Postoperative Care 1 Care in the PACU PACU


- Slides: 65

Postoperative Care 1
Care in the PACU • PACU nurse receives report from OR • • • General info (name, age, surgery, etc) Medical History Intra-operative Course &Management (meds, blood loss, fluids given, unexpected events, V/S, lab tests/results) • PACU Plan 2
Care in the PACU • Priorities in PACU • ABC! • Assess and manage respiratory and circulatory function • Pain management • Temperature • Surgical site 3
Care in the PACU: Initial Assessment • Respiratory Assessment • Airway, breathing, auscultate, oxygen Cardiovascular Assessment • Neurological Assessment 4
Initial Assessments cont’d in PACU • Urinary assessment • Wound assessment 5
Potential Alterations in Respiratory Function • Airway obstruction (tongue!, laryngospasm, laryngeal edema) • • • Hypoxemia (Sa. O 2 < 90%; agitation → somnolence) Atelectasis (alveolar collapse) Pulmonary edema (fluid-filled alveoli) Aspiration of gastric secretions Bronchospasm Hypoventilation 6
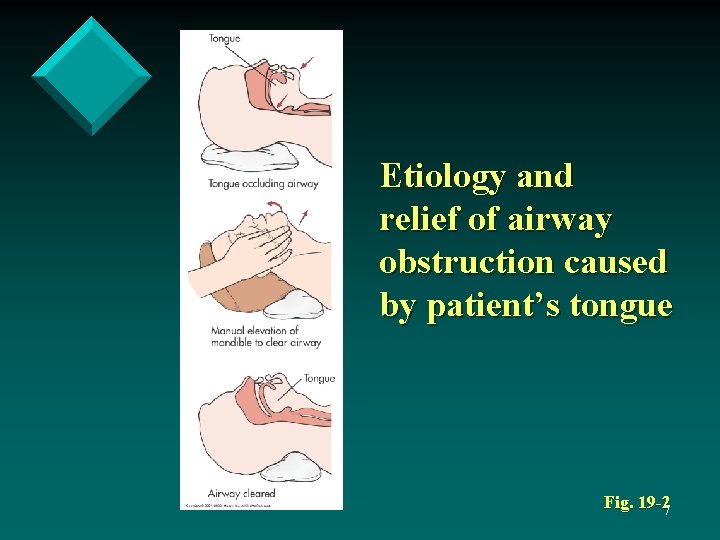
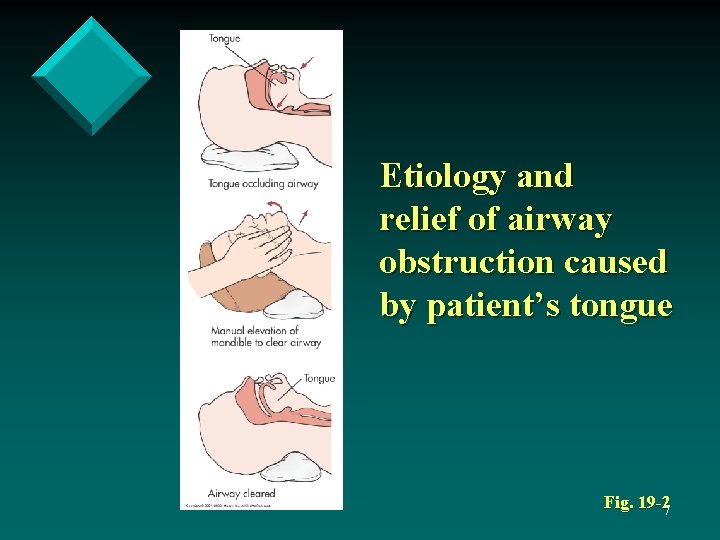
Etiology and relief of airway obstruction caused by patient’s tongue Fig. 19 -27

Nursing Management Respiratory Complications • Nursing Diagnoses • • • Ineffective airway clearance Ineffective breathing pattern Impaired gas exchange Risk for aspiration Potential complication: hypoxemia 8
Nursing Management Respiratory Complications • Nursing Implementation • • • Positioning (lateral recovery) DB & C Oxygen therapy as appropriate Physiotherapy Suctioning 9
Potential Complications in Cardiovascular Function Most common complications • • • Hypotension Hypertension Dysrhythmia Greatest risk: • Cardiac history • Elderly • Debilitated or critically ill 10
Potential Complications in Cardiovascular Function • Hypotension • Indications? • Causes? • Hypertension (r/t pain, anxiety, bladder distension, hx of HTN, hypothermia) • Dysrhythmia 11
Potential Complications in Cardiovascular Function 12
Nursing Management Cardiovascular Complications • Nursing Assessment • V/S Q 15 minute or more often until stable, then less frequent (compare with what? ) • Skin color, temp, LOC • Notify if : • SBP < 90 or > 160 • HR < 60 or > 120 • Narrowing pulse pressure (SBP-DBP) • Dysrhythmia (irregular heart rhythm) • Change from pre-op 13
Nursing Management Cardiovascular Complications • Nursing Diagnoses • • • Decreased cardiac output Deficient fluid volume Ineffective tissue perfusion Excess fluid volume Potential complication: hypovolemic shock 14
Nursing Management Cardiovascular Complications • Nursing Implementation • • • Oxygen and fluid for hypotension Dysrhythmias – medications, tx cause HTN – treat cause (pain, anxiety, etc. ) 15
Nursing Management Neurologic Complications • Nursing Assessments • LOC, orientation, ability to follow commands • Pupils • Sensory and motor status 16
Nursing Management Neurologic Complications • Nursing Diagnoses • • Disturbed sensory perception Risk for injury Disturbed thought processes Impaired verbal communication 17
Nursing Management Neurologic Complications • Agitation • • • Hypoxemia is most common cause Oxygen therapy Protect the client 18
Pain and Discomfort • • Assessment Nursing Diagnoses • Acute pain • Anxiety • Nursing Implementation 19
Nursing Management • • Hypothermia (T < 36°) Nausea and Vomiting 20
Care of Postoperative Patient on Clinical Unit • • PACU nurse gives report to receiving nurse summarizing operative and postoperative periods Vital signs obtained and compared to report 21
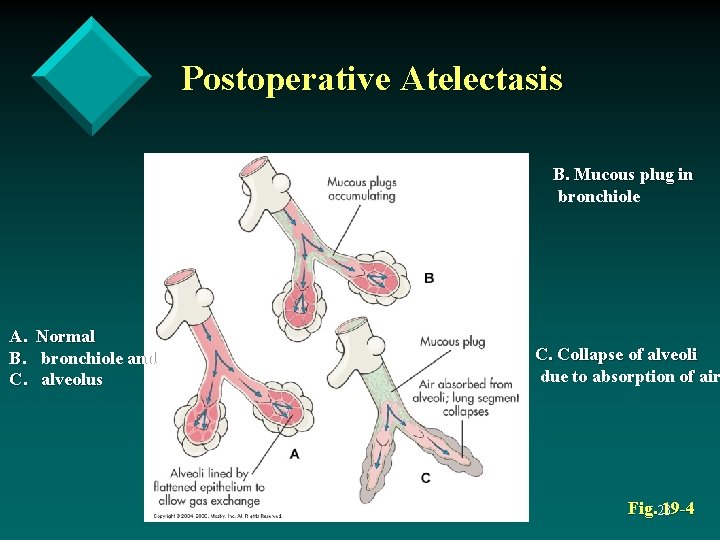
Potential Complications in Respiratory Function • Atelectasis and pneumonia common after abdominal and thoracic surgery 22
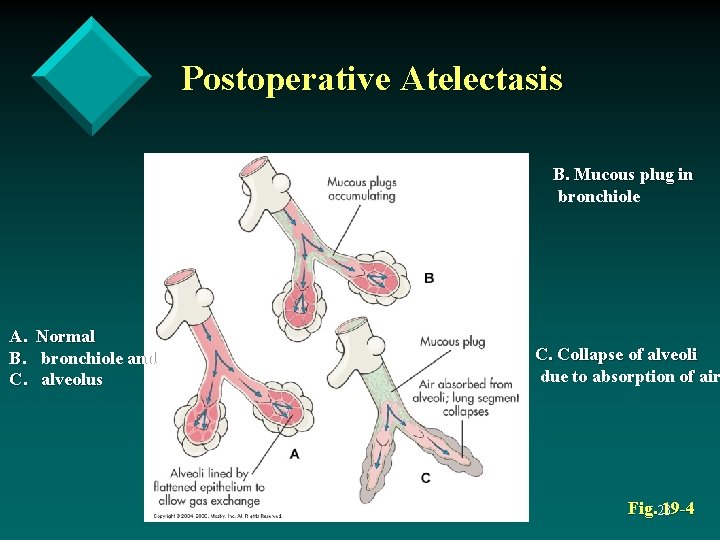
Postoperative Atelectasis B. Mucous plug in bronchiole A. B. C. Normal bronchiole and alveolus C. Collapse of alveoli due to absorption of air Fig. 23 19 -4
Potential Complications in Respiratory Function • Nursing Diagnoses • • • Ineffective airway clearance Ineffective breathing pattern Impaired gas exchange Potential complication: pneumonia Potential complication: atelectasis 24
Potential Complications in Respiratory Function • Nursing Implementation • • DB & C Incentive spirometer Splinting Diaphragmatic breathing (in through nose; out through mouth) • • Change position q 2 h Ambulation ASAP Pain Management Adequate hydration 25
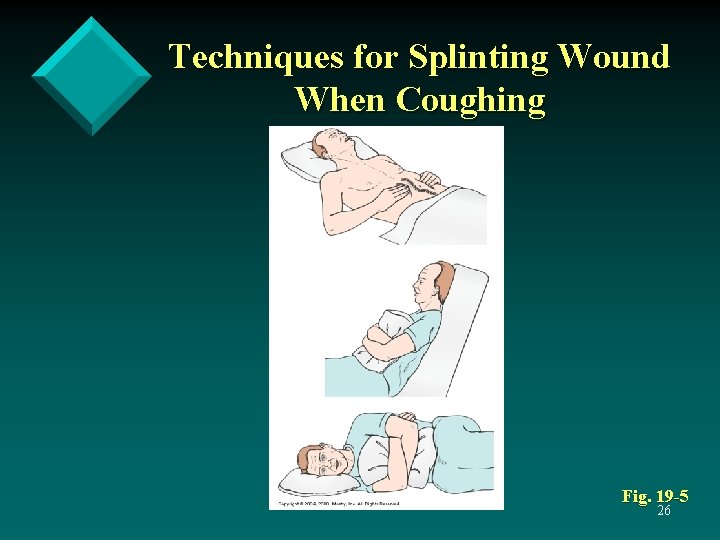
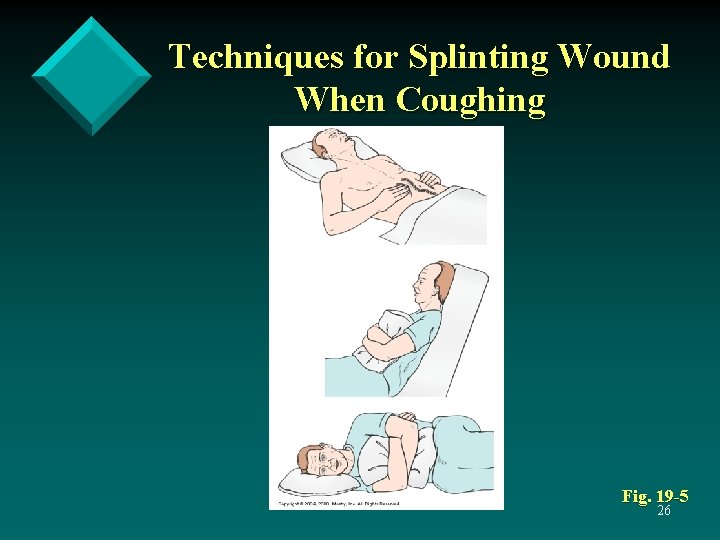
Techniques for Splinting Wound When Coughing Fig. 19 -5 26
Potential Alterations in Cardiovascular Function • Fluid and electrolyte imbalances contribute to alterations in CV fxn • Stress response post-op → retention • (ADH and aldosterone) • Too much/too fast IV fluid • Renal or cardiac disease 27
Potential Alterations in Cardiovascular Function • Deep vein thrombosis (DVT) • Most common in older adults, obese patients, immobilized patients • DVT → Pulmonary embolus (potentially fatal) • S/S: chest pain, tachypnea, tachycardia, hypotension, hemoptysis, dysrhythmias 28
Nursing Management Cardiovascular Complications • Nursing Assessment • Regular monitoring of BP, HR, pulse, and skin temperature and color • Compare preoperative and postoperative findings 29
Nursing Management Cardiovascular Complications • Nursing Diagnoses • • • Decreased cardiac output Deficient fluid volume Excess fluid volume Ineffective tissue perfusion Activity intolerance Potential complication: thromboembolism 30
Nursing Management Cardiovascular Complications • Nursing Implementation • Accurate I&Os • Monitor laboratory findings (lytes, CBC) • Assessment of infusion rate 31
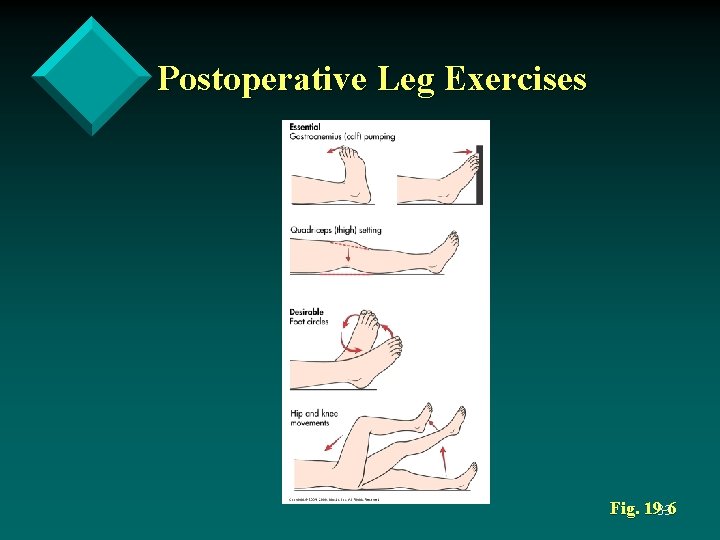
Nursing Management Cardiovascular Complications • DVT prophylaxis • • • Leg exercise (10 -12/Q 1 -2 hr) Elastic stockings Sequential compression devices Anticoagulants (Heparin, LMWH) Early ambulation • Slowly progress • Monitor pulse • Assess for feelings of faintness 32
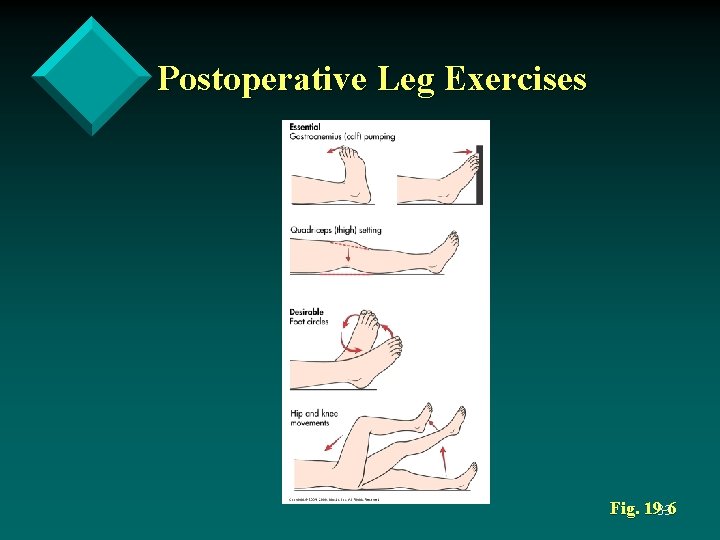
Postoperative Leg Exercises Fig. 19 -6 33
Potential Alterations in Urinary Function • • Low urinary output (800 – 1500 ml) may be expected in the first 24 hours, regardless of intake Urinary retention 34
Nursing Management Urinary Complications • Nursing Assessment • Urine examined for quantity and quality • Note color, amount, consistency, and odor • Assess indwelling catheters for patency • Urine output should be at least 0. 5 ml/kg per hour or 30 cc/hr. 35
Nursing Management Urinary Complications • Nursing Diagnoses • Impaired urinary elimination • Potential complication: acute urinary retention 36
Nursing Management Urinary Complications • Nursing Implementation • • • Position patient for normal voiding Reassure patient of ability to void Use techniques such as running water, drinking water, pouring water over perineum, ambulation, or use of bedside commode 37
Potential Alterations in Gastrointestinal Function • • Nausea and vomiting may be caused from anesthetic agents or narcotics, delayed gastric emptying, slowed peristalsis, resumption of oral intake too soon after surgery Abdominal distention from decreased peristalsis caused by handling of bowel during surgery 38
Potential Alterations in Gastrointestinal Function • • Swallowed air and GI secretions may accumulate in colon, producing distention and gas pains Hiccoughs from irritation of phrenic nerve 39
Nursing Management Gastrointestinal Complications • Nursing Assessment • Auscultate abdomen in all four quadrants for presence, frequency, and characteristics of bowel sounds • Can be absent or diminished in immediate postoperative period • Looking for return of bowel motility accompanied by flatus 40
Potential Alterations in Gastrointestinal Function • Nursing Diagnoses • Nausea • Imbalanced nutrition: less than body requirements • Potential complication: paralytic ileus • Potential complication: hiccoughs 41
Potential Alterations in Gastrointestinal Function • Nursing Implementation • May resume intake upon return of gag reflex • NPO until return of bowel sounds for patient with abdominal surgery • IVF, NG for decompression • Clear liquids, advance as tolerated 42
Potential Alterations in Gastrointestinal Function • Nursing Implementation • Regular mouth care when NPO • Antiemetics administered for nausea • NG tube if symptoms persist • Early and frequent ambulation to prevent abdominal distention • Assess patient regularly for resumption of normal peristalsis 43
Potential Alterations in Gastrointestinal Function • Nursing Implementation • Encourage patient to expel flatus and explain expulsion is necessary and desirable • Relief of gas pains by frequent ambulation and repositioning • Suppositories prn • Determine cause of hiccoughs 44
Nursing Management Surgical Wounds • Nursing Assessment • Knowledge of type of wound, drains, and expected drainage • Drainage should change from sanguineous to serous with decreasing output 45
Potential Alterations of the Integument • Nursing Diagnoses • Risk for infection • Potential complication: impaired wound healing 46
Potential Alterations of the Integument • Nursing Implementation • Note type, amount, color, and consistency of drainage • Assess affect of position changes on drainage 47
Potential Alterations of the Integument • Notify surgeon of excessive or abnormal drainage and significant changes in vitals • Note number and type of drains when changing dressing • Examine incision site • Clean gloves and sterile technique 48
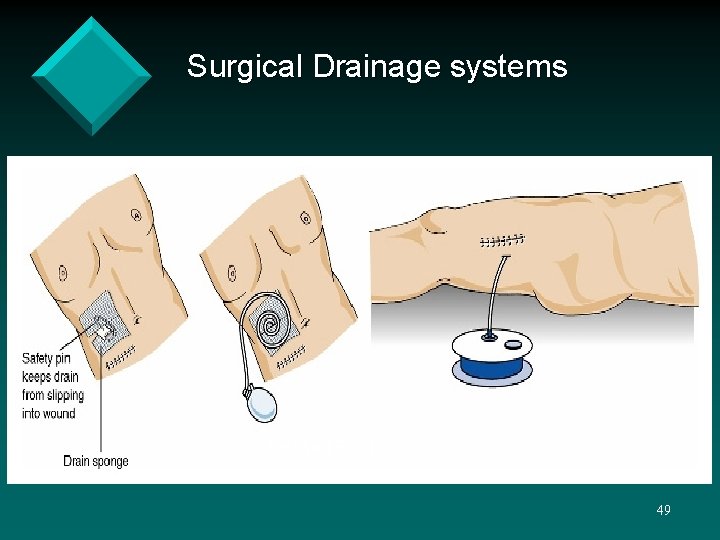
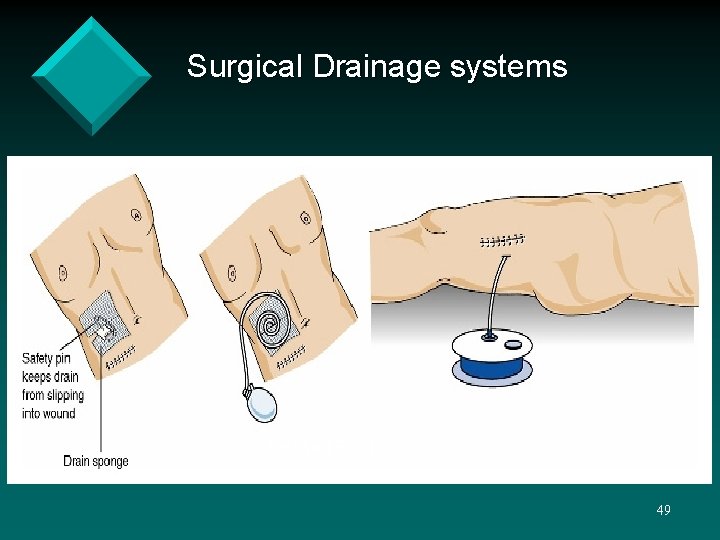
Surgical Drainage systems Jackson Pratt 49
Potential Alterations of the Integument • • • Incision disrupts skin barrier and healing is major concern during postoperative period Adequate nutrition impt for healing Impaired wound healing with chronic disease and elderly 50
Potential Alterations of the Integument • Infection • Evidence of wound infection usually not apparent until 3 rd to 5 th postoperative day • Local manifestations: redness, edema, pain, and tenderness, purulent drainage • Systemic manifestations: fever, leukocytosis (↑ WBCs) 51
Complications of Wound Healing • Dehiscence • Separation and disruption of previously joined wound edges (incision bursts open) • Treatment: keep clean, use packing or dressings; allow to heal 52
Complications of Wound Healing • Evisceration – wound edges separate such that intestines protrude through wound • • • A medical emergency Generally between 5 -10 days post-op At-risk patients: obese, excessive coughing, vomiting, straining, failure to splint 53
Complications of Wound Healing • Evisceration • • Notify MD immediately Monitor V/S closely May decompress with NGT Prepare for surgery 54
Pain and Discomfort • Postoperative pain caused by a number of physiologic and psychologic interactions • • • Traumatization of skin and tissues Reflex muscle spasms Anxiety/fear increase muscle tone and spasm 55
Nursing Management Pain • • Nursing Assessment Nursing Diagnoses • Acute pain • Disturbed sensory perception • Nursing Implementation 56
Potential Alterations in Temperature • • Hypothermia may be present in immediate postoperative period Fever may occur at any time • Mild elevation (up to 38 degrees C) may result from stress response • Moderate elevation (>38° C) usually caused by respiratory congestion or atelectasis and rarely by dehydration 57
Potential Alterations in Temperature • • Wound infection often accompanied by fever spiking in afternoon and near-normal in morning Intermittent high fever with shaking chills and diaphoresis indicates septicemia 58
Nursing Management Altered Temperature • • Nursing Assessment Nursing Diagnoses • • • Risk for imbalanced body temperature Hyperthermia Hypothermia 59
Nursing Management Altered Temperature • Nursing Implementation • Measure temperature q 4 h for first 48 hours postoperatively • Asepsis with wound and IV sites • Encourage airway clearance • Chest x-rays and cultures if infection suspected • Antipyretics and body-cooling >39. 4° C 60
Potential Alterations in Psychologic Function • • Anxiety and depression may be more pronounced with radical surgery or with poor prognosis Confusion and delirium may result from psychologic and physiologic sources 61
Nursing Management Psychologic Function • Nursing Diagnoses • • Anxiety Ineffective coping Disturbed body image Decisional conflict 62
Nursing Management Psychologic Function • Nursing Implementation • Provide adequate support • Listen and talk with patient, offer explanations, reassure, and encourage involvement of significant other • Discuss expectation of activity and assistance needed after discharge 63
Nursing Management Psychologic Function • Patient must be included in discharge planning and provided with information and support to make informed decisions about continuing care • Recognition of alcohol withdrawal syndrome • Report any unusual behavior for immediate diagnosis and treatment 64
Planning for Discharge and Follow-up Care • Planning for discharge begins in preoperative period • Provide information to patient and caregivers What information is needed? 65