Post ERCP Perforation Joint Hospital Surgical Grand Round



- Slides: 29
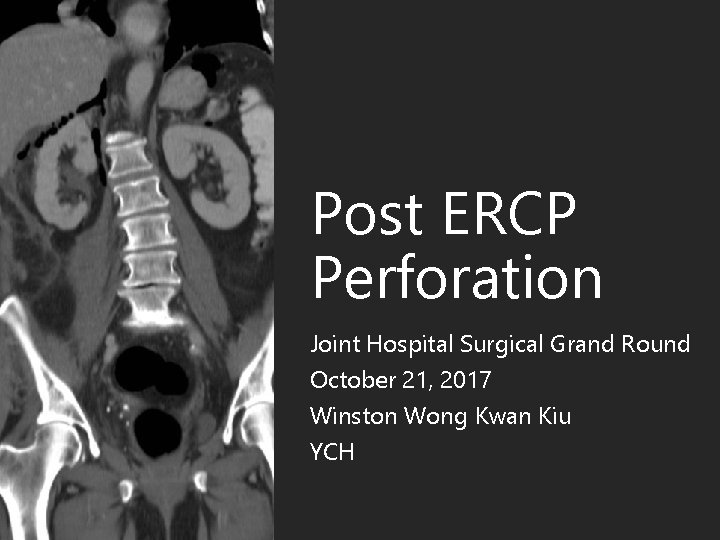
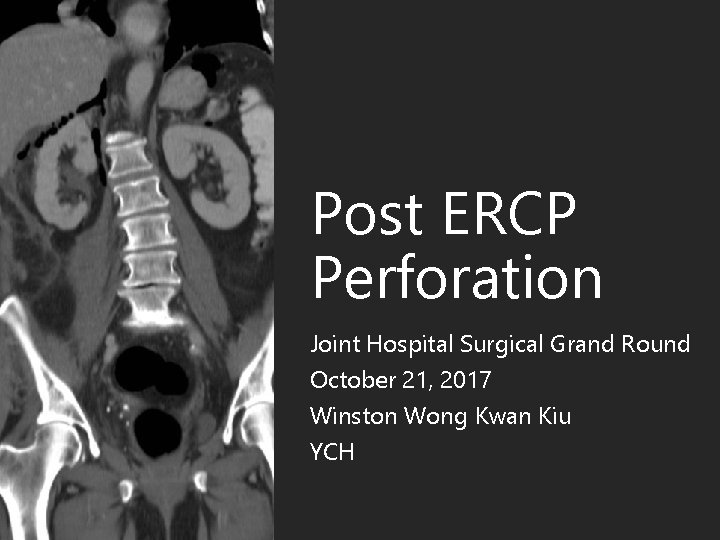
Post ERCP Perforation Joint Hospital Surgical Grand Round October 21, 2017 Winston Wong Kwan Kiu YCH
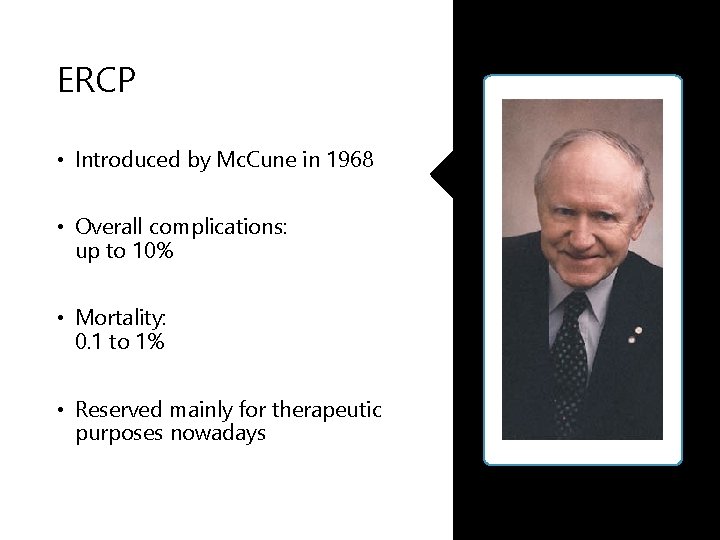
ERCP • Introduced by Mc. Cune in 1968 • Overall complications: up to 10% • Mortality: 0. 1 to 1% • Reserved mainly for therapeutic purposes nowadays
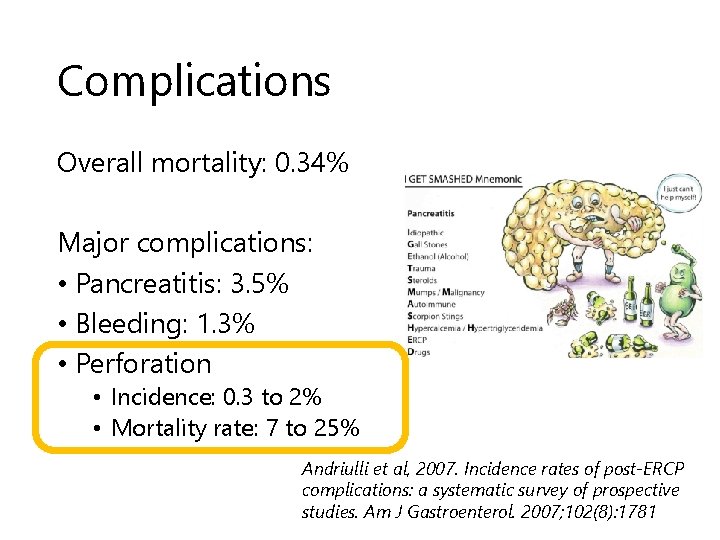
Complications Overall mortality: 0. 34% Major complications: • Pancreatitis: 3. 5% • Bleeding: 1. 3% • Perforation • Incidence: 0. 3 to 2% • Mortality rate: 7 to 25% Andriulli et al, 2007. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007; 102(8): 1781

