Positive and Safe reducing the need for restrictive


- Slides: 15

Positive and Safe: reducing the need for restrictive interventions
Why? Winterbourne View • • 2 Restraint was not always used only as a last resort Concerns about the use of anti-psychotic and antidepressant medications Other restrictive practices common Subsequent investigations show that these findings are widespread Reducing the need for restrictive interventions
Reducing the need for restrictive interventions Mind Count. Report Me In Census 30% of Trusts people with inpatient settings • • 49 Differences NHS in the use. LD ofinphysical restraint experienced physical restraint • • 20, 000 Over-use incidents does occur of restraint 14% of people in MH inpatient settings experienced • Range Not always 3, 000 as–last lessresort than 50 per Trust restraint • • 19, 000 AWhat number people of deaths retrained have been associated about other settings with the use of physical restraint • 1, 000 restraint related injuries (60% • 3 Reducing the need for restrictive interventions response) Doesn’t include Independent sector
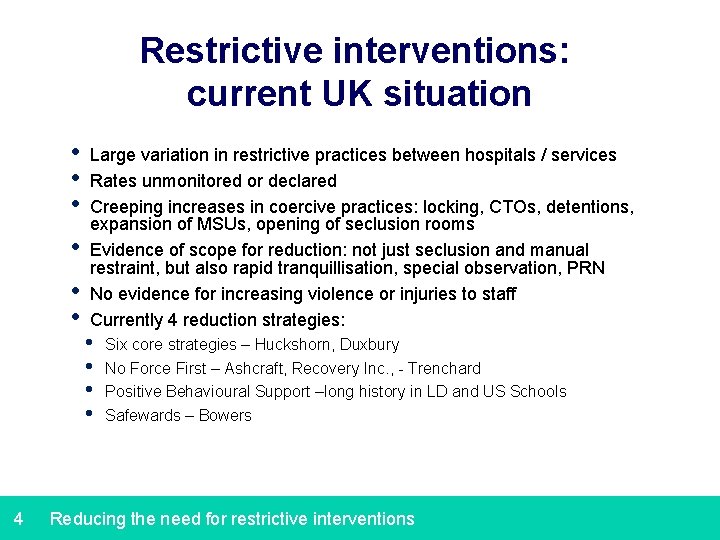
Restrictive interventions: current UK situation • • • 4 Large variation in restrictive practices between hospitals / services Rates unmonitored or declared Creeping increases in coercive practices: locking, CTOs, detentions, expansion of MSUs, opening of seclusion rooms Evidence of scope for reduction: not just seclusion and manual restraint, but also rapid tranquillisation, special observation, PRN No evidence for increasing violence or injuries to staff Currently 4 reduction strategies: • • Six core strategies – Huckshorn, Duxbury No Force First – Ashcraft, Recovery Inc. , - Trenchard Positive Behavioural Support –long history in LD and US Schools Safewards – Bowers Reducing the need for restrictive interventions
Reducing the need for restrictive interventions 10 shared commitments 1. Above all - health & care services should be positive, caring and safe 2. Promoting a therapeutic environment, enabling positive, compassionate caring that promoting physical and emotional wellness 3. Treating all people with dignity; caring and talking to them in a safe and therapeutic way 4. Restrictive practices have no place in a modern, compassionate health and care service 5. Restraining, secluding or excessively medicating people should only ever be used as a last resort 5 Enter the presentation's title using the menu option View > Header and Footer
