PNS For distribution spinal nerves n n Since
PNS For distribution
spinal nerves n n Since there are 8 cervical spinal nerves but only 7 cervical vertebra, cervical spinal nerves exit above the vertebra with the corresponding number. That is, the 1 st cervical spinal nerve exits above the atlas, the C 7 spinal nerve exits above the C 7 vertebra, and the C 8 spinal nerve exits above the T 1 vertebra. The other spinal nerves exit below the corresponding vertebra.
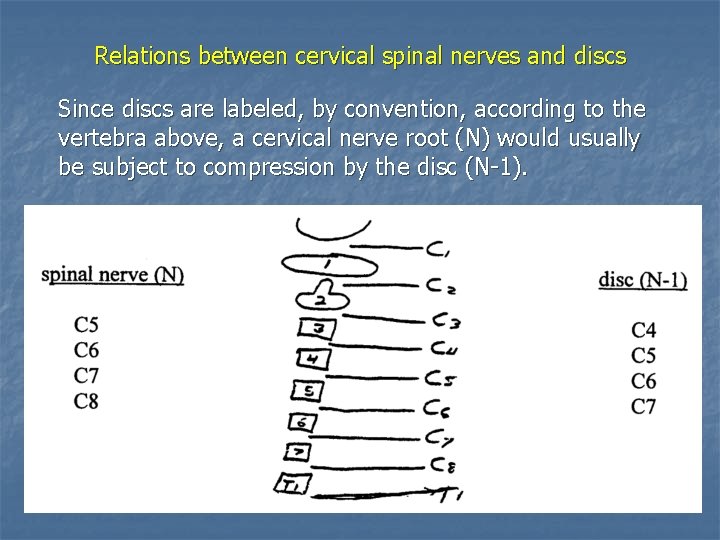
Relations between cervical spinal nerves and discs Since discs are labeled, by convention, according to the vertebra above, a cervical nerve root (N) would usually be subject to compression by the disc (N-1).
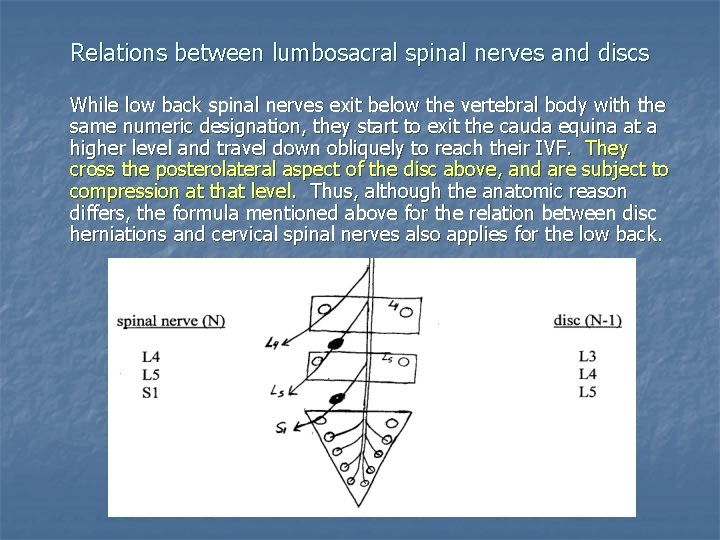
Relations between lumbosacral spinal nerves and discs While low back spinal nerves exit below the vertebral body with the same numeric designation, they start to exit the cauda equina at a higher level and travel down obliquely to reach their IVF. They cross the posterolateral aspect of the disc above, and are subject to compression at that level. Thus, although the anatomic reason differs, the formula mentioned above for the relation between disc herniations and cervical spinal nerves also applies for the low back.
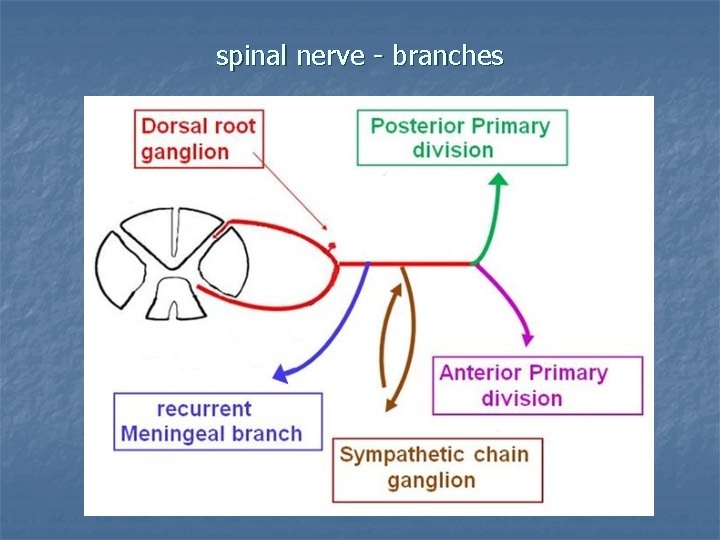
spinal nerve - branches
radiculopathy n Spinal nerve disorder is known as “radiculopathy”. n Common causes of radiculopathy include: 1. 2. Disc herniation IVF stenosis (secondary to vertebral DJD) § Other causes include tumors, fracture, infections.
radiculopathy Lumbosacral radiculopathy is more common than cervical radiculopathy. The L 5 & S 1 spinal nerves are most commonly affected (“sciatica”). L 4 radiculopathy is less common, and radiculopathy of the upper lumbar nerve roots is significantly less common. When cervical radiculopathy occurs, the C 6 & C 7 spinal nerves are most commonly affected, followed by C 5 and C 8. Thoracic radiculopathy is much less common (herpes zoster – “shingles” - is an important cause).
