Practice Facilitators A New Profession Practice Facilitators In






- Slides: 15

Practice Facilitators, A New Profession Practice Facilitators In OKPRN Cara Vaught, MPH Katy D Smith, MS Crystal Turner, MPH Eileen Merchen, MS Zsolt Nagykaldi Ph. D, James Mold MD, MPH and Cheryl Aspy, Ph. D Oklahoma Physicians Resource/Research Network
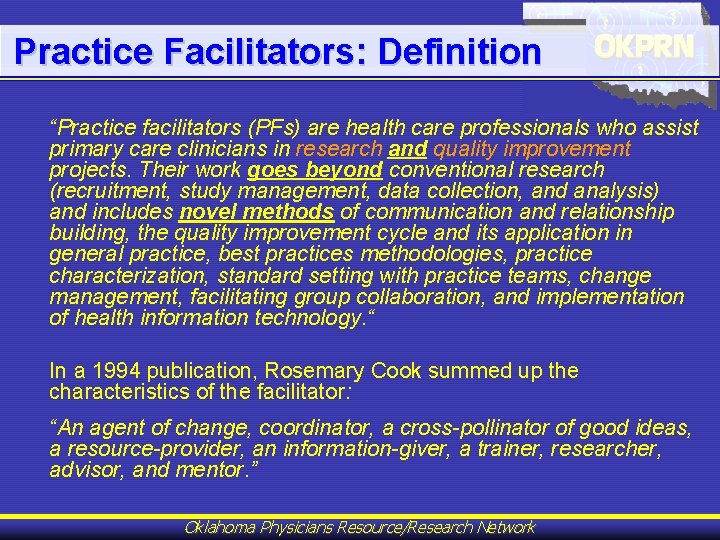
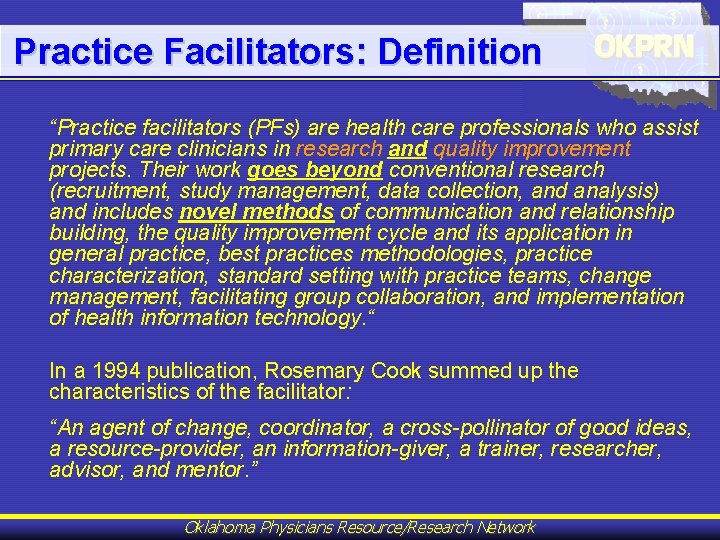
Practice Facilitators: Definition “Practice facilitators (PFs) are health care professionals who assist primary care clinicians in research and quality improvement projects. Their work goes beyond conventional research (recruitment, study management, data collection, and analysis) and includes novel methods of communication and relationship building, the quality improvement cycle and its application in general practice, best practices methodologies, practice characterization, standard setting with practice teams, change management, facilitating group collaboration, and implementation of health information technology. “ In a 1994 publication, Rosemary Cook summed up the characteristics of the facilitator: “An agent of change, coordinator, a cross-pollinator of good ideas, a resource-provider, an information-giver, a trainer, researcher, advisor, and mentor. ” Oklahoma Physicians Resource/Research Network

Practice Facilitators: Origin Of The Concept 1) Oxford Prevention of Heart Attack and Stroke Project (Oxford Project) in England (1982 -84) * 2) Dr. Arnold Elliott, the first peer physician facilitator 3) Earliest reports by Elaine Fullard et al (The Oxford Centre For Primary Care Prevention). PFs were employed “for the purpose of promoting prevention in primary health care” and to “bridge the gap, or establish a new * Fullard E. Extending the roles. . . Practitioner 1987; 231(1436): 1283 -6. channel of communication between the Physicians Resource/Research Network general. Oklahoma practitioner and his coworkers”.

