PostPCI DAPT Duration Impact of Clinical Angiographic and
- Slides: 29
Post-PCI DAPT Duration Impact of Clinical, Angiographic and Procedural Factors Gregg W. Stone, MD Columbia University Medical Center New. York-Presbyterian Hospital Cardiovascular Research Foundation
Disclosures • Gregg W. Stone - none
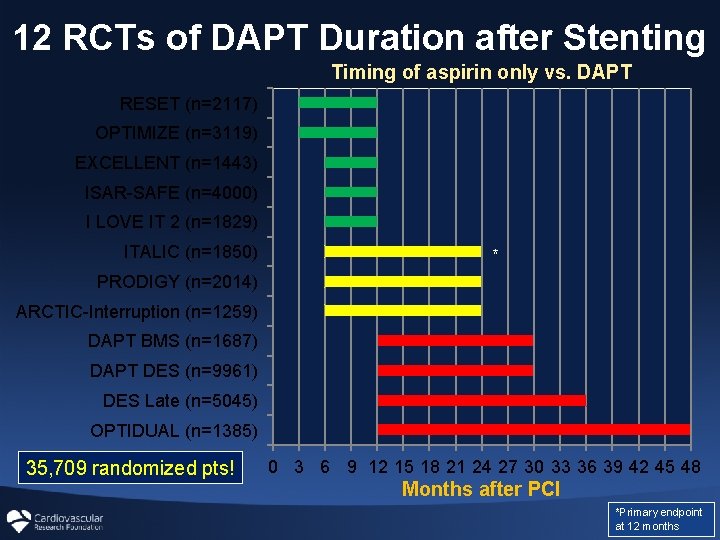
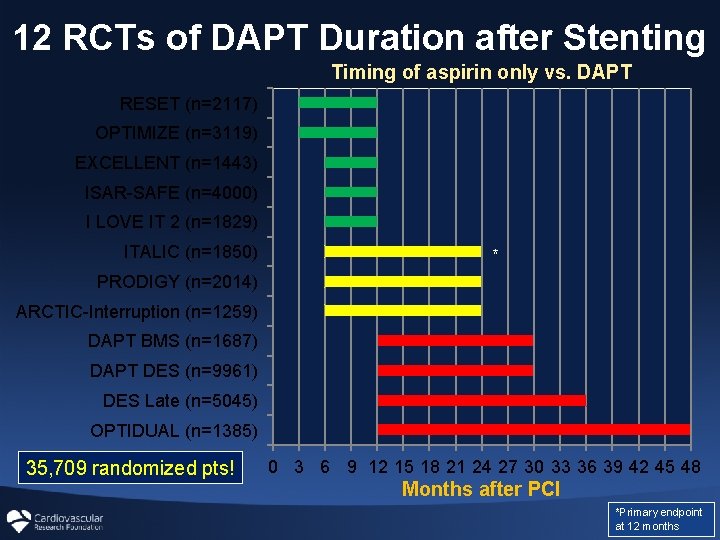
12 RCTs of DAPT Duration after Stenting Timing of aspirin only vs. DAPT RESET (n=2117) OPTIMIZE (n=3119) EXCELLENT (n=1443) ISAR-SAFE (n=4000) I LOVE IT 2 (n=1829) ITALIC (n=1850) * PRODIGY (n=2014) ARCTIC-Interruption (n=1259) DAPT BMS (n=1687) DAPT DES (n=9961) DES Late (n=5045) OPTIDUAL (n=1385) 35, 709 randomized pts! 0 3 6 9 12 15 18 21 24 27 30 33 36 39 42 45 48 Months after PCI *Primary endpoint at 12 months
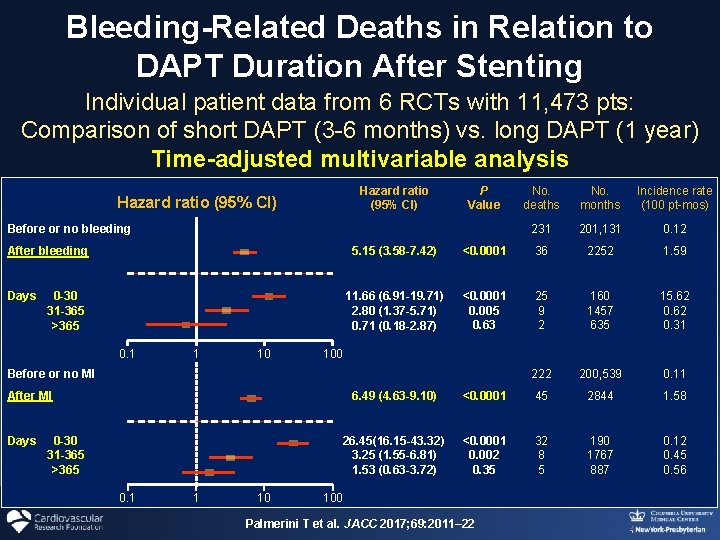
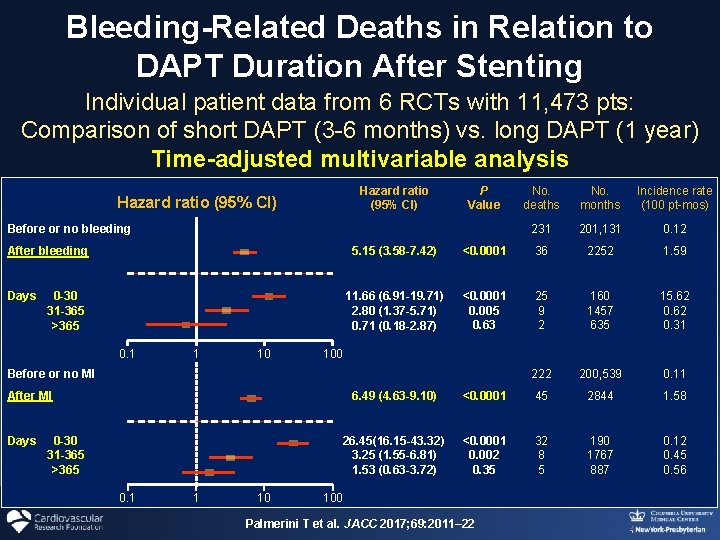
Bleeding-Related Deaths in Relation to DAPT Duration After Stenting Individual patient data from 6 RCTs with 11, 473 pts: Comparison of short DAPT (3 -6 months) vs. long DAPT (1 year) Time-adjusted multivariable analysis Hazard ratio (95% CI) P Value Before or no bleeding After bleeding Days 0 -30 31 -365 >365 0. 1 1 10 Incidence rate (100 pt-mos) 231 201, 131 0. 12 <0. 0001 36 2252 1. 59 11. 66 (6. 91 -19. 71) 2. 80 (1. 37 -5. 71) 0. 71 (0. 18 -2. 87) <0. 0001 0. 005 0. 63 25 9 2 160 1457 635 15. 62 0. 31 222 200, 539 0. 11 100 After MI 0 -30 31 -365 >365 No. months 5. 15 (3. 58 -7. 42) Before or no MI Days No. deaths 6. 49 (4. 63 -9. 10) <0. 0001 45 2844 1. 58 26. 45(16. 15 -43. 32) 3. 25 (1. 55 -6. 81) 1. 53 (0. 63 -3. 72) <0. 0001 0. 002 0. 35 32 8 5 190 1767 887 0. 12 0. 45 0. 56 100 Palmerini T et al. JACC 2017; 69: 2011– 22
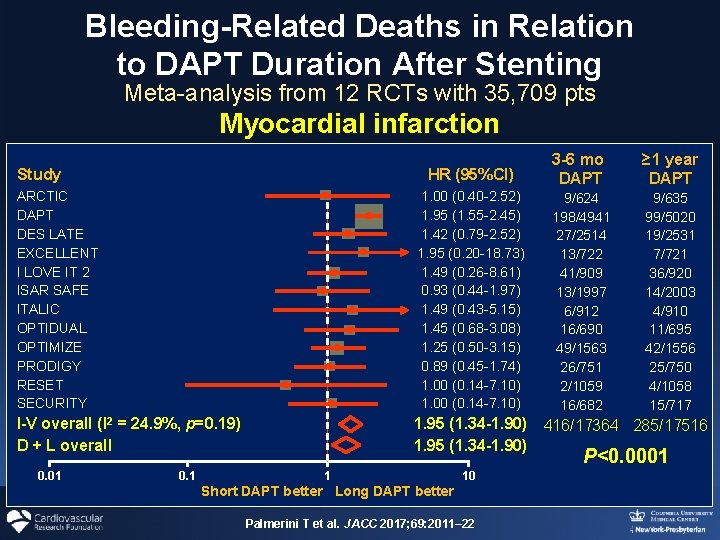
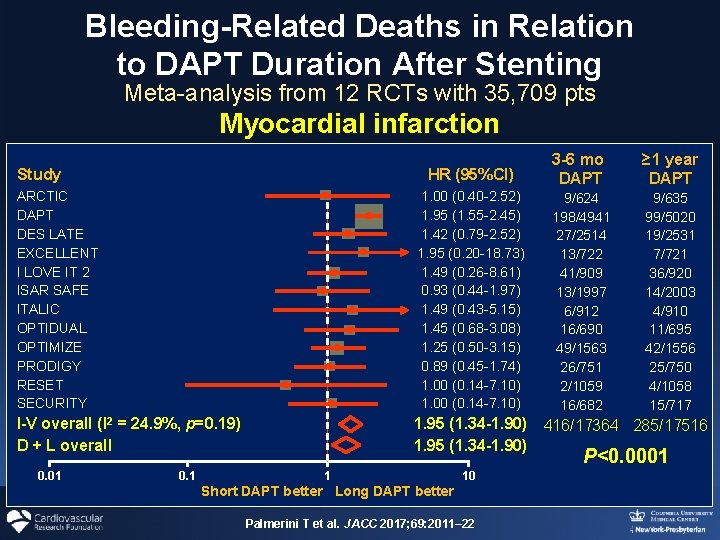
Bleeding-Related Deaths in Relation to DAPT Duration After Stenting Meta-analysis from 12 RCTs with 35, 709 pts Myocardial infarction HR (95%CI) 3 -6 mo DAPT ≥ 1 year DAPT ARCTIC DAPT DES LATE EXCELLENT I LOVE IT 2 ISAR SAFE ITALIC OPTIDUAL OPTIMIZE PRODIGY RESET SECURITY 1. 00 (0. 40 -2. 52) 1. 95 (1. 55 -2. 45) 1. 42 (0. 79 -2. 52) 1. 95 (0. 20 -18. 73) 1. 49 (0. 26 -8. 61) 0. 93 (0. 44 -1. 97) 1. 49 (0. 43 -5. 15) 1. 45 (0. 68 -3. 08) 1. 25 (0. 50 -3. 15) 0. 89 (0. 45 -1. 74) 1. 00 (0. 14 -7. 