Polypharmacy as a rational treatment approach for chronic











- Slides: 42

Polypharmacy as a rational treatment approach for chronic pain Rollin M. Gallagher, MD, MPH University of Pennsylvania School of Medicine Philadelphia Veterans Medical Center Email: rgallagh@mail. med. upenn. edu
Goals of This Presentation 1) To review mechanisms of acute pain and chronic pain diseases and conditions 2) To discuss the rational use of polypharmacy and integrated multimodality treatment for chronic pain
Medication selection in pain is based upon more than just pain severity • Diagnosis • Mechanisms of pain(s) • Efficacy – Clinical trial data • Comorbidities: medical and psychiatric • Prior treatment responses • Side-effect burden, toxicity risk, drug and disease interactions • Gallagher RM, Verma S. Sem Neurosurg. 2004; 15: 31 -46. • Sindrup SH, Jensen TS. Pain. 1999; 83: 389 -400. • Galer BS. Neurology. 1995; 45(12 suppl 9): S 17 -S 25.
Medication selection in pain is based upon more than just pain severity • Ease of use – Dosing simplicity – Titration simplicity – Patient competence and convenience • Pain’s psychosocial context and the doctorpatient relationship: - stigma - cost - illness behavior - risk of treatment non-adherence - risk of medication misuse • Sindrup SH, Jensen TS. Pain. 1999; 83: 389 -400. • Galer BS. Neurology. 1995; 45(12 suppl 9): S 17 -S 25. • Gallagher RM, Verma S. Sem Neurosurg. 2004; 15: 31 -46.
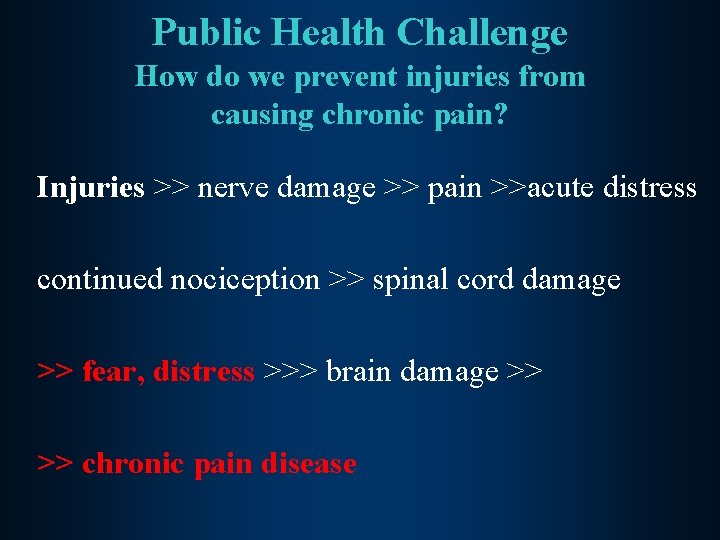
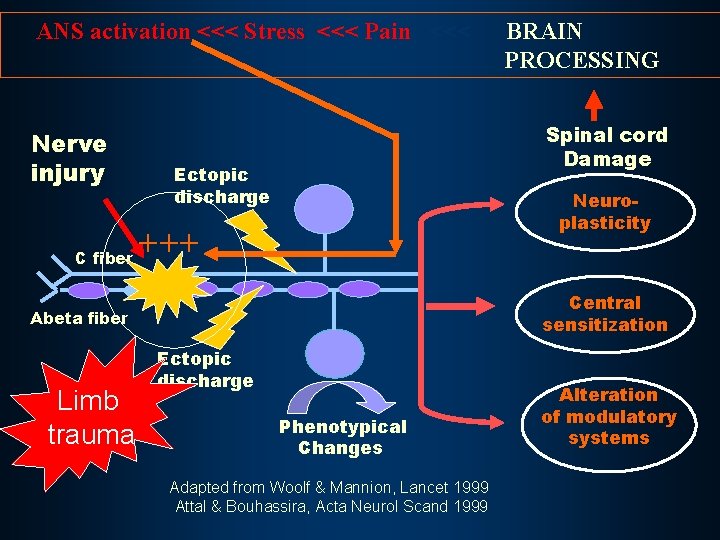
Public Health Challenge How do we prevent injuries from causing chronic pain? Injuries >> nerve damage >> pain >>acute distress continued nociception >> spinal cord damage >> fear, distress >>> brain damage >> >> chronic pain disease
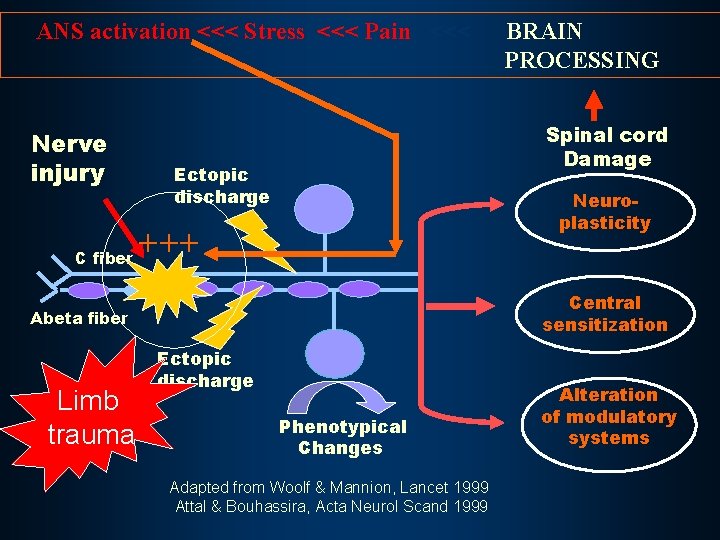
ANS activation <<< Stress <<< Pain <<< Nerve injury C fiber Spinal cord Damage Ectopic discharge Neuroplasticity +++ Central sensitization Abeta fiber Limb trauma BRAIN PROCESSING Ectopic discharge Phenotypical Changes Adapted from Woolf & Mannion, Lancet 1999 Attal & Bouhassira, Acta Neurol Scand 1999 Alteration of modulatory systems

THE END: CPRS Pain Cycle Pathophysiology of Maintenance: -Radiculopathy -Neuroma traction -Myofascial sensitization Psychopathology Acute injury of maintenance: and pain -Encoded anxiety dysregulation - PTSD -Emotional allodynia and mood Neurogenic disorder Inflammation: - Glial activation - Pro-inflammatory cytokines - blood-nerve barrier dysruption Pathology: -Muscle atrophy, weakness; -Bone demineralization; -Depression Central sensitization Disability Less active Kinesophobia Peripheral Decreased Sensitization: motivation Na+ channels Increased Lower threshold isolation Role loss

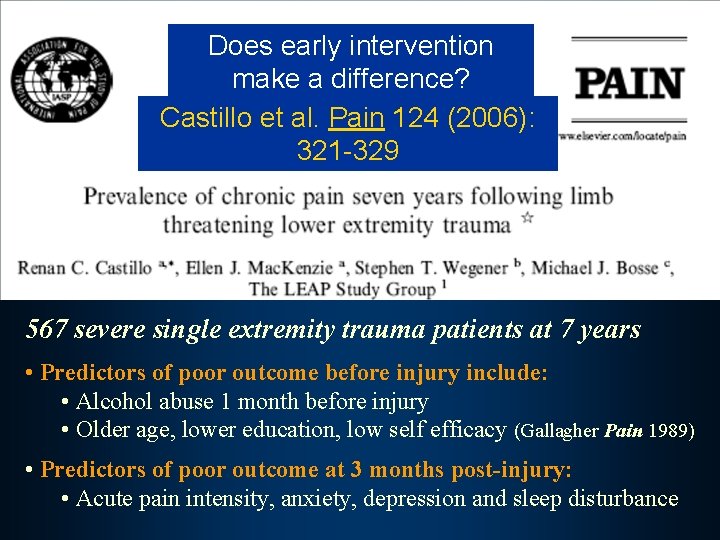
Challenges of OEF/OIF Veteran Cohort Recent evidence suggests that access to pain treatment after severe limb trauma leads to better outcomes.