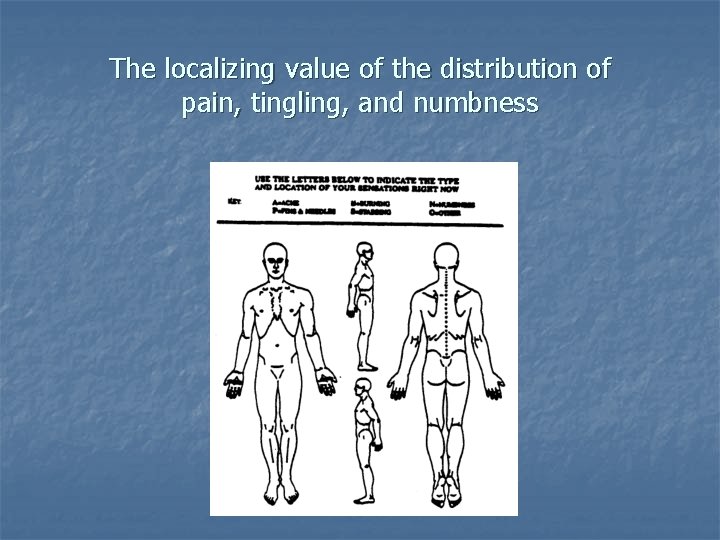
The localizing value of the distribution of pain, tingling, and numbness
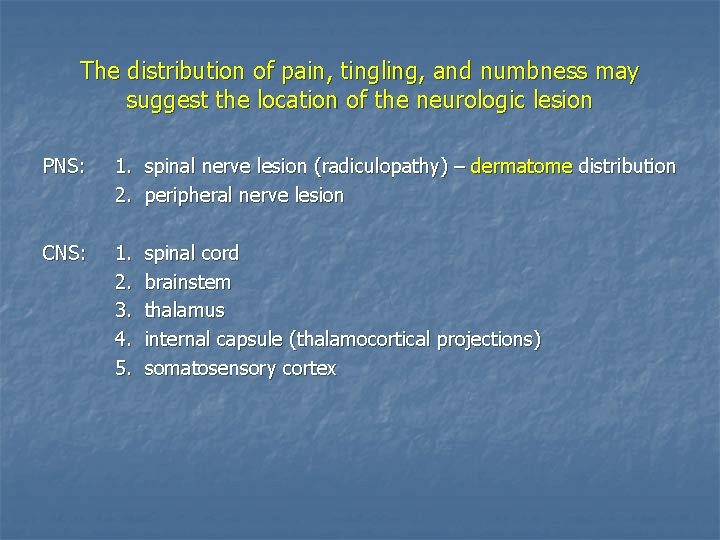
The distribution of pain, tingling, and numbness may suggest the location of the neurologic lesion PNS: 1. spinal nerve lesion (radiculopathy) – dermatome distribution 2. peripheral nerve lesion CNS: 1. 2. 3. 4. 5. spinal cord brainstem thalamus internal capsule (thalamocortical projections) somatosensory cortex
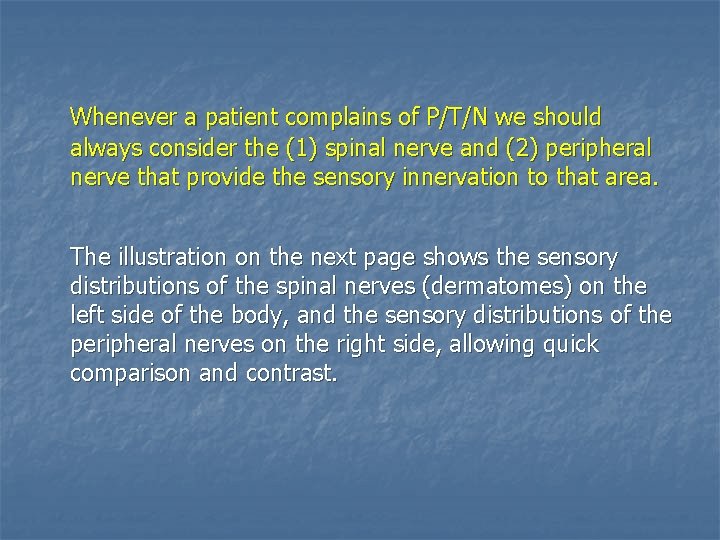
Whenever a patient complains of P/T/N we should always consider the (1) spinal nerve and (2) peripheral nerve that provide the sensory innervation to that area. The illustration on the next page shows the sensory distributions of the spinal nerves (dermatomes) on the left side of the body, and the sensory distributions of the peripheral nerves on the right side, allowing quick comparison and contrast.