10) 9/624 198/4941 27/2514 13/722 41/909 13/1997 6/912 16/690 49/1563 26/751 2/1059 16/682 9/635 99/5020 19/2531 7/721 36/920 14/2003 4/910 11/695 42/1556 25/750 4/1058 15/717 I-V overall (I 2 = 24. 9%, p=0. 19) D + L overall 1. 95 (1. 34 -1. 90) 416/17364 285/17516 1. 95 (1. 34 -1. 90) Study 0. 01 0. 1 P<0. 0001 1 10 Short DAPT better Long DAPT better Palmerini T et al. JACC 2017; 69: 2011– 22
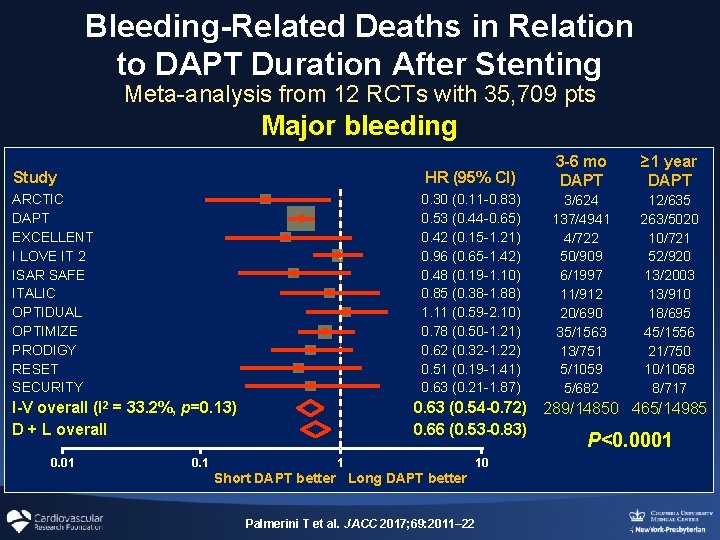
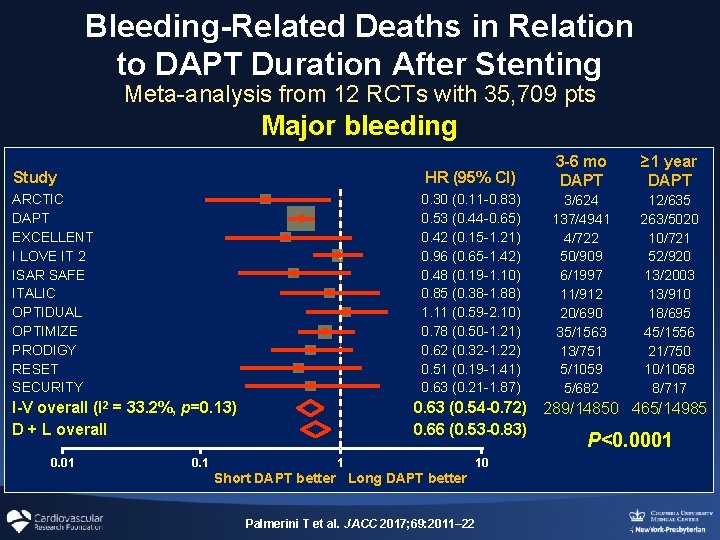
Bleeding-Related Deaths in Relation to DAPT Duration After Stenting Meta-analysis from 12 RCTs with 35, 709 pts Major bleeding Study ARCTIC DAPT EXCELLENT I LOVE IT 2 ISAR SAFE ITALIC OPTIDUAL OPTIMIZE PRODIGY RESET SECURITY I-V overall (I 2 = 33. 2%, p=0. 13) D + L overall 0. 01 0. 1 HR (95% CI) 3 -6 mo DAPT ≥ 1 year DAPT 0. 30 (0. 11 -0. 83) 0. 53 (0. 44 -0. 65) 0. 42 (0. 15 -1. 21) 0. 96 (0. 65 -1. 42) 0. 48 (0. 19 -1. 10) 0. 85 (0. 38 -1. 88) 1. 11 (0. 59 -2. 10) 0. 78 (0. 50 -1. 21) 0. 62 (0. 32 -1. 22) 0. 51 (0. 19 -1. 41) 0. 63 (0. 21 -1. 87) 3/624 137/4941 4/722 50/909 6/1997 11/912 20/690 35/1563 13/751 5/1059 5/682 12/635 263/5020 10/721 52/920 13/2003 13/910 18/695 45/1556 21/750 10/1058 8/717 0. 63 (0. 54 -0. 72) 289/14850 465/14985 0. 66 (0. 53 -0. 83) P<0. 0001 1 Short DAPT better Long DAPT better Palmerini T et al. JACC 2017; 69: 2011– 22 10
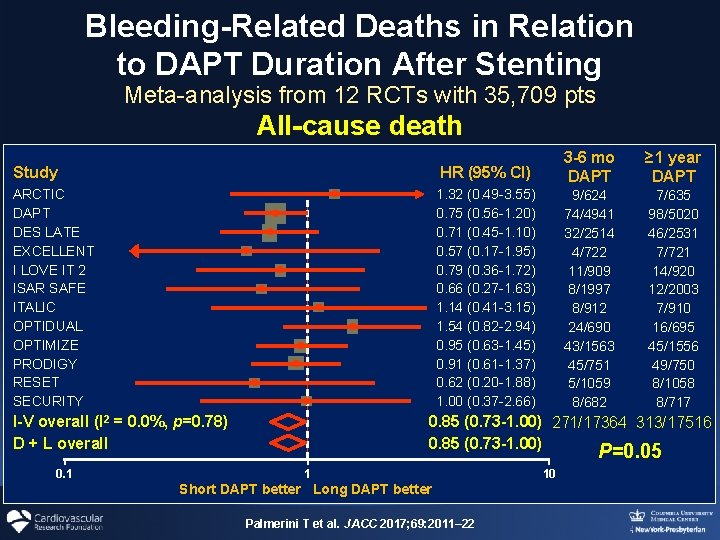
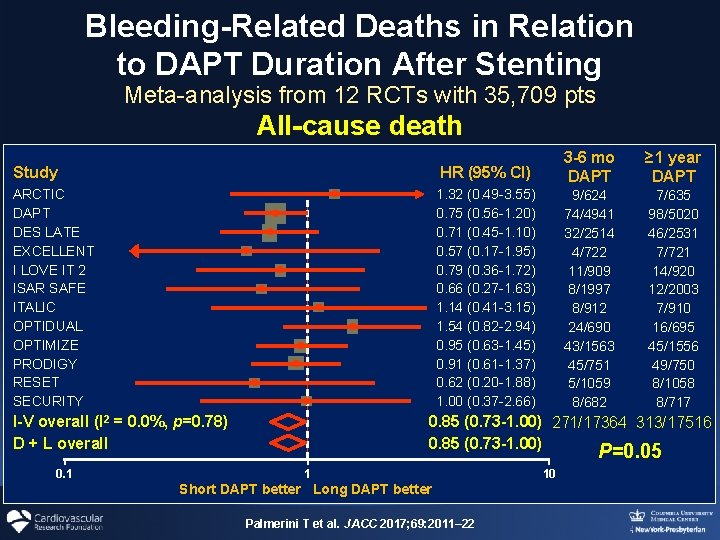
Bleeding-Related Deaths in Relation to DAPT Duration After Stenting Meta-analysis from 12 RCTs with 35, 709 pts All-cause death Study ARCTIC DAPT DES LATE EXCELLENT I LOVE IT 2 ISAR SAFE ITALIC OPTIDUAL OPTIMIZE PRODIGY RESET SECURITY I-V overall (I 2 = 0. 0%, p=0. 78) D + L overall 0. 1 HR (95% CI) 3 -6 mo DAPT ≥ 1 year DAPT 1. 32 (0. 49 -3. 55) 0. 75 (0. 56 -1. 20) 0. 71 (0. 45 -1. 10) 0. 57 (0. 17 -1. 95) 0. 79 (0. 36 -1. 72) 0. 66 (0. 27 -1. 63) 1. 14 (0. 41 -3. 15) 1. 54 (0. 82 -2. 94) 0. 95 (0. 63 -1. 45) 0. 91 (0. 61 -1. 37) 0. 62 (0. 20 -1. 88) 1. 00 (0. 37 -2. 66) 9/624 74/4941 32/2514 4/722 11/909 8/1997 8/912 24/690 43/1563 45/751 5/1059 8/682 7/635 98/5020 46/2531 7/721 14/920 12/2003 7/910 16/695 45/1556 49/750 8/1058 8/717 0. 85 (0. 73 -1. 00) 271/17364 313/17516 0. 85 (0. 73 -1. 00) P=0. 05 1 Short DAPT better Long DAPT better Palmerini T et al. JACC 2017; 69: 2011– 22 10
