Popliteal vessel injury Supparerk Prichayudh M D the













- Slides: 40
Popliteal vessel injury Supparerk Prichayudh, M. D.
• the most limb threatening of peripheral vascular injuries (amputation 14. 5%: NTDB) – The popliteal artery is a true end artery with a tenuous collateral supply. – The popliteal vein provides the bulk of lower leg and foot drainage.
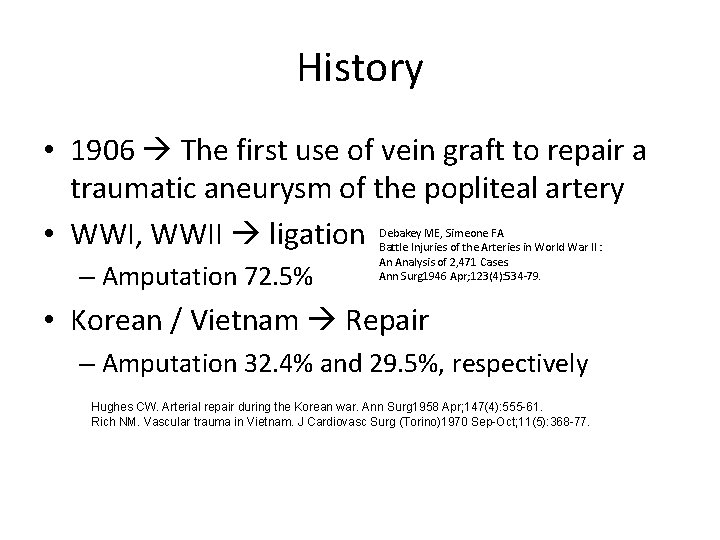
History • 1906 The first use of vein graft to repair a traumatic aneurysm of the popliteal artery • WWI, WWII ligation – Amputation 72. 5% Debakey ME, Simeone FA. Battle Injuries of the Arteries in World War II : An Analysis of 2, 471 Cases. Ann Surg 1946 Apr; 123(4): 534 -79. • Korean / Vietnam Repair – Amputation 32. 4% and 29. 5%, respectively Hughes CW. Arterial repair during the Korean war. Ann Surg 1958 Apr; 147(4): 555 -61. Rich NM. Vascular trauma in Vietnam. J Cardiovasc Surg (Torino)1970 Sep-Oct; 11(5): 368 -77.
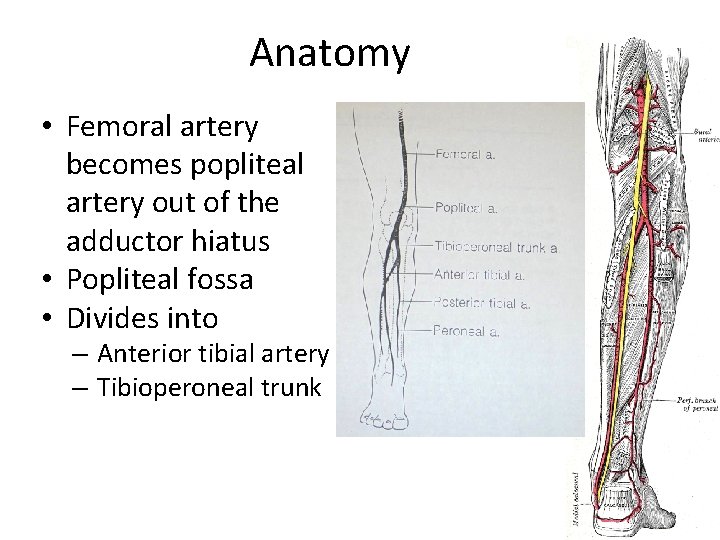
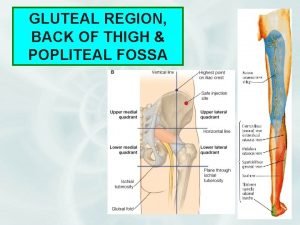
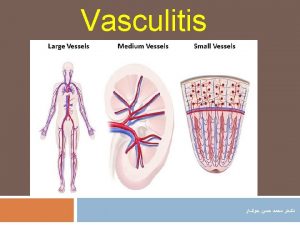
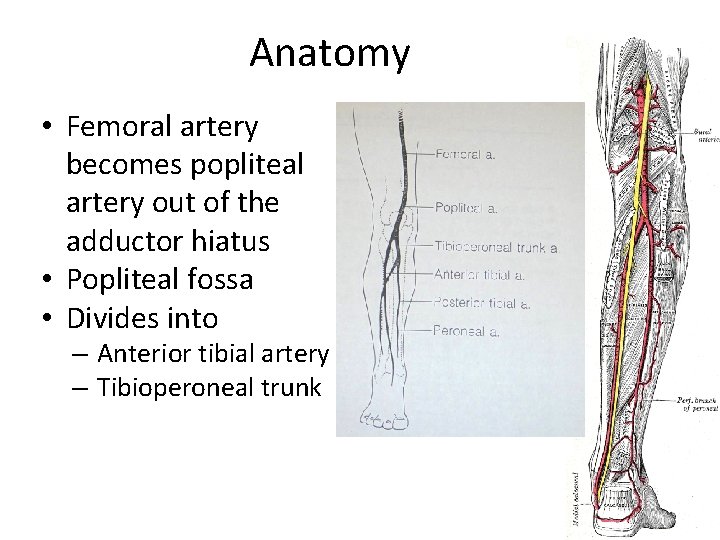
Anatomy • Femoral artery becomes popliteal artery out of the adductor hiatus • Popliteal fossa • Divides into – Anterior tibial artery – Tibioperoneal trunk

Popliteal fossa • Medial Pes Ancerinus – Satorius – Gracilis – Semimembranosus, Semitendinosus • Lateral Bicep femoris • Inferior Gastrocnemius

Incidence: popliteal a. injury • • NTDB 0. 1% 19% of all extremity arterial injuries Military 20 -26% Civilian – blunt mechanisms 20% to 75 – 5. 6 per 1000 cases of penetrating – 1. 6 per 1000 cases of blunt Fryburg, Surg Clin N Am, 2002

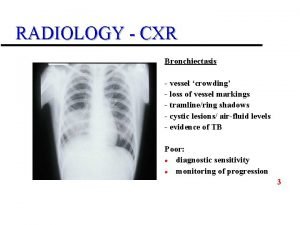
Diagnosis • PE • • • Deformity, wounds Bleeding, hematoma Pulses Signs of ischemia Neurological examination Posterior knee dislocation – Popliteal a. injury up to 25%