Cutaneous innervation: spinal nerve (dermatome) vs. peripheral nerve distributions
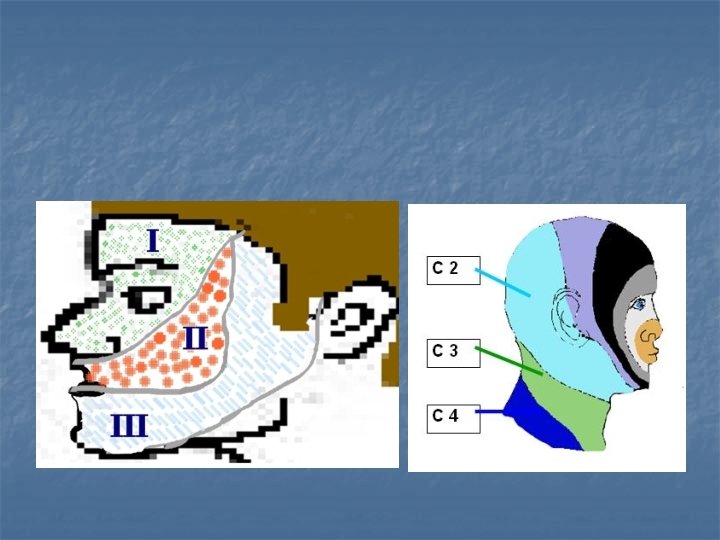

Spinal nerve sensory distributions (“dermatomes”)
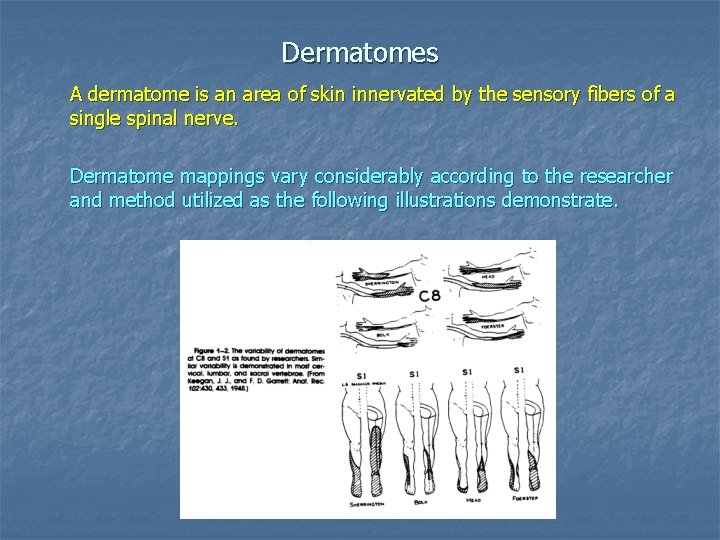
Dermatomes A dermatome is an area of skin innervated by the sensory fibers of a single spinal nerve. Dermatome mappings vary considerably according to the researcher and method utilized as the following illustrations demonstrate.
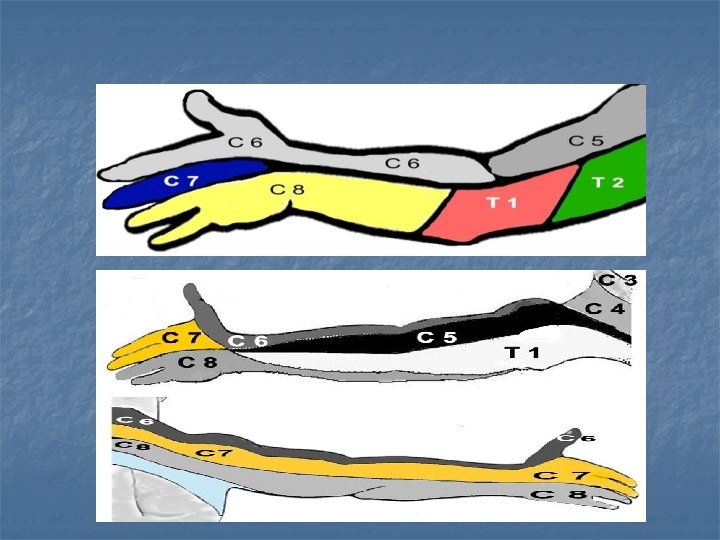
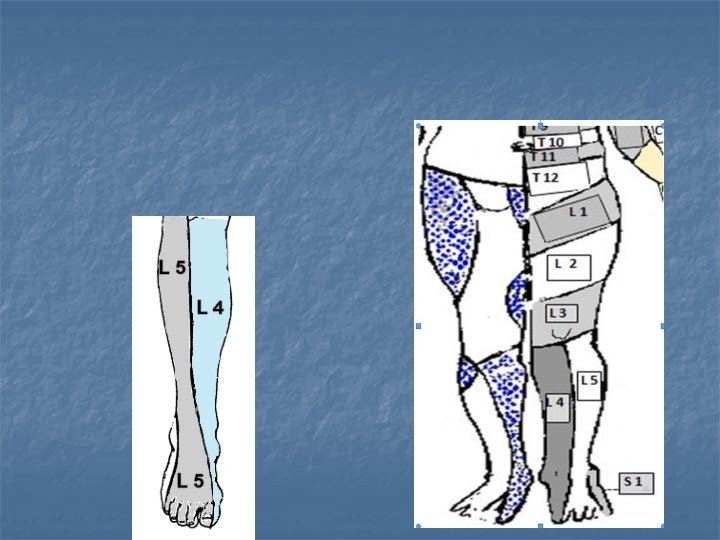
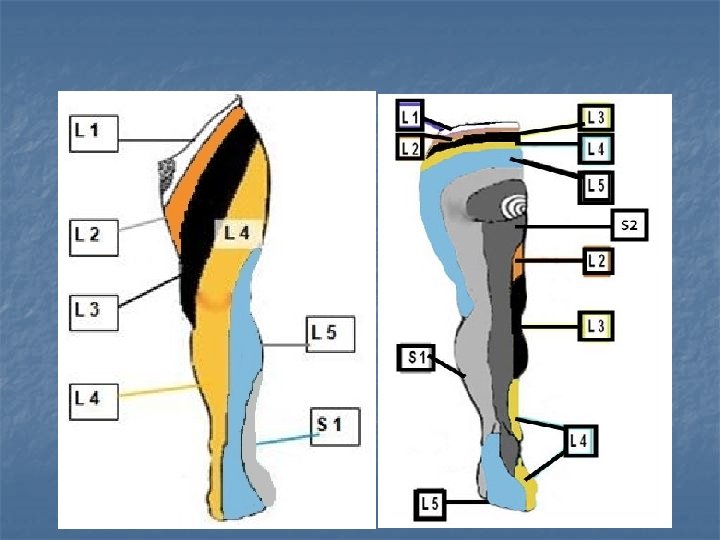
