Postoperative care Post Anesthesia Care Unit PACU PACU





- Slides: 34
Postoperative care Post Anesthesia Care Unit “PACU”
PACU • Design should match function • Location: • Close to the operating suite. • Access to x-ray, blood bank & clinical labs. • Monitoring equipment • Emergency equipment • Personnel
Admission to PACU • Coordinate prior to arrival, • Assess airway, • Administer oxygen, • Apply monitors, • Obtain vital signs, • Receive report from anesthesia personnel.
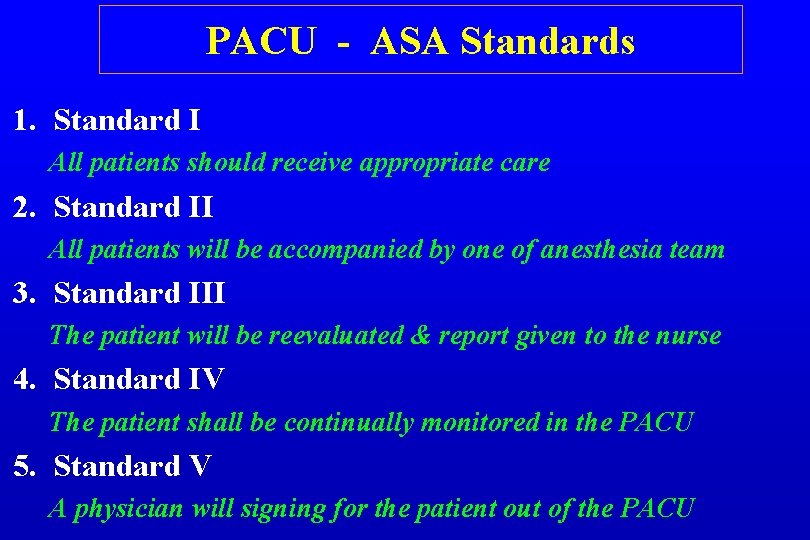
PACU - ASA Standards 1. Standard I All patients should receive appropriate care 2. Standard II All patients will be accompanied by one of anesthesia team 3. Standard III The patient will be reevaluated & report given to the nurse 4. Standard IV The patient shall be continually monitored in the PACU 5. Standard V A physician will signing for the patient out of the PACU
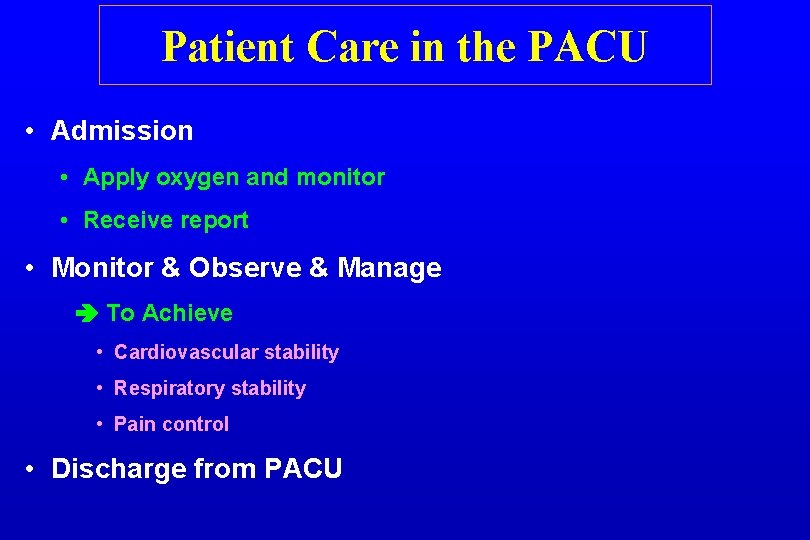
Patient Care in the PACU • Admission • Apply oxygen and monitor • Receive report • Monitor & Observe & Manage To Achieve • Cardiovascular stability • Respiratory stability • Pain control • Discharge from PACU
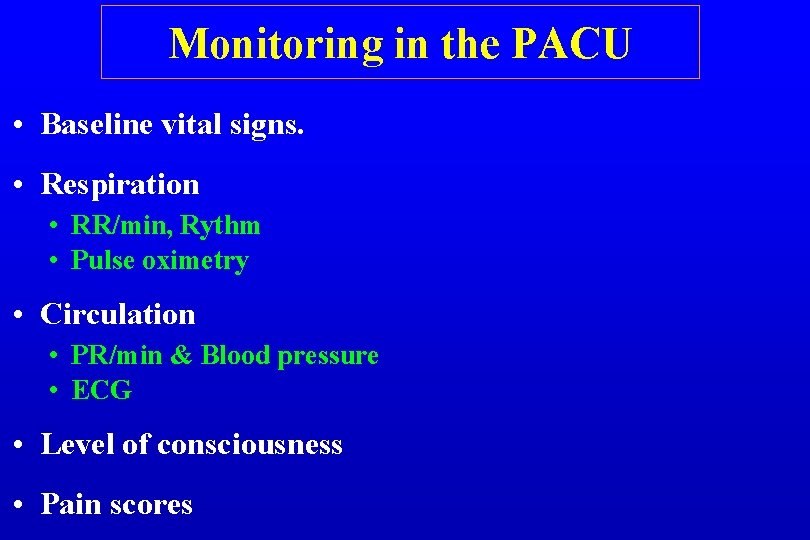
Monitoring in the PACU • Baseline vital signs. • Respiration • RR/min, Rythm • Pulse oximetry • Circulation • PR/min & Blood pressure • ECG • Level of consciousness • Pain scores
Initial Assessment 1. Color 2. Respiration 3. Circulation 4. Consciousness 5. Activity
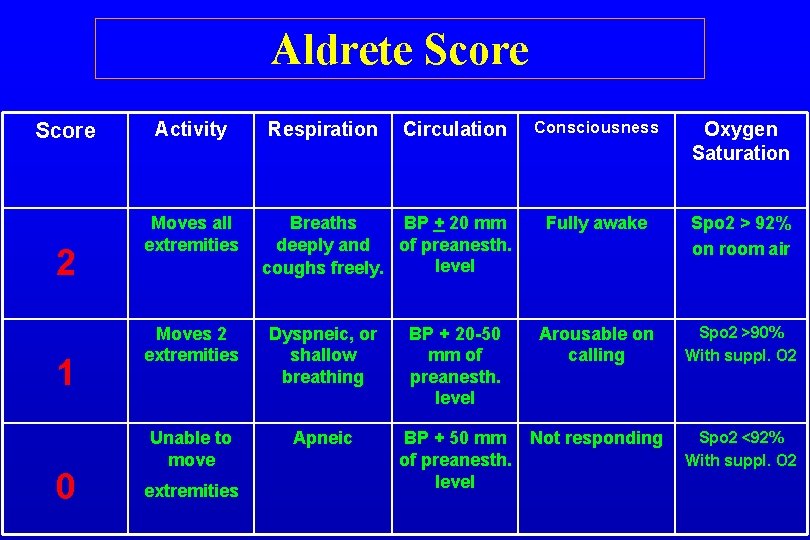
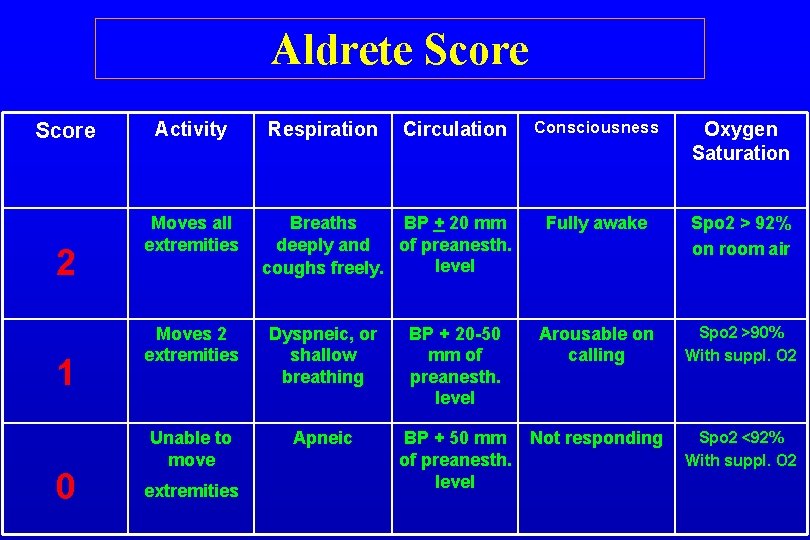
Aldrete Score 2 1 0 Activity Moves all extremities Respiration Circulation Breaths BP + 20 mm deeply and of preanesth. level coughs freely. Consciousness Oxygen Saturation Fully awake Spo 2 > 92% on room air Moves 2 extremities Dyspneic, or shallow breathing BP + 20 -50 mm of preanesth. level Arousable on calling Spo 2 >90% With suppl. O 2 Unable to move Apneic BP + 50 mm of preanesth. level Not responding Spo 2 <92% With suppl. O 2 extremities
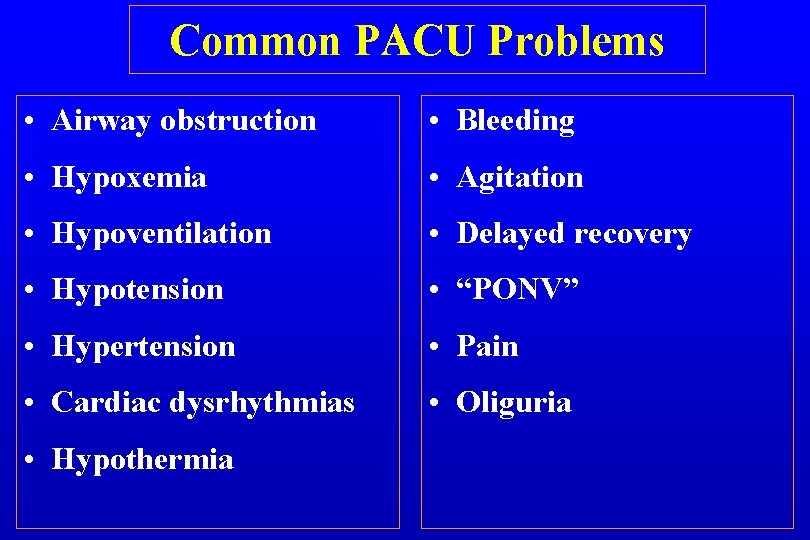
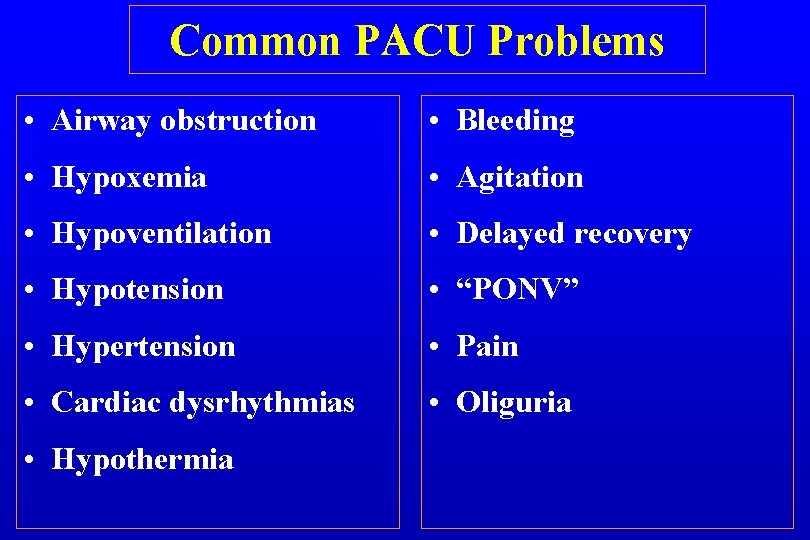
Common PACU Problems • Airway obstruction • Bleeding • Hypoxemia • Agitation • Hypoventilation • Delayed recovery • Hypotension • “PONV” • Hypertension • Pain • Cardiac dysrhythmias • Oliguria • Hypothermia
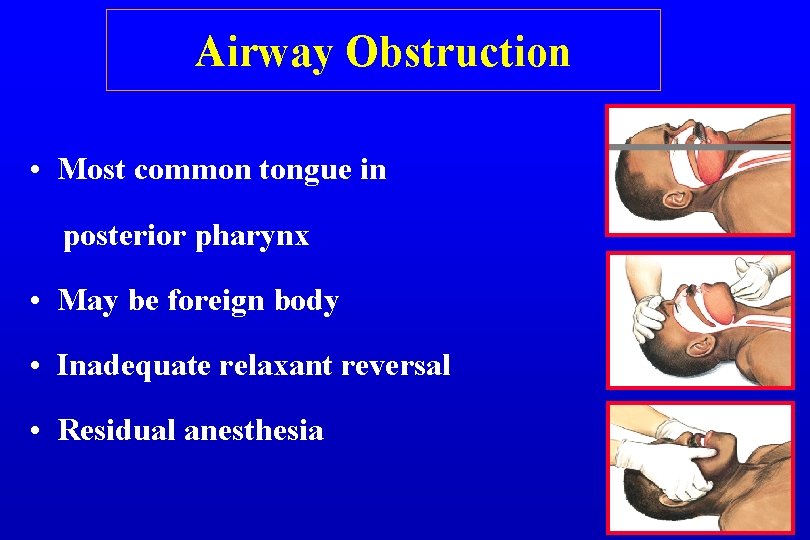
Airway Obstruction • Most common tongue in posterior pharynx • May be foreign body • Inadequate relaxant reversal • Residual anesthesia
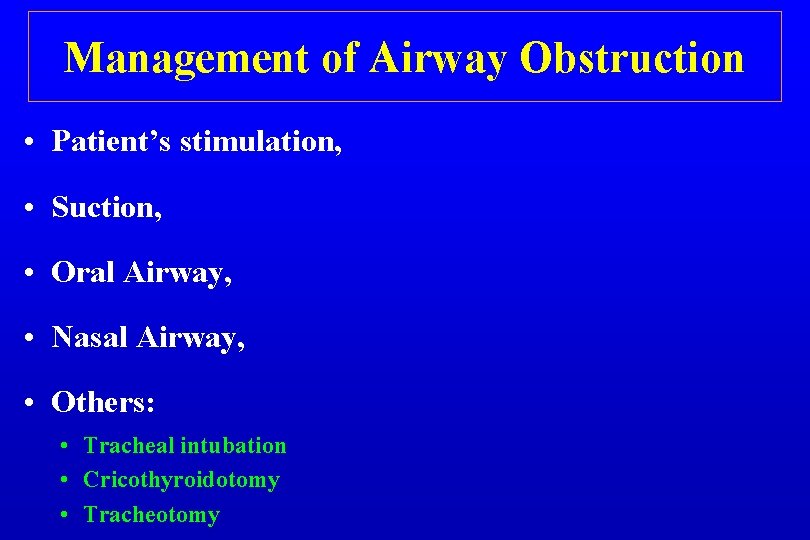
Management of Airway Obstruction • Patient’s stimulation, • Suction, • Oral Airway, • Nasal Airway, • Others: • Tracheal intubation • Cricothyroidotomy • Tracheotomy
Hypoventilation • Residual anesthesia • Narcotics • Inhalation agent • Residual Relaxant • Post oper - Analgesia • Intravenous • Epidural

Hypoventilation Treatment • Close observation, • Assess the problem, • Treatment of the cause: • Reverse relaxant • Reverse narcotic • Reverse midazolam
Hypertension • Common causes: e. g. • Pain • Full Bladder • Hypertensive patients • Fluid overload • Excessive use of vasopressors
Hypertension Treatment • Effective pain control • Sedation • Anti-hypertensives: • • Beta blockers Alpha blockers Hydralazine (Apresoline) Calcium channel blockers

Hypotension • Decreased venous return • Hypovolemia, • fluid intake • losses • Bleeding • Sympathectomy, • 3 rd space loss, • Left ventricular dysfunction
Treatment of Hypotension • Initially treat with fluid bolus, • + Vasopressors, • + Correction of the cause
Dysrhythmias • Secondary to • hypoxemia • hypercarbia • Acidosis • Catecholamines • Electrolyte abnormalities • Hypothermia
Dysrhythmia Treatment • Identify and treat the cause, • Assure oxygenation, • Pharmacological

Urine Output • Oliguria • • Hypovolemia, Surgical trauma, Impaired renal function, Mechanical blocking of catheter. • Treatment: • Assess catheter patency • Fluid bolus • Diuretics e. g. Lasix
Post op Bleeding Causes: • Usually surgical problem • Coagulopathy Treatment: • Start i. v. lines push fluids • Blood sample, - Cross matching, CBC, - Coagulopathy • Notify the surgeon, • Correction of the cause
Hypothermia • Most of patients will arrive cold • Treatment: • Get baseline temperature • Actively rewarm • Administer oxygen if shivering • Take care for: • Pediatric, • Geriatric.

Altered Mental Status • Reaction to drugs? • Drugs e. g. sedatives, anticholinergics • Intoxication / Drug abusers • • • Pain Full bladder Hypoventilation Low COP CVA
Treatment of Altered Mental Status • Reassurances, • Always protect the patient, • Evaluate the cause, • Treatment of symptoms, • Sedatives / Opioids if necessary.
Delayed Recovery • Systematic evaluation • Pre-op status • Intraoperative events • Ventilation • Response to Stimulation • Cardiovascular status
Delayed Recovery • The most common cause: • Residual anesthesia Consider reversal • Hypothermia, • Metabolic e. g. diabetic coma, • Underlying psychiatric problem • CVA
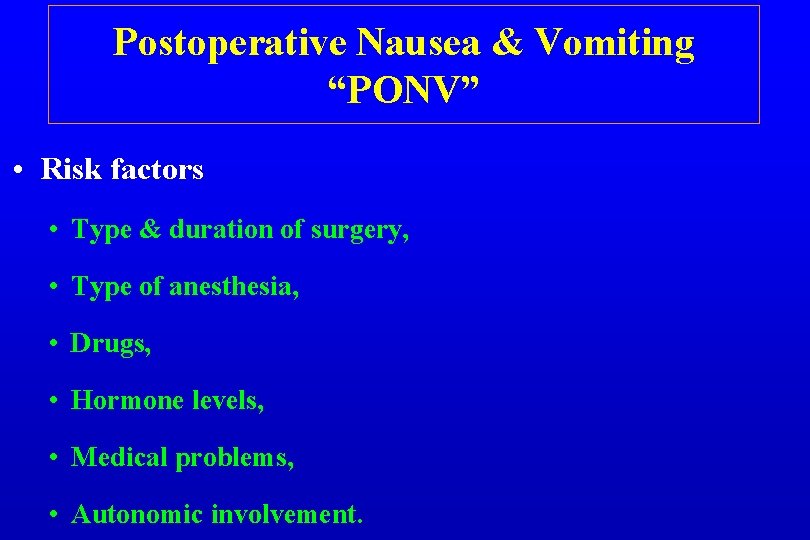
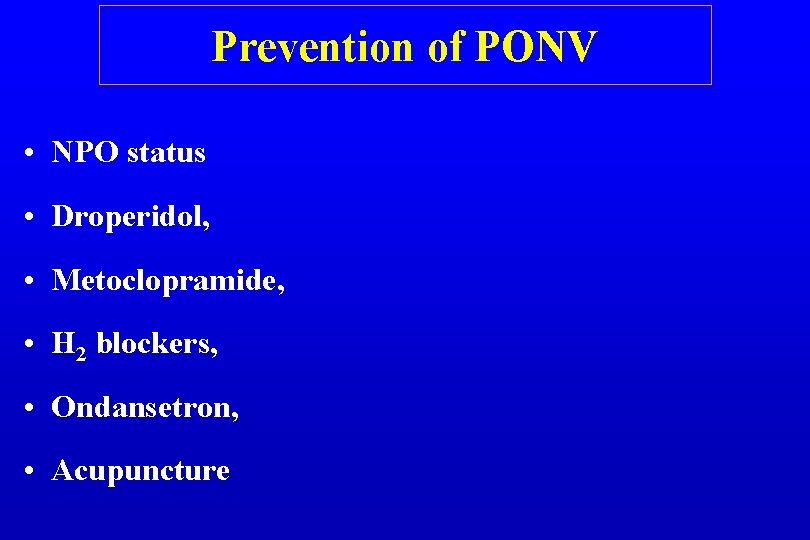
Postoperative Nausea & Vomiting “PONV” • Risk factors • Type & duration of surgery, • Type of anesthesia, • Drugs, • Hormone levels, • Medical problems, • Autonomic involvement.
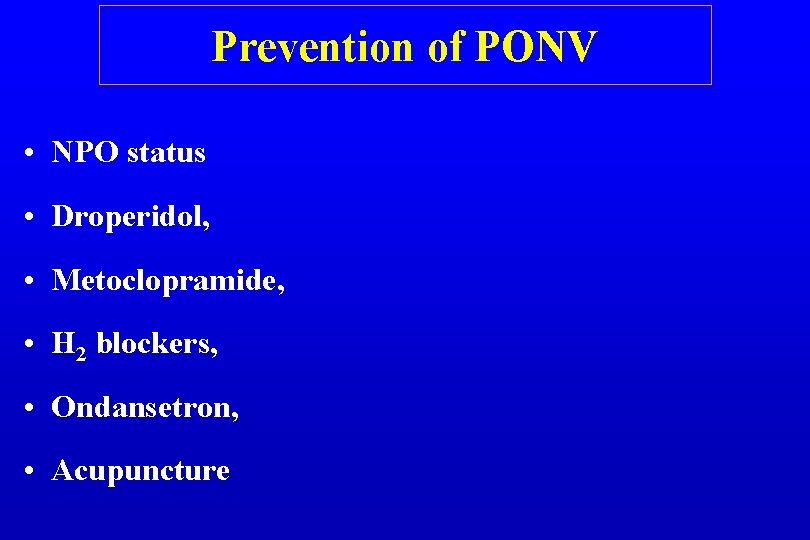
Prevention of PONV • NPO status • Droperidol, • Metoclopramide, • H 2 blockers, • Ondansetron, • Acupuncture
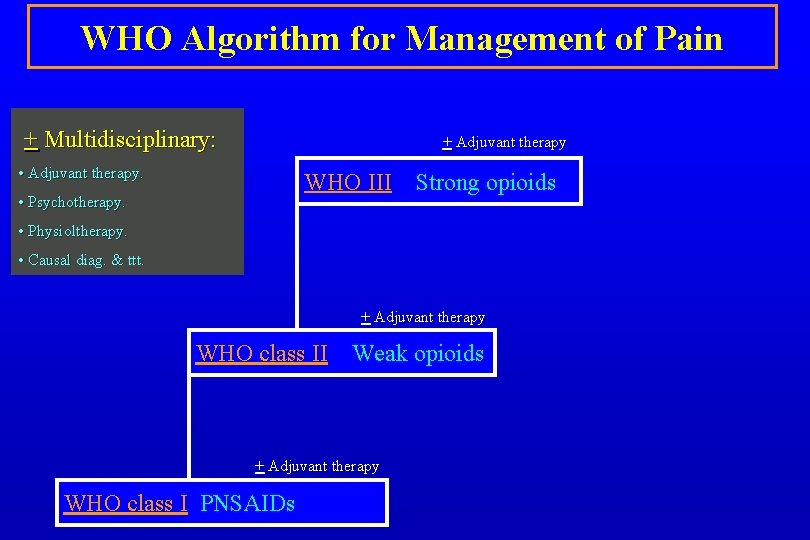
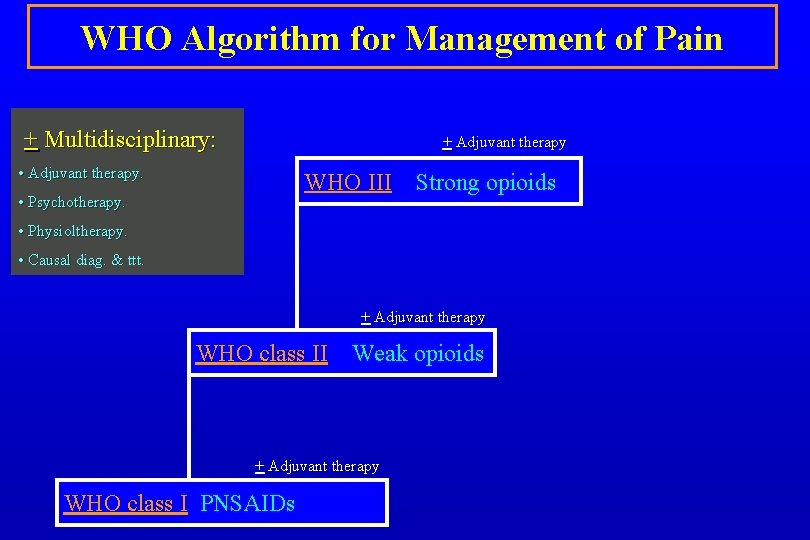
WHO Algorithm for Management of Pain + Multidisciplinary: + Adjuvant therapy • Adjuvant therapy. WHO III • Psychotherapy. Strong opioids • Physioltherapy. • Causal diag. & ttt. + Adjuvant therapy WHO class II Weak opioids + Adjuvant therapy WHO class I PNSAIDs
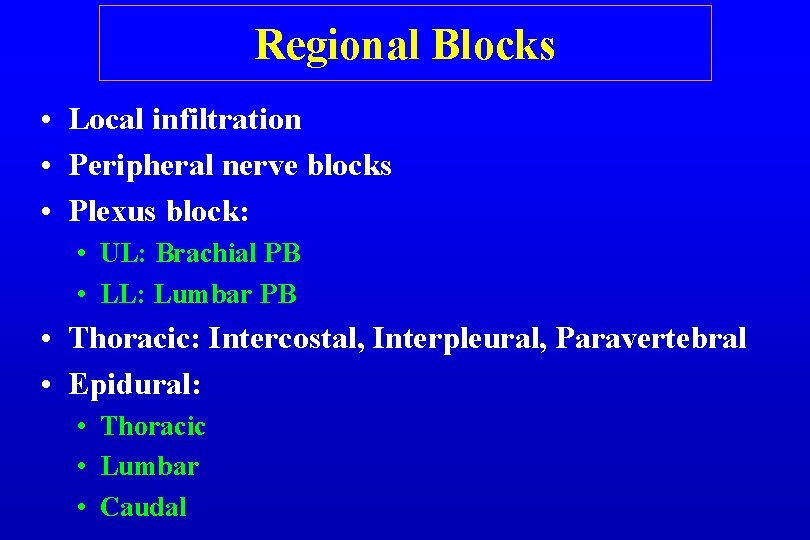
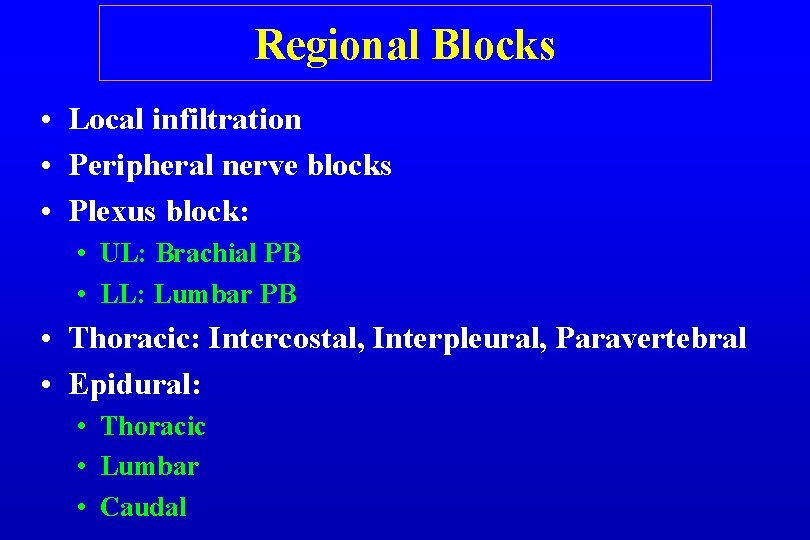
Regional Blocks • Local infiltration • Peripheral nerve blocks • Plexus block: • UL: Brachial PB • LL: Lumbar PB • Thoracic: Intercostal, Interpleural, Paravertebral • Epidural: • Thoracic • Lumbar • Caudal
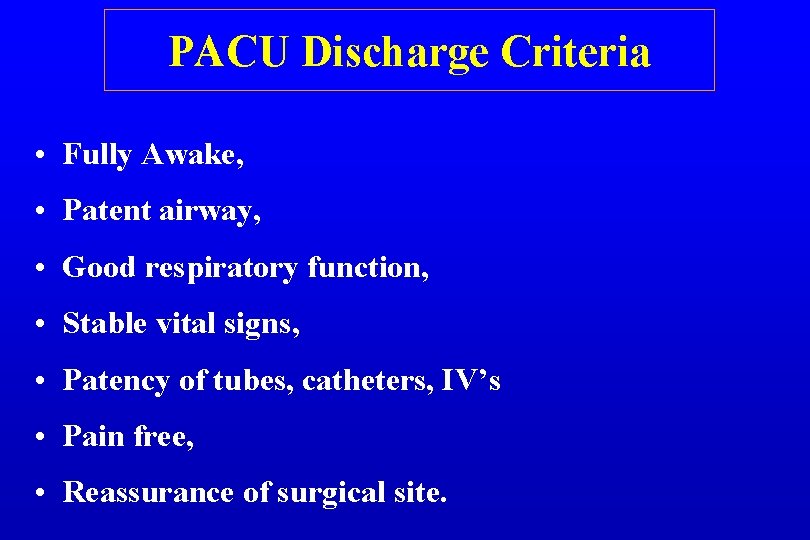
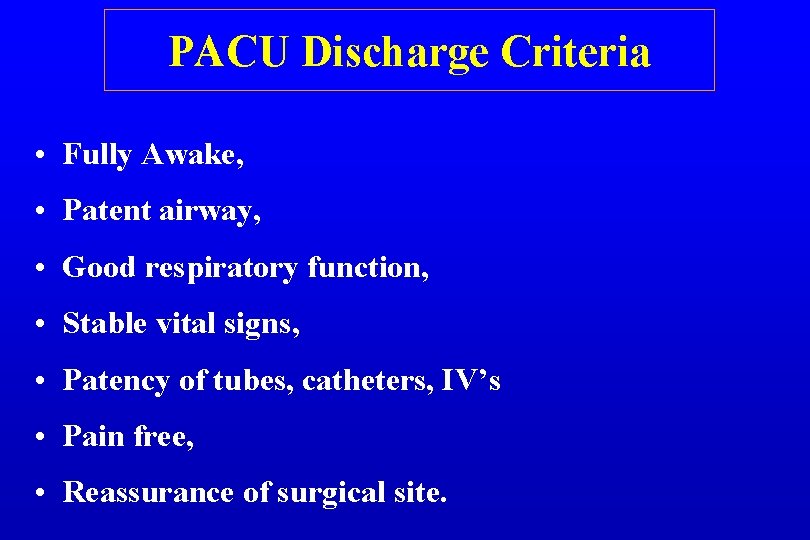
PACU Discharge Criteria • Fully Awake, • Patent airway, • Good respiratory function, • Stable vital signs, • Patency of tubes, catheters, IV’s • Pain free, • Reassurance of surgical site.
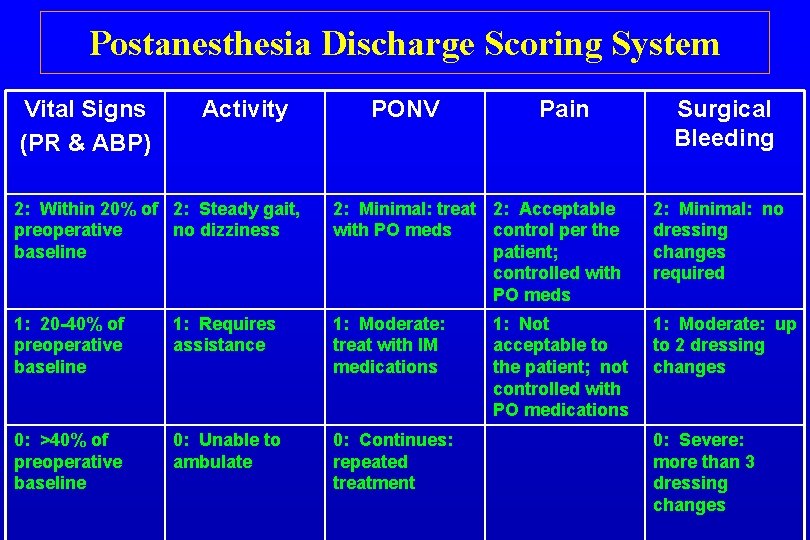
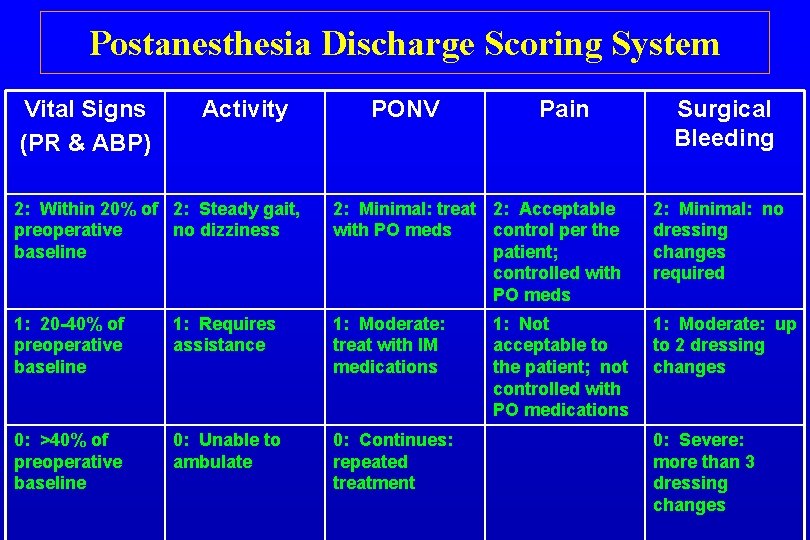
Postanesthesia Discharge Scoring System Vital Signs (PR & ABP) Activity PONV Pain Surgical Bleeding 2: Within 20% of 2: Steady gait, preoperative no dizziness baseline 2: Minimal: treat 2: Acceptable with PO meds control per the patient; controlled with PO meds 2: Minimal: no dressing changes required 1: 20 -40% of preoperative baseline 1: Requires assistance 1: Moderate: treat with IM medications 1: Moderate: up to 2 dressing changes 0: >40% of preoperative baseline 0: Unable to ambulate 0: Continues: repeated treatment 1: Not acceptable to the patient; not controlled with PO medications 0: Severe: more than 3 dressing changes

Post-operative Care “PACU” Thank You