Does early intervention make a difference? Castillo et al. Pain 124 (2006): 321 -329 567 severe single extremity trauma patients at 7 years • Predictors of poor outcome before injury include: • Alcohol abuse 1 month before injury • Older age, lower education, low self efficacy (Gallagher Pain 1989) • Predictors of poor outcome at 3 months post-injury: • Acute pain intensity, anxiety, depression and sleep disturbance
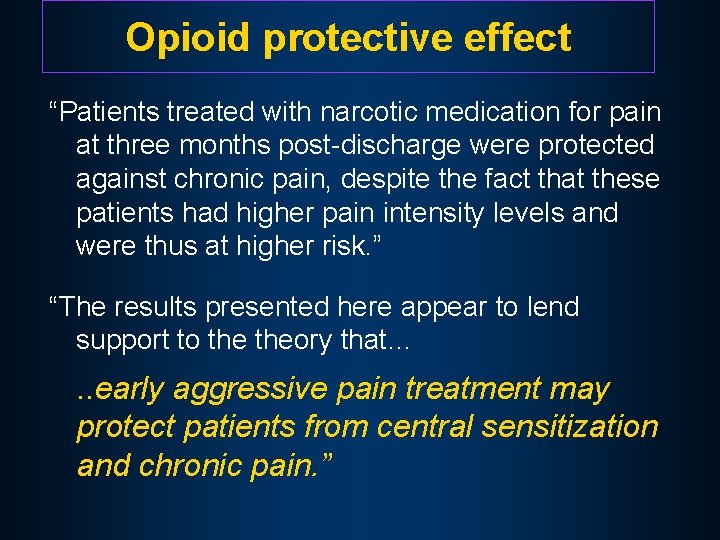
Opioid protective effect “Patients treated with narcotic medication for pain at three months post-discharge were protected against chronic pain, despite the fact that these patients had higher pain intensity levels and were thus at higher risk. ” “The results presented here appear to lend support to theory that… . . early aggressive pain treatment may protect patients from central sensitization and chronic pain. ”
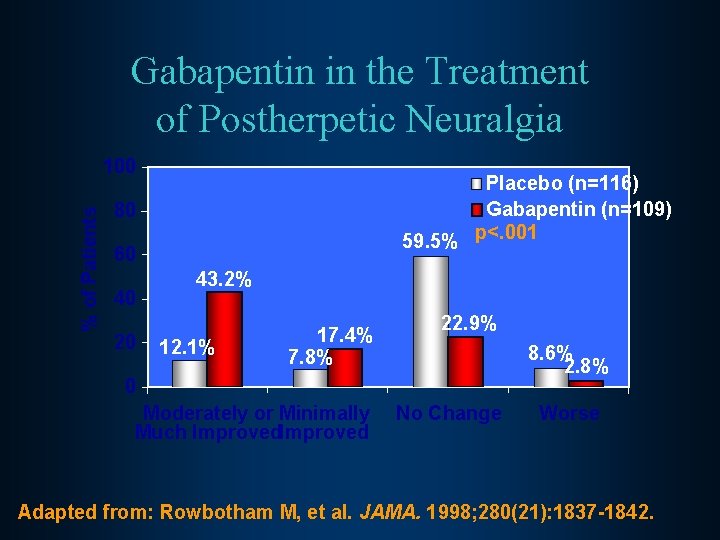
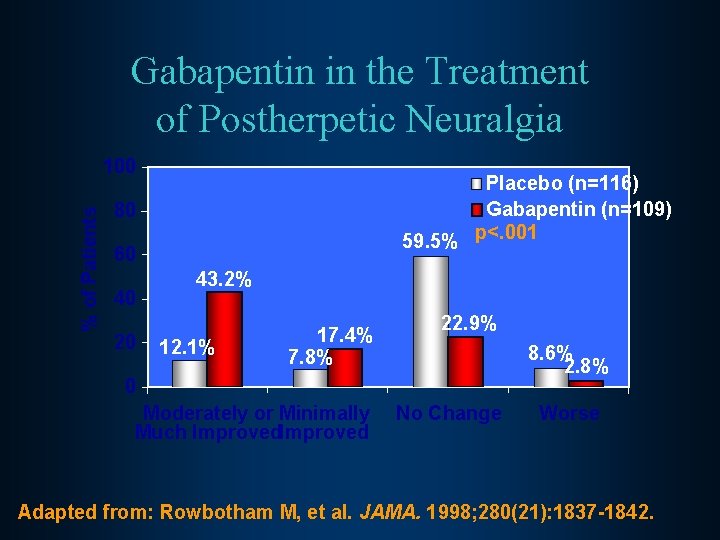
Gabapentin in the Treatment of Postherpetic Neuralgia % of Patients 100 Placebo (n=116) Gabapentin (n=109) 59. 5% p<. 001 80 60 40 20 43. 2% 12. 1% 17. 4% 7. 8% 22. 9% 8. 6% 2. 8% 0 Moderately or Minimally Much Improved No Change Worse Adapted from: Rowbotham M, et al. JAMA. 1998; 280(21): 1837 -1842.
What happens above the spinal cord?
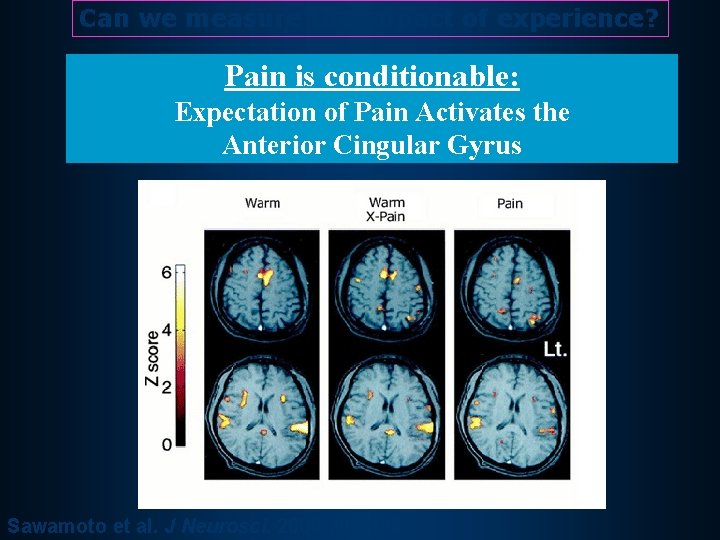
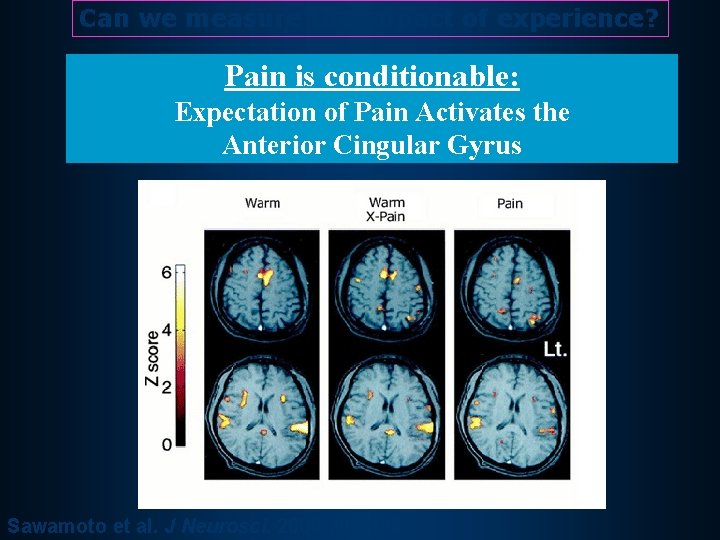
Can we measure the impact of experience? Pain is conditionable: Expectation of Pain Activates the Anterior Cingular Gyrus Sawamoto et al. J Neurosci. 2000; 20: 7438.

PAIN and EMOTION Serotonin and Norepinephrine in Depression and Pain Prefront al Cortex anterior cingulat e Limbic System Serotonin Pathways Norepinephrine Pathways Locus Ceruleus Raphe Verma S, Gallagher RM. Int Rev Psychiatry. 2000; 12(2): 103 -114. Blier P, Abbott FV. J Psychiatry Neurosci.