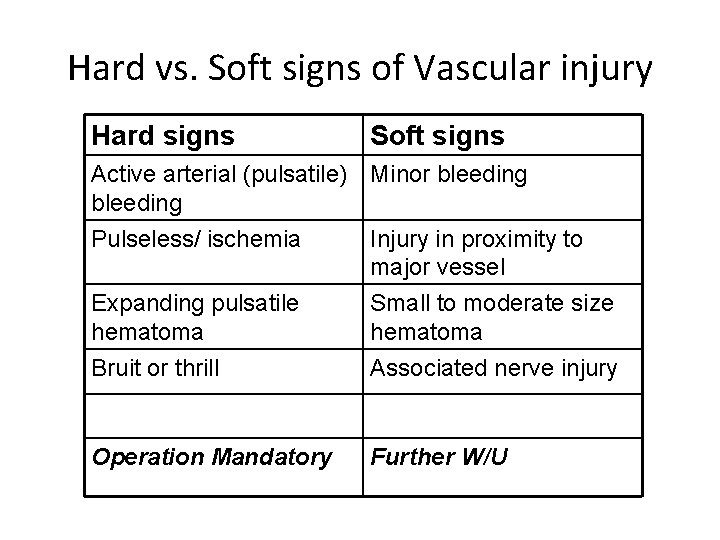
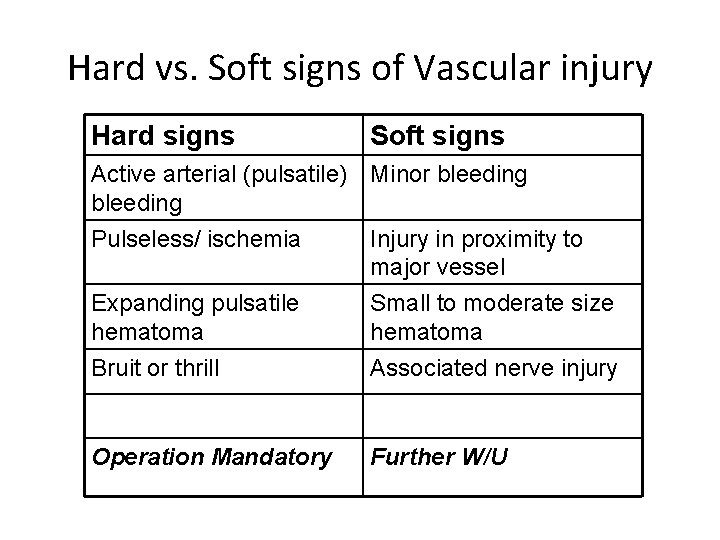
Hard vs. Soft signs of Vascular injury Hard signs Soft signs Active arterial (pulsatile) Minor bleeding Pulseless/ ischemia Injury in proximity to major vessel Expanding pulsatile hematoma Bruit or thrill Small to moderate size hematoma Associated nerve injury Operation Mandatory Further W/U
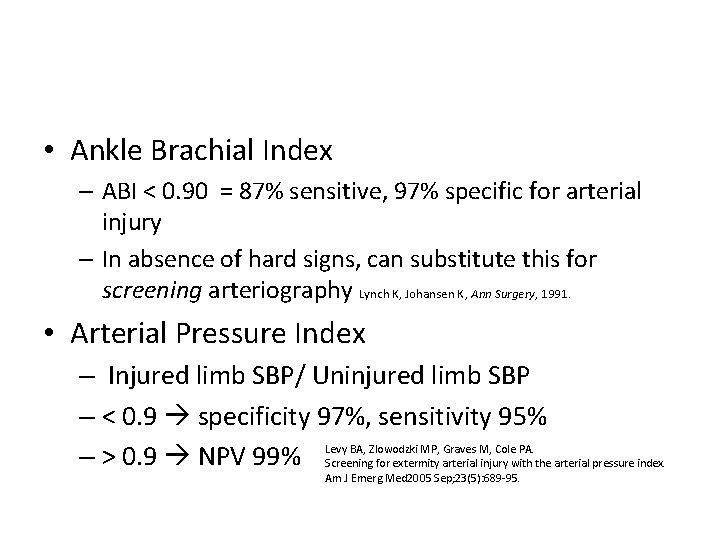
• Ankle Brachial Index – ABI < 0. 90 = 87% sensitive, 97% specific for arterial injury – In absence of hard signs, can substitute this for screening arteriography Lynch K, Johansen K, Ann Surgery, 1991. • Arterial Pressure Index – Injured limb SBP/ Uninjured limb SBP – < 0. 9 specificity 97%, sensitivity 95% – > 0. 9 NPV 99% Levy BA, Zlowodzki MP, Graves M, Cole PA. Screening for extermity arterial injury with the arterial pressure index. Am J Emerg Med 2005 Sep; 23(5): 689 -95.
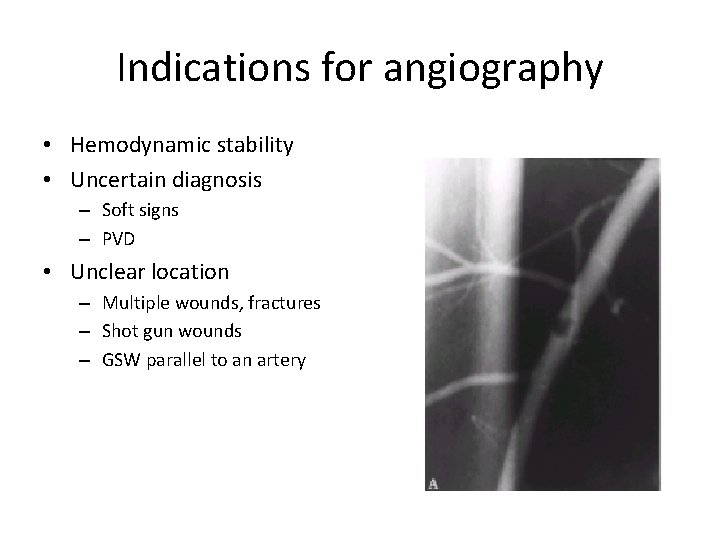
Indications for angiography • Hemodynamic stability • Uncertain diagnosis – Soft signs – PVD • Unclear location – Multiple wounds, fractures – Shot gun wounds – GSW parallel to an artery
Non invasive studies • Doppler US – sensitivity 50% • CT Angiography – Sens 95 -100%, Spec 87% – Limitations: • difficulty differentiating spasm from occlusion • artifact from high attenuation structures like bullet fragments or other foreign matter Rieger M, et al. A, Traumatic arterial injuries of the extremities: initial evaluation with MDCT angiography. Am J Roentgenol 2006 Mar; 186(3): 656 -64. Peng PD, et al. , Brundage SI. CT angiography effectively evaluates extremity vascular trauma. Am Surg 2008 Feb; 74(2): 103 -7. Fishman EK, et al. Multidetector CT and three-dimensional CT angiography for suspected vascular trauma of the extremities. Radiographics 2008 May-Jun; 28(3): 653 -65; discussion 65 -6.
