PPV Positive Pressure Ventilation by dr behzad barekatain
PPV Positive Pressure Ventilation by: dr. behzad barekatain Assistant professor of pediatrics neonatalogist Isfahan university of medical science
PPV via 1. ambobag 2. ventilator(mechanical ventilation) Definition & Importance most common approach for treatment of res. failure in both term &pre-term neonate

Classification Volume-controlled ventilator Pressure-preset ventilator VOLUME vs PRESSURE VENTILATOR Pressure ventilator is preferable because of: 1. greater simplicity of design & compact design 2. lower cost 3. simple to operate 4. same pressure in each breathe 5. type of pul. dis in neonate & better responsive to pressure ven.
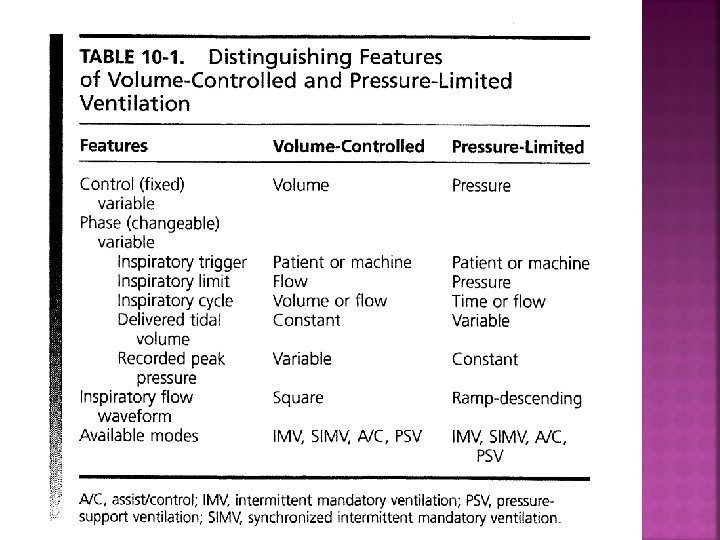
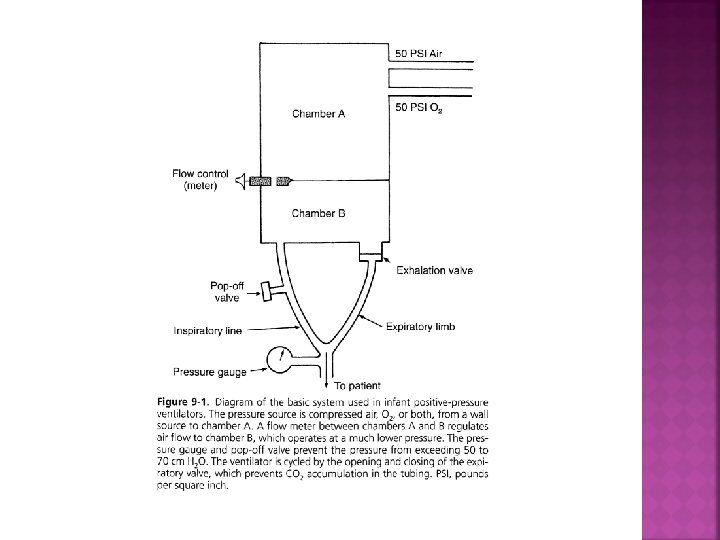
CONTROL (fixed)VARIABLE Volume: in volume-controlled ventilator Pressure: in pressure-preset ventilator PHASE (changeable)VARIABLE Triggering* ﺷﺮﻭﻉ ﺩﻡ ﺭﺍ کﻨﺘﺮﻝ ﻣیکﻨﺪ : ﺍﻏﺎﺯگﺮ . time triggering>>>>>in IMV mode (ALS, IVH). patient