Positive Impact of a Structural Intervention on Knowledge
- Slides: 24
Positive Impact of a Structural Intervention on Knowledge of and Use of School-based Condom Availability Programs by Urban High School Students Emily Q. Chung MPH, CHES, Patricia Dittus, Ph. D, Christine J. De Rosa, Ph. D, Kathleen Ethier, Ph. D, Esteban Martinez, Kathy Wong, MS, Peter R. Kerndt, MD, MPH For the PROJECT CONNECT Study Team Funded by Centers for Disease Control and Prevention, Cooperative Agreement U 30/CCU 922283 -06
Condom Availability Program (CAP) • CAPs make condoms available in schools as part • • of a coordinated school health program A 1996 report found 50 school districts, 431 schools with CAPs provide opportunities § Direct interaction with students § Prevention counseling § Provision of information • CAPs vary substantially in number of condoms distributed and students served
Los Angeles Unified School District (LAUSD) CAP • Implemented in 1992 • All LAUSD high schools mandated to make • • • condoms available to students Schools set up a committee, including school nurse Committee defines parameters Condoms obtained from district coordinator Prevention materials handed out with condoms Passive parental consent
Formative Research, LAUSD CAP • Most students (55%) unaware they could get a • • condoms at school a Fewer than 1 in 4 sexually experienced students ever received condoms from CAPa Multiple barriersb a. Based § § § Left to health clinics Confusion/difficulty with consent Administrative buy-in Lack of awareness among school staff Added logistical burdens on youth surveys b. Based on key informant interviews
CAP Intervention Goals • Enhance implementation of district- mandated CAP • Increase the number of students who are aware of the CAP • Increase the number of students who receive condoms from the CAP
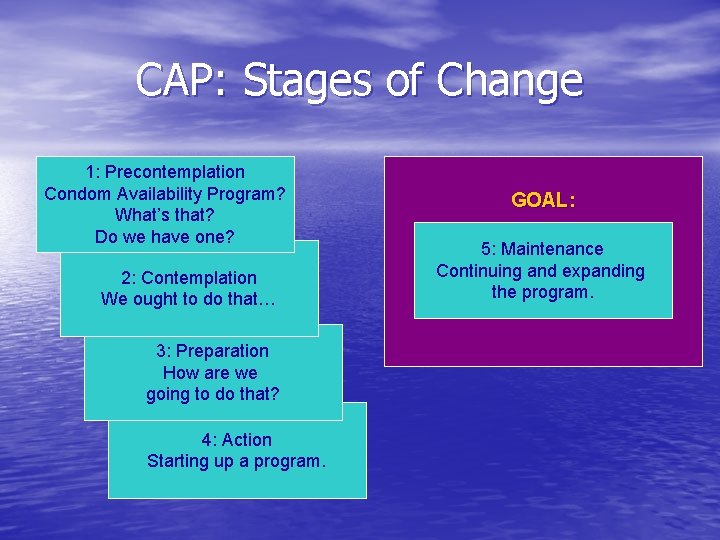
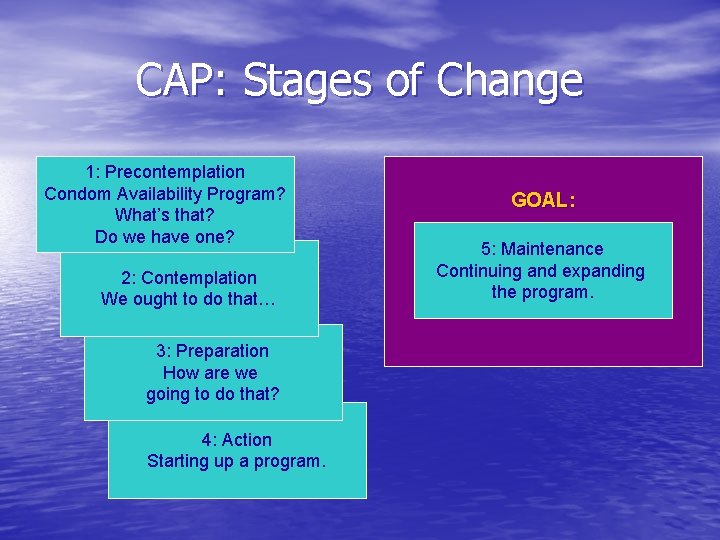
CAP: Stages of Change 1: Precontemplation Condom Availability Program? What’s that? Do we have one? 2: Contemplation We ought to do that… 3: Preparation How are we going to do that? 4: Action Starting up a program. GOAL: 5: Maintenance Continuing and expanding the program.