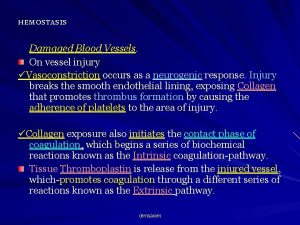
General Principle of management ABCs Active bleeding, limb threatening ischemia OR Stable, good limb viability may investigate Non-operative management non-occlusive lesion in asymptomatic patient • Pre-operative management • • – Prophylactic antibiotic – Single dose heparin iv if no C/I • Do not reperfuse dead limb! amputation
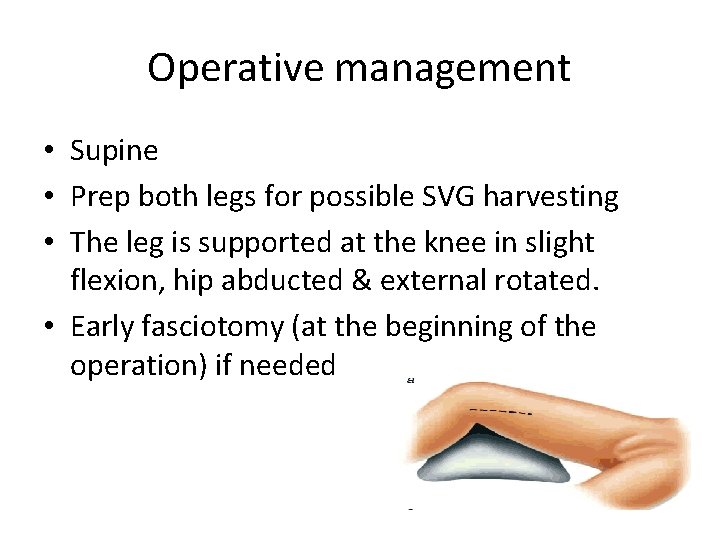
Operative management • Supine • Prep both legs for possible SVG harvesting • The leg is supported at the knee in slight flexion, hip abducted & external rotated. • Early fasciotomy (at the beginning of the operation) if needed
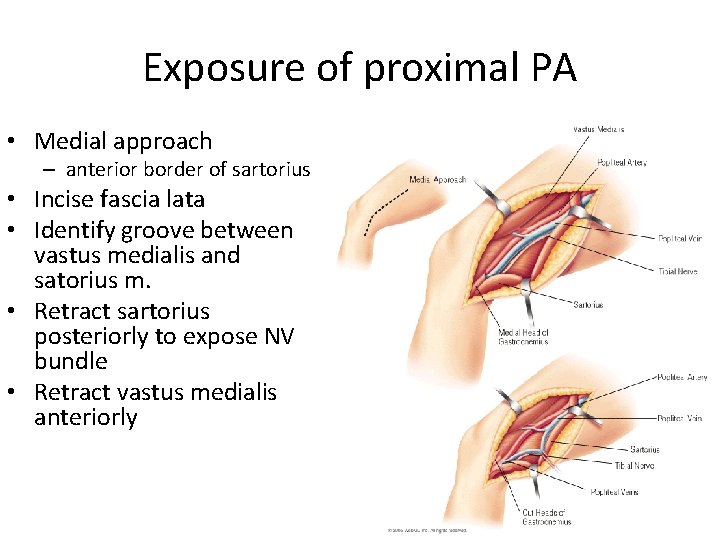
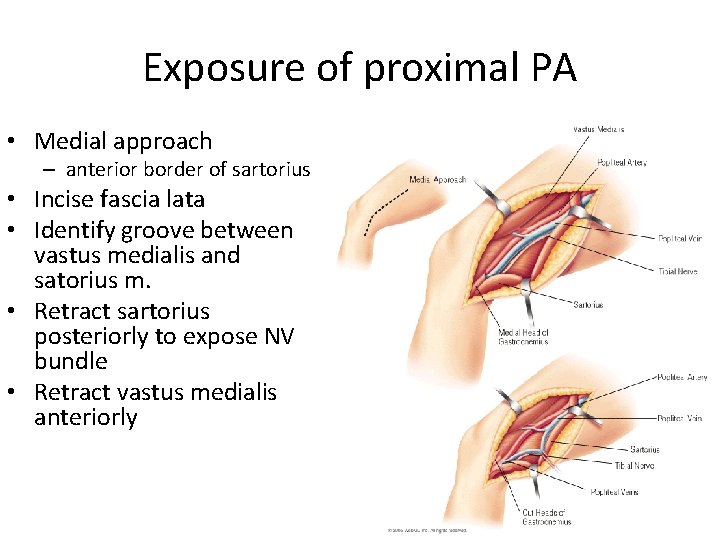
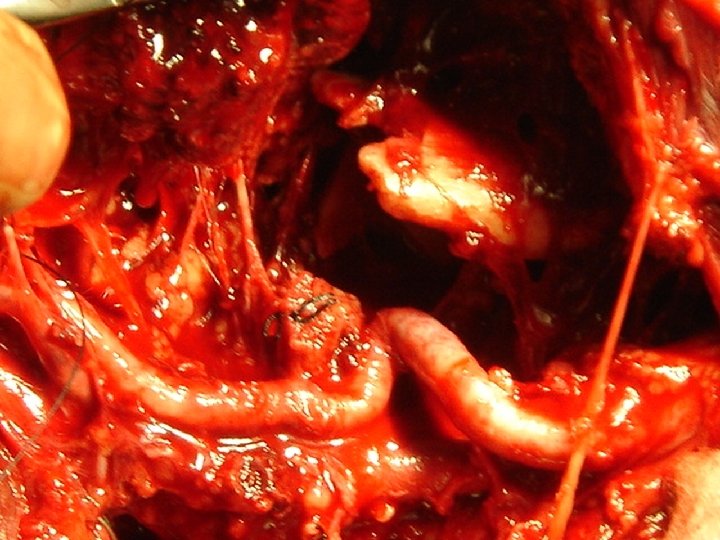
