Practice Management TripleThreat Individual Team and PCMH Skill









- Slides: 35
Practice Management Triple-Threat: Individual, Team and PCMH Skill Development Andrea Darby-Stewart, MD St. Joseph’s FMR, AZ Sharry Veres, MD St. Anthony FMR, CO

ACTIVITY DISCLAIMER The material presented at this activity is being made available by the American Academy of Family Physicians for educational purposes only. This material is not intended to represent the only, nor necessarily best, method or procedure appropriate for the medical situations discussed but, rather, is intended to present an approach, view, statement or opinion of the faculty that may be helpful to others who face similar situations. The AAFP disclaims any and all liability for injury or other damages resulting to any individual attending this program and for all claims that may arise out of the use of the techniques demonstrated therein by such individuals, whether these claims shall be asserted by a physician or any other person. Every effort has been made to ensure the accuracy of the data presented at these activities. Physicians may care to check specific details such as drug doses and contraindications, etc. in standard sources prior to clinical application. These materials have been produced solely for the education of attendees. Any use of content or the name of the speaker or AAFP is prohibited without written consent of the AAFP. FACULTY DISCLOSURE The AAFP has selected all faculty appearing in this program. It is the policy of the AAFP that all CME planning committees, faculty, authors, editors, and staff disclose relationships with commercial entities upon nomination or invitation of participation. Disclosure documents are reviewed for potential conflicts of interest and, if identified, they are resolved prior to confirmation of participation. Only those participants who had no conflict of interest or who agreed to an identified resolution process prior to their participation were involved in this CME activity.
Objectives • Identify level-specific goals and objectives for each year of a Practice Management (PM) longitudinal curriculum • Identify areas in the FMR where participants can integrate PM curricula into existing programs, meetings, task forces and clinic operations • Discuss challenges to implementing this type of curriculum into an FMR including preconceived ideas about what learners can accomplish at each level of training and time barriers to completion
Objectives • Identify level-specific goals and objectives for each year a Practice Management (PM) Andof. NOW WHAT DO WE DO longitudinal curriculum • Identify areas in the FMR where participants can integrate PM curricula into existing programs, Withtask NAS andand Milestones? ? ? meetings, forces clinic operations • Discuss challenges to implementing this type of curriculum into an FMR including preconceived ideas about what learners can accomplish at each level of training and time barriers to completion
PM Curriculum Formats • What is the format of your current PM (Management of Health Systems) curriculum? • What do you tell the site visitor about your PM curriculum? – What will “they” be looking for during a selfstudy?
Timeline and Inspiration • April 2011: New EMR challenges preconceived notions of the “system” that FMR is working in • October 2011: New Program Director and 5 new faculty added to mix • November 2011: NCQA Level 3 PCMH designation achieved