Activities by Stage • Stages 1 and 2: Educational meetings about policy and adolescent reproductive health • Stage 3: Self-assessment, plan and materials development • Stage 4: Implementing plan, follow-up • Stage 5: Outreach
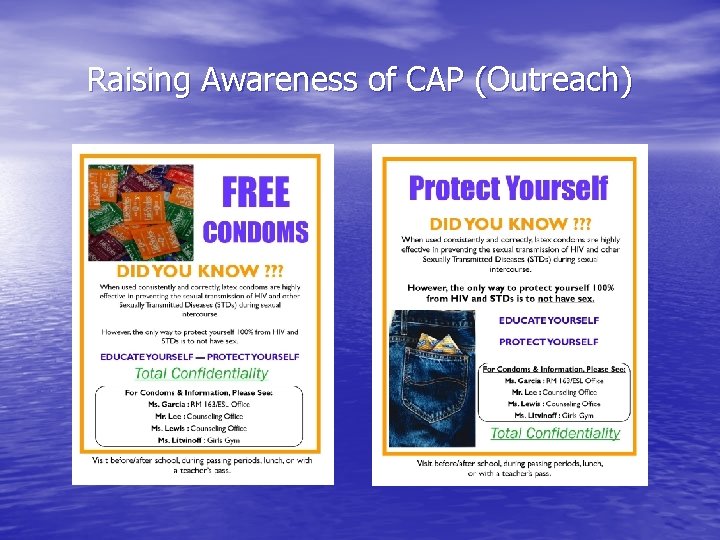
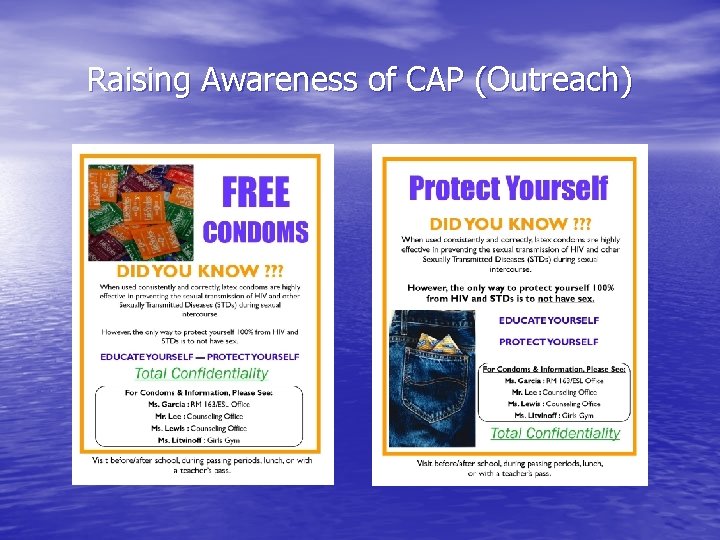
Raising Awareness of CAP (Outreach)
Youth Survey Measures • Research Question § Do our enhancements to the CAP result in increased knowledge of the program and increased use of the program? • High school surveys only § Does someone at your school (like a nurse or counselor) give out condoms to students who want them? § Have you ever gotten condoms from this person at your school?