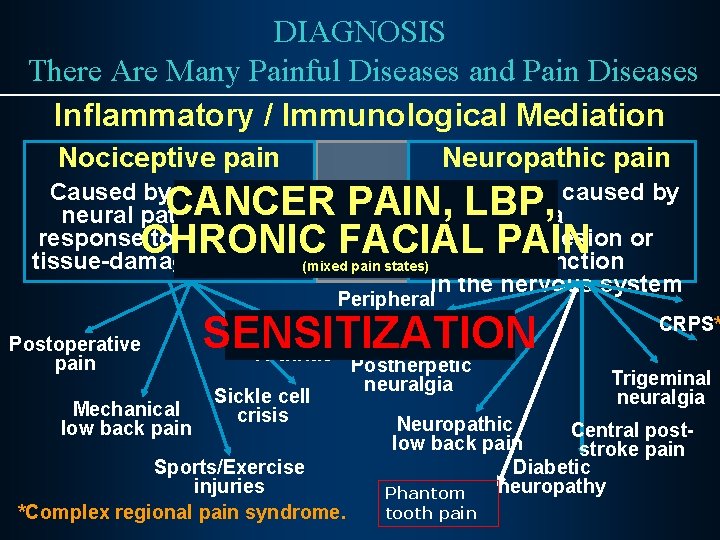
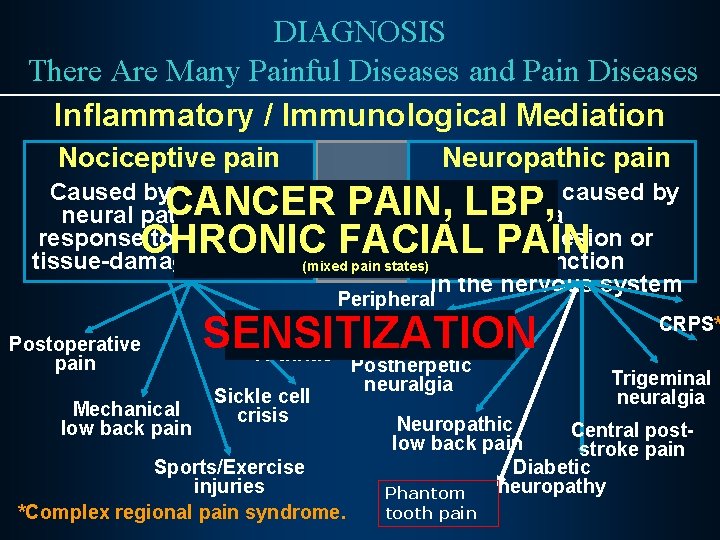
DIAGNOSIS There Are Many Painful Diseases and Pain Diseases Inflammatory / Immunological Mediation Nociceptive pain Neuropathic pain Caused by activity in Initiated or caused by neural pathways in a response to potentially primary lesion or tissue-damaging stimuli(mixed pain states) dysfunction in the nervous system CANCER PAIN, LBP, CHRONIC FACIAL PAIN Peripheral neuropathy Postoperative pain Mechanical low back pain SENSITIZATION Arthritis Sickle cell crisis Sports/Exercise injuries *Complex regional pain syndrome. Postherpetic neuralgia CRPS* Trigeminal neuralgia Neuropathic Central postlow back pain stroke pain Diabetic neuropathy Phantom tooth pain
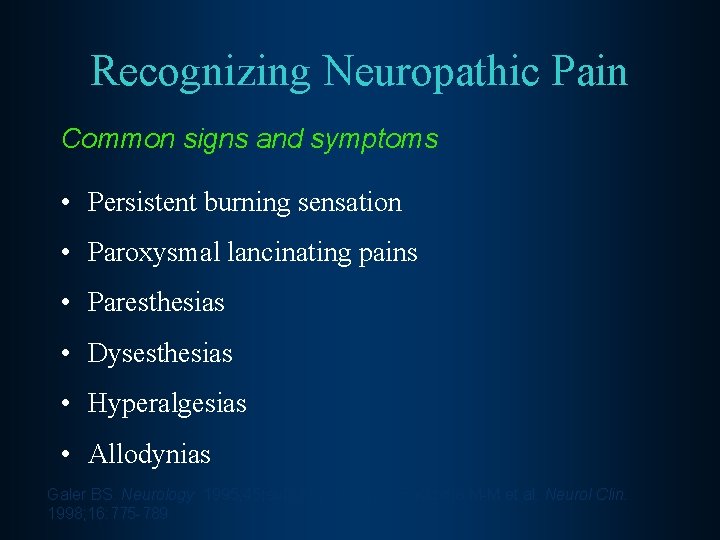
Recognizing Neuropathic Pain Common signs and symptoms • Persistent burning sensation • Paroxysmal lancinating pains • Paresthesias • Dysesthesias • Hyperalgesias • Allodynias Galer BS. Neurology. 1995; 45(suppl 9): S 17 -S 25; Backonja M-M et al. Neurol Clin. 1998; 16: 775 -789.

Pain Drawing & Neuropathy Types Boulton AJM et al. Med Clin North Am. 1998; 82: 909 -929; Portenoy RK. Pain Management: Theory and Practice. 1996: 108 -113; Katz N. Clin J Pain. 2000; 16: S 41 -S 48
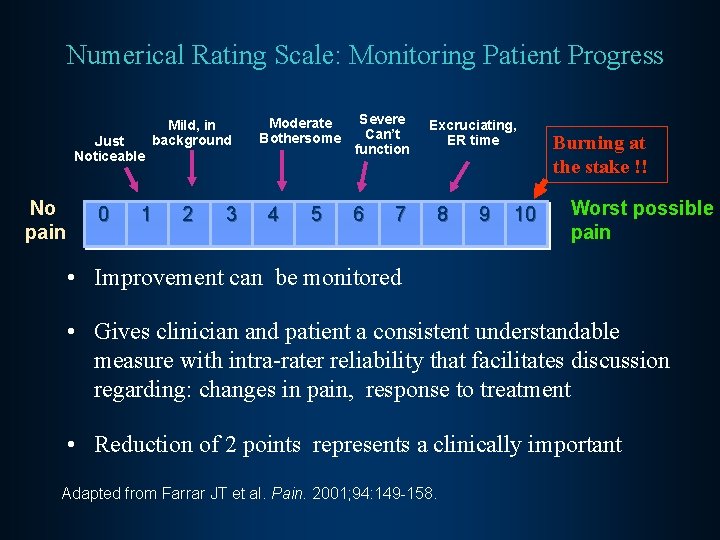
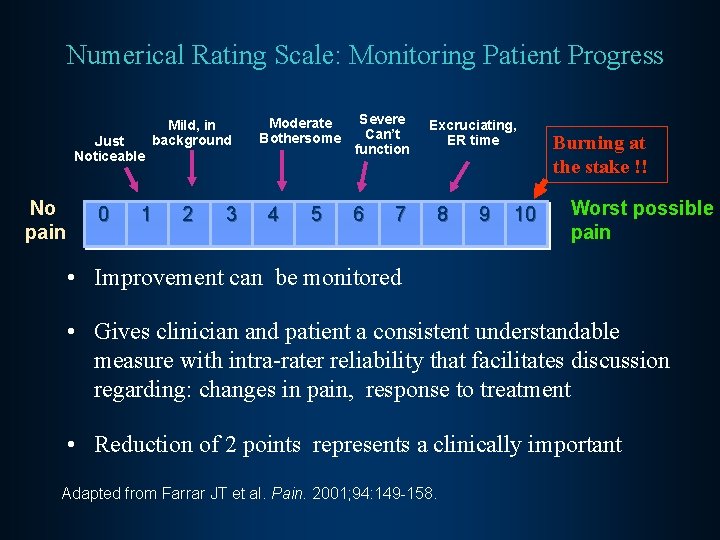
Numerical Rating Scale: Monitoring Patient Progress Just Noticeable No pain 0 Mild, in background 1 2 3 Moderate Bothersome 4 5 Severe Can’t function 6 7 Excruciating, ER time 8 9 10 Burning at the stake !! Worst possible pain • Improvement can be monitored • Gives clinician and patient a consistent understandable measure with intra-rater reliability that facilitates discussion regarding: changes in pain, response to treatment • Reduction of 2 points represents a clinically important Adapted from Farrar JT et al. Pain. 2001; 94: 149 -158.

