PPI prophylaxis for GI bleeding in ICU Summary
PPI prophylaxis for GI bleeding in ICU
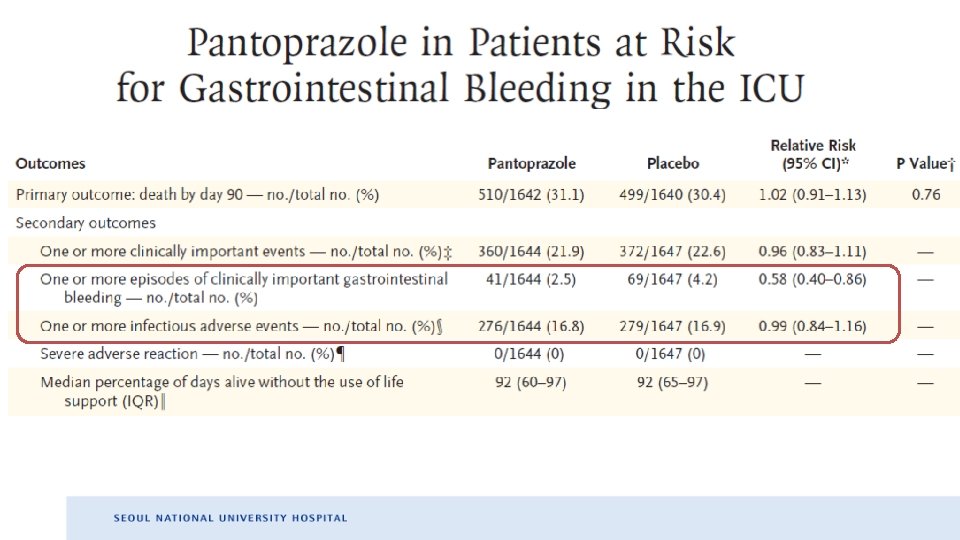
Summary: NEJM • Participants with at least one risk factor for CIGIB – Stayed in the ICU for a median of 6 days – Received trial agent for a median of 4 days • No significant differences in 90 -day mortality and clinically important adverse event • Low incidence rate of CIGIB in PPI group (2. 5% vs. 4. 2%)
Critical appraisal: NEJM • Short duration of PPI Ø Can we properly assess the impact of PPI on these endpoints? • More patients with SAPS (Simplified acute physiology score) ≥ 53 included in the placebo group Ø favorable impact on PPI group? • No significant difference in clinical important event between two group Ø Interpretation: 1) Do we really have to use PPI? Or 2) What is the big deal in using PPI?
Summary: CHEST • Patients with at least one risk factors – LOS < 72 h or GI bleeding within the first 72 h excluded • Less common CIGIB rates (0. 6%) than previous reports • Various analyses in various conditions to overcome limitation of retrospective study Ø PPIs associated with higher risk of CIGIB in nearly all scenarios
Critical appraisal: CHEST • Not well-balanced baseline characteristics – Limitation of large-population study? – Skewed tendency of risk factor distribution toward PPI group • Patients with PPI might have more risk factor than H 2 RA group • Better resuscitated patients à less severe mucosal damage à greater capacity to respond to H 2 RA?