triggering>>>>in SIMV OR A/C mode(sensor) Limitting* ﻭﻗﺘی : ﻣﺤﺪﻭﺩ کﻨﻨﺪﻩ ﻓﺎکﺘﻮﺭﻫﺎی ﺗﻨﻔﺴی یﺎ ﺣﺪﺍکﺜﺮ ﻣﺠﺎﺯ ﻭﻧﺘیﻼﺗﻮﺭ ﺑﻪ ﺣﺪﺍکﺜﺮ ﻣﺠﺎﺯ آﻦ ﻣﺘﻐییﺮ ﺑﺮﺳﺪ ﺩﺭیچﻪ ﻫﺎی ﺗﺨﻠیﻪ ﺭﺍ ﺑﺎﺯ . ﻣیکﻨﺪ Cycling* پﺎیﺎﻥ ﺩﻡ ﺭﺍ کﻨﺘﺮﻝ ﻣیکﻨﺪ . Volume-cycled. Time-cycled

IMPORTANT ISSUSES IN SUCCESSFULLY RES. CARE 1. operation by device(hardware)>>>5% 2. principles of physiology(software)>>>95% 3. other pripheral issues. infection control. nutritional support. fluid & electrolyte management. comfort & pain relief. assessment of circulation. tempreture
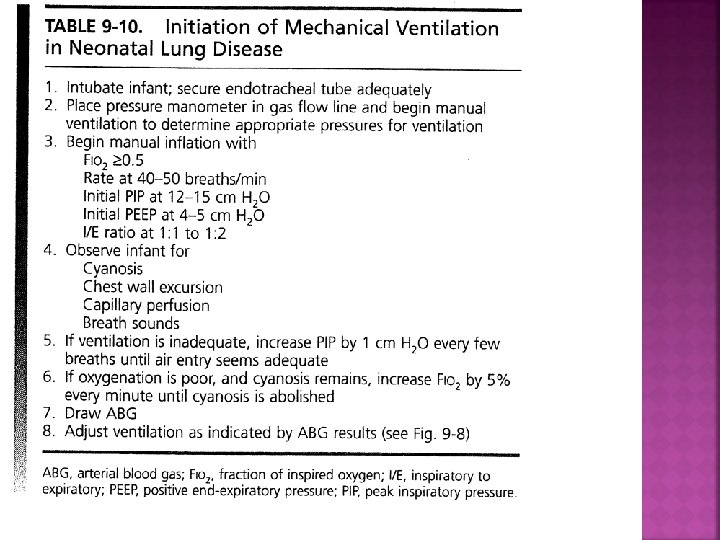
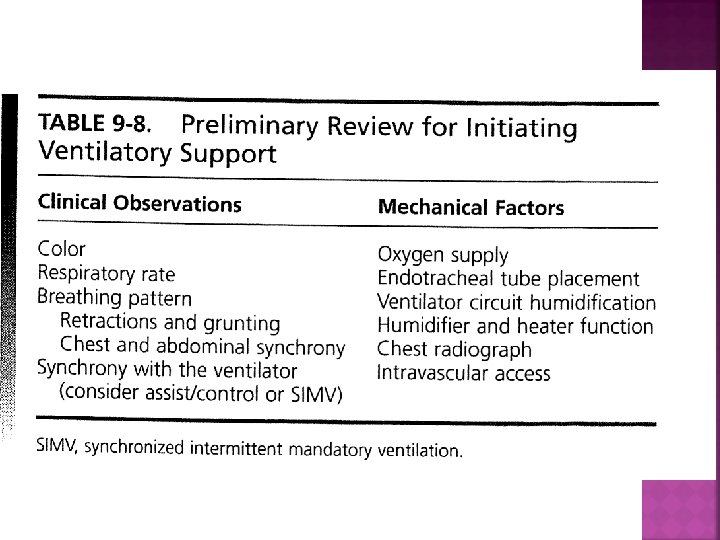
Procedure for initiating M. V 1. electrical connection 2. O 2 & air gas source to provide adequate prssure(50 psi) 3. all connection must fit securely 4. tube & circuit shoud be specific for ventilator 5. humidification system Low>>>necrotizing tracheobronchitis High>>>overhydration & increase resistant 6. temperature 35 to 36 (+, - 2) Low>>>bronchospasm High>>>airway inflamation
