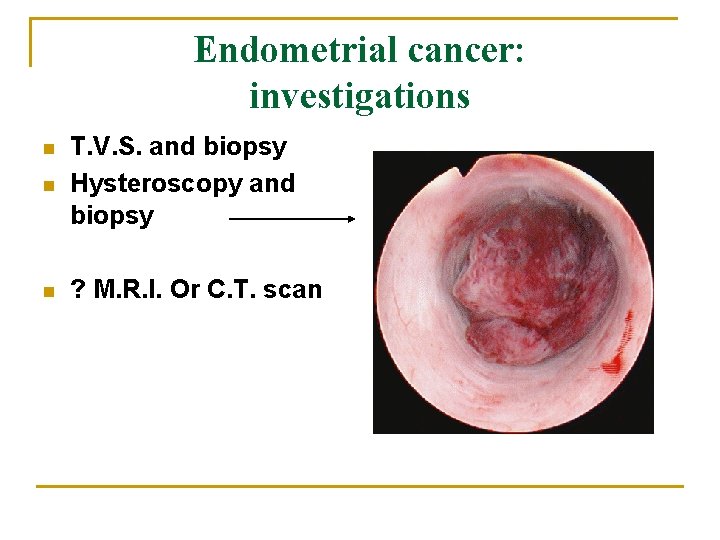
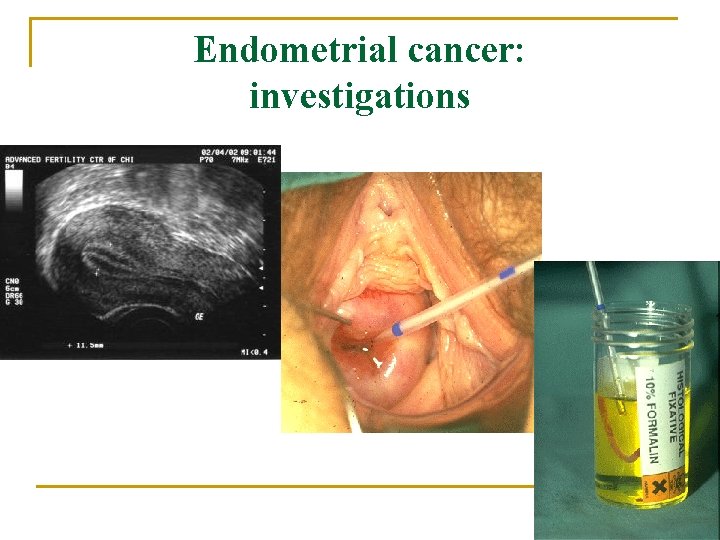
Endometrial cancer: investigations n T. V. S. and biopsy Hysteroscopy and biopsy n ? M. R. I. Or C. T. scan n
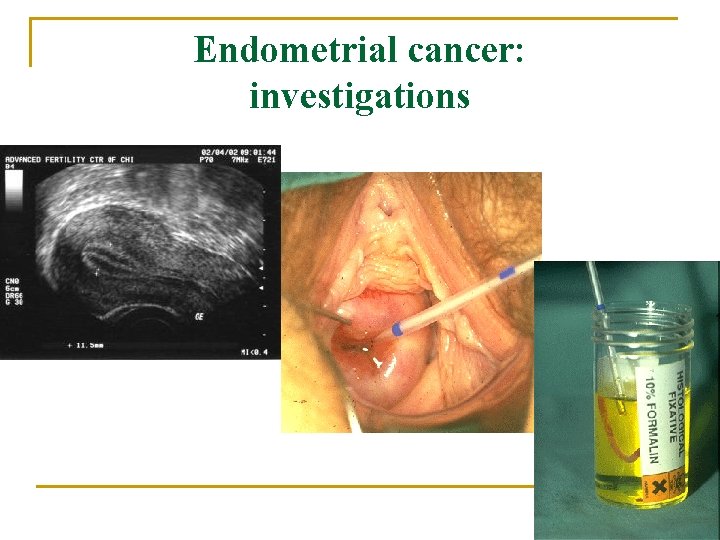
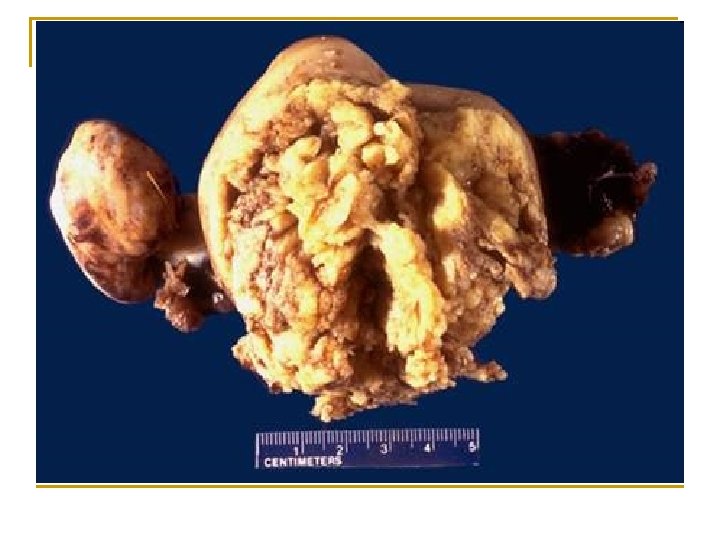
Endometrial cancer: investigations
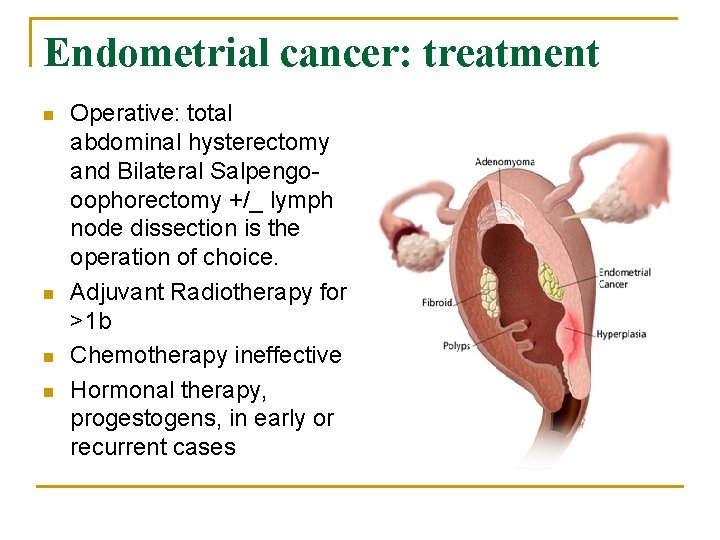
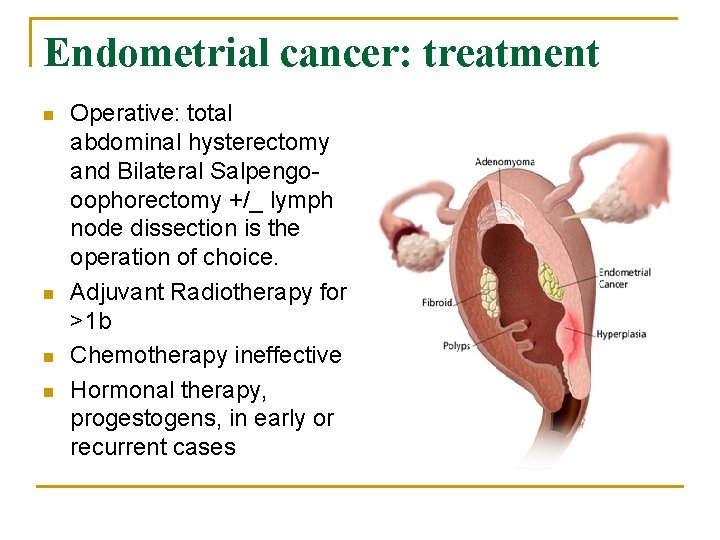
Endometrial cancer: treatment n n Operative: total abdominal hysterectomy and Bilateral Salpengooophorectomy +/_ lymph node dissection is the operation of choice. Adjuvant Radiotherapy for >1 b Chemotherapy ineffective Hormonal therapy, progestogens, in early or recurrent cases