Analysis • Chi-square analyses § Outcomes by data collection wave § Analyses performed by condition and sexual experience (yes/no) • Logistic regression models included condition, waves, and condition X wave interaction terms • Analyses restricted to high school students
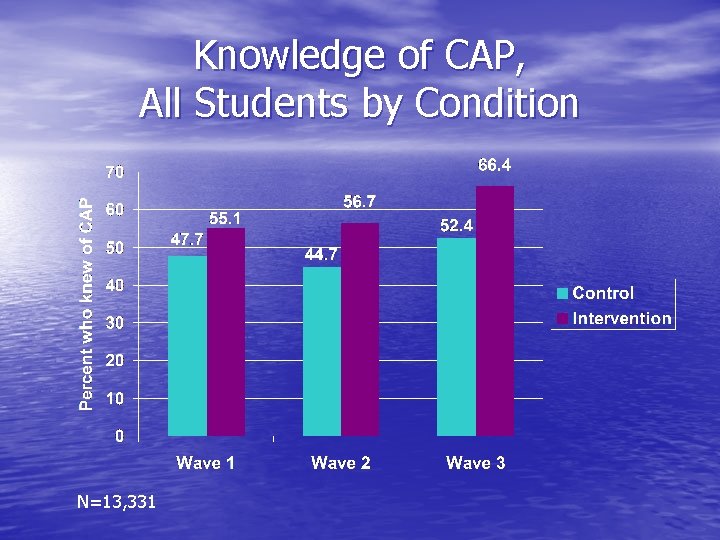
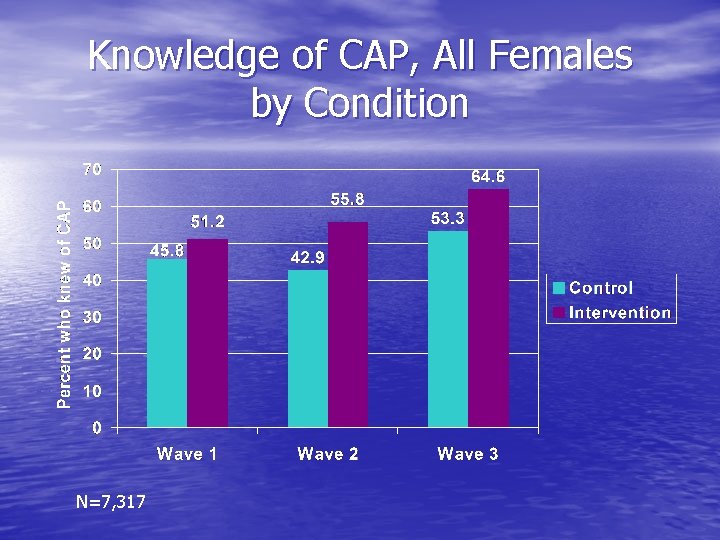
Change in Knowledge of CAP Among all participants: Increase in knowledge of CAP across waves was significantly greater for intervention than control participants § 55. 1% - 56. 7% - 66. 4% vs. 47. 7% - 44. 7% - 52. 4%, wave X condition interactions p<. 05 Driven by change among intervention females § 51. 2% - 55. 8% - 64. 6% vs. 45. 8% - 42. 9% - 53. 3%, wave X condition interactions p<. 05
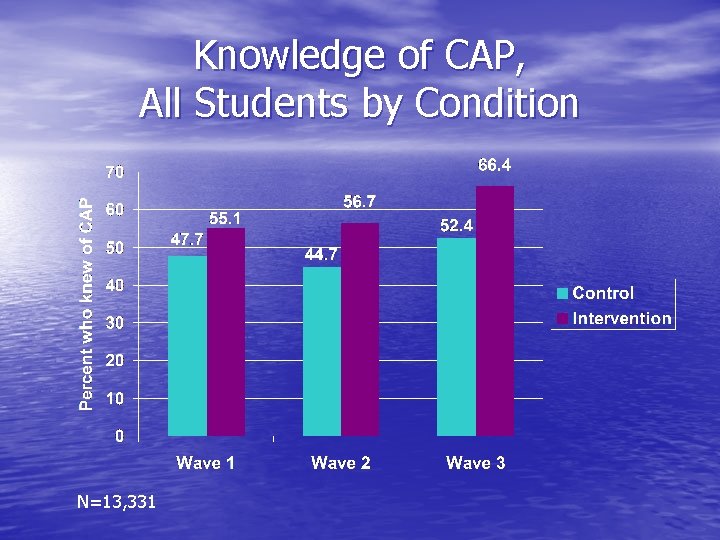
Knowledge of CAP, All Students by Condition N=13, 331
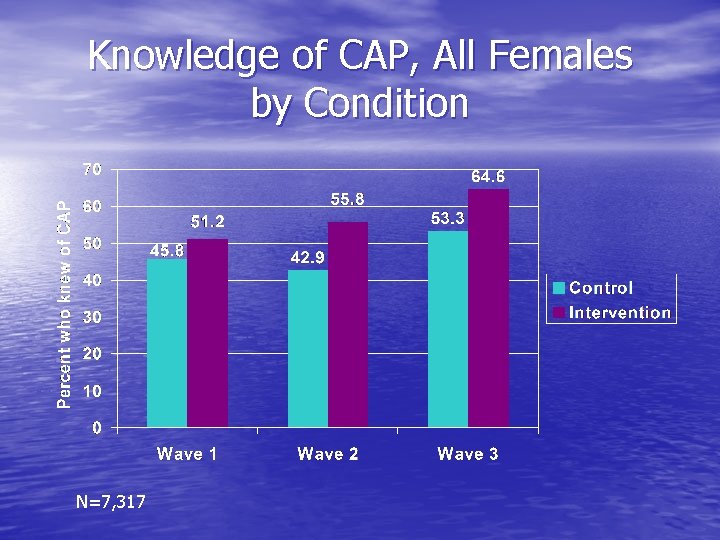