VENTILATOR CONTROLS . fio 2. pip. peep. rate. flow. Ti , Te, I/E ratio. assist sensitivity. termination sensitivity. alarm setting. graphic monitoring. map. other(psv, manual breath, hf mode, demand flow)_

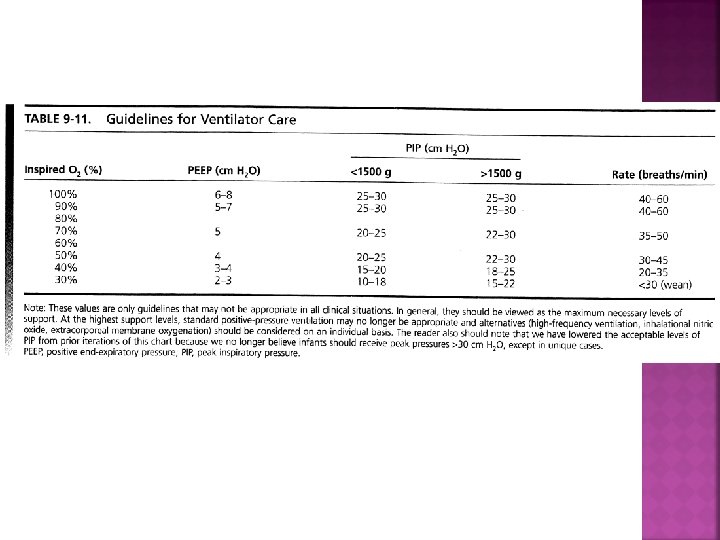
FIO 2 is the Most commonly used DRUGin nicu Inadequate O 2 >>>hypoxemia & neurologic injury Exessive VARIATION in O 2 adm>>>ROP High level of O 2>>>BPD Depended on disease(eg; MAS or PH) or associated condition(eg; duct depended heart disease) SO Accurate measurment of O 2 (via puls oximetry or ABG is mandatory in NICU care

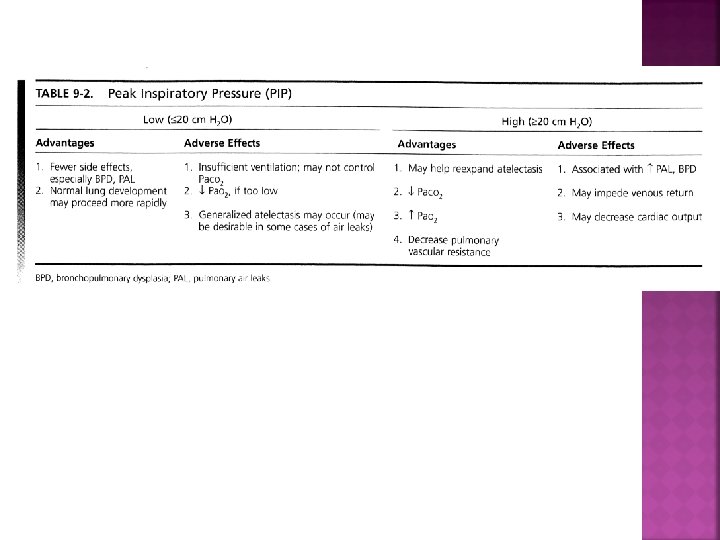
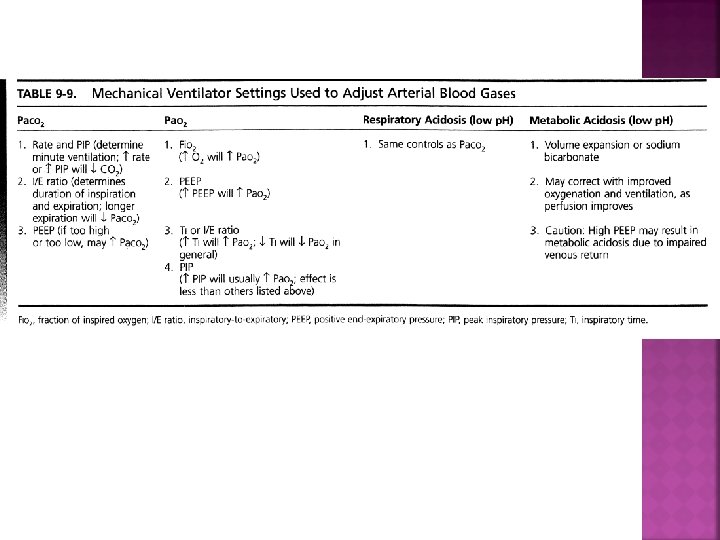
PEAK INSPIRATORY PRESSURE (PIP) Major factor in determining tidal volume(PIP_EDP) in pressure preset vent Starting level depend on: GA, W, type & severity of disease, lung compl, Resistance, time constant, mode of ventilator, . . . Check before & after attachment to patient(2 -3 cmh 2 o) Appropriate PIP can be judged on examination(chest expantion) and ABG analysis The lowest PIP that adequately ventilated neonate is optimal