Efficacy – Medication Trials Disease specific vs Mechanism specific
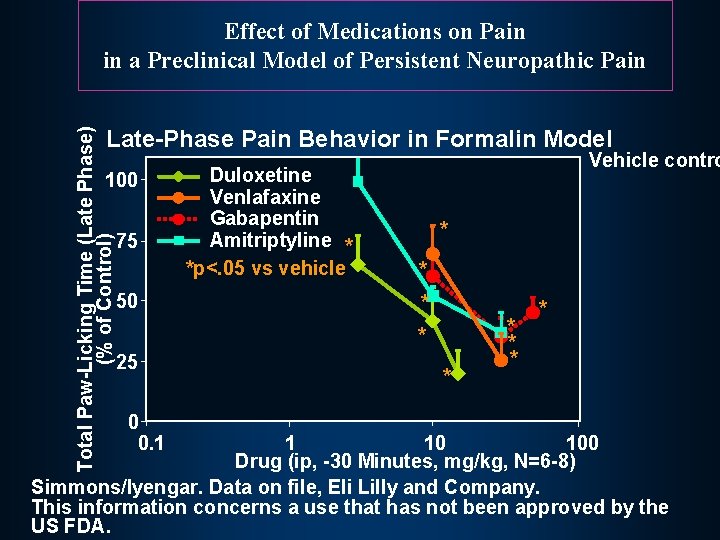
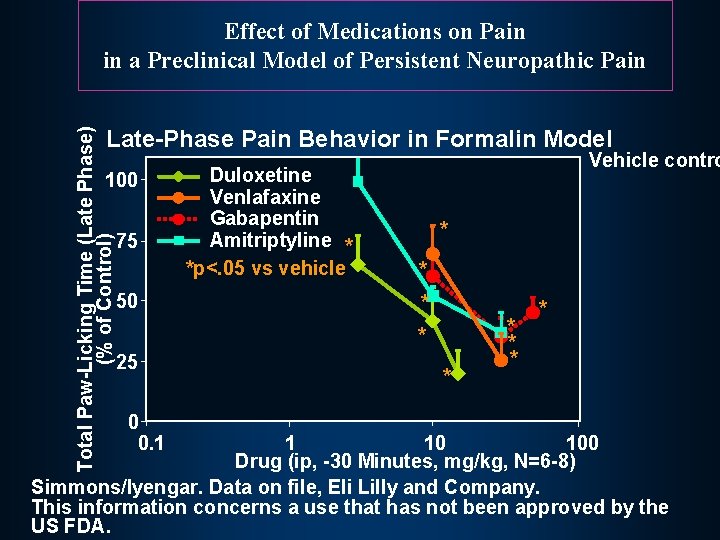
Effect of Medications on Pain in a Preclinical Model of Persistent Neuropathic Pain Total Paw-Licking Time (Late Phase) (% of Control) Late-Phase Pain Behavior in Formalin Model 100 75 50 Duloxetine Venlafaxine Gabapentin Amitriptyline * *p<. 05 vs vehicle Vehicle contro * * 25 0 0. 1 * * * 1 10 100 Drug (ip, -30 Minutes, mg/kg, N=6 -8) Simmons/Iyengar. Data on file, Eli Lilly and Company. This information concerns a use that has not been approved by the US FDA.
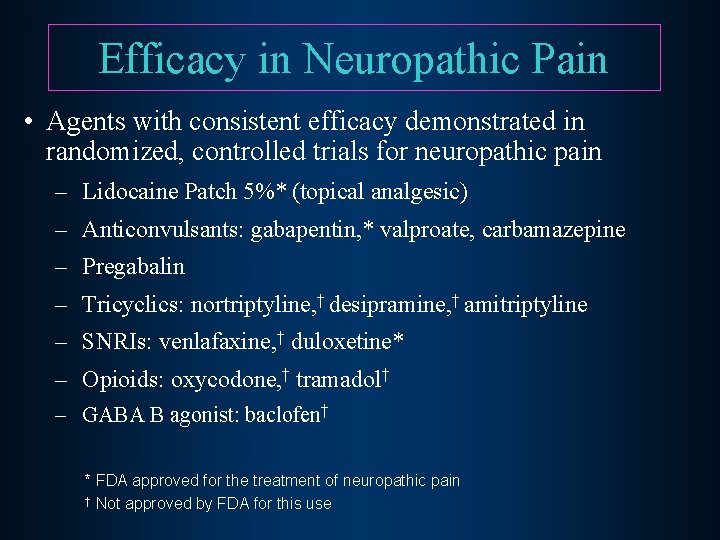
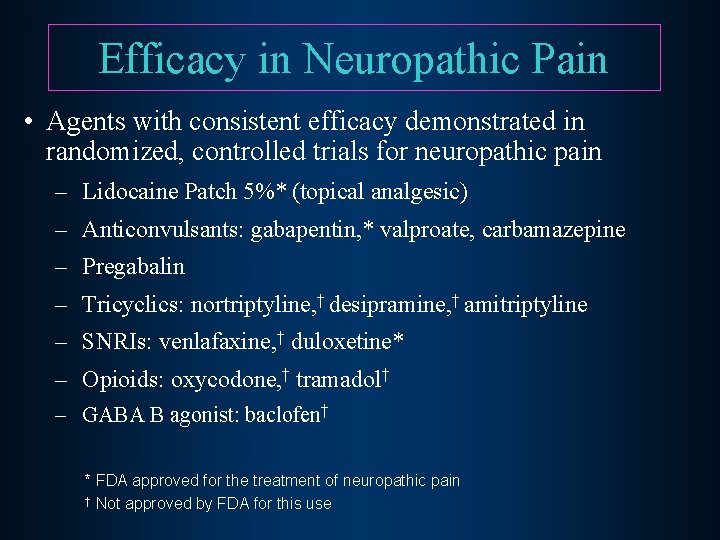
Efficacy in Neuropathic Pain • Agents with consistent efficacy demonstrated in randomized, controlled trials for neuropathic pain – Lidocaine Patch 5%* (topical analgesic) – Anticonvulsants: gabapentin, * valproate, carbamazepine – Pregabalin – Tricyclics: nortriptyline, † desipramine, † amitriptyline – SNRIs: venlafaxine, † duloxetine* – Opioids: oxycodone, † tramadol† – GABA B agonist: baclofen† * FDA approved for the treatment of neuropathic pain † Not approved by FDA for this use
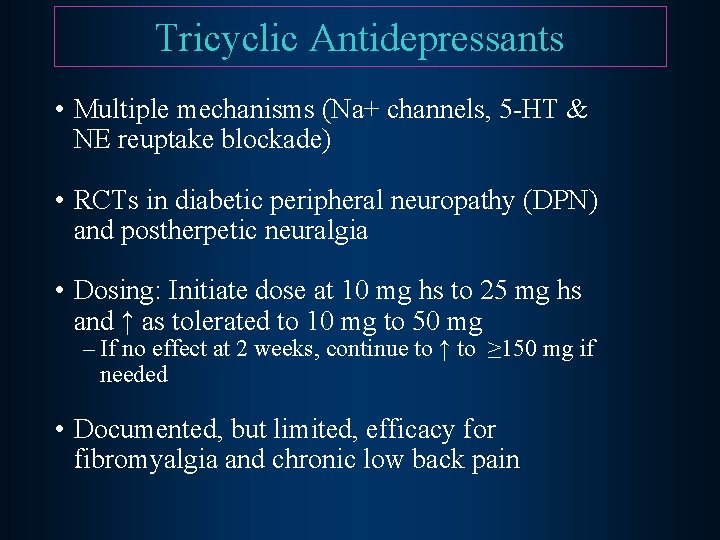
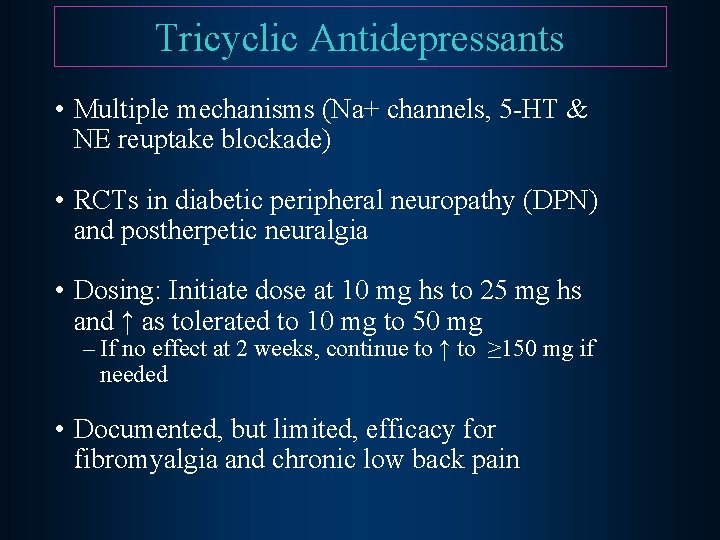
Tricyclic Antidepressants • Multiple mechanisms (Na+ channels, 5 -HT & NE reuptake blockade) • RCTs in diabetic peripheral neuropathy (DPN) and postherpetic neuralgia • Dosing: Initiate dose at 10 mg hs to 25 mg hs and ↑ as tolerated to 10 mg to 50 mg – If no effect at 2 weeks, continue to ↑ to ≥ 150 mg if needed • Documented, but limited, efficacy for fibromyalgia and chronic low back pain