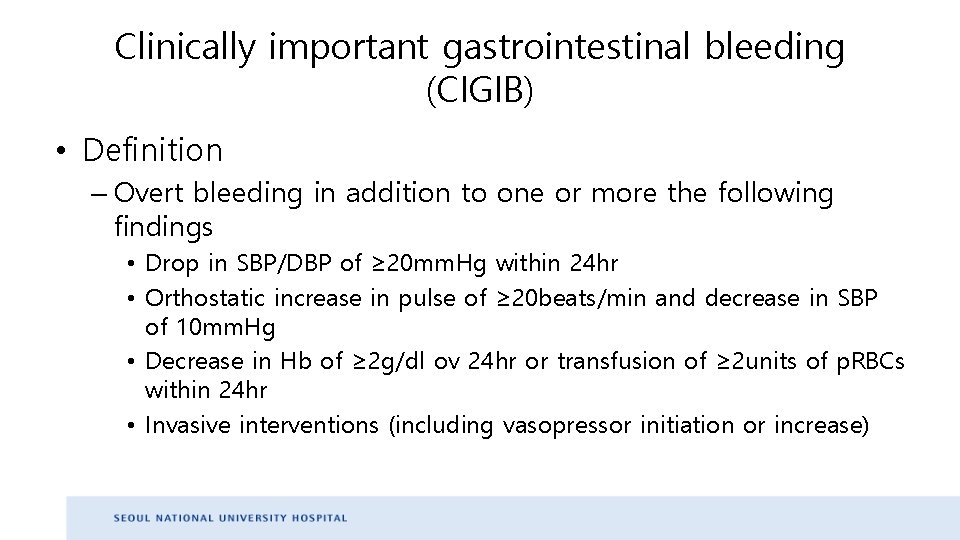
Clinically important gastrointestinal bleeding (CIGIB) • Definition – Overt bleeding in addition to one or more the following findings • Drop in SBP/DBP of ≥ 20 mm. Hg within 24 hr • Orthostatic increase in pulse of ≥ 20 beats/min and decrease in SBP of 10 mm. Hg • Decrease in Hb of ≥ 2 g/dl ov 24 hr or transfusion of ≥ 2 units of p. RBCs within 24 hr • Invasive interventions (including vasopressor initiation or increase)
Clinically important gastrointestinal bleeding (CIGIB) • Incidence – 3% among critically ill patients – 0. 2% among patients in medical/surgical units • Prophylaxis – 70% in critically ill pts. – 60% in medical/surgical units
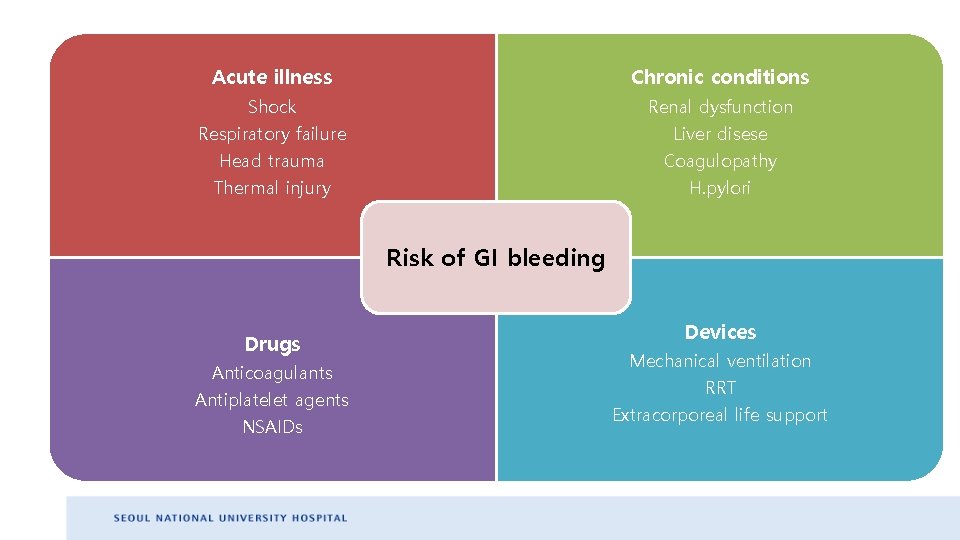
Acute illness Chronic conditions Shock Respiratory failure Renal dysfunction Liver disese Head trauma Thermal injury Coagulopathy H. pylori Risk of GI bleeding Drugs Anticoagulants Antiplatelet agents NSAIDs Devices Mechanical ventilation RRT Extracorporeal life support
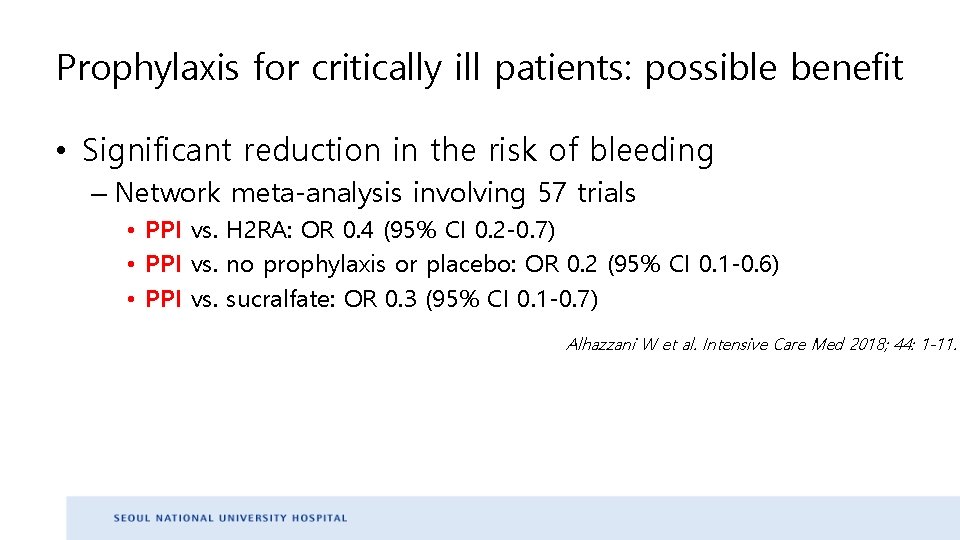
Prophylaxis for critically ill patients: possible benefit • Significant reduction in the risk of bleeding – Network meta-analysis involving 57 trials • PPI vs. H 2 RA: OR 0. 4 (95% CI 0. 2 -0. 7) • PPI vs. no prophylaxis or placebo: OR 0. 2 (95% CI 0. 1 -0. 6) • PPI vs. sucralfate: OR 0. 3 (95% CI 0. 1 -0. 7) Alhazzani W et al. Intensive Care Med 2018; 44: 1 -11.