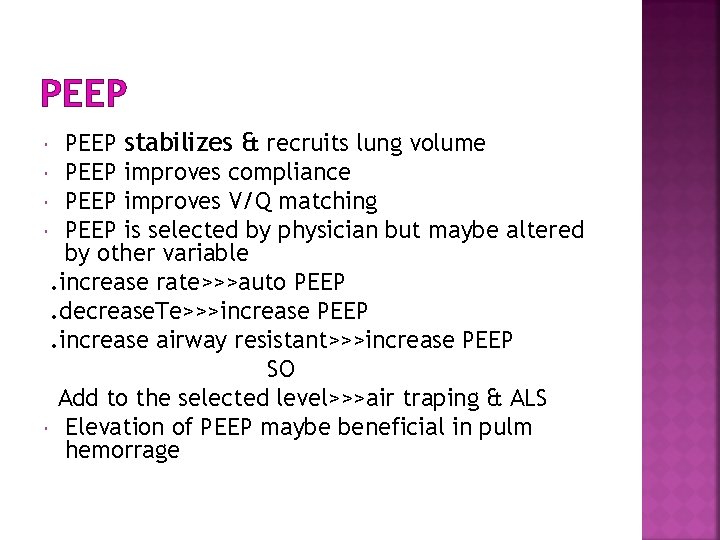
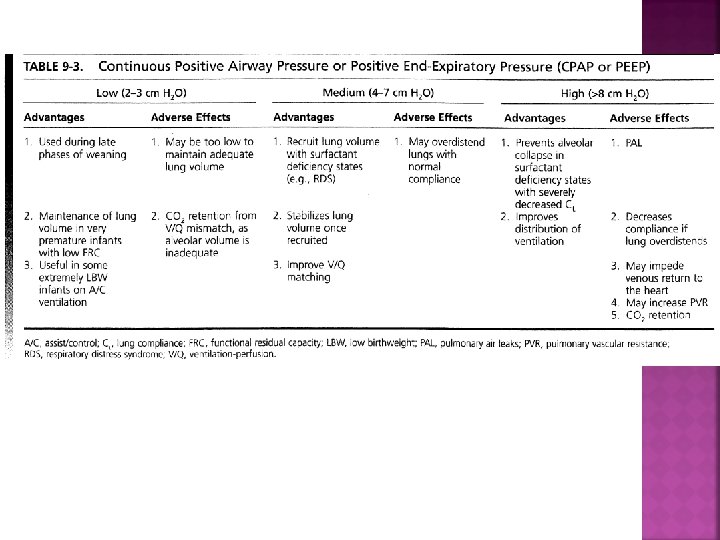
PEEP stabilizes & recruits lung volume PEEP improves compliance PEEP improves V/Q matching PEEP is selected by physician but maybe altered by other variable. increase rate>>>auto PEEP. decrease. Te>>>increase PEEP. increase airway resistant>>>increase PEEP SO Add to the selected level>>>air traping & ALS Elevation of PEEP maybe beneficial in pulm hemorrage
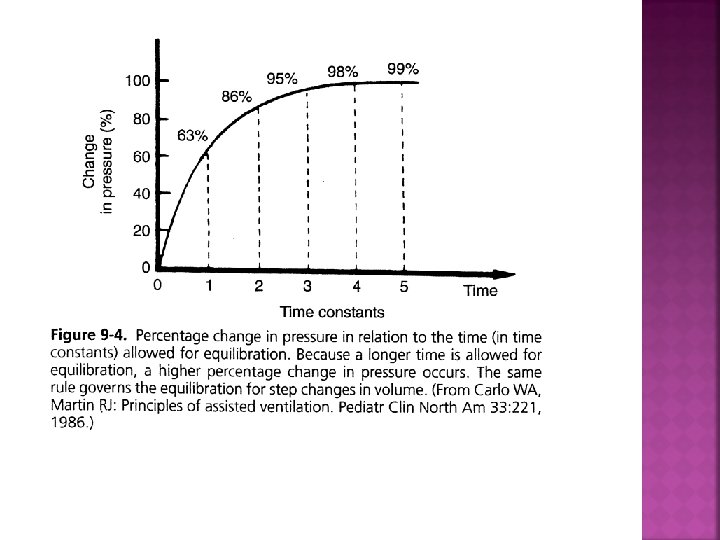
TIME CONSTANT: RESISTANT. COMPLIANCE IN RDS: >>>compliance decrease>>>T. C decrease IN MAS: >>>resistant increase>>>T. C increase

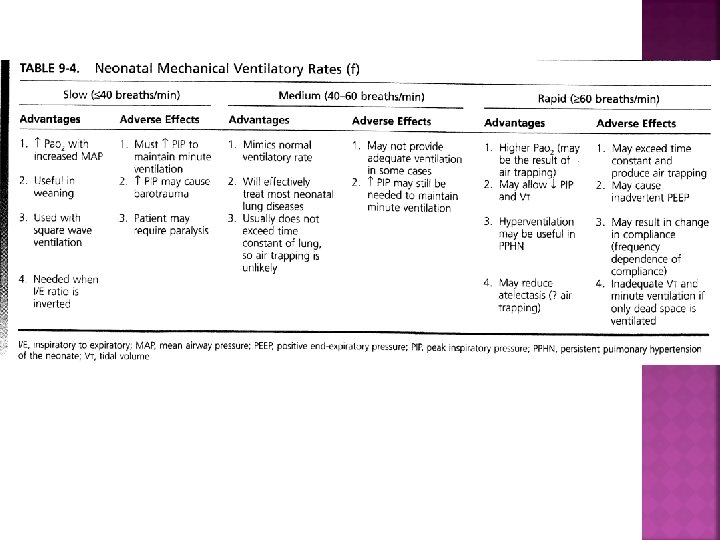
RATE (F) Minute ventilation=rate. Vt>>>↑ Rate >>> ↑ alveolar ventilation >>> ↓PCO 2 Controlled by directly selecting in timecycled ventilator ↑ ↑ rate short TE incomplete expiration gas trapping decresed compliance, intrinsic PEEP ↓VT ↑PCO 2 Optimal rate: 40 -60 with Ti: 0/3_0/4 sec because of low TC in most pul. disease such as RDS High rate in PH & low rate in weaning