Exposure of proximal PA • Medial approach – anterior border of sartorius • Incise fascia lata • Identify groove between vastus medialis and satorius m. • Retract sartorius posteriorly to expose NV bundle • Retract vastus medialis anteriorly

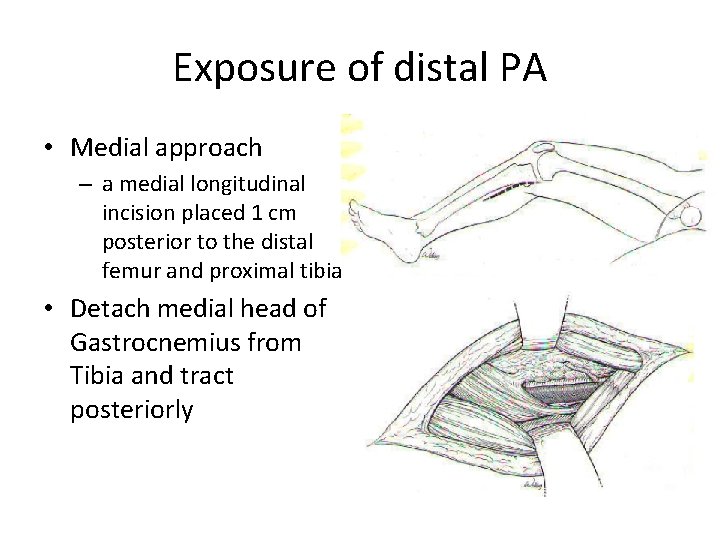
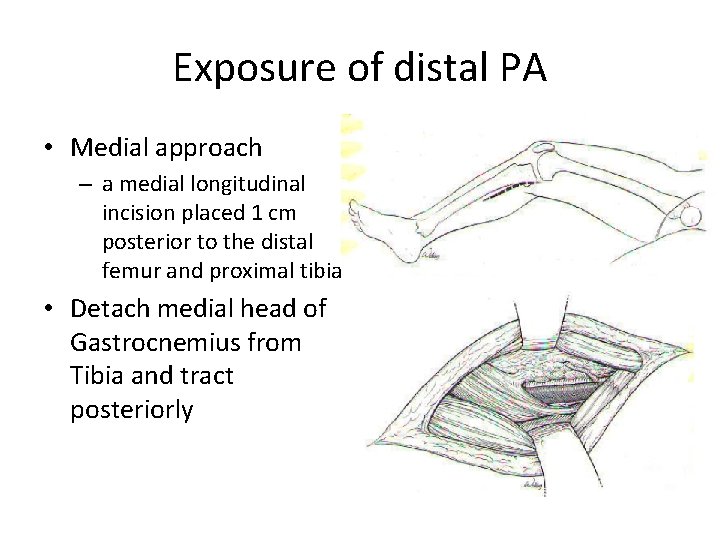
Exposure of distal PA • Medial approach – a medial longitudinal incision placed 1 cm posterior to the distal femur and proximal tibia • Detach medial head of Gastrocnemius from Tibia and tract posteriorly
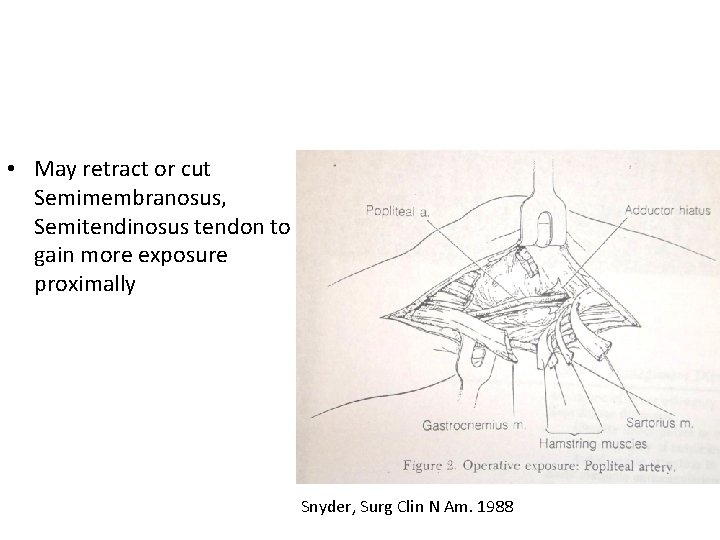
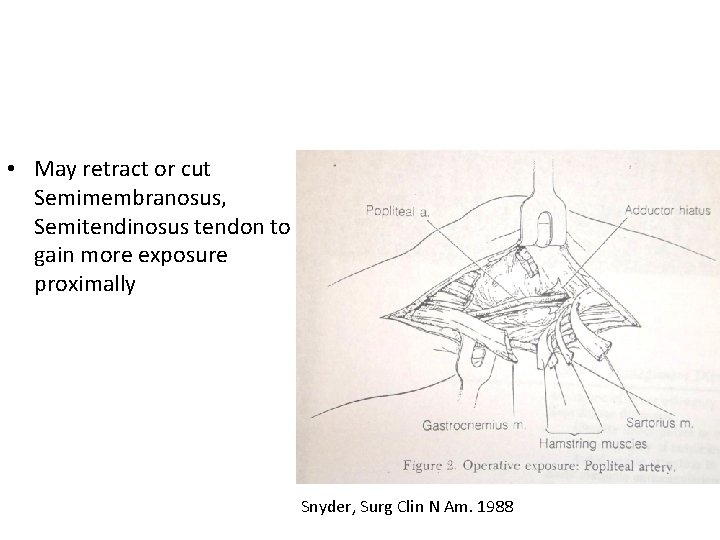
• May retract or cut Semimembranosus, Semitendinosus tendon to gain more exposure proximally Snyder, Surg Clin N Am. 1988
Principle of repair • Proximal & distal control • Identify injury • Resect the injured segment • Thrombectomy with a Fogarty catheter obtain good inflow and back-bleeding before the repair.
