Position Statement for People with Types 1 and





- Slides: 39
Position Statement for People with Types 1 and 2 Diabetes Who Fast during Ramadan Harpreet Singh Bajaj MD, MPH, FACE; Tyceer Abouhassan BEd, MD, MBA, FRCPC; Muhammad Rauf Ahsan, MD, FRCSC; Amel Arnaout, MD, FRCPC; Mohamed Hassanein FRCP, CCST, MPhil, MBCHB; Robyn L. Houlden MD, FRCPC; Tayyab Khan MD, MASc, FRCPC; Hasnain Khandwala MBBS, FRCPC, FACE; Subodh Verma MD, Ph. D, FRCSC
Objectives • Discuss the need for a Canadian position statement on diabetes and Ramadan • Educate on key recommendations for risk stratification and counseling prior to Ramadan fasting for Muslims living with diabetes • Highlight pharmacotherapy and glucose monitoring approaches for safe diabetes management during Ramadan fasting
Key Messages • This statement is intended to guide Canadian healthcare providers on management of people with type 1 or type 2 diabetes who intend to fast during Ramadan • Adults with type 1 and type 2 diabetes who intend to fast should receive an individualized assessment pre-Ramadan, with risk categorization and formulation of an individualized diabetes management plan
Canadian Muslims • 1, 053, 945 Muslims - 3. 2% of Canadian population • Estimated 95, 000 Muslims live with diabetes in Canada • Muslim population estimated to increase to 2. 7 million or 6. 6% of the Canadian population by 2030 • Majority of the Muslims across the world fast during Ramadan Statistics Canada. 2011 National Household Survey – Data Tables Public Health Agency of Canada. (2011). Diabetes in Canada: Facts and figures from a public health perspective. Ottawa, Ont. 2011 Ghani F. Most Muslims say they fast during Ramadan. http: //www. pewresearch. org/fact-tank/2013/07/09/global-median-of-93 -of-muslims-say-they-fast-duringramadan/; 2013
