Postpartum Hemorrhage 1 PPH is defined as 1000
- Slides: 2
Postpartum Hemorrhage (1) • • PPH is defined as >1000 ml blood loss after vaginal or cesarean delivery or blood loss significant enough to cause changes in vital signs. PPH is the leading cause of maternal mortality in US. Risk factors: prolonged labor, infection, macrosomia, polyhydramnios, anticoagulant use, pre-eclampsia, coagulopathy, multifetal gestation, uterine fibroids, precipitous delivery, abruption. Consider Type and Cross if high risk. Causes- “The 4 Ts” ○ Tone- cause for 70 -80% of PPH ○ Trauma/Tear (perineal/vaginal/cervical lacerations, uterine rupture, uterine inversion, hematomas) ○ Tissue- retained placenta, invasive placenta ○ Thrombin- DIC, coagulopathy, anticoagulants Prevention○ Active Management of the Third Stage of Labor. Pitocin, gentle cord traction, fundal massage ○ Labor management to minimize dystocia and prolonged rupture of membranes Delayed PPH Defined as 24 hours after delivery up to 12 weeks postpartum. Most likely subinvolution of the placental site, retained POCs, infection, inherited coagulation defects. Updated 4/20
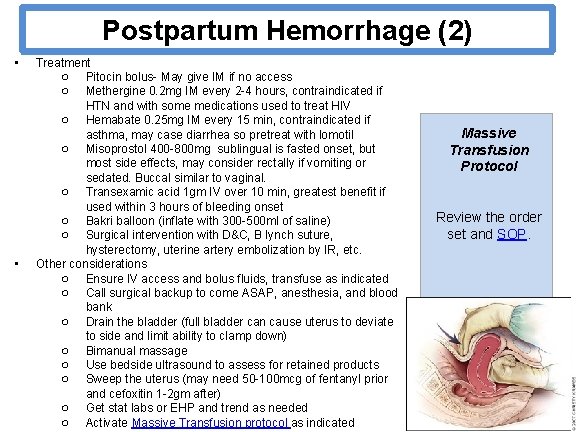
Postpartum Hemorrhage (2) • • Treatment ○ Pitocin bolus- May give IM if no access ○ Methergine 0. 2 mg IM every 2 -4 hours, contraindicated if HTN and with some medications used to treat HIV ○ Hemabate 0. 25 mg IM every 15 min, contraindicated if asthma, may case diarrhea so pretreat with lomotil ○ Misoprostol 400 -800 mg sublingual is fasted onset, but most side effects, may consider rectally if vomiting or sedated. Buccal similar to vaginal. ○ Transexamic acid 1 gm IV over 10 min, greatest benefit if used within 3 hours of bleeding onset ○ Bakri balloon (inflate with 300 -500 ml of saline) ○ Surgical intervention with D&C, B lynch suture, hysterectomy, uterine artery embolization by IR, etc. Other considerations ○ Ensure IV access and bolus fluids, transfuse as indicated ○ Call surgical backup to come ASAP, anesthesia, and blood bank ○ Drain the bladder (full bladder can cause uterus to deviate to side and limit ability to clamp down) ○ Bimanual massage ○ Use bedside ultrasound to assess for retained products ○ Sweep the uterus (may need 50 -100 mcg of fentanyl prior and cefoxitin 1 -2 gm after) ○ Get stat labs or EHP and trend as needed ○ Activate Massive Transfusion protocol as indicated Massive Transfusion Protocol Review the order set and SOP.