PRACTICE GUIDELINES CLINICAL PATHWAY ON MANAGEMENT OF DYSPEPSIA

- Slides: 22
PRACTICE GUIDELINES & CLINICAL PATHWAY ON MANAGEMENT OF DYSPEPSIA
Clinical Scenario 30 year old, male Call center representative Epigastric pain Denies any alarm features Smoker; alcohol and coffee drinker Unremarkable past medical & family history Direct epigastric tenderness
Dyspepsia Presence of 1 or more of the following symptoms (Rome III Committee): Postprandial fullness Early satiety Epigastric pain or burning
Assessment & Diagnosis Based on history and physical and exam Consider or rule out: Dietary indiscretion Medication induced Cardiac disease Gastroparesis Hepatobiliary disorders Other systemic disease
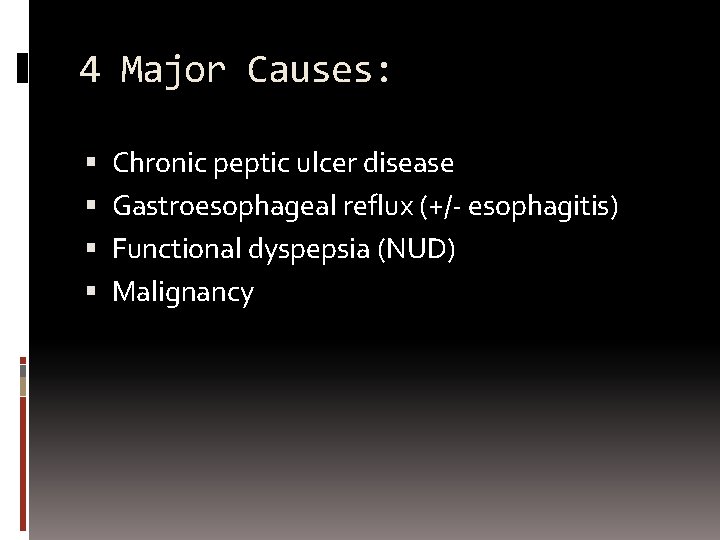
4 Major Causes: Chronic peptic ulcer disease Gastroesophageal reflux (+/- esophagitis) Functional dyspepsia (NUD) Malignancy
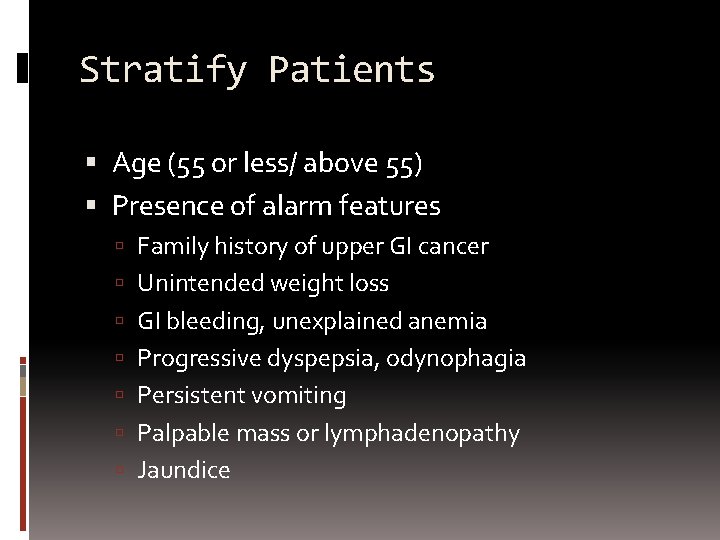
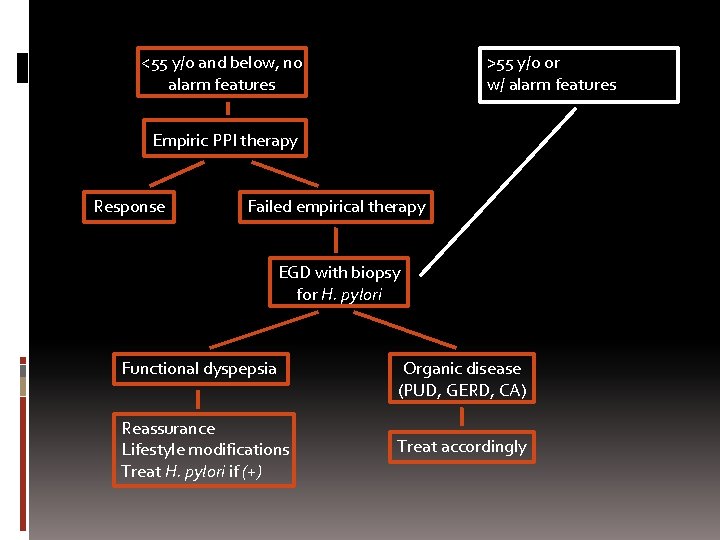