Ramadan – basics • One of the pillars of Islam • Fasting from dawn to dusk – abstaining from water and food • Exceptions for those unable to fast (traveling, sick, or at risk of serious harm to health) – many choose to fast despite their medical condition • Changes in sleeping and eating habits: pre-dawn and sunset meals • Each year, Ramadan occurs ~10 days earlier than the previous year
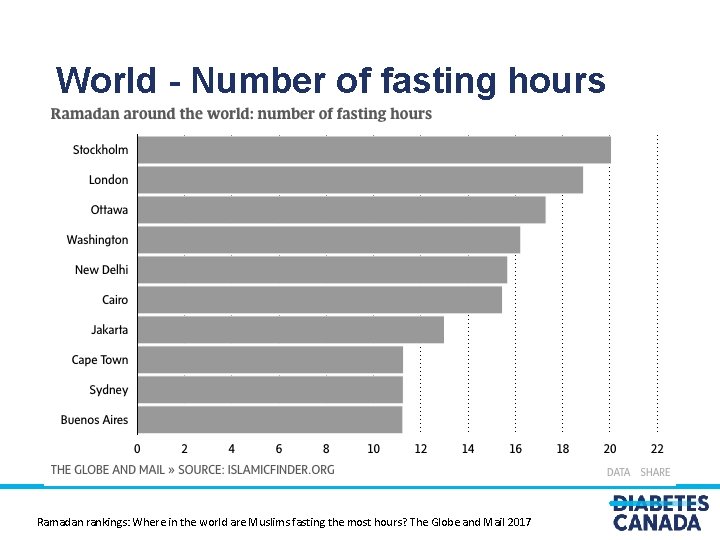
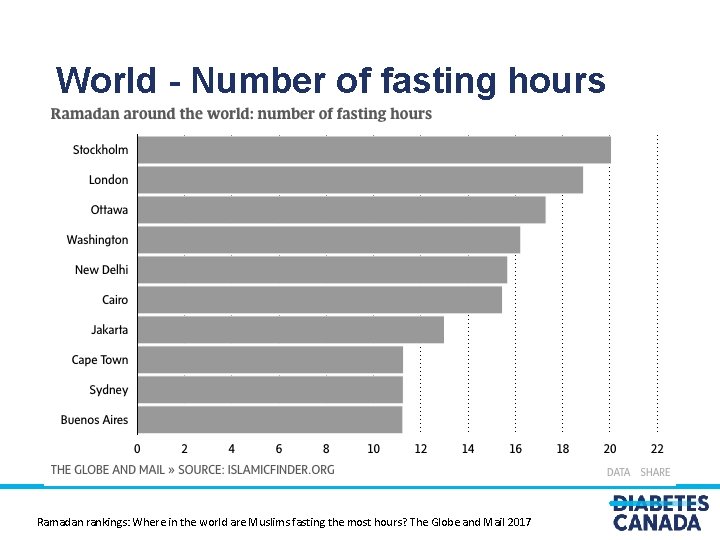
World - Number of fasting hours Ramadan rankings: Where in the world are Muslims fasting the most hours? The Globe and Mail 2017
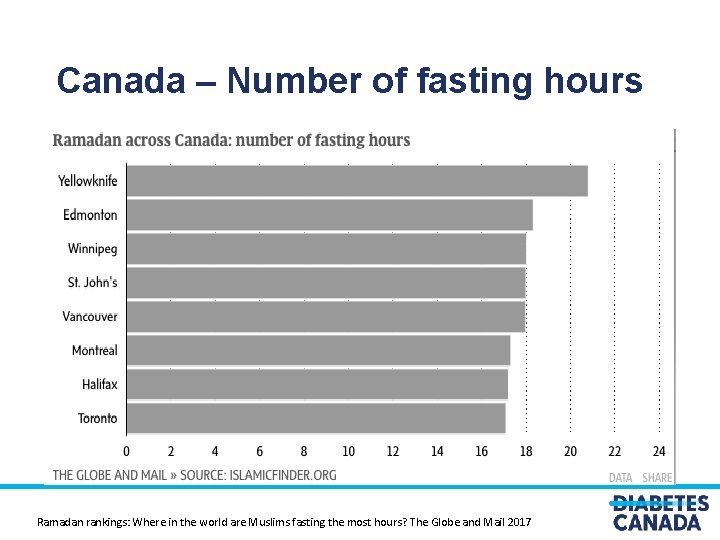
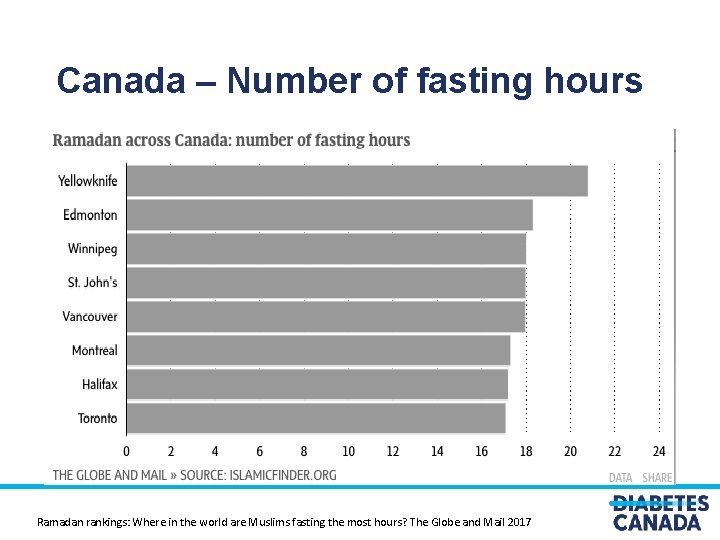
Canada – Number of fasting hours Ramadan rankings: Where in the world are Muslims fasting the most hours? The Globe and Mail 2017

Hassanein M et al. Diabetes and Ramadan: Practical guidelines. Diabetes Res Clin Pract (2017), http: //dx. doi. org/10. 1016/j. diabres. 2017. 03. 003 IDF-DAR Practical Guidelines
The Need for a Canadian Diabetes & Ramadan Position Statement Differences from Middle Eastern or South Asian, Muslim dominant countries: • hours of fasting • work hours and peer support • pharmacotherapy (insulin and non-insulin) in type 2 diabetes • insulin pump use in type 1 diabetes • Glucose, continuous/flash monitoring technology usage Muslims in Canada, Canada 2011 National Household Survey The Profile of Muslims In Canada Archived 2012 -02 -03 at the Wayback Machine. , Abdul Malik Mujahid. Grenier, Éric (27 April 2016). "Muslim Canadians increasingly proud of and attached to Canada, survey suggests". CBC News. Retrieved 19 April 2017
Diabetes Canada Position Statement • Published in the Canadian Journal of Diabetes • Dietary counseling not covered. Follow International Diabetes Federation - Diabetes and Ramadan International Alliance and Diabetes Canada Clinical Practice Guidelines • Medications or glucose monitoring devices with Health Canada Notice of Compliance granted by February 15, 2018 included • Islamic Society of North America (ISNA) Canada endorsed the position statement and provided letter of support https: //doi. org/10. 1016/j. jcjd. 2018. 04. 007