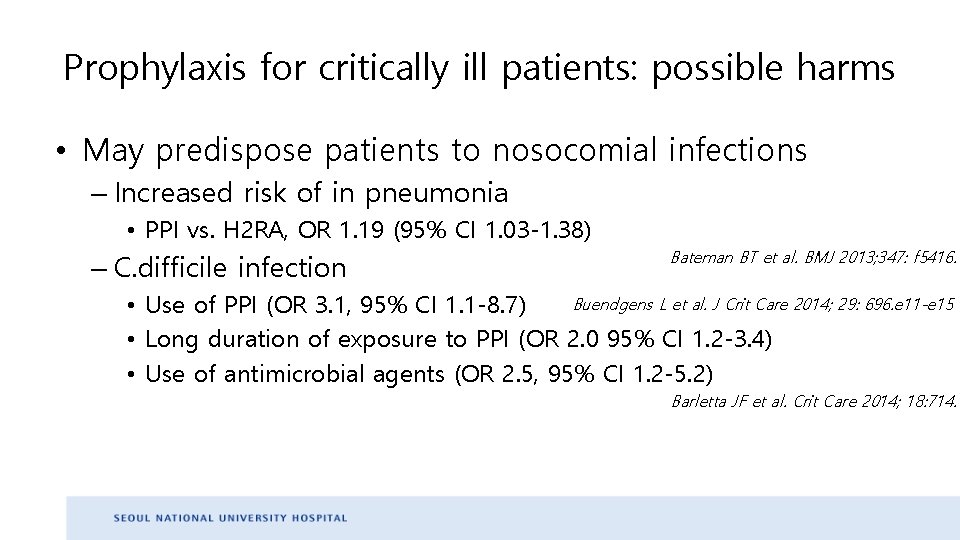
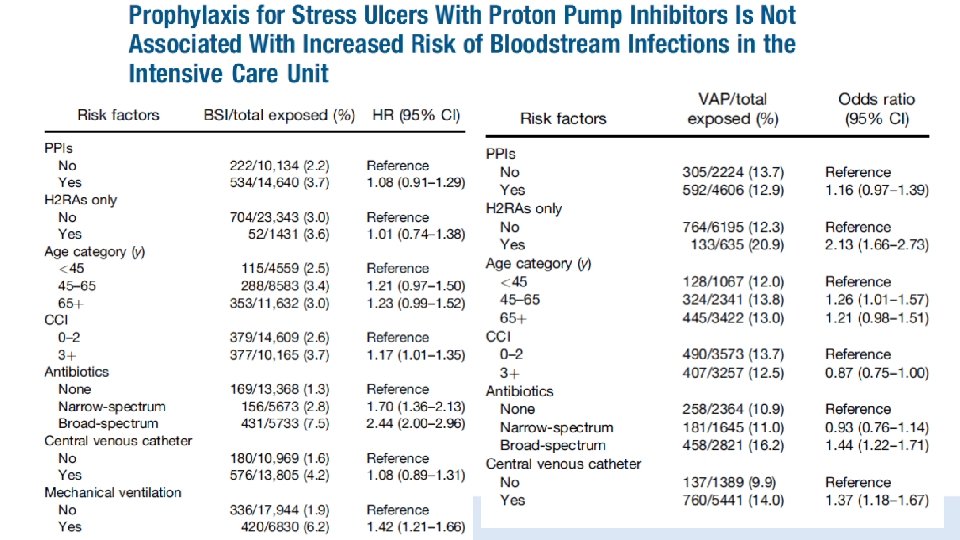
Prophylaxis for critically ill patients: possible harms • May predispose patients to nosocomial infections – Increased risk of in pneumonia • PPI vs. H 2 RA, OR 1. 19 (95% CI 1. 03 -1. 38) – C. difficile infection Bateman BT et al. BMJ 2013; 347: f 5416. Buendgens L et al. J Crit Care 2014; 29: 696. e 11 -e 15 • Use of PPI (OR 3. 1, 95% CI 1. 1 -8. 7) • Long duration of exposure to PPI (OR 2. 0 95% CI 1. 2 -3. 4) • Use of antimicrobial agents (OR 2. 5, 95% CI 1. 2 -5. 2) Barletta JF et al. Crit Care 2014; 18: 714.