Reducing the need for restrictive interventions 10 shared commitments 6. Promoting positive alternatives, such as positive behaviour support and deescalation techniques, are the most effective means of reducing restrictive interventions 7. Being open, honest and transparent about the use of restraint and restrictions. They must be recorded, reported openly and reviewed. Patients and families should be communicated with 8. Genuine co-production, with experts by experience, of’ policies and training. These should include alternative, positive measures and means of de-escalation 9. Destructive and dangerous cultures must change. Leaders must stand up publicly for stopping outdated and damaging restraint and restrictions in health and care services 10. Assault is assault. The intentional use of pain, restraints or restrictions to punish, hurt or humiliate is never acceptable and will not be tolerated 6 Enter the presentation's title using the menu option View > Header and Footer
Positive and Proactive Care Key Principles: 1. Compliance with the relevant rights in the European Convention on Human Rights 2. Understanding people’s behaviour allows their unique needs, aspirations, experiences and strengths to be recognised and their quality of life to be enhanced 3. Involvement and participation of people with care and support needs, their families, carers and advocates is essential 4. People must be treated with compassion, dignity and kindness 5. Services must support people to balance safety from harm and freedom of choice 6. Positive relationships between the people who deliver services and the people they support must be protected and preserved. 7 Enter the presentation's title using the menu option View > Header and Footer
Positive and Proactive Care Aims 1. Cultural change 2. Therapeutic environments 3. Focus on quality of life 4. Governance models 5. Reducing reliance on restrictive interventions 6. Learning, sharing and promoting practice innovation 7. To ensure that restrictive interventions are used in a transparent, legal and ethical manner 8
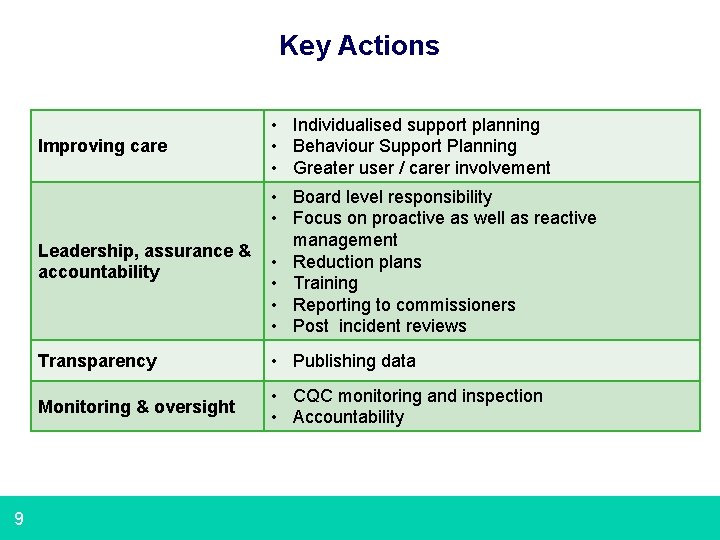
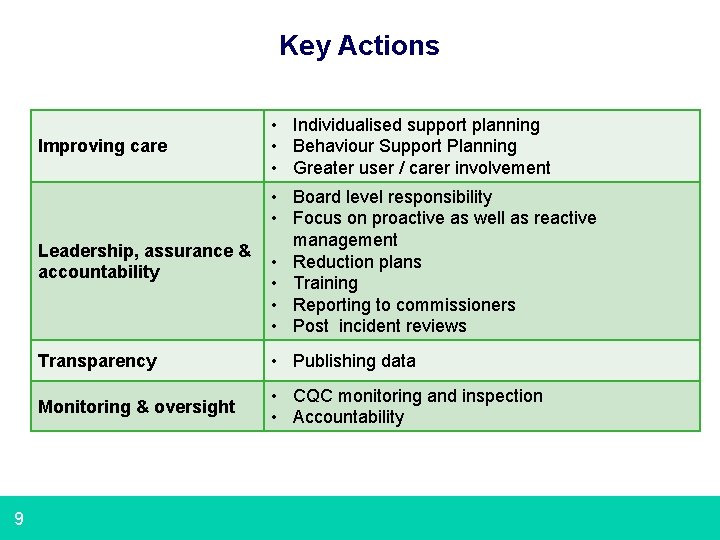
Key Actions 9 Improving care • Individualised support planning • Behaviour Support Planning • Greater user / carer involvement Leadership, assurance & accountability • Board level responsibility • Focus on proactive as well as reactive management • Reduction plans • Training • Reporting to commissioners • Post incident reviews Transparency • Publishing data Monitoring & oversight • CQC monitoring and inspection • Accountability