Risk factors for perforation • Patient factors • • • Old age Suspected Sphincter of Oddi dysfunction Dilated bile duct Papillary stenosis Abnormal anatomy e. g. Billroth II reconstruction • Procedural factors • Precut sphincterotomy • Long procedure duration • Biliary stricture dilatation • Operator factors • Experience Enns et al, 2002. ERCP-related perforations: risk factors and management. Endoscopy 34: 293 -98
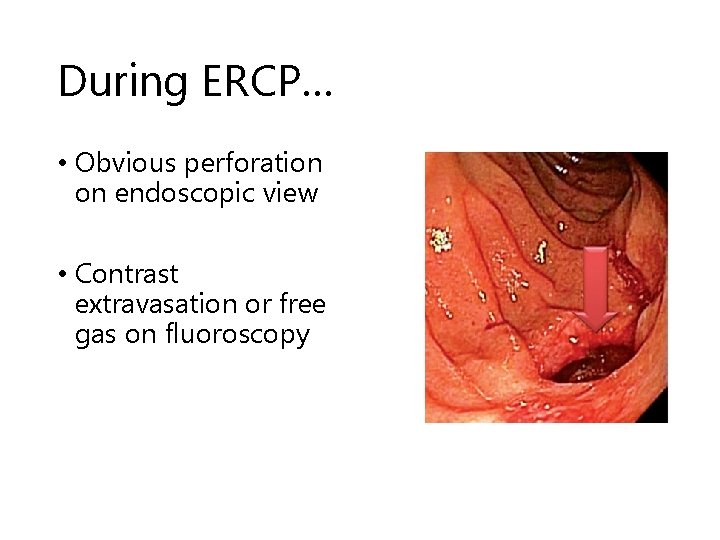
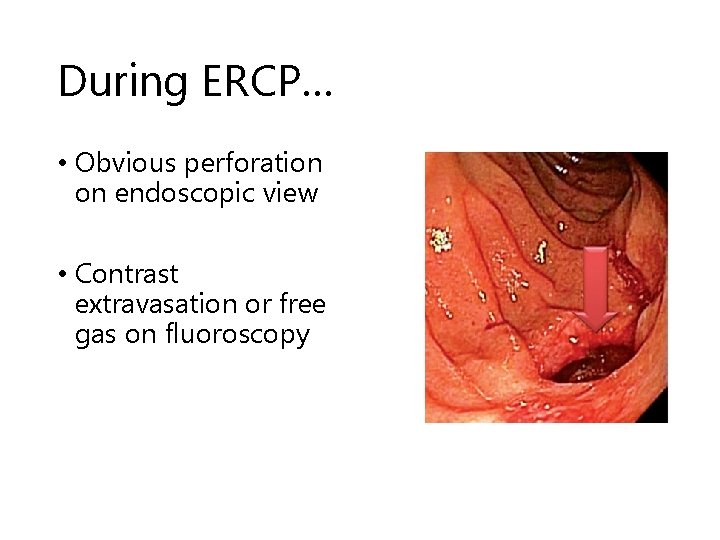
During ERCP… • Obvious perforation on endoscopic view • Contrast extravasation or free gas on fluoroscopy
After ERCP… • Sign & symptoms • • • Usually nonspecific Severe epigastric pain Vomiting Fever Epigastric tenderness progressing to boardlike rigidity • Blood tests • Also non-specific • Leukocytosis • Amylase • Raised amylase points to post-ERCP pancreatitis but may be concurrent with perforation!