The two most commonly referenced dermatomal maps are illustrated on the next several pages (Keegan & Garrett, Anat. Rec. , 1943; Haymaker & Woodhall, Peripheral Nerve Injuries, 2 nd ed. , 1953). At first glance, one is struck by the differences between the maps, especially in the arms and thighs. However, after some review you will note they agree on many important points: Upper extremity: 1. the lateral forearm and thumb are innervated by C 6 2. the middle finger is innervated by C 7 3. the ring finger & pinky are innervated by C 8 Lower extremity: 1. the medial shin and medial foot are innervated by L 4 2. the lateral shin, top of foot, and big toe are innervated by L 5 3. the lateral foot and little toe are innervated by S 1
Dermatomes of the upper extremity - similarities At first glance, one is struck by the differences between the dermatome maps of the upper extremity. However, after some review you will note they agree on many important points: 1. the lateral forearm and thumb are innervated by C 6 2. the middle finger is innervated by C 7 3. the ring finger & pinky are innervated by C 8
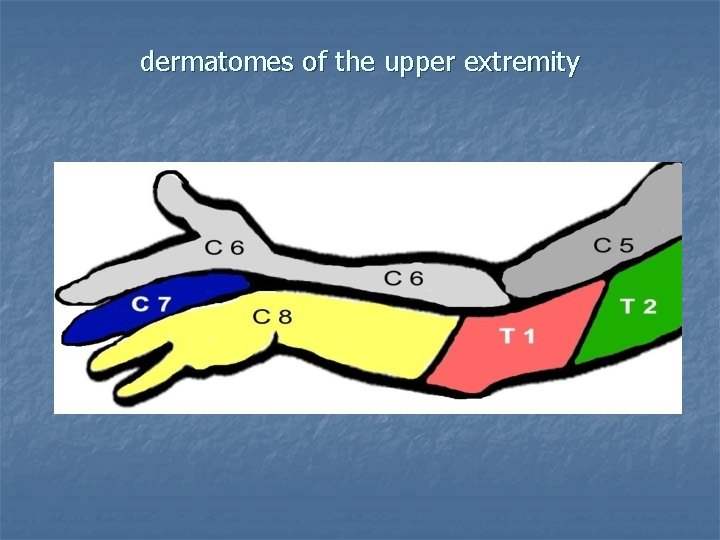
dermatomes of the upper extremity
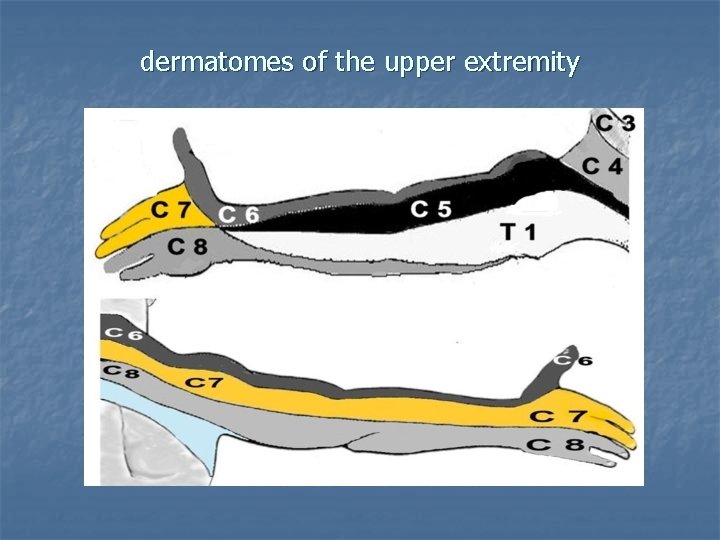
dermatomes of the upper extremity
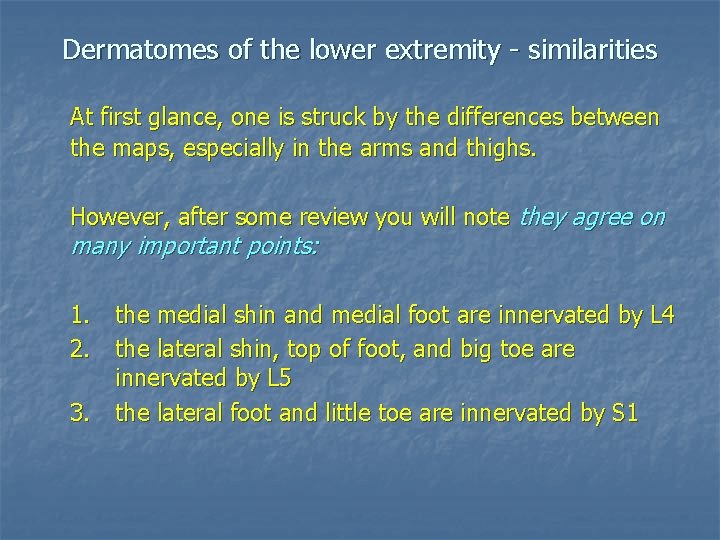
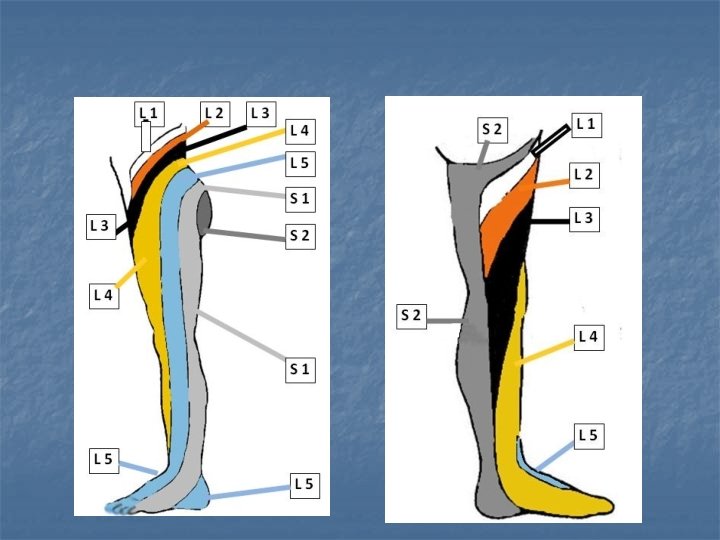