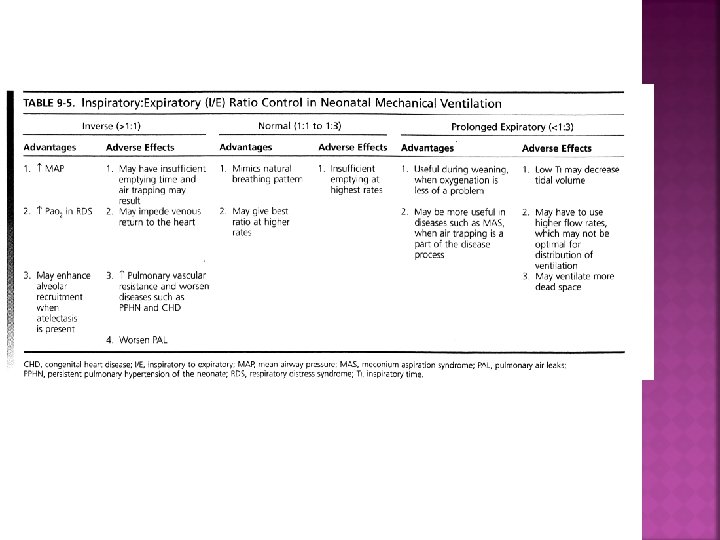
I/E RATIO NORMAL: 1/3 – 1/1 The major effect on oxygenation ↑ ratio or even reversed I/E (Ti longer than Te) ↑ PO 2 but its effect is less than change in PIP and PEEP. CO 2 elimination is usually not altered by changes in I/E ratio. Reversed I/E ratio may lead to increase in the incidence of pneumothorax, co 2 retention, decrease co, increase PVR, Reversed I/E ratio maybe used in CLD because of long TC. I/E<1/3 maybe used in weaning or MAS
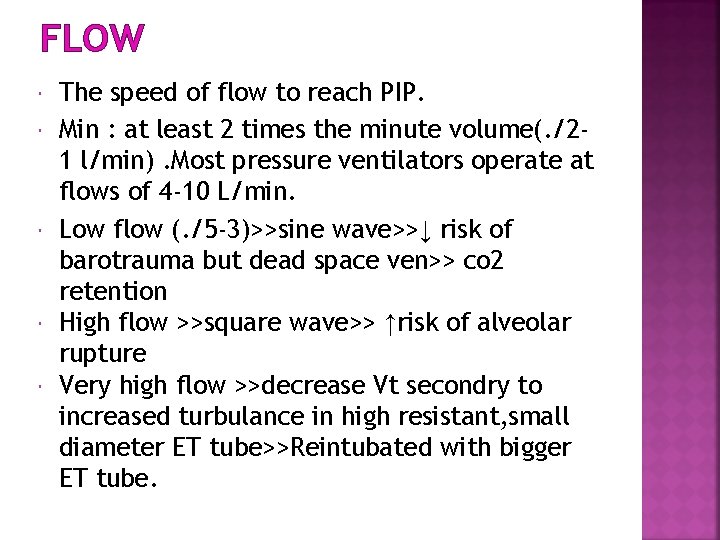
FLOW The speed of flow to reach PIP. Min : at least 2 times the minute volume(. /21 l/min). Most pressure ventilators operate at flows of 4 -10 L/min. Low flow (. /5 -3)>>sine wave>>↓ risk of barotrauma but dead space ven>> co 2 retention High flow >>square wave>> ↑risk of alveolar rupture Very high flow >>decrease Vt secondry to increased turbulance in high resistant, small diameter ET tube>>Reintubated with bigger ET tube.