Position Statement: Sections • Pre-Ramadan diabetes management planning, including risk stratification • Non-insulin pharmacotherapy for type 2 diabetes during Ramadan • Insulin management for type 2 diabetes during Ramadan • Type 1 diabetes management during Ramadan • Monitoring glycemic control while fasting in Ramadan

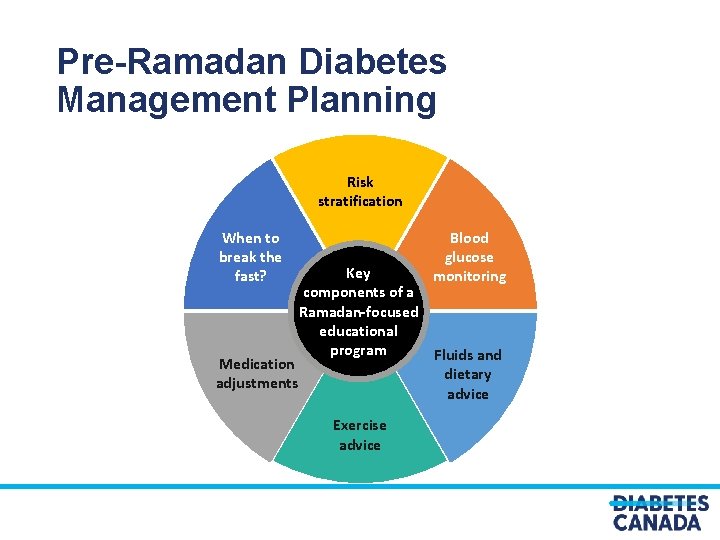
Pre-Ramadan Diabetes Management Planning Healthcare provider assessment is recommended 1 -3 months prior to Ramadan for those intending to fast: • Risk stratification • Review of positive and adverse experiences from previous fasting • Formulate individualized treatment plan
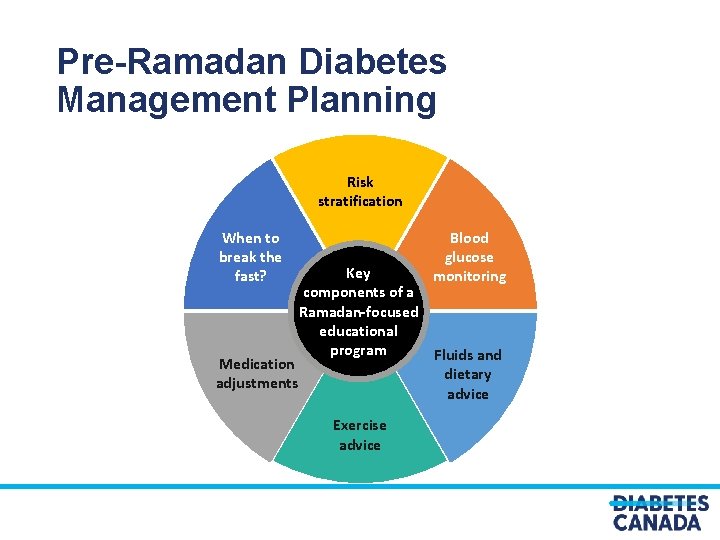
Pre-Ramadan Diabetes Management Planning Risk stratification When to break the fast? Blood glucose monitoring Key components of a Ramadan-focused educational program Fluids and Medication dietary adjustments advice Exercise advice
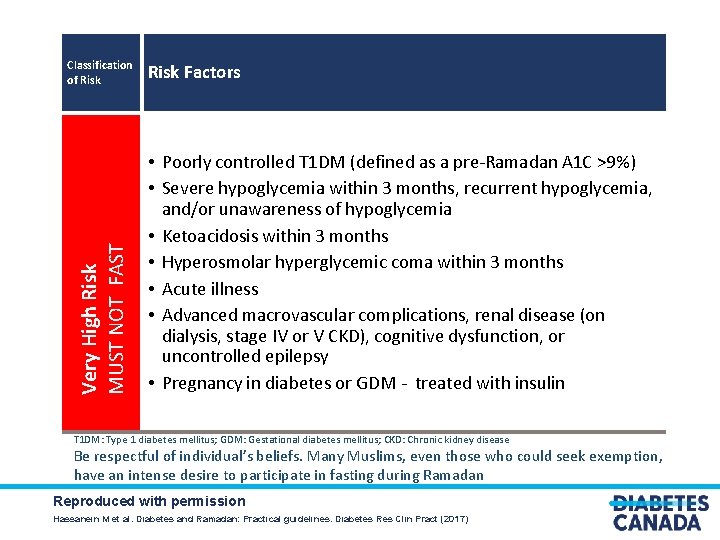
Risk stratification for fasting during Ramadan for people living with diabetes
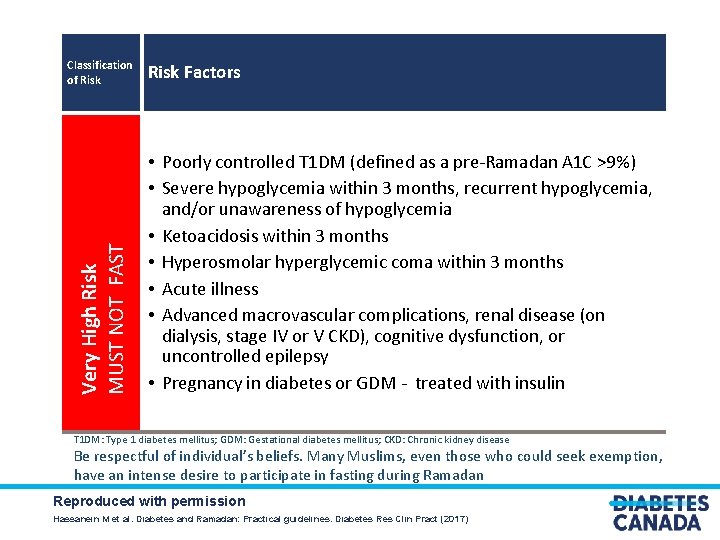
Very High Risk MUST NOT FAST Classification of Risk Factors • Poorly controlled T 1 DM (defined as a pre-Ramadan A 1 C >9%) • Severe hypoglycemia within 3 months, recurrent hypoglycemia, and/or unawareness of hypoglycemia • Ketoacidosis within 3 months • Hyperosmolar hyperglycemic coma within 3 months • Acute illness • Advanced macrovascular complications, renal disease (on dialysis, stage IV or V CKD), cognitive dysfunction, or uncontrolled epilepsy • Pregnancy in diabetes or GDM - treated with insulin T 1 DM: Type 1 diabetes mellitus; GDM: Gestational diabetes mellitus; CKD: Chronic kidney disease Be respectful of individual’s beliefs. Many Muslims, even those who could seek exemption, have an intense desire to participate in fasting during Ramadan Reproduced with permission Hassanein M et al. Diabetes and Ramadan: Practical guidelines. Diabetes Res Clin Pract (2017)