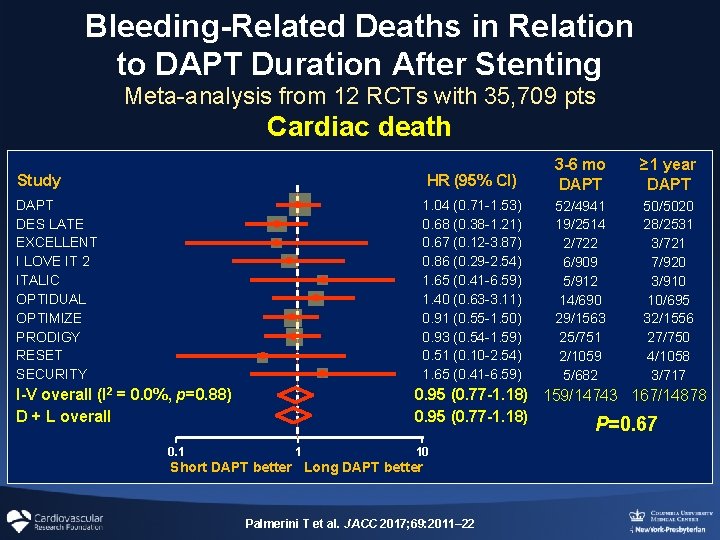
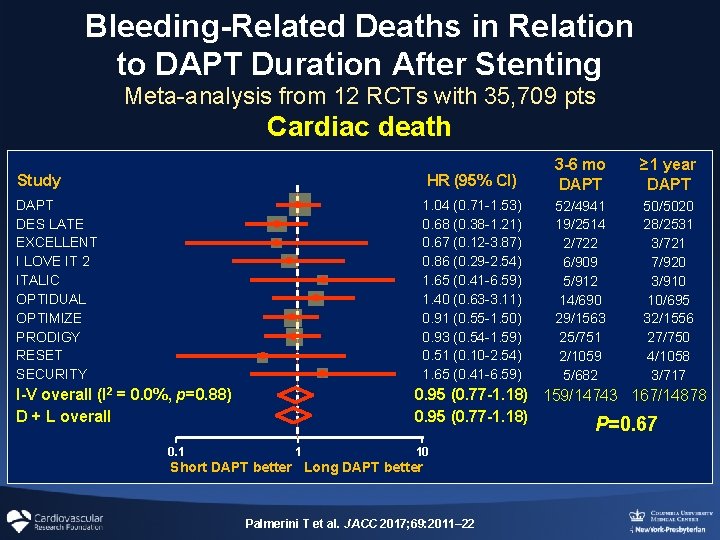
Bleeding-Related Deaths in Relation to DAPT Duration After Stenting Meta-analysis from 12 RCTs with 35, 709 pts Cardiac death HR (95% CI) 3 -6 mo DAPT ≥ 1 year DAPT 1. 04 (0. 71 -1. 53) 0. 68 (0. 38 -1. 21) 0. 67 (0. 12 -3. 87) 0. 86 (0. 29 -2. 54) 1. 65 (0. 41 -6. 59) 1. 40 (0. 63 -3. 11) 0. 91 (0. 55 -1. 50) 0. 93 (0. 54 -1. 59) 0. 51 (0. 10 -2. 54) 1. 65 (0. 41 -6. 59) 52/4941 19/2514 2/722 6/909 5/912 14/690 29/1563 25/751 2/1059 5/682 50/5020 28/2531 3/721 7/920 3/910 10/695 32/1556 27/750 4/1058 3/717 Study DAPT DES LATE EXCELLENT I LOVE IT 2 ITALIC OPTIDUAL OPTIMIZE PRODIGY RESET SECURITY I-V overall (I 2 = 0. 0%, p=0. 88) D + L overall 0. 1 0. 95 (0. 77 -1. 18) 159/14743 167/14878 0. 95 (0. 77 -1. 18) P=0. 67 1 10 Short DAPT better Long DAPT better Palmerini T et al. JACC 2017; 69: 2011– 22
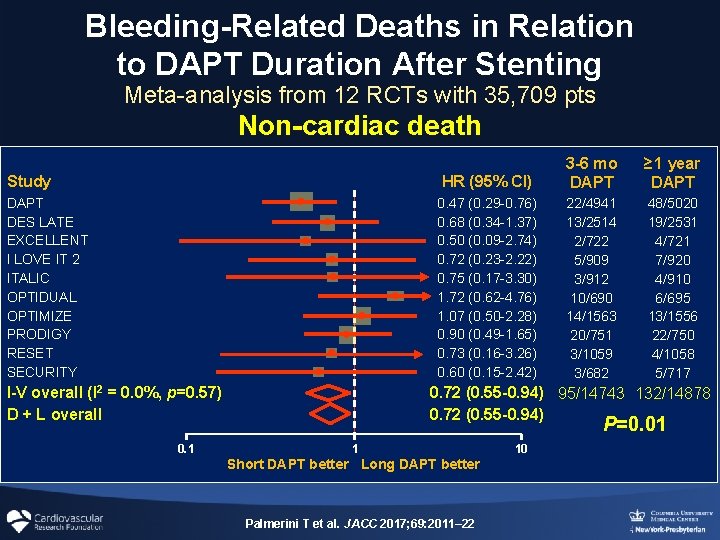
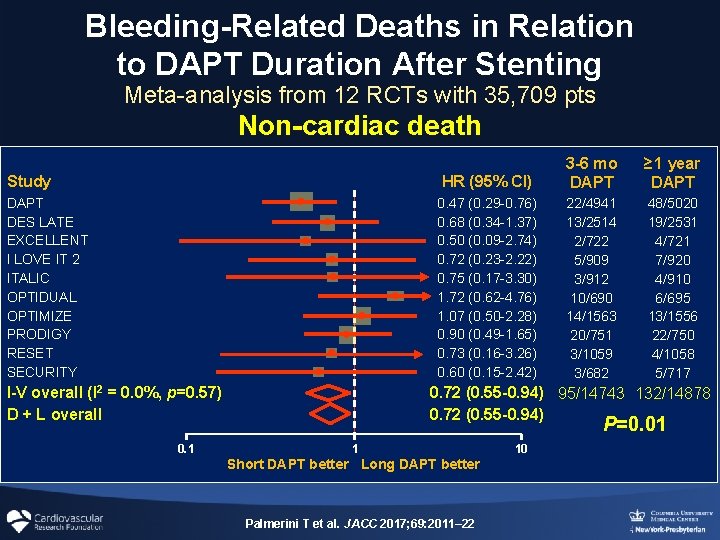
Bleeding-Related Deaths in Relation to DAPT Duration After Stenting Meta-analysis from 12 RCTs with 35, 709 pts Non-cardiac death Study DAPT DES LATE EXCELLENT I LOVE IT 2 ITALIC OPTIDUAL OPTIMIZE PRODIGY RESET SECURITY I-V overall (I 2 = 0. 0%, p=0. 57) D + L overall 0. 1 HR (95% CI) 3 -6 mo DAPT ≥ 1 year DAPT 0. 47 (0. 29 -0. 76) 0. 68 (0. 34 -1. 37) 0. 50 (0. 09 -2. 74) 0. 72 (0. 23 -2. 22) 0. 75 (0. 17 -3. 30) 1. 72 (0. 62 -4. 76) 1. 07 (0. 50 -2. 28) 0. 90 (0. 49 -1. 65) 0. 73 (0. 16 -3. 26) 0. 60 (0. 15 -2. 42) 22/4941 13/2514 2/722 5/909 3/912 10/690 14/1563 20/751 3/1059 3/682 48/5020 19/2531 4/721 7/920 4/910 6/695 13/1556 22/750 4/1058 5/717 0. 72 (0. 55 -0. 94) 95/14743 132/14878 0. 72 (0. 55 -0. 94) P=0. 01 1 Short DAPT better Long DAPT better Palmerini T et al. JACC 2017; 69: 2011– 22 10
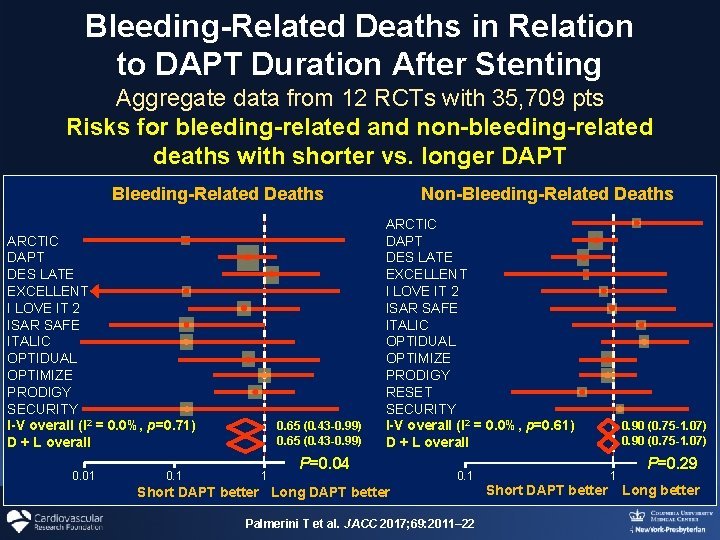
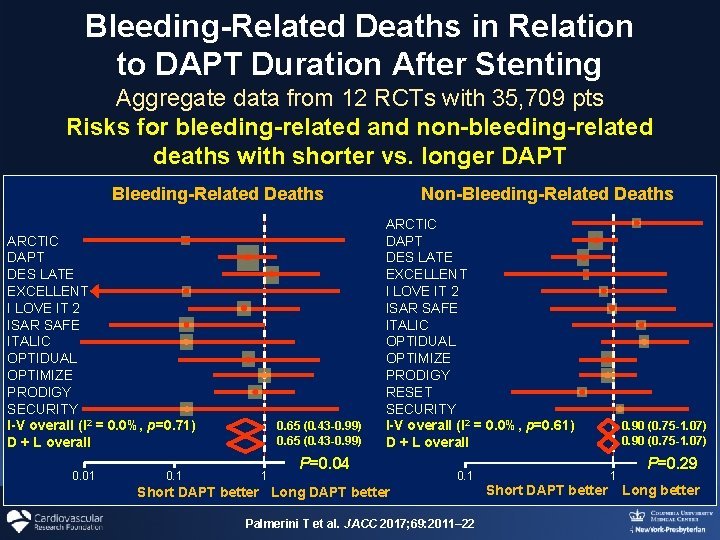
Bleeding-Related Deaths in Relation to DAPT Duration After Stenting Aggregate data from 12 RCTs with 35, 709 pts Risks for bleeding-related and non-bleeding-related deaths with shorter vs. longer DAPT Bleeding-Related Deaths ARCTIC DAPT DES LATE EXCELLENT I LOVE IT 2 ISAR SAFE ITALIC OPTIDUAL OPTIMIZE PRODIGY SECURITY I-V overall (I 2 = 0. 0%, p=0. 71) D + L overall 0. 01 0. 65 (0. 43 -0. 99) 1 Non-Bleeding-Related Deaths ARCTIC DAPT DES LATE EXCELLENT I LOVE IT 2 ISAR SAFE ITALIC OPTIDUAL OPTIMIZE PRODIGY RESET SECURITY I-V overall (I 2 = 0. 0%, p=0. 61) D + L overall P=0. 04 0. 1 Short DAPT better Long DAPT better Palmerini T et al. JACC 2017; 69: 2011– 22 0. 90 (0. 75 -1. 07) 1 Short DAPT better P=0. 29 Long better