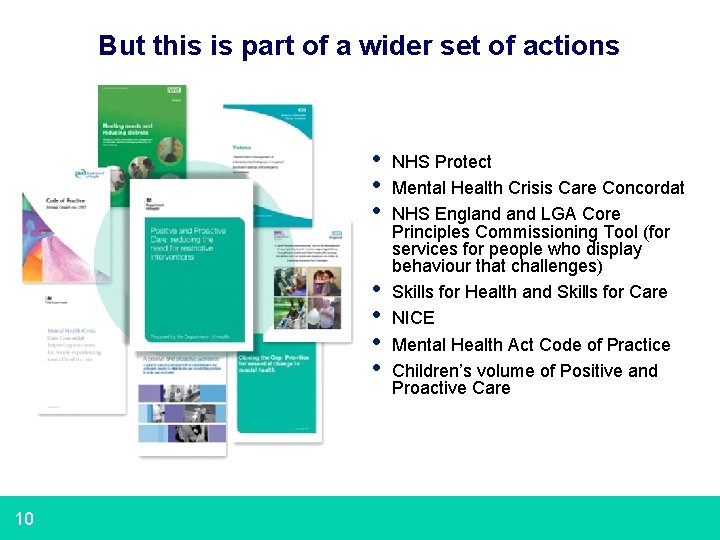
But this is part of a wider set of actions • • 10 NHS Protect Mental Health Crisis Care Concordat NHS England LGA Core Principles Commissioning Tool (for services for people who display behaviour that challenges) Skills for Health and Skills for Care NICE Mental Health Act Code of Practice Children’s volume of Positive and Proactive Care
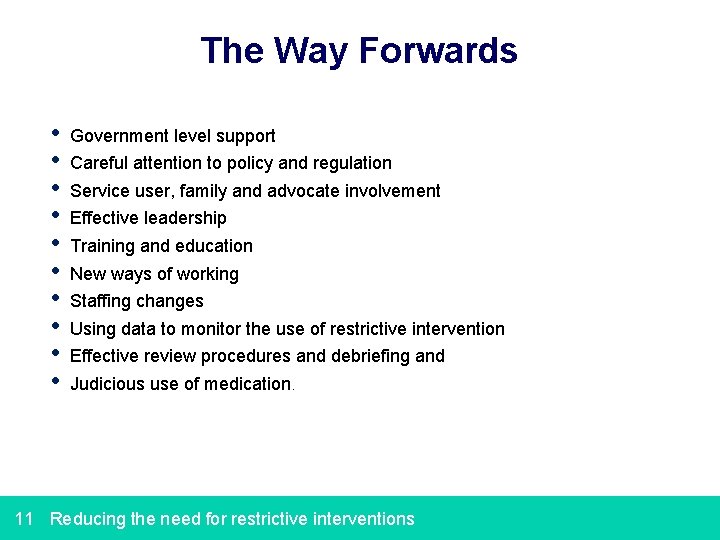
The Way Forwards • • • Government level support Careful attention to policy and regulation Service user, family and advocate involvement Effective leadership Training and education New ways of working Staffing changes Using data to monitor the use of restrictive intervention Effective review procedures and debriefing and Judicious use of medication. 11 Reducing the need for restrictive interventions
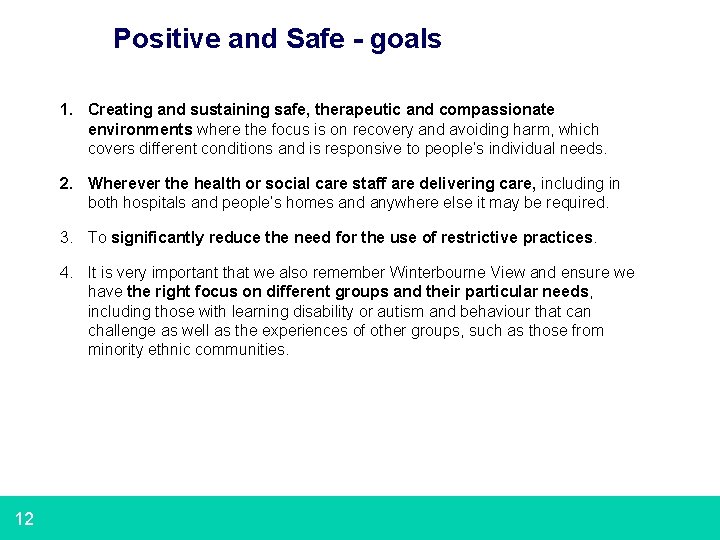
Positive and Safe - goals 1. Creating and sustaining safe, therapeutic and compassionate environments where the focus is on recovery and avoiding harm, which covers different conditions and is responsive to people’s individual needs. 2. Wherever the health or social care staff are delivering care, including in both hospitals and people’s homes and anywhere else it may be required. 3. To significantly reduce the need for the use of restrictive practices. 4. It is very important that we also remember Winterbourne View and ensure we have the right focus on different groups and their particular needs, including those with learning disability or autism and behaviour that can challenge as well as the experiences of other groups, such as those from minority ethnic communities. 12
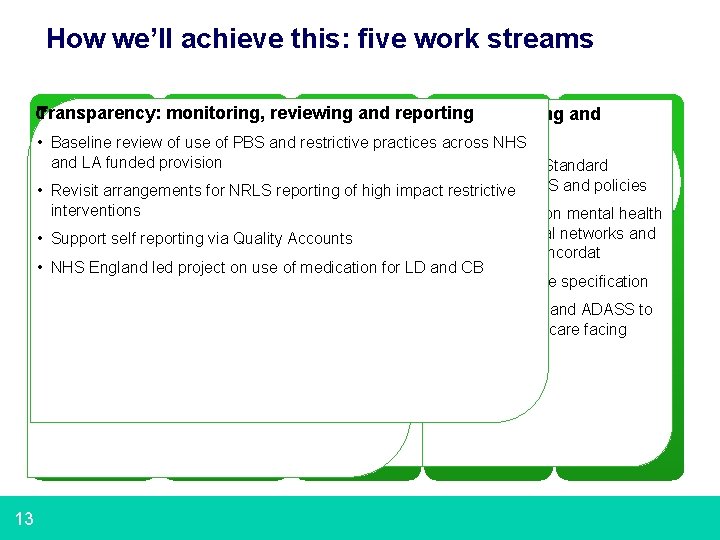
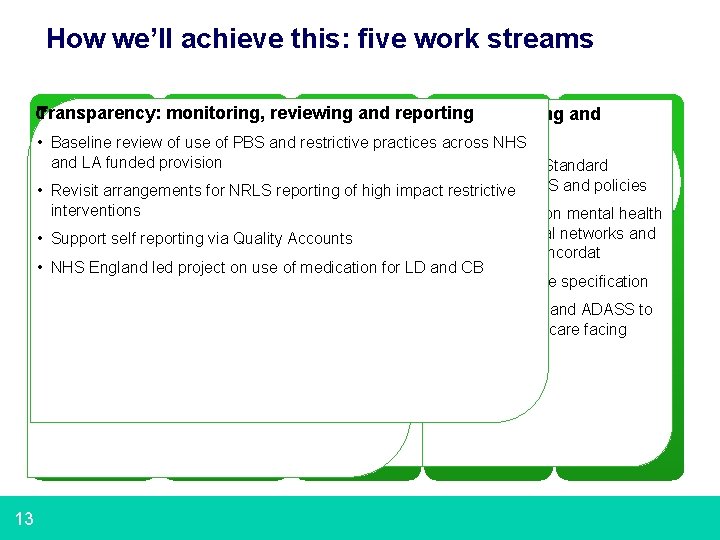
How we’ll achieve this: five work streams Transparency: monitoring, and maintaining reporting Communications, Standards, culture & reviewing guidance leadership Workforce, training Commissioning andcompliance development and. . contracts Baseline review of • use offundamental PBS and restrictive practices across NHS • • Champions initiative CQC • Positive standards and proactive workforce and LA funded provision • Revised NHS Standard • Web based information • Positive and practice and Proactive • exchange HEECare mandate and Skills for Care programme Contract re PBS and policies • Revisit