Plasmodium species that infect humans Four plasmodium species
- Slides: 13
Plasmodium species that infect humans: Four plasmodium species that were considered responsible for malaria disease in humans: -Plasmodium vivax: It is The predominant malarial parasite in most parts of the world. Producing benign tertian malaria. -Plasmodium ovale: it seems to be rather widely distributed in tropical African. It causes Bennign tertian malaria. -Plasmodium malariae: Occurring primarily in those subtropical and temperate areas. Producing quartan malaria. -Plasmodium falciparum: Falciparurm malaria is almost entirely confined to the tropics and subtropics. It causes malignant subtertian malaria.
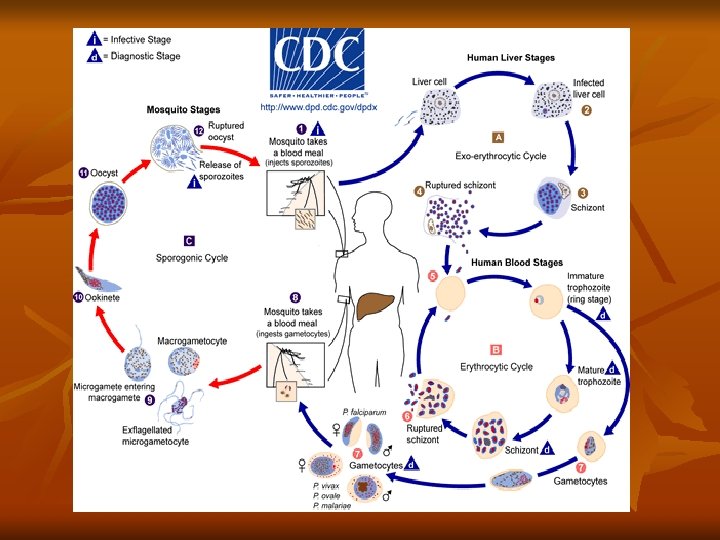
Mode of infection 1 -By bite of female Anopheles mosquito: Infective stage is the sporozoite. 2 -Blood transfusion: Infective stage is the schizont or merozoite. 3 -Congenital: Infective stage is the merozoite. Life cycle of Plasmodium: The life cycle of the parasite is completed in two different hosts. 1 -Asexual cycle "Schizogony" occurs in man. a) Pre- erythrocytic and exo- erythrocytic cycle in liver cells. b) Blood cycle or Erythrocytic cycle which takes place inside the RBCs. 2 -Sexual cycle, "Gametogony" and "Sporogony" occur in the female Anopheles mosquito. Asexual cycle: (Schizogony) ) Pre-erythrocytic (exo-erythrocytic cycles): Infection of malaria done when infected female Anopheles bites a man, it injects the sporozoites into his blood (slender motile organisms).
Sporozoites reach the liver cells to start a pre-erythrocytic cycle where they multiply producing schizonts, which lasts about 8 days. Rupture of schizonts release merozoites most of them invade quickly R. B. Cs. to begin the erythrocytic cycle. In P. vivax and P. ovale some merozoites re-invade liver cells and differentiate into nonsexual hypnozoites that remain dormant for weeks, or even years. The activated hypnozoites undergo exo-erythrocytic schizogony, forming a wave of merozoites that cause a relapse. b)Erythrocytic cycle: Merozoites invade the red blood cells, where it grows and reproduces on the expense of the hemoglobin of the infected red blood cells. The developmental stages inside the RB. Cs. are: - Ring stage. - Trophozoite. - Schizont. - Gametocyte.
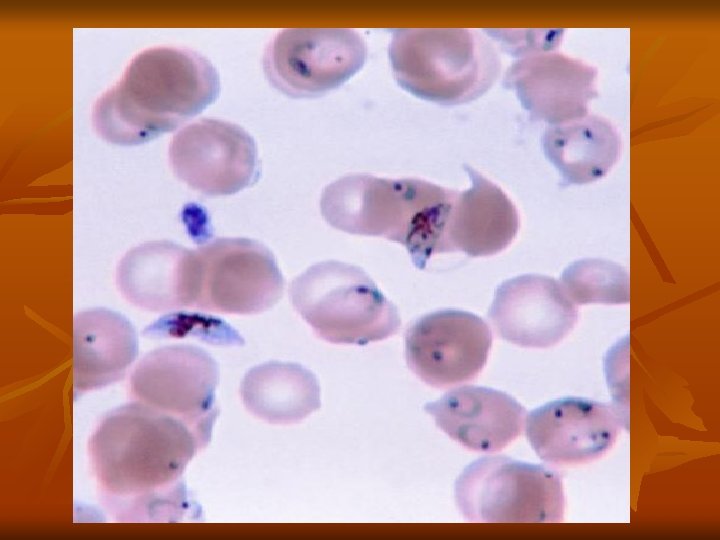
1 -Ring stage: A small rounded mass of cytoplasm with a single nucleus, and then a small vacuole develops inside the cytoplasm pushing the nucleus to one side, giving the parasite a ring shape. 2 -Trophozoite stage: The parasite shows a very active amoeboid movement with pseudopodia. Infected red cells are paler in color and in P. vivax they become larger. Pigment granules appear in the cytoplasm of the parasite known as hemozoin (malarial pigment). 3 -Schizont stage: Develop binary fission resulting in the formation of a large number of daughter nuclei, followed by division of the cytoplasm that collects around each nuclei leading to the formation of merozoites. Pigment granules tend to collect in the center of schizont. Shcizogony take a period of 48 h in P. vivax, P. ovale, 36 -48 h in P. falciparum, and 72 h in P. malariae.