1 Resuscitation 2 Establish diagnosis Management 3 Select candidates who require surgical management
Resuscitation NPO Parenteral antibiotics IVF / Parenteral nutrition Continuous close monitoring • +/- Nasogastric drainage • •
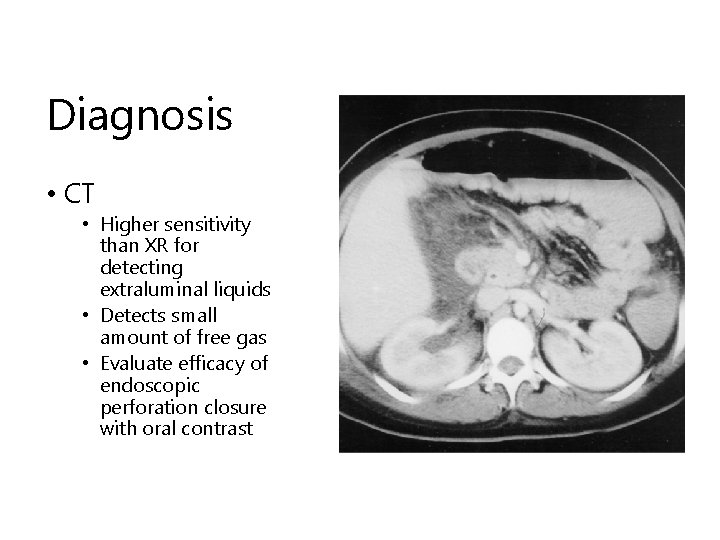
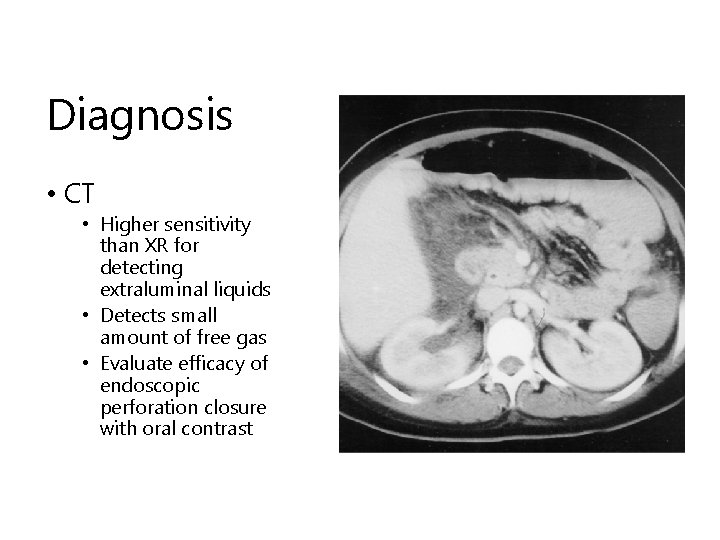
Diagnosis • CT • Higher sensitivity than XR for detecting extraluminal liquids • Detects small amount of free gas • Evaluate efficacy of endoscopic perforation closure with oral contrast
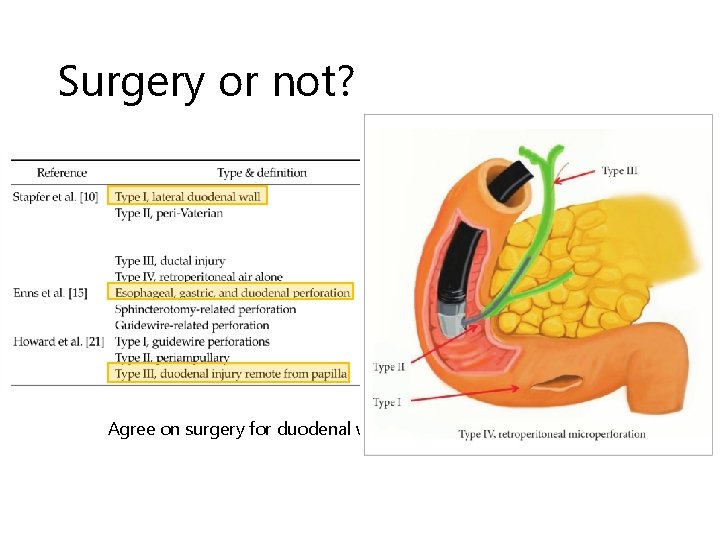
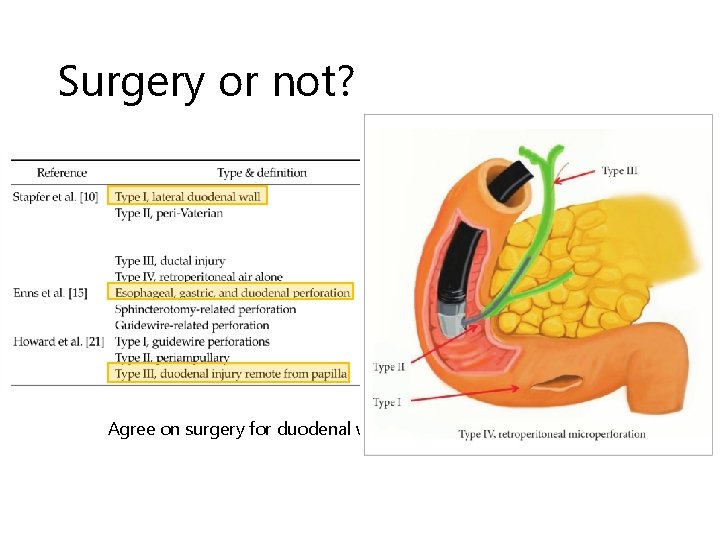
Surgery or not? Agree on surgery for duodenal wall perforation (Stapfer type 1)