“Old” PM paradigm • One month block rotation PGY 2 or PGY 3 year – “Insert knowledge” – Clinic QI project – individual interest • Some maintain traction, others fade away… – FMR meetings, Az. AFP Practice Management annual meeting for residents count toward hours • No regular information on practice or productivity – Citation during last site visit – Major challenges with transition to new EMR • Individuals interested in population management seek out those opportunities
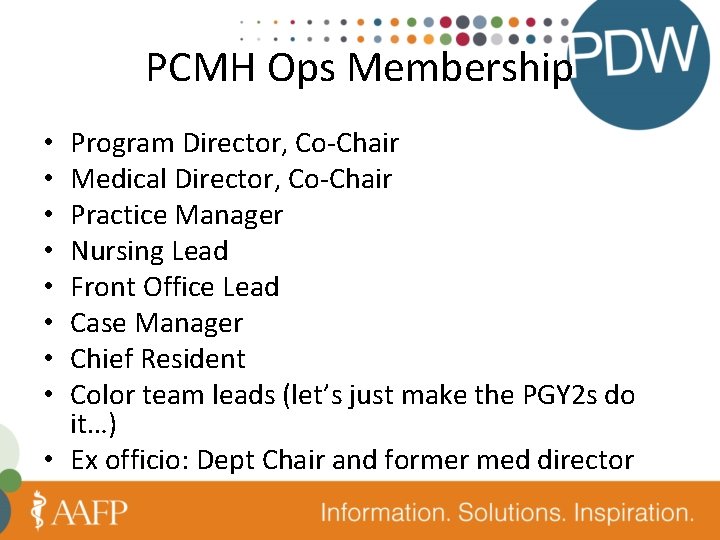
PCMH Operations Committee • The Patient-Centered Medical Home Operations Committee (PCMH Ops. Com) is charged with strategic planning and development of projects for the Peppertree Family Medicine Residency Clinic (FMC). • Goals: • Optimize clinic functioning so that patient’s receive timely, evidence-based and patient-centered care. • Achieve ongoing NCQA PCHM Level 3 status (next renewal 2014) • Identify best practices for patient care, systems management and operations of the FMRC. • Ensure alignment of various subcommittees with the overarching goals of patient-care in the FMC • Identify and mitigate risk management opportunities including root cause analysis as indicated
PCMH Ops Committee • Subcommittees to the PCMH Ops. Com: • Process Improvement Committee (detailed identification of operations processes/practices; recommendations for implementation) • Academic Committee (identification of educational related issues in ambulatory, procedures and practice management curricula) • Color Teams (daily care of patients with direct and indirect care as well as PI project implementation) • Block Committee (communication of educational information and patient-care related information to residency constituents) • OB Risk Management Group (identification of educational related issues in maternity and newborn care as well as implementation of operations/processes for maternity and newborn patients)
PCMH Ops Membership Program Director, Co-Chair Medical Director, Co-Chair Practice Manager Nursing Lead Front Office Lead Case Manager Chief Resident Color team leads (let’s just make the PGY 2 s do it…) • Ex officio: Dept Chair and former med director • •
What are We Really Teaching ? ? ? • What are your goals for your PM rotation?
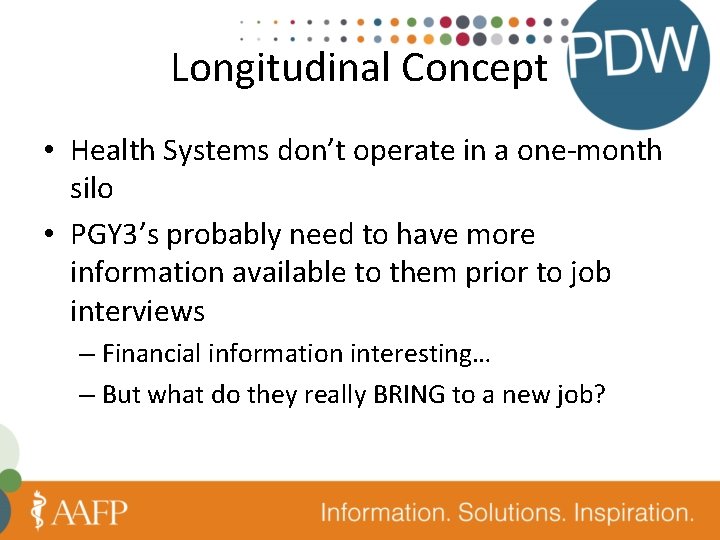
Longitudinal Concept • Health Systems don’t operate in a one-month silo • PGY 3’s probably need to have more information available to them prior to job interviews – Financial information interesting… – But what do they really BRING to a new job?
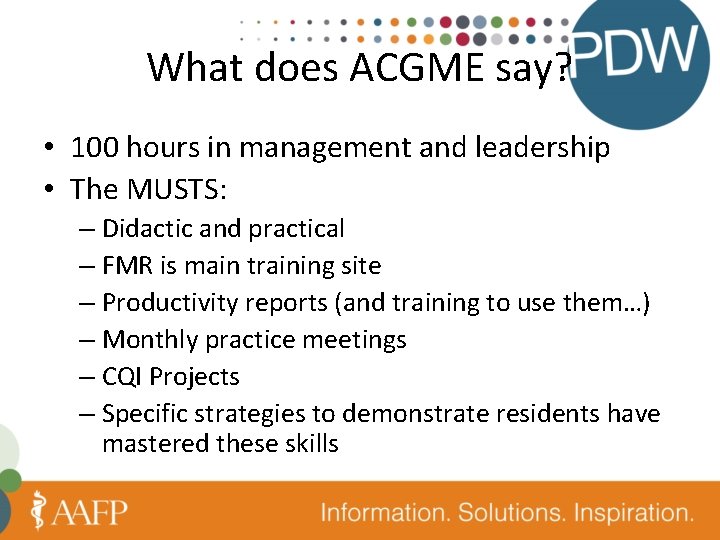
What does ACGME say? • 100 hours in management and leadership • The MUSTS: – Didactic and practical – FMR is main training site – Productivity reports (and training to use them…) – Monthly practice meetings – CQI Projects – Specific strategies to demonstrate residents have mastered these skills
What Does ACGME say? • The SHOULDS: – Billing, budgeting, staffing, technology, value in marketplace, customer satisfaction, clinical quality, tort liability, risk management, scheduling, computers, employment law, personnel management, media relations – Leadership training is a SHOULD, not a MUST • REALLY? ? ? • Practice, hospital, specialty and community leadership all mentioned
Wait for it…. • Draft Program Requirements (March 2013) • IV. A. 6. t). (1) Residents must have at least 100 hours or one month dedicated to health system management experiences. – This curriculum should prepare residents to be active participants and leaders in their practices, their communities, and the profession of medicine. To accomplish this objective, residents should be a member of a health system or professional group committee.

