PLANT POISONS Every thing is poisonous only the


- Slides: 64

PLANT POISONS
Every thing is poisonous, only the amount differentiates a poison from a
Types of Poisoning Accidental Intentional-Suicidal, Medicinal the Raw plant, tea made from plant
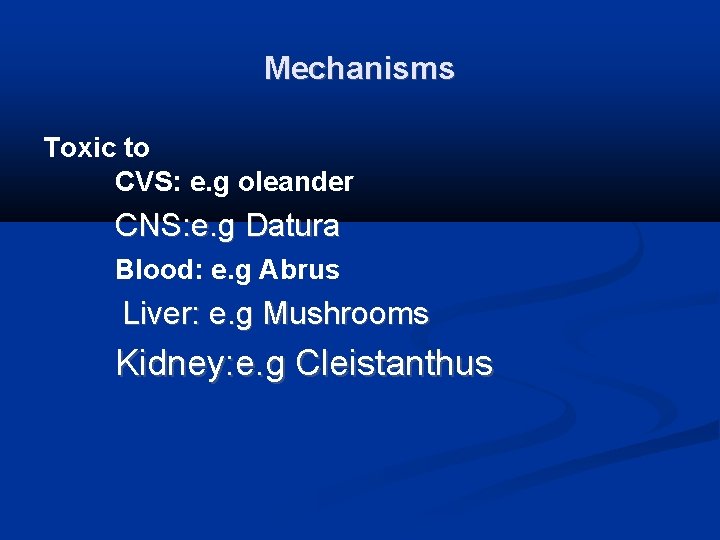
Mechanisms Toxic to CVS: e. g oleander CNS: e. g Datura Blood: e. g Abrus Liver: e. g Mushrooms Kidney: e. g Cleistanthus
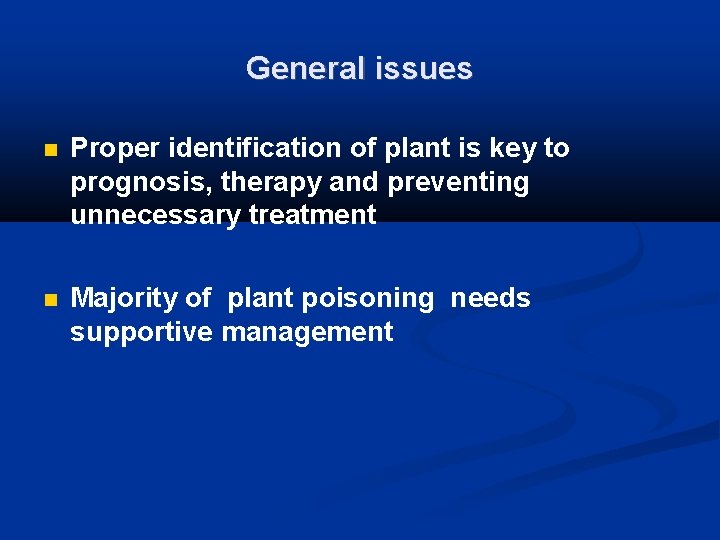
General issues Proper identification of plant is key to prognosis, therapy and preventing unnecessary treatment Majority of plant poisoning needs supportive management