Prophylaxis for critically ill patients Cook D et al. N Engl J Med 2018; 378: 2506 -16.
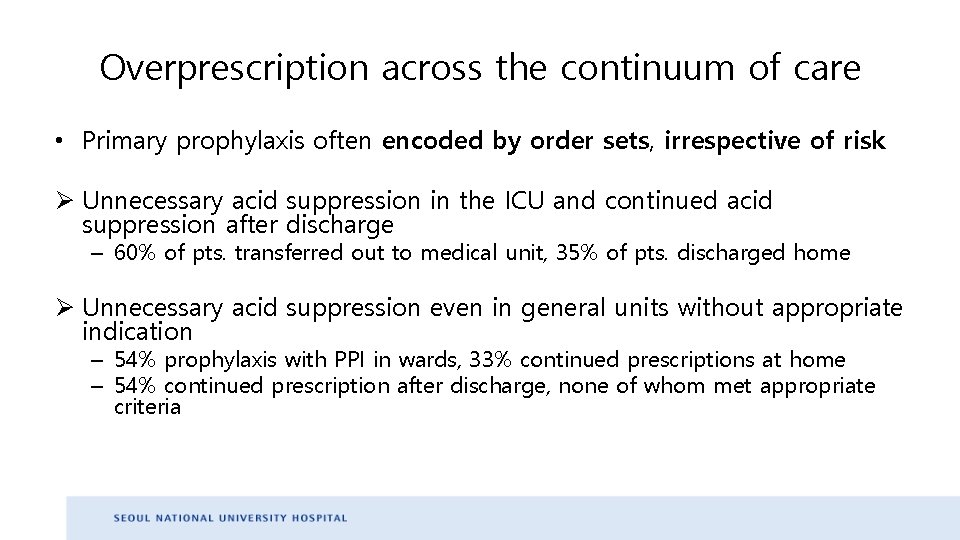
Overprescription across the continuum of care • Primary prophylaxis often encoded by order sets, irrespective of risk Ø Unnecessary acid suppression in the ICU and continued acid suppression after discharge – 60% of pts. transferred out to medical unit, 35% of pts. discharged home Ø Unnecessary acid suppression even in general units without appropriate indication – 54% prophylaxis with PPI in wards, 33% continued prescriptions at home – 54% continued prescription after discharge, none of whom met appropriate criteria
Concern: Long-term complication of PPI
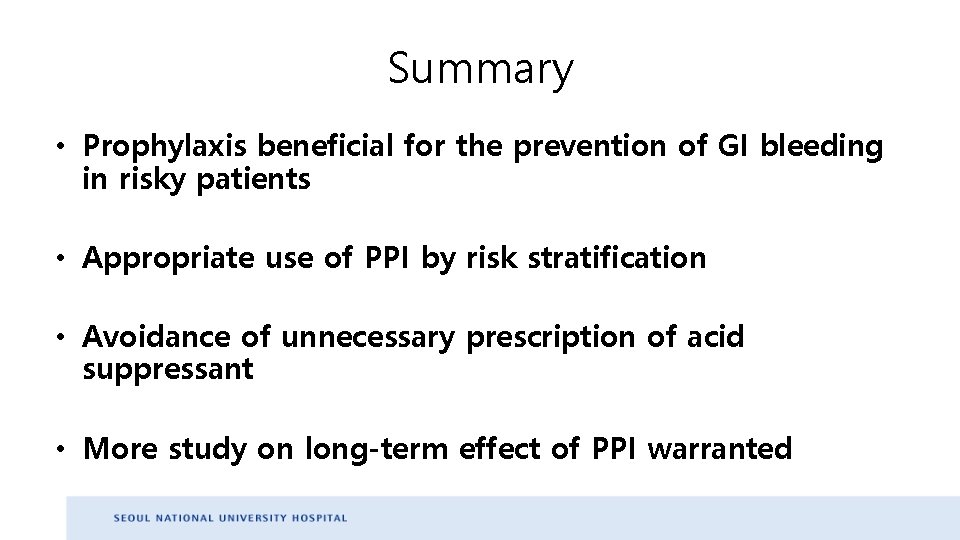
Summary • Prophylaxis beneficial for the prevention of GI bleeding in risky patients • Appropriate use of PPI by risk stratification • Avoidance of unnecessary prescription of acid suppressant • More study on long-term effect of PPI warranted
- Slides: 16