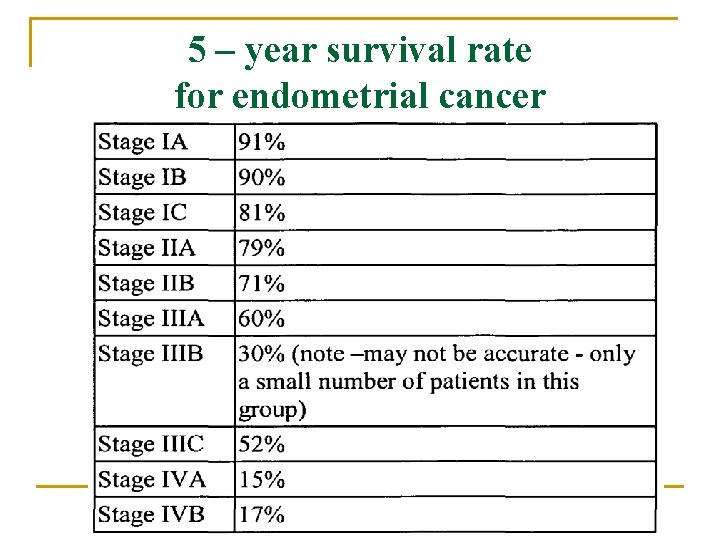
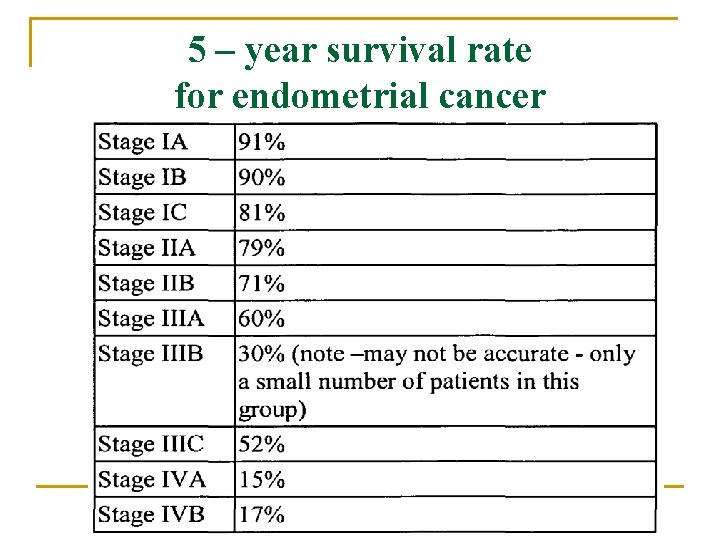
5 – year survival rate for endometrial cancer
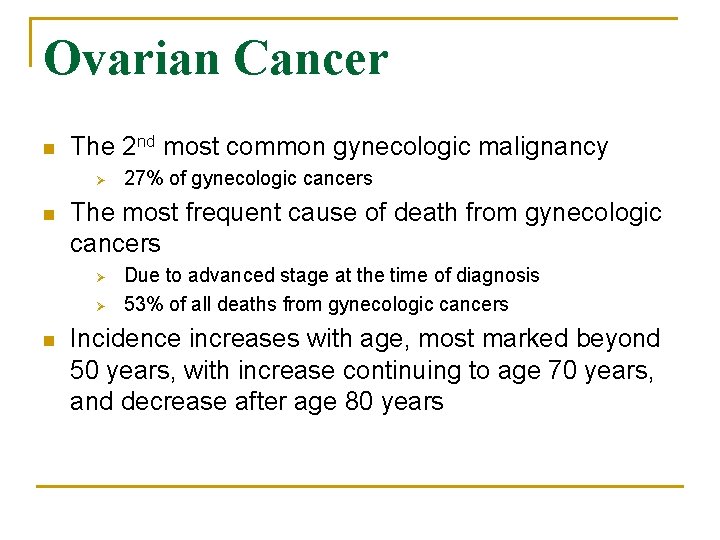
Ovarian Cancer n The 2 nd most common gynecologic malignancy Ø n The most frequent cause of death from gynecologic cancers Ø Ø n 27% of gynecologic cancers Due to advanced stage at the time of diagnosis 53% of all deaths from gynecologic cancers Incidence increases with age, most marked beyond 50 years, with increase continuing to age 70 years, and decrease after age 80 years