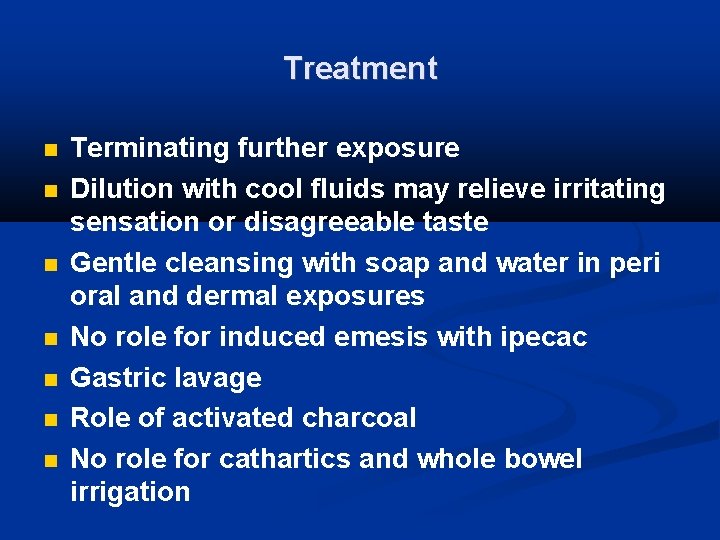
Treatment Terminating further exposure Dilution with cool fluids may relieve irritating sensation or disagreeable taste Gentle cleansing with soap and water in peri oral and dermal exposures No role for induced emesis with ipecac Gastric lavage Role of activated charcoal No role for cathartics and whole bowel irrigation
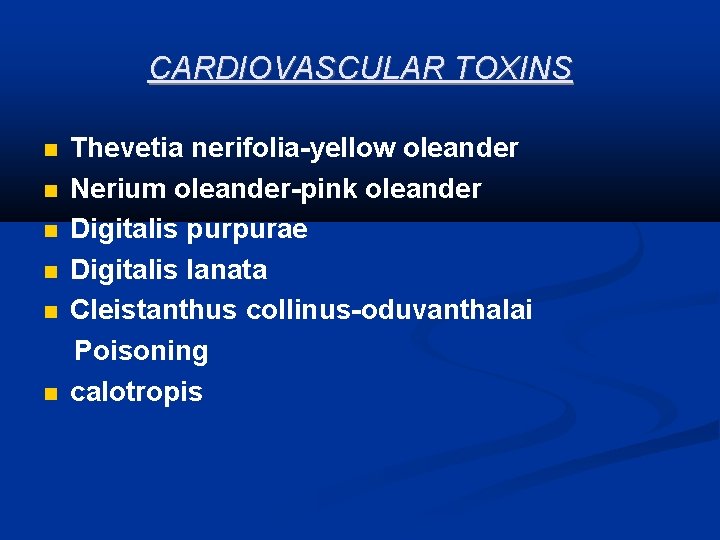