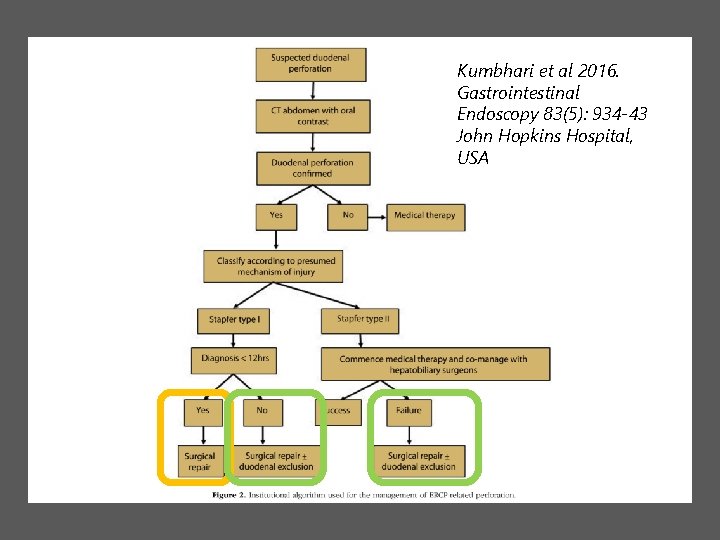
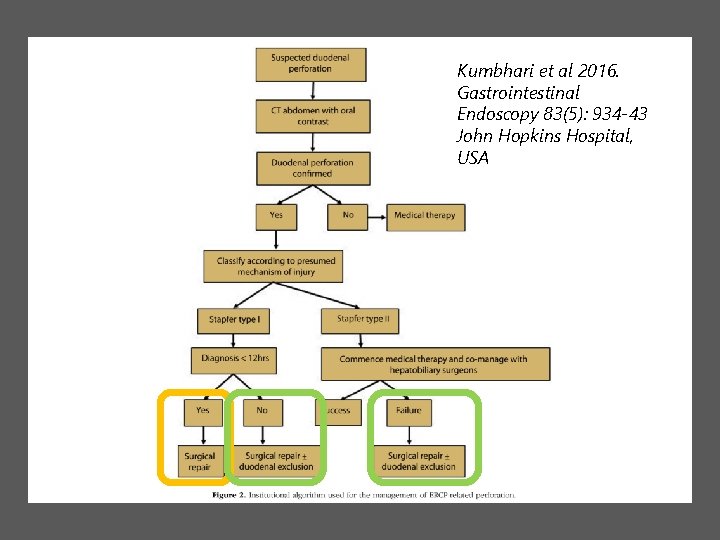
Kumbhari et al 2016. Gastrointestinal Endoscopy 83(5): 934 -43 John Hopkins Hospital, USA
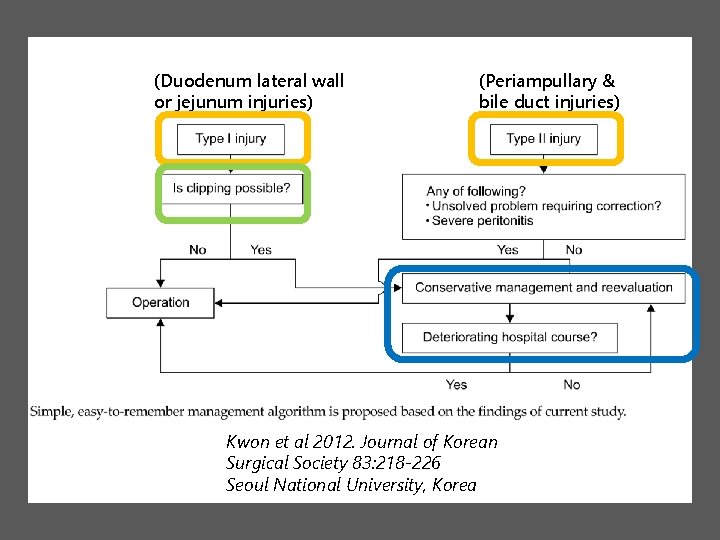
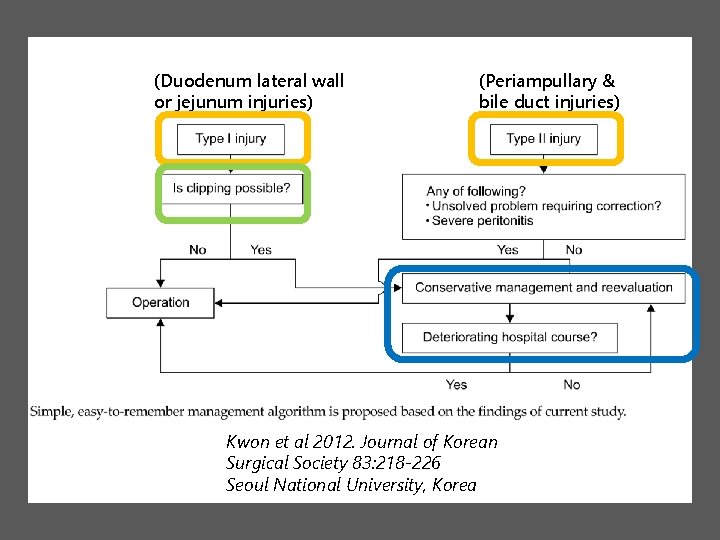
(Duodenum lateral wall or jejunum injuries) (Periampullary & bile duct injuries) Kwon et al 2012. Journal of Korean Surgical Society 83: 218 -226 Seoul National University, Korea

Paspatis et al, 2014. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy 46(8): 693 -711
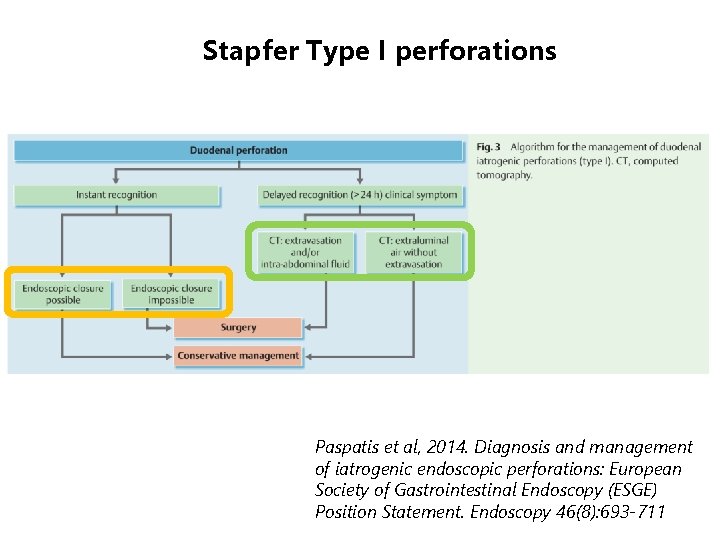
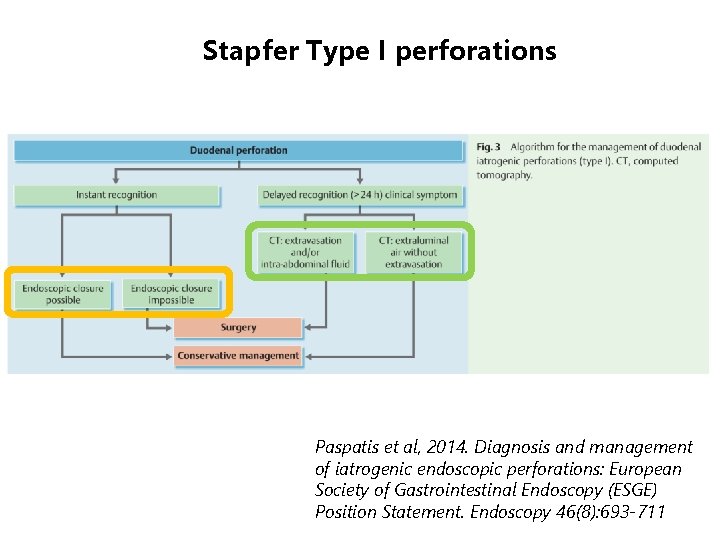
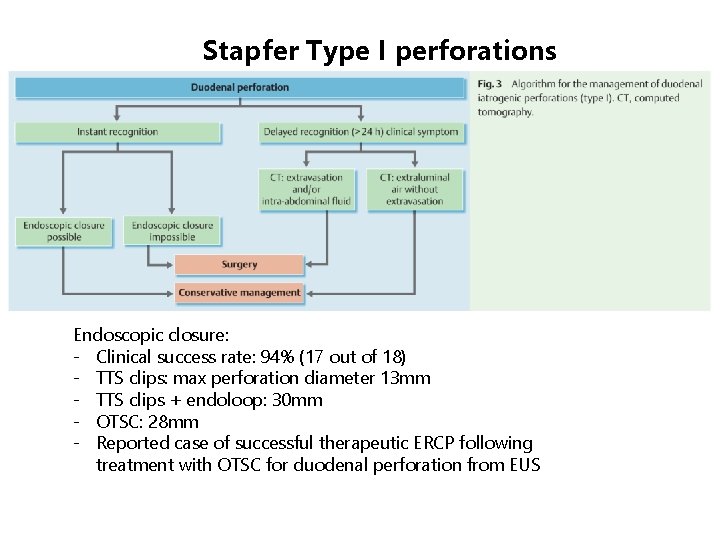
Stapfer Type I perforations Paspatis et al, 2014. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy 46(8): 693 -711