Risk factors n Family history of cancer n Personal history of cancer: Women who have had cancer of the breast, uterus, colon, or rectum have a higher risk of ovarian cancer Age over 55 Never pregnant: Menopausal hormone therapy: estrogen taking n n n
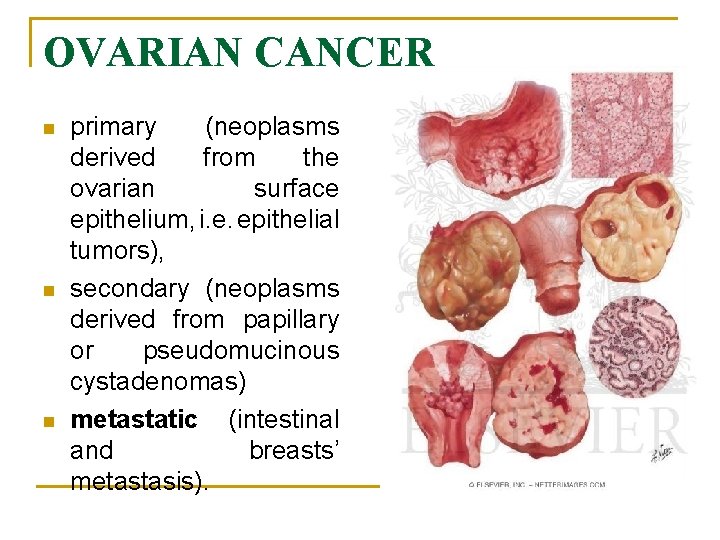
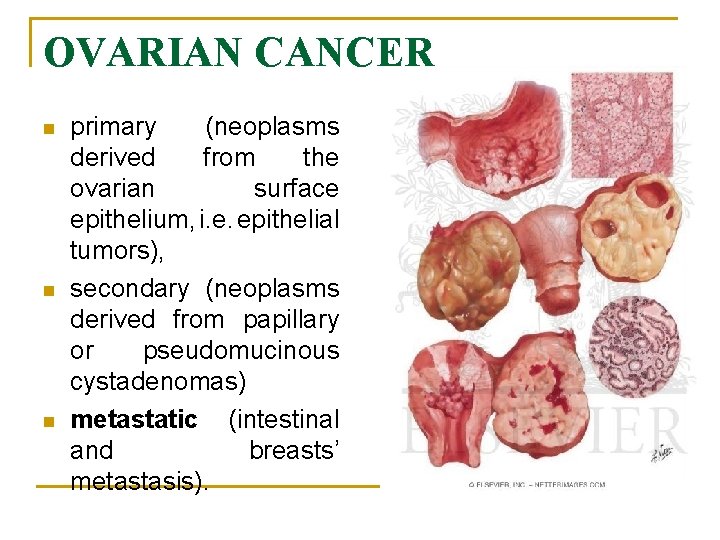
OVARIAN CANCER n n n primary (neoplasms derived from the ovarian surface epithelium, i. e. epithelial tumors), secondary (neoplasms derived from papillary or pseudomucinous cystadenomas) metastatic (intestinal and breasts’ metastasis).