What Factors Affect Optimal DAPT Duration after PCI? Impact of ACS vs. Stable CAD on DAPT Duration Short-term 3 vs. 6 vs. 12 months Long-term 1 year vs. longer
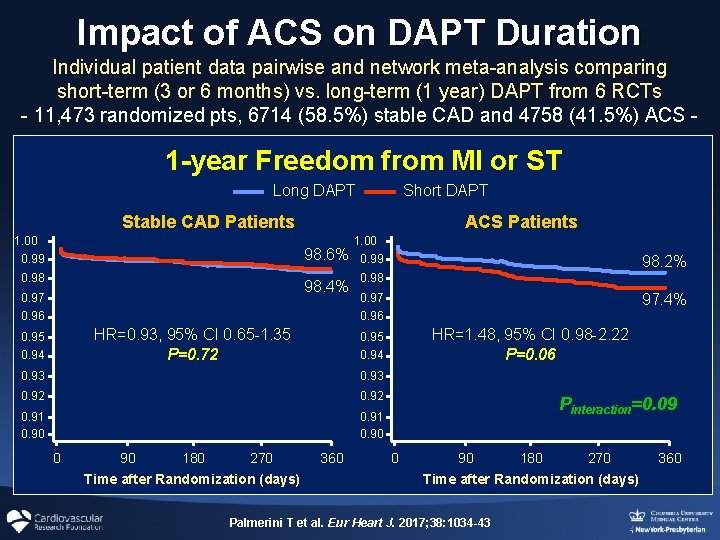
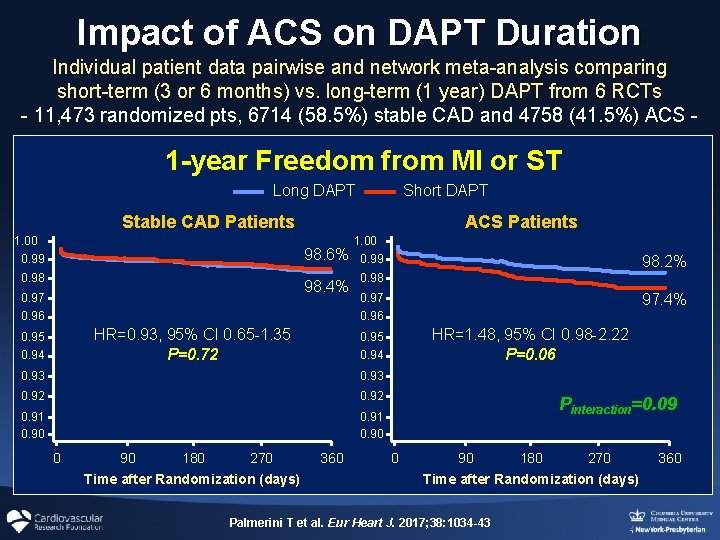
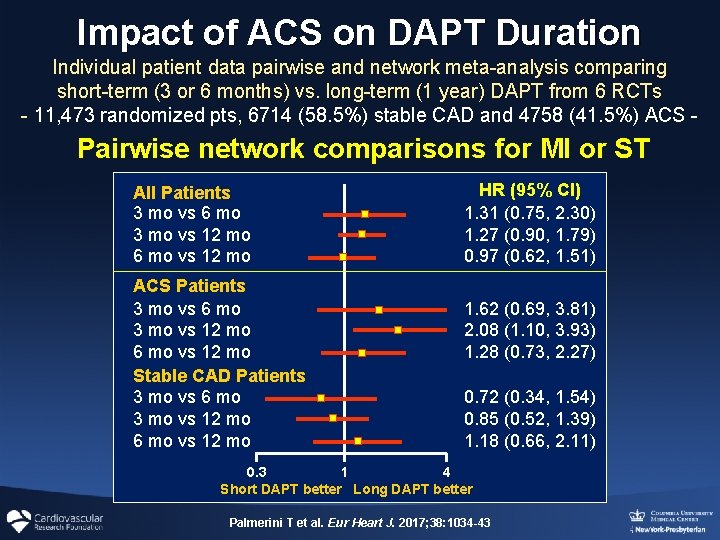
Impact of ACS on DAPT Duration Individual patient data pairwise and network meta-analysis comparing short-term (3 or 6 months) vs. long-term (1 year) DAPT from 6 RCTs - 11, 473 randomized pts, 6714 (58. 5%) stable CAD and 4758 (41. 5%) ACS - 1 -year Freedom from MI or ST Long DAPT Short DAPT Stable CAD Patients 1. 00 0. 99 ACS Patients 98. 6% 0. 98 98. 4% 0. 97 0. 96 1. 00 0. 99 98. 2% 0. 98 97. 4% 0. 97 0. 96 HR=0. 93, 95% CI 0. 65 -1. 35 P=0. 72 0. 95 0. 94 0. 93 0. 92 0. 91 0. 90 0 90 180 270 Time after Randomization (days) HR=1. 48, 95% CI 0. 98 -2. 22 P=0. 06 0. 95 360 Pinteraction=0. 09 0 90 180 270 Time after Randomization (days) Palmerini T et al. Eur Heart J. 2017; 38: 1034 -43 360
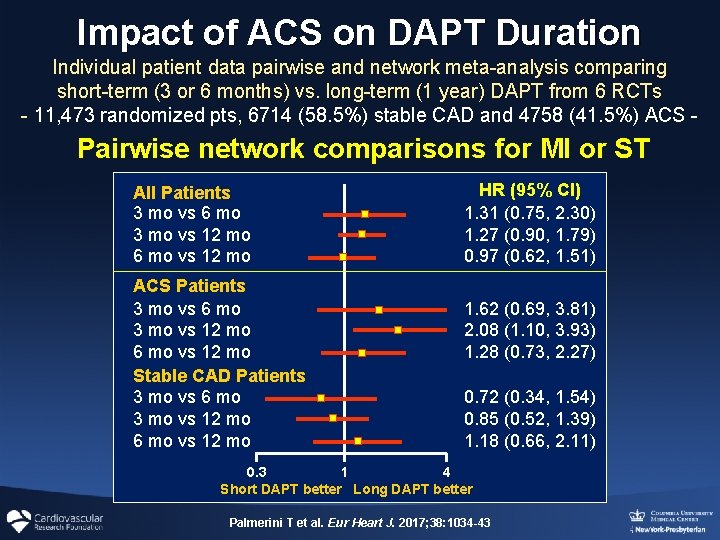
Impact of ACS on DAPT Duration Individual patient data pairwise and network meta-analysis comparing short-term (3 or 6 months) vs. long-term (1 year) DAPT from 6 RCTs - 11, 473 randomized pts, 6714 (58. 5%) stable CAD and 4758 (41. 5%) ACS - Pairwise network comparisons for MI or ST All Patients 3 mo vs 6 mo 3 mo vs 12 mo 6 mo vs 12 mo ACS Patients 3 mo vs 6 mo 3 mo vs 12 mo 6 mo vs 12 mo Stable CAD Patients 3 mo vs 6 mo 3 mo vs 12 mo 6 mo vs 12 mo HR (95% CI) 1. 31 (0. 75, 2. 30) 1. 27 (0. 90, 1. 79) 0. 97 (0. 62, 1. 51) 1. 62 (0. 69, 3. 81) 2. 08 (1. 10, 3. 93) 1. 28 (0. 73, 2. 27) 0. 72 (0. 34, 1. 54) 0. 85 (0. 52, 1. 39) 1. 18 (0. 66, 2. 11) 0. 3 1 4 Short DAPT better Long DAPT better Palmerini T et al. Eur Heart J. 2017; 38: 1034 -43
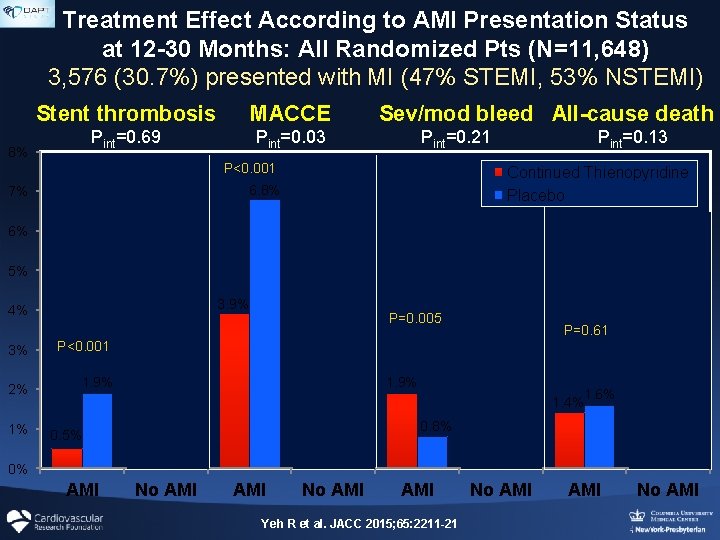
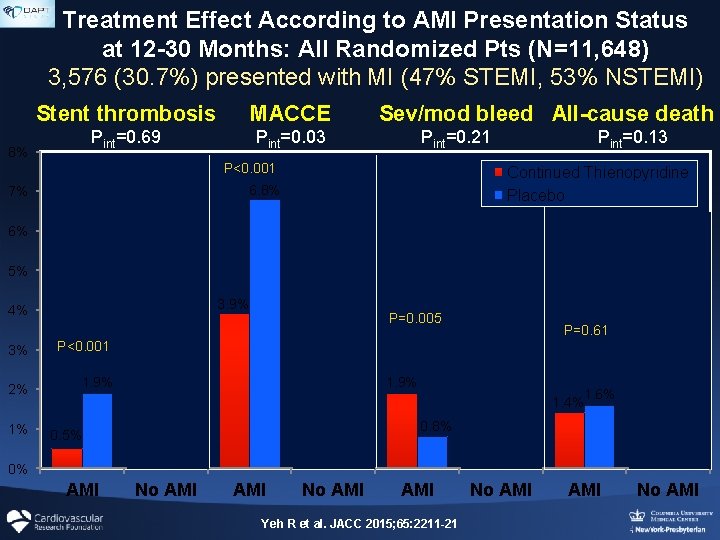
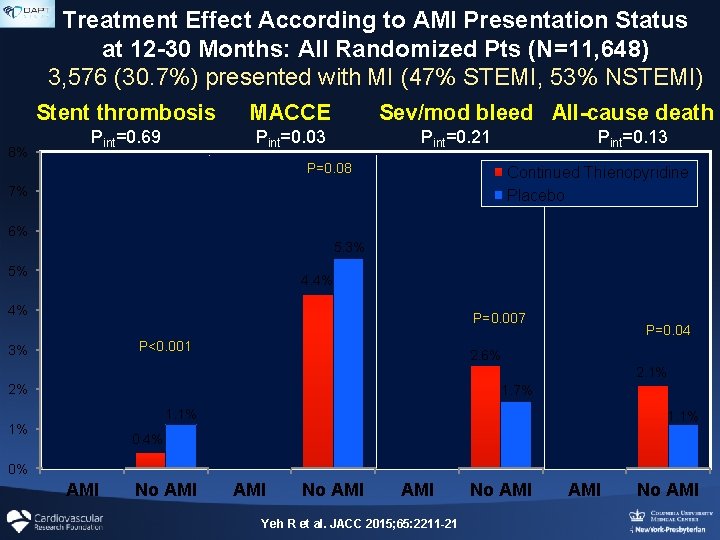