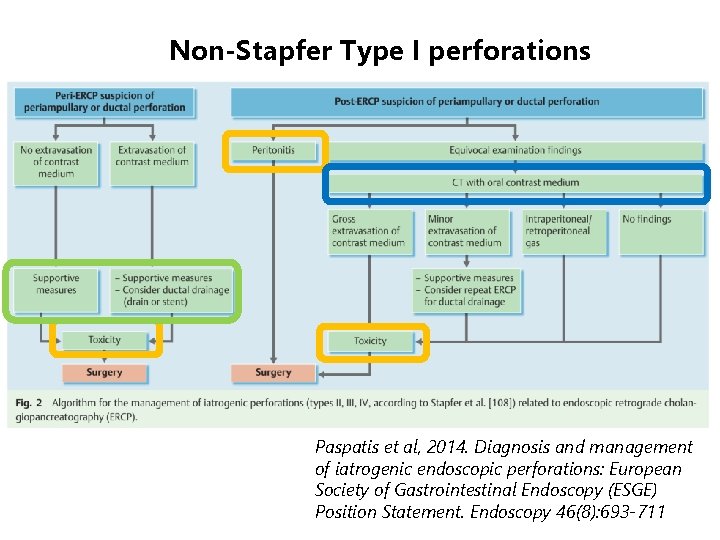
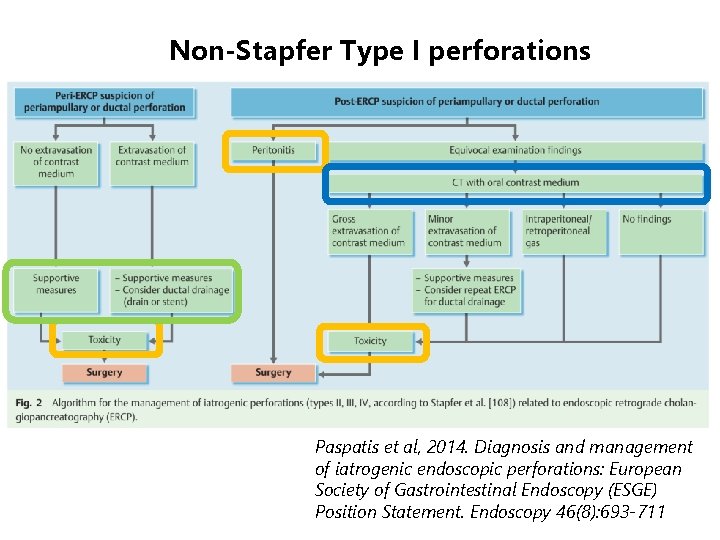
Non-Stapfer Type I perforations Paspatis et al, 2014. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy 46(8): 693 -711
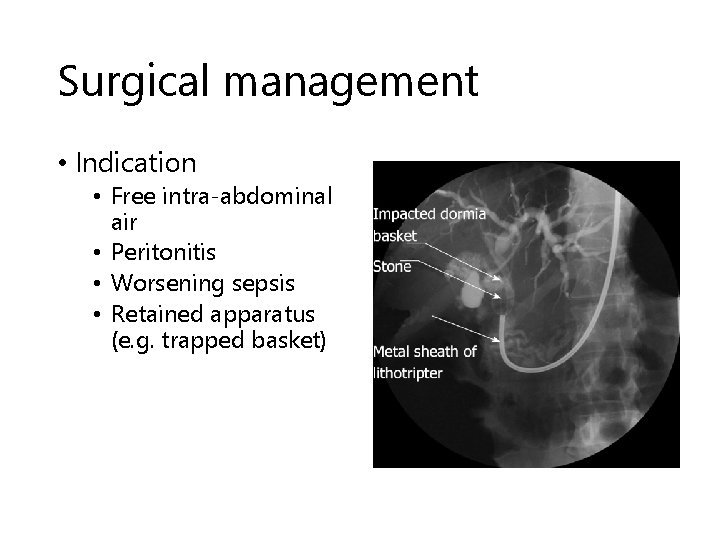
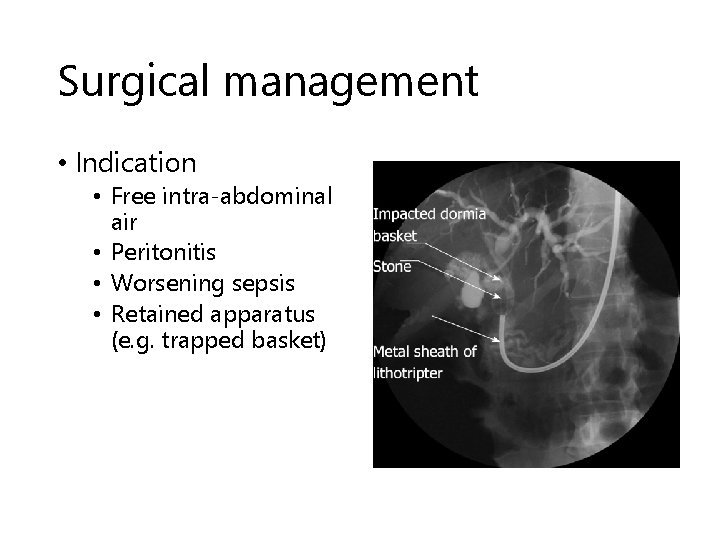
Surgical management • Indication • Free intra-abdominal air • Peritonitis • Worsening sepsis • Retained apparatus (e. g. trapped basket)
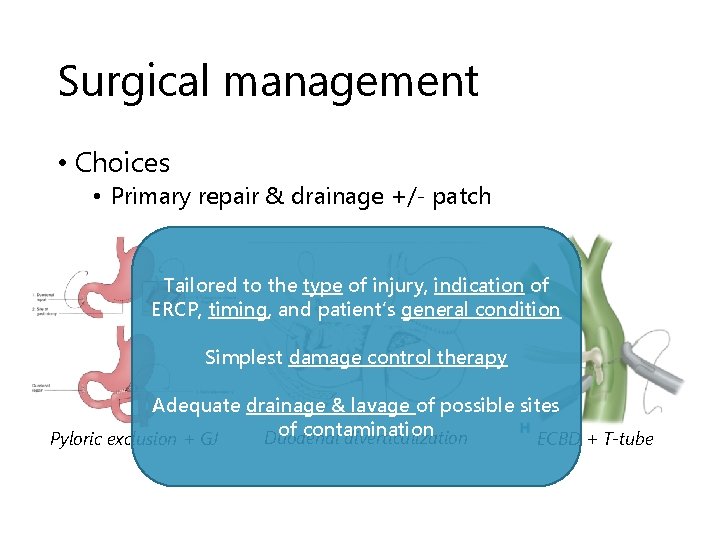
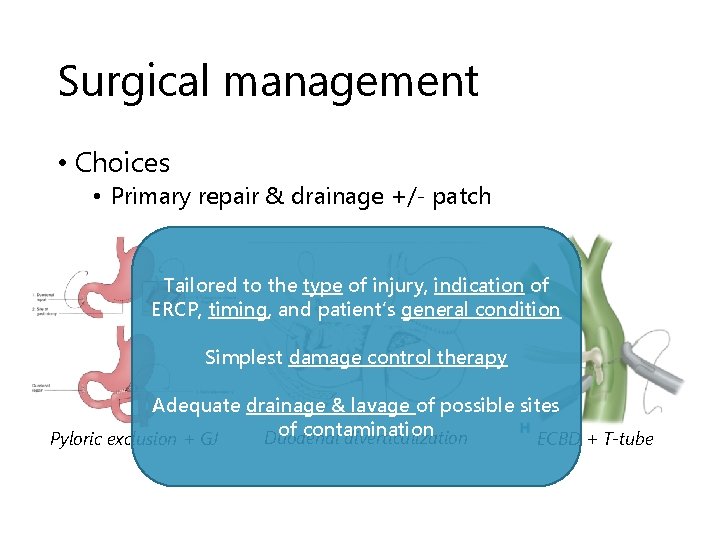
Surgical management • Choices • Primary repair & drainage +/- patch Tailored to the type of injury, indication of ERCP, timing, and patient’s general condition Simplest damage control therapy Adequate drainage & lavage of possible sites of contamination Duodenal diverticulization ECBD + T-tube Pyloric exclusion + GJ