Practice Facilitators: Employment & Financing Employment: • PFs were generally hired by an academic medical center (Netherlands, Canada, and the US) or by the government, Family Health Services Authority (FHSA, England) Financing: • • Funding for individual projects was provided from government sources (England), or academic research grants (Netherlands, Canada, Australia, and the US) sustainability of PF work across projects (longterm financing the PF’s work) has always been Oklahoma Physicians Resource/Research Network a challenge
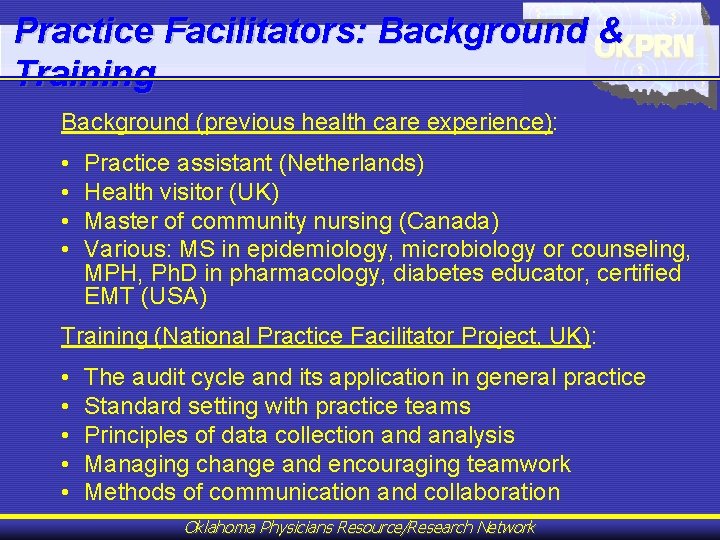
Practice Facilitators: Background & Training Background (previous health care experience): • • Practice assistant (Netherlands) Health visitor (UK) Master of community nursing (Canada) Various: MS in epidemiology, microbiology or counseling, MPH, Ph. D in pharmacology, diabetes educator, certified EMT (USA) Training (National Practice Facilitator Project, UK): • • • The audit cycle and its application in general practice Standard setting with practice teams Principles of data collection and analysis Managing change and encouraging teamwork Methods of communication and collaboration Oklahoma Physicians Resource/Research Network
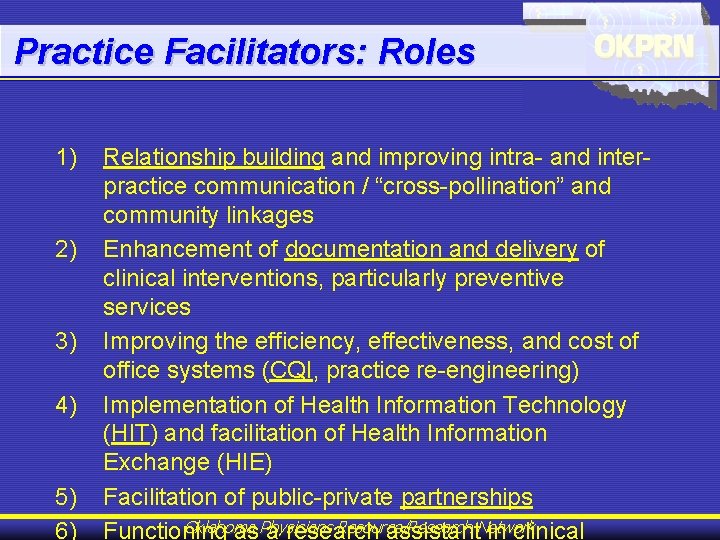
Practice Facilitators: Roles 1) 2) 3) 4) 5) 6) Relationship building and improving intra- and interpractice communication / “cross-pollination” and community linkages Enhancement of documentation and delivery of clinical interventions, particularly preventive services Improving the efficiency, effectiveness, and cost of office systems (CQI, practice re-engineering) Implementation of Health Information Technology (HIT) and facilitation of Health Information Exchange (HIE) Facilitation of public-private partnerships Oklahoma Resource/Research Functioning as. Physicians a research assistant. Network in clinical