Other NP agents Voltage gated Calcium channels: 1) Gabapentin: Every 3 -5 days 1) 2) 3) 4) 5) 6) • 0 300 300 600 0 0 300 300 600 300 mg 600 mg Pregabalin: Every 1 -2 weeks as tolerated • • 50 mg TID or 75 mg BID 100 mg TID or 150 mg BID
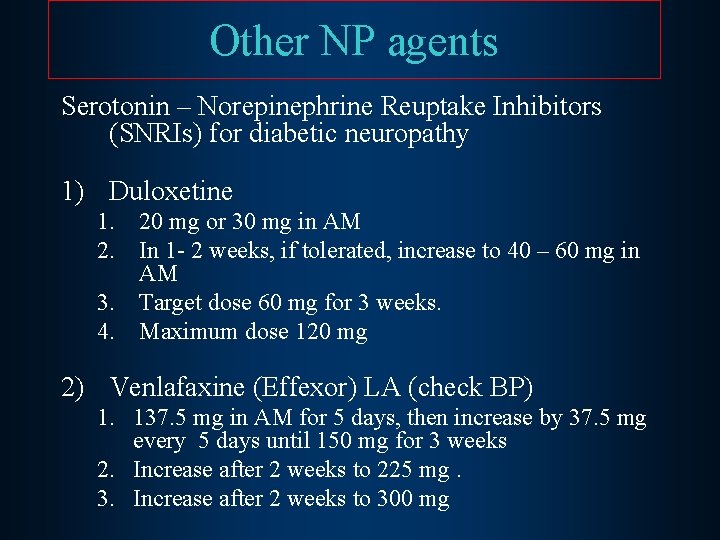
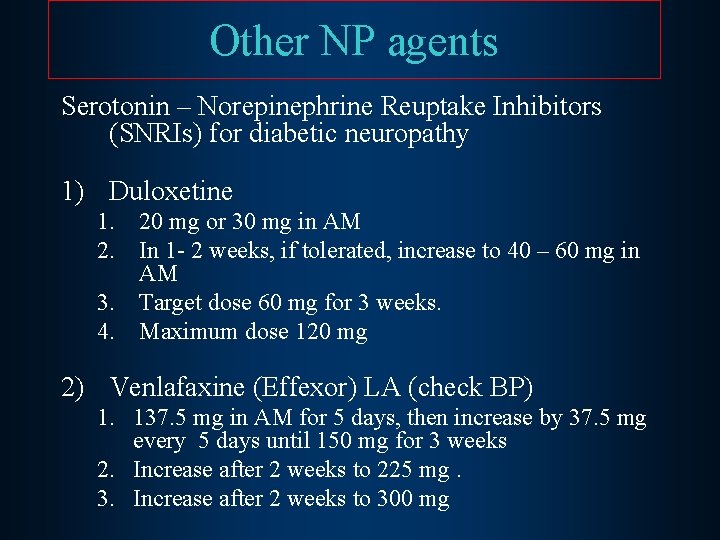
Other NP agents Serotonin – Norepinephrine Reuptake Inhibitors (SNRIs) for diabetic neuropathy 1) Duloxetine 1. 20 mg or 30 mg in AM 2. In 1 - 2 weeks, if tolerated, increase to 40 – 60 mg in AM 3. Target dose 60 mg for 3 weeks. 4. Maximum dose 120 mg 2) Venlafaxine (Effexor) LA (check BP) 1. 137. 5 mg in AM for 5 days, then increase by 37. 5 mg every 5 days until 150 mg for 3 weeks 2. Increase after 2 weeks to 225 mg. 3. Increase after 2 weeks to 300 mg
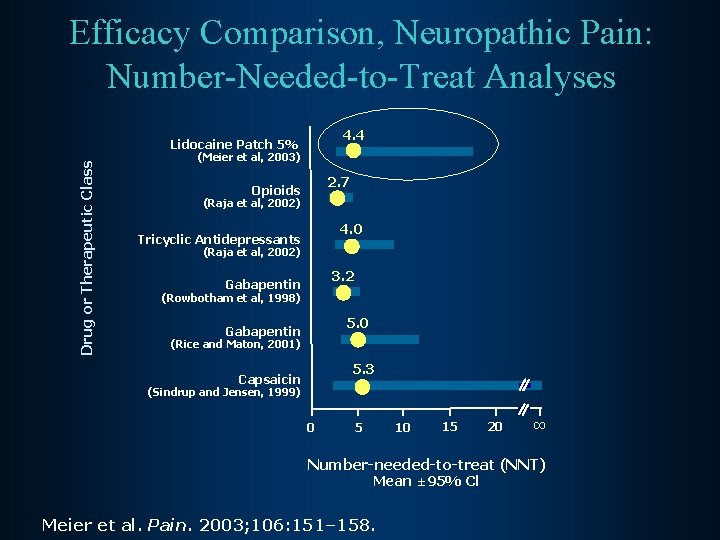
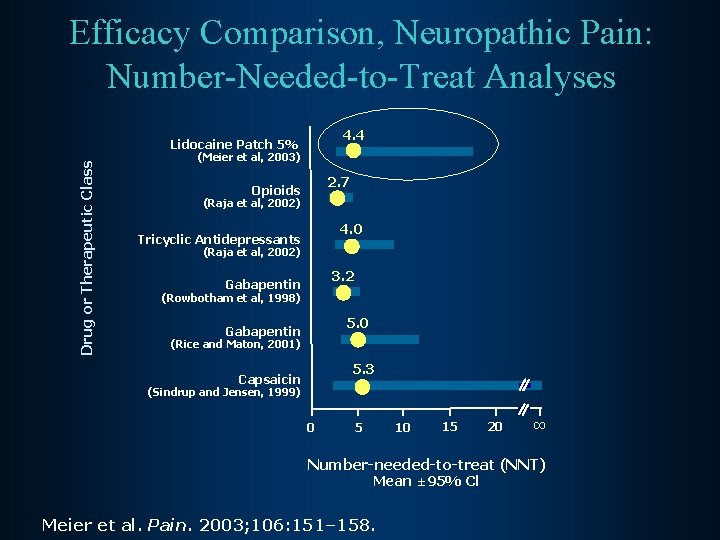
Efficacy Comparison, Neuropathic Pain: Number-Needed-to-Treat Analyses 4. 4 Drug or Therapeutic Class Lidocaine Patch 5% (Meier et al, 2003) 2. 7 Opioids (Raja et al, 2002) 4. 0 Tricyclic Antidepressants (Raja et al, 2002) 3. 2 Gabapentin (Rowbotham et al, 1998) 5. 0 Gabapentin (Rice and Maton, 2001) 5. 3 Capsaicin (Sindrup and Jensen, 1999) 0 10 5 15 20 ∞ Number-needed-to-treat (NNT) Mean ± 95% Cl Meier et al. Pain. 2003; 106: 151– 158.
Evidence for Disease Specificity in Efficacy Trials for NP Pain EFFICACY: SPECIFIC FOR DISEASE? - Postherpetic neuralgia - Spinal cord injury pain - Painful HIV neuropathy - Chemotherapy neuropathy - Diabetic neuropathy - Phantom tooth pain? GENERALIZED TO NEUROPATHIC MECHANISM?