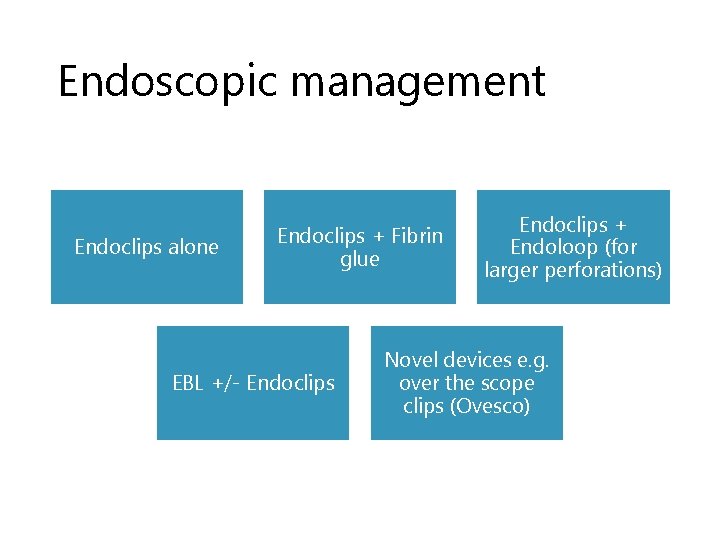
Endoscopic management Endoclips alone Endoclips + Fibrin glue EBL +/- Endoclips + Endoloop (for larger perforations) Novel devices e. g. over the scope clips (Ovesco)
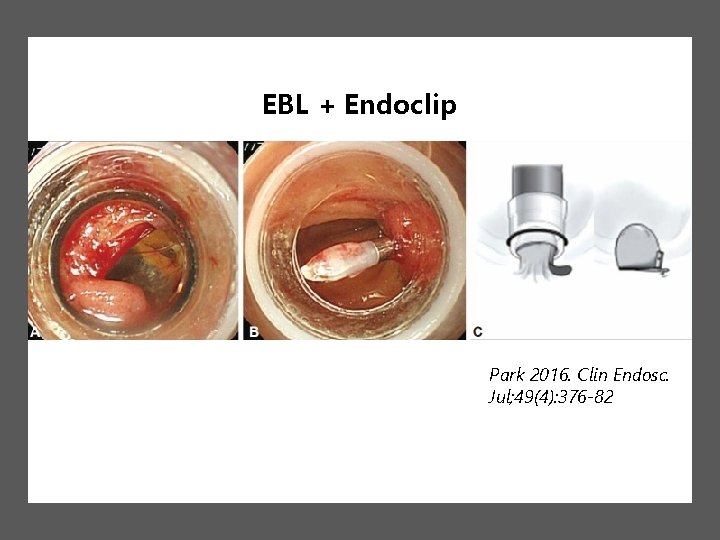
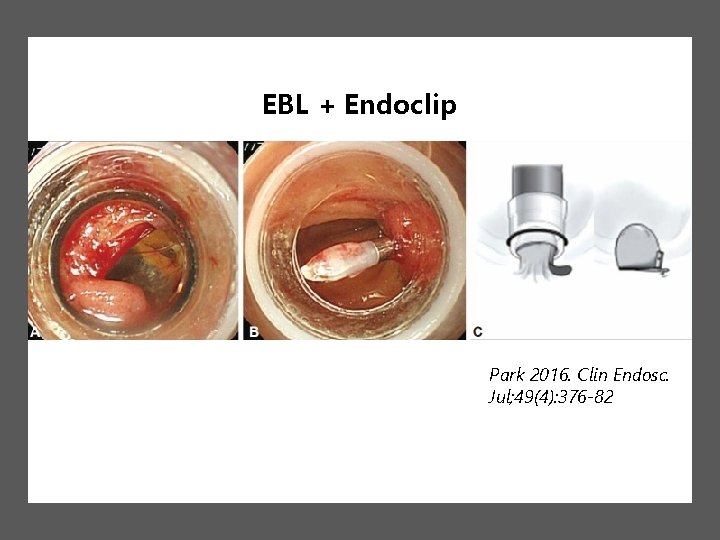
EBL + Endoclip Park 2016. Clin Endosc. Jul; 49(4): 376 -82
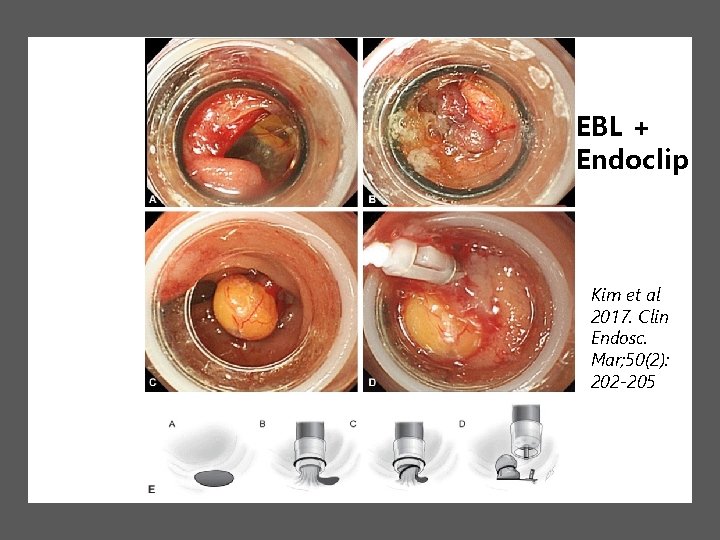
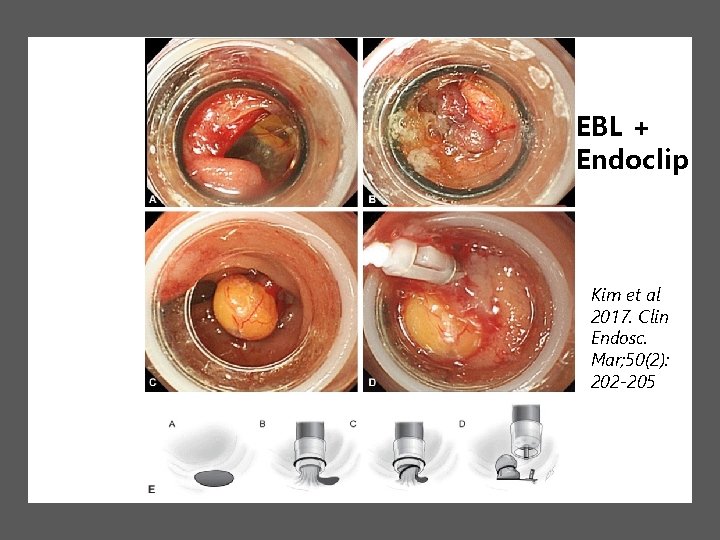
EBL + Endoclip Kim et al 2017. Clin Endosc. Mar; 50(2): 202 -205
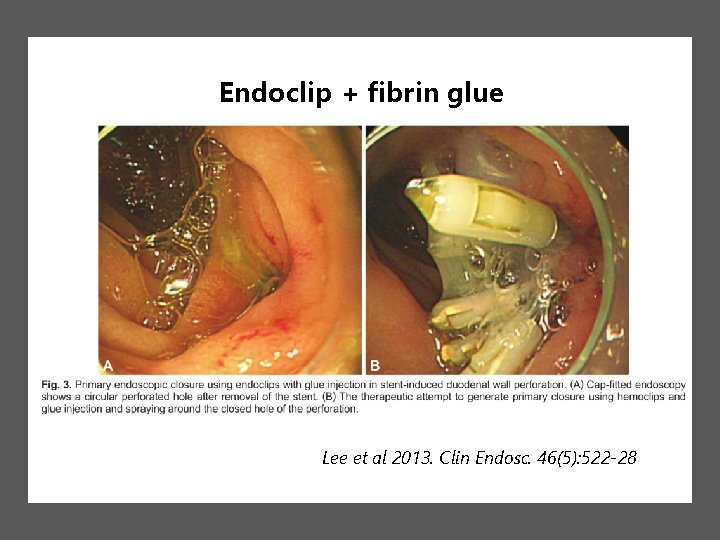
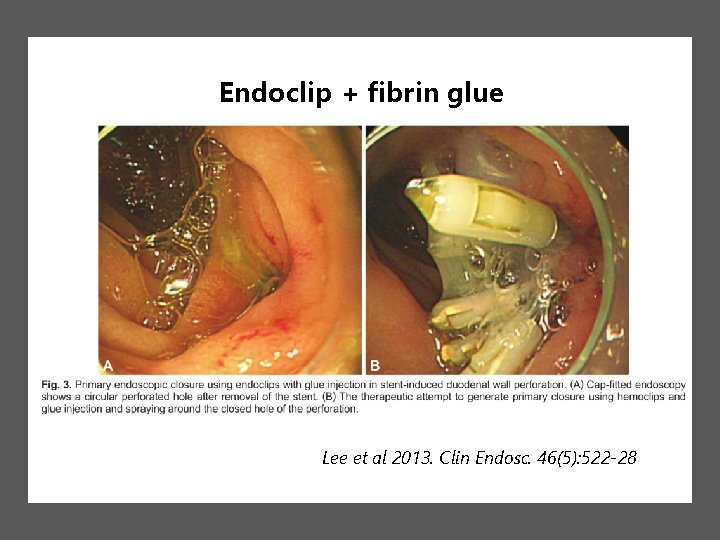
Endoclip + fibrin glue Lee et al 2013. Clin Endosc. 46(5): 522 -28
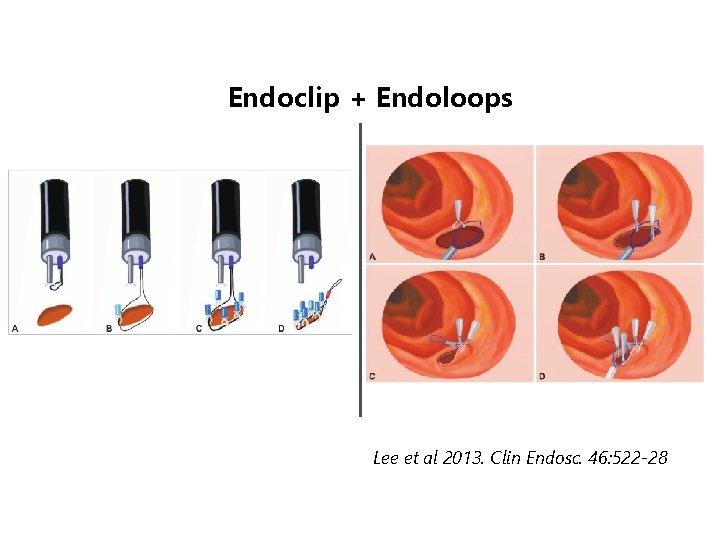
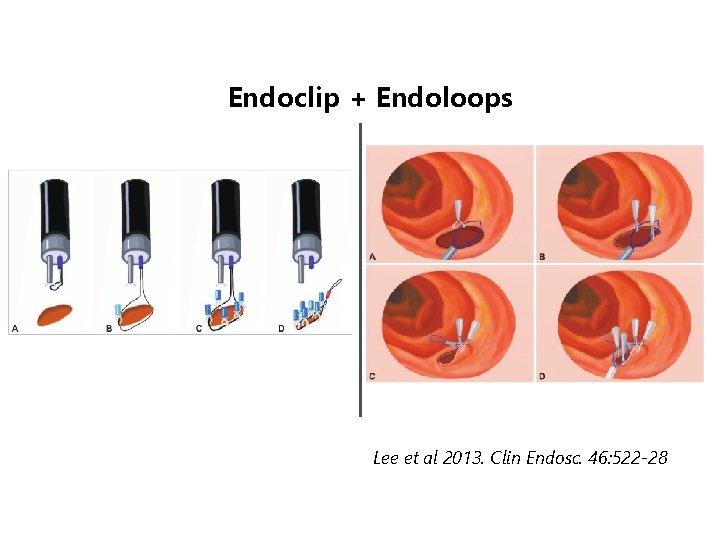