CARDIOVASCULAR TOXINS Thevetia nerifolia-yellow oleander Nerium oleander-pink oleander Digitalis purpurae Digitalis lanata Cleistanthus collinus-oduvanthalai Poisoning calotropis
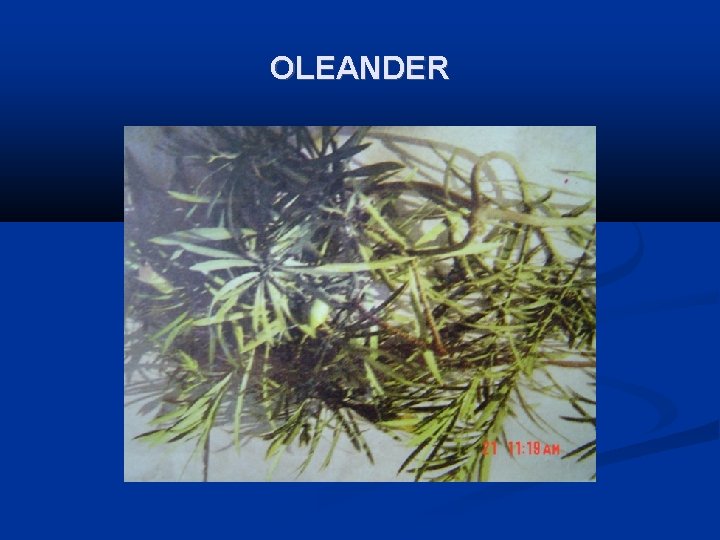
OLEANDER
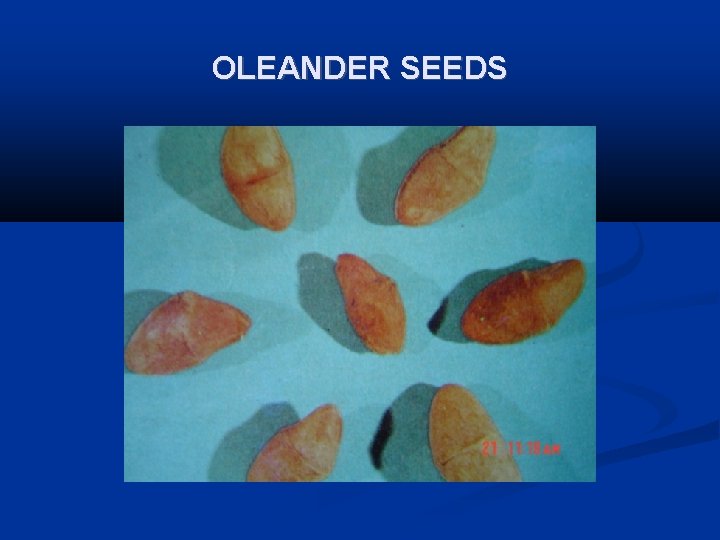
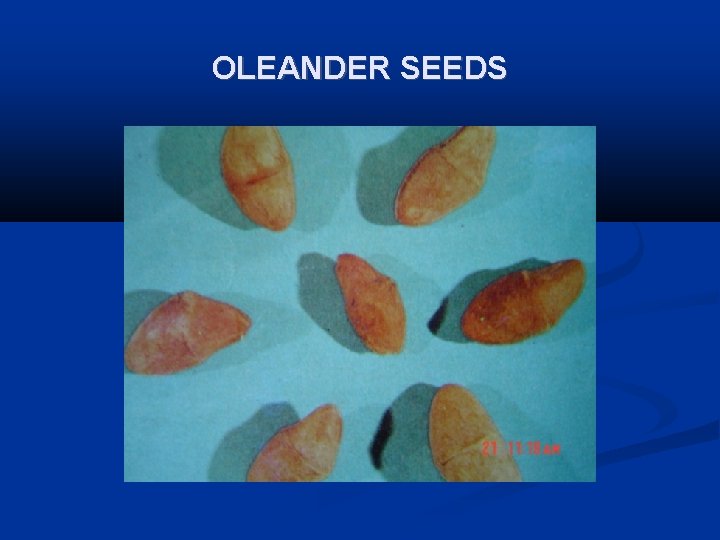
OLEANDER SEEDS
PINK OLEANDER
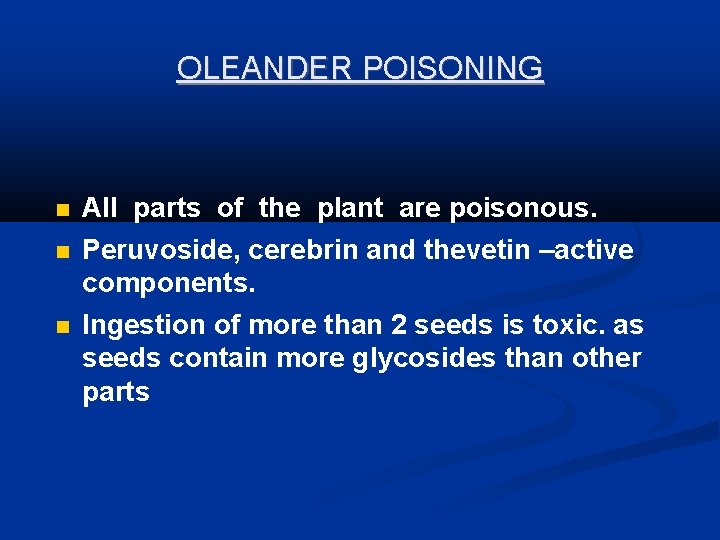
OLEANDER POISONING All parts of the plant are poisonous. Peruvoside, cerebrin and thevetin –active components. Ingestion of more than 2 seeds is toxic. as seeds contain more glycosides than other parts
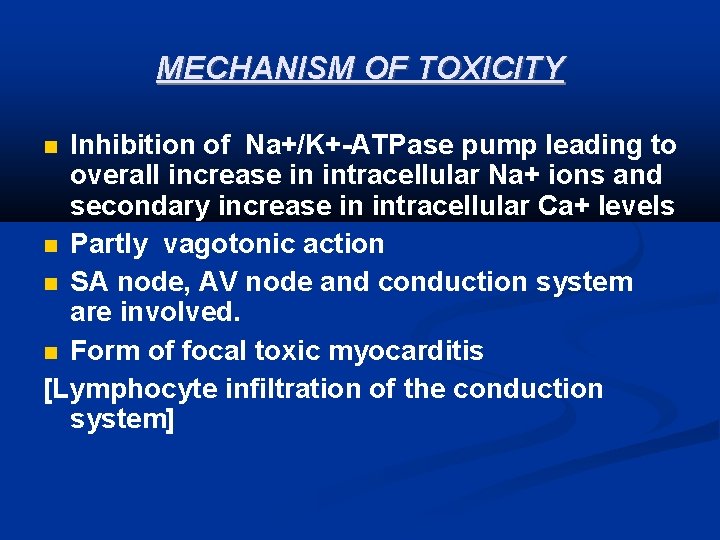