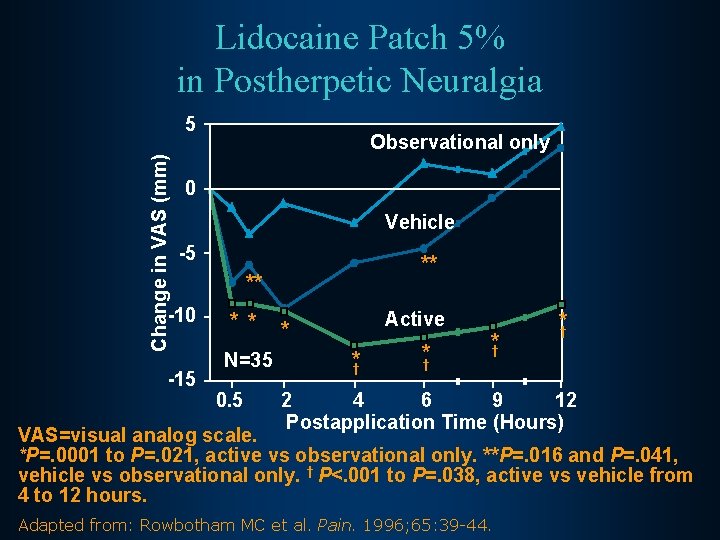
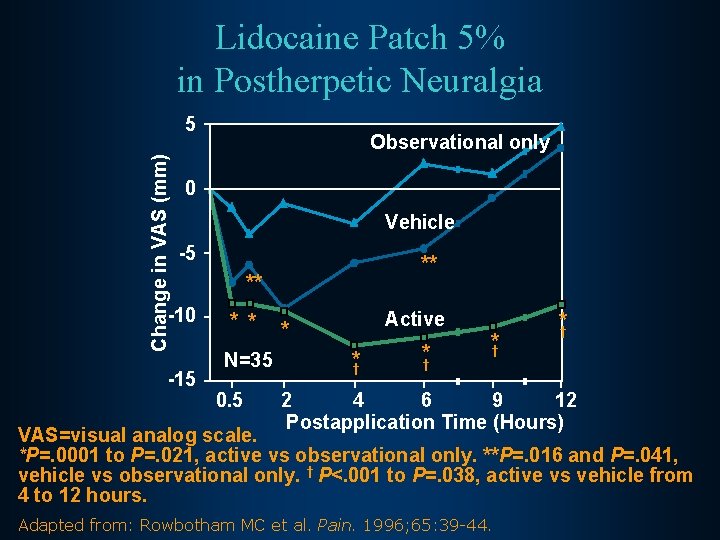
Lidocaine Patch 5% in Postherpetic Neuralgia Change in VAS (mm) 5 Observational only 0 Vehicle -5 -10 -15 ** ** * * N=35 0. 5 Active * *† * † *† *† 2 4 6 9 12 Postapplication Time (Hours) VAS=visual analog scale. *P=. 0001 to P=. 021, active vs observational only. **P=. 016 and P=. 041, vehicle vs observational only. † P<. 001 to P=. 038, active vs vehicle from 4 to 12 hours. Adapted from: Rowbotham MC et al. Pain. 1996; 65: 39 -44.
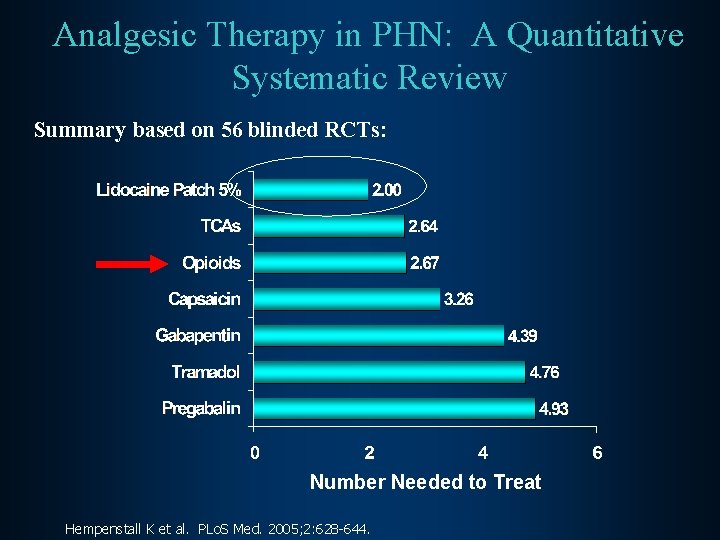
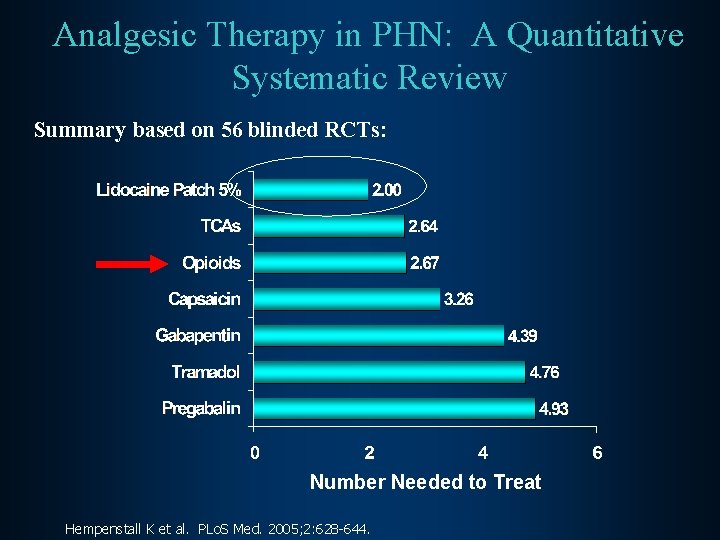
Analgesic Therapy in PHN: A Quantitative Systematic Review Summary based on 56 blinded RCTs: Number Needed to Treat Hempenstall K et al. PLo. S Med. 2005; 2: 628 -644.

Efficacy Comparison, Neuropathic Pain: Number-Needed-to-Treat Analyses 4. 4 Drug or Therapeutic Class Lidocaine Patch 5% (Meier et al, 2003) 2. 7 Opioids (Raja et al, 2002) 4. 0 Tricyclic Antidepressants (Raja et al, 2002) 3. 2 Gabapentin (Rowbotham et al, 1998) 5. 0 Gabapentin (Rice and Maton, 2001) 5. 3 Capsaicin (Sindrup and Jensen, 1999) 0 10 5 15 20 ∞ Number-needed-to-treat (NNT) Mean ± 95% Cl Meier et al. Pain. 2003; 106: 151– 158.