Intraoperative angiogram • Identify injury (limb threatening ischemia) • Save time • Amputation rate compared to formal angiogram (0% v. s. 30%) Callcut RA, et al. Impact of intraoperative arteriography on limb salvage for traumatic popliteal artery injury. J Trauma. 2009 Aug; 67(2): 252 -7. • Completion angiogram detect unsuspected problems requiring intervention in 8% Pasch AR, Bishara RA, Lim LT, et al: Optimal limb salvage in penetrating civilian vascular trauma. J Vasc Surg 3: 189– 195, 1986





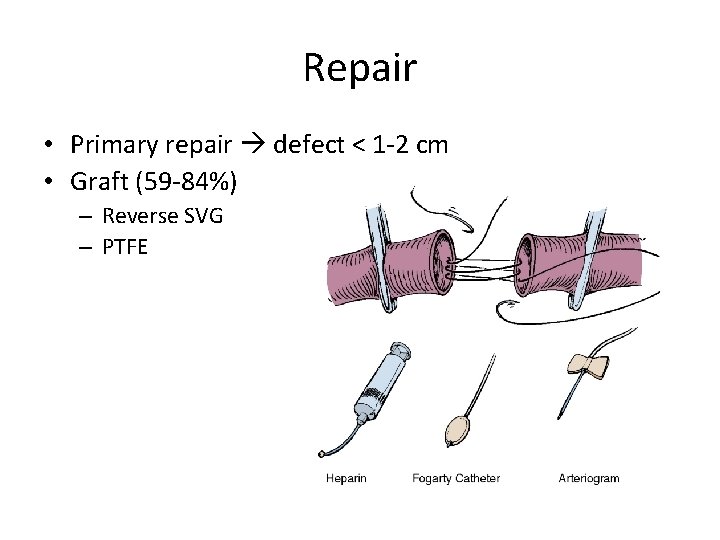
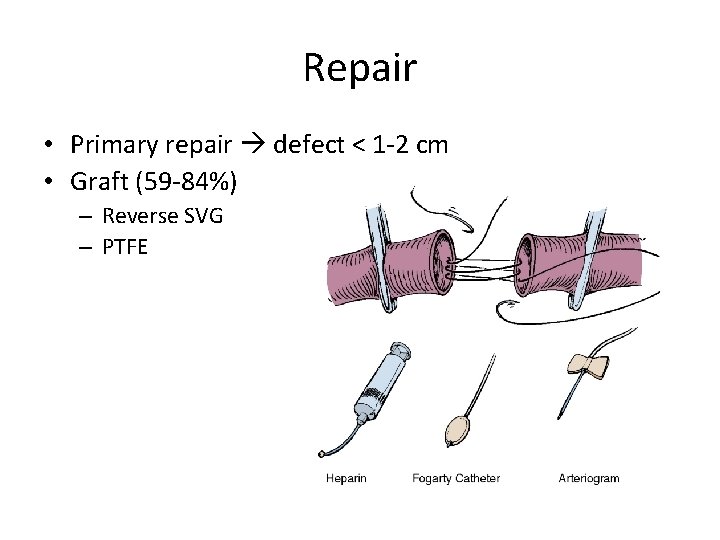
Repair • Primary repair defect < 1 -2 cm • Graft (59 -84%) – Reverse SVG – PTFE
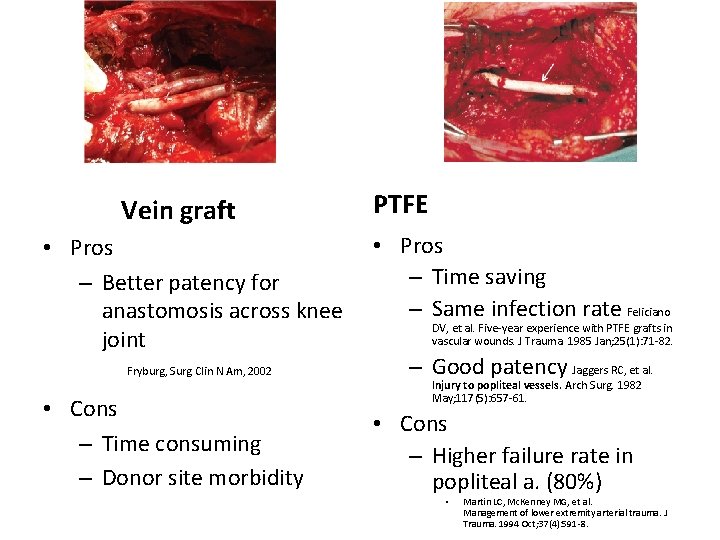
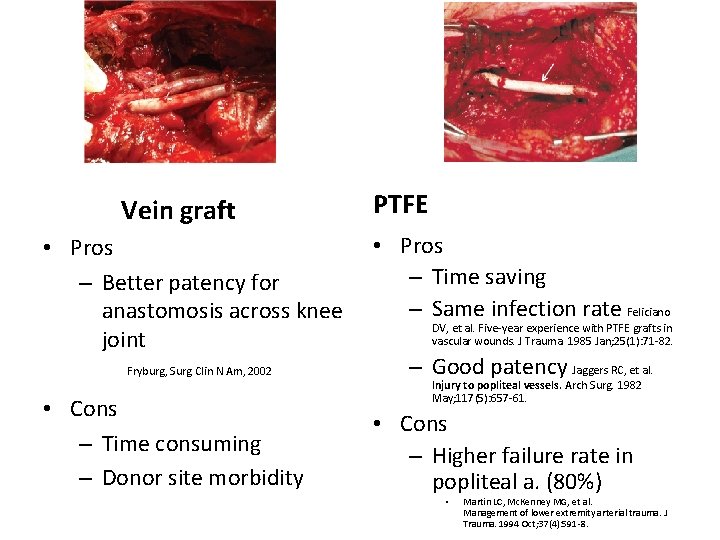
Vein graft • Pros – Better patency for anastomosis across knee joint Fryburg, Surg Clin N Am, 2002 • Cons – Time consuming – Donor site morbidity PTFE • Pros – Time saving – Same infection rate Feliciano DV, et al. Five-year experience with PTFE grafts in vascular wounds. J Trauma. 1985 Jan; 25(1): 71 -82. – Good patency Jaggers RC, et al. Injury to popliteal vessels. Arch Surg. 1982 May; 117(5): 657 -61. • Cons – Higher failure rate in popliteal a. (80%) • Martin LC, Mc. Kenney MG, et al. Management of lower extremity arterial trauma. J Trauma. 1994 Oct; 37(4): 591 -8.