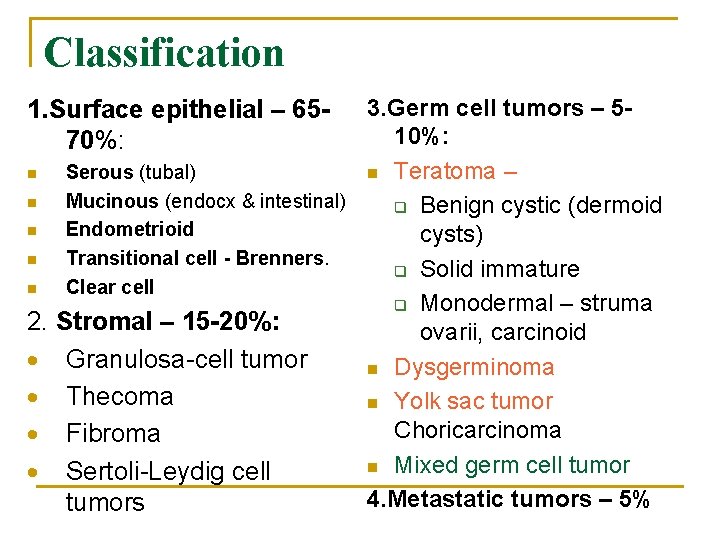
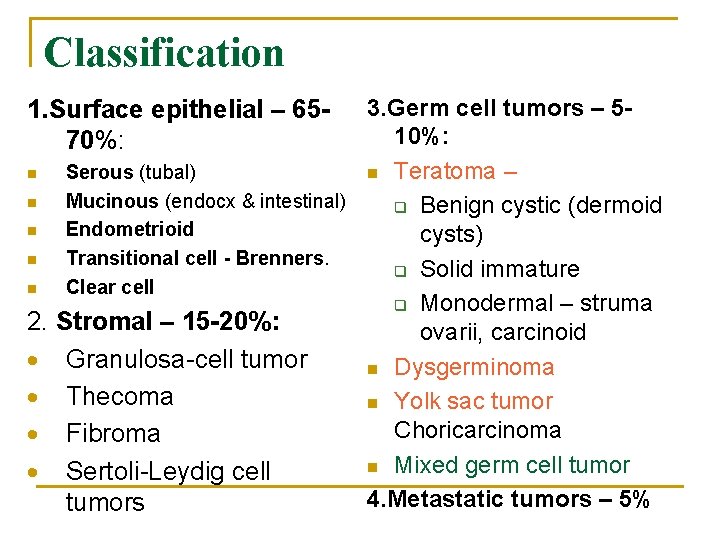
Classification 3. Germ cell tumors – 510%: Serous (tubal) n Teratoma – Mucinous (endocx & intestinal) q Benign cystic (dermoid Endometrioid cysts) Transitional cell - Brenners. q Solid immature Clear cell q Monodermal – struma Stromal – 15 -20%: ovarii, carcinoid Granulosa-cell tumor n Dysgerminoma Thecoma n Yolk sac tumor Choricarcinoma Fibroma n Mixed germ cell tumor Sertoli-Leydig cell 4. Metastatic tumors – 5% tumors 1. Surface epithelial – 6570%: n n n 2.