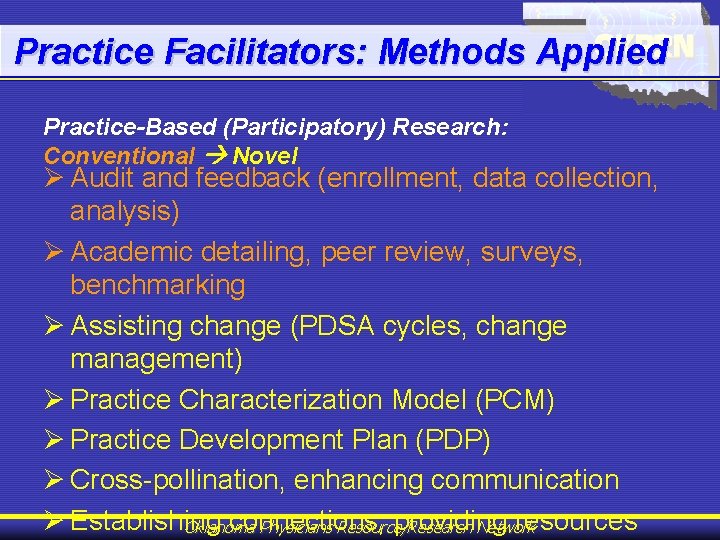
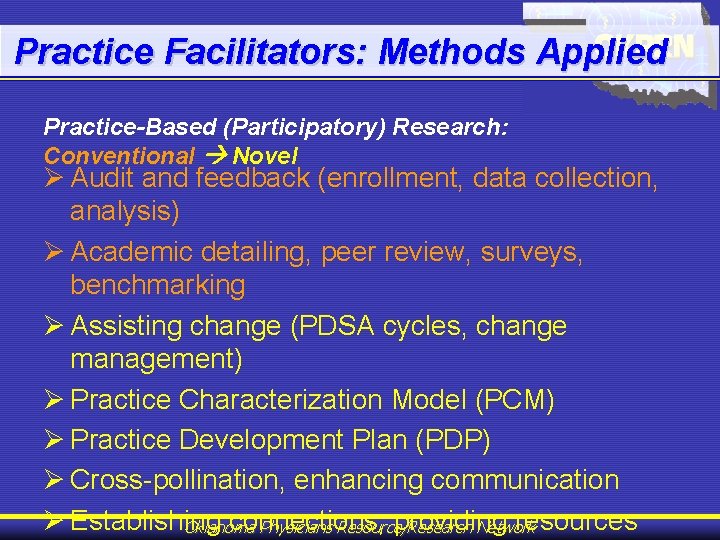
Practice Facilitators: Methods Applied Practice-Based (Participatory) Research: Conventional Novel Ø Audit and feedback (enrollment, data collection, analysis) Ø Academic detailing, peer review, surveys, benchmarking Ø Assisting change (PDSA cycles, change management) Ø Practice Characterization Model (PCM) Ø Practice Development Plan (PDP) Ø Cross-pollination, enhancing communication Ø Establishing connections, providing resources Oklahoma Physicians Resource/Research Network
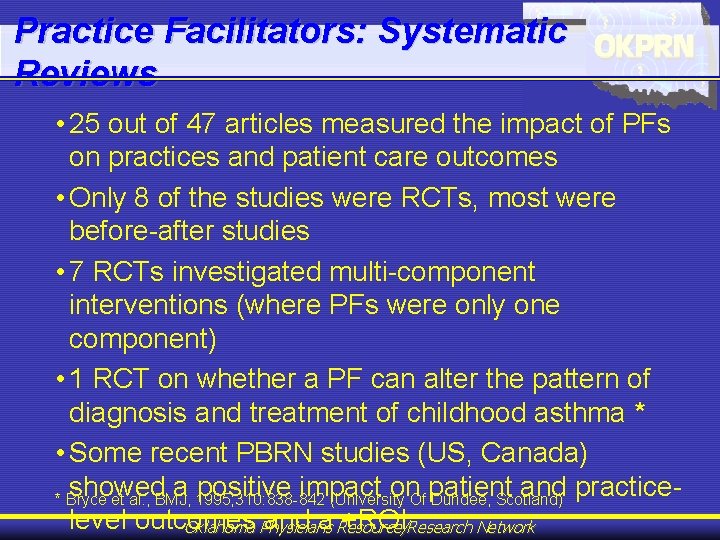
Practice Facilitators: Systematic Reviews • 25 out of 47 articles measured the impact of PFs on practices and patient care outcomes • Only 8 of the studies were RCTs, most were before-after studies • 7 RCTs investigated multi-component interventions (where PFs were only one component) • 1 RCT on whether a PF can alter the pattern of diagnosis and treatment of childhood asthma * • Some recent PBRN studies (US, Canada) showed a positive impact on patient and practice* Bryce et al. , BMJ, 1995; 310: 838 -842 (University Of Dundee, Scotland) level outcomes and a Resource/Research +ROI Oklahoma Physicians Network

PF Training In OKPRN: PEA Syllabus Upon completion of this training module, participants will be able to: • • • • • Comply with all departmental administrative procedures Comply with Human Subjects Protection codes of conduct Comply with HIPPA codes of conduct Understand implement the Practice Facilitator (PEA) concept Describe and apply practice-based research methods and analysis principles Conduct chart audits with 95% accuracy Characterize primary care practices and facilitate change to improve the quality of care