POSTOPERATIVE FEVER Objectives Identify the common causes of

POST-OPERATIVE FEVER
Objectives • Identify the common causes of postoperative fever • Establish a differential diagnosis based on timing of the fever • Know when and how to appropriately work -up postoperative fever
Post-op Fever • Common – Incidence 14 -91% • Cause varies based on timing – Immediate: onset in the OR or within hours – Acute: onset in the first week – Subacute: 1 -4 weeks after surgery – Delayed: more than 1 month after surgery
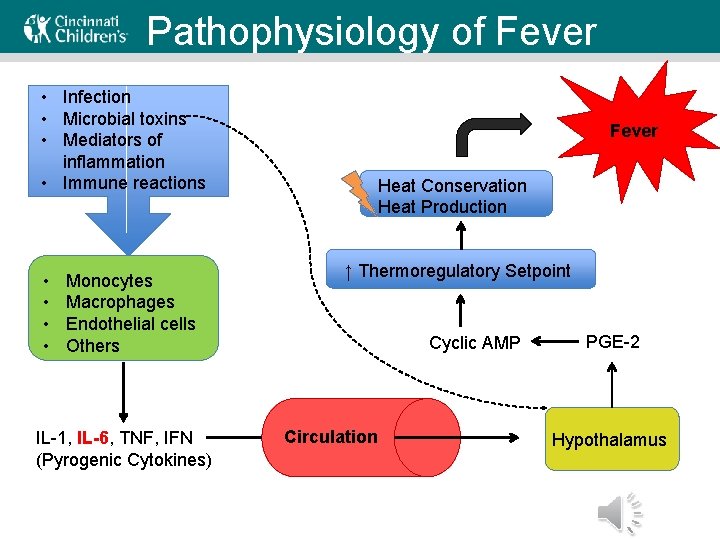
Pathophysiology of Fever • Infection • Microbial toxins • Mediators of inflammation • Immune reactions • • Monocytes Macrophages Endothelial cells Others IL-1, IL-6, TNF, IFN (Pyrogenic Cytokines) Fever Heat Conservation Heat Production ↑ Thermoregulatory Setpoint Cyclic AMP Circulation PGE-2 Hypothalamus
Pathophysiology of Post-op Fever • More traumatic the surgery, higher risk of post-op fever • Genetic factors may influence magnitude of cytokine release in response to trauma • NSAIDs and glucocorticoids suppress cytokine release (and decrease magnitude of febrile response)
Case 1 • 3 mo old male with craniosynostosis – Otherwise healthy, normal birth and development – Underwent extensive frontotemporal-parietal craniectomy with multiple osteotomies and harvesting of bone graft for craniofacial reconstruction (craniosynostosis) – Today is POD#1 – Called for fever of 39. 1˚C – On exam, his eyes are swollen shut, fussy but otherwise well-appearing
Case 1 What work-up would you recommend for this patient? A. B. C. D. E. CBC & Blood culture UA & Urine culture Chest xray ESR/CRP Observation only Click forward to see the answer and hear the explanation