Dermatomes of the lower extremity - similarities At first glance, one is struck by the differences between the maps, especially in the arms and thighs. However, after some review you will note they agree on many important points: 1. the medial shin and medial foot are innervated by L 4 2. the lateral shin, top of foot, and big toe are innervated by L 5 3. the lateral foot and little toe are innervated by S 1
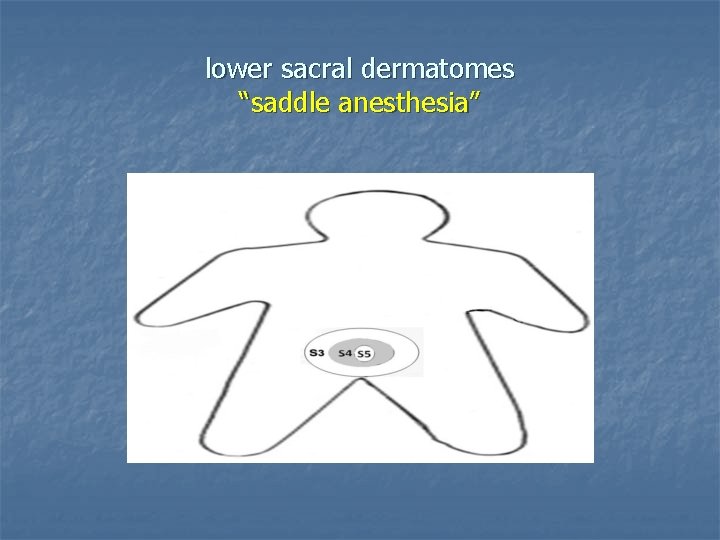
lower sacral dermatomes “saddle anesthesia”
Spinal cord & cauda equina Fig. 2. 8
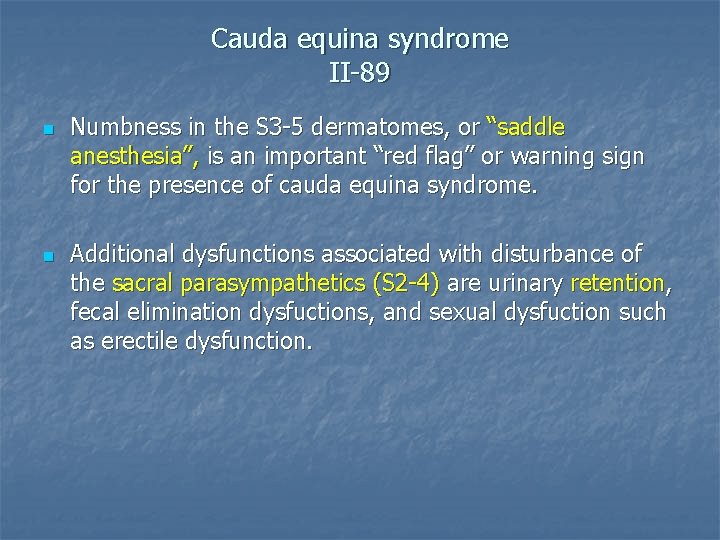