Endoclip + Endoloops Lee et al 2013. Clin Endosc. 46: 522 -28
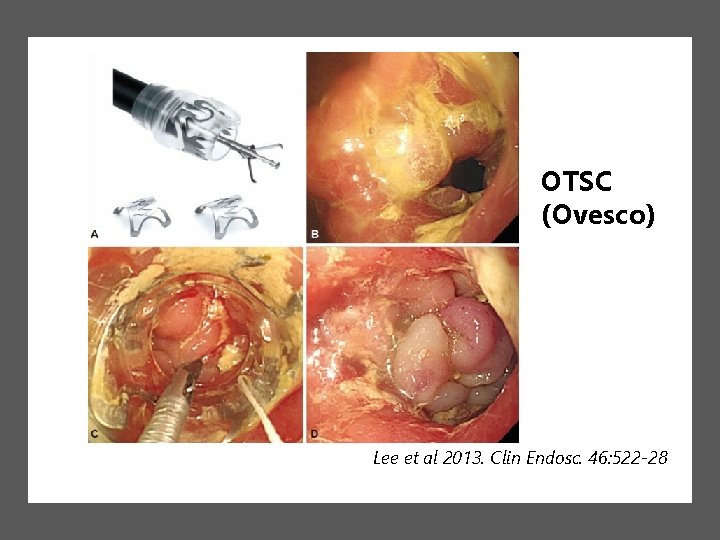
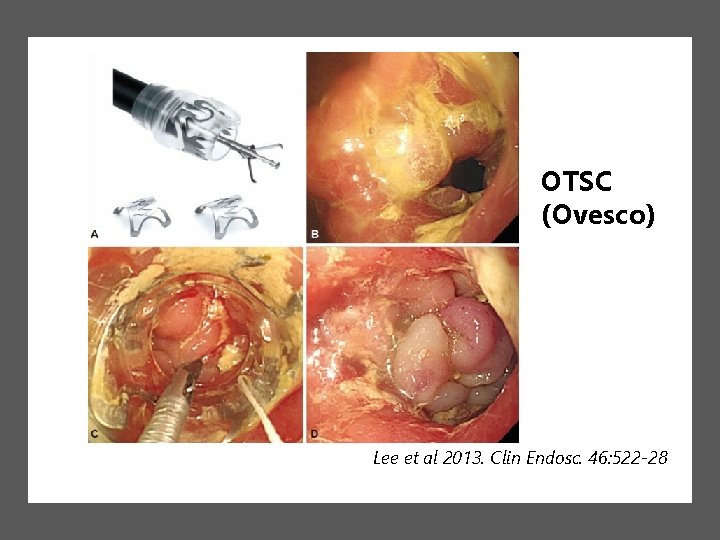
OTSC (Ovesco) Lee et al 2013. Clin Endosc. 46: 522 -28
Any consensus? • No high quality evidence • No RCTs due to ethical problems and rarity of perforations No definite guidelines
Take home messages • Prevention better than treatment. ERCP is a highly specialized procedure that should be done by experienced, skilled endoscopist to minimize complications. • Stapfer Type 1 (duodenal perforations) are best managed by surgery. Endoscopic repair is a promising option in expert hands if recognized early. • Non-duodenal perforations are managed supportively. Close monitoring is required to avoid delay in surgical treatment.
