POST PRIMARY TUBERCULOSIS ADULT TYPE TUBERCULOSIS Tuberculosis after
POST PRIMARY TUBERCULOSIS -ADULT TYPE TUBERCULOSIS -Tuberculosis after development of immunity --Most important because most common
PATHOGENESIS n (1) Direct Progression of primary lesion - 95% Primary lesions heal without treatment - 5% develop progressive disease - In some lesions there is caseous necrosis and liquefaction of central part of lesion. This liquefied material may reach to other parts of the lung or contra lateral lung via bronchi causing post primary TB- Bronchogenic spread
WAYS ……. (2)- Activation of quiscent primary or post primary lesion -May occur any time in patient’s life -Dormant bacilli become virulent whence there is waning of immunity due to any reason n
Predisposing Factors n n (1) Nutrition- Malnutrition (2) Housing-Poor Housing, Over crowding (3) Occupation- silicosis: - stone cutters, masons, coal miners etc Silica-silicic acid -►Toxic effect on pulmonary macrophages-►decrease in number causing lowering of lung defences (4) Alcoholism – malnutrition and direct effect on host defences
Predisposing Factors……. . n n n (5) Cigarette smoking – Macrophages engulf carbon particles. Over laden macrophages burst and thus decrease in number resulting in lowering of lung immunity (6) steroids and Immunosuppressive drugs (7) concomitant diseases- Diseases associated with impaired cellular immunity such as Hodgkin's disease, leukemia, lymphoma, Diabetes, AIDS, gastractomy, Post partum etc
WAYS……. . n (3) Haematogenous spread of disease. Tubercle bacilli reach the lung from other primary focus- mainly by lymphatics primary focus-> Rt side of heart-> pulmonary arteries-> lungs may spread by bronchial arteries Primary focus-> pulmonary veins-> Lt side of heart-> aorta-> other parts of body
WAYS…………. n - (4) Exogenous infection- by inhalation of droplet nuclei source- A patient of TB INFECTIVITY OF PATIENT Smear positivity Coughing, sneezing, speaking Thickness of sputum-Tenacious sputum has more bacilli than watery sputum Living conditions – Sunlight, dilution of air Type of lung lesion- Cavity-109 bacilli - 1 Gm tissue-10 4 bacilli
PATHOLOGY n n n Tubercle formation with caseous necrosis in the center Proliferation of bacilli in caseous center followed by softening and liquefaction of caseous material which may discharge into bronchus, some is absorbed, with resultant cavity formation. Spread of caseous and liquified material through bronchial tree may disseminate the infection to other lung zones.
SITE n n n Upper lung zones- most frequently posterior segment of upper lobe or apical segment of lower lobe No part is exempt Lower lung zone TB is a little more common in immuno suppressed and elderly patients than in normal subjects.
CLINICAL FEATURES n - SYMPTOMS No symptoms Onset gradual over weeks Cough with or without expectoration Haemoptysis Fever General symptoms- malaise, tiredness, loss of appetite, loss of weight etc Night sweats Recurrent colds Chest pain
FEVER n n Low grade, Evening rise Cause of fever- Release of cytokines. Lymphocytes release lymphokines which activates Macrophages release monokines- IL-1, ץ Interferon, TNF-α, etc Much of tissue necrosis is caused by TNF-α. Its prolonged secretion is responsible for persistent low grade fever and general malaise
FEVER……… Cause of evening rise 1 - Increased BMR towards evening 2 - Increasing concentration of TNF-α in the blood towards evening As the activity of patient increases after getting up in the morning, blood circulation increases and more blood passes through necrotic areas and more TNF-α is released in the blood. Its concentration is highest in the evening causing rise in temp. It gradually washes out from circulation when patient rests at night.
Haemoptysis……. n n Necrosis of blood vessels Rupture of micro aneurysms (Rasmussen’s) Antigen- Antibody reaction on the walls of blood vessels Erosion of blood vessels by a calcified focus through a bronchus.
SIGNS n n n No signs Crepitations Bronchial breathing over cavity or consolidation
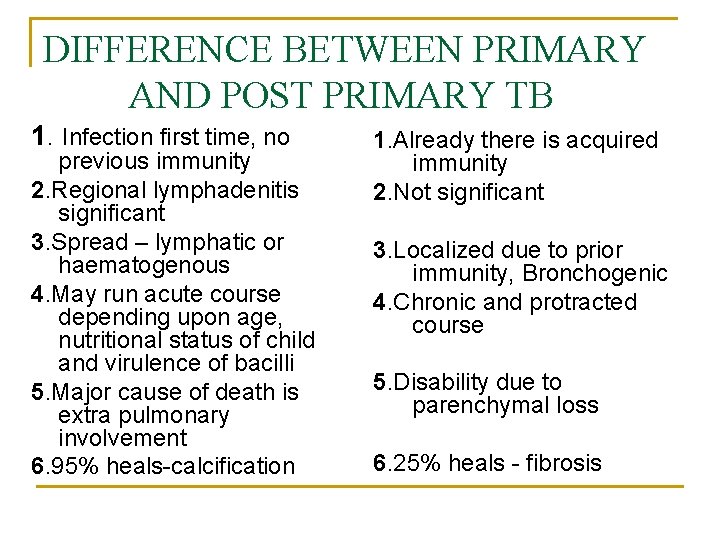
DIFFERENCE BETWEEN PRIMARY AND POST PRIMARY TB 1. Infection first time, no previous immunity 2. Regional lymphadenitis significant 3. Spread – lymphatic or haematogenous 4. May run acute course depending upon age, nutritional status of child and virulence of bacilli 5. Major cause of death is extra pulmonary involvement 6. 95% heals-calcification 1. Already there is acquired immunity 2. Not significant 3. Localized due to prior immunity, Bronchogenic 4. Chronic and protracted course 5. Disability due to parenchymal loss 6. 25% heals - fibrosis
Thanks
- Slides: 16