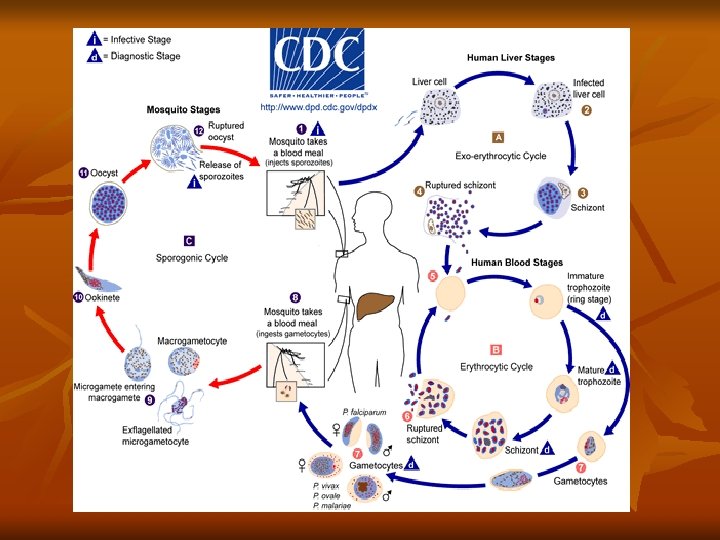
Infected red blood cell ruptures releasing merozoites and hemozoin pigment, which is the cause of the malarial paroxysm. Merozoites attack a new red blood cells and the cycle is repeated. 3 -Gametocyte stage: Some of the merozoites give rise to form gametocytes, male microgametocytes and female macrogametocytes. (2) Sexual cycle (Gametogony and Sporogony): 1 -Female Anopheles mosquito sucks up blood from a malarial patient. In the stomach of mosquito, gametes (Gametogony). Male and female gametocyte develops to a microgamete, and a macrogamete. Fertilization takes place between the male and female gametes resulting "zygote“ , which develop to ookinete then "oocyst". 2 -Oocyst increases in size, nucleus divides into a large number of nuclei to give sporozoites which migrate to the salivary glands of the mosquito (Sporogony). Infection to man is by the saliva containing sporozoite injected by the mosquito during biting to prevent blood coagulation.
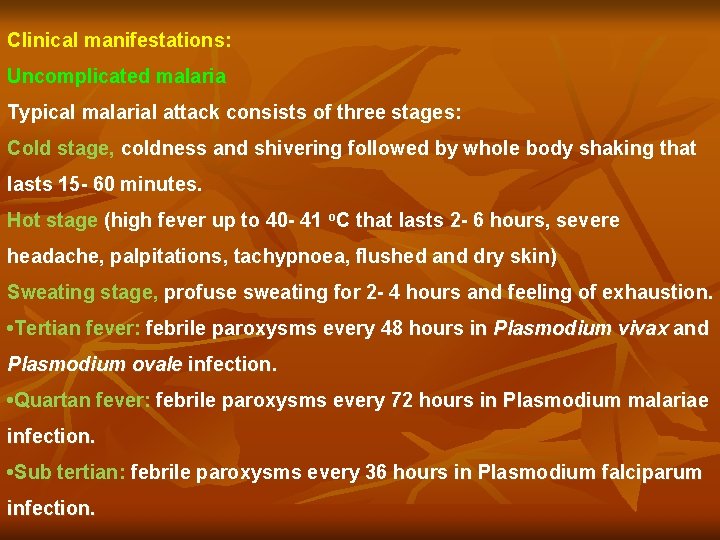
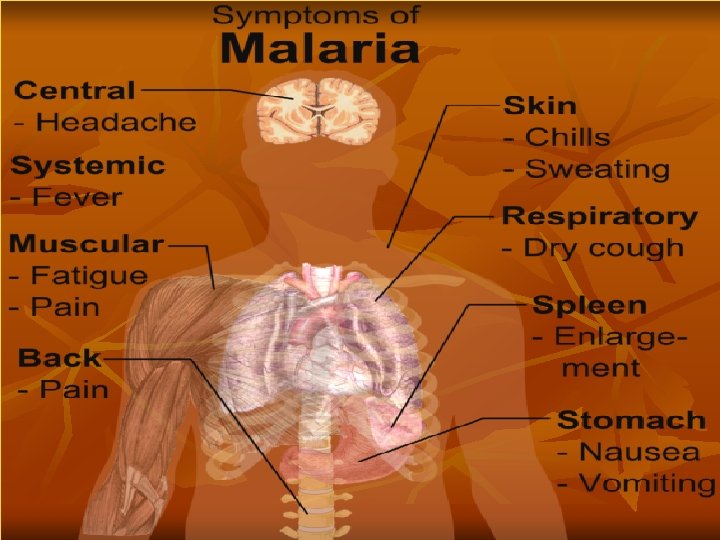