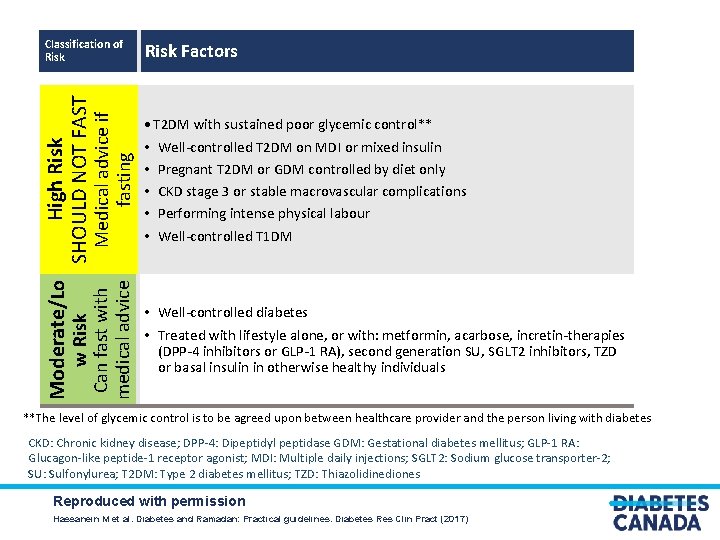
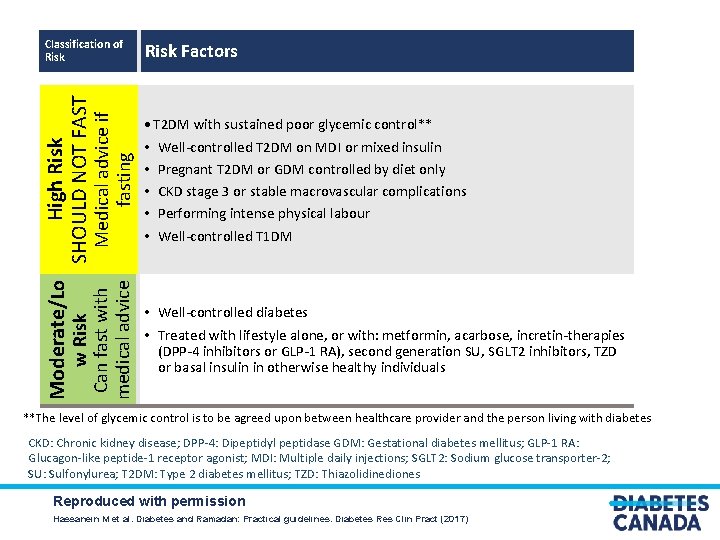
Moderate/Lo w Risk Can fast with medical advice Medical advice if fasting High Risk SHOULD NOT FAST Classification of Risk Factors • T 2 DM with sustained poor glycemic control** • • • Well-controlled T 2 DM on MDI or mixed insulin Pregnant T 2 DM or GDM controlled by diet only CKD stage 3 or stable macrovascular complications Performing intense physical labour Well-controlled T 1 DM • Well-controlled diabetes • Treated with lifestyle alone, or with: metformin, acarbose, incretin-therapies (DPP-4 inhibitors or GLP-1 RA), second generation SU, SGLT 2 inhibitors, TZD or basal insulin in otherwise healthy individuals **The level of glycemic control is to be agreed upon between healthcare provider and the person living with diabetes CKD: Chronic kidney disease; DPP-4: Dipeptidyl peptidase GDM: Gestational diabetes mellitus; GLP-1 RA: Glucagon-like peptide-1 receptor agonist; MDI: Multiple daily injections; SGLT 2: Sodium glucose transporter-2; SU: Sulfonylurea; T 2 DM: Type 2 diabetes mellitus; TZD: Thiazolidinediones Reproduced with permission Hassanein M et al. Diabetes and Ramadan: Practical guidelines. Diabetes Res Clin Pract (2017)
Non-insulin pharmacotherapy for type 2 diabetes
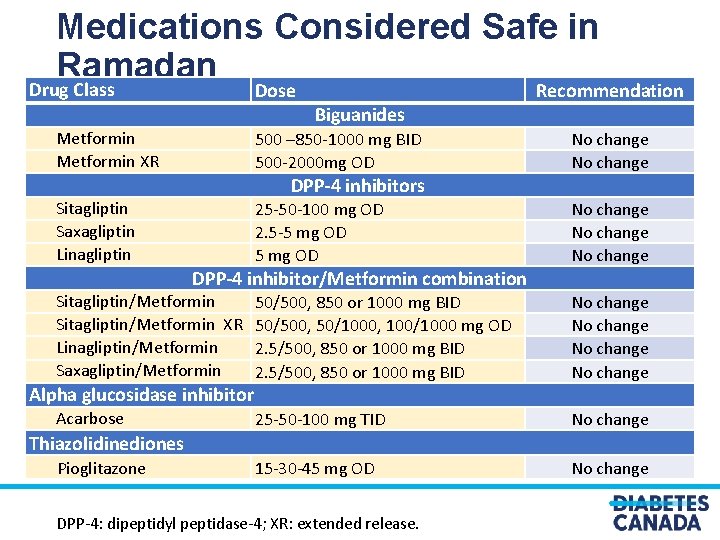
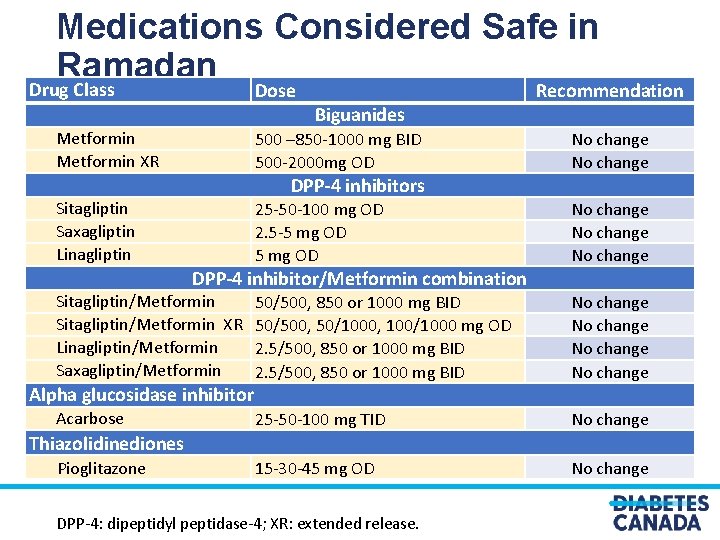
Medications Considered Safe in Ramadan Drug Class Dose Metformin XR Biguanides 500 – 850 -1000 mg BID 500 -2000 mg OD No change 25 -50 -100 mg OD 2. 5 -5 mg OD No change 50/500, 850 or 1000 mg BID 50/500, 50/1000, 100/1000 mg OD 2. 5/500, 850 or 1000 mg BID No change 25 -50 -100 mg TID No change 15 -30 -45 mg OD No change DPP-4 inhibitors Sitagliptin Saxagliptin Linagliptin DPP-4 inhibitor/Metformin combination Sitagliptin/Metformin XR Linagliptin/Metformin Saxagliptin/Metformin Alpha glucosidase inhibitor Acarbose Recommendation Thiazolidinediones Pioglitazone DPP-4: dipeptidyl peptidase-4; XR: extended release.