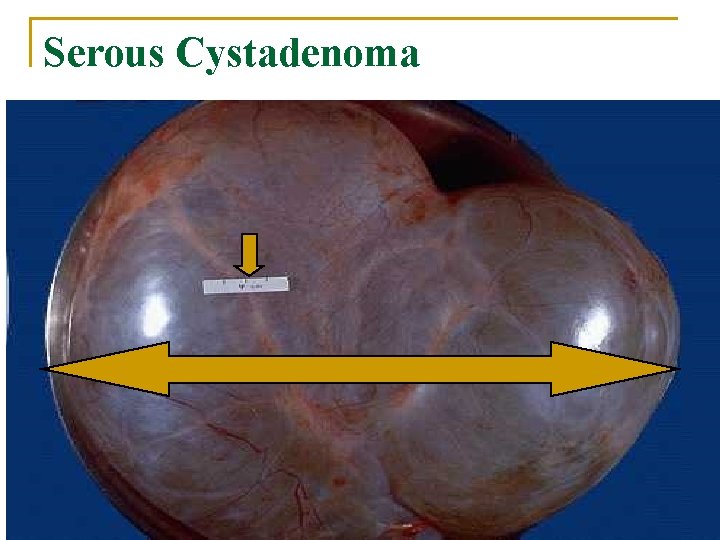
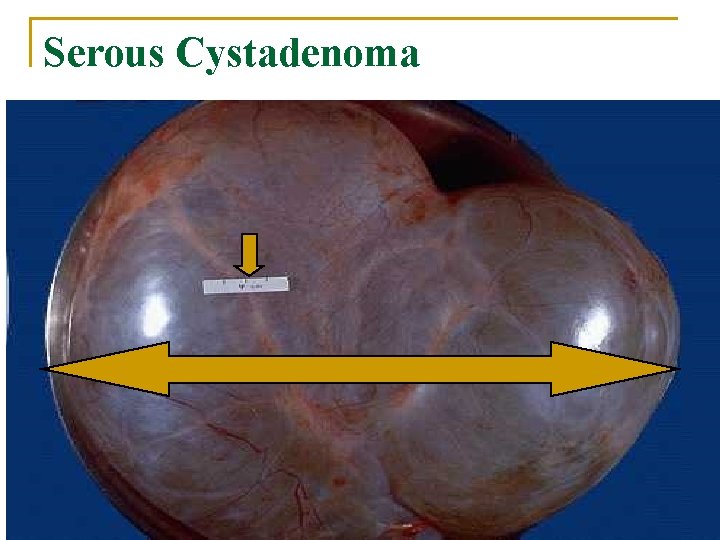
Serous Cystadenoma
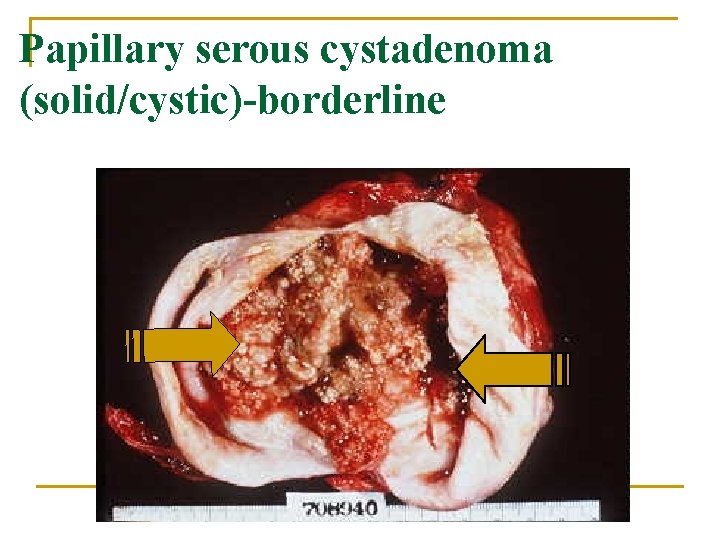
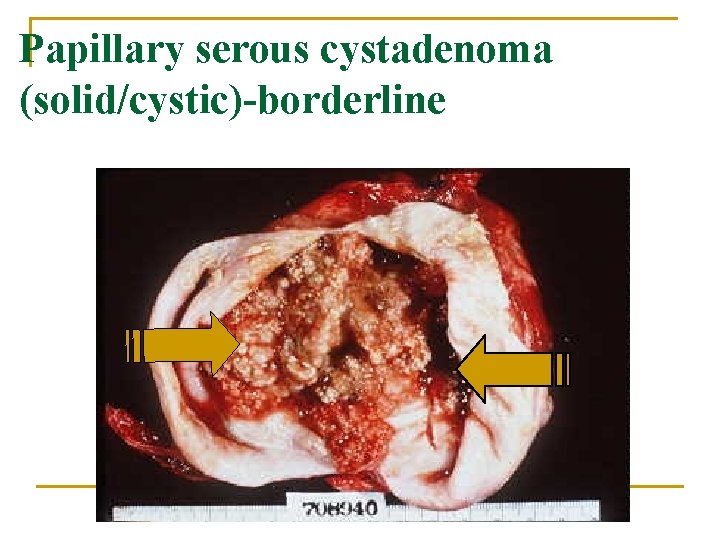
Papillary serous cystadenoma (solid/cystic)-borderline
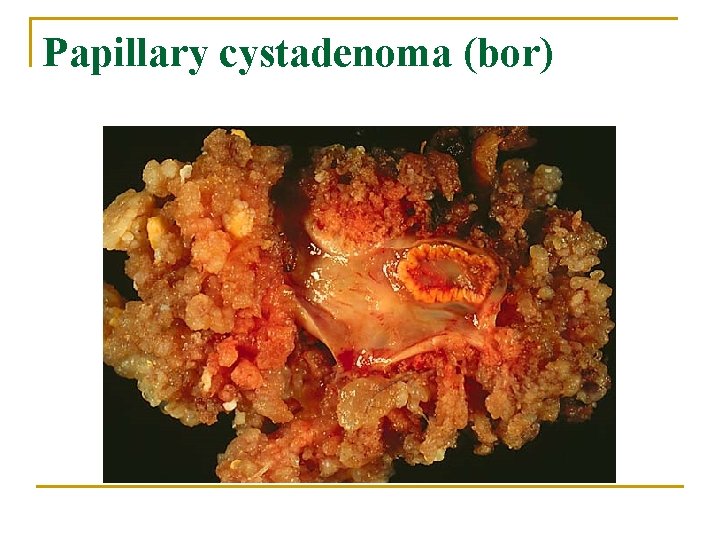
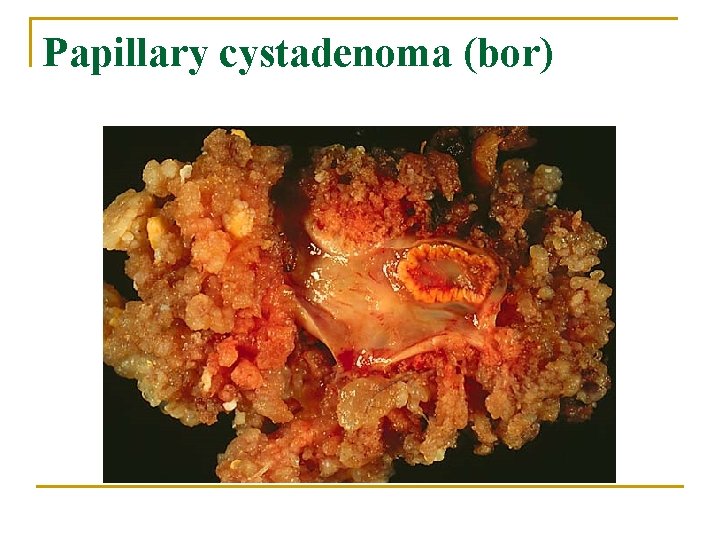
Papillary cystadenoma (bor)
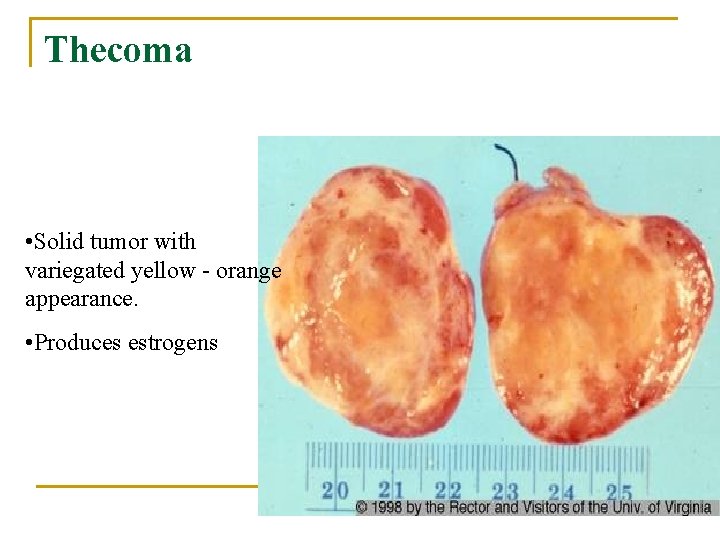
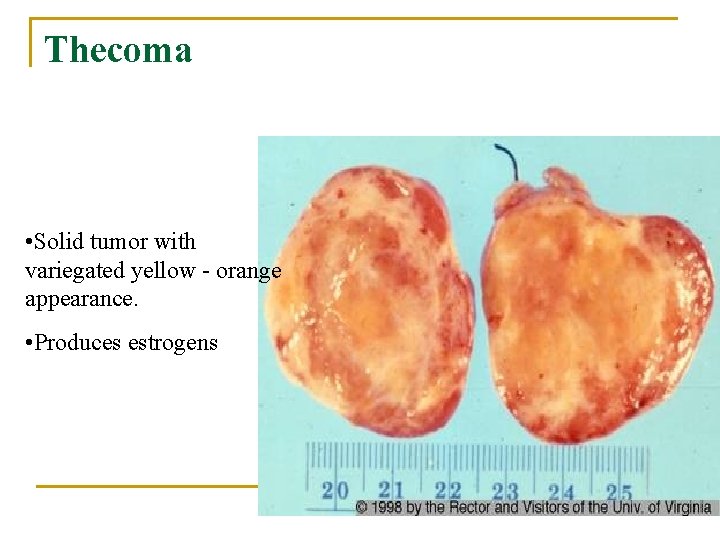
Thecoma • Solid tumor with variegated yellow - orange appearance. • Produces estrogens
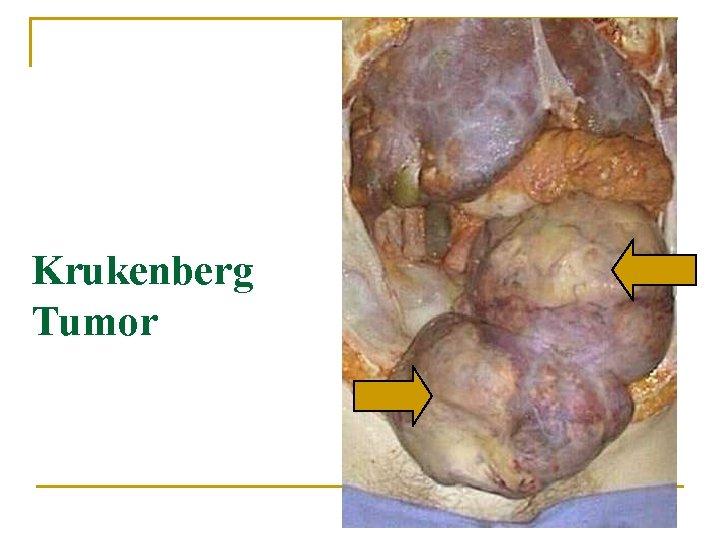
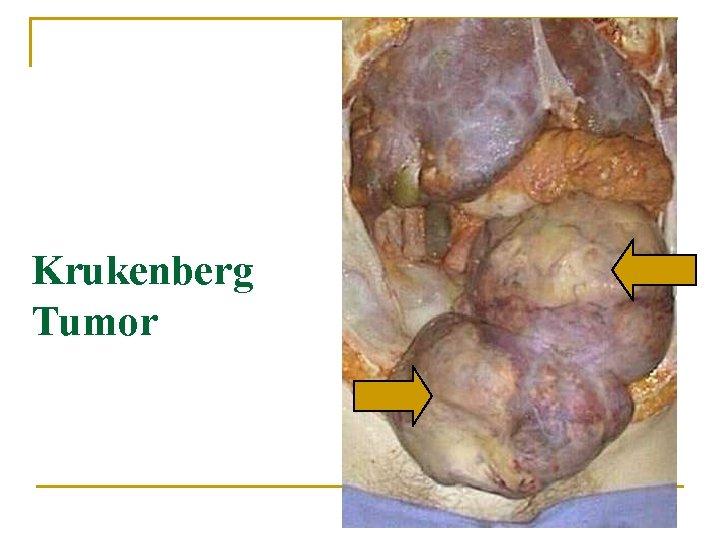
Krukenberg Tumor

FIGO classification
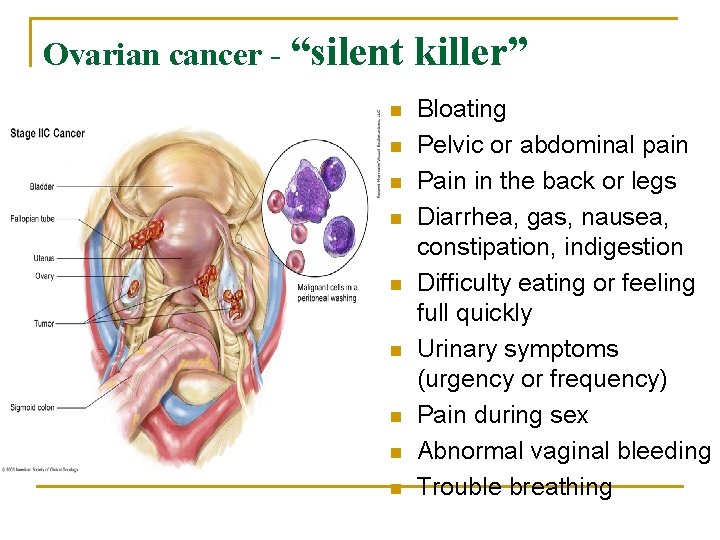
Ovarian cancer - “silent n n n n n killer” Bloating Pelvic or abdominal pain Pain in the back or legs Diarrhea, gas, nausea, constipation, indigestion Difficulty eating or feeling full quickly Urinary symptoms (urgency or frequency) Pain during sex Abnormal vaginal bleeding Trouble breathing