Clinical manifestations: Uncomplicated malaria Typical malarial attack consists of three stages: Cold stage, coldness and shivering followed by whole body shaking that lasts 15 - 60 minutes. Hot stage (high fever up to 40 - 41 o. C that lasts 2 - 6 hours, severe headache, palpitations, tachypnoea, flushed and dry skin) Sweating stage, profuse sweating for 2 - 4 hours and feeling of exhaustion. • Tertian fever: febrile paroxysms every 48 hours in Plasmodium vivax and Plasmodium ovale infection. • Quartan fever: febrile paroxysms every 72 hours in Plasmodium malariae infection. • Sub tertian: febrile paroxysms every 36 hours in Plasmodium falciparum infection.
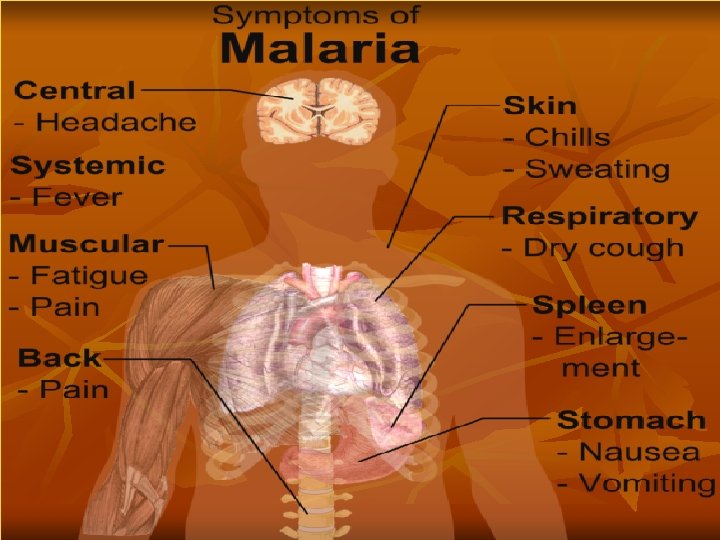
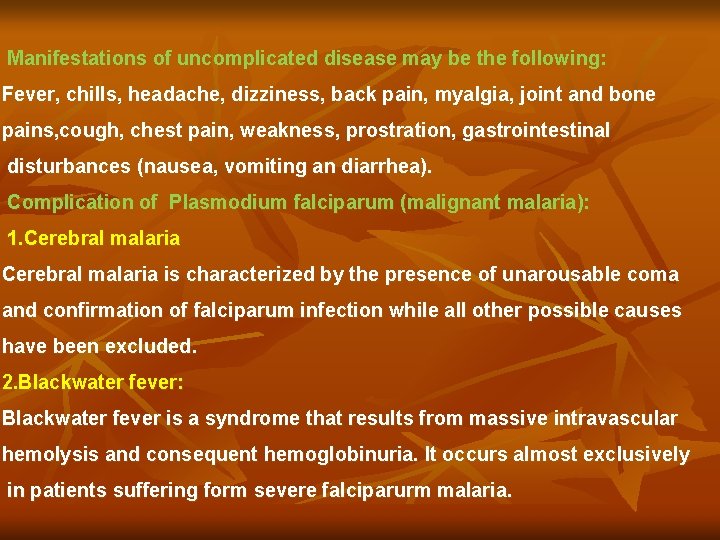
Manifestations of uncomplicated disease may be the following: Fever, chills, headache, dizziness, back pain, myalgia, joint and bone pains, cough, chest pain, weakness, prostration, gastrointestinal disturbances (nausea, vomiting an diarrhea). Complication of Plasmodium falciparum (malignant malaria): 1. Cerebral malaria is characterized by the presence of unarousable coma and confirmation of falciparum infection while all other possible causes have been excluded. 2. Blackwater fever: Blackwater fever is a syndrome that results from massive intravascular hemolysis and consequent hemoglobinuria. It occurs almost exclusively in patients suffering form severe falciparurm malaria.