Develop Rapid Cycle QI projects Facilitate group discussions and decision-making Adapt projects for implementation in diverse practice settings Properly implement health IT resources in practices relevant to PEA projects Identify learning goals and resources relevant to health IT solutions Access the Clin-IQ database and teach practitioners to use this database List and describe previous PBRN studies Describe and utilize the “Best Practices” study process Develop Project Notebooks to inform and facilitate project implementation Understand help practices implement Preventive Service Guidelines Use the “Electronic Practice Record” including practice objectives and outcome measures Perform tasks as required for specific projects Oklahoma Physicians Resource/Research Network
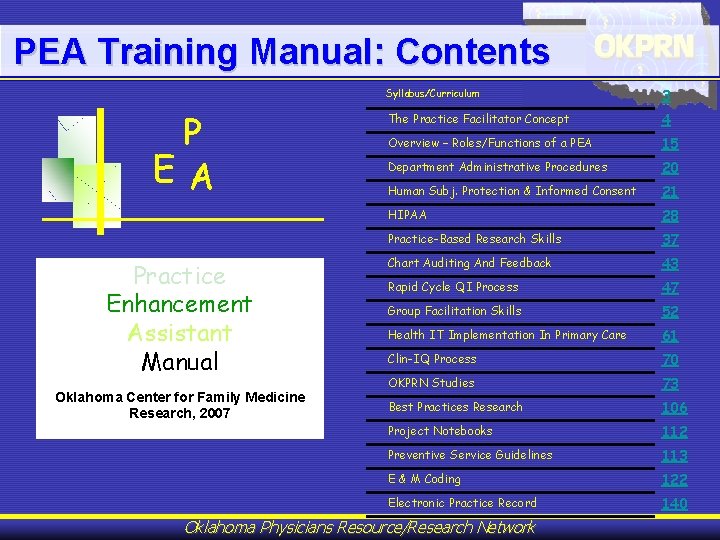
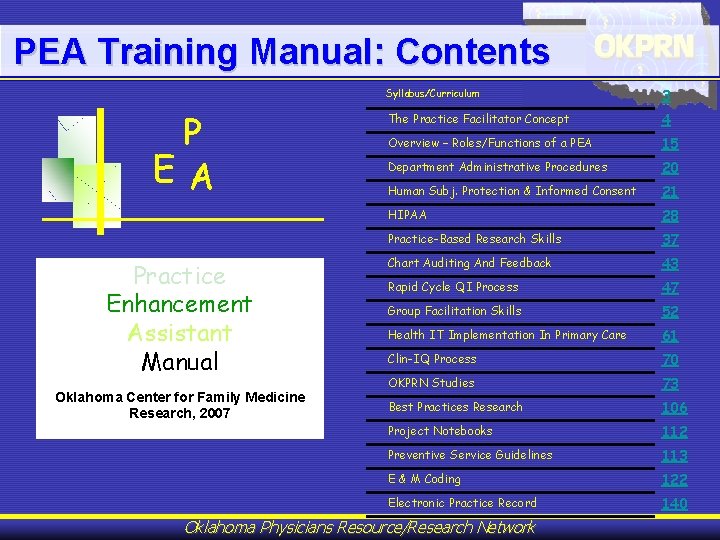
PEA Training Manual: Contents P EA Practice Enhancement Assistant Manual Oklahoma Center for Family Medicine Research, 2007 Syllabus/Curriculum 3 The Practice Facilitator Concept 4 Overview – Roles/Functions of a PEA 15 Department Administrative Procedures 20 Human Subj. Protection & Informed Consent 21 HIPAA 28 Practice-Based Research Skills 37 Chart Auditing And Feedback 43 Rapid Cycle QI Process 47 Group Facilitation Skills 52 Health IT Implementation In Primary Care 61 Clin-IQ Process 70 OKPRN Studies 73 Best Practices Research 106 Project Notebooks 112 Preventive Service Guidelines 113 E & M Coding 122 Electronic Practice Record 140 Oklahoma Physicians Resource/Research Network
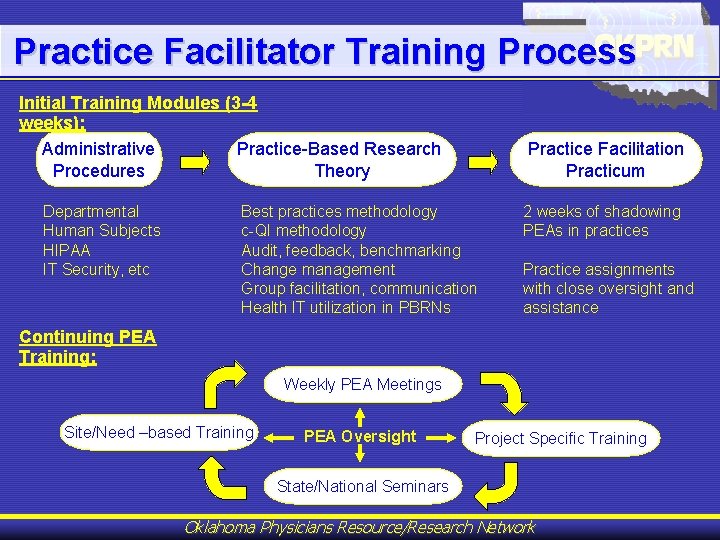
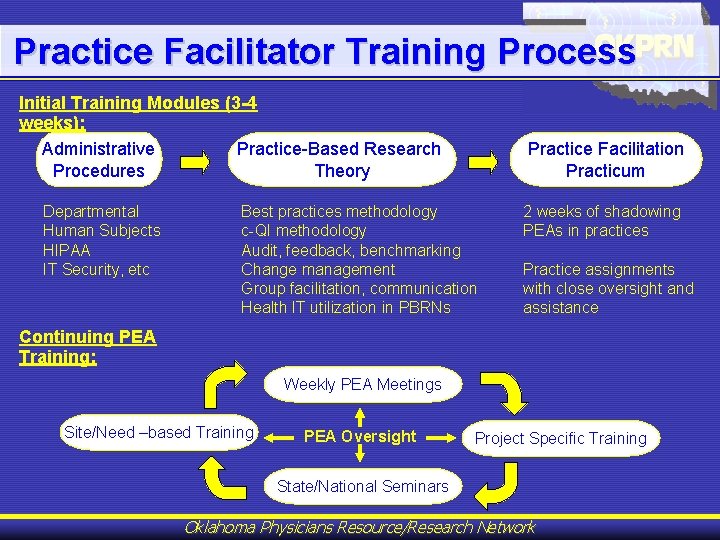