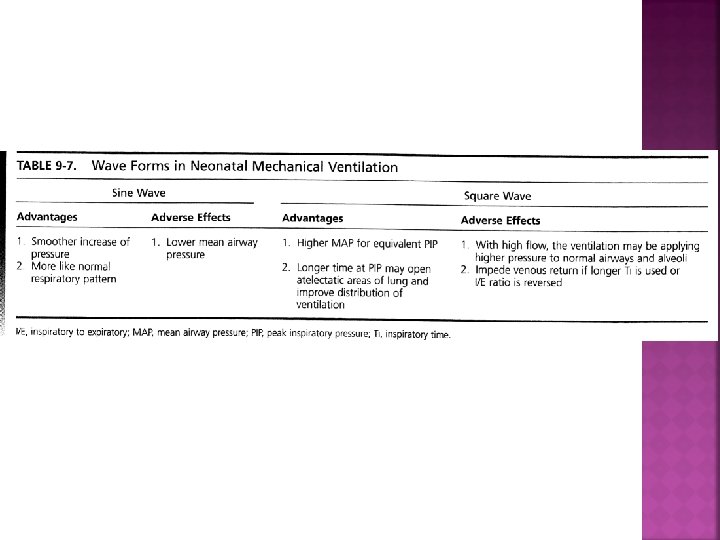
Wave Forms Sine wave: more closely to normal spontaneous breathing Square wave: provide a higher map than do sine waveform if identical PIP used because the PIP is reached more rapidly with square waves.


MAP: (PIP_PEEP). (Ti/Ti+Te)+PEEP

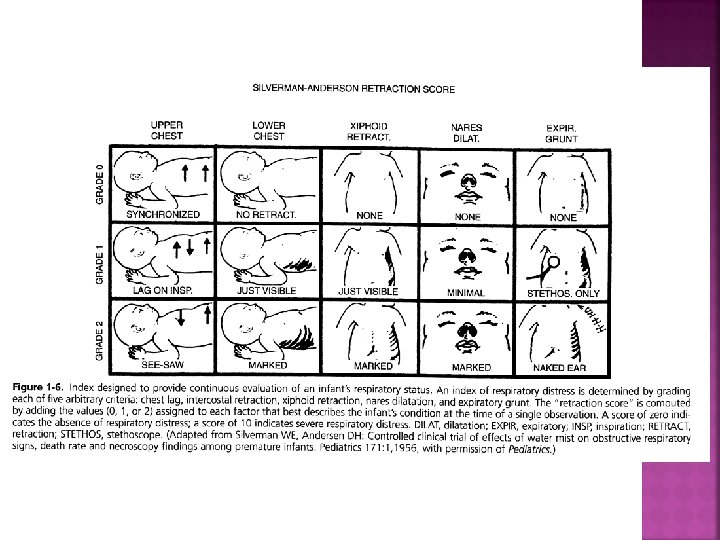
Definition of Res. failure Two or more criteria from the following clinical & laboratory categories: . clinical: 1. Retraction(intercostal, supraclavi, suprasternal) 2. Grunting 3. rate>60 4. Central cyanosis 5. Intractable Apnea 6. Decrease activity & movment. laboratory: 1. Paco 2>60 mmhg 2. Po 2<50 mmhg or O 2 sat<80%(Fio 2=1. 0) 3. PH<7. 25

An aggressive (but gentle)early approach often is preferable in neonates, regardless of their disease. RDS SCORE: 1. rate(<60: 0, 60 -80: 1, >80: 2) 2. cyanosis(no in room air: 0, no under hood: 1, yes under hood: 2) 3. intercostal retraction(no: 0, mod: 1, severe: 2) 4. air