Knowledge of CAP, All Females by Condition N=7, 317
Change in Knowledge of CAP Among Sexually Experienced Participants • Knowledge of CAP increased across waves § 62. 6% - 63. 7% - 70. 3% vs. 51. 4% - 49. 1% 60. 7%, wave X condition interactions n. s. • Change was not significantly different for intervention vs. control participants
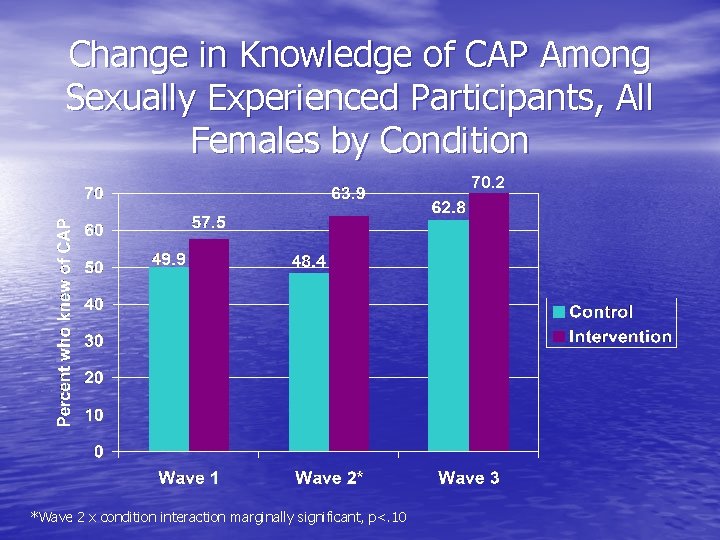
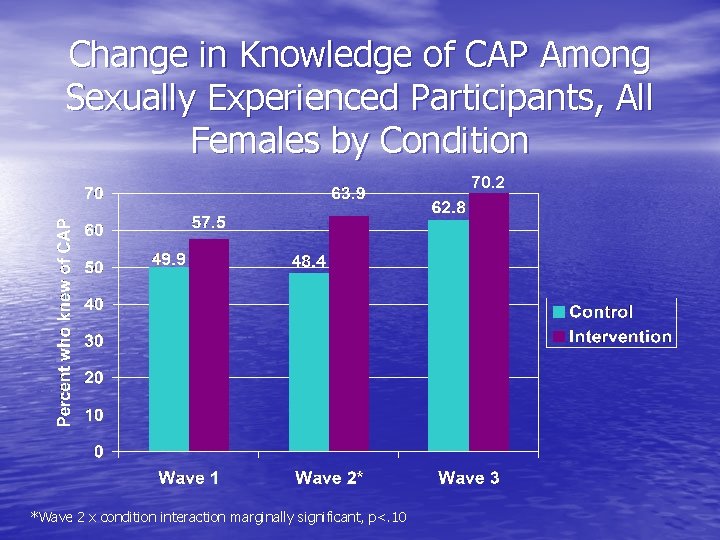
Change in Knowledge of CAP Among Sexually Experienced Participants, All Females by Condition 70. 2 *Wave 2 x condition interaction marginally significant, p<. 10
Used CAP, All Students Who Knew of It* • Use of CAP did not differ between conditions • Use of CAP increased across waves in both conditions § Intervention: 27. 0% - 32. 4% - 34. 0% § Control: 27. 4% - 33. 1% - 32. 8% § Wave X condition interactions n. s. *Among all students regardless of sexual experience