Draft requirements • Must – Receive regular reports of individual and practice productivity, financial performance and clinical quality • Training to read report – Attend regular FMP business meetings with staff and faculty to discuss practice-related policies and procedures, business and service goals, and practice efficiency and quality.

And then there are Milestones SBP-2 Emphasizes patient safety • Level 1: Understands that medical errors affect patient health and safety and their occurrence varies across settings and between providers • Level 2: Recognizes medical errors when they occur, including those that do not have adverse outcomes ; Understands and follows protocols to promote patient safety and prevents medical errors • Level 3: Uses current methods of analysis to identify individual and system causes of medical errors common to family medicine; Develops individual and system improvement plans that promote patient safety and prevents medical errors • Level 4: Consistently engages in self-directed and practice improvement activities that seek to identify and address medical errors and patient safety in daily practice; Fosters adherence to patient care protocols amongst team members that enhance patient safety and prevents medical errors • Level 5: Role models self-directed and system improvement activities that seek to continuously anticipate, identify and prevent medical errors to improve patient safety in all practice settings including the development, use, and promotion of patient care protocols and other tools

Milestones… SBP-4 Coordinates team based care • Level 1: Understands quality patient care requires coordination and teamwork and participates as a willing team member • Level 2: Understands the roles and responsibilities of oneself and of patients, families, consultants and interprofessional team members needed to optimize care and accepts responsibility for coordination of care • Level 3: Engages the appropriate care team needed to provide accountable team-based, coordinated care centered on individual patient needs; Assumes responsibility for seamless transitions of care • Level 4: Assumes ultimate responsibility for the coordination of care and directs appropriate care teams to optimize the care of patients; Sustains a personal relationship with his/her own patients • Level 5: Role models leadership, integration, and optimization of care teams to provide quality, individualized patient care

