Poster e P 149 Disclosure No Disclosure Flow
- Slides: 25
Poster: e. P- 149
Disclosure ØNo Disclosure
Flow Diverter (FD) Stent Treatment for Blood Blister-like Aneurysms (BBAs) Satya Patro, MD (Interventional Neuroradiology fellow) Daniela Iancu, MD Taleb Al Mansoori, MD Cheemun Lum, MD Howard Lesiuk, MD The Ottawa Hospital, University of Ottawa, Canada
Introduction ØBlood blister-like aneurysms (BBAs) are small and irregularly shaped aneurysms with a broad base, commonly located at the non-branching sites of intracranial arteries ØRelatively rare lesions, comprising <2% of all intracranial aneurysms. ØCommonly present with subarachnoid hemorrhage and demonstrated on DSA ØHistopathology: abrupt loss of both intima and media with dome surrounded by adventitia and thrombus ØExtremely fragile and thin walled
Introduction ØNo optimal treatment ØRoutine surgical clipping and endovascular coiling with or without stenting are associated with very high morbidity and mortality ØEndovascular treatment has high risk of peri-procedural and post-procedural rupture and hemorrhage ØParent artery sacrifice is a safe alternative; however associated with poor outcome
Introduction ØFlow Diverter (FD) stents are special kind of intracranial stents, have been used for complex, wide neck and fusiform aneurysms ØIt acts by reconstructing the vessel wall and diverting the blood flow away from the aneurysm, thus resulting in thrombosis and occlusion of the aneurysm ØSILK stent (Balt Extrusion, Montmorency, France) was introduced in early 2007, is a self-expanding FD made of a braided multi alloy cylindrical mesh
Purpose ØHere we report single neurointervention center experience on the endovascular treatment by implantation of SILK flow diverter stents (Balt Extrusion, Montmorency, France) of 7 patients with subarachnoid
Materials & Methods ØRetrospective study approved by our institution REB ØDuration of Study: July’ 2012 to Oct’ 2015 ØPatients with SAH secondary to BBAs ØInitial and follow-up clinical data, technical results, and angiographic findings of the patients were assessed ØAll patients underwent CT head/CTA head and neck
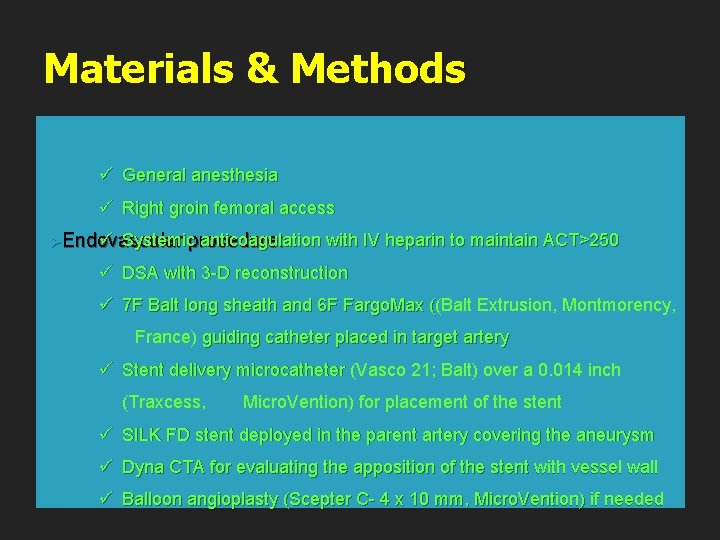
Materials & Methods ü General anesthesia ü Right groin femoral access ü Systemicprocedure: anticoagulation ØEndovascular with IV heparin to maintain ACT>250 ü DSA with 3 -D reconstruction ü 7 F Balt long sheath and 6 F Fargo. Max ((Balt Extrusion, Montmorency, ( France) guiding catheter placed in target artery ü Stent delivery microcatheter (Vasco 21; Balt) over a 0. 014 inch (Traxcess, Micro. Vention) for placement of the stent ü SILK FD stent deployed in the parent artery covering the aneurysm ü Dyna CTA for evaluating the apposition of the stent with vessel wall ü Balloon angioplasty (Scepter C- 4 x 10 mm, Micro. Vention) if needed
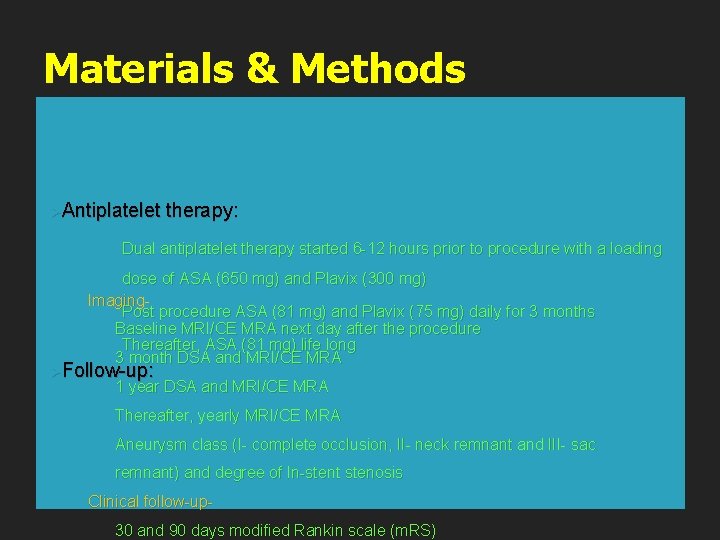
Materials & Methods ØAntiplatelet therapy: Dual antiplatelet therapy started 6 -12 hours prior to procedure with a loading dose of ASA (650 mg) and Plavix (300 mg) Imaging. Post procedure ASA (81 mg) and Plavix (75 mg) daily for 3 months Baseline MRI/CE MRA next day after the procedure Thereafter, ASA (81 mg) life long 3 month DSA and MRI/CE MRA ØFollow-up: 1 year DSA and MRI/CE MRA Thereafter, yearly MRI/CE MRA Aneurysm class (I- complete occlusion, II- neck remnant and III- sac remnant) and degree of In-stent stenosis Clinical follow-up 30 and 90 days modified Rankin scale (m. RS)
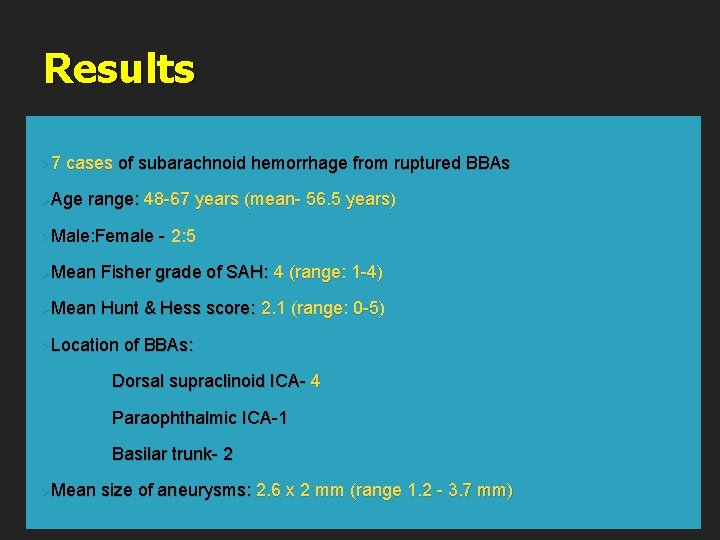
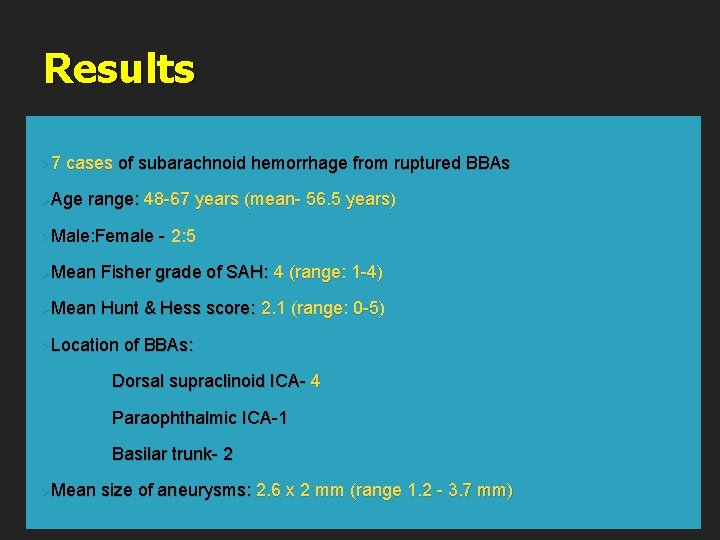
Results Ø 7 cases of subarachnoid hemorrhage from ruptured BBAs ØAge range: 48 -67 years (mean- 56. 5 years) ØMale: Female - 2: 5 ØMean Fisher grade of SAH: 4 (range: 1 -4) ØMean Hunt & Hess score: 2. 1 (range: 0 -5) ØLocation of BBAs: Dorsal supraclinoid ICA- 4 Paraophthalmic ICA-1 Basilar trunk- 2 ØMean size of aneurysms: 2. 6 x 2 mm (range 1. 2 - 3. 7 mm)
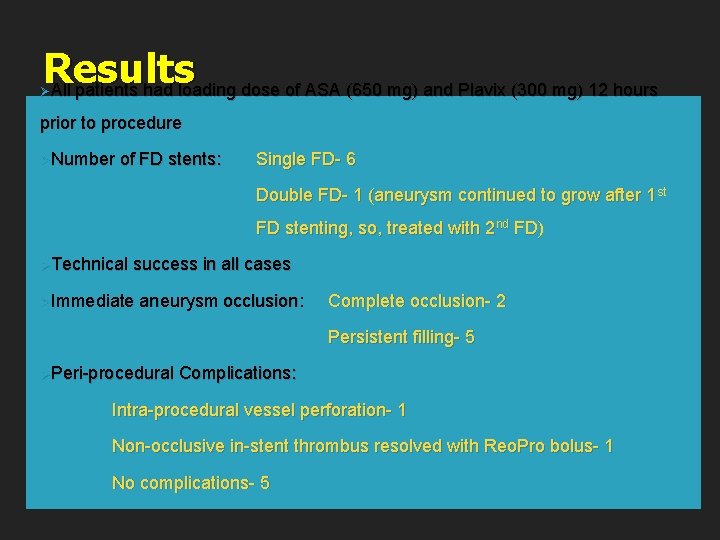
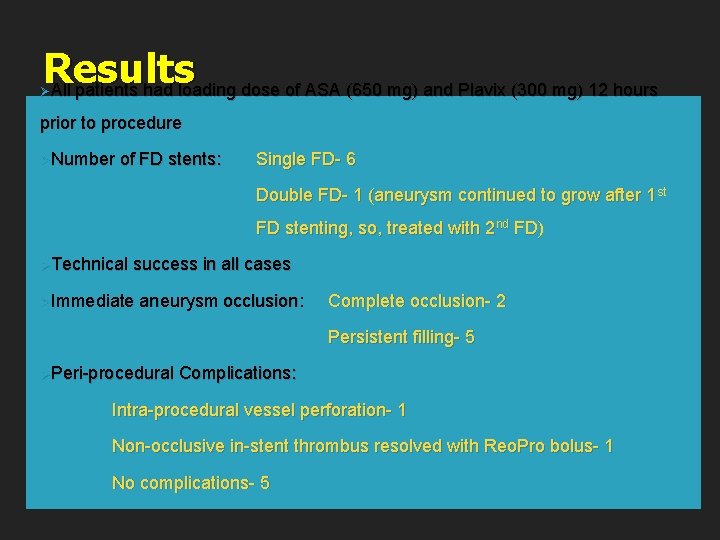
Results All patients had loading dose of ASA (650 mg) and Plavix (300 mg) 12 hours Ø prior to procedure ØNumber of FD stents: Single FD- 6 Double FD- 1 (aneurysm continued to grow after 1 st FD stenting, so, treated with 2 nd FD) ØTechnical success in all cases ØImmediate aneurysm occlusion: Complete occlusion- 2 Persistent filling- 5 ØPeri-procedural Complications: Intra-procedural vessel perforation- 1 Non-occlusive in-stent thrombus resolved with Reo. Pro bolus- 1 No complications- 5
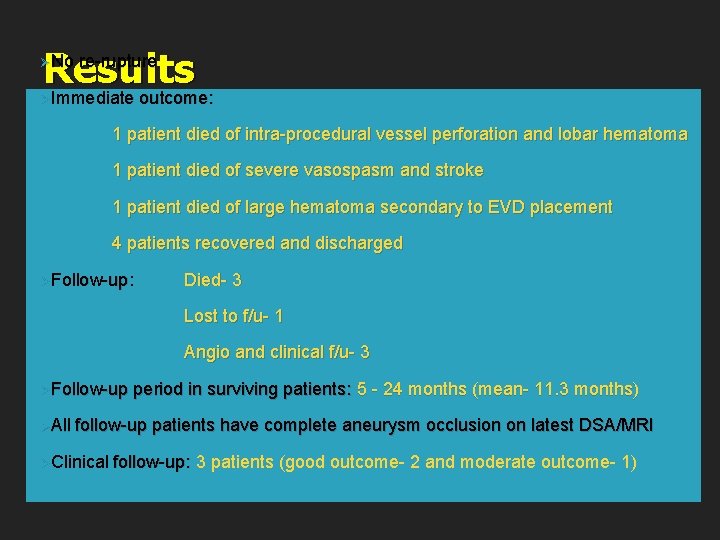
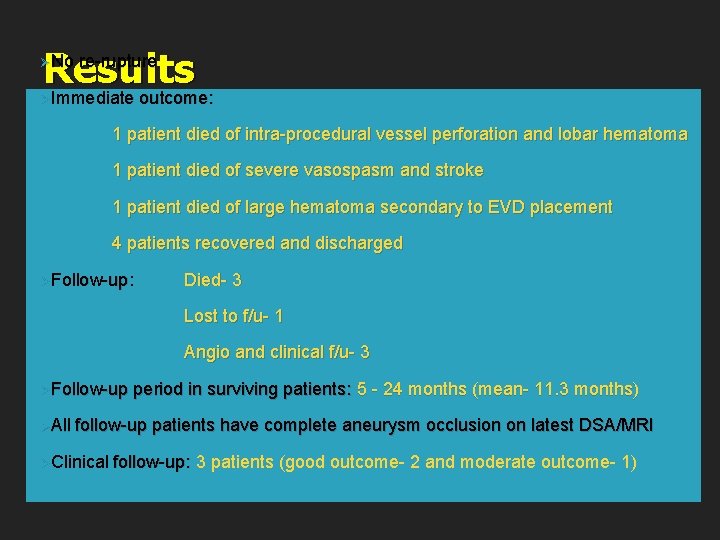
Results Immediate outcome: ØNo re-rupture Ø 1 patient died of intra-procedural vessel perforation and lobar hematoma 1 patient died of severe vasospasm and stroke 1 patient died of large hematoma secondary to EVD placement 4 patients recovered and discharged ØFollow-up: Died- 3 Lost to f/u- 1 Angio and clinical f/u- 3 ØFollow-up ØAll period in surviving patients: 5 - 24 months (mean- 11. 3 months) follow-up patients have complete aneurysm occlusion on latest DSA/MRI ØClinical follow-up: 3 patients (good outcome- 2 and moderate outcome- 1)
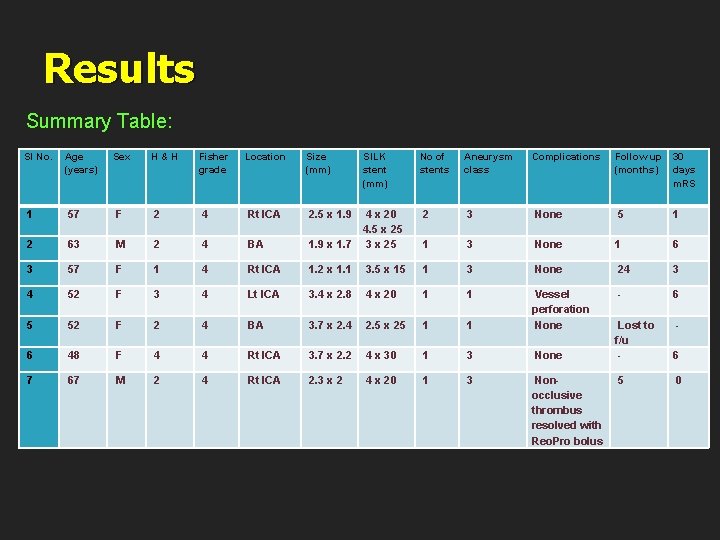
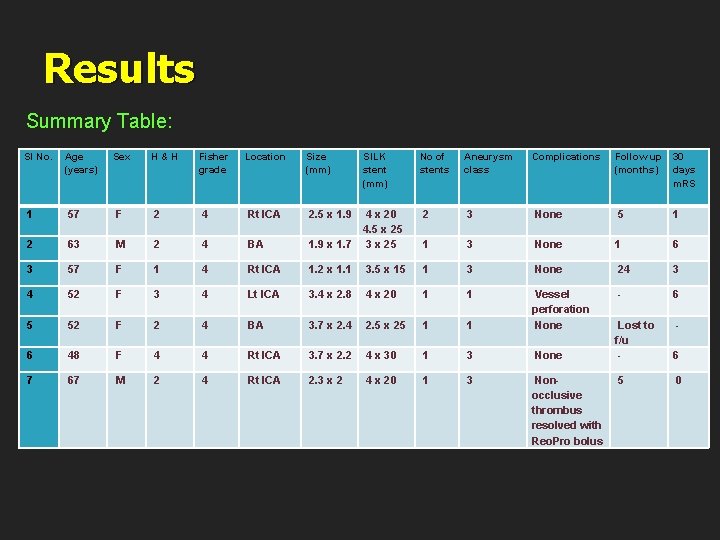
Results Summary Table: Sl No. Age (years) Sex H & H Fisher grade Location Size (mm) SILK stent (mm) No of stents Aneurysm class Complications Follow up 30 (months) days m. RS 1 57 F 2 4 Rt ICA 2. 5 x 1. 9 2 3 None 5 1 2 63 M 2 4 BA 1. 9 x 1. 7 4 x 20 4. 5 x 25 3 x 25 1 3 None 1 6 3 57 F 1 4 Rt ICA 1. 2 x 1. 1 3. 5 x 15 1 3 None 24 3 4 52 F 3 4 Lt ICA 3. 4 x 2. 8 4 x 20 1 1 - 6 5 52 F 2 4 BA 3. 7 x 2. 4 2. 5 x 25 1 1 Vessel perforation None - 6 48 F 4 4 Rt ICA 3. 7 x 2. 2 4 x 30 1 3 None Lost to f/u - 7 67 M 2 4 Rt ICA 2. 3 x 2 4 x 20 1 3 Non 5 occlusive thrombus resolved with Reo. Pro bolus 6 0
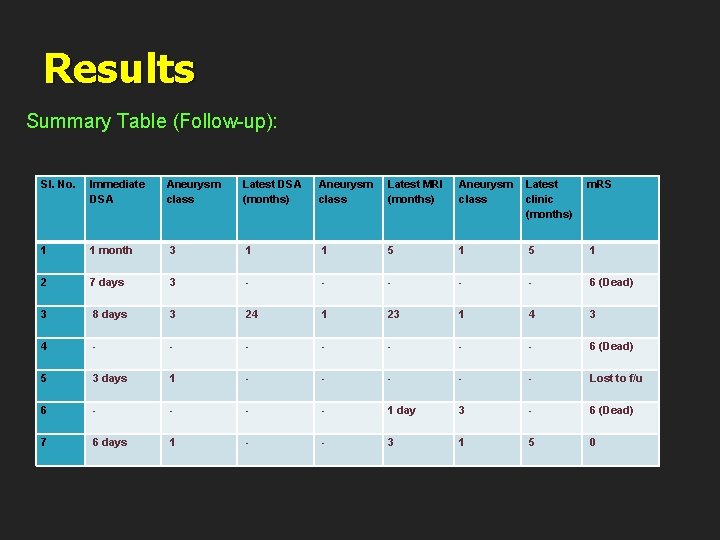
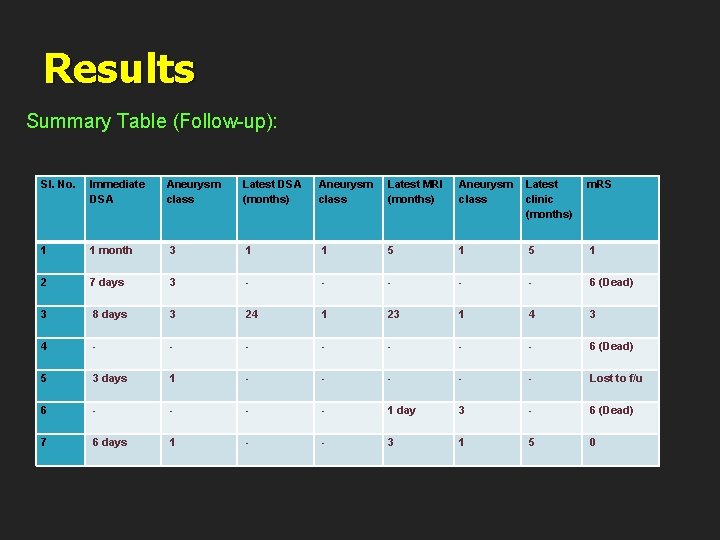
Results Summary Table (Follow-up): Sl. No. Immediate DSA Aneurysm class Latest DSA (months) Aneurysm class Latest MRI (months) Aneurysm Latest class clinic (months) m. RS 1 1 month 3 1 1 5 1 5 1 2 7 days 3 - - - - - 6 (Dead) 3 8 days 3 24 1 23 1 4 3 4 - - - - - 6 (Dead) 5 3 days 1 - - - - - Lost to f/u 6 - - 1 day 3 - 6 (Dead) 7 6 days 1 - - 3 1 5 0
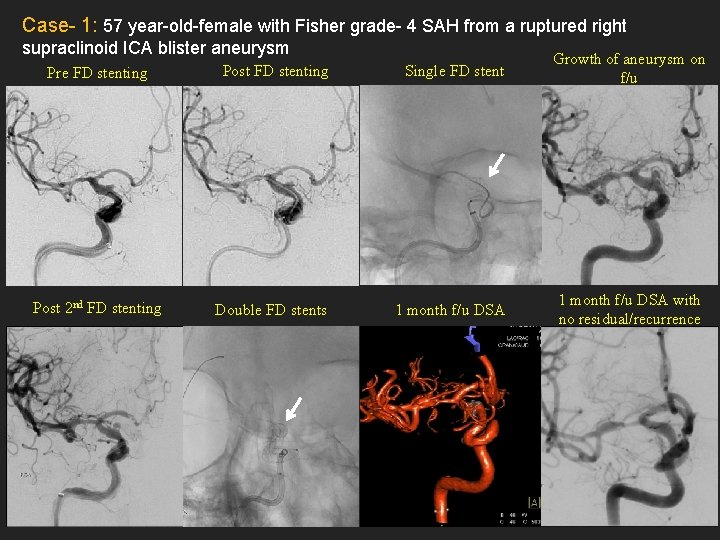
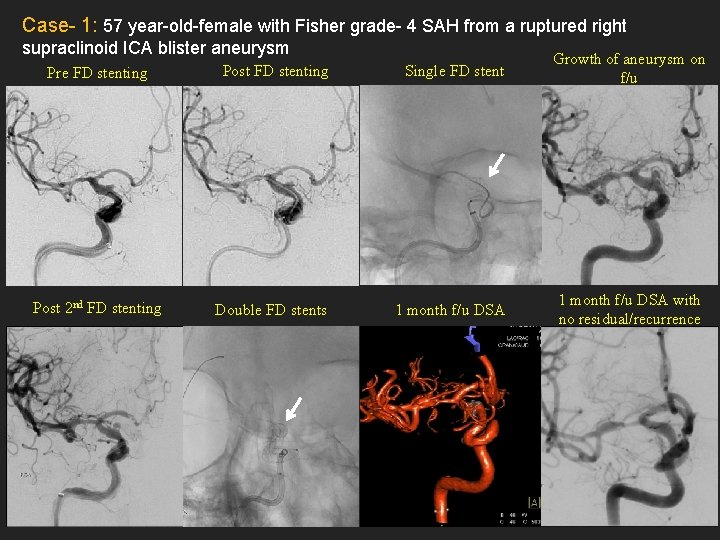
Case- 1: 57 year-old-female with Fisher grade- 4 SAH from a ruptured right supraclinoid ICA blister aneurysm Pre FD stenting Post FD stenting Single FD stent Growth of aneurysm on f/u Post 2 nd FD stenting Double FD stents 1 month f/u DSA with no residual/recurrence
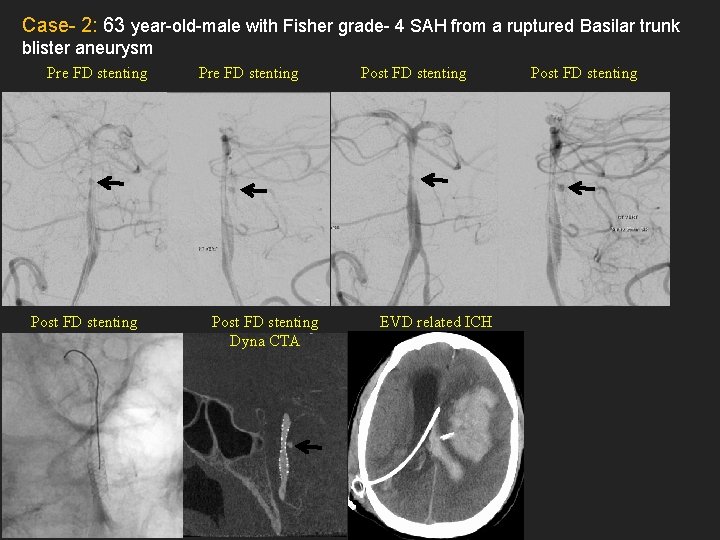
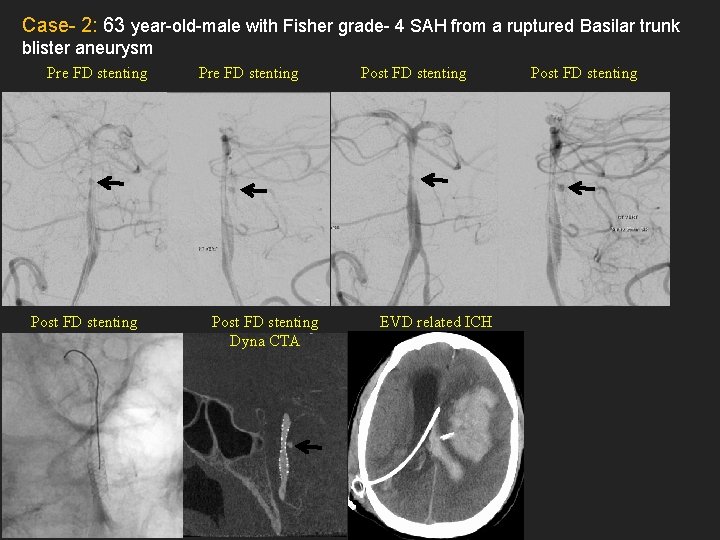
Case- 2: 63 year-old-male with Fisher grade- 4 SAH from a ruptured Basilar trunk blister aneurysm Pre FD stenting Post FD stenting Dyna CTA Post FD stenting EVD related ICH Post FD stenting
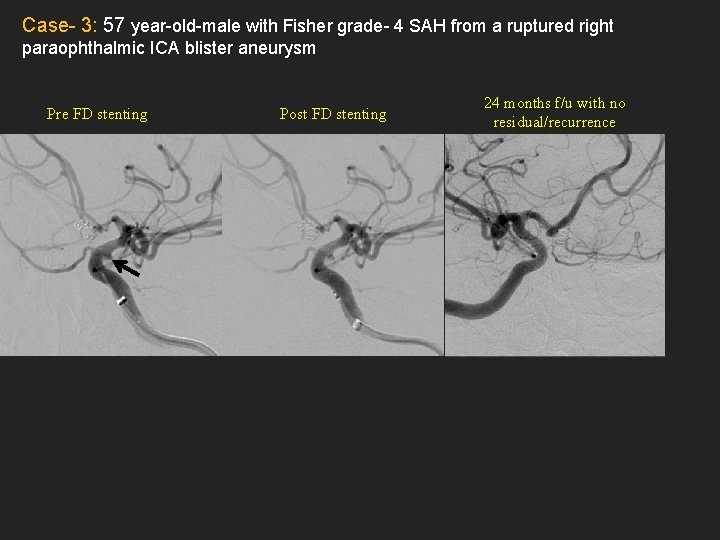
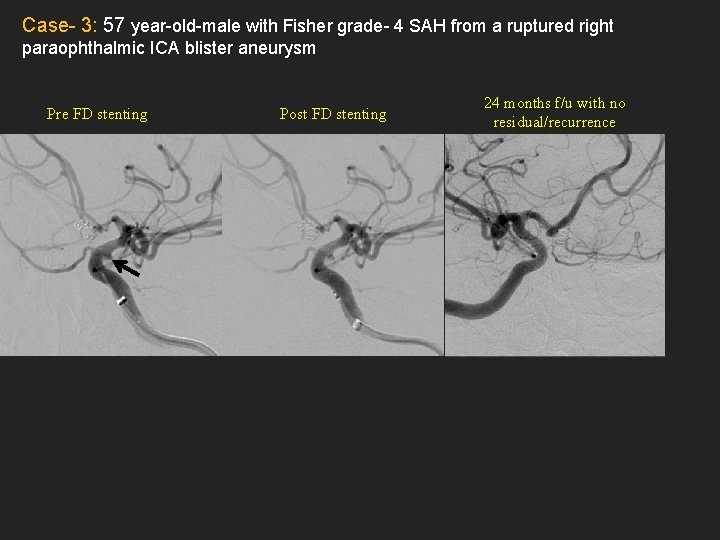
Case- 3: 57 year-old-male with Fisher grade- 4 SAH from a ruptured right paraophthalmic ICA blister aneurysm Pre FD stenting Post FD stenting 24 months f/u with no residual/recurrence
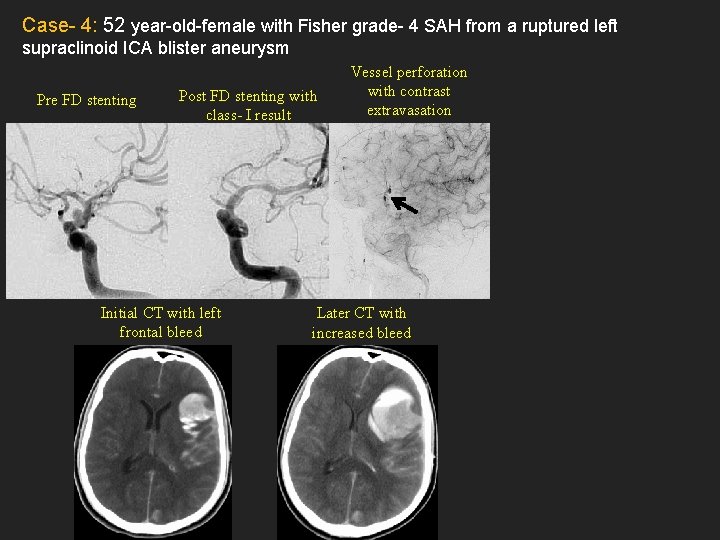
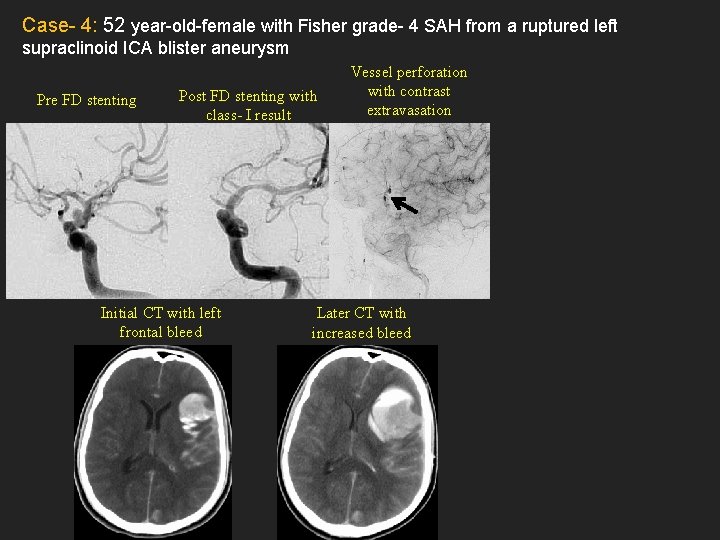
Case- 4: 52 year-old-female with Fisher grade- 4 SAH from a ruptured left supraclinoid ICA blister aneurysm Pre FD stenting Post FD stenting with class- I result Initial CT with left frontal bleed Vessel perforation with contrast extravasation Later CT with increased bleed
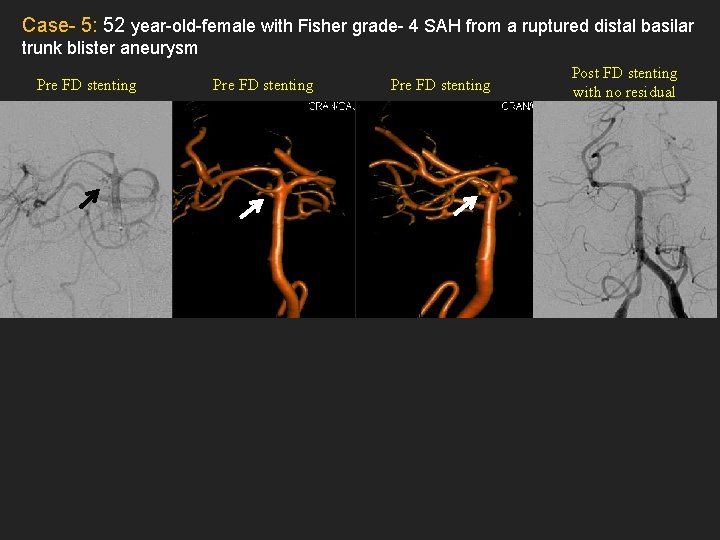
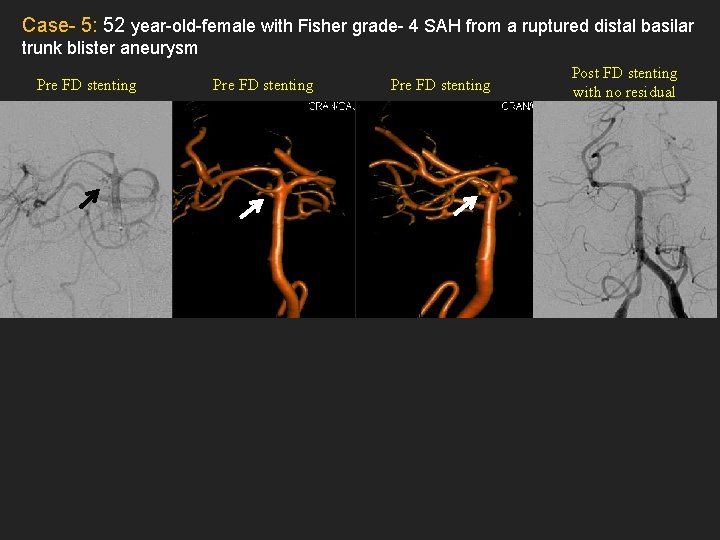
Case- 5: 52 year-old-female with Fisher grade- 4 SAH from a ruptured distal basilar trunk blister aneurysm Pre FD stenting Post FD stenting with no residual
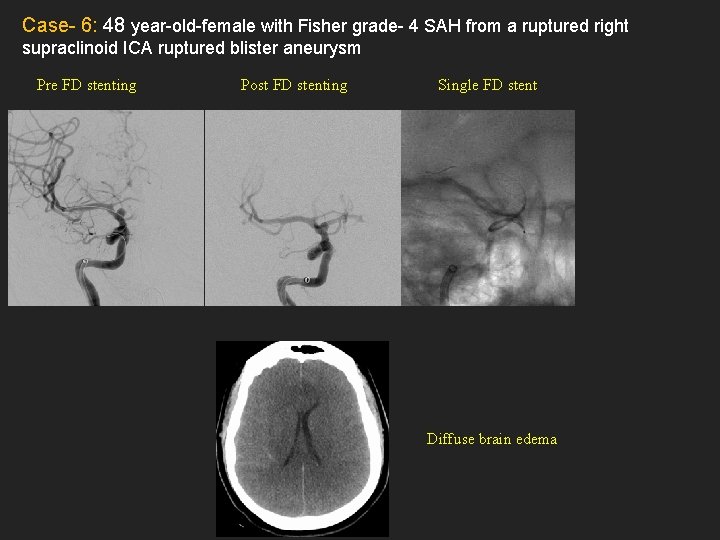
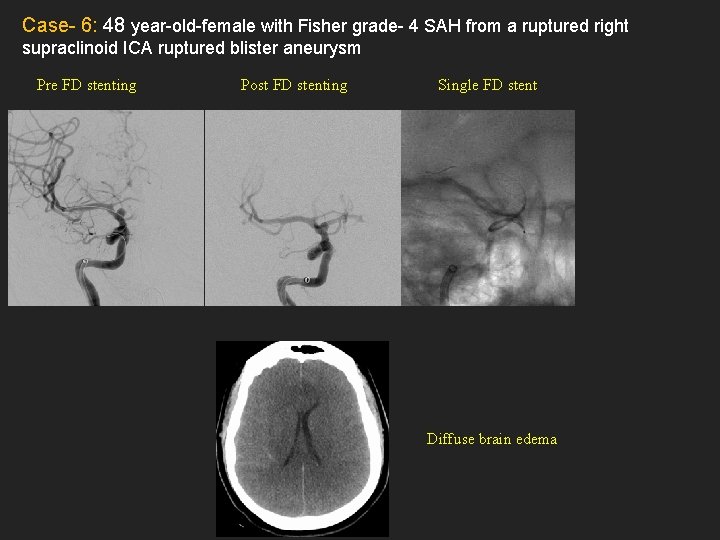
Case- 6: 48 year-old-female with Fisher grade- 4 SAH from a ruptured right supraclinoid ICA ruptured blister aneurysm Pre FD stenting Post FD stenting Single FD stent Diffuse brain edema
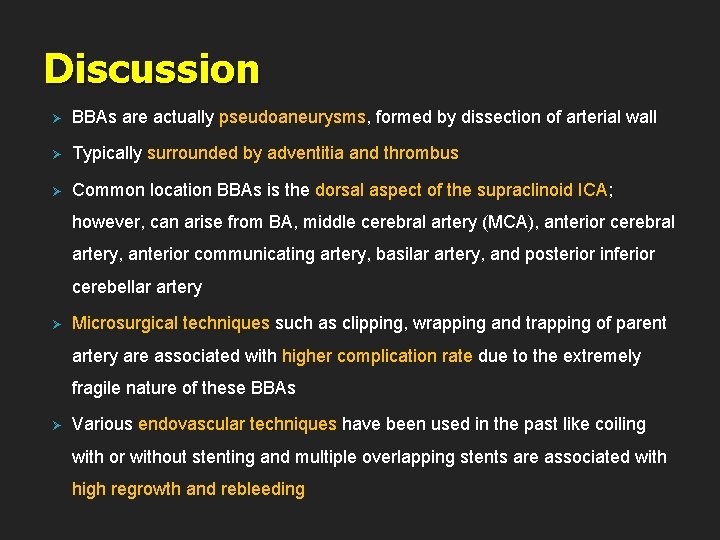
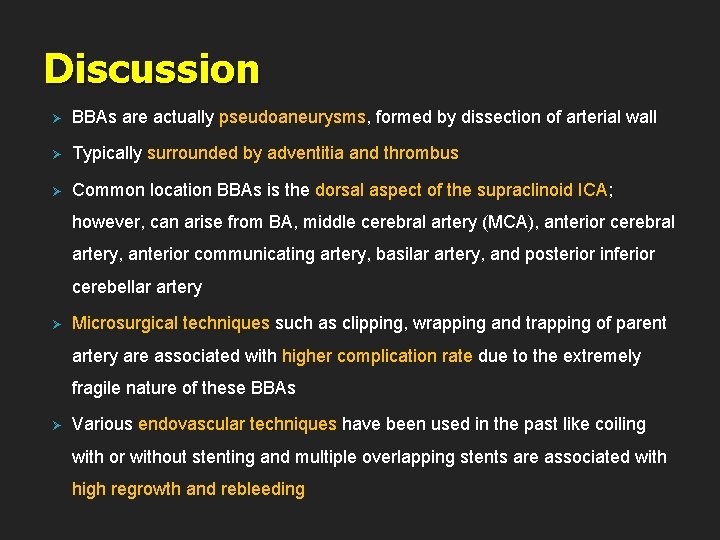
Discussion Ø BBAs are actually pseudoaneurysms, formed by dissection of arterial wall Ø Typically surrounded by adventitia and thrombus Ø Common location BBAs is the dorsal aspect of the supraclinoid ICA; however, can arise from BA, middle cerebral artery (MCA), anterior cerebral artery, anterior communicating artery, basilar artery, and posterior inferior cerebellar artery Ø Microsurgical techniques such as clipping, wrapping and trapping of parent artery are associated with higher complication rate due to the extremely fragile nature of these BBAs Ø Various endovascular techniques have been used in the past like coiling with or without stenting and multiple overlapping stents are associated with high regrowth and rebleeding
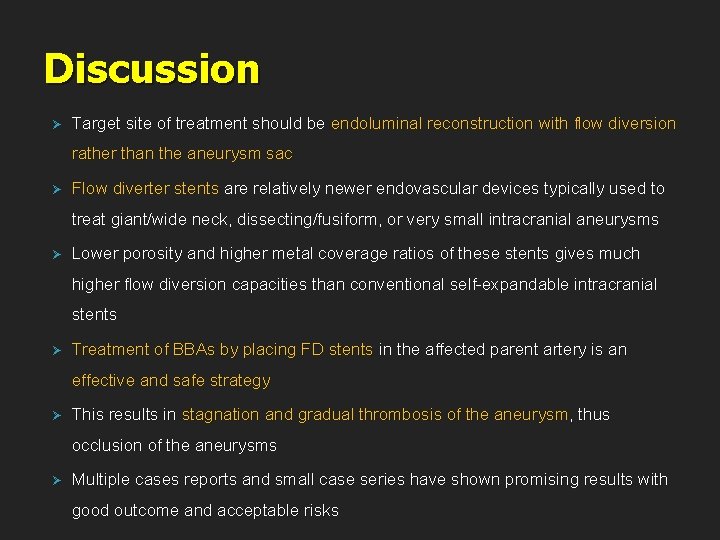
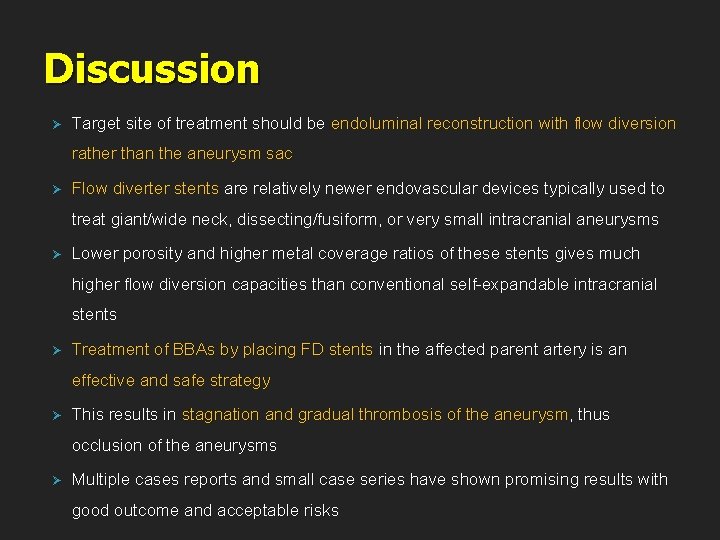
Discussion Ø Target site of treatment should be endoluminal reconstruction with flow diversion rather than the aneurysm sac Ø Flow diverter stents are relatively newer endovascular devices typically used to treat giant/wide neck, dissecting/fusiform, or very small intracranial aneurysms Ø Lower porosity and higher metal coverage ratios of these stents gives much higher flow diversion capacities than conventional self-expandable intracranial stents Ø Treatment of BBAs by placing FD stents in the affected parent artery is an effective and safe strategy Ø This results in stagnation and gradual thrombosis of the aneurysm, thus occlusion of the aneurysms Ø Multiple cases reports and small case series have shown promising results with good outcome and acceptable risks
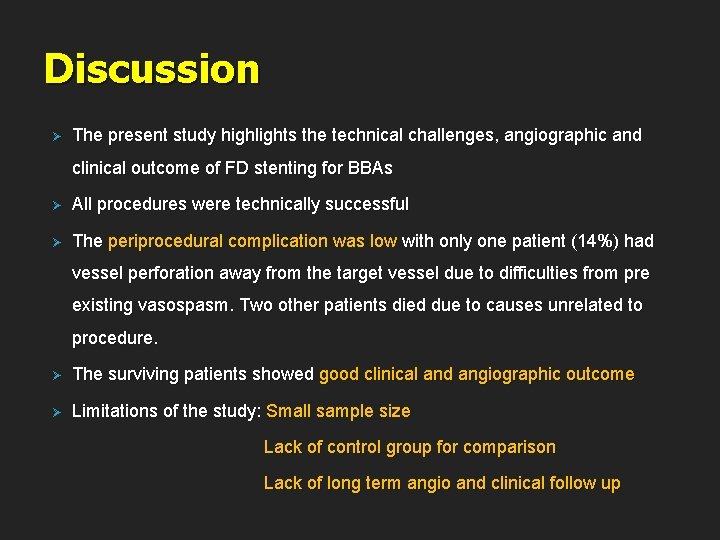
Discussion Ø The present study highlights the technical challenges, angiographic and clinical outcome of FD stenting for BBAs Ø All procedures were technically successful Ø The periprocedural complication was low with only one patient (14%) had vessel perforation away from the target vessel due to difficulties from pre existing vasospasm. Two other patients died due to causes unrelated to procedure. Ø The surviving patients showed good clinical and angiographic outcome Ø Limitations of the study: Small sample size Lack of control group for comparison Lack of long term angio and clinical follow up
Conclusion Ø The use of endovascular treatment for BBAs is still debated because of limited experience; however the results of this study and various other published literature indicate that implantation of FD stents is a feasible alternative approach for treatment of these dangerous aneurysms