Diagnosis n n n n Physical examination Pelvic examination Rectovaginal examination Ultrasound Magnetic resonance imaging CA-125 high falsepositive rate HE 4 marker more sensitive than CA 125 Laparoscopy, microscopy The combination of HE 4 and CA 125 was more sensitive than either marker alone - Risk of Ovarian Malignancy Algorithm (ROMA) is calculated
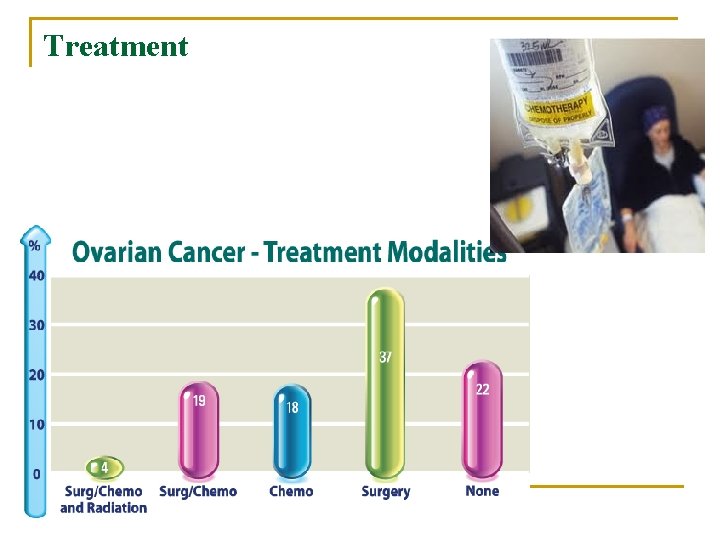
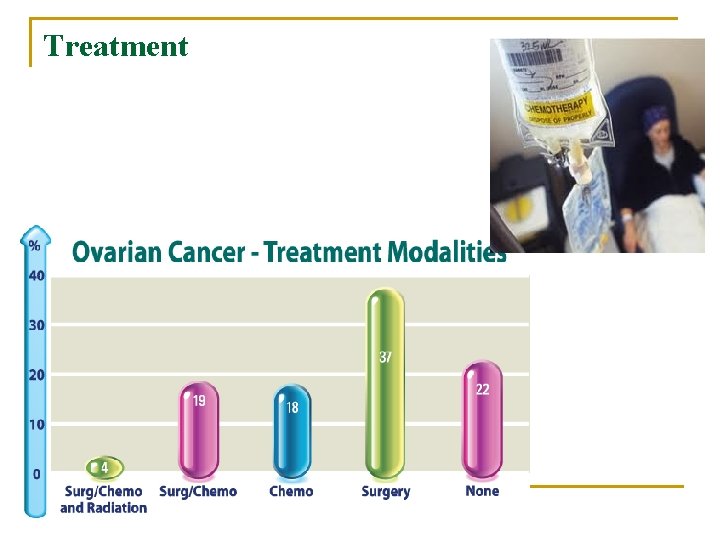
Treatment
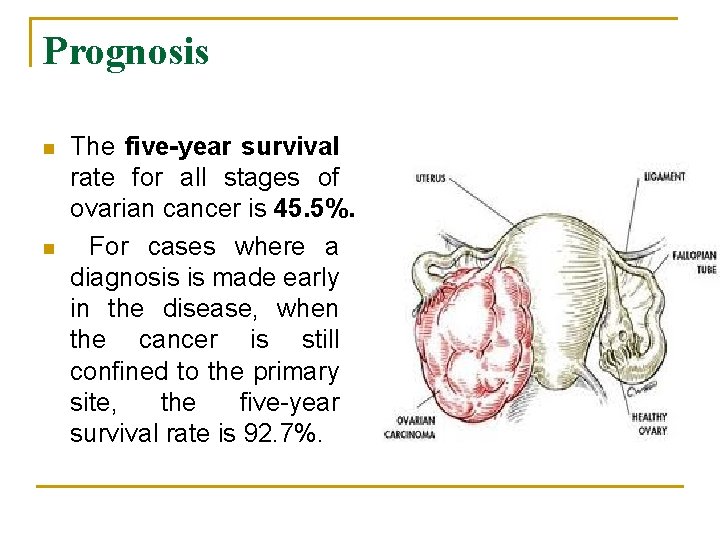
Prognosis n n The five-year survival rate for all stages of ovarian cancer is 45. 5%. For cases where a diagnosis is made early in the disease, when the cancer is still confined to the primary site, the five-year survival rate is 92. 7%.

 Sperm fructose
Sperm fructose Female organs
Female organs What is gonads
What is gonads Chapter 16 lesson 3 the female reproductive system
Chapter 16 lesson 3 the female reproductive system Mucous membrane reproductive system