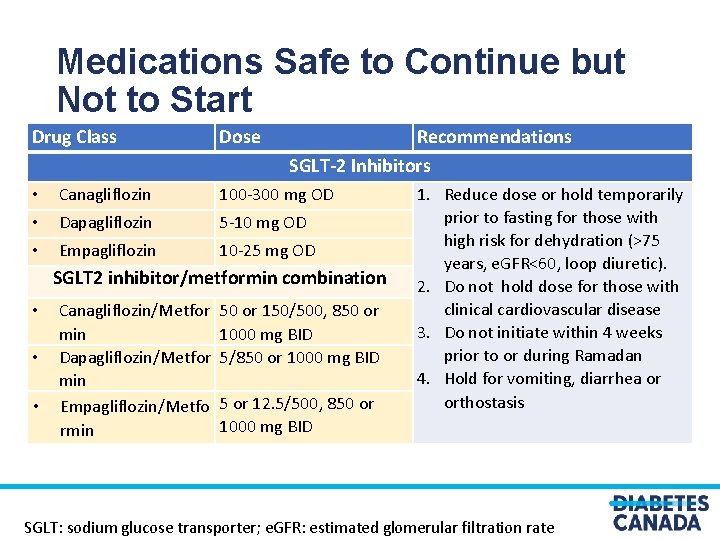
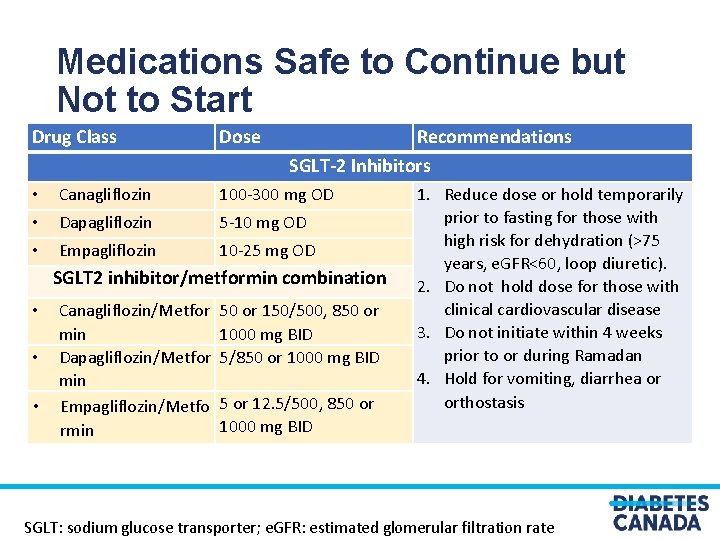
Medications Safe to Continue but Not to Start Drug Class Dose Recommendations SGLT-2 Inhibitors • Canagliflozin 100 -300 mg OD • Dapagliflozin 5 -10 mg OD • Empagliflozin 10 -25 mg OD SGLT 2 inhibitor/metformin combination • • • Canagliflozin/Metfor min Dapagliflozin/Metfor min Empagliflozin/Metfo rmin 50 or 150/500, 850 or 1000 mg BID 5/850 or 1000 mg BID 5 or 12. 5/500, 850 or 1000 mg BID 1. Reduce dose or hold temporarily prior to fasting for those with high risk for dehydration (>75 years, e. GFR<60, loop diuretic). 2. Do not hold dose for those with clinical cardiovascular disease 3. Do not initiate within 4 weeks prior to or during Ramadan 4. Hold for vomiting, diarrhea or orthostasis SGLT: sodium glucose transporter; e. GFR: estimated glomerular filtration rate
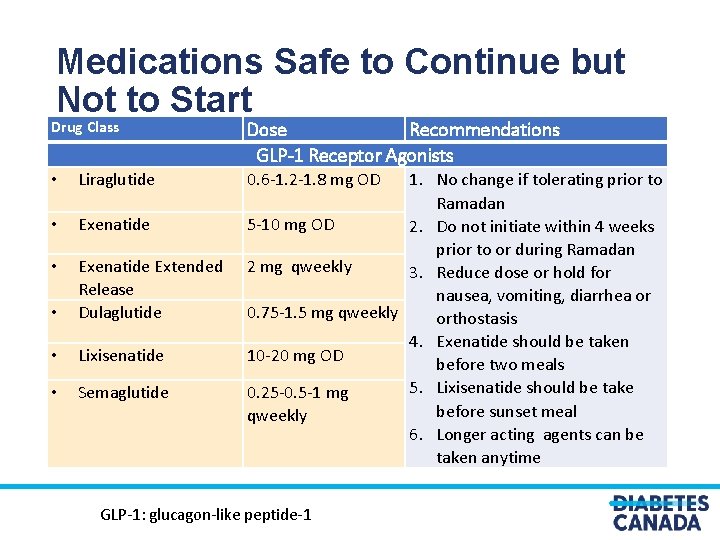
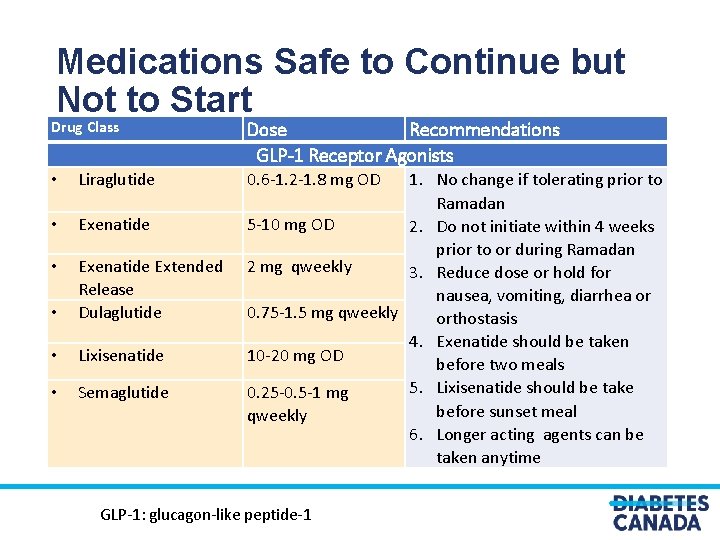
Medications Safe to Continue but Not to Start Drug Class • Liraglutide • Exenatide • • Exenatide Extended Release Dulaglutide • Lixisenatide • Semaglutide Dose Recommendations GLP-1 Receptor Agonists 1. No change if tolerating prior to Ramadan 5 -10 mg OD 2. Do not initiate within 4 weeks prior to or during Ramadan 2 mg qweekly 3. Reduce dose or hold for nausea, vomiting, diarrhea or 0. 75 -1. 5 mg qweekly orthostasis 4. Exenatide should be taken 10 -20 mg OD before two meals 5. Lixisenatide should be take 0. 25 -0. 5 -1 mg before sunset meal qweekly 6. Longer acting agents can be taken anytime 0. 6 -1. 2 -1. 8 mg OD GLP-1: glucagon-like peptide-1

Medications that may need to be adjusted/changed due to risk of hypoglycemia Secretagogue Dose Glimepiride 1 -2 -3 -4 mg OD Glyburide Gliclazide MR Repaglinide Recommendations 1. Consider switching to an alternate drug class with lower risk of hypoglycemia for the duration of 2. 5 -5 -10 mg BID the fasting month 30 -60 -120 mg OD 2. If continuing, consider switching to safer agent within class with lower risk of hypoglycemia and reduce dose by 25 -50% 0. 5 -1 -2 -4 mg AC 3. Repaglinide may be safest in class. meals Adjust according to alteration of meal times and sizes during Ramadan