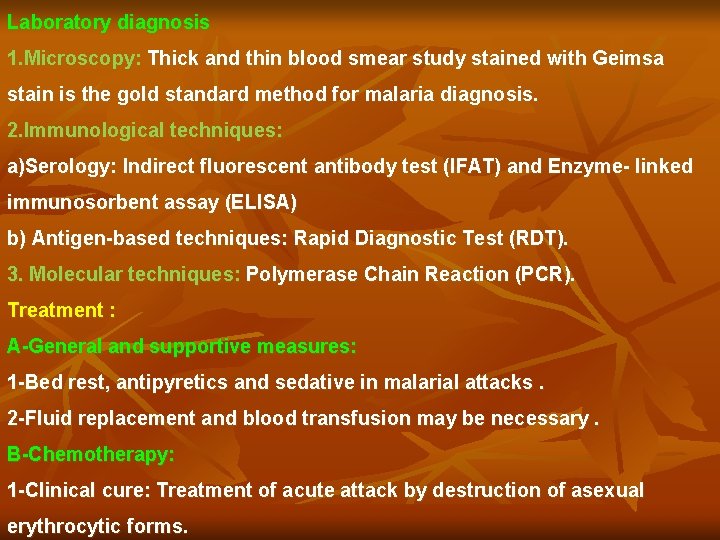
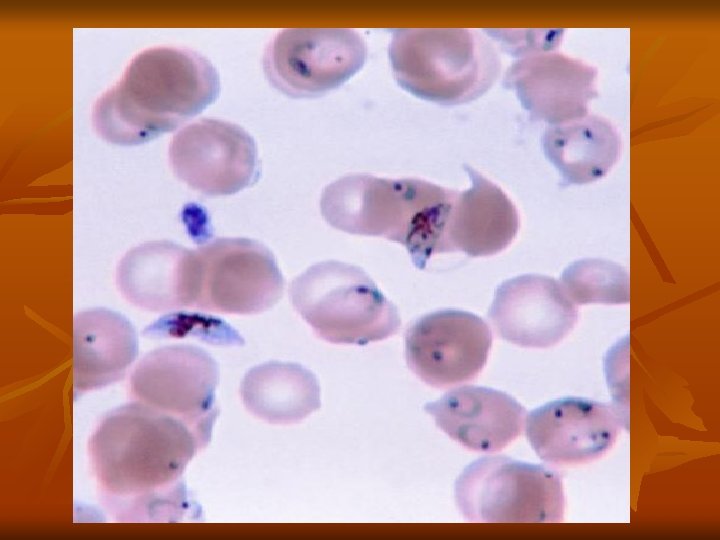
Laboratory diagnosis 1. Microscopy: Thick and thin blood smear study stained with Geimsa stain is the gold standard method for malaria diagnosis. 2. Immunological techniques: a)Serology: Indirect fluorescent antibody test (IFAT) and Enzyme- linked immunosorbent assay (ELISA) b) Antigen-based techniques: Rapid Diagnostic Test (RDT). 3. Molecular techniques: Polymerase Chain Reaction (PCR). Treatment : A-General and supportive measures: 1 -Bed rest, antipyretics and sedative in malarial attacks. 2 -Fluid replacement and blood transfusion may be necessary. B-Chemotherapy: 1 -Clinical cure: Treatment of acute attack by destruction of asexual erythrocytic forms.
For all plasmodia except resistant P. falciparum we use Chloroquine phosphate and for P. falciparum we use Quinine sulphate + combination of pyrimethamine / sulphadoxine. 2 -Radical cure: Prevention of relapses in P. vivax and oval by destruction of the late pre- erythrocytic forms by Primaquine phospate. 3 -Prophylaxis: Prevention of primary attack and clinical symptoms by destruction of pre-erythrocytic forms , in patients visiting an endemic areas by Chloroquine phosphate or Mefloquine Prevention and control: 1 -Personal protection from mosquitoes bites e. g. by using of skin repellents and bed nets. 2 -Mosquitoes control. 3 -Treatment of infected cases to reduce the source of infection. 4 -Health education.