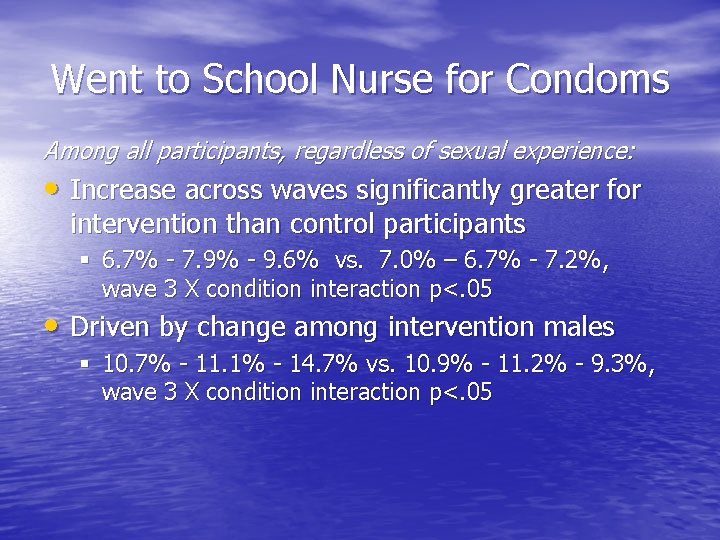
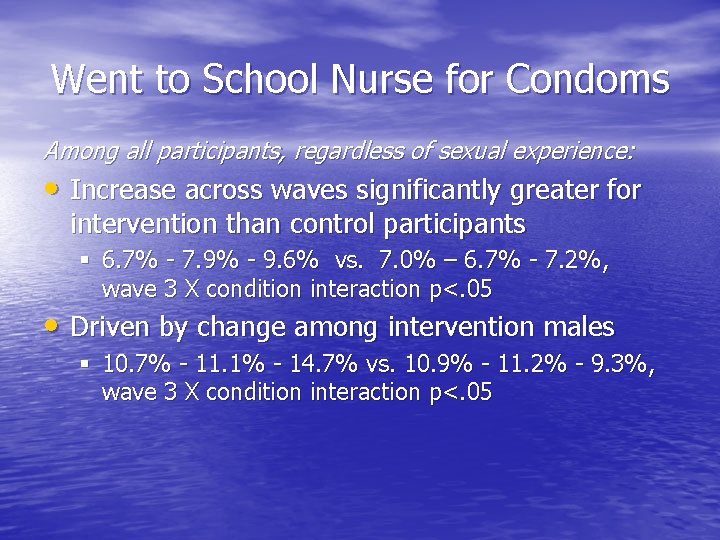
Went to School Nurse for Condoms Among all participants, regardless of sexual experience: • Increase across waves significantly greater for intervention than control participants § 6. 7% - 7. 9% - 9. 6% vs. 7. 0% – 6. 7% - 7. 2%, wave 3 X condition interaction p<. 05 • Driven by change among intervention males § 10. 7% - 11. 1% - 14. 7% vs. 10. 9% - 11. 2% - 9. 3%, wave 3 X condition interaction p<. 05
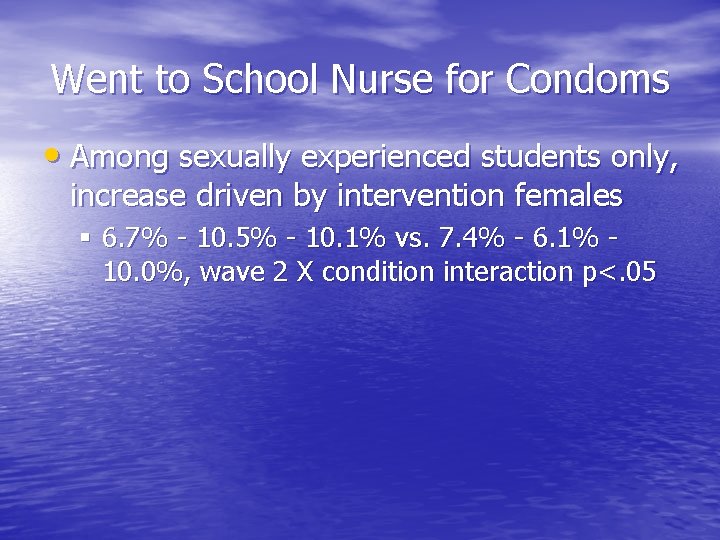
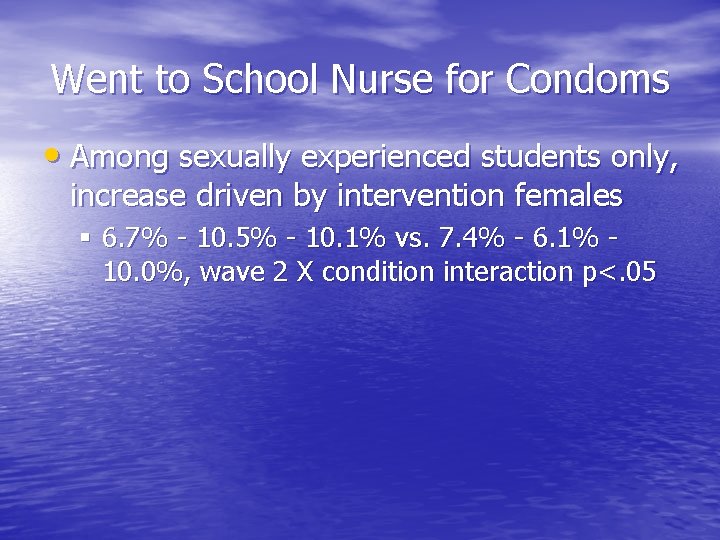
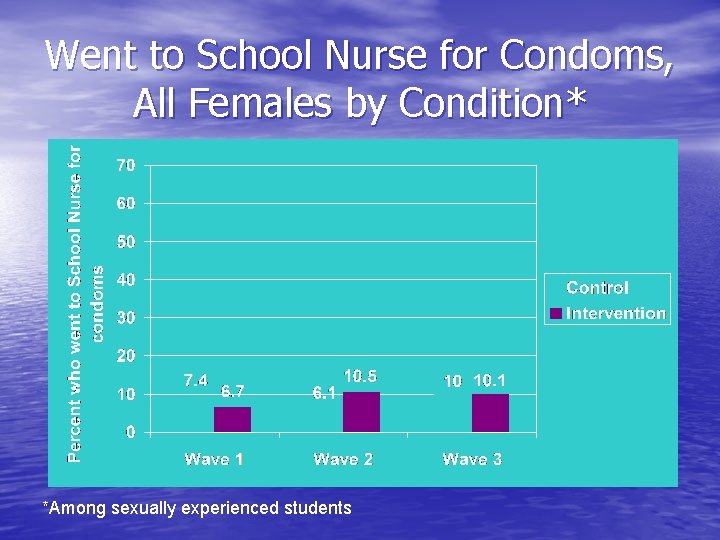
Went to School Nurse for Condoms • Among sexually experienced students only, increase driven by intervention females § 6. 7% - 10. 5% - 10. 1% vs. 7. 4% - 6. 1% 10. 0%, wave 2 X condition interaction p<. 05