exchange(good: 0, decreased: 1, no: 2) 5. grunting(no: 0, with stethos: 1, without stethos: 2) <3: O 2+follow up 4 -6: NICU care + supportive management 6 -8: cpap >8: intubation+MV
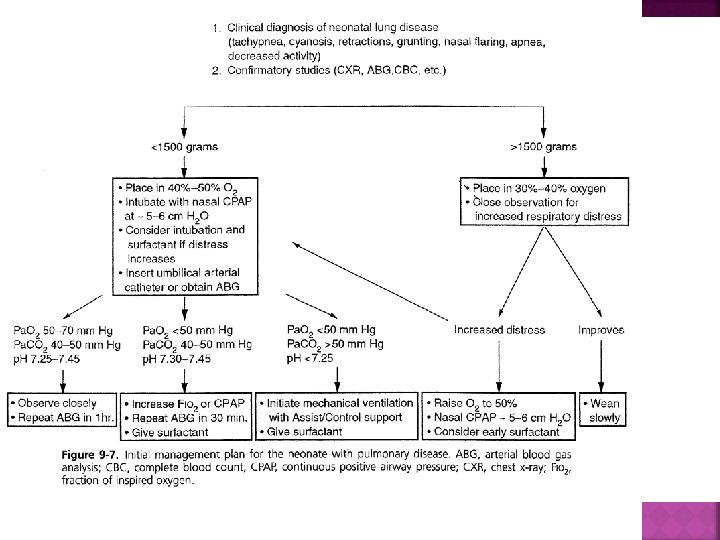
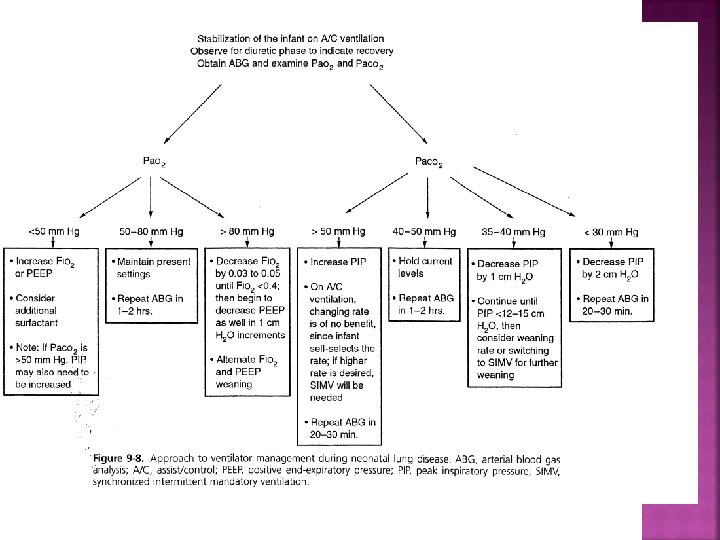
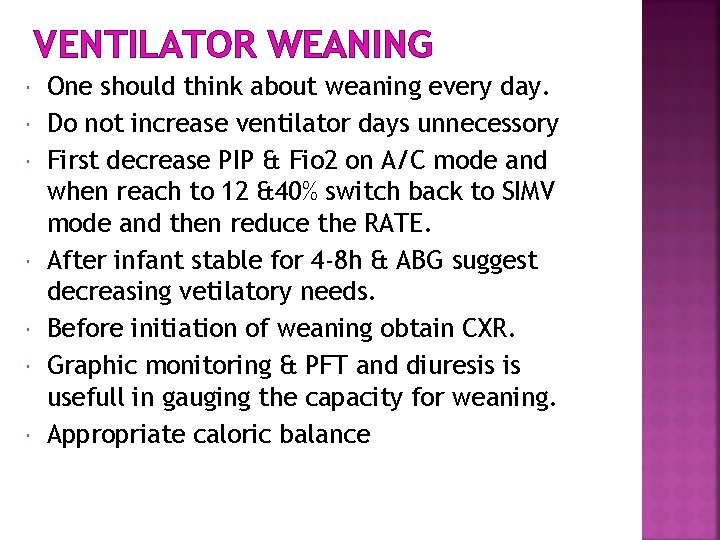
VENTILATOR WEANING One should think about weaning every day. Do not increase ventilator days unnecessory First decrease PIP & Fio 2 on A/C mode and when reach to 12 &40% switch back to SIMV mode and then reduce the RATE. After infant stable for 4 -8 h & ABG suggest decreasing vetilatory needs. Before initiation of weaning obtain CXR. Graphic monitoring & PFT and diuresis is usefull in gauging the capacity for weaning. Appropriate caloric balance
If at any point : Fi. O 2 increased to >60%, ↑spontaneous breathing or distressed with accessory muscle use, agitation or lethargic, hypercarbia weaning should be paused and the support level increased.