Thank you! Joint Hospital Surgical Grand Round October 21, 2017 Winston Wong Kwan Kiu YCH • Senderey A et al, 2017. Management of endoscopic retrograde cholangiopancreatography-related perforations: Experience of a tertiary center. Surgery 161(4): 920 -929. • Dubecz et al, 2012. Management of ERCP-related small bowel perforations: the pivotal role of physical investigation. Can J Zsur 55(2): 99 -104. • Kwon et al, 2012. Proposal of an endoscopic retrograde cholangiopancreatography-related perforation management guideline based on perforation type. • Lee et al, 2013. Endoscopic Treatments of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforations. Clin Endosc. 46: 522 -528. • Stapfer et al, 2000. Management of Duodenal Perforation After Endoscopic Retrograde Cholangiopancreatography and Sphincterotomy. Annals of Surgery 232(2): 191 -98. • Kumbhari et al, 2016. Algorithm for the management of ERCP-related perforations. Gastrointestinal Endoscopy 83(5): 934 -43. • Park, 2016. Recent Advanced Endoscopic Management of Endoscopic Retrograde Cholangiopancreatography Related Duodenal Perforations. Clinical Endoscopy 49(4): 376 -382. • Kim et al, 2017. Repair of an Endoscopic Retrograde Cholangiopancreatography-Related Large Duodenal Perforation Using Double Endoscopic Band Ligation and Endoclipping. Clinical Endoscopy 50(2): 202 -205. • Lee et al, 2013. Endoscopic Treatments of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforations. Clinical Endoscopy 46(5): 522 -28.
Non-surgical management • Insert biliary stent • Watch out for • Intra-abdominal fluid collection • Need drainage (percutaneous / surgical) • Sepsis • High morbidity and mortality with longer hospital stay in failed case or those delayed >24 hrs before surgery • Consider water soluble contrast study prior to resuming diet
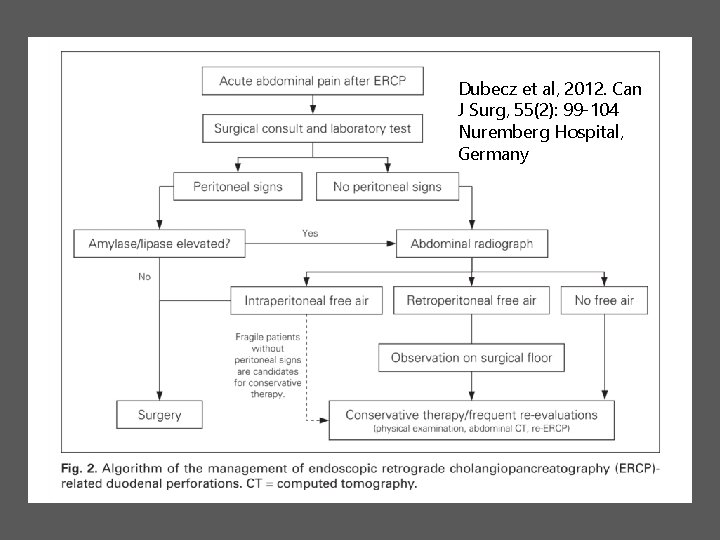
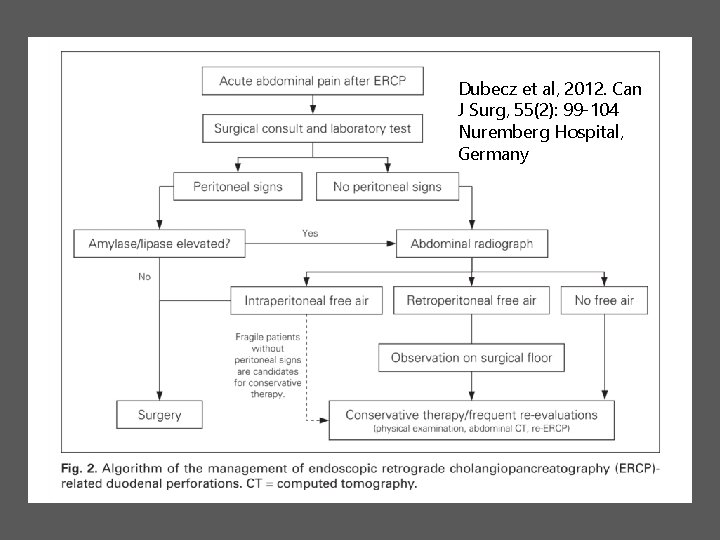
Dubecz et al, 2012. Can J Surg, 55(2): 99 -104 Nuremberg Hospital, Germany
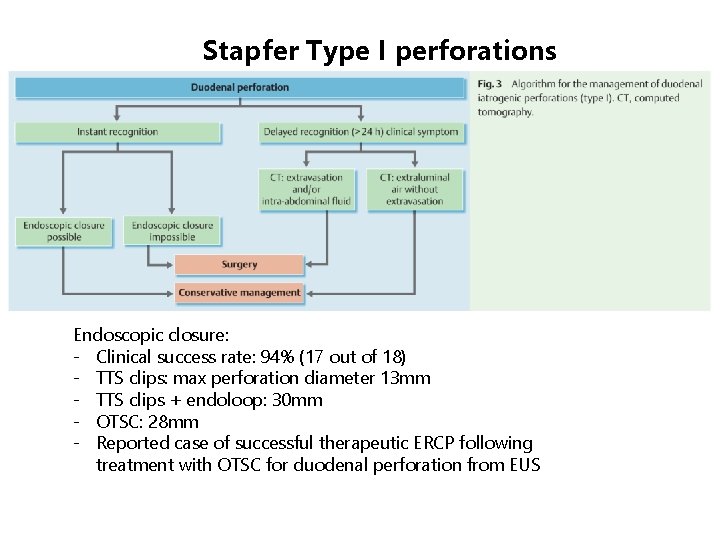
Stapfer Type I perforations Endoscopic closure: - Clinical success rate: 94% (17 out of 18) - TTS clips: max perforation diameter 13 mm - TTS clips + endoloop: 30 mm - OTSC: 28 mm - Reported case of successful therapeutic ERCP following treatment with OTSC for duodenal perforation from EUS