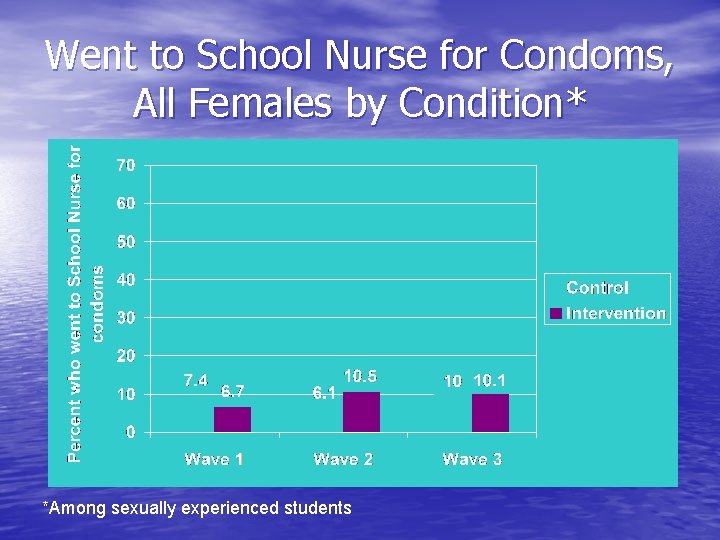
Went to School Nurse for Condoms, All Females by Condition* *Among sexually experienced students
Summary of Findings • Increase in knowledge of CAP greater in intervention schools • Going to School Nurse for condoms significantly greater for intervention than for control participants
Conclusions • Enhancements to implementation of CAP are feasible, practical, low-cost • Enhancements resulted in: § Greater increase in knowledge of program among students in intervention schools § Increase in seeing School Nurse for condoms among students in intervention schools
Implications for Interventions • Implementation of district-mandated CAP can vary: § Enforcement § Person responsible • Minor enhancements (i. e. , moving personnel • through stages of change) can result in substantial improvement in implementation Improved implementation results in greater student knowledge of CAP and seeking condoms from School Nurse
Condom Availability Programs: Next Steps • Intervention: § Enlist student leadership groups in normalizing use of CAP § Increase outreach § Maintain functioning of programs • Evaluation: § Examine how changes in knowledge and use of CAP impact participant condom use § Examine relationship between number of condoms distributed and participant condom use
Thank You! Collaborators: Peter Kerndt, MD, MPH Kathleen Ethier, Ph. D Patricia Dittus, Ph. D Nicole Liddon, Ph. D Abdelmonem Afifi, Ph. D William Cumberland, Ph. D Harlan Rotblatt Ric Loya Robin Jeffries, MPH Sharon Hudson, Ph. D Project Staff: Christine J. De Rosa, Ph. D Emily Q. Chung, MPH, CHES Steve Martinez, BA Kathy Wong, MS Lindsay Du Plessis, MPH …for the Project Connect Study Team Email: echung@hra-paramount. org