Practice Facilitator Training Process Initial Training Modules (3 -4 weeks): Administrative Practice-Based Research Procedures Theory Departmental Human Subjects HIPAA IT Security, etc Practice Facilitation Practicum Best practices methodology c-QI methodology Audit, feedback, benchmarking Change management Group facilitation, communication Health IT utilization in PBRNs 2 weeks of shadowing PEAs in practices Practice assignments with close oversight and assistance Continuing PEA Training: Weekly PEA Meetings Site/Need –based Training PEA Oversight Project Specific Training State/National Seminars Oklahoma Physicians Resource/Research Network
Practice Facilitator Oversight • PEAs meet with an assigned faculty for 30 minutes individually every week (physically or via Access Grid video-conference). They discuss current projects, practice-specific issues, goal setting and stage of practice improvement (what works what doesn’t), and future interventions. • Then, PEAs meet as a group with faculty and PIs for over 60 minutes. Partner agencies are often represented (e. g. OFMQ, OHCA). They report to each other and share resources / lessons learned. • PEAs write and post their reports and “progress notes” via the EPR and their visit mileage via the Internet in the course of the week. • PEAs are evaluated yearly along with Department staff by the network director. Oklahoma Physicians Resource/Research Network

PEA Project Examples Quality Improvement Activities: Research Activities (Studies): • Pre- and post-intervention audits on immunization and preventive services rates, feedback with benchmarking • Developed flow charts & educational materials for diabetes care • Assisted with the use of the PDA/PC Hardware and Software • Helped to upload patient information from paper charts to electronic medical records • Developed surveys and questionnaires on patient satisfaction • Brainstormed to help solve problems such as how to have high patient compliance