Treatment Effect According to AMI Presentation Status at 12 -30 Months: All Randomized Pts (N=11, 648) 3, 576 (30. 7%) presented with MI (47% STEMI, 53% NSTEMI) Stent thrombosis MACCE Pint=0. 69 Pint=0. 03 8% P<0. 001 Sev/mod bleed All-cause death Pint=0. 21 Pint=0. 13 P=0. 08 Continued Thienopyridine Placebo 6. 8% 7% 6% 5. 3% 5% 4. 4% 3. 9% 4% 3% P<0. 001 2% 1. 9% 1% P=0. 005 P<0. 001 P=0. 61 P=0. 04 2. 6% 2. 1% 1. 9% 1. 1% 0. 5% P=0. 007 1. 7% 1. 6% 1. 4% 0. 8% 0. 4% 1. 1% 0% AMI No AMI AMI Yeh R et al. JACC 2015; 65: 2211 -21 No AMI
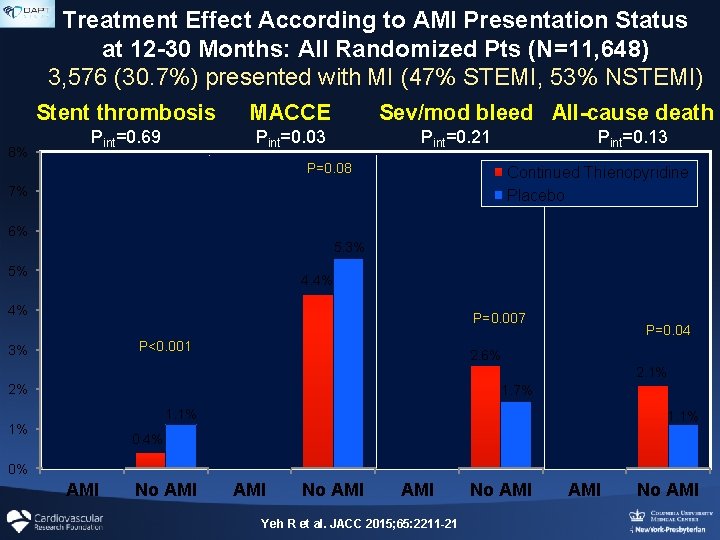
Treatment Effect According to AMI Presentation Status at 12 -30 Months: All Randomized Pts (N=11, 648) 3, 576 (30. 7%) presented with MI (47% STEMI, 53% NSTEMI) Stent thrombosis MACCE Pint=0. 69 Pint=0. 03 8% P<0. 001 Sev/mod bleed All-cause death Pint=0. 21 Pint=0. 13 P=0. 08 Continued Thienopyridine Placebo 6. 8% 7% 6% 5. 3% 5% 4. 4% 3. 9% 4% 3% P<0. 001 2% 1. 9% 1% P=0. 005 P<0. 001 P=0. 61 P=0. 04 2. 6% 2. 1% 1. 9% 1. 1% 0. 5% P=0. 007 1. 7% 1. 6% 1. 4% 0. 8% 0. 4% 1. 1% 0% AMI No AMI AMI Yeh R et al. JACC 2015; 65: 2211 -21 No AMI
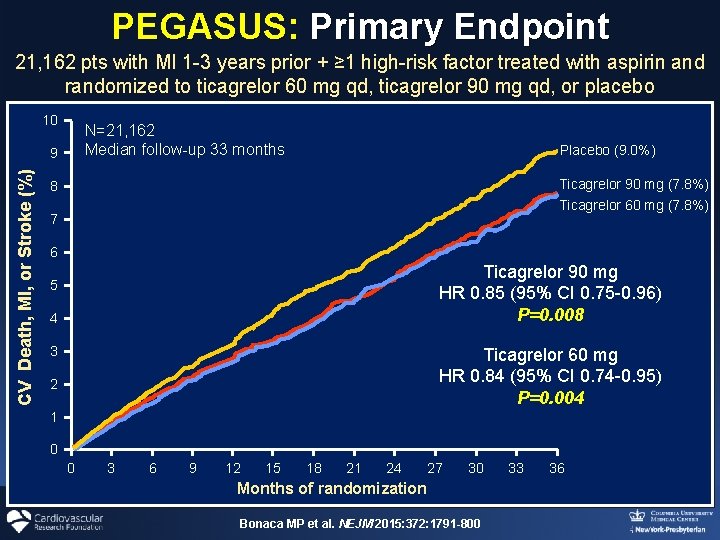
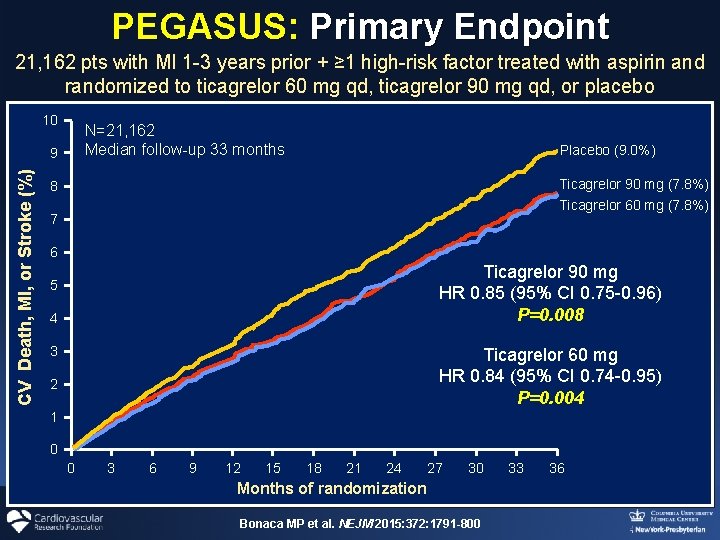
PEGASUS: Primary Endpoint 21, 162 pts with MI 1 -3 years prior + ≥ 1 high-risk factor treated with aspirin and randomized to ticagrelor 60 mg qd, ticagrelor 90 mg qd, or placebo 10 N=21, 162 Median follow-up 33 months CV Death, MI, or Stroke (%) 9 Placebo (9. 0%) Ticagrelor 90 mg (7. 8%) Ticagrelor 60 mg (7. 8%) 8 7 6 Ticagrelor 90 mg HR 0. 85 (95% CI 0. 75 -0. 96) P=0. 008 5 4 3 Ticagrelor 60 mg HR 0. 84 (95% CI 0. 74 -0. 95) P=0. 004 2 1 0 0 3 6 9 12 15 18 21 24 27 30 Months of randomization Bonaca MP et al. NEJM 2015: 372: 1791 -800 33 36
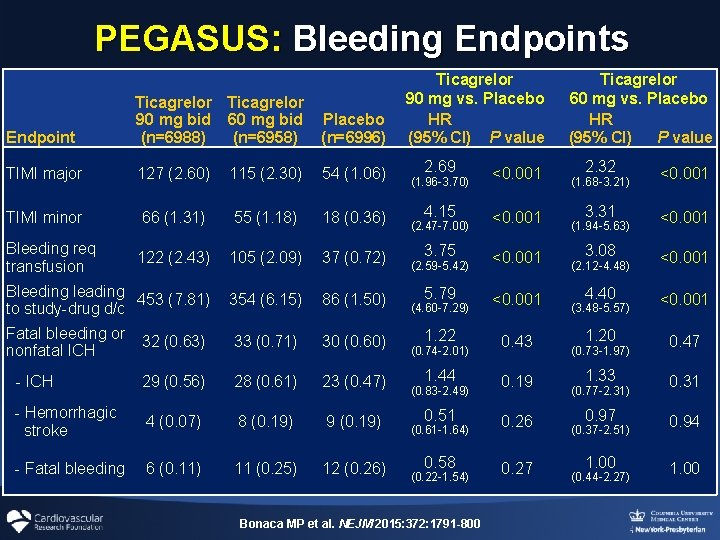
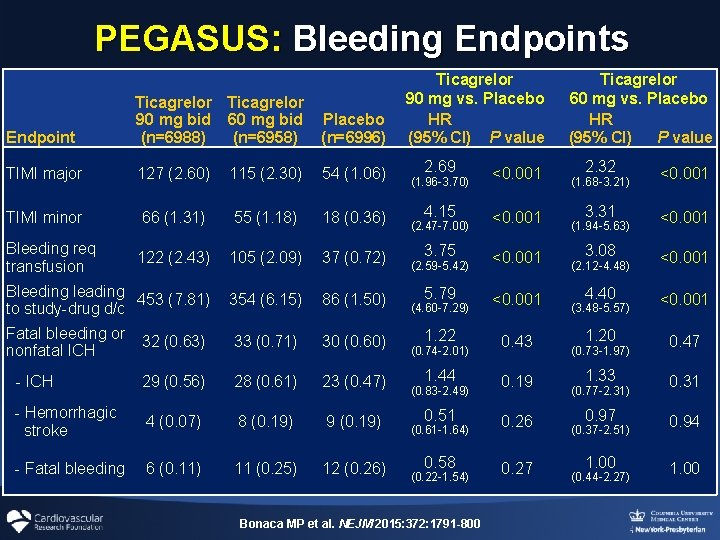
PEGASUS: Bleeding Endpoints Endpoint Ticagrelor 90 mg bid 60 mg bid (n=6988) (n=6958) Placebo (n=6996) TIMI major 127 (2. 60) 115 (2. 30) 54 (1. 06) TIMI minor 66 (1. 31) 55 (1. 18) 18 (0. 36) Bleeding req transfusion 122 (2. 43) 105 (2. 09) 37 (0. 72) Bleeding leading 453 (7. 81) to study-drug d/c 354 (6. 15) 86 (1. 50) Fatal bleeding or nonfatal ICH 32 (0. 63) 33 (0. 71) 30 (0. 60) - ICH 29 (0. 56) 28 (0. 61) 23 (0. 47) - Hemorrhagic stroke 4 (0. 07) 8 (0. 19) 9 (0. 19) - Fatal bleeding 6 (0. 11) 11 (0. 25) 12 (0. 26) Ticagrelor 90 mg vs. Placebo HR (95% CI) P value 2. 69 <0. 001 4. 15 <0. 001 3. 75 <0. 001 5. 79 <0. 