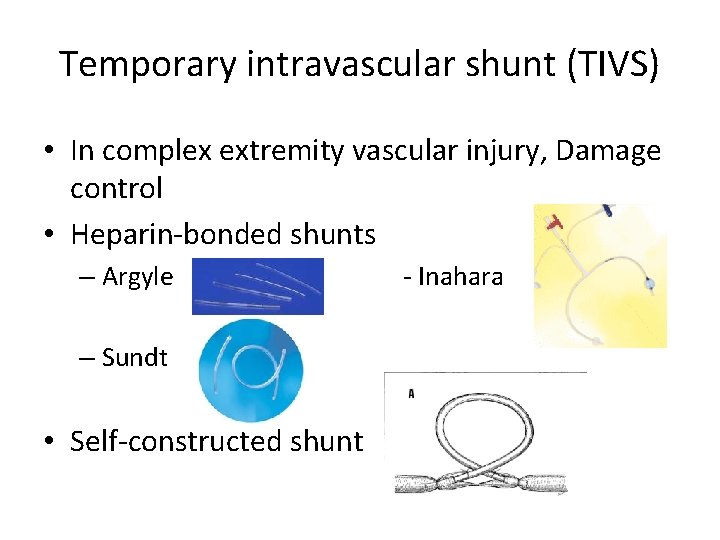
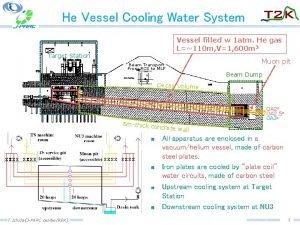
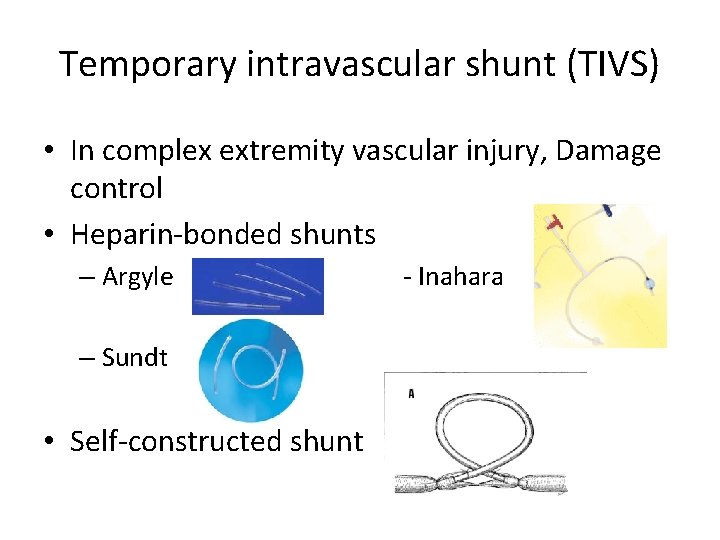
Temporary intravascular shunt (TIVS) • In complex extremity vascular injury, Damage control • Heparin-bonded shunts – Argyle – Sundt • Self-constructed shunt - Inahara

Venous injury • Should be repaired in stable patient if technically feasible – – Lateral venorrhaphy, EEA Complex repair (PTFE, SVG) Patency 75% Before arterial repair Management and short-term patency of lower extremity venous injuries with various repairs. Parry NG, Feliciano DV, et al. Am J Surg. 2003 Dec; 186(6): 631 -5. • Limb threatening ischemia Shunt a. repair v. • Ligation is safe alternative esp. in unstable patients, complex injuries. – 86% free of edema at D/C Yelon, et al. J Trauma 1992 – DVT 78%, no significant sequelae of CVI Kurtoglu, et al. Am Surg 2007 – Long term anticoagulation?
Combined vascular and orthopedic injury • Restore perfusion 1 st ! • Definitive repair – stable, minimally displaced Fx • TIVS – complex, displaced Fx – TIVS Bone manipulation definitive repair – avoid major stress on vascular anastomosis
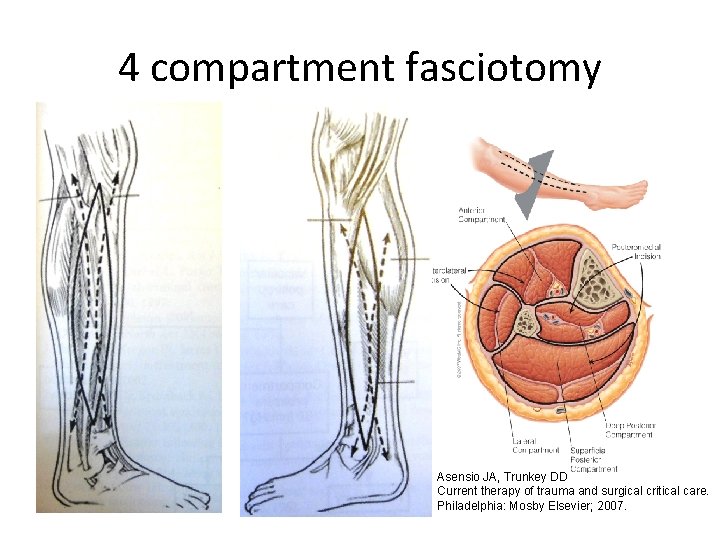
Early fasciotomy • • • Extremity swelling Severe distal musculoskeletal injury Prolonged shock Delayed restoration of flow (>4 -6 hr) Combined arterial-venous injuries Ligation of popliteal or multiple shank veins Snyder, Surg Clin N Am. 1988
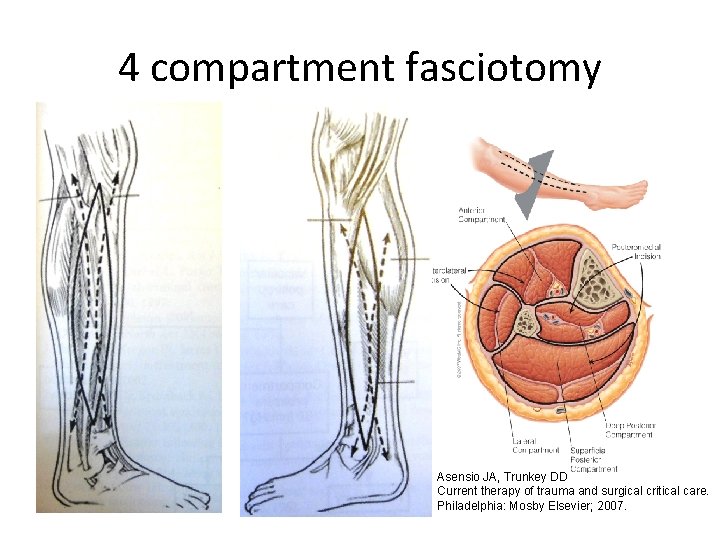
4 compartment fasciotomy Asensio JA, Trunkey DD Current therapy of trauma and surgical critical care. Philadelphia: Mosby Elsevier; 2007.