Cauda equina syndrome II-89 n n Numbness in the S 3 -5 dermatomes, or “saddle anesthesia”, is an important “red flag” or warning sign for the presence of cauda equina syndrome. Additional dysfunctions associated with disturbance of the sacral parasympathetics (S 2 -4) are urinary retention, fecal elimination dysfuctions, and sexual dysfuction such as erectile dysfunction.
Peripheral nerves
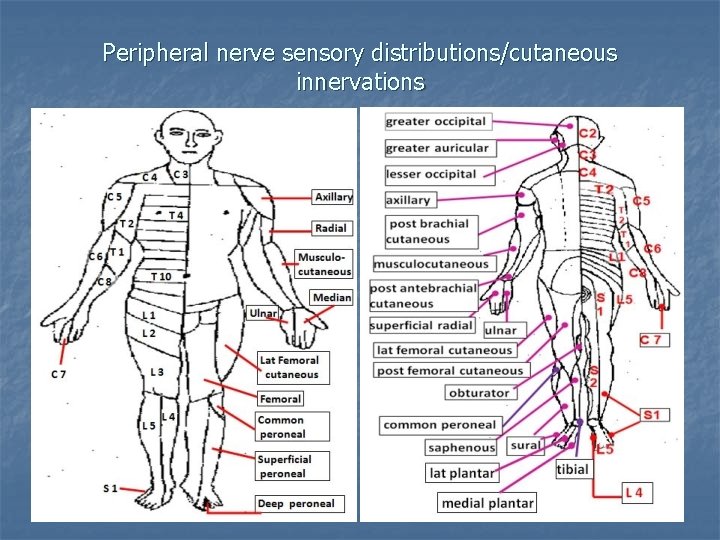
Peripheral nerve sensory distributions/cutaneous innervations
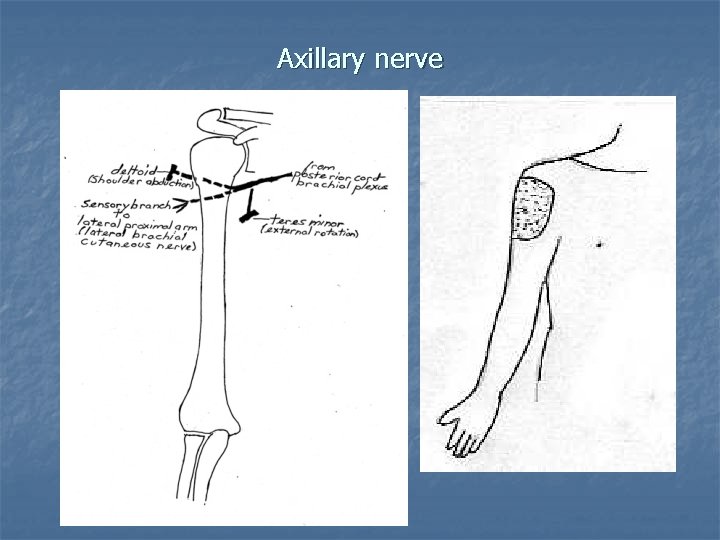
Axillary nerve
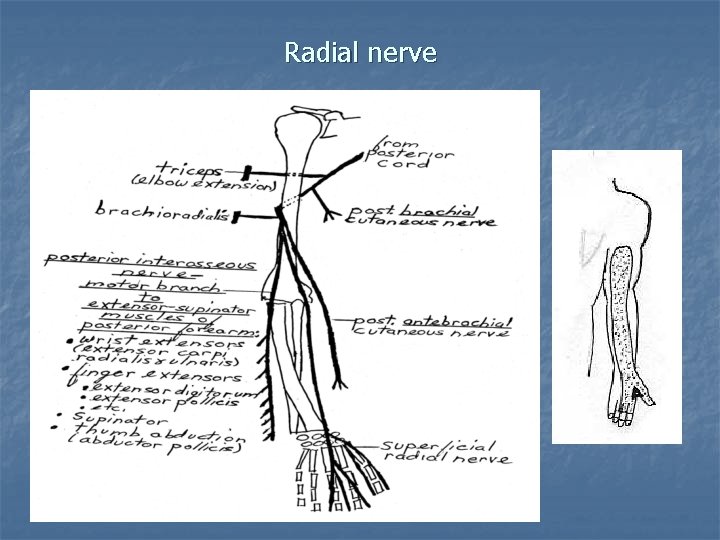
Radial nerve
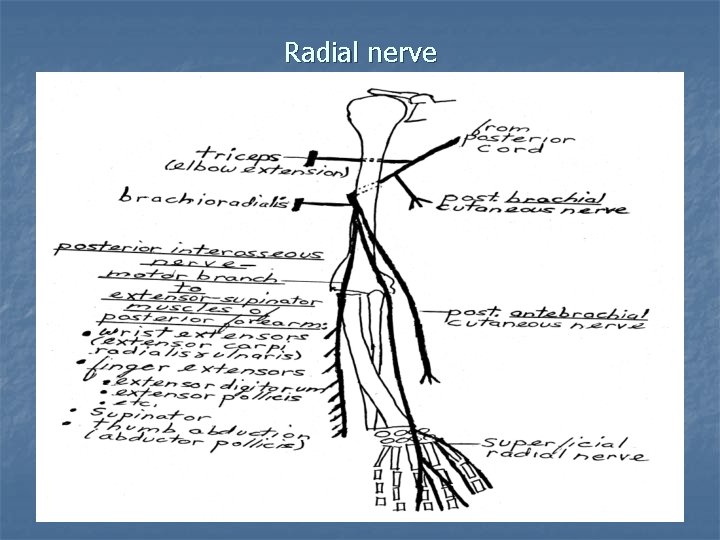
Radial nerve
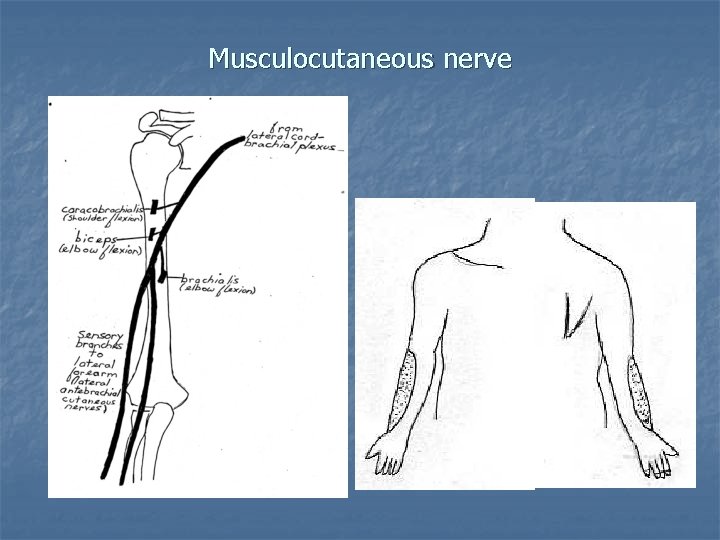
Musculocutaneous nerve