001 1. 22 0. 43 1. 44 0. 19 0. 51 0. 26 0. 58 0. 27 (1. 96 -3. 70) (2. 47 -7. 00) (2. 59 -5. 42) (4. 60 -7. 29) (0. 74 -2. 01) (0. 83 -2. 49) (0. 61 -1. 64) (0. 22 -1. 54) Bonaca MP et al. NEJM 2015: 372: 1791 -800 Ticagrelor 60 mg vs. Placebo HR (95% CI) P value 2. 32 <0. 001 3. 31 <0. 001 3. 08 <0. 001 4. 40 <0. 001 1. 20 0. 47 1. 33 0. 31 0. 97 0. 94 1. 00 (1. 68 -3. 21) (1. 94 -5. 63) (2. 12 -4. 48) (3. 48 -5. 57) (0. 73 -1. 97) (0. 77 -2. 31) (0. 37 -2. 51) (0. 44 -2. 27)
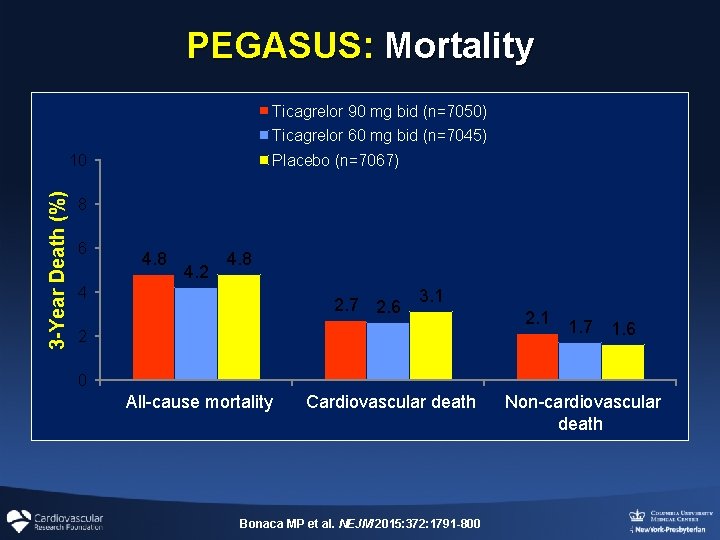
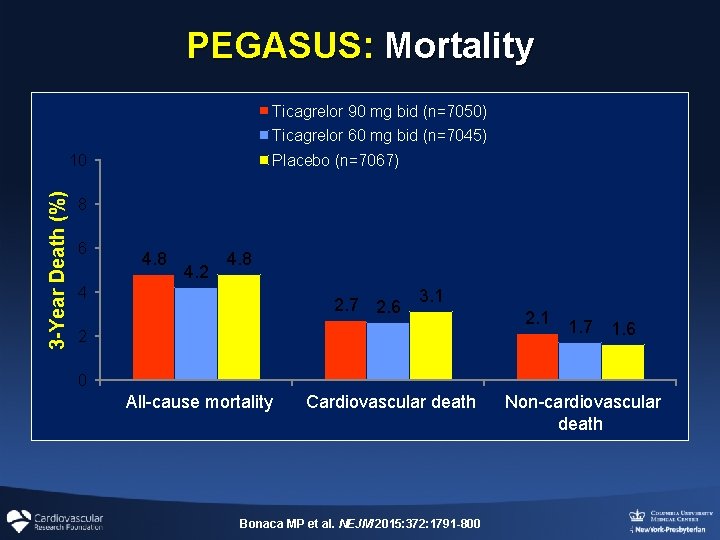
PEGASUS: Mortality Ticagrelor 90 mg bid (n=7050) Ticagrelor 60 mg bid (n=7045) Placebo (n=7067) 3 -Year Death (%) 10 8 6 4. 8 4. 2 4. 8 4 2. 7 2. 6 3. 1 2 2. 1 1. 7 1. 6 0 All-cause mortality Cardiovascular death Bonaca MP et al. NEJM 2015: 372: 1791 -800 Non-cardiovascular death
What Factors Affect Optimal DAPT Duration after PCI? Impact of Patient Age on DAPT Duration
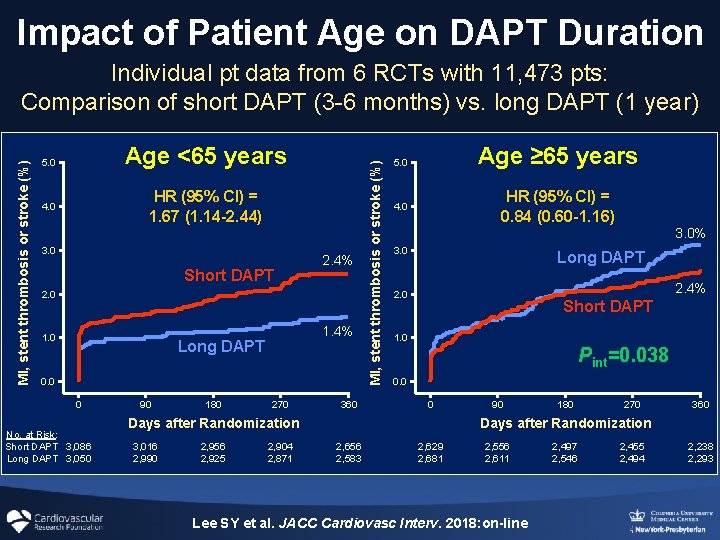
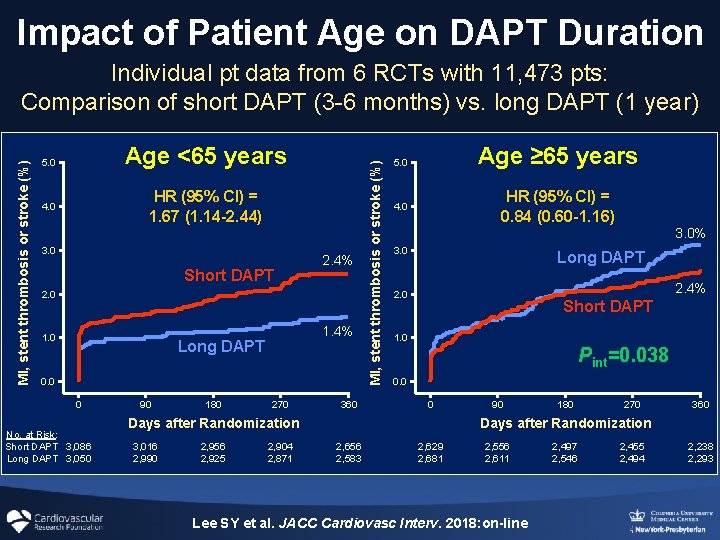
Impact of Patient Age on DAPT Duration Age <65 years 5. 0 HR (95% CI) = 1. 67 (1. 14 -2. 44) 4. 0 3. 0 Short DAPT 2. 4% 2. 0 1. 4% Long DAPT 0. 0 0 No. at Risk: Short DAPT 3, 086 Long DAPT 3, 050 90 180 270 360 MI, stent thrombosis or stroke (%) Individual pt data from 6 RCTs with 11, 473 pts: Comparison of short DAPT (3 -6 months) vs. long DAPT (1 year) Age ≥ 65 years 5. 0 HR (95% CI) = 0. 84 (0. 60 -1. 16) 4. 0 3. 0% 3. 0 Long DAPT 2. 4% 2. 0 Short DAPT 1. 0 Pint=0. 038 0. 0 0 Days after Randomization 3, 016 2, 990 2, 956 2, 925 2, 904 2, 871 90 180 270 360 Days after Randomization 2, 656 2, 583 2, 629 2, 681 2, 556 2, 611 Lee SY et al. JACC Cardiovasc Interv. 2018: on-line 2, 497 2, 546 2, 455 2, 494 2, 238 2, 293
What Factors Affect Optimal DAPT Duration after PCI? Impact of Disease Complexity on DAPT Duration
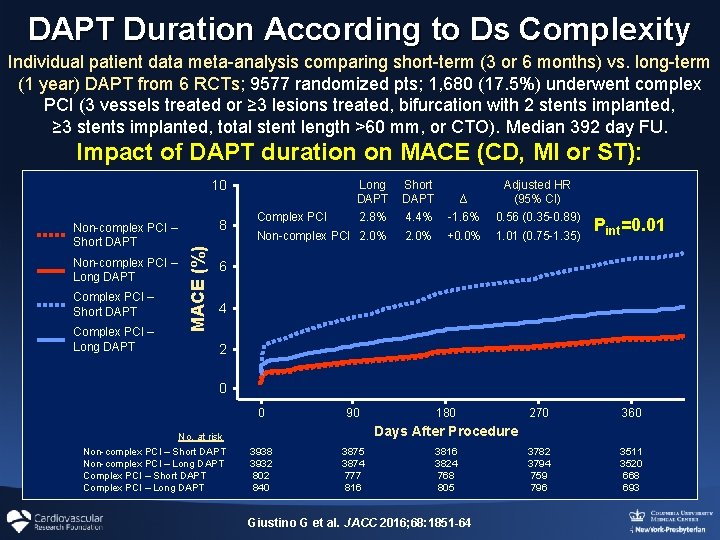
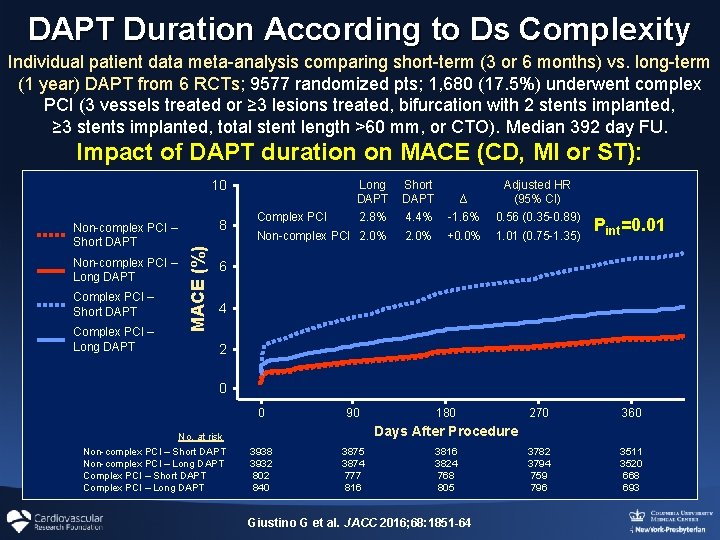
DAPT Duration According to Ds Complexity Individual patient data meta-analysis comparing short-term (3 or 6 months) vs. long-term (1 year) DAPT from 6 RCTs; 9577 randomized pts; 1, 680 (17. 5%) underwent complex PCI (3 vessels treated or ≥ 3 lesions treated, bifurcation with 2 stents implanted, ≥ 3 stents implanted, total stent length >60 mm, or CTO). Median 392 day FU. Impact of DAPT duration on MACE (CD, MI or ST): 10 Non-complex PCI – Long DAPT Complex PCI – Short DAPT Complex PCI – Long DAPT 8 MACE (%) Non-complex PCI – Short DAPT Long DAPT 2. 