Stratify Patients Age (55 or less/ above 55) Presence of alarm features Family history of upper GI cancer Unintended weight loss GI bleeding, unexplained anemia Progressive dyspepsia, odynophagia Persistent vomiting Palpable mass or lymphadenopathy Jaundice
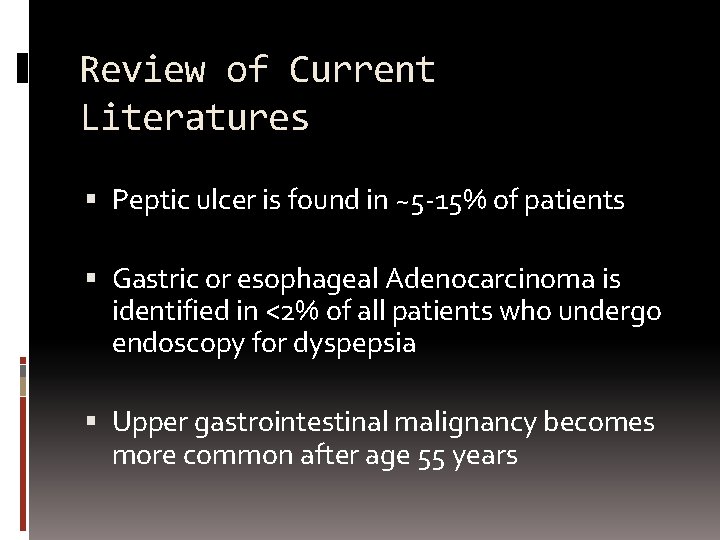
Review of Current Literatures Peptic ulcer is found in ~5 -15% of patients Gastric or esophageal Adenocarcinoma is identified in <2% of all patients who undergo endoscopy for dyspepsia Upper gastrointestinal malignancy becomes more common after age 55 years
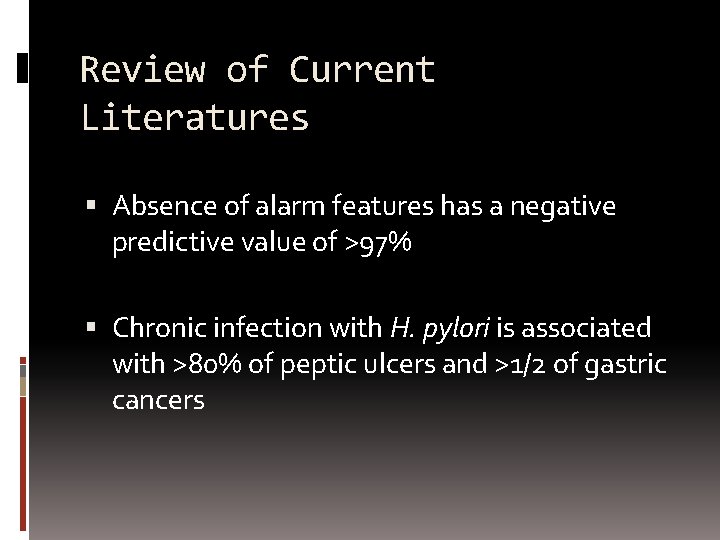
Review of Current Literatures Absence of alarm features has a negative predictive value of >97% Chronic infection with H. pylori is associated with >80% of peptic ulcers and >1/2 of gastric cancers
Patient Profile 30 year old, male Burning epigastric pain No alarm symptoms
Empiric PPI Therapy Empiric therapy with proton pump inhibitors for 4 - 6 weeks Reassurance No further investigations if symptoms improve Out patient clinic follow-up