EXTUBATION Fio 2<40%, RATE: 10, PIP: 10 -12 NPO for 4 hrs before extubation. CXR before & 2 and 24 h after ext. The procedure is carried out by 2 nurses. Give prolonged sigh of 15 -20 cmh 2 Owhile the ET tube is extracted. Aspiration of NG tube before extubation ETT & oropharyngeal suctioning to remove secretion and good gag reflex Prepare emergency equipments (O 2, suction, airway, humidifier, emergency intubation equipments) NPO for 4 -6 h after extubation OR until the infant can make an audible cry.
In <1500 gr use CPAP after extubation for 2 -3 day. in >1500 gr placed under oxyhood or nasal o 2 with an O 2 5% greater. Watch for several minute after ext.
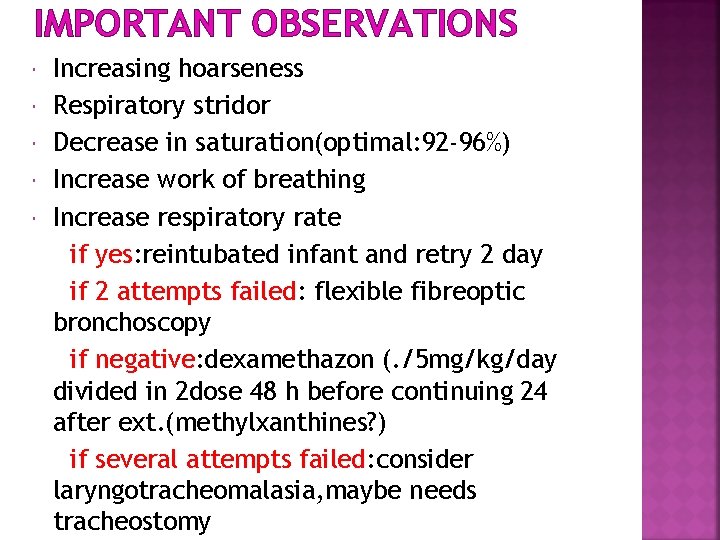
IMPORTANT OBSERVATIONS Increasing hoarseness Respiratory stridor Decrease in saturation(optimal: 92 -96%) Increase work of breathing Increase respiratory rate if yes: reintubated infant and retry 2 day if 2 attempts failed: flexible fibreoptic bronchoscopy if negative: dexamethazon (. /5 mg/kg/day divided in 2 dose 48 h before continuing 24 after ext. (methylxanthines? ) if several attempts failed: consider laryngotracheomalasia, maybe needs tracheostomy
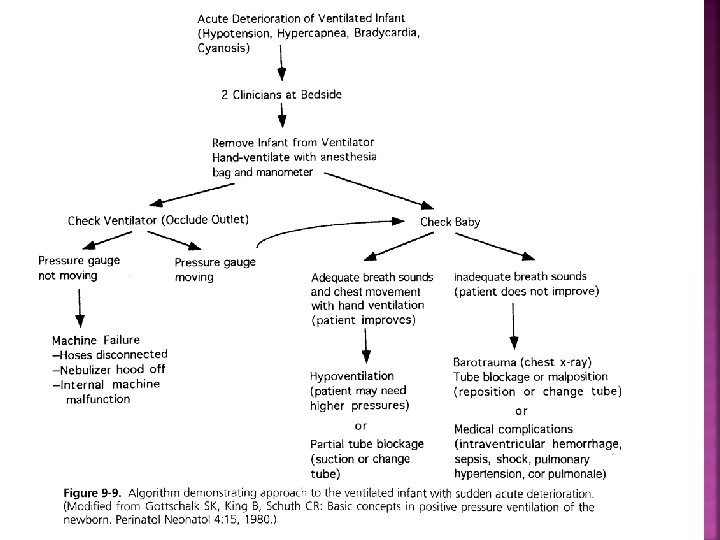
IMMEDIATE MEASURES DOPE Ø D : Displacement Ø O : Obstruction Ø P : Pneumothorax Ø E : Equipment failure


THANKS
- Slides: 47