arrangements for NRLS reporting of high impact restrictive • Sharing stories along • Updating the journey the MHA • Explore Code ofissues Practice re training accreditation interventions • Develop work on mental health • Research and academic • Exploring partners the need • LD forprofessional other legislative senate / national andclinical / orpolicy MH Joint guidance strategic networks and • Support self reporting via Quality Accounts Commissioning Panel key principles for Crisis– Care Concordat • User and carer group • NICE involvement guidancee. g. due. MIND, 2015 • NHS England led project on use of medication training for LD and CB mencap etc. . • NHS LD service specification • Work with NHS Protect • Develop expert by experience guide Transparency: to training Standards, • Explore behaviour change project Workforce, Communications, • Work with LGAand ADASS to guidance and Commissioning monitoring, • training Work with HSE and culture and • Support access todevelop PBS training social carereporting facing and maintaining contracts • BME focused groupdevelopment re afro-carribean and users and leadership • Children and Young People Guidance compliance reviewing non discriminatory practice • Explore e. Learningprojects opportunities 13

How we’ll achieve this: reporting and partners Mental Health Systems Board Positive and Safe Steering Group Agreed projects, initiatives and actions 14 Champions Group Partners: • Patients, service users, carers, families and support and advocacy organisations • NHS England • LGA and ADASS • CQC • HEE, Skills for Health, Skills for Care • NICE, SCIE • NHS Protect • HSE • CCGs and LAs • providers, esp provider boards and senior management teams • Royal Colleges, directors of nursing and other professional leaders, trade unions and networks • Learning Disability Professional Senate • Academics and researchers • BILD • Df. E, Mo. J, Home Office • Etc…
Issues for today? • How can we work together to identify and agree the actions required from now to deliver the outcomes and establish and maintain momentum for this work, including leadership for particular activities or themes. • How can we co-ordinate various activities. • How can we identify and secure relevant resources within our organisations and recognise when we might be a resource to others • How we best communicate the cultural changes that are the programme’s goal 15 Enter the presentation's title using the menu option View > Header and Footer