Milestones… • PBLI – 3 Improves systems in which the physician provides care • Level 1: Recognizes inefficiencies, variation, and quality gaps in health care delivery • Level 2: Compares care provided by self and clinic to external standards and identifies areas for improvement • Level 3: Uses systematic improvement method (e. g. PDSA cycle) to address an identified area of improvement; Uses an organized method, such as a registry, to assess and manage population health • Level 4: Comfortable with establishing protocols for continuous review and comparison of practice procedures and outcomes and implementing changes to address areas needing improvement Level 5: Role models continuous quality improvement of personal practice as well as larger health systems or complex projects using advanced methodologies (e. g. six sigma) and skill sets •
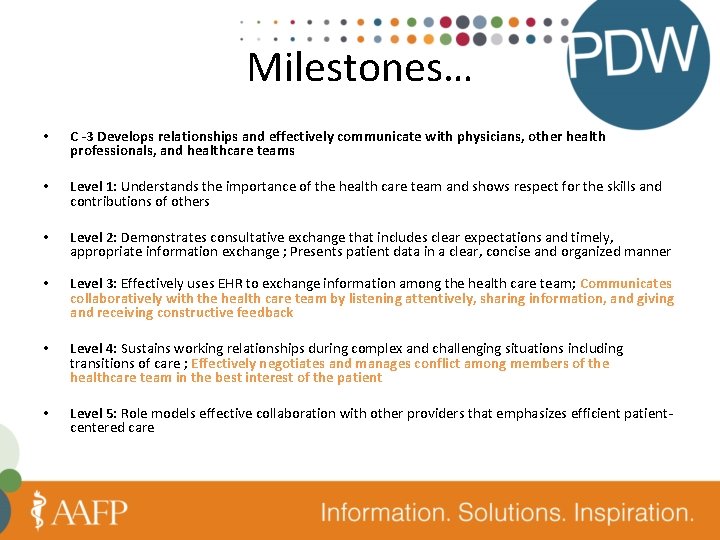
Milestones… • C -3 Develops relationships and effectively communicate with physicians, other health professionals, and healthcare teams • Level 1: Understands the importance of the health care team and shows respect for the skills and contributions of others • Level 2: Demonstrates consultative exchange that includes clear expectations and timely, appropriate information exchange ; Presents patient data in a clear, concise and organized manner • Level 3: Effectively uses EHR to exchange information among the health care team; Communicates collaboratively with the health care team by listening attentively, sharing information, and giving and receiving constructive feedback • Level 4: Sustains working relationships during complex and challenging situations including transitions of care ; Effectively negotiates and manages conflict among members of the healthcare team in the best interest of the patient • Level 5: Role models effective collaboration with other providers that emphasizes efficient patientcentered care