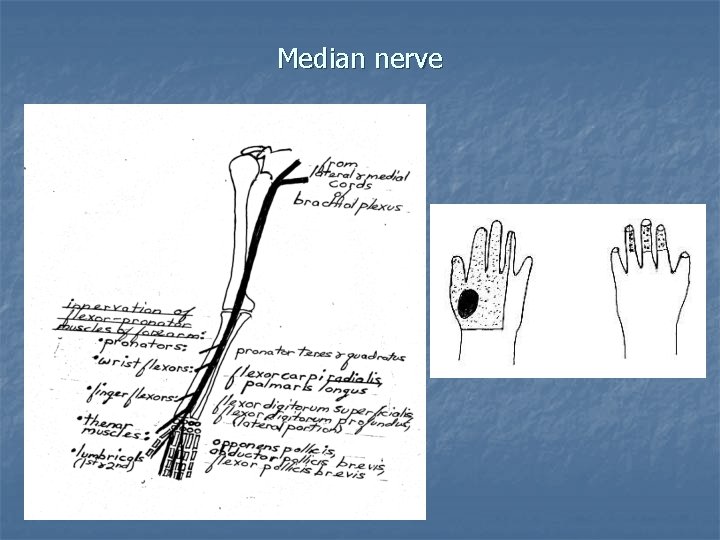
Median nerve
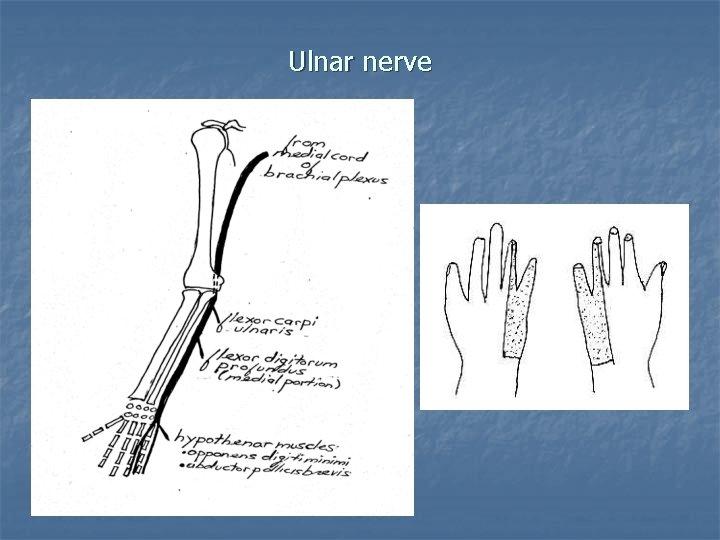
Ulnar nerve
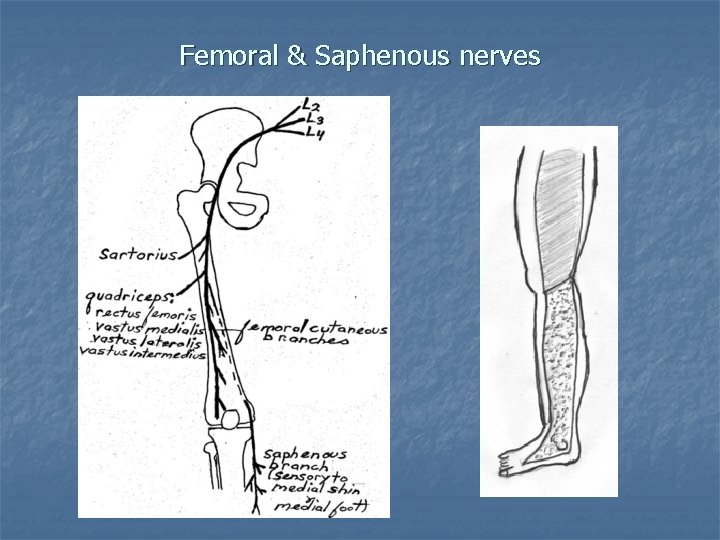
Femoral & Saphenous nerves
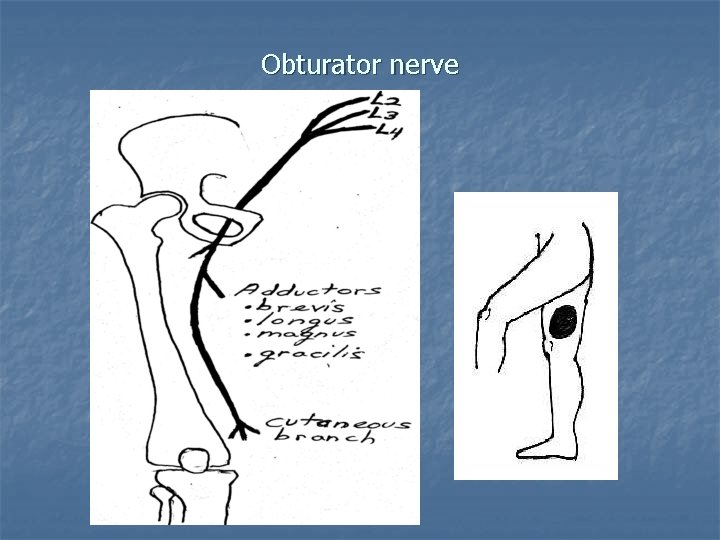
Obturator nerve
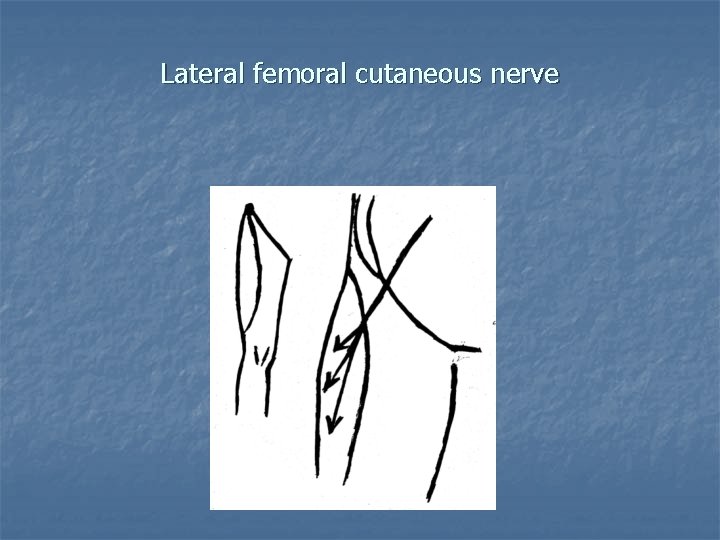
Lateral femoral cutaneous nerve
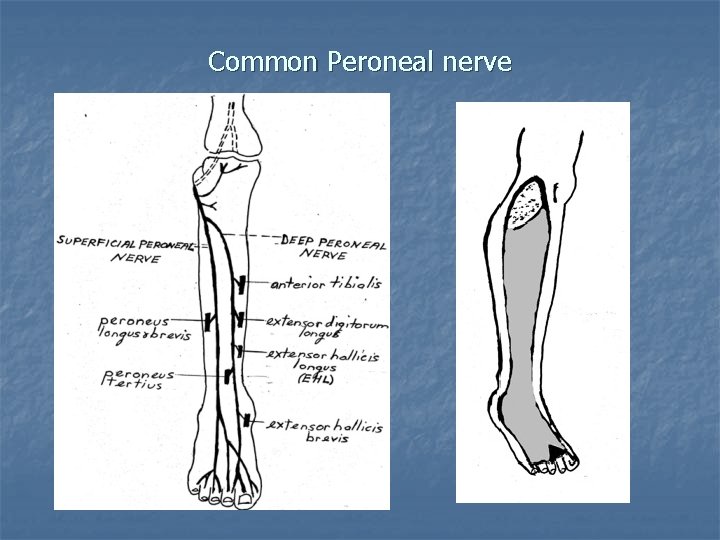
Common Peroneal nerve
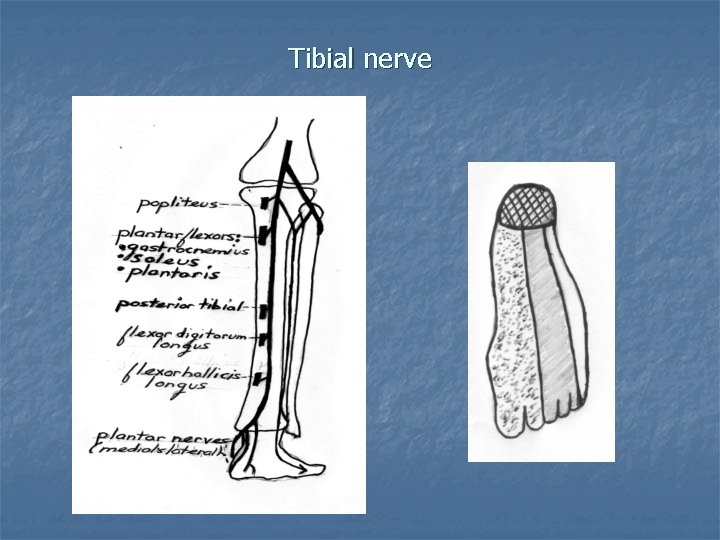
Tibial nerve
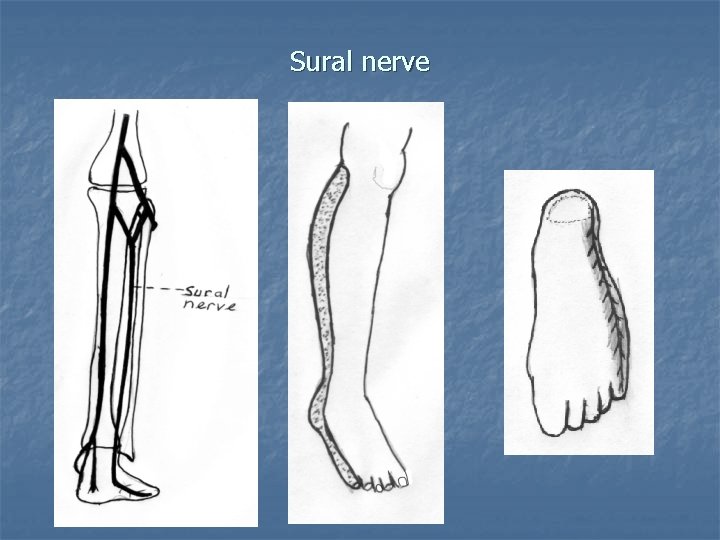
Sural nerve
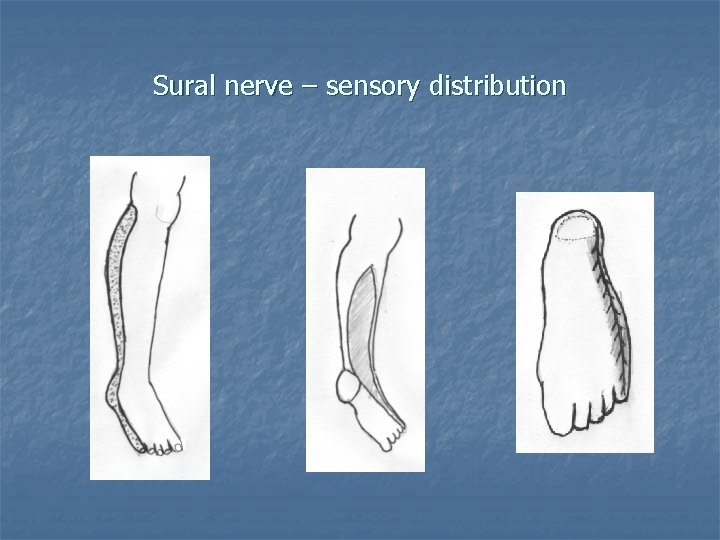
Sural nerve – sensory distribution
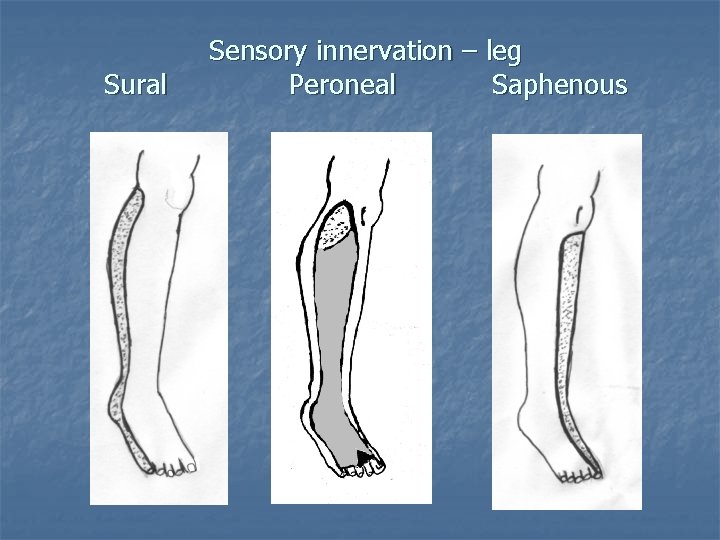
Sural Sensory innervation – leg Peroneal Saphenous
- Slides: 42