8% Short DAPT 4. 4% ∆ -1. 6% Adjusted HR (95% CI) 0. 56 (0. 35 -0. 89) Non-complex PCI 2. 0% +0. 0% 1. 01 (0. 75 -1. 35) Pint=0. 01 270 360 3782 3794 759 796 3511 3520 668 693 Complex PCI 6 4 2 0 0 No. at risk Non-complex PCI – Short DAPT Non-complex PCI – Long DAPT Complex PCI – Short DAPT Complex PCI – Long DAPT 90 180 Days After Procedure 3938 3932 802 840 3875 3874 777 816 3824 768 805 Giustino G et al. JACC 2016; 68: 1851 -64
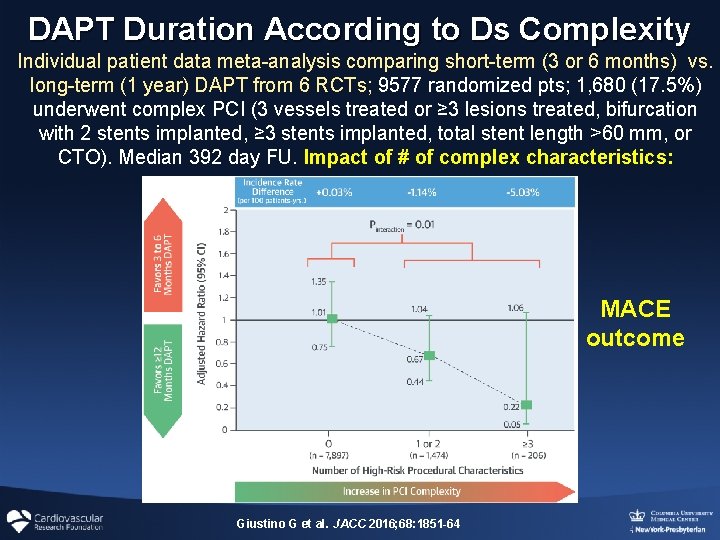
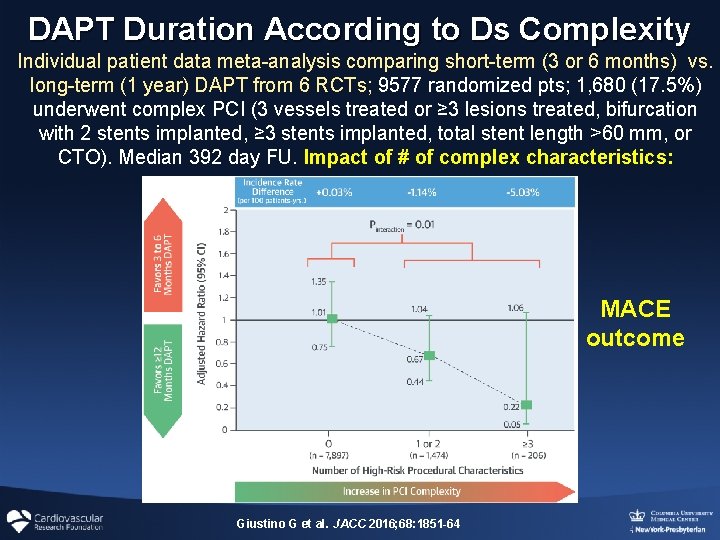
DAPT Duration According to Ds Complexity Individual patient data meta-analysis comparing short-term (3 or 6 months) vs. long-term (1 year) DAPT from 6 RCTs; 9577 randomized pts; 1, 680 (17. 5%) underwent complex PCI (3 vessels treated or ≥ 3 lesions treated, bifurcation with 2 stents implanted, ≥ 3 stents implanted, total stent length >60 mm, or CTO). Median 392 day FU. Impact of # of complex characteristics: MACE outcome Giustino G et al. JACC 2016; 68: 1851 -64
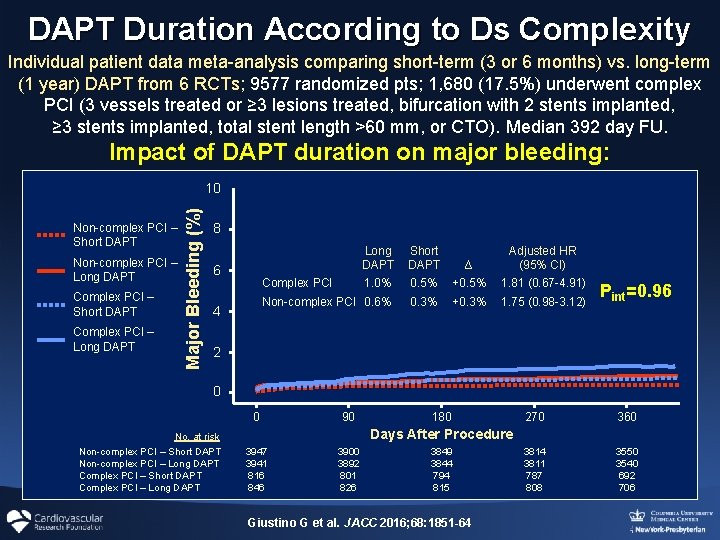
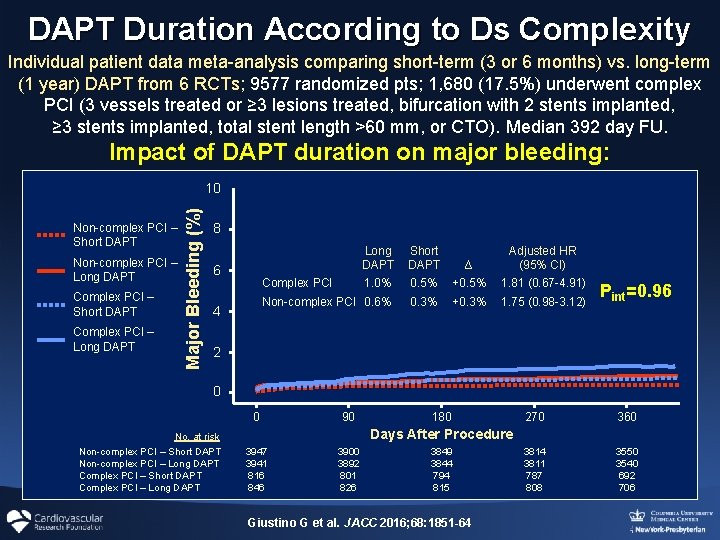
DAPT Duration According to Ds Complexity Individual patient data meta-analysis comparing short-term (3 or 6 months) vs. long-term (1 year) DAPT from 6 RCTs; 9577 randomized pts; 1, 680 (17. 5%) underwent complex PCI (3 vessels treated or ≥ 3 lesions treated, bifurcation with 2 stents implanted, ≥ 3 stents implanted, total stent length >60 mm, or CTO). Median 392 day FU. Impact of DAPT duration on major bleeding: Non-complex PCI – Short DAPT Non-complex PCI – Long DAPT Complex PCI – Short DAPT Complex PCI – Long DAPT Major Bleeding (%) 10 8 6 Long DAPT 1. 0% Short DAPT 0. 5% ∆ +0. 5% Adjusted HR (95% CI) 1. 81 (0. 67 -4. 91) Non-complex PCI 0. 6% 0. 3% +0. 3% 1. 75 (0. 98 -3. 12) Complex PCI 4 Pint=0. 96 2 0 0 No. at risk Non-complex PCI – Short DAPT Non-complex PCI – Long DAPT Complex PCI – Short DAPT Complex PCI – Long DAPT 90 180 270 360 3814 3811 787 808 3550 3540 692 706 Days After Procedure 3947 3941 816 846 3900 3892 801 826 3849 3844 794 815 Giustino G et al. JACC 2016; 68: 1851 -64
What Factors Affect Optimal DAPT Duration after PCI? Should Stent Type Affect DAPT Duration?