Counseling for Sick Day Management during Ramadan Vomiting, diarrhea or orthostasis during Ramadan • Break the fast immediately, • Hold certain antihyperglycemic medications (metformin, secretagogues, GLP-1 receptor agonists, SGLT 2 inhibitors), • Continue blood glucose monitoring and • Seek immediate medical attention
Insulin adjustment/change recommendations for type 2 diabetes
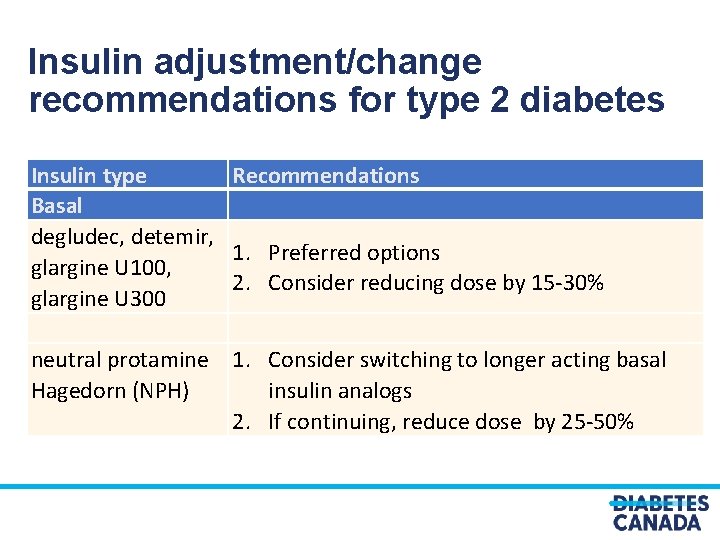
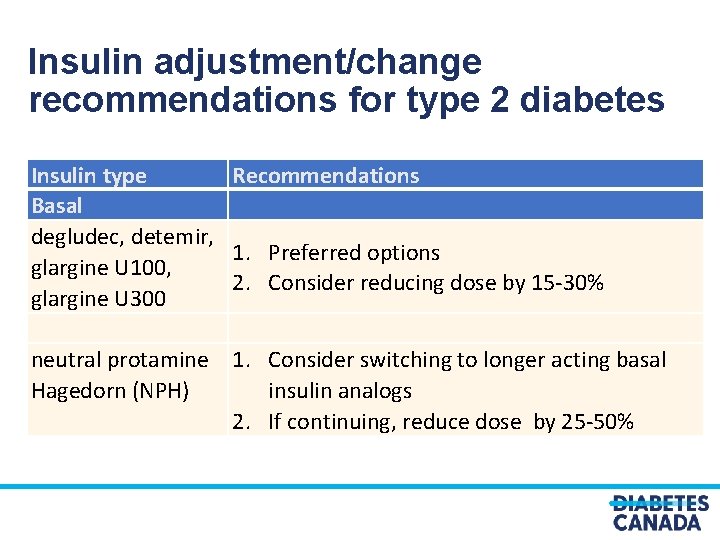
Insulin adjustment/change recommendations for type 2 diabetes Insulin type Basal degludec, detemir, glargine U 100, glargine U 300 Recommendations 1. Preferred options 2. Consider reducing dose by 15 -30% neutral protamine 1. Consider switching to longer acting basal Hagedorn (NPH) insulin analogs 2. If continuing, reduce dose by 25 -50%
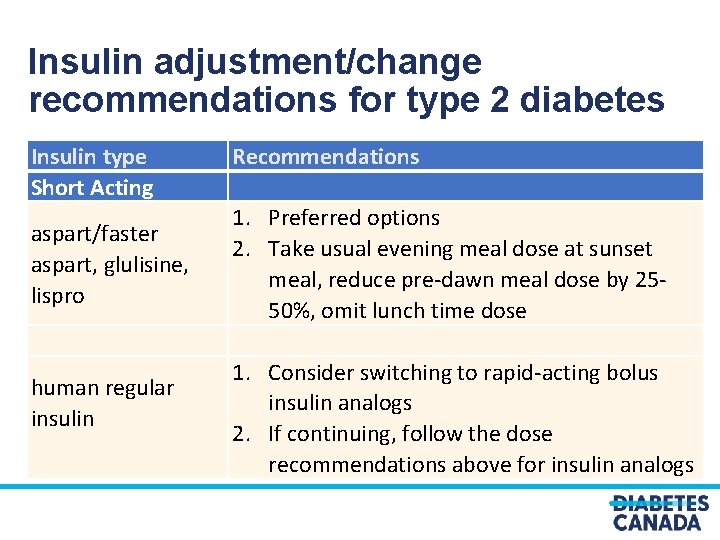
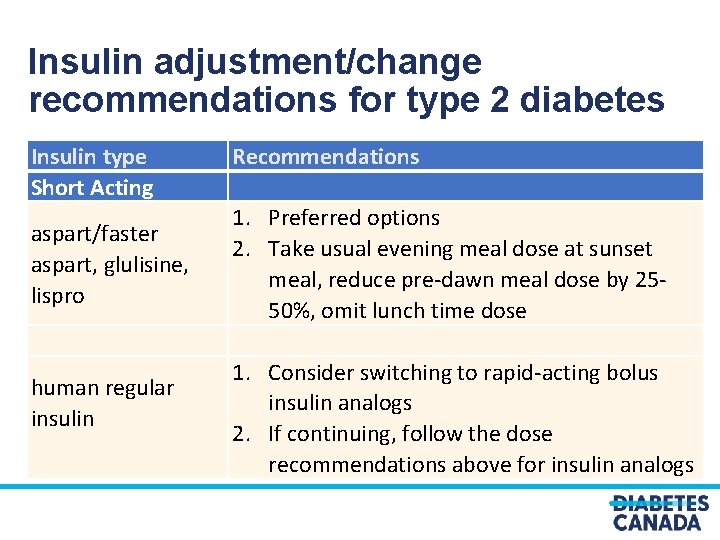
Insulin adjustment/change recommendations for type 2 diabetes Insulin type Short Acting aspart/faster aspart, glulisine, lispro human regular insulin Recommendations 1. Preferred options 2. Take usual evening meal dose at sunset meal, reduce pre-dawn meal dose by 2550%, omit lunch time dose 1. Consider switching to rapid-acting bolus insulin analogs 2. If continuing, follow the dose recommendations above for insulin analogs
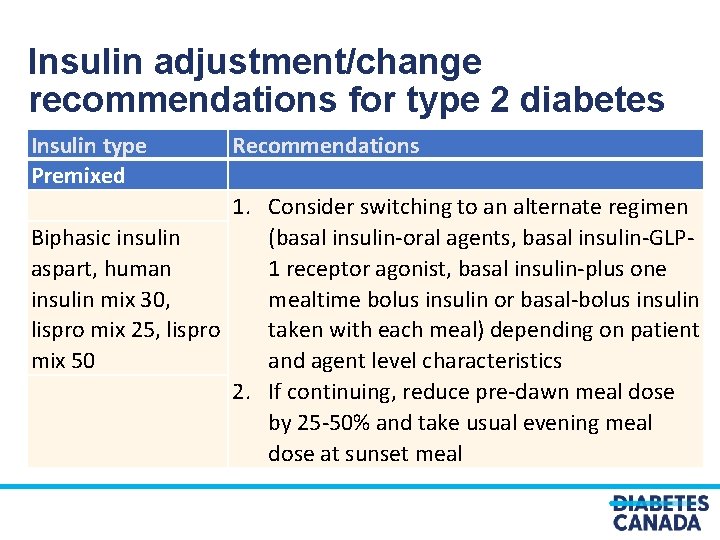
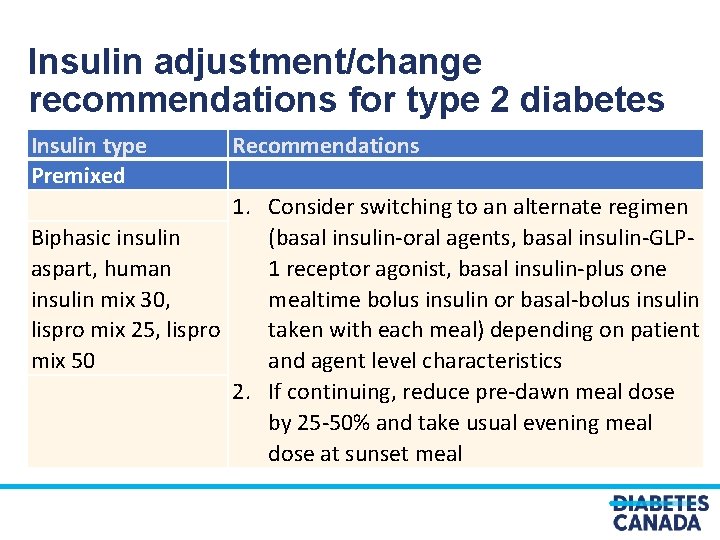
Insulin adjustment/change recommendations for type 2 diabetes Insulin type Premixed Recommendations 1. Consider switching to an alternate regimen Biphasic insulin (basal insulin-oral agents, basal insulin-GLPaspart, human 1 receptor agonist, basal insulin-plus one insulin mix 30, mealtime bolus insulin or basal-bolus insulin lispro mix 25, lispro taken with each meal) depending on patient mix 50 and agent level characteristics 2. If continuing, reduce pre-dawn meal dose by 25 -50% and take usual evening meal dose at sunset meal
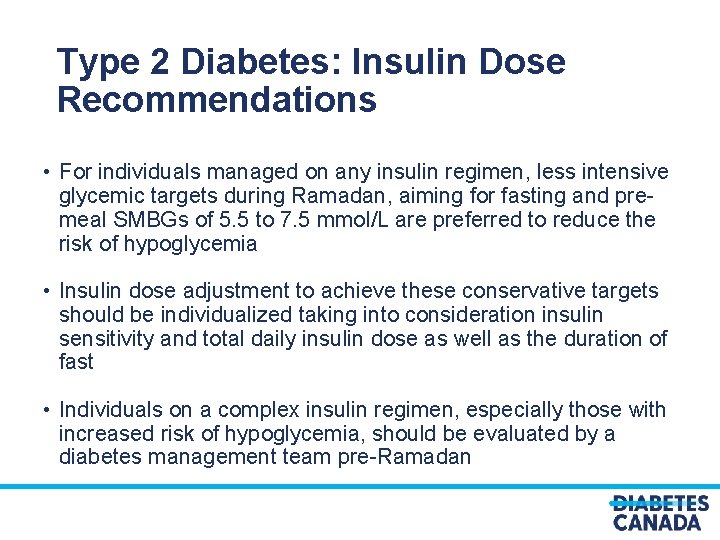
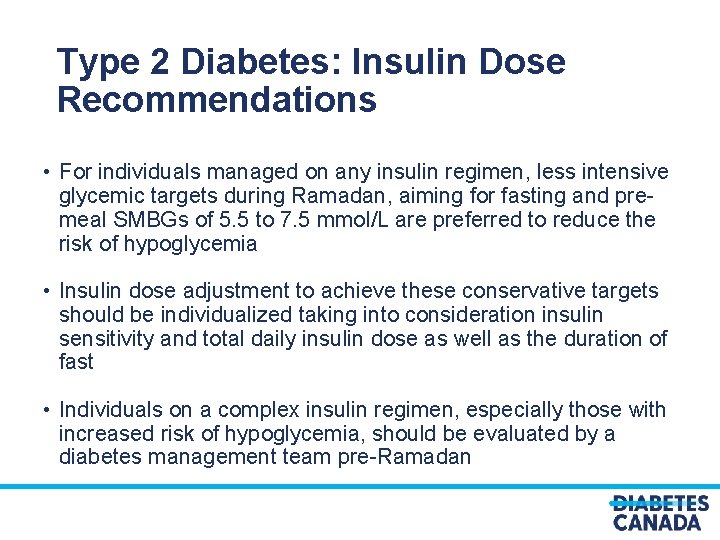
Type 2 Diabetes: Insulin Dose Recommendations • For individuals managed on any insulin regimen, less intensive glycemic targets during Ramadan, aiming for fasting and premeal SMBGs of 5. 5 to 7. 5 mmol/L are preferred to reduce the risk of hypoglycemia • Insulin dose adjustment to achieve these conservative targets should be individualized taking into consideration insulin sensitivity and total daily insulin dose as well as the duration of fast • Individuals on a complex insulin regimen, especially those with increased risk of hypoglycemia, should be evaluated by a diabetes management team pre-Ramadan
Type 1 diabetes
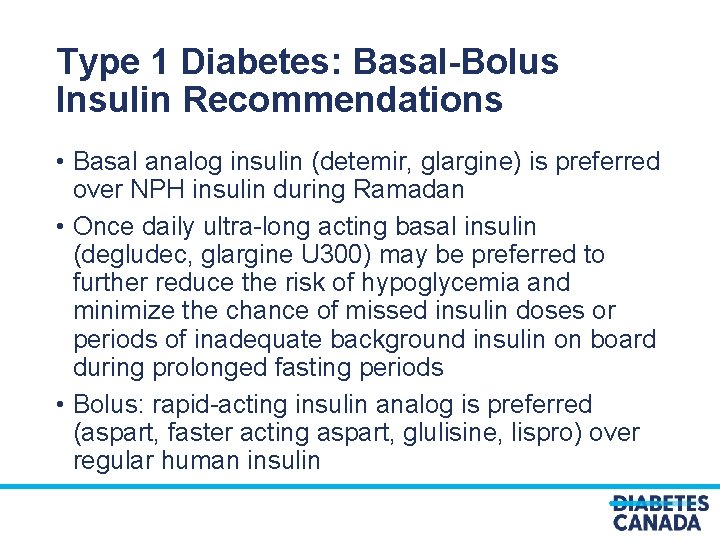
Type 1 Diabetes: Basal-Bolus Insulin Recommendations • Basal analog insulin (detemir, glargine) is preferred over NPH insulin during Ramadan • Once daily ultra-long acting basal insulin (degludec, glargine U 300) may be preferred to further reduce the risk of hypoglycemia and minimize the chance of missed insulin doses or periods of inadequate background insulin on board during prolonged fasting periods • Bolus: rapid-acting insulin analog is preferred (aspart, faster acting aspart, glulisine, lispro) over regular human insulin
Type 1 Diabetes: Insulin Dose Recommendations • All basal insulin doses (or daytime basal doses on insulin pump therapy) should be reduced by a minimum of 20% for fasting days to reduce the risk of hypoglycemia and reassessed weekly (physically or virtually) for further adjustments • Insulin-to-carbohydrate ratio and insulin sensitivity factor should remain unchanged during fasting if stable and well controlled