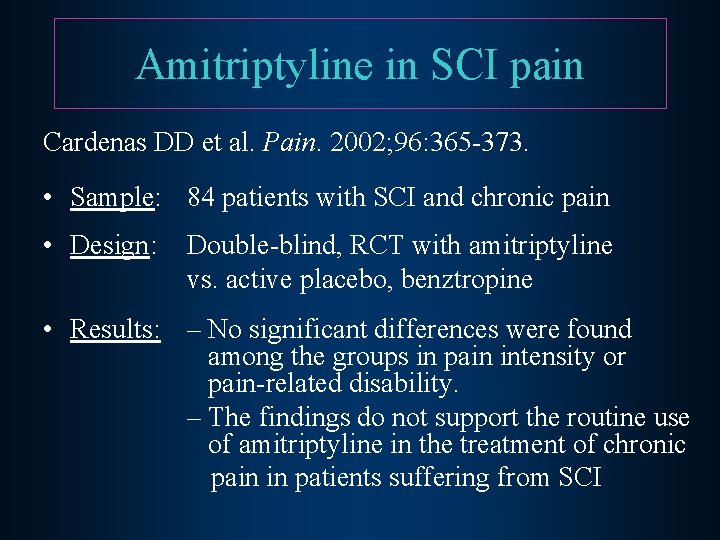
Amitriptyline in SCI pain Cardenas DD et al. Pain. 2002; 96: 365 -373. • Sample: 84 patients with SCI and chronic pain • Design: Double-blind, RCT with amitriptyline vs. active placebo, benztropine • Results: – No significant differences were found among the groups in pain intensity or pain-related disability. – The findings do not support the routine use of amitriptyline in the treatment of chronic pain in patients suffering from SCI
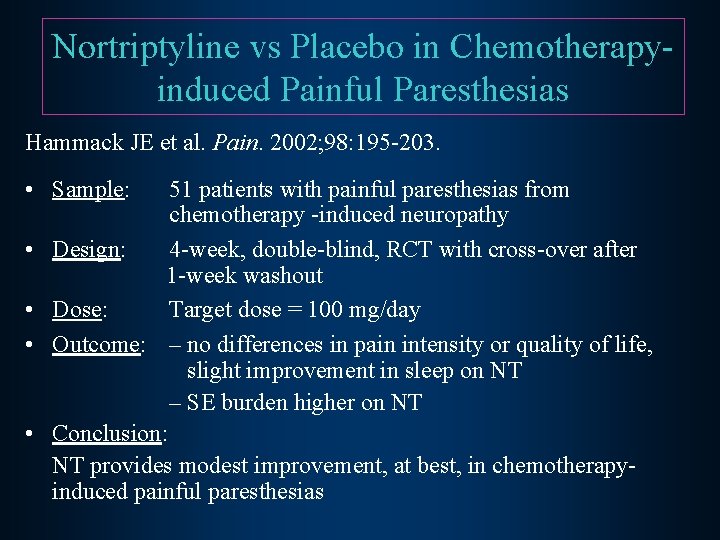
Nortriptyline vs Placebo in Chemotherapyinduced Painful Paresthesias Hammack JE et al. Pain. 2002; 98: 195 -203. • Sample: • • 51 patients with painful paresthesias from chemotherapy -induced neuropathy Design: 4 -week, double-blind, RCT with cross-over after 1 -week washout Dose: Target dose = 100 mg/day Outcome: – no differences in pain intensity or quality of life, slight improvement in sleep on NT – SE burden higher on NT Conclusion: NT provides modest improvement, at best, in chemotherapyinduced painful paresthesias
Chronic facial pain and depression Gallagher, R. M. , Marbach, J. , Raphael, K. , Dohrenwend, B. , Cloitre, M. : Is there co-morbidity between temporomandibular pain dysfunction syndrome and depression? : A pilot study. Clinical Journal of Pain, 7: 219 -225, 1991 Gallagher, R. M. , Marbach, J. , Raphael, K. , Handte, J. , Dohrenwend, B. : Seasonal Variation in chronic TMPDS Pain and Mood Intensity Pain, 61[1]: 113 -120, 1995. Dohrenwend, B. , Marbach, J. , Raphael, K. , Gallagher, R. M. : Why is depression co-morbid with chronic facial pain? A family study test of alternative hypotheses. Pain 83: 183 -192, 1999
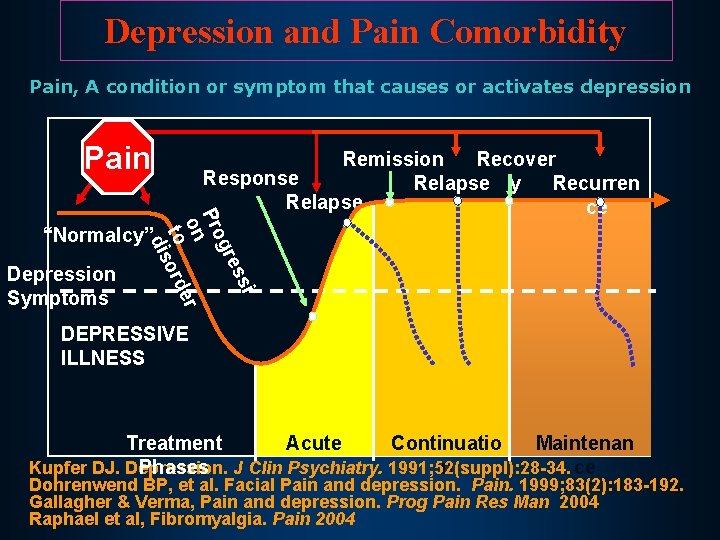
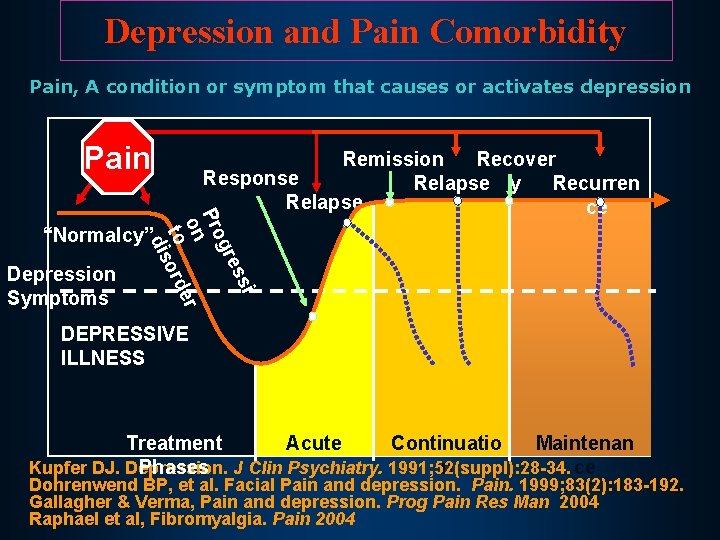
Depression and Pain Comorbidity Pain, A condition or symptom that causes or activates depression Pain i ss gre Pro on er to ord dis Remission Recover Response Relapse y Recurren Relapse ce “Normalcy” Depression Symptoms DEPRESSIVE ILLNESS Acute Continuatio Maintenan Treatment Kupfer DJ. Depression. n ce Phases J Clin Psychiatry. 1991; 52(suppl): 28 -34. Dohrenwend BP, et al. Facial Pain and depression. Pain. 1999; 83(2): 183 -192. Gallagher & Verma, Pain and depression. Prog Pain Res Man 2004 Raphael et al, Fibromyalgia. Pain 2004
CHOOSING MEDICATION Expect partial effects: use multiple agents with different mechanisms: – from different classes – from the same class

Target – keeping pain below 5 to enable quality of life Just Noticeable No pain 0 Mild, in background 1 2 3 Moderate Bothersome 4 5 Severe Can’t function 6 7 Excruciating, ER time 8 9 10 Burning at the stake !! Worst possible pain • Improvement can be monitored • Gives clinician and patient a consistent understandable measure with intra-rater reliability that facilitates discussion regarding: changes in pain, response to treatment • Reduction of 2 points is clinically meaningful Adapted from Farrar JT et al. Pain. 2001; 94: 149 -158.

Algorithm for Medication Selection in Chronic Pain With and Without Comorbid Depression Nociceptive pain Evaluate risks NSAIDs, Cox-IIs, opioids, lidocaine p. ? doxepin cr. ? Neuropathic Secondary pain Secondary sleep disturbance Persists after adequate analgesia depressio n Pain condition + depression Persists after adequate analgesia Evaluate risks SSRI trial Evaluate risks Antihistamine, Trazodone zolpidem, Low-dose etc. TCA Lidocaine patch; gabapentin & other AED (Ca+ & Na+ channels); alpha 2 agonists (tizanidine, clonidine); opioids SNRIs: venlafaxine, duloxetine Titrate TCAs (Na+ channels and SNRI) : desipramine, nortriptyline, Adapted from Gallagher RM, Verma S. Semin Clin Neurosurgery. 2004. This information concerns uses that have not been approved by the US FDA. Primary D.