First 48 Hours • Common Causes – Reaction to anesthesia or other intra-op meds – Reaction to trauma and stress – Healing inflammatory response – Reaction to pyrogenic implant • Sign of infection? – Incidence of infection < 10% of patients – Height of fever is not a reliable marker of infection
First 48 Hours • Typical Course – Resolves within 2 -3 days • Usual management: observation only – Unless the patient is ill-appearing or has some other reason for concern – Consider pre-op period (occult communityacquired infection) – Did they receive blood products? Think transfusion reaction
First 48 Hours • Reasons to worry – Myonecrosis – look at the wound – Pulmonary embolism – Bowel leak, pancreatitis – Adrenal insufficiency (genetic, iatrogenic) – Malignant hyperthermia (within 10 hr of GA) – Alcohol withdrawal – Transfusion reaction – Immune-mediated drug reaction – hypotension, rash – Hematoma
Case 2 • 9 yo female with juvenile idiopathic scoliosis, o/w healthy, s/p posterior spinal fusion – Spiked fever to 38. 7˚C on POD#1 – Called for continued fever on POD#2 – Has pain at the incision site – Foley catheter will be removed later today – Physical exam normal except for mild bibasilar crackles on lung exam

Case 2
Case 2 What is the most likely cause of her fever? A. UTI B. Atelectasis C. DVT D. Other Click forward to see the answer and hear the explanation
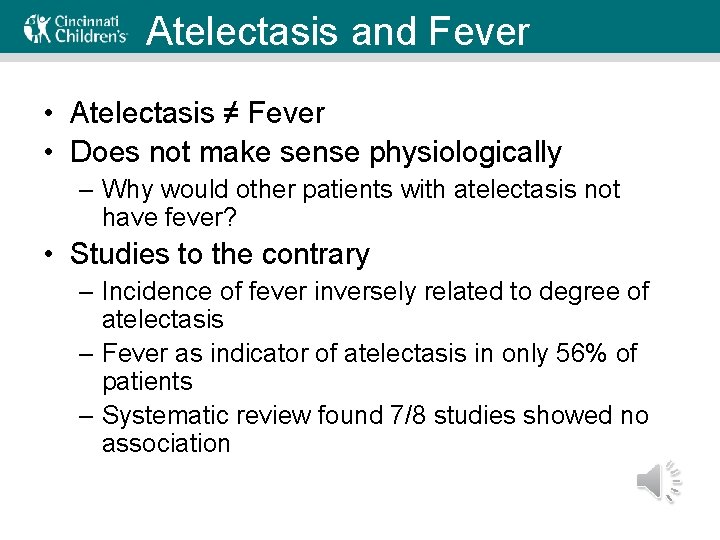