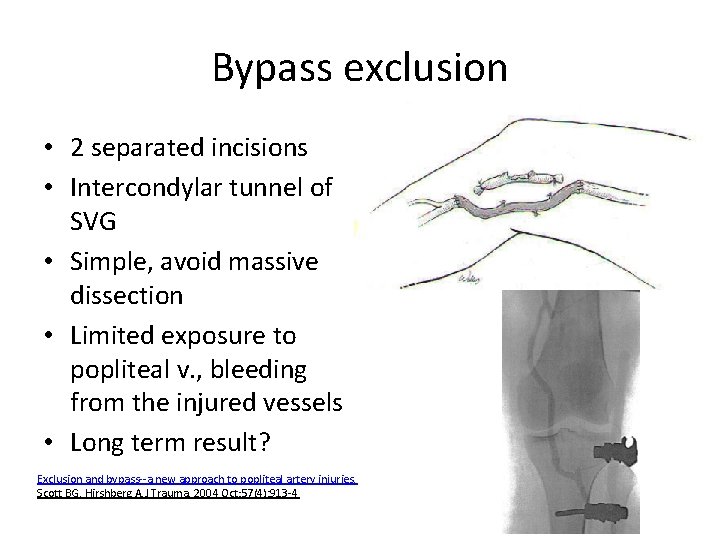
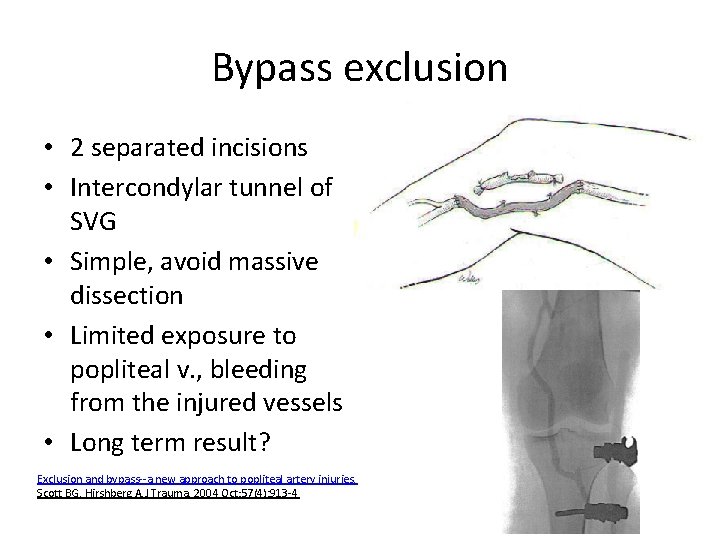
Bypass exclusion • 2 separated incisions • Intercondylar tunnel of SVG • Simple, avoid massive dissection • Limited exposure to popliteal v. , bleeding from the injured vessels • Long term result? Exclusion and bypass--a new approach to popliteal artery injuries. Scott BG, Hirshberg A. J Trauma. 2004 Oct; 57(4): 913 -4
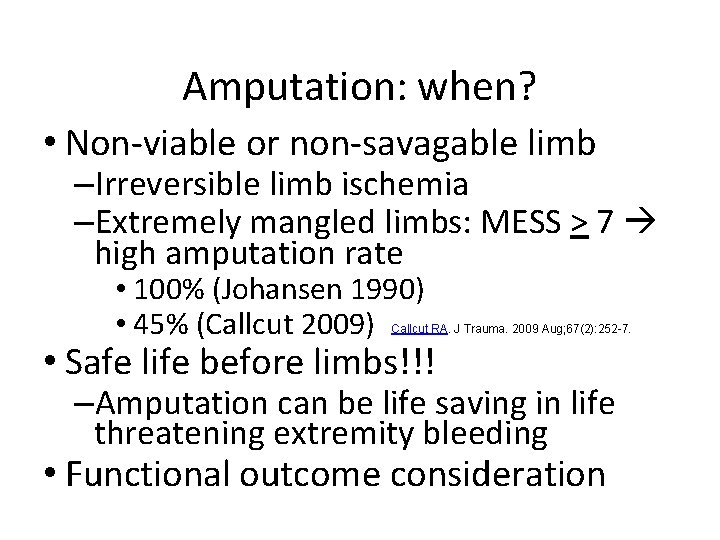
Amputation: when? • Non-viable or non-savagable limb –Irreversible limb ischemia –Extremely mangled limbs: MESS > 7 high amputation rate • 100% (Johansen 1990) • 45% (Callcut 2009) Callcut RA. J Trauma. 2009 Aug; 67(2): 252 -7. • Safe life before limbs!!! –Amputation can be life saving in life threatening extremity bleeding • Functional outcome consideration
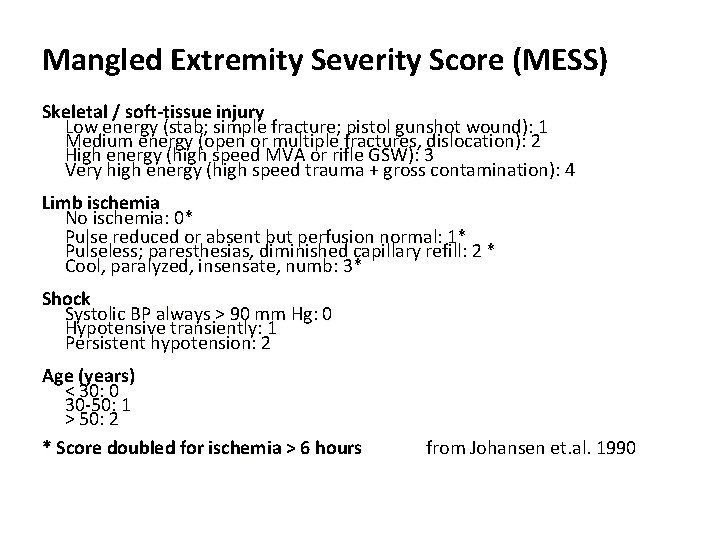
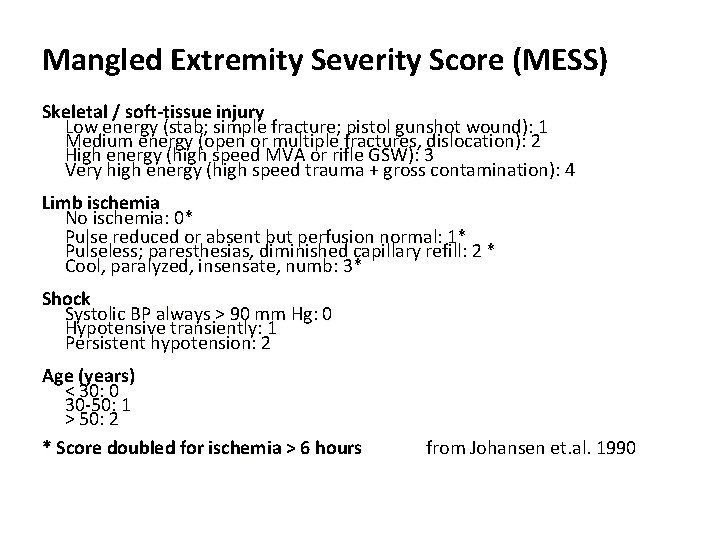
Mangled Extremity Severity Score (MESS) Skeletal / soft-tissue injury Low energy (stab; simple fracture; pistol gunshot wound): 1 Medium energy (open or multiple fractures, dislocation): 2 High energy (high speed MVA or rifle GSW): 3 Very high energy (high speed trauma + gross contamination): 4 Limb ischemia No ischemia: 0* Pulse reduced or absent but perfusion normal: 1* Pulseless; paresthesias, diminished capillary refill: 2 * Cool, paralyzed, insensate, numb: 3* Shock Systolic BP always > 90 mm Hg: 0 Hypotensive transiently: 1 Persistent hypotension: 2 Age (years) < 30: 0 30 -50: 1 > 50: 2 * Score doubled for ischemia > 6 hours from Johansen et. al. 1990
Factors associated with amputation • • • Extensive soft-tissue injuries Associated skeletal trauma Knee dislocations Prolonged ischemic times Nerve injury High extremity AIS 1)Yahya et al. ANZ J Surg, 2005 2) NTDB J Vasc Surg. 2006 Jul; 44(1): 94 -100

Amputation rate 0 -44%
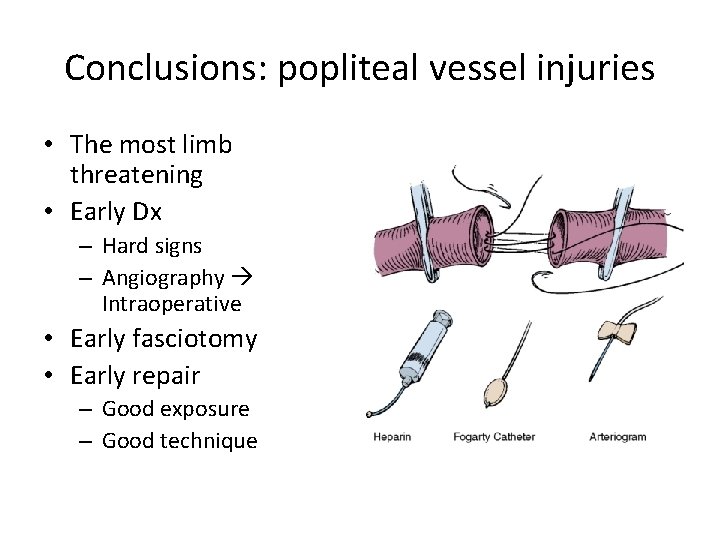
Conclusions: popliteal vessel injuries • The most limb threatening • Early Dx – Hard signs – Angiography Intraoperative • Early fasciotomy • Early repair – Good exposure – Good technique
 Failure to sense vs failure to capture
Failure to sense vs failure to capture Example of intentional injury
Example of intentional injury Femoral pulse location
Femoral pulse location Buttock popliteal length
Buttock popliteal length Superficial abdominal lymph nodes
Superficial abdominal lymph nodes Sports physician sachin khullar
Sports physician sachin khullar Clubfoot clinical features
Clubfoot clinical features Popliteal block coverage
Popliteal block coverage Thigh compartment muscles
Thigh compartment muscles Long saphenous vein
Long saphenous vein Compartments of the thigh
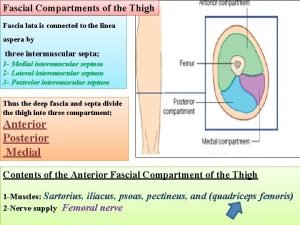
Compartments of the thigh Supraklavikuler lap
Supraklavikuler lap Oblique popliteal ligament
Oblique popliteal ligament Lumbar plexus
Lumbar plexus Mid inguinal point
Mid inguinal point Landau reflex vs parachute reflex
Landau reflex vs parachute reflex Anterior thigh
Anterior thigh Popliteal fossa structures
Popliteal fossa structures Popliteal length
Popliteal length Art genus
Art genus Popliteal fossa borders
Popliteal fossa borders Popliteal fossa
Popliteal fossa Posterior tibial artery
Posterior tibial artery Vertical definition
Vertical definition Floor of the popliteal fossa
Floor of the popliteal fossa Polietilen
Polietilen Popliteal entrapment
Popliteal entrapment Brachial pulse
Brachial pulse Oblique popliteal
Oblique popliteal Popliteal entrapment syndrome
Popliteal entrapment syndrome Diễn thế sinh thái là
Diễn thế sinh thái là đại từ thay thế
đại từ thay thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Công thức tiính động năng
Công thức tiính động năng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể độ dài liên kết
độ dài liên kết Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Môn thể thao bắt đầu bằng từ chạy
Môn thể thao bắt đầu bằng từ chạy