Mucous membrane reproductive system Female organs
Female organs Internal genital organs female
Internal genital organs female Female reproductive organs sagittal section
Female reproductive organs sagittal section Female organs
Female organs Umbilical regions
Umbilical regions Female secondary sexual characteristics
Female secondary sexual characteristics Common female sexual fantasies
Common female sexual fantasies Bổ thể
Bổ thể Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Các số nguyên tố là gì
Các số nguyên tố là gì Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Sơ đồ cơ thể người
Sơ đồ cơ thể người Tư thế ngồi viết
Tư thế ngồi viết đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Thang điểm glasgow
Thang điểm glasgow ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Thể thơ truyền thống
Thể thơ truyền thống Cái miệng xinh xinh thế chỉ nói điều hay thôi
Cái miệng xinh xinh thế chỉ nói điều hay thôi Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Tư thế ngồi viết
Tư thế ngồi viết Ví dụ giọng cùng tên
Ví dụ giọng cùng tên Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ đại từ thay thế
đại từ thay thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Frameset trong html5
Frameset trong html5 Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phản ứng thế ankan
Phản ứng thế ankan Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập điện thế nghỉ
điện thế nghỉ Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Epidemiological triad
Epidemiological triad Retrocuspid papilla interdental clefts in primary teeth
Retrocuspid papilla interdental clefts in primary teeth X linked diseases
X linked diseases Difference between communicable and noncommunicable
Difference between communicable and noncommunicable Venn diagram of communicable and non-communicable diseases
Venn diagram of communicable and non-communicable diseases Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders