Post Traumatic Stress Disorder PTSD in EMS Matthew
- Slides: 42
Post Traumatic Stress Disorder (PTSD) in EMS Matthew M Eschelbach, MS, DO, FACEP, CPE Medical Director of EMS and Trauma St. Charles Medical Center Redmond
Goals � This is not Phycology 401 - Leave with an understanding of PTSD and how it may present. � Learn Who is susceptible � Learn how recognize the symptoms and potentially the situations where this might occur. � Develop a plan in your department to deal with it. � Sage advice from others.
St Josephs Medical Center Philadelphia � 17 y. o. female presents to the ER with a cc of abdominal pain and vaginal bleeding. � Pt assigned to MSIV for evaluation. � Pt denies PMH, denies being “sexually active” � Vitals BP 120/65 , P 120, R 20, Temp 98. 6 F � Pelvic exam reveals vaginal bleeding with a foot protruding from the cervix. � Code 99 called by MSIV
� Spontaneous vaginal delivery within 5 minutes of a viable 25 week old fetus, HR 130 , Resp 36, BP ? ? � New born mom states, “ You're not going to try and save it are you? ” � Trauma GSW is brought into ER as child is being delivered. � No OB in house, No ER resident, no ER attending, anesthesia in trauma bay, no intern � Code 99 Heat, umbilical line, intubation, atropine, CPR. � Hahnemann University Neonatal Resuscitation team arrives as child is pronounced 60 minutes after delivery.
Mountain View Hospital, Madras OR � 5 yo Hispanic male is brought in by EMS after a cattle gate fell on his chest at JC Fairgrounds. � Pt. is found pulseless, apneic, cyanotic, down time is unknown. � EMS began CPR and transported to ER. � Pt. arrives in ER, no IV, BVM, CPR in progress, � No BP, HR 0, Temp ? ? ? � In ER IV X 2 , Epi, Atropine, � Intubation by anesthesia.
Lo siento, ya murio. � Cut down done for IV access, � CPR , and resuscitation continues for 75 minutes without ROSC. � Code called after nearly 2 hours after patient was discovered down. � Parents told in the hallway, “Lo siento , Juan, ya murio”
Central Oregon District Hospital , Redmond , OR � 14 y o male brought in from CRR after an accidental GSW to right chest. � PTA CPR, No IV, BVM, Vitals BP 0, HR 0, R 0 � Trauma Code called, IV Cutdown by EP for access, while surgeon opened the chest in the ER for direct cardiac massage. � No ROSC achieved after 60 minutes, code called. � Post mortem discovery of bullet disruption to azygous vein.
SCMC Redmond ER � 53 yo male self-inflicted GSW to right temple is brought in by EMS. GSW was un-witnessed but girlfriend reported recent divorce from wife in progress and dispute with custody of children. � Intubation by RSI on scene, two large bore IVs established. � BP 120/80, R 16 bagged, ETCO 2 37 with good wave form, HR 85, GCS 3. Trauma Code called PTA
Redirected Goal for Treatment � PE large entry wound in right temple with golf ball sized exit wound in left temple. � BP begins to drop to 90/60 bleeding remains brisk from head wound. Attempts to reapply pressure to scalp wound is met with crepitus and unsatisfactory tamponade of flow. � IV Dopamine/ IV Neosynephrine started � Urine Catheter output “ 0” reinserted still “ 0” � Police continue involvement � Permission for organ donation obtained. � Admission ICU/Transfer Care to transplant team
Lapine /Sunriver/ Oregon � She was 19 and hung herself from a tree in her backyard. You have the crumpled note that says goodbye. Her mother collapsed when you told her she had died. Her father wept into his hands. A chill crept up your spine. You hug your daughter extra close at home.
� What about the man whose trachea was crushed in that fight? He died from his injury, slowly, right in front of you as you struggled with his airway. � The burns from the high tension line that covered that teenager, the one whose arm was blown off by the electricity. � The 23 year old Heroin overdose who you worked desperately to save but never regains a pulse. She looks like your neice.
Post Traumatic Stress Disorder PTSD
PTSD � “Fine” and “OK” are common responses to any inquiry about how a member of the emergency team is faring after a traumatic event in the emergency department or in the field , which is ironic given that EDs are more prone to violence than ever before. � Violent acts are only part of a cadre of acute stressors called “personally disturbing incidents” that can lead to PTSD, which is characterized by unrelenting recollection and intrusive images that interfere with normal thinking and sleep. � (J Emerg Med 2012; 43[4]: 736. )
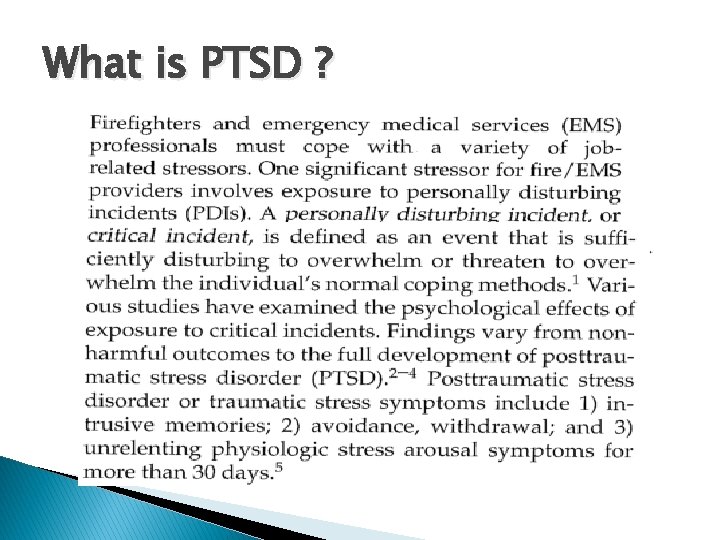
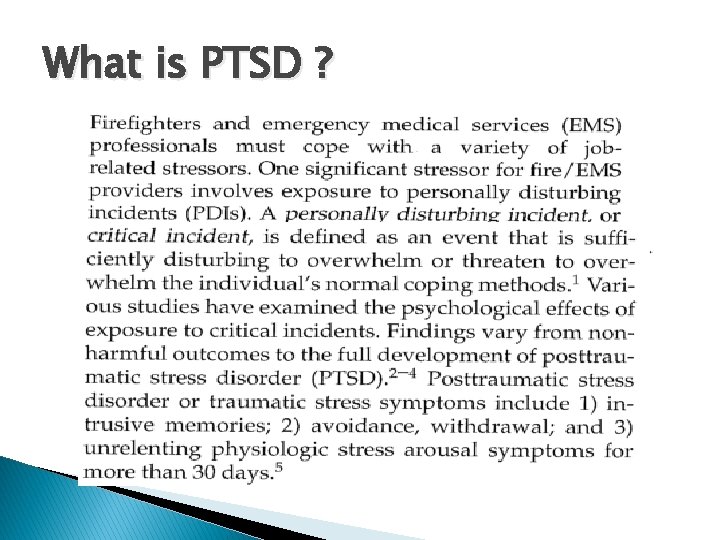
What is PTSD ?
PTSD Comes Down To � 1) Memories � 2) Withdrawal � 3) Stress
Criterion for PTSD The person has been exposed to a traumatic event in which both of the following have been present: 1. The person has experienced, witnessed, or been confronted with an event or events that involve actual or threatened death or serious injury, or a threat to the physical integrity of oneself or others. 2. The person’s response involved intense fear, helplessness, or horror. Note: in children, it may be expressed instead by disorganized or agitated behavior.
PTSD � Susceptibility seems highest when rescue efforts fail for victims injured by a crime, a fire, or a natural disaster. The risk is heightened when these occur in children or among those known by those providing medical care. EMS STRESSORS
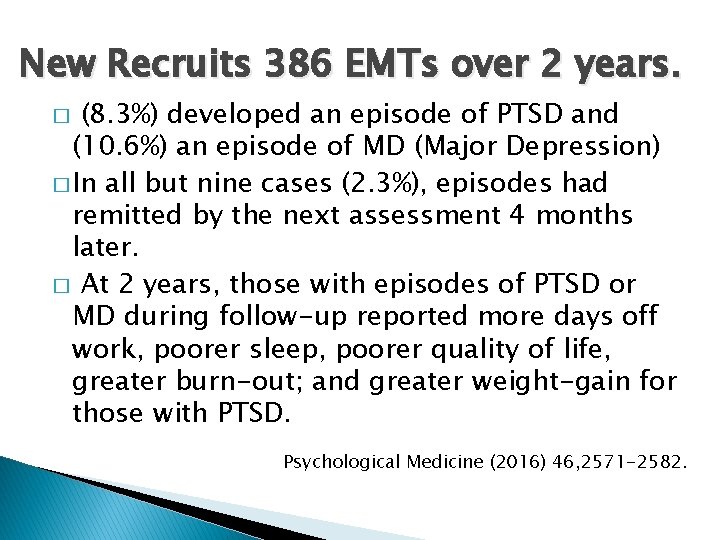
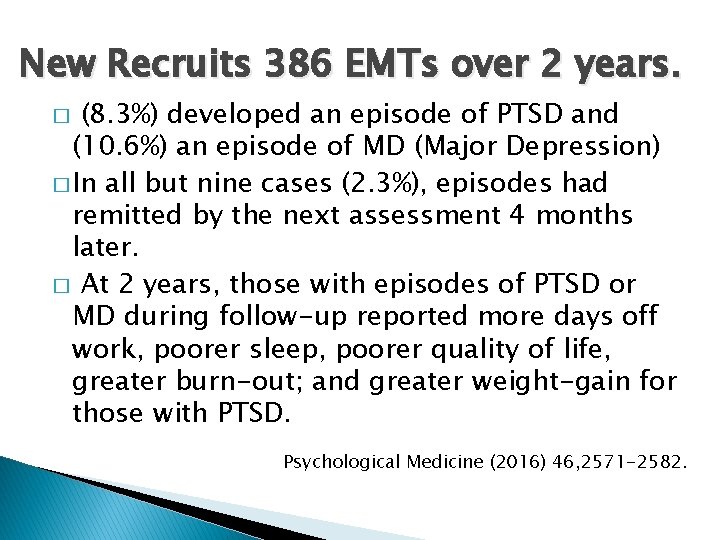
New Recruits 386 EMTs over 2 years. (8. 3%) developed an episode of PTSD and (10. 6%) an episode of MD (Major Depression) � In all but nine cases (2. 3%), episodes had remitted by the next assessment 4 months later. � At 2 years, those with episodes of PTSD or MD during follow-up reported more days off work, poorer sleep, poorer quality of life, greater burn-out; and greater weight-gain for those with PTSD. � Psychological Medicine (2016) 46, 2571 -2582.
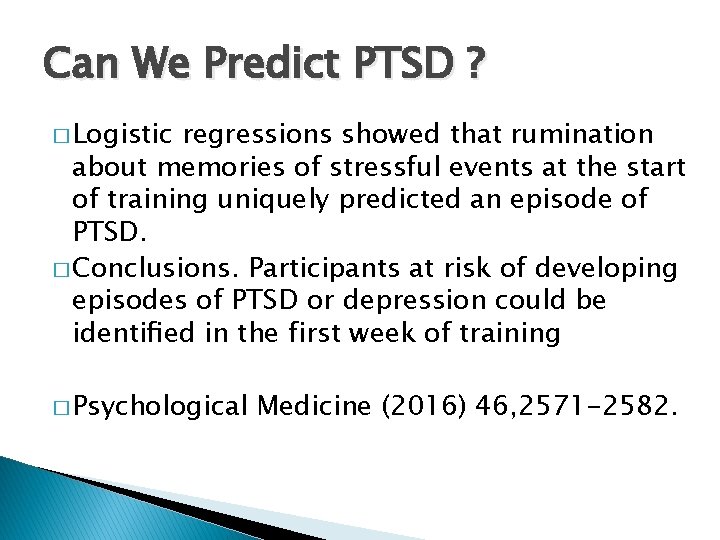
Can We Predict PTSD ? � Logistic regressions showed that rumination about memories of stressful events at the start of training uniquely predicted an episode of PTSD. � Conclusions. Participants at risk of developing episodes of PTSD or depression could be identified in the first week of training � Psychological Medicine (2016) 46, 2571 -2582.
PTSD result may be increased hostility and emotional liability, but denial or masking of mood changes is typical. � New events may trigger a learned response from a prior trauma. � Emergency physicians and nurses, and EMTs can get what is called vicarious traumatization from dealing with so much trauma � “A trigger to a flashback happens more than an EMT, MD/DO or RN on a trauma team likes to admit “ � The
Symptoms of PTSD � The main symptoms of PTSD are repeated and unwanted re-experiencing of the event, hyperarousal, emotional numbing, and avoidance of stimuli that could act as reminders of the event. � Many of the people who develop PTSD recover without treatment over the next few months, but in a substantial subgroup (30 -40%) the symptoms persist, often for many years
PTSD � Post-traumatic stress is strongly associated with multiple and recent critical incidents, particularly where professionals feel helpless in their inability to manage the physical or emotional trauma being suffered by the victim � PTSD becomes persistent when individuals process the trauma in a way that leads to a sense of serious, current threat. � The sense of threat arises as a consequence of excessively negative appraisals of the trauma.
Varied presentation of post-traumatic stress disorder � Visitations to a specific geographical location � Visual and audible nightmares � A sudden belief that the traumatic event was recurring—flashbacks � Exposure to a specific event—such as anniversaries, location, and media coverage � Persistent avoidance of aspects associated with the situations that incur memories of the incident
Varied presentation of posttraumatic stress disorder � Psychogenic amnesia—an inability to recall an important aspect of the trauma � Feelings of detachment and isolation, appreciable behavioral alterations, and suppression of emotions � A change of mood and sleep pattern; increased irritability; anger; becoming inwardly concerned and less aware of surroundings, family, and work environment � Possible increase in alcohol or drug misuse � Physiological reactivity on exposure to events that symbolize or remind a person of the trauma —for example, intense fear of travel and of motor vehicles BMJ Careers 26 Feb 2005; http: //bit. ly/10 x 9 N 3 P. )
Psychogenic Amnesia Set up a scene.
Who is at risk? � Younger emergency care providers who lack strong ties to friends or family seem particularly vulnerable. � Older adults who have a network of social support seem to have more of a built-in buffer, � Emergency physicians accumulate significantly more stress compared with other salaried physicians. (Emerg Med J 2011; 28[5]: 397. )
What doesn't work? �A coping style that avoids thinking about or discussing a personally disturbing incident, that denies its impact, that attempts to deal with it by “sucking it up, ” Don’t, “ Suck it up”
Conversion PDI to PTSD � Conversion to PTSD is associated with a sense of isolation � Studies on soldiers suggest it is likely to occur in a culture that values action over talk and discourages seeking emotional support. � Not sharing such damaging experiences with family or friends outside of work range from a desire to shield loved ones to the perception that telling others may lead to prurient fascination, which is counterproductive to feeling understood. � Feelings of shame and guilt can be activated with new impunity in the absence of a sympathetic listener.
PTSD � More than four percent of 159 physicians in rural or remote areas of Ontario, Canada, met the criteria for the PTSD, and the disorder was associated with overwork, lack of resources, and relational problems. � A personally disturbing incident can happen even in a situation where there is not the remotest chance for a different outcome, such as a resuscitation attempt for a bystander already dead from a hail of bullets. (Fam Pract 2010; 27[3]: 339. )
� 4% of EMS personnel in a Hawaiian survey met clinical diagnostic criteria for PTSD. � 83 % reported experiencing some symptoms of it. � Analysis showed that serious injury or death of a co-worker along with incidents involving children were considered very stressful; � General work conditions also contributed to the overall stress levels. (Emerg Med J 2010; 27[9]: 708. )
Recognizing PTSD untreated or unaddressed, detachment or overreaction to patients can begin to occur. � “Downplaying” a patient's physical complaints or proffering responses to him that clearly only provide “lip service. ” � Conversely, those with PTSD can over-identify with someone seeking medical attention in a way that may make the health care provider seem like a crusader, expressing self-anger at not being able to do enough for a particular patient or voicing hostility against colleagues who set ordinary and appropriate treatment boundaries. (Torture 2006; 16[1]: 1. ) � Left
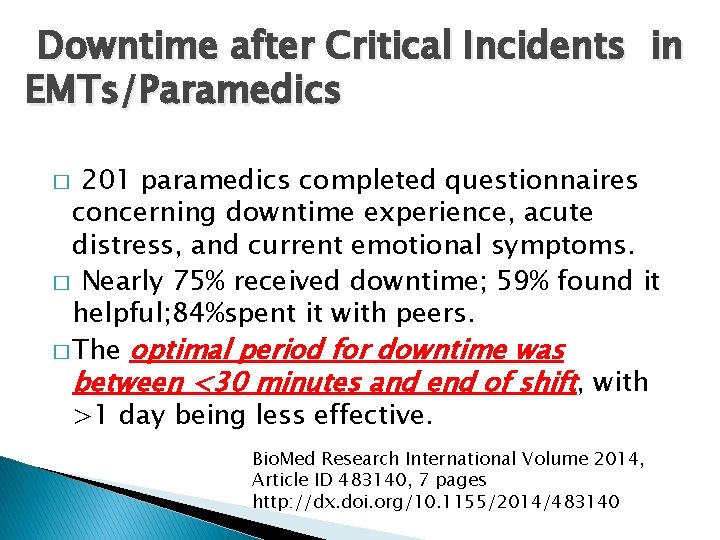
Downtime after Critical Incidents in EMTs/Paramedics 201 paramedics completed questionnaires concerning downtime experience, acute distress, and current emotional symptoms. � Nearly 75% received downtime; 59% found it helpful; 84%spent it with peers. � The optimal period for downtime was between <30 minutes and end of shift, with >1 day being less effective. � Bio. Med Research International Volume 2014, Article ID 483140, 7 pages http: //dx. doi. org/10. 1155/2014/483140
� Downtime after a critical incident is significantly associated with lower depressive symptoms scores in EMT/paramedics on long-term follow-up. � This association is mediated by neither faster recovery from acute stress nor feeling helped by others during the downtime. � The optimum length of downtime seems to be up to one day. � Since depression is an important long-term outcome of critical incidents in EMT/paramedics, a brief downtime period may be a worthwhile intervention for EMS organizations to adopt.
Prevention of PTSD-Failures can occur even in the most nurturing environment as a result of the perception of the traumatic experience. � Some psychological therapies have a track record for effectively treating most of those affected by PTSD, � Cognitive behavioral therapy is one example � Barriers have included cost and training. � PTSD (Psychological Science in the Public Interest 2013; 14[2]: 65. )
Evaluation � The nature of the evaluation for PTSD can vary widely depending on how the evaluation will be used and the training of the professional evaluator. An interviewer may take anywhere from 15 minutes to eight or more 1 hour sessions when the information is needed for legal or disability claims. Regardless of the length of the evaluation, it will include in-depth questioning of the traumatic event and symptoms being experienced as a result of these experiences.
Evaluation Continued More thorough assessments are likely to include: � Detailed structured interviews and psychological tests on which you record your thoughts and feelings � Close family member may be asked to provide more information � Client may undergo a procedure that examines your physiological reactions (heart rate, blood pressure, plasma NE measurements) to mild reminders of your trauma.
Treatment �Individual Therapy �Group Support (especially for Chronic PTSD) �Medication
Treatment � Acute PTSD - Stress debriefing and psychotherapy � Severe Acute PTSD - Stress debriefing, medication, group and individual psychotherapy � Chronic PTSD - Stress debriefing, medication, group and individual psychotherapy � For PTSD in children, adolescents, and geriatrics the preferred treatment is psychotherapy
Treatment � Exposure Therapy- Education about common reactions to trauma, breathing retraining, and repeated exposure to the past trauma in graduated doses. The goal is for the traumatic event to be remembered without anxiety or panic resulting. � Cognitive Therapy- Separating the intrusive thoughts from the associated anxiety that they produce. � Stress inoculation training- variant of exposure training teaches client to relax. Helps the client relax when thinking about traumatic event exposure by providing client a script.
Treatment � “Cognitive Restructuring involves; � Reinforcing self-monitoring of thoughts and emotions, � Identifying distressing emotions, � Learning about different types of cognitive distortions � Working to get rid of them. (Mc. Donagh, A. , Mc. Hugo, G. , Sengupta, A, Demment C. C. , et al. , (2005) Randomized Trial of Cognitive-Behavioral Therapy for Chronic Posttraumatic Stress Disorder in Adult Female Survivors of Childhood Sexual Abuse. Journal of Consulting and Clinical Psychology, 73, 515524. )
The End Questions ? ?