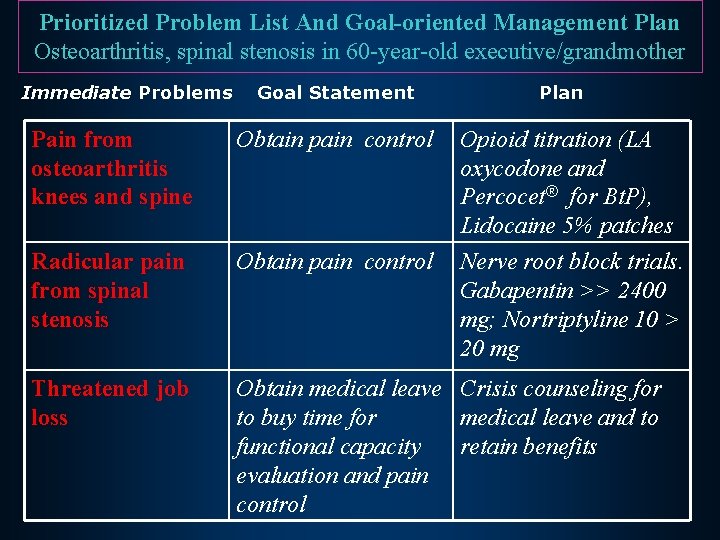
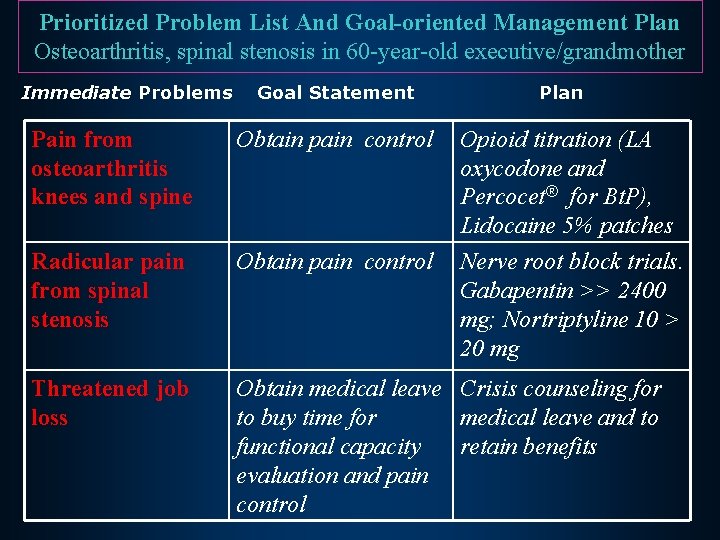
Prioritized Problem List And Goal-oriented Management Plan Osteoarthritis, spinal stenosis in 60 -year-old executive/grandmother Immediate Problems Goal Statement Plan Pain from osteoarthritis knees and spine Obtain pain control Opioid titration (LA oxycodone and Percocet® for Bt. P), Lidocaine 5% patches Nerve root block trials. Gabapentin >> 2400 mg; Nortriptyline 10 > 20 mg Radicular pain from spinal stenosis Obtain pain control Threatened job loss Obtain medical leave Crisis counseling for to buy time for medical leave and to functional capacity retain benefits evaluation and pain control
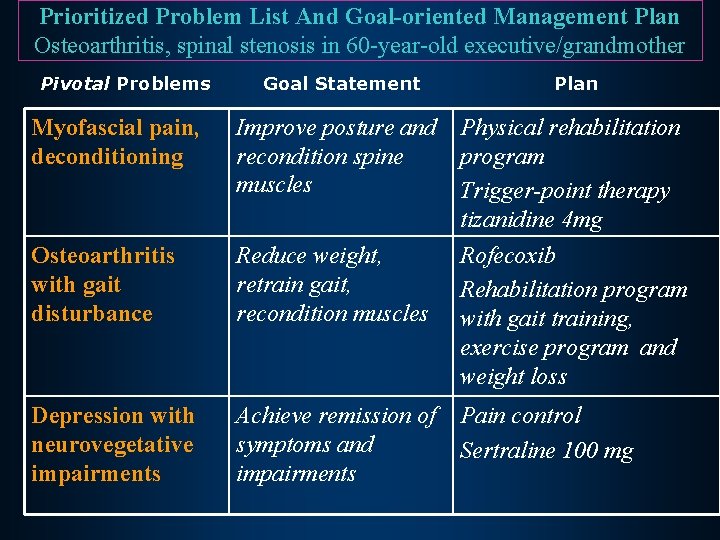
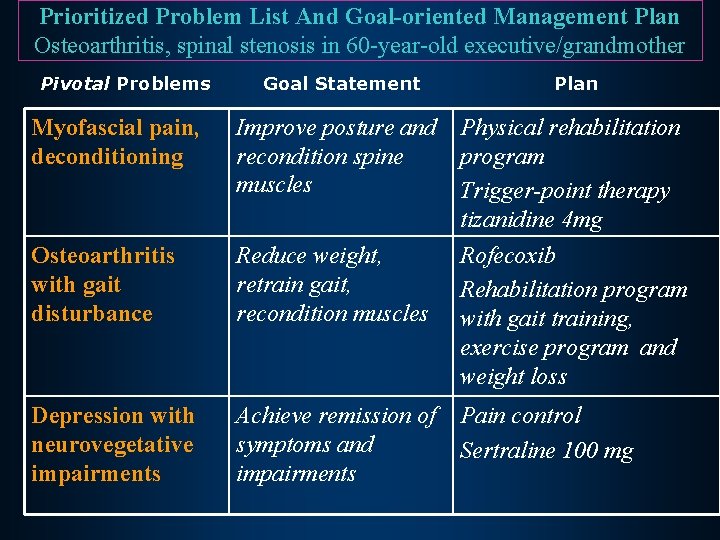
Prioritized Problem List And Goal-oriented Management Plan Osteoarthritis, spinal stenosis in 60 -year-old executive/grandmother Pivotal Problems Goal Statement Plan Myofascial pain, deconditioning Improve posture and Physical rehabilitation recondition spine program muscles Trigger-point therapy tizanidine 4 mg Osteoarthritis with gait disturbance Reduce weight, retrain gait, recondition muscles Depression with neurovegetative impairments Achieve remission of Pain control symptoms and Sertraline 100 mg impairments Rofecoxib Rehabilitation program with gait training, exercise program and weight loss
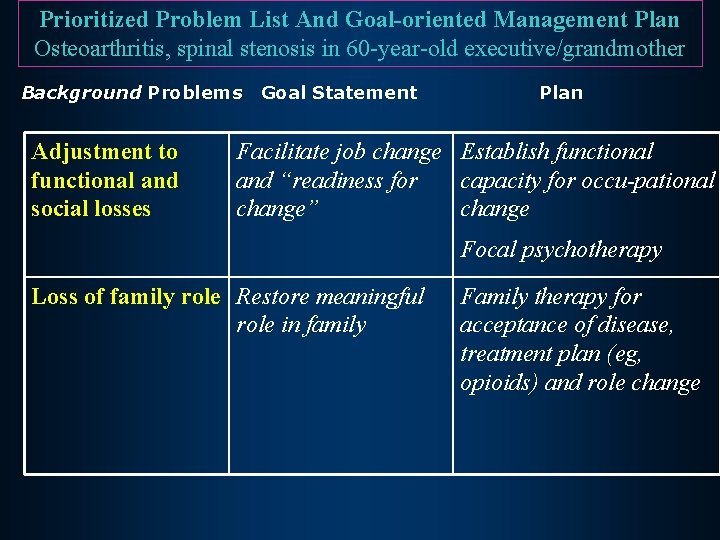
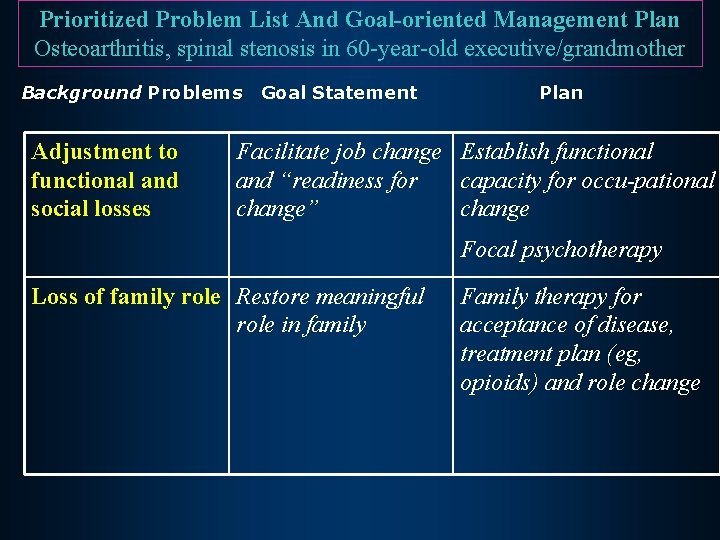
Prioritized Problem List And Goal-oriented Management Plan Osteoarthritis, spinal stenosis in 60 -year-old executive/grandmother Background Problems Adjustment to functional and social losses Goal Statement Plan Facilitate job change Establish functional and “readiness for capacity for occu-pational change” change Focal psychotherapy Loss of family role Restore meaningful role in family Family therapy for acceptance of disease, treatment plan (eg, opioids) and role change
Final Thoughts • A medication that is effective in one neuropathic pain disorder may not be effective in others. But it may be, so try it. • Mechanisms of neuropathic pain may differ in different diseases and within diseases, accounting for variability in study results. • Be aware of drug interactions in patients with several chronic conditions.

Final Thoughts Success in rational polypharmacy requires: • Establish appropriate goals—pain relief and quality of life • Know mechanism and disease-specific data related to efficacy • Present recommendations with confidence based upon evidence, not just charisma • Establish patient and doctor responsibilities
Final Thoughts Success in rational polypharmacy requires: • Run sequential clinical trials of medications based on efficacy, SE burden and toxicity, comorbidities, ease of use, and patient adherence. • If partial effects, maintain on minimal effective dose while pursuing additional medication trials, one at a time. • Look for additive benefit of several medications, targeting different mechanisms, to obtain control of pain to improve quality of life.