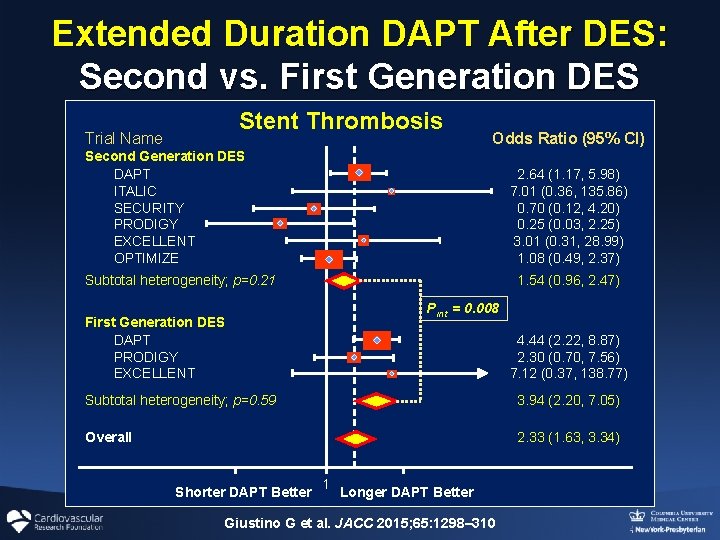
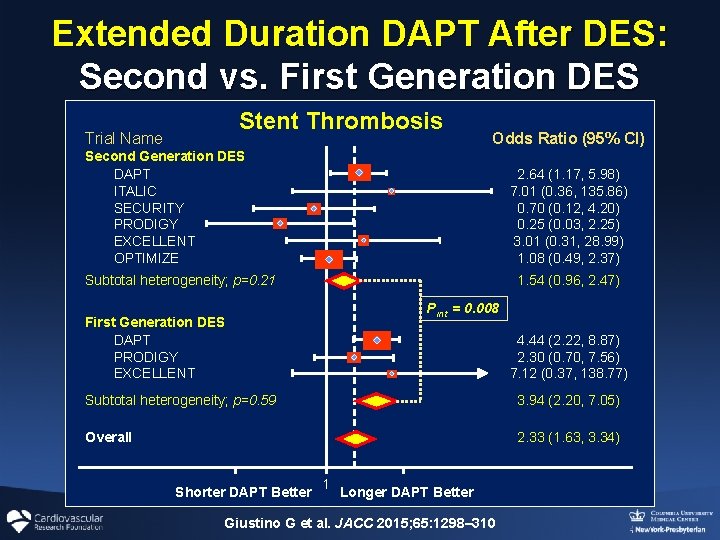
Extended Duration DAPT After DES: Second vs. First Generation DES Stent Thrombosis Trial Name Odds Ratio (95% CI) Second Generation DES DAPT ITALIC SECURITY PRODIGY EXCELLENT OPTIMIZE 2. 64 (1. 17, 5. 98) 7. 01 (0. 36, 135. 86) 0. 70 (0. 12, 4. 20) 0. 25 (0. 03, 2. 25) 3. 01 (0. 31, 28. 99) 1. 08 (0. 49, 2. 37) Subtotal heterogeneity; p=0. 21 1. 54 (0. 96, 2. 47) Pint = 0. 008 First Generation DES DAPT PRODIGY EXCELLENT 4. 44 (2. 22, 8. 87) 2. 30 (0. 70, 7. 56) 7. 12 (0. 37, 138. 77) Subtotal heterogeneity; p=0. 59 3. 94 (2. 20, 7. 05) Overall 2. 33 (1. 63, 3. 34) Shorter DAPT Better 1 Longer DAPT Better Giustino G et al. JACC 2015; 65: 1298– 310
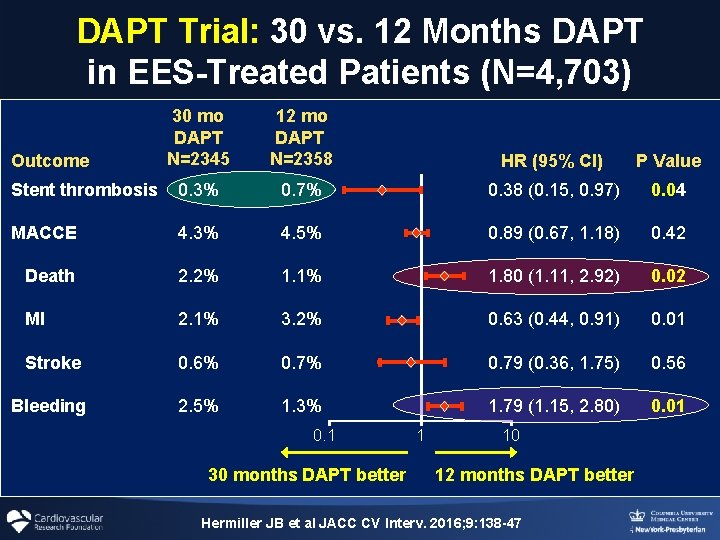
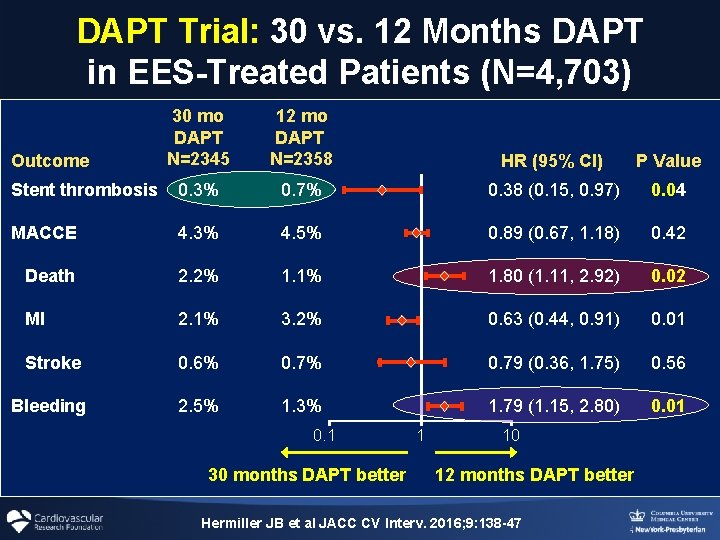
DAPT Trial: 30 vs. 12 Months DAPT in EES-Treated Patients (N=4, 703) 30 mo DAPT N=2345 12 mo DAPT N=2358 HR (95% CI) P Value Stent thrombosis 0. 3% 0. 7% 0. 38 (0. 15, 0. 97) 0. 04 MACCE 4. 3% 4. 5% 0. 89 (0. 67, 1. 18) 0. 42 Death 2. 2% 1. 1% 1. 80 (1. 11, 2. 92) 0. 02 MI 2. 1% 3. 2% 0. 63 (0. 44, 0. 91) 0. 01 Stroke 0. 6% 0. 79 (0. 36, 1. 75) 0. 56 Bleeding 2. 5% 1. 3% 1. 79 (1. 15, 2. 80) 0. 01 Outcome 0. 1 30 months DAPT better 1 10 12 months DAPT better Hermiller JB et al JACC CV Interv. 2016; 9: 138 -47
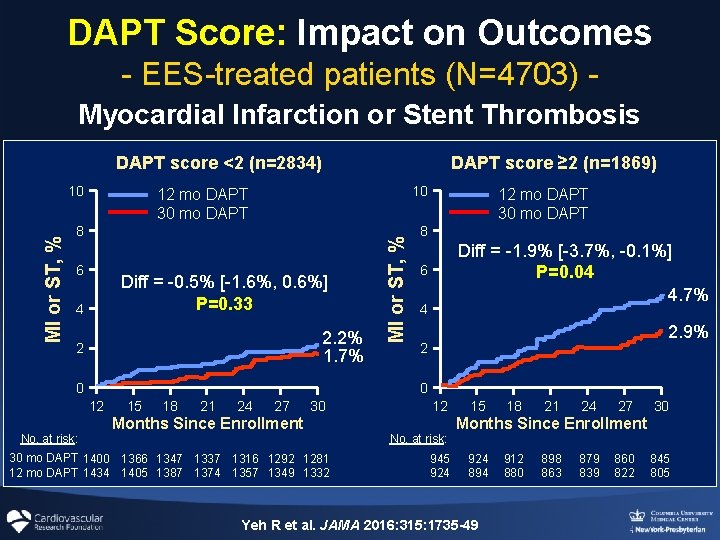
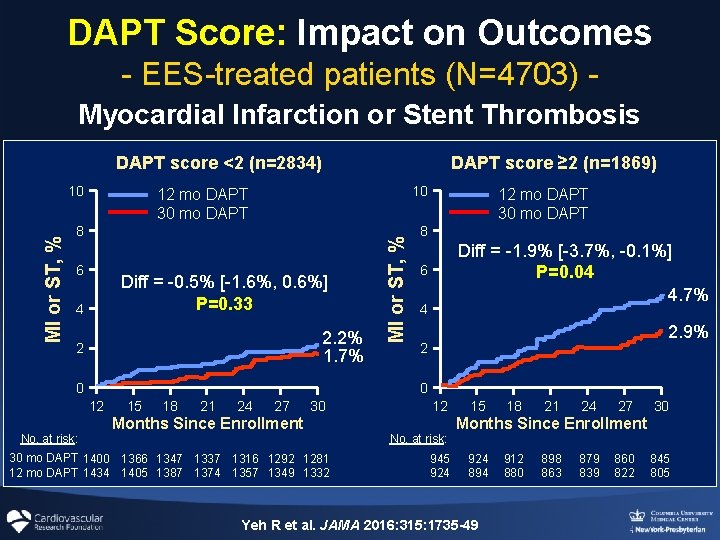
DAPT Score: Impact on Outcomes - EES-treated patients (N=4703) Myocardial Infarction or Stent Thrombosis DAPT score <2 (n=2834) 10 12 mo DAPT 30 mo DAPT 8 6 Diff = -0. 5% [-1. 6%, 0. 6%] P=0. 33 4 2. 2% 1. 7% 2 0 12 mo DAPT 30 mo DAPT 8 Diff = -1. 9% [-3. 7%, -0. 1%] P=0. 04 4. 7% 6 4 2. 9% 2 0 12 No. at risk: MI or ST, % 10 DAPT score ≥ 2 (n=1869) 15 18 21 24 27 30 Months Since Enrollment 30 mo DAPT 1400 1366 1347 1337 1316 1292 1281 12 mo DAPT 1434 1405 1387 1374 1357 1349 1332 12 No. at risk: 945 924 15 18 21 24 27 30 Months Since Enrollment 924 894 Yeh R et al. JAMA 2016: 315: 1735 -49 912 880 898 863 879 839 860 822 845 805
DAPT Duration: Factors to be weighed When assessing ischemic and bleeding risk, clinical presentation (ACS vs SIHD), age, disease/PCI complexity and stent type are important factors to consider Palmerini T and Stone GW. Eur Heart J 2016; 37: 353 -64