POSTPARTUM CARE DEFINITION OF THE POSTPARTUM PERIOD Six







- Slides: 26

POSTPARTUM CARE
DEFINITION OF THE POSTPARTUM PERIOD Six to eight weeks after delivery Some authors describe women as postpartum for as long as 12 months after deliver

Treatment Supportive with warm blankets and/or warm air Anesthesia-related shivering can be treated pharmacologically
Uterine involution Immediately after delivery: the fundus is normally firm, nontender, globular, and located midway between the symphysis pubis and umbilicus the end of the two postpartum week: It is not palpable six to eight weeks postpartum: normal nonpregnant size The weight of the uterus decreases from approximately 1000 g immediately postpartum to 60 g six to eight weeks later.
Lochia The basal portion of the decidua remains after the placenta separates. This decidua divides into two layers: The superficial layer is shed and the deep layer regenerates new endometrium, which covers the entire endometrial cavity by the 16 th postpartum day Normal shedding of blood and decidua is referred to as lochia rubra : first few days following delivery Vaginal discharge then becomes increasingly watery, called lochia serosa (pinkish brown) : two to three weeks The discharge turns yellowish white, the lochia alba. Microscopically, lochia consists of serous exudate, erythrocytes, leukocytes, decidua, epithelial cells, and bacteria.
Cervix — After delivery: Soft and floppy Small lacerations Few postpartum days: Remains 2 to 3 cm dilated One week: less than 1 cm dilated The external os never resumes its pregravid sha

Human chorionic gonadotropin (h. CG): Median time of elimination : 12 days (two to four weeks)
Breast engorgement results in breast fullness and firmness pain and tenderness primarily areolar involvement , more peripheral involvement Primary engorgement is due to interstitial edema and onset of copious milk production. 24 and 72 hours postpartum, with a normal range of one to seven days; peak symptomatology averages three to five days postpartum. Secondary engorgement typically occurs later if the mother's milk supply exceeds the amount of milk removed by her infant.
Rooming in — Rooming in 24 hours a day is one component of the Baby-friendly Hospital Initiative launched by the World Health Organization and UNICEF
Maternal monitoring — In addition to routine vital signs: ●Vaginal bleeding ●Over distended bladder ●The perineum Perineal care: Stool softeners and laxati Laboratory testing
Prevention of venous thrombosis thromboembolism (VTE) is more common in postpartum women than in antepartum and nonpregnant women, and more common after cesarean than vaginal birth Several factors increase the risk, including but not limited to previous VTE, thrombophilia, certain medical comorbidities (eg, sickle cell disease), obesity, smoking, cesarean delivery, and postpartum hemorrhage Prophylaxis is recommended for women at high risk of having a thromboembolic event, although specific criteria to identify these women vary among institutions and guidelines
— Rh(D)-negative mothers of Rh(D)-positive infants should be given anti-D immune globulin as soon as possible after delivery and within 72 hours Pelvic muscle exercises — PFME in the immediate postpartum period may be contraindicated in women who sustain injury to the levator ani muscle complex at childbirth because exercise may be harmful in the early phase of injury recovery.
Pain management After pains multiparous in women in whom the uterus was overdistended before delivery (eg, multiple gestation, polyhydramnios). Afterpains usually spontaneously resolve by the end of the first postpartum week. Mild analgesics (eg, acetaminophen, ibuprofen, diclofenac suppositories) are effective, and the nonsteroidal anti-inflammatory drugs (NSAIDs) appear to be more effective than acetaminophen (paracetamol) Opioids should be avoided.

Perineal pain — oral analgesics ( acetaminophen, ibuprofen) topical treatments (cold or warm packs) and topical anesthetics Opioids should be avoided
Cesarean delivery ●Acetaminophen ●NSAIDs – Ibuprofen and diclofenac suppositories, a short half-life (<6 hours) Naproxen should be avoided, long half-life (>6 hours) ●Opioids butorphanol, morphine, or hydromorphone is preferable to meperidine or pethidine infant monitored for sedation not using codeine and tramadol

Voiding difficulty and urinary retention Postpartum urinary retention (PUR): Injury to the pudendal nerve during the birth process Prolonged pudendal nerve terminal motor latency has been demonstrated Last for two to three months postpartum Rare women have long-term dysfunction.
Overt PUR : The absence of spontaneous micturition within six hours of vaginal delivery or within six hours of removal of an indwelling catheter after cesarean delivery Covert PUR: postvoid residual bladder volume of at least 150 m. L after spontaneous micturition, as verified by catheterization or ultrasound.
●Risk factors – Epidural anesthesia Primiparity Instrument-assisted delivery Episiotomy
●Management intermittent catheterization. Pharmacological therapies are not effective. Catheterization is indicated if the bladder can be palpated abdominally and the woman is unable to void or she voids only small amounts suggestive of overflow. ●Course – typically self-limited resolve within one week in most patients
Symptomatic lower extremity varicose veins Pregnancy is a risk factor , may appear and become symptomatic anytime during the antepartum or postpartum period Leg elevation, exercise, and compression therapy improve oxygen transport to the skin and subcutaneous tissues, decrease edema, reduce inflammation, and compress dilated veins Varicose veins are a risk factor for superficial phlebitis and thrombosis

Neuropathy 1 percent of deliveries mononeuropathies that result from compression, stretch, transection, or vascular injury. lateral femoral cutaneous nerve femoral nerve, peroneal nerve, lumbosacral plexus, sciatic nerve, and obturator nerve Rarely, neuropathic symptoms can reflect complications that directly result from neuraxial anesthesia, such as epidural hematoma and epidural abscess [94]. Risk factors : fetal macrosomia or malpresentation, sensory blockade (can impair recognition of discomfort), prolonged lithotomy position, prolonged second stage of labor, extremes of maternal weight, and improper use of leg stirrups or retractors
• The lateral femoral cutaneous nerve does not contain motor fibers; thus, neurologic symptoms are restricted to sensory changes. Lateral hip pain accompanied by paresthesias (burning pain) or hypesthesias (numbness and tingling) over the upper outer thigh is the classic presentation of compression of this nerve. femoral neuropathy develop weakness involving the quadriceps muscle group with sparing of adduction. In addition to muscle weakness, sensory loss over the anterior thigh and most of the medial thigh is typical.
Peroneal nerve compression results in foot drop. It can be caused by prolonged squatting, sustained knee flexion, or pressure on the fibular head from stirrups or palmar pressure during pushing. • Obturator neuropathies are an uncommon complication of delivery and present with medial thigh pain and adductor weakness.

●Treatment depends on the woman's symptoms anti-inflammatory drugs topical patches peripheral nerve block Muscle weakness is assessed by a physical therapist ●Prognosis – spontaneous resolution of their symptoms over days to weeks; the median time for recovery is eight weeks
 Rncob
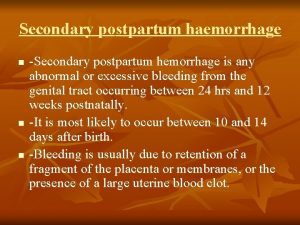
Rncob Secondary postpartum haemorrhage
Secondary postpartum haemorrhage Homan signs
Homan signs Primary secondary and tertiary care
Primary secondary and tertiary care A polygon with six congruent sides and six congruent angles
A polygon with six congruent sides and six congruent angles The development of children 7th edition
The development of children 7th edition A&p flix activity: resting membrane potential
A&p flix activity: resting membrane potential Is hyperpolarization the same as refractory period
Is hyperpolarization the same as refractory period Critical period vs sensitive period
Critical period vs sensitive period Critical/sensitive periods
Critical/sensitive periods Critical period vs sensitive period
Critical period vs sensitive period Less complicated texture than baroque (more homophonic)
Less complicated texture than baroque (more homophonic) Metallic, period 4, 20 electrons
Metallic, period 4, 20 electrons What served as the seed of activism?
What served as the seed of activism? Stability period vs measurement period
Stability period vs measurement period Trustee period and royal period
Trustee period and royal period Prehistory vocabulary
Prehistory vocabulary Vertical
Vertical Bubble-he assessment
Bubble-he assessment Secondary postpartum haemorrhage
Secondary postpartum haemorrhage Pph treatment algorithm
Pph treatment algorithm Rubin's psychological changes of the puerperium
Rubin's psychological changes of the puerperium Bubble postpartum
Bubble postpartum Postpartum thyroiditis
Postpartum thyroiditis Bubble he assessment
Bubble he assessment Postpartum bleeding stages
Postpartum bleeding stages Postpartum hemorrhage treatment drugs
Postpartum hemorrhage treatment drugs