Failed Empirical Therapy No response to therapy after 7 -10 days Symptoms has not resolved after 6 -8 weeks EGD with biopsy for H. pylori Organic disease (PUD, GERD, CA) Treat accordingly
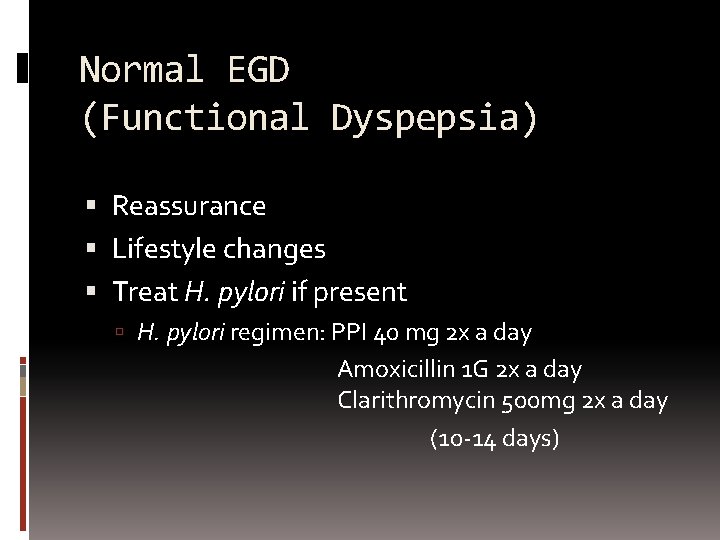
Normal EGD (Functional Dyspepsia) Reassurance Lifestyle changes Treat H. pylori if present H. pylori regimen: PPI 40 mg 2 x a day Amoxicillin 1 G 2 x a day Clarithromycin 500 mg 2 x a day (10 -14 days)
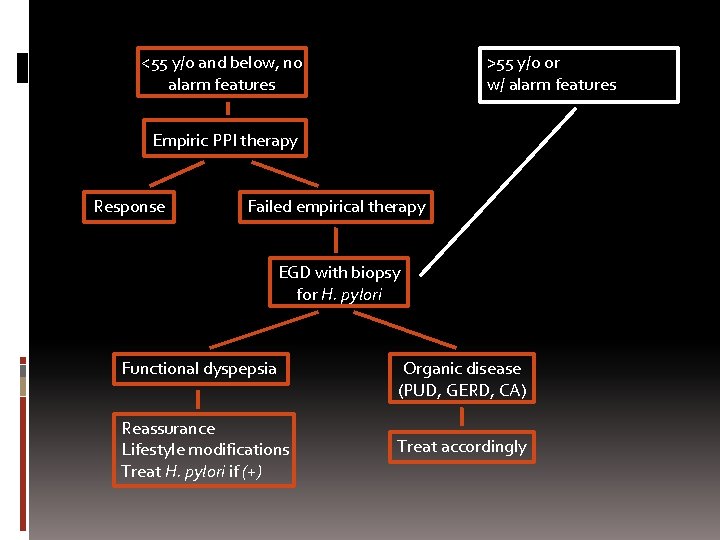
<55 y/o and below, no alarm features >55 y/o or w/ alarm features Empiric PPI therapy Response Failed empirical therapy EGD with biopsy for H. pylori Functional dyspepsia Reassurance Lifestyle modifications Treat H. pylori if (+) Organic disease (PUD, GERD, CA) Treat accordingly
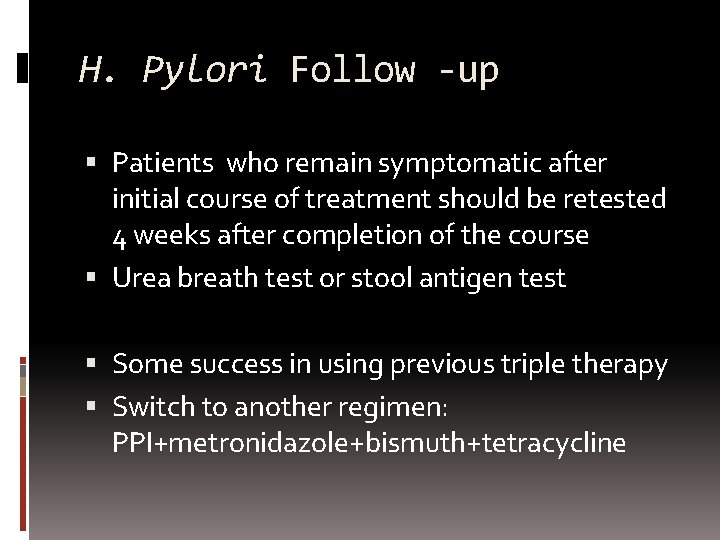
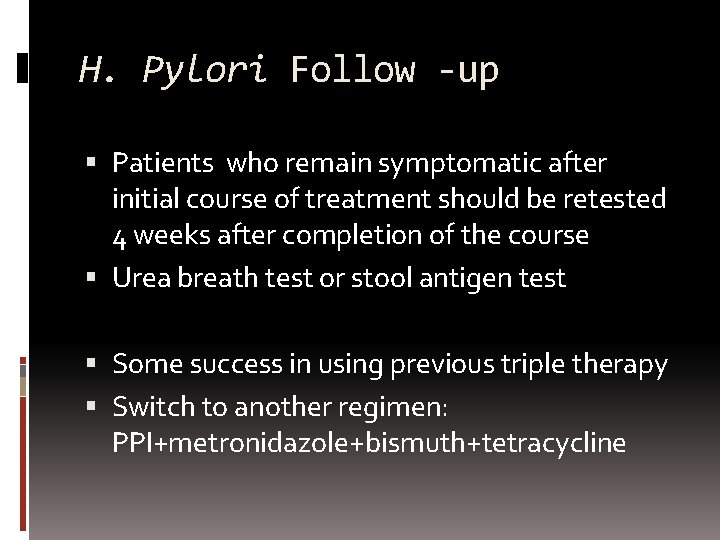