DKA during Ramadan People with type 1 diabetes should monitor blood ketones when SMBG readings are elevated >14. 0 mmol/L to screen for DKA. Those with blood ketones > 0. 6 mmol/L should: • break their fast, • take a supplemental dose of rapid-acting insulin for correction of blood ketones and • re-evaluate their ability to safely fast during Ramadan in the future DKA: Diabetic ketoacidosis; SMBG: Self-monitoring of blood glucose
Monitoring glycemic control while fasting in Ramadan
Self-monitoring of Blood Glucose (SMBG): Myths & Misconceptions • Does pricking the skin invalidate the fast? Response: Religious authorities agree that glucose monitoring does not invalidate the fast • Will frequent SMBG checks increase the chances to break the fast? Response: frequent SMBG may reduce the frequency and severity of hypoglycemic episodes so that fasting can be performed safely
SMBG Frequency • At least 5 times per day for type 1 diabetes • 2 -5 times per day for type 2 diabetes on insulin • Type 2 diabetes not requiring insulin: individualize SMBG frequency depending on the type of therapy, risk of hypoglycemia or hyperglycemia, level of glycemic control and duration of fast • Additional testing for periods of symptomatic hyperglycemia or hypoglycemia
When to Break The Fast? Counseling to break the fast, treat the problem appropriately and seek immediate medical attention for: • Symptomatic or documented (< 4 mmol/L) hypoglycemia or • Symptomatic hyperglycemia or documented blood glucose above 16. 7 mmol/L
Continuous (CGM) or Flash (FGM) Glucose Monitoring During Ramadan fasting, real-time CGM or FGM may be considered for people with type 1 or those with type 2 diabetes who are on complex insulin regimen (defined as basal plus at least one bolus insulin)
Visit guidelines. diabetes. ca

Or download the App
Diabetes Canada Clinical Practice Guidelines http: //guidelines. diabete s. ca – for health-care providers 1 -800 -BANTING (2268464) http: //diabetes. ca – for people with diabetes