Posterior Capsular Rupture Vitrectomy Farid Karimian M D




- Slides: 31

Posterior Capsular Rupture & Vitrectomy Farid Karimian M. D 2002
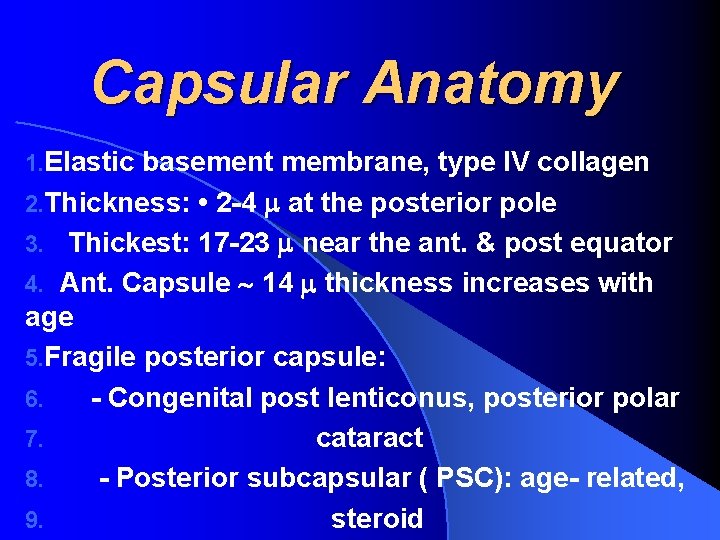
Capsular Anatomy 1. Elastic basement membrane, type IV collagen 2. Thickness: • 2 -4 at the posterior pole 3. Thickest: 17 -23 near the ant. & post equator 4. Ant. Capsule 14 thickness increases with age 5. Fragile posterior capsule: 6. - Congenital post lenticonus, posterior polar 7. cataract 8. - Posterior subcapsular ( PSC): age- related, 9. steroid
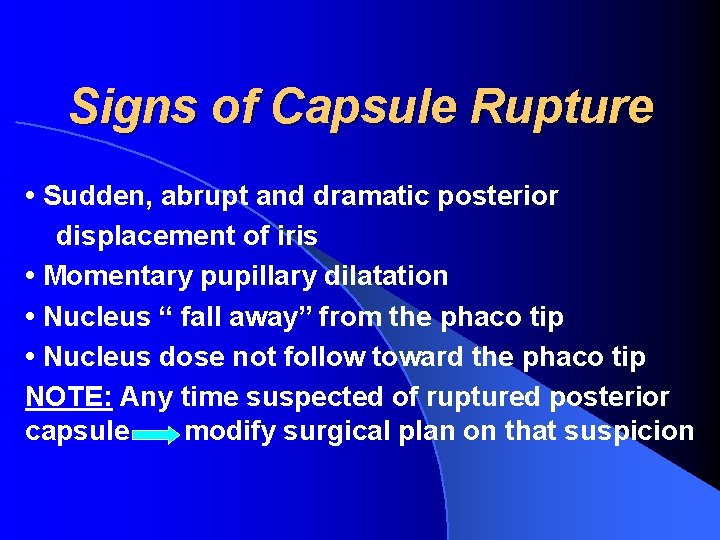
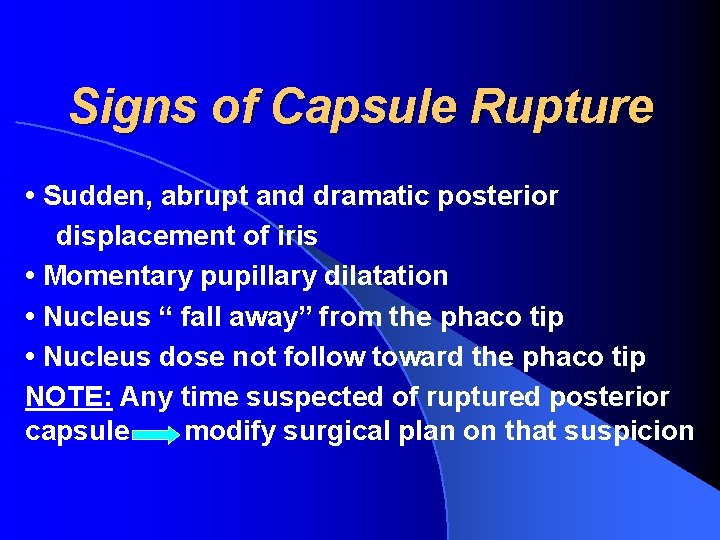
Signs of Capsule Rupture • Sudden, abrupt and dramatic posterior displacement of iris • Momentary pupillary dilatation • Nucleus “ fall away” from the phaco tip • Nucleus dose not follow toward the phaco tip NOTE: Any time suspected of ruptured posterior capsule modify surgical plan on that suspicion
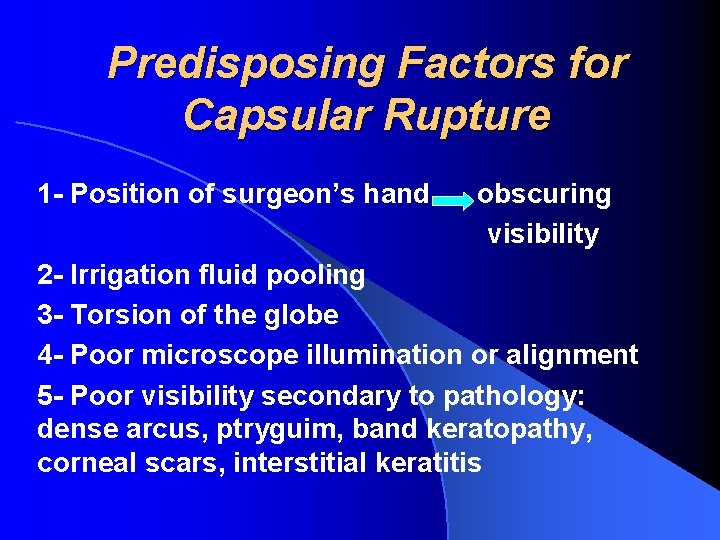
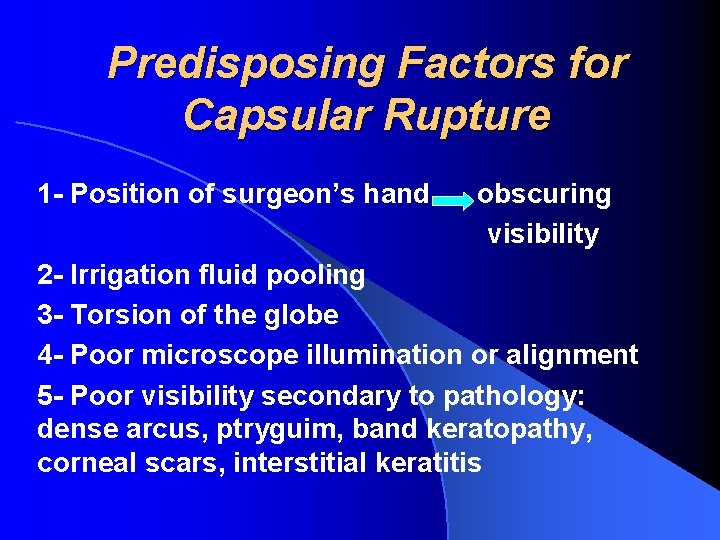
Predisposing Factors for Capsular Rupture 1 - Position of surgeon’s hand obscuring visibility 2 - Irrigation fluid pooling 3 - Torsion of the globe 4 - Poor microscope illumination or alignment 5 - Poor visibility secondary to pathology: dense arcus, ptryguim, band keratopathy, corneal scars, interstitial keratitis
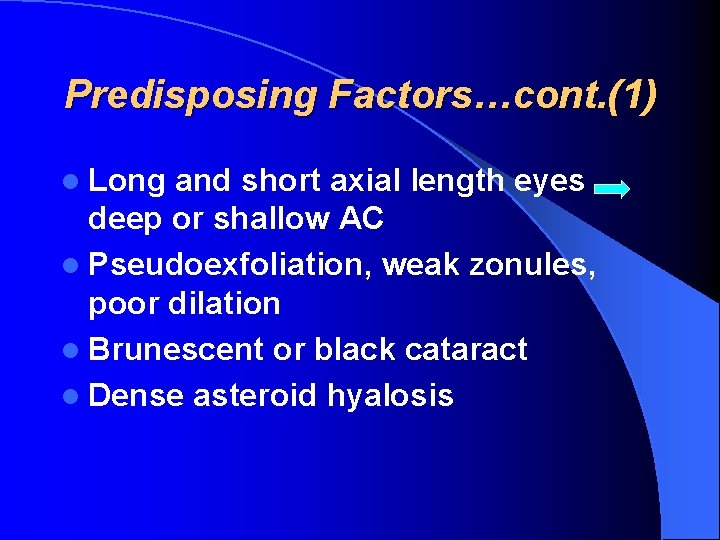
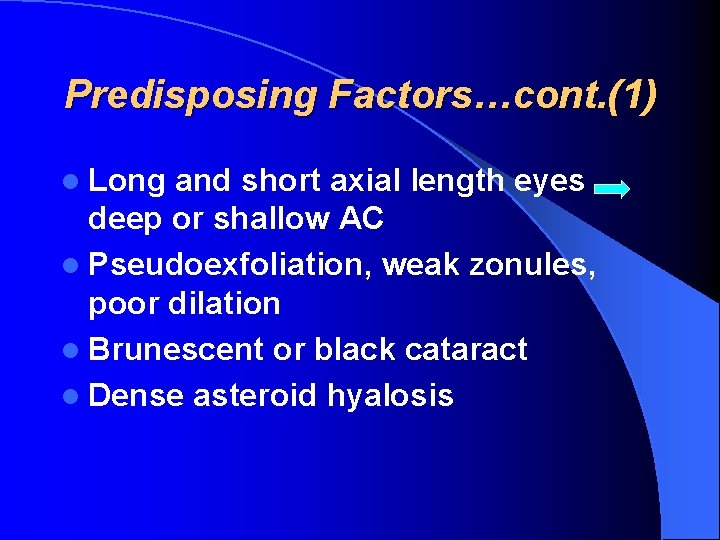
Predisposing Factors…cont. (1) l Long and short axial length eyes deep or shallow AC l Pseudoexfoliation, weak zonules, poor dilation l Brunescent or black cataract l Dense asteroid hyalosis
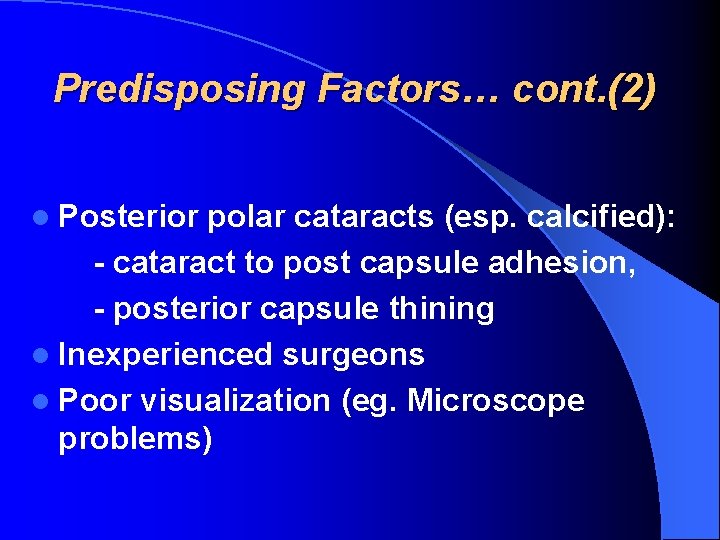
Predisposing Factors… cont. (2) l Posterior polar cataracts (esp. calcified): - cataract to post capsule adhesion, - posterior capsule thining l Inexperienced surgeons l Poor visualization (eg. Microscope problems)
Predisposing Factors… cont. (3) l Demented, disoriented, anxious, and addict patients: inadvertant movement l Equipment malfunction l Pre-existing trauma unseen capsular or zonular damage l Small pupils
When the Posterior Capsule is Torn? l Terminal stages of phaco for emulsification of last pieces of endonucleus l During posterior capsule polishing l During I/A l Hydrodissection, IOL insertion: less common
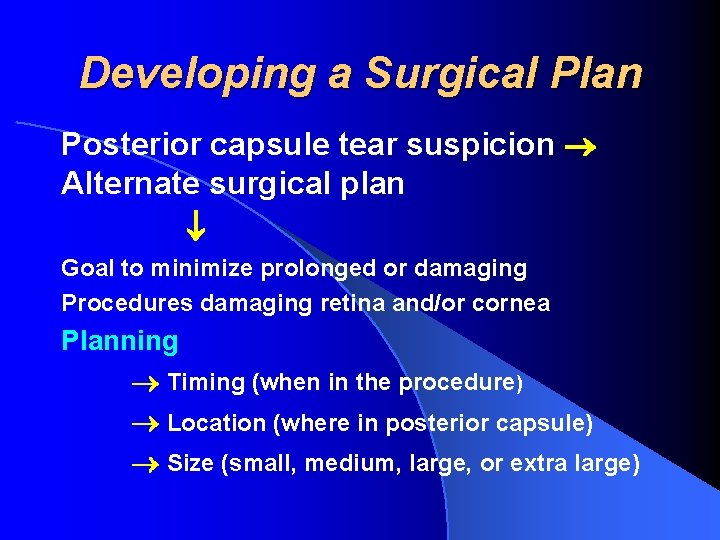
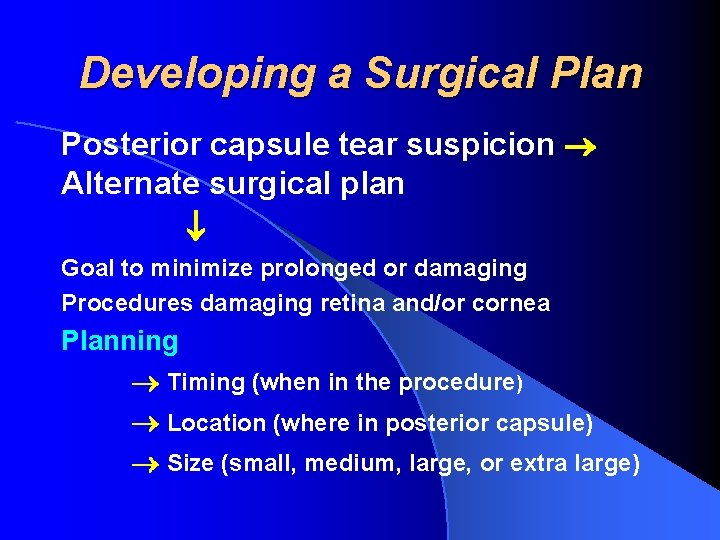
Developing a Surgical Plan Posterior capsule tear suspicion Alternate surgical plan Goal to minimize prolonged or damaging Procedures damaging retina and/or cornea Planning Timing (when in the procedure) Location (where in posterior capsule) Size (small, medium, large, or extra large)
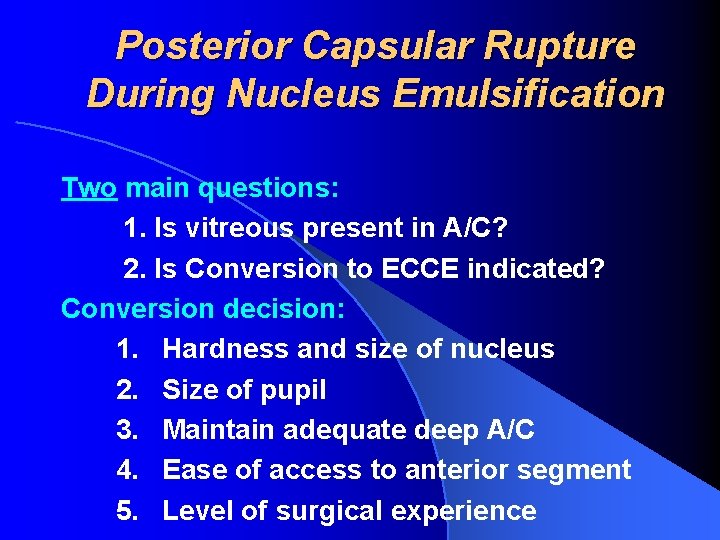
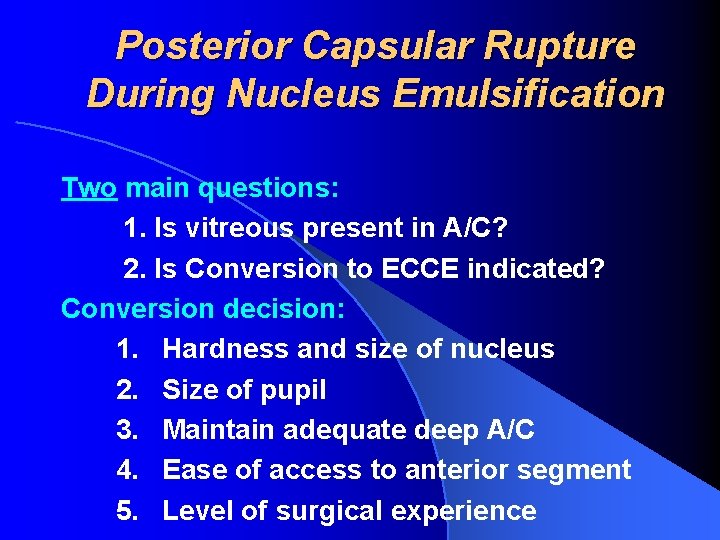
Posterior Capsular Rupture During Nucleus Emulsification Two main questions: 1. Is vitreous present in A/C? 2. Is Conversion to ECCE indicated? Conversion decision: 1. Hardness and size of nucleus 2. Size of pupil 3. Maintain adequate deep A/C 4. Ease of access to anterior segment 5. Level of surgical experience
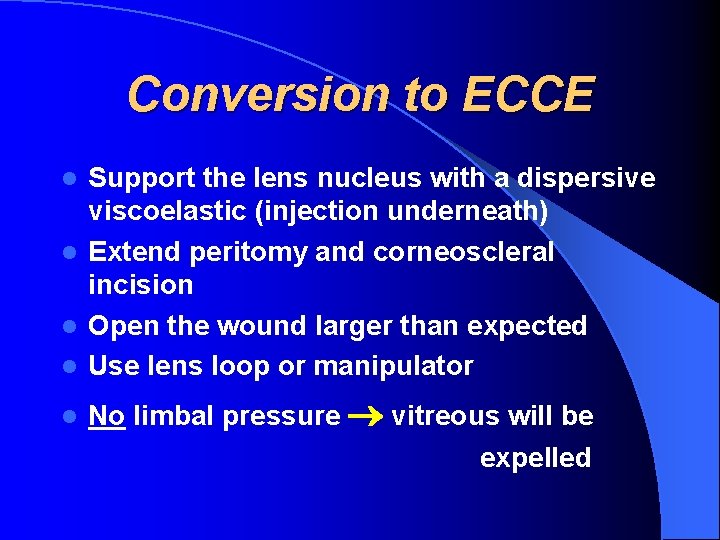
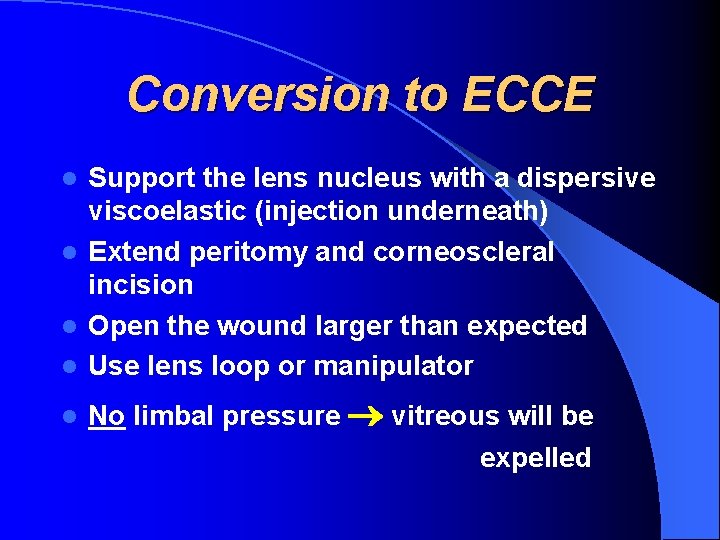
Conversion to ECCE Support the lens nucleus with a dispersive viscoelastic (injection underneath) l Extend peritomy and corneoscleral incision l Open the wound larger than expected l Use lens loop or manipulator l l No limbal pressure vitreous will be expelled
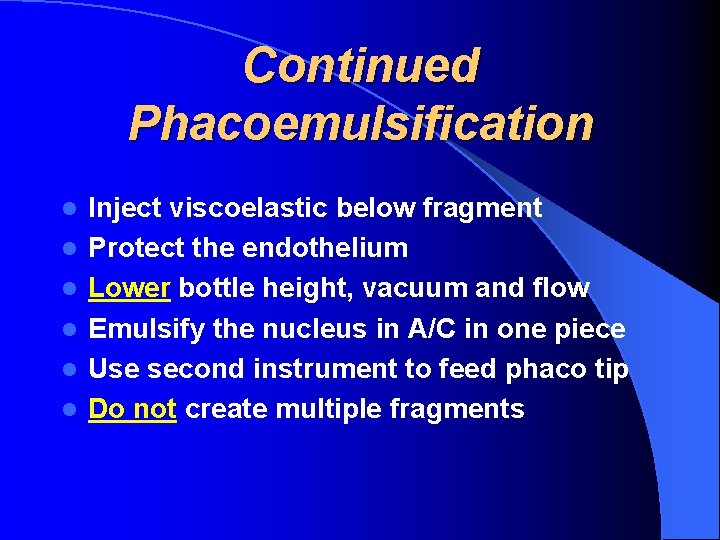
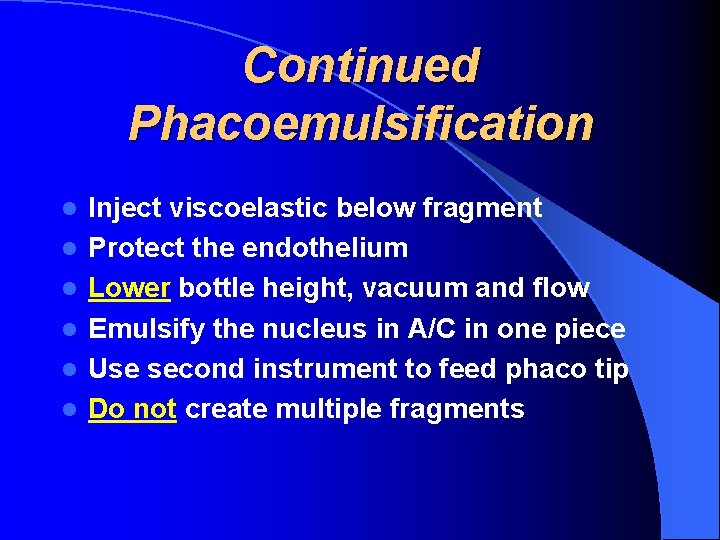
Continued Phacoemulsification l l l Inject viscoelastic below fragment Protect the endothelium Lower bottle height, vacuum and flow Emulsify the nucleus in A/C in one piece Use second instrument to feed phaco tip Do not create multiple fragments
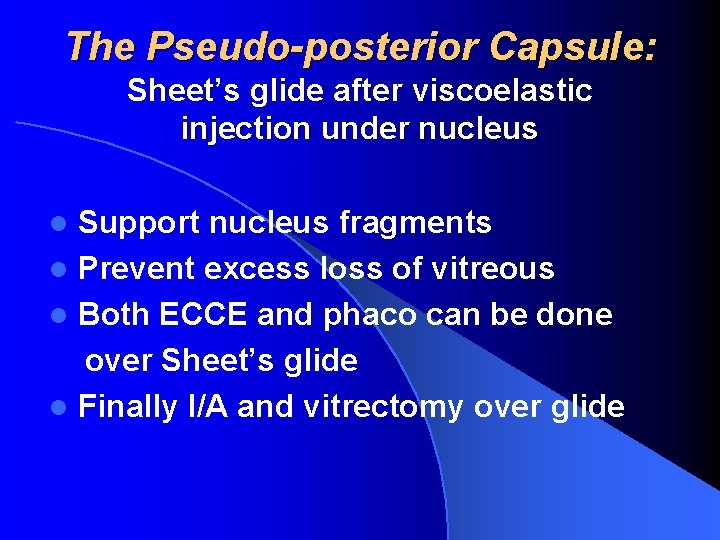
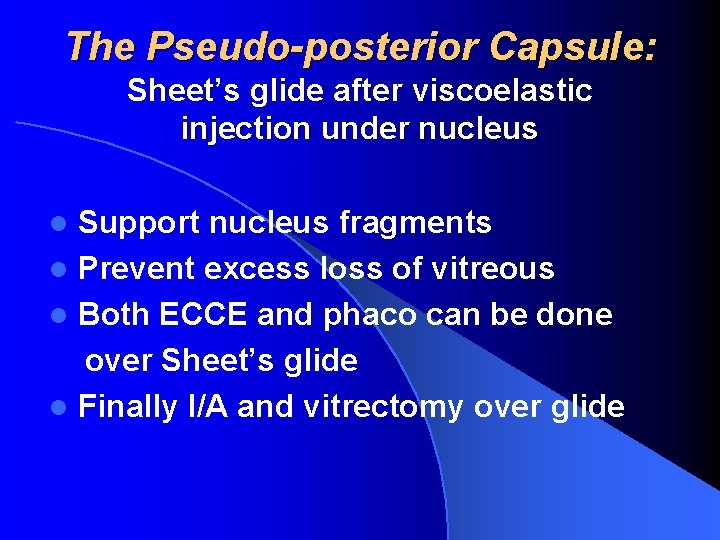
The Pseudo-posterior Capsule: Sheet’s glide after viscoelastic injection under nucleus Support nucleus fragments l Prevent excess loss of vitreous l Both ECCE and phaco can be done over Sheet’s glide l Finally I/A and vitrectomy over glide l
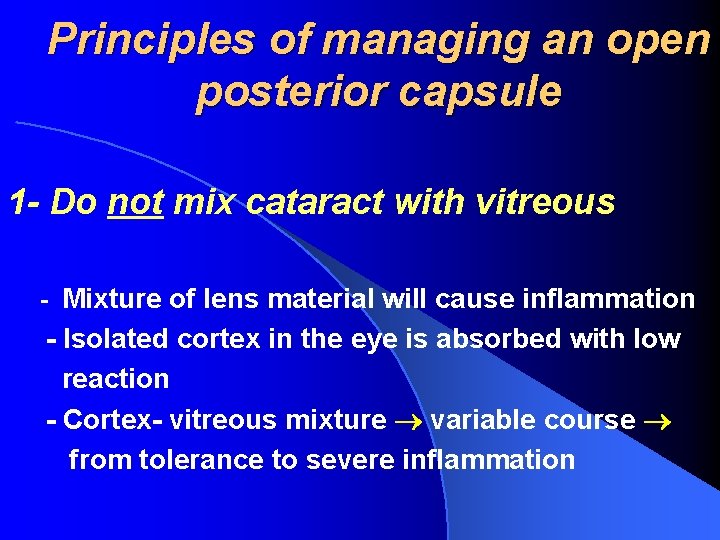
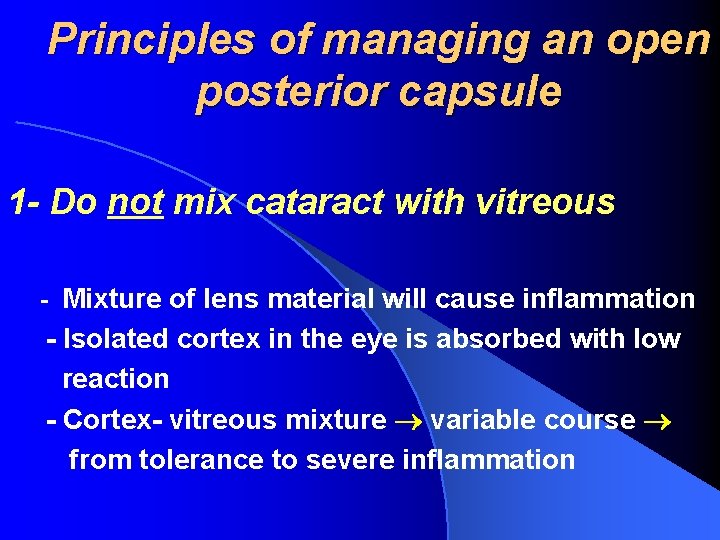
Principles of managing an open posterior capsule 1 - Do not mix cataract with vitreous - Mixture of lens material will cause inflammation - Isolated cortex in the eye is absorbed with low reaction - Cortex- vitreous mixture variable course from tolerance to severe inflammation
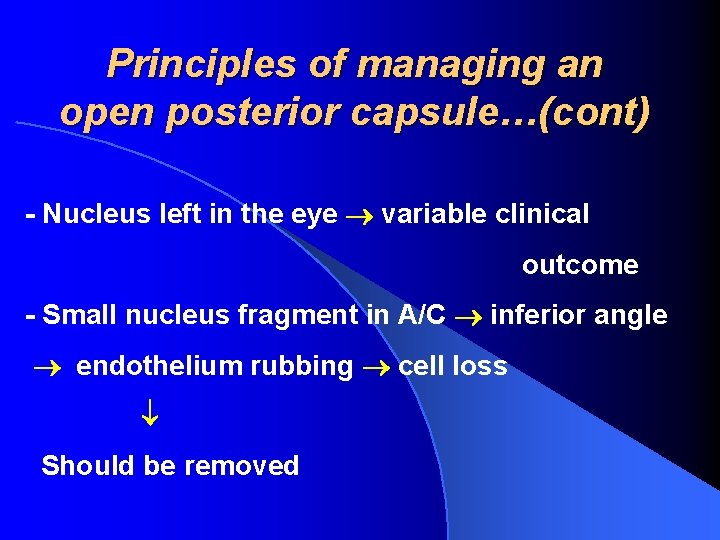
Principles of managing an open posterior capsule…(cont) - Nucleus left in the eye variable clinical outcome - Small nucleus fragment in A/C inferior angle endothelium rubbing cell loss Should be removed
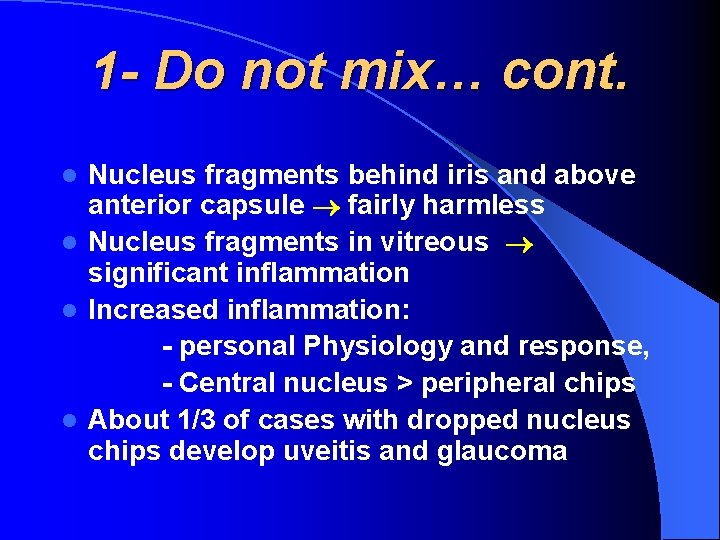
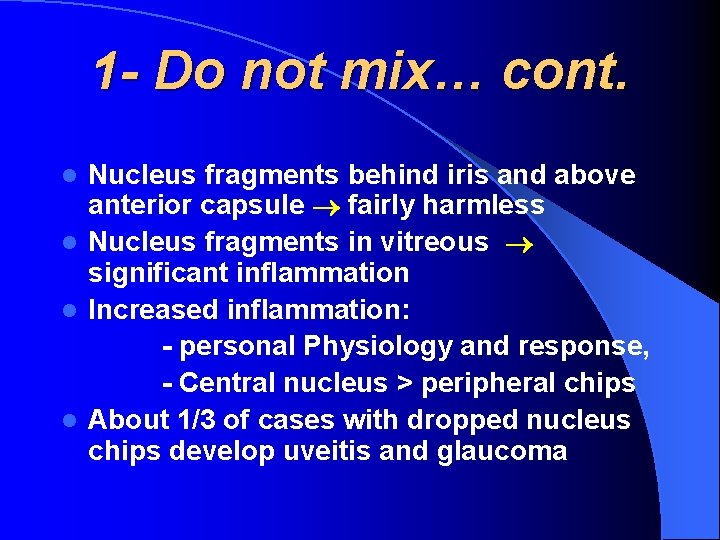
1 - Do not mix… cont. Nucleus fragments behind iris and above anterior capsule fairly harmless l Nucleus fragments in vitreous significant inflammation l Increased inflammation: - personal Physiology and response, - Central nucleus > peripheral chips l About 1/3 of cases with dropped nucleus chips develop uveitis and glaucoma l
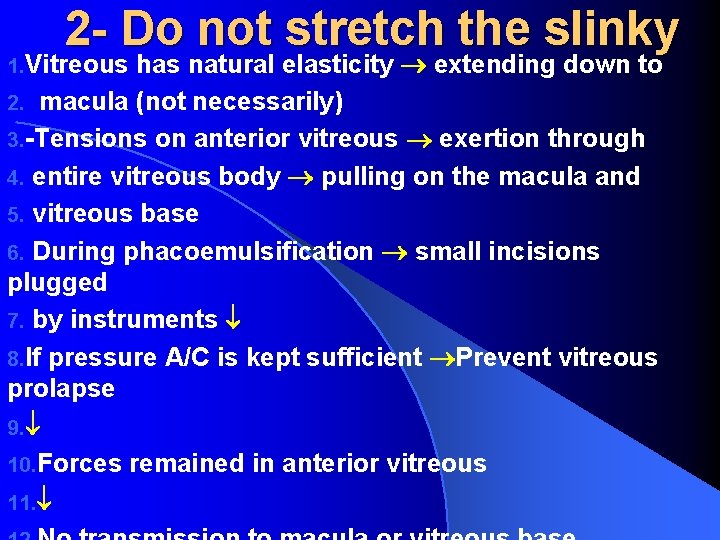
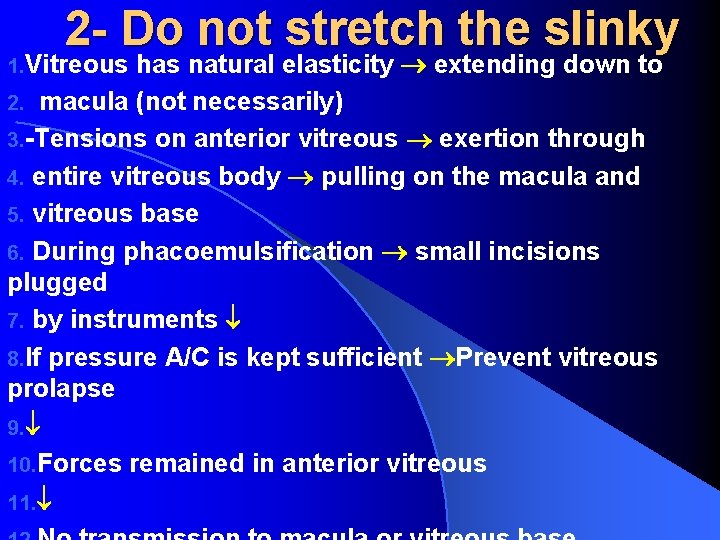
2 - Do not stretch the slinky has natural elasticity extending down to 2. macula (not necessarily) 3. -Tensions on anterior vitreous exertion through 4. entire vitreous body pulling on the macula and 5. vitreous base 6. During phacoemulsification small incisions plugged 7. by instruments 8. If pressure A/C is kept sufficient Prevent vitreous prolapse 9. 10. Forces remained in anterior vitreous 11. 1. Vitreous
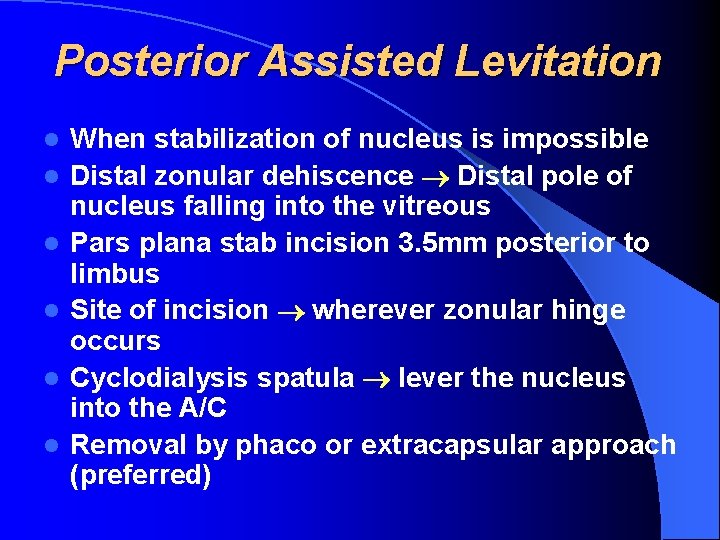
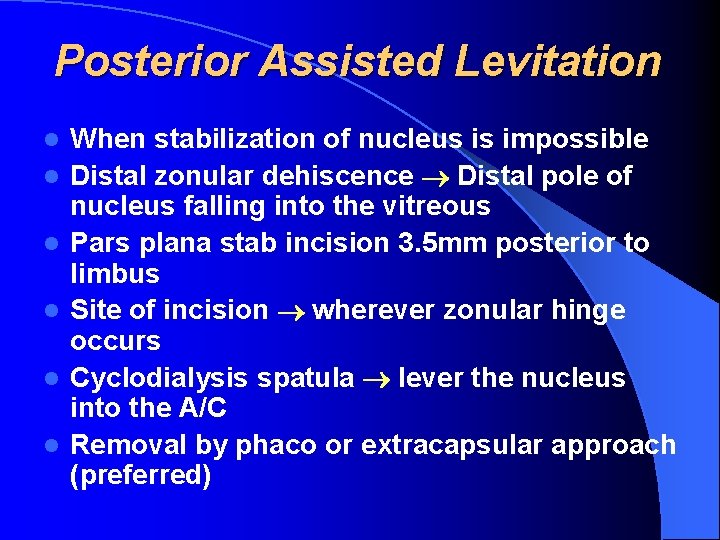
Posterior Assisted Levitation l l l When stabilization of nucleus is impossible Distal zonular dehiscence Distal pole of nucleus falling into the vitreous Pars plana stab incision 3. 5 mm posterior to limbus Site of incision wherever zonular hinge occurs Cyclodialysis spatula lever the nucleus into the A/C Removal by phaco or extracapsular approach (preferred)

Specific Clinical Situations Posterior capsule rupture and vitreous loss situations 1 - During Capsulotomy and Hydrodissection -poorly directed anterior capsule peripheral extension Tear usually stops by zonule network High volume with rapid injection extends radial tear into equator and back to posterior capsule
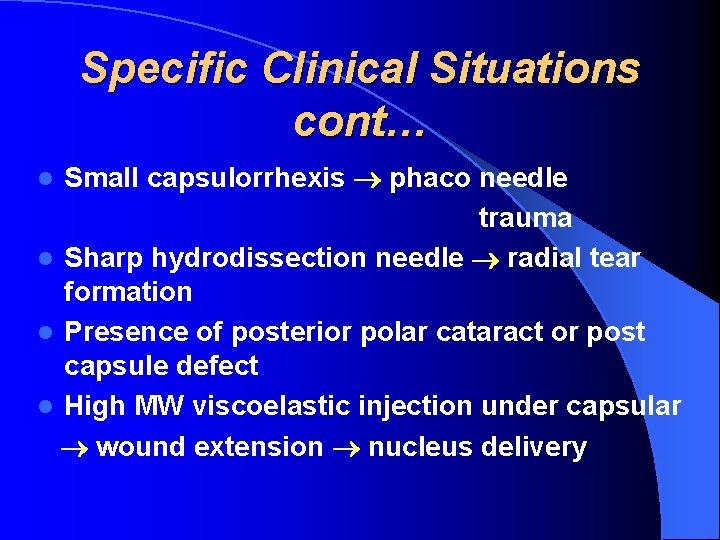
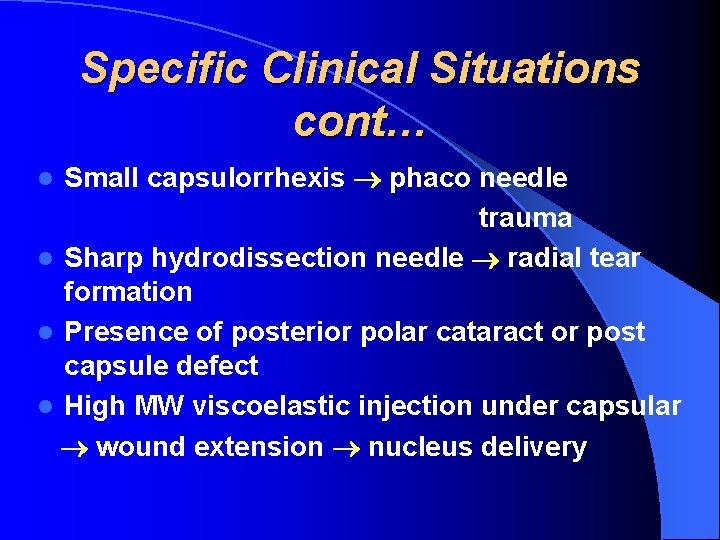
Specific Clinical Situations cont… Small capsulorrhexis phaco needle trauma l Sharp hydrodissection needle radial tear formation l Presence of posterior polar cataract or post capsule defect l High MW viscoelastic injection under capsular wound extension nucleus delivery l
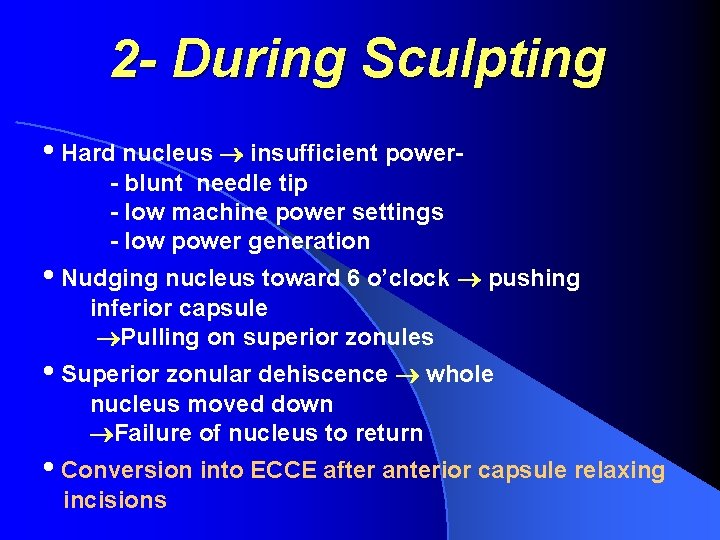
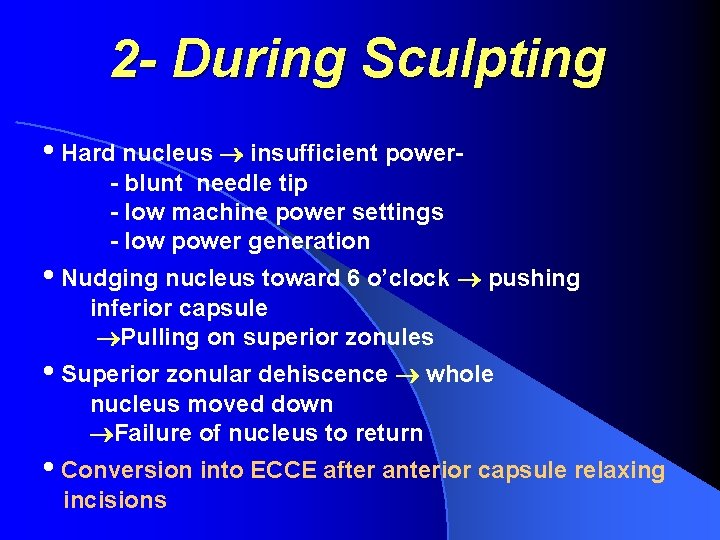
2 - During Sculpting • Hard nucleus insufficient power- blunt needle tip - low machine power settings - low power generation • Nudging nucleus toward 6 o’clock pushing inferior capsule Pulling on superior zonules • Superior zonular dehiscence whole nucleus moved down Failure of nucleus to return • Conversion into ECCE after anterior capsule relaxing incisions
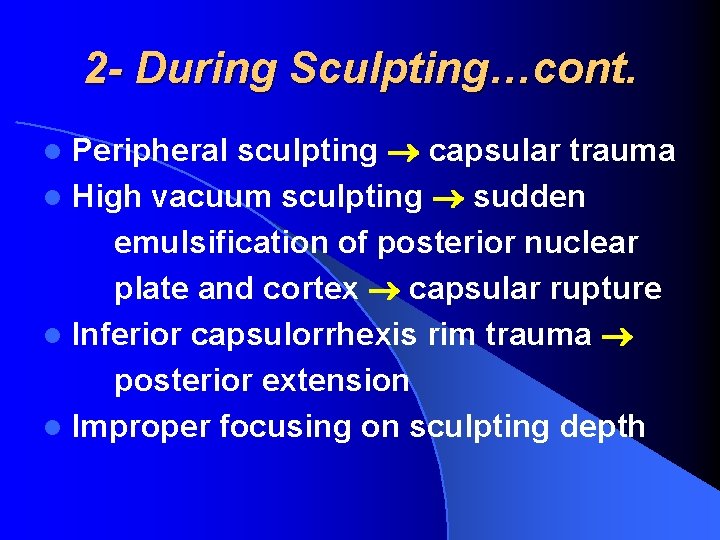
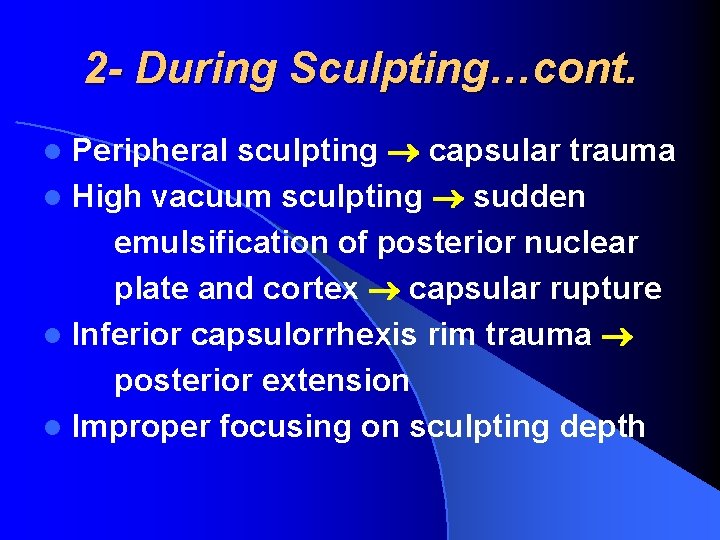
2 - During Sculpting…cont. Peripheral sculpting capsular trauma l High vacuum sculpting sudden emulsification of posterior nuclear plate and cortex capsular rupture l Inferior capsulorrhexis rim trauma posterior extension l Improper focusing on sculpting depth l
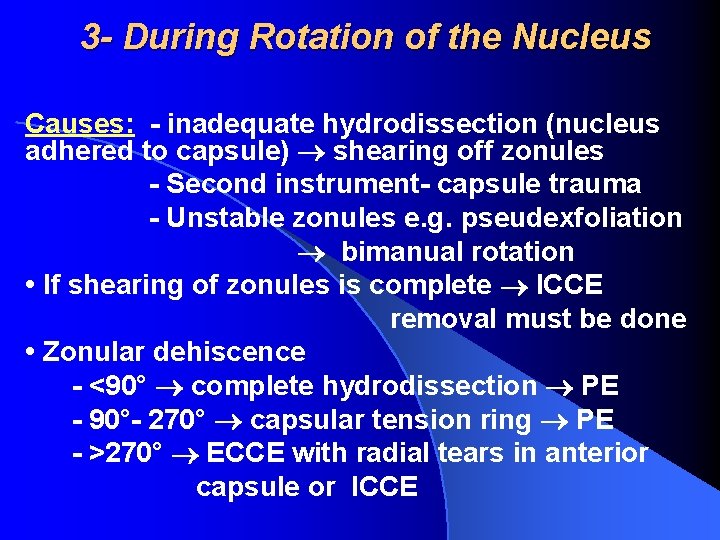
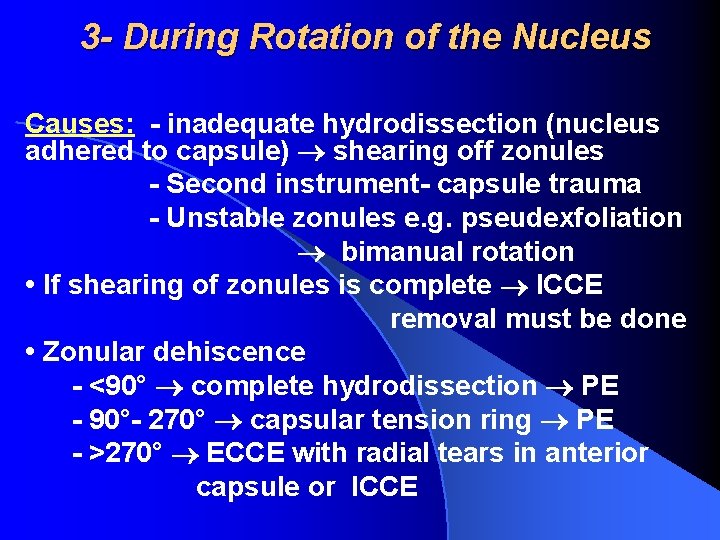
3 - During Rotation of the Nucleus Causes: - inadequate hydrodissection (nucleus adhered to capsule) shearing off zonules - Second instrument- capsule trauma - Unstable zonules e. g. pseudexfoliation bimanual rotation • If shearing of zonules is complete ICCE removal must be done • Zonular dehiscence - <90° complete hydrodissection PE - 90°- 270° capsular tension ring PE - >270° ECCE with radial tears in anterior capsule or ICCE
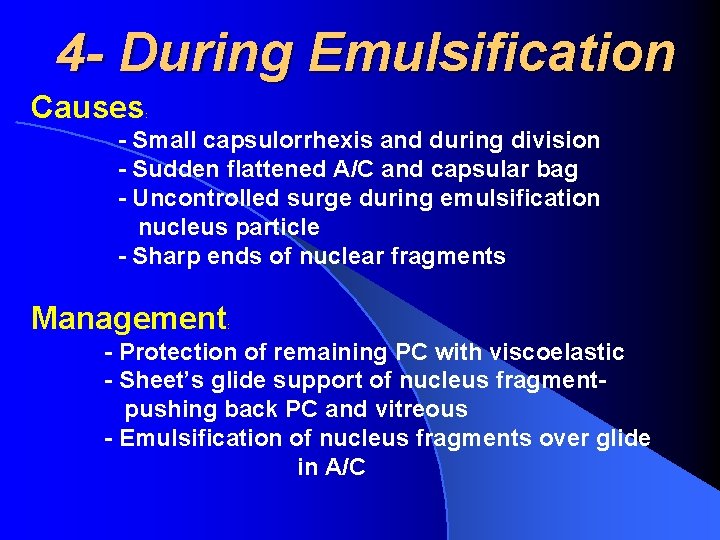
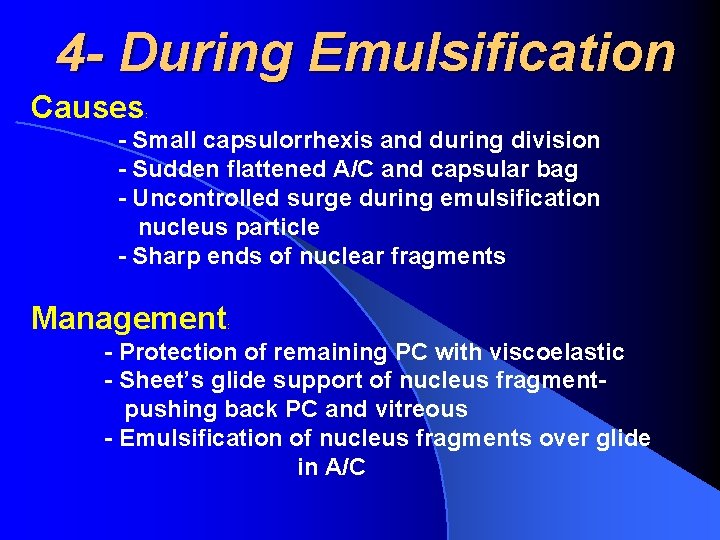
4 - During Emulsification Causes : - Small capsulorrhexis and during division - Sudden flattened A/C and capsular bag - Uncontrolled surge during emulsification nucleus particle - Sharp ends of nuclear fragments Management : - Protection of remaining PC with viscoelastic - Sheet’s glide support of nucleus fragmentpushing back PC and vitreous - Emulsification of nucleus fragments over glide in A/C

5 - During Cortical Aspiration Causes : Post capsule trauma by I&A tip: Flat AC, excess aspiration • Anterior capsule entrapment in aspiration port traction • Inadequate hydrodissection • Management: - Place dispersive viscoelastic over the vent - Embed I&A tip into the cortex apply vacuum (not aspirating vitreous) - Stripping toward capsule tear - Lower infusion bottle inflow, turbulence - Vitrectomy tip can be used for cortical removal - Leave cortical material: if not too much!
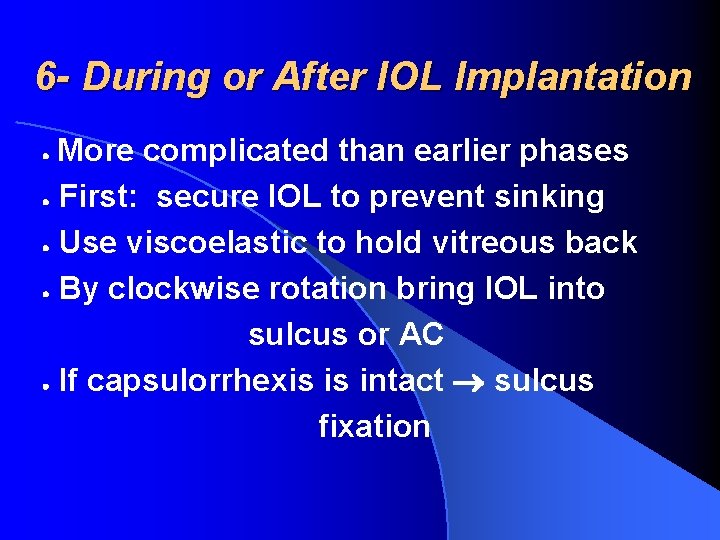
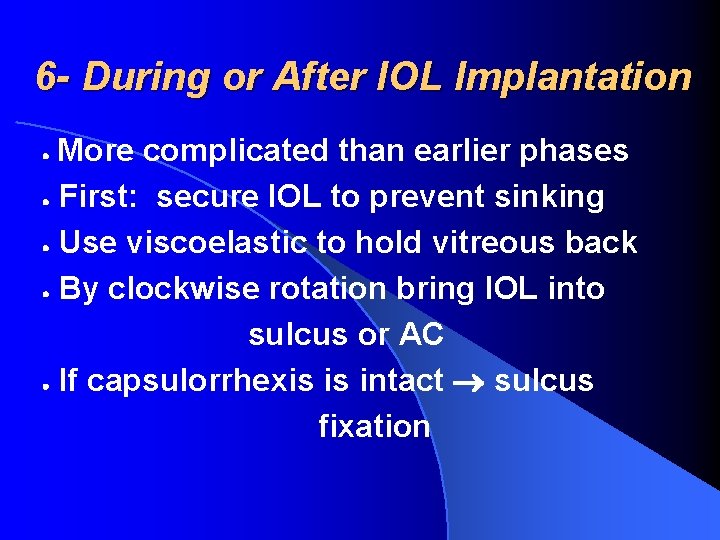
6 - During or After IOL Implantation More complicated than earlier phases First: secure IOL to prevent sinking Use viscoelastic to hold vitreous back By clockwise rotation bring IOL into sulcus or AC If capsulorrhexis is intact sulcus fixation
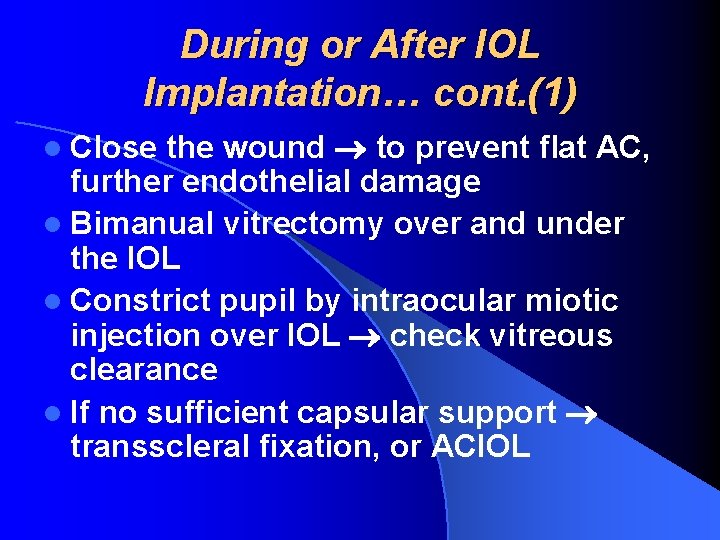
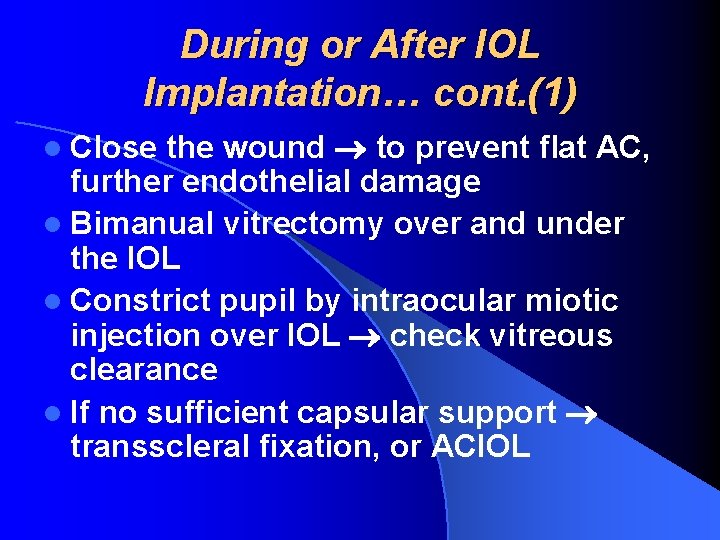
During or After IOL Implantation… cont. (1) the wound to prevent flat AC, further endothelial damage l Bimanual vitrectomy over and under the IOL l Constrict pupil by intraocular miotic injection over IOL check vitreous clearance l If no sufficient capsular support transscleral fixation, or ACIOL l Close
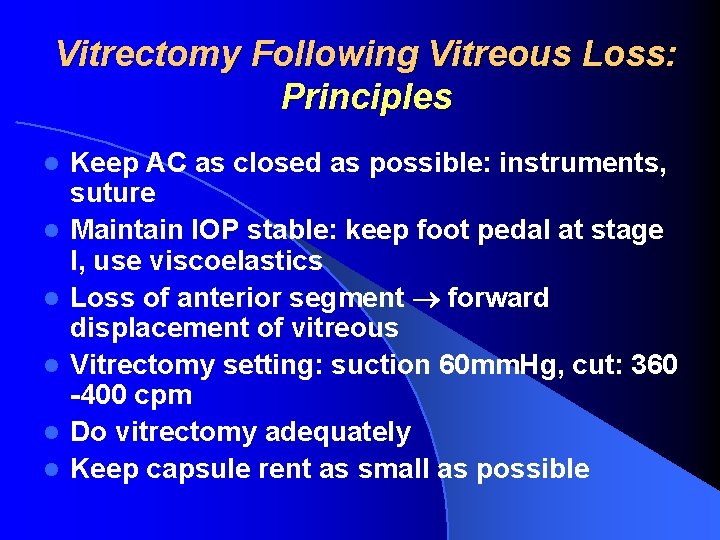
Vitrectomy Following Vitreous Loss: Principles l l l Keep AC as closed as possible: instruments, suture Maintain IOP stable: keep foot pedal at stage I, use viscoelastics Loss of anterior segment forward displacement of vitreous Vitrectomy setting: suction 60 mm. Hg, cut: 360 -400 cpm Do vitrectomy adequately Keep capsule rent as small as possible
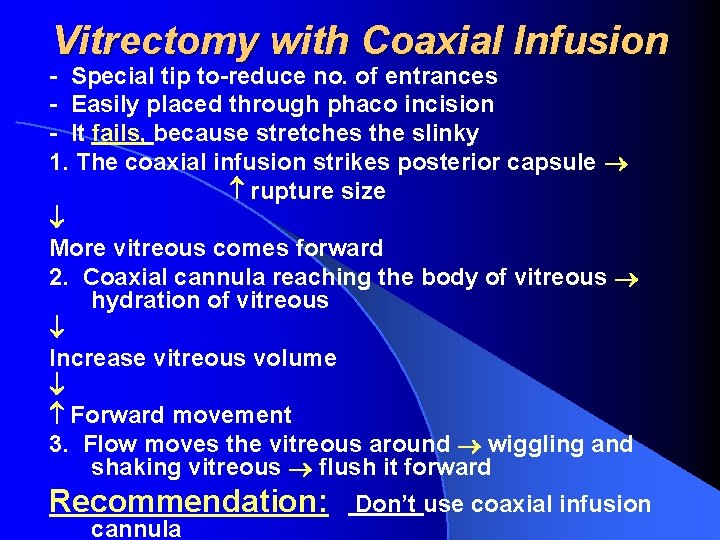
Vitrectomy with Coaxial Infusion - Special tip to-reduce no. of entrances - Easily placed through phaco incision - It fails, because stretches the slinky 1. The coaxial infusion strikes posterior capsule rupture size More vitreous comes forward 2. Coaxial cannula reaching the body of vitreous hydration of vitreous Increase vitreous volume Forward movement 3. Flow moves the vitreous around wiggling and shaking vitreous flush it forward Recommendation: cannula Don’t use coaxial infusion

Two-handed (port) Vitrectomy l l l Close the entrance wounds for vitrectomy tip i. e. make a closed system Procedure will be performed rapidly and conveniently Perform small vitrectomy without irrigation Prevent eye softening by repeated injection of viscoelastic push vitreous back Chamber-maintainer through side-port forms AC Remove the vitreous to below the level of posterior capsule
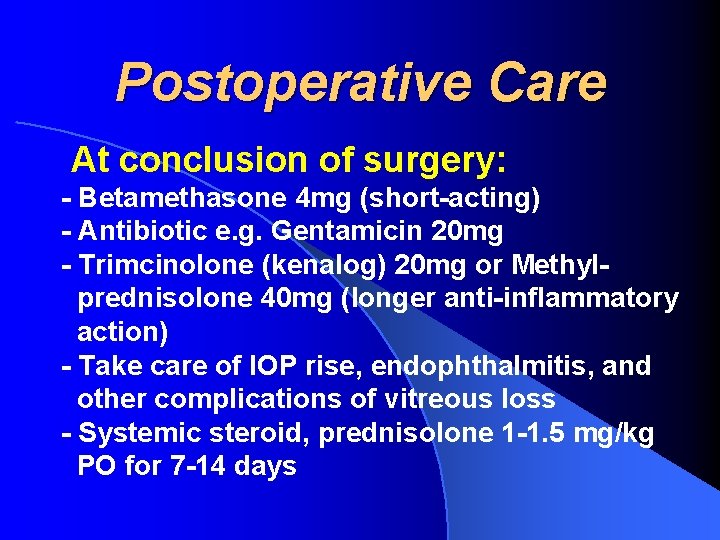
Postoperative Care At conclusion of surgery: - Betamethasone 4 mg (short-acting) - Antibiotic e. g. Gentamicin 20 mg - Trimcinolone (kenalog) 20 mg or Methylprednisolone 40 mg (longer anti-inflammatory action) - Take care of IOP rise, endophthalmitis, and other complications of vitreous loss - Systemic steroid, prednisolone 1 -1. 5 mg/kg PO for 7 -14 days