H. Pylori Follow -up Patients who remain symptomatic after initial course of treatment should be retested 4 weeks after completion of the course Urea breath test or stool antigen test Some success in using previous triple therapy Switch to another regimen: PPI+metronidazole+bismuth+tetracycline
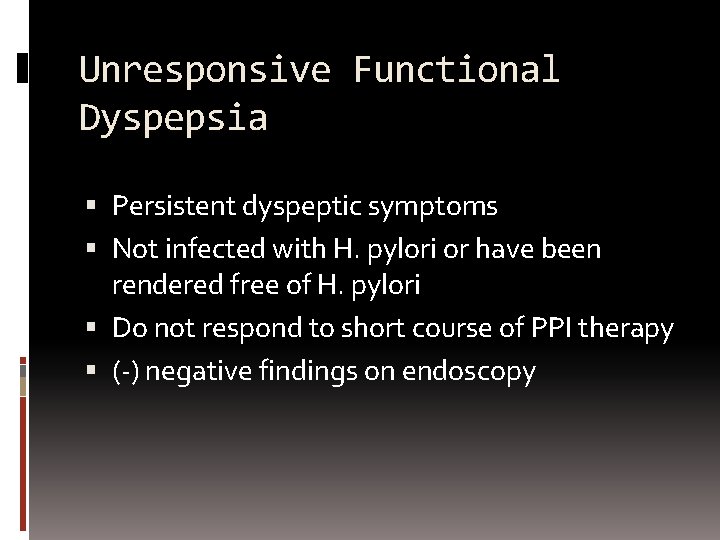
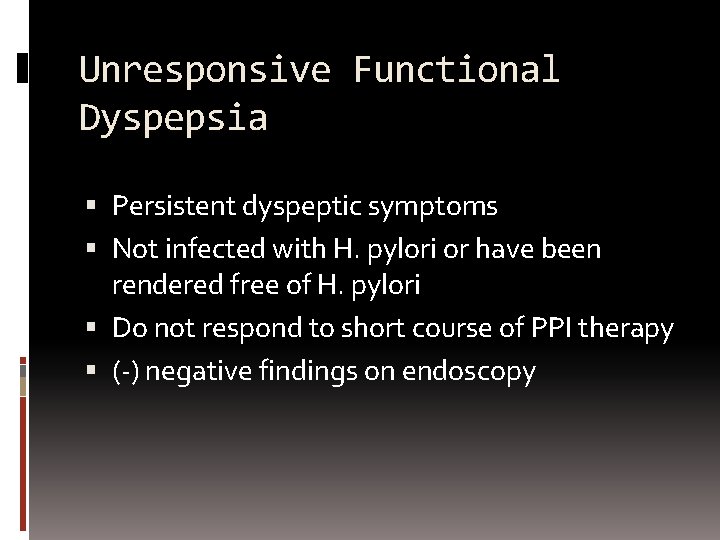
Unresponsive Functional Dyspepsia Persistent dyspeptic symptoms Not infected with H. pylori or have been rendered free of H. pylori Do not respond to short course of PPI therapy (-) negative findings on endoscopy
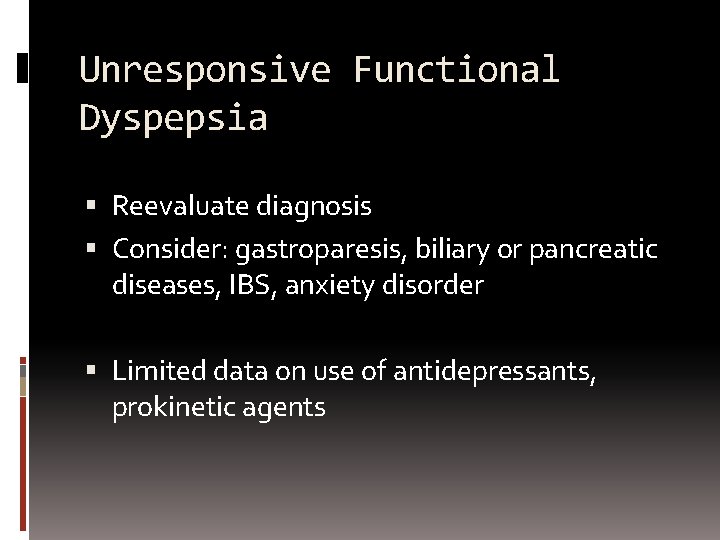
Unresponsive Functional Dyspepsia Reevaluate diagnosis Consider: gastroparesis, biliary or pancreatic diseases, IBS, anxiety disorder Limited data on use of antidepressants, prokinetic agents

References Talley NJ, Vakil NB, Moayyedi P: American Gastroenterological Association Technical Review: Evaluation of Dyspepsia. Gasteroenterology 2005, 129: 1756 -1780. American Gastroenterological Association Medical Position Statement: Evaluation of Dyspepsia Gastroenterology 2005, 129: 1753 -1755. Lam SK, Talley NJ: Report for the 1997 Asia Pacific. Consensus Guidelines on the management of H. pylori. Journal Gasteroenterology & Hepatology 1998, 13: 1 -2. American Society for Gastrointestinal Endoscopy’s The role of endoscopy in dyspepsia. Gastrointestinal Endoscopy 2007, 6: 1071 -1075 Sleisenger and Fordtran’s Gastrointestinal and Liver Disease 8 th Edition
Prepared by: Dr. Ernesto Olympia Dr. Benjamin Benitez Dr. Patricia Prodigalidad Dr. William Rodriguez
THANK YOU AND GOOD DAY.
Test-and-Treat Approach Test for H. pylori (Urea Breath Test or Stool Antigen Test) Treat if (+) Trial of PPI therapy if (-) Do endoscopy if no symptom improvement
Need for in-patient work-up and care Severity of dyspepsia Alarm symptoms present Need for additional lab tests and imaging studies
Possible Scenario 50 year old with CAD on ASA Severe epigastric pain, weakness, melena Pale Will need: Hospital admission for medical management Early endosocopy, CBC Blood transfusion