in taking their medications • Aided a clinic on how to optimize chart filing • Developed databases to help improve clinic functions, e. g. a database to help keep track of colon screenings • Trained staff on how to do effective cognitive testing • Researched topics of interest, for example, the use of digital transcription and the use of digital cameras • Found resources such as a Spanish medical dictionary or monofilaments • Organized files, such as note cards with colon screening dates • Helped to develop diabetes templates for the clinic’s EHR • Organized quality circles of several practices to improve delivery of behavioral interventions • Collected examples of “best practice” solutions and shared them with the network • Discovered community resources and linked practices to resources to improve patient care • • • • Management of Brown Recluse Spider Bites Study Diabetes Best Practice Study & Diabetes Patient Tracker Palm Sleep Study Primary Care Network Survey (PRINS) Study Prescription Management Project Smoke Free Families / Beginnings Study Preventative Services Reminder System Phase I-IV Studies Laboratory Tests Results Management Study Delivery of Preventive Services in Primary Care Study Improving Colorectal Cancer Screening in Primary Care Study Azithromycin Trial in Community Settings (AZMATICS) Enhance the Rate and Quality of EPSDT Visits Study Creating a New Model of Preventive Service Delivery Study Systematic Delivery of Behavioral Counseling in Primary Care Study Oklahoma Physicians Resource/Research Network
Practice Facilitators: Clinician Testimonials Scott Stewart, MD Shawnee, Oklahoma Michael Pontious, MD Enid, Oklahoma Physicians Resource/Research Network

Practice Facilitators – Network Demos >> Moving Forward Oklahoma Physicians Resource/Research Network