• How do you achieve ALL of this with your residents?
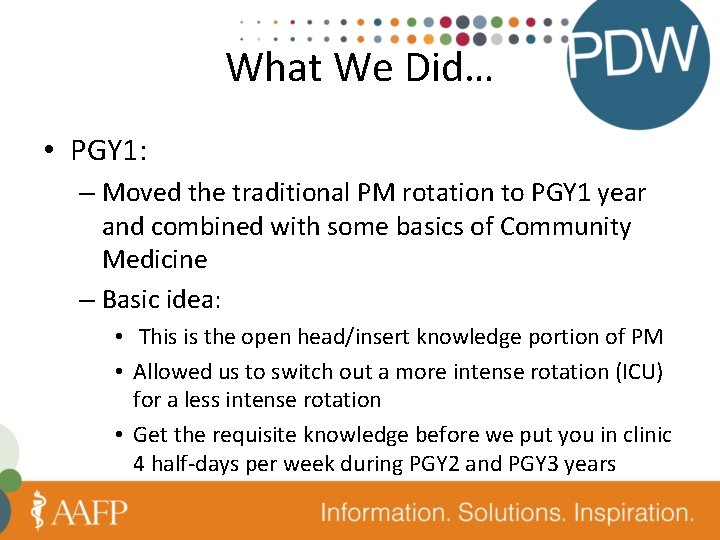
What We Did… • PGY 1: – Moved the traditional PM rotation to PGY 1 year and combined with some basics of Community Medicine – Basic idea: • This is the open head/insert knowledge portion of PM • Allowed us to switch out a more intense rotation (ICU) for a less intense rotation • Get the requisite knowledge before we put you in clinic 4 half-days per week during PGY 2 and PGY 3 years
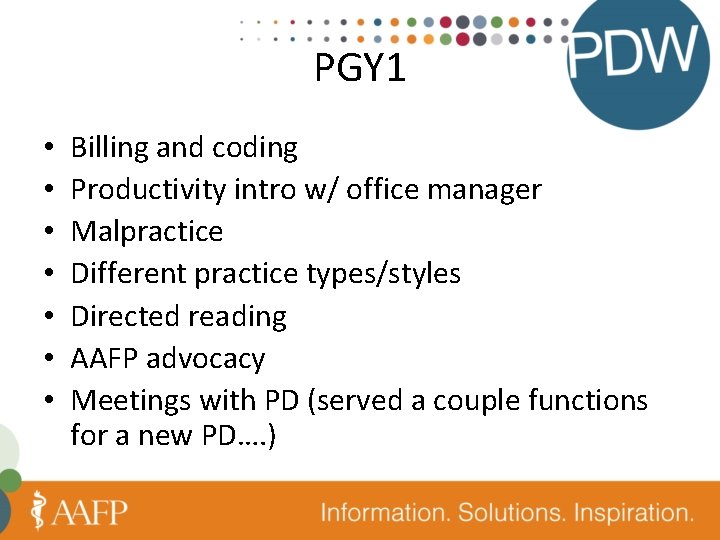
PGY 1 • • Billing and coding Productivity intro w/ office manager Malpractice Different practice types/styles Directed reading AAFP advocacy Meetings with PD (served a couple functions for a new PD…. )
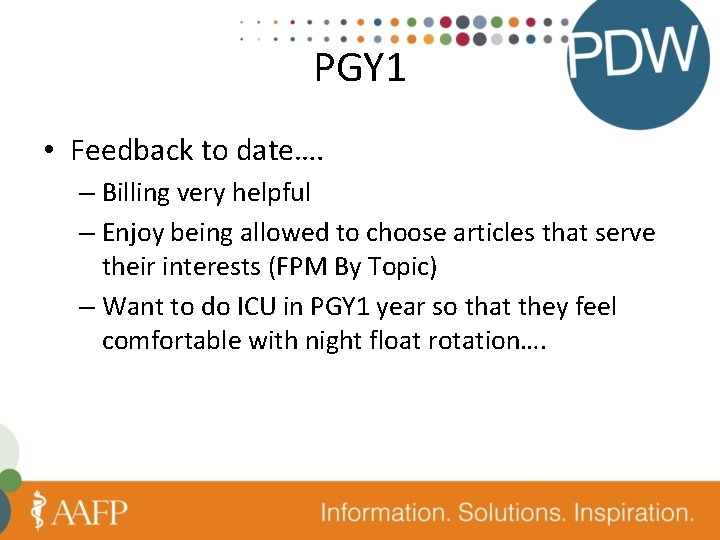
PGY 1 • Feedback to date…. – Billing very helpful – Enjoy being allowed to choose articles that serve their interests (FPM By Topic) – Want to do ICU in PGY 1 year so that they feel comfortable with night float rotation….
PGY 2 • Leading the Clinical Team – 5 clinical teams in our practice (Faculty, resident, RN, MA) – 6 months as clinical team lead – Directed activities with dedicated faculty member • • Leadership assessment Self-determined goals CQI project leadership for team based on quality metrics PCMH Ops Committee Representative – FM Clinic Month during this time period
PGY 2 • Mixed in the first 6 months – either busy work or helpful – Everyone wants more time to do the projects • Project was a bit challenging as we discovered that our EHR couldn’t really run the right reports… • Second group to go through has more enthusiasm and ideas for projects – Probably a function of “first followers” and just knowing what to expect
PGY 3 PCMH Project Leadership: • 2 longitudinal experiences in core administrative or clinical areas in the FMC – Focus on group and systems management • Hone skills in critically evaluating clinical or population data – Assess the effectiveness of care at the systems level – Planning and initiate improved workflow and/or clinic operations
PGY 3 Experiences • • • Emergency Preparedness Triage Team Multidisciplinary Care Management Team Therapeutics, equipment, testing and vaccines Behavioral Health and Chronic Disease
PGY 3 • Herding cats… – “we already did a QI project” – Want more time to do projects – Had to reduce to one per year due to inertia and change fatigue
Keeping with Tradition… • We still… – Count all meetings toward PM hours – Have Dignity Health Recruiters come talk about risk management, CVs, practice options, how to avoid a lawsuit – Have St. Joseph’s CMO’s come talk about meaningful use, P 4 P, core measures, new EMR in hospital, etc… – Participate in Az. AFP Annual Practice Management Forum (PGY 3 s and PM resident)

Barriers • What to you see as barriers?
Barriers… • Resistance to moving ICU rotation to PGY 2 year • Change (in and of itself) • PGY 2 s “can’t lead teams” – too inexperienced – Hidden barrier: faculty can’t step back and LET them lead teams…. • We already did our project! • When do we have time to do these projects?

Next Steps • More robust population management • Empowering teams further to identify their own patients – Incorporate Care Management Committee principles to teams • Change our block didactics to team-based population and patient management time • Ensure FM resident participation in new St. Joseph’s IHI Chapter
• What other goals would you have for this curriculum?

THANK YOU!