Atelectasis and Fever • Atelectasis ≠ Fever • Does not make sense physiologically – Why would other patients with atelectasis not have fever? • Studies to the contrary – Incidence of fever inversely related to degree of atelectasis – Fever as indicator of atelectasis in only 56% of patients – Systematic review found 7/8 studies showed no association
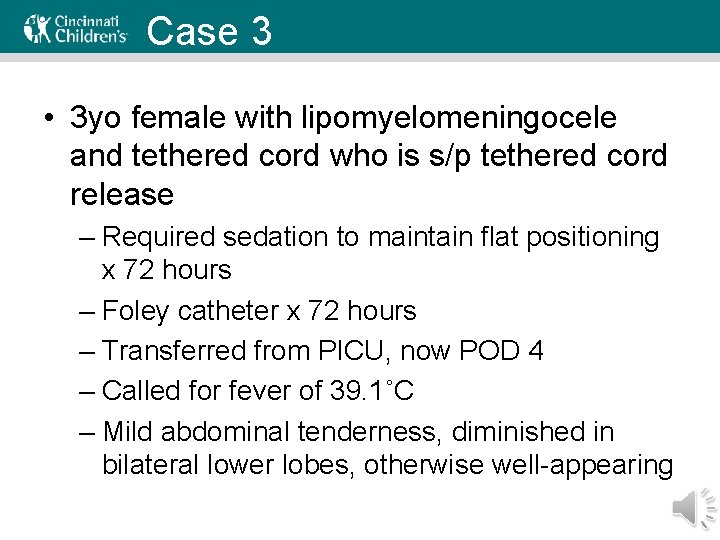
Case 3 • 3 yo female with lipomyelomeningocele and tethered cord who is s/p tethered cord release – Required sedation to maintain flat positioning x 72 hours – Foley catheter x 72 hours – Transferred from PICU, now POD 4 – Called for fever of 39. 1˚C – Mild abdominal tenderness, diminished in bilateral lower lobes, otherwise well-appearing
Case 3 Which of the following is the most likely source of her fever? A. B. C. D. E. Pneumonia Atelectasis UTI Wound infection Drug fever Click forward to see the answer and hear the explanation
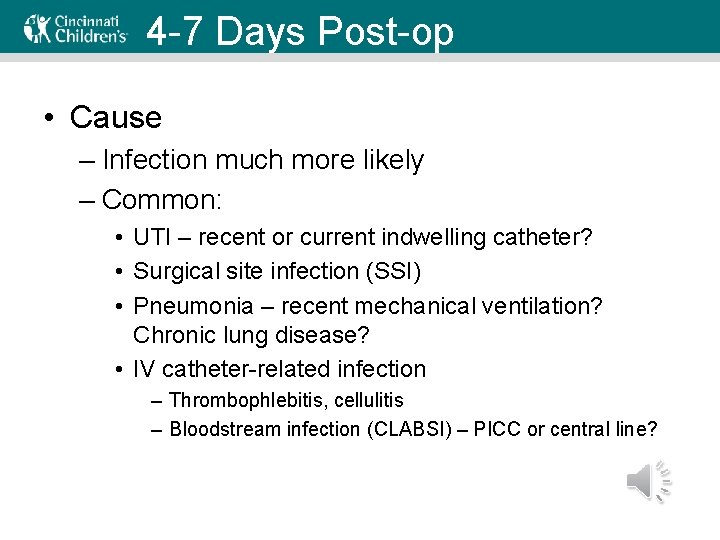
4 -7 Days Post-op • Cause – Infection much more likely – Common: • UTI – recent or current indwelling catheter? • Surgical site infection (SSI) • Pneumonia – recent mechanical ventilation? Chronic lung disease? • IV catheter-related infection – Thrombophlebitis, cellulitis – Bloodstream infection (CLABSI) – PICC or central line?
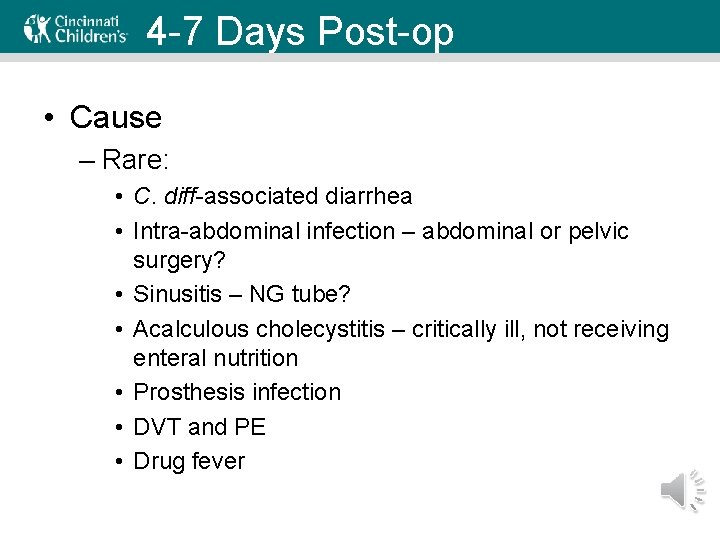
4 -7 Days Post-op • Cause – Rare: • C. diff-associated diarrhea • Intra-abdominal infection – abdominal or pelvic surgery? • Sinusitis – NG tube? • Acalculous cholecystitis – critically ill, not receiving enteral nutrition • Prosthesis infection • DVT and PE • Drug fever
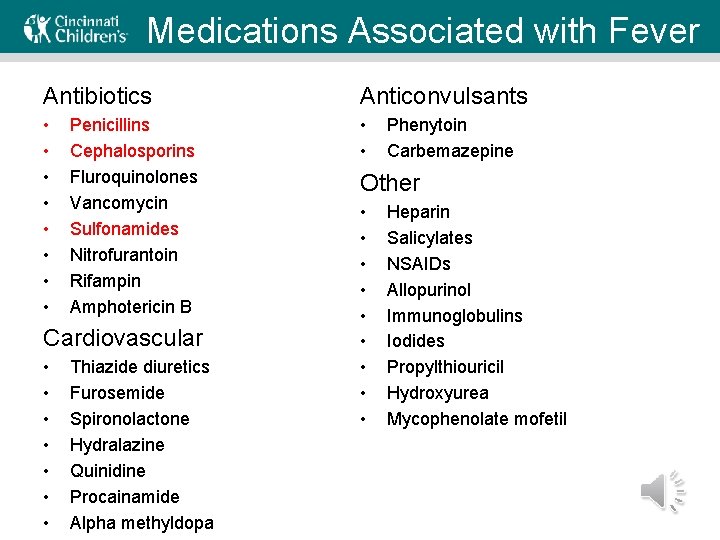
Medications Associated with Fever Antibiotics Anticonvulsants • • • Penicillins Cephalosporins Fluroquinolones Vancomycin Sulfonamides Nitrofurantoin Rifampin Amphotericin B Cardiovascular • • Thiazide diuretics Furosemide Spironolactone Hydralazine Quinidine Procainamide Alpha methyldopa Phenytoin Carbemazepine Other • • • Heparin Salicylates NSAIDs Allopurinol Immunoglobulins Iodides Propylthiouricil Hydroxyurea Mycophenolate mofetil
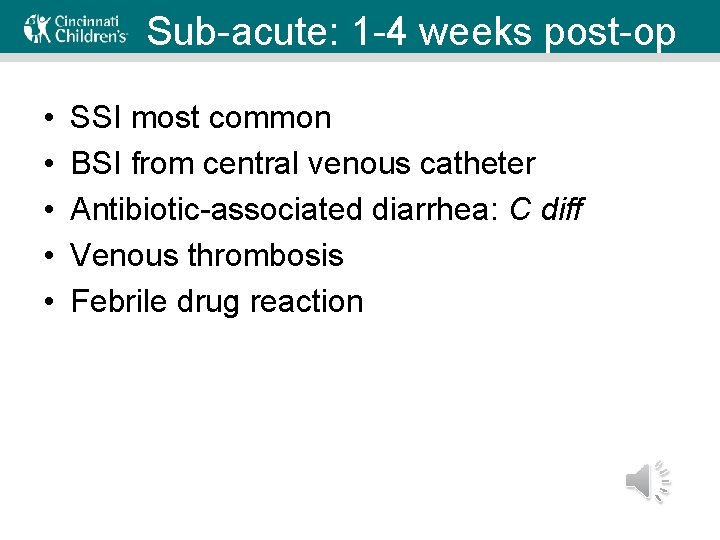
Sub-acute: 1 -4 weeks post-op • • • SSI most common BSI from central venous catheter Antibiotic-associated diarrhea: C diff Venous thrombosis Febrile drug reaction
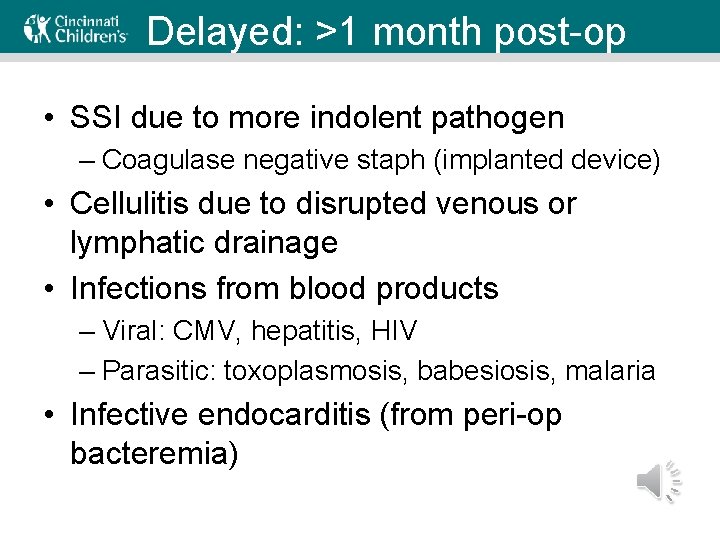
Delayed: >1 month post-op • SSI due to more indolent pathogen – Coagulase negative staph (implanted device) • Cellulitis due to disrupted venous or lymphatic drainage • Infections from blood products – Viral: CMV, hepatitis, HIV – Parasitic: toxoplasmosis, babesiosis, malaria • Infective endocarditis (from peri-op bacteremia)
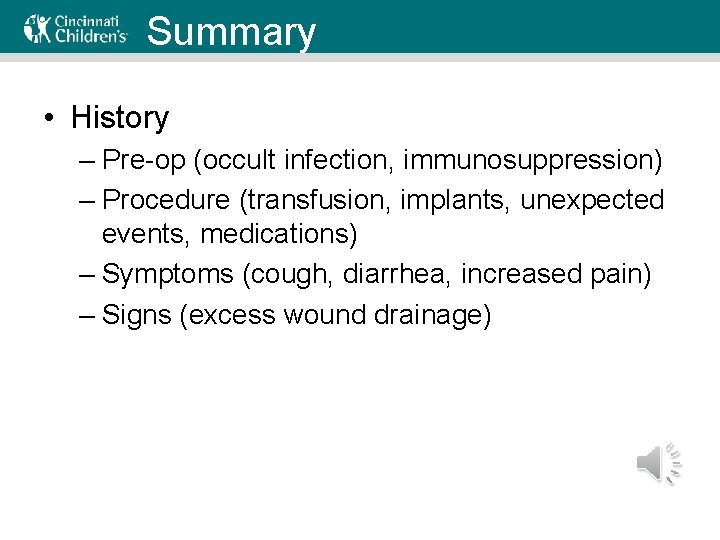
Summary • History – Pre-op (occult infection, immunosuppression) – Procedure (transfusion, implants, unexpected events, medications) – Symptoms (cough, diarrhea, increased pain) – Signs (excess wound drainage)
Summary • Physical Exam – Vitals: look at trends – Heart and lungs – Wound: dressing and palpation. Do not remove dressing without talking to surgeon – Catheter sites – Other wounds/lesions – Extremity swelling/pain
Summary • Work-up – First 48 hr • Sparingly • Blood culture if extra concern (appear septic, central line, immunosuppressed, obvious wound infection) – After 48 hr • Based on history, symptoms, exam findings
The Five W’s and More • Wind – Pneumonia, aspiration (not atelectasis) • Water – UTI • Wound – SSI (surgical site infection) • Walk – DVT, PE • What did we do? – Drug fever, CLABSI (PICC? CVC? ), C diff (abxassoc diarrhea), transfusion reaction
Key Points • Although rare, fever may signify serious complications • Assess the patient with targeted history and physical exam to guide further evaluation • Timing of fever onset can be helpful in determining cause
Questions for Review • Provide a cause of post-op fever in the immediate, acute, sub-acute and delayed time periods. • When is a patient most likely to have a fever due to a surgical site infection?
Further Discussion • You have just been consulted on a patient who is post-op day 3 with fever for the past 3 days. The primary team feels the fever is most likely due to atelectasis. How would you discuss your recommendations for further evaluation with team?
Sources • Engoren M. (1995) Lack of association between atelectasis and fever. Chest. Jan: 107 (1): 81 -4. • Garibaldi RA et al (1985). Evidence for the non-infectious etiology of early post operative fever. Infection Control. July: 6 (7): 273 -7. • Harrison, G. W. (2014). Postoperative fever. In H. Sanfey (Ed. ), Up. To. Date. Retrieved from http: //www. uptodate. com • Mavros, M. N. , Velmahos, G. C. , & Falagas, M. E. (2011). Atelectasis as a cause of postoperative fever: where is the clinical evidence? . CHEST Journal, 140(2), 418 -424. • Pile, J. C. (2006). Evaluating postoperative fever: a focused approach. Cleveland Clinic journal of medicine, 73(Suppl 1), S 62. • Shaw JA and Chung R. (1999). Febrile response after knee and hip arthroplasty. Clin Orthop Relat Res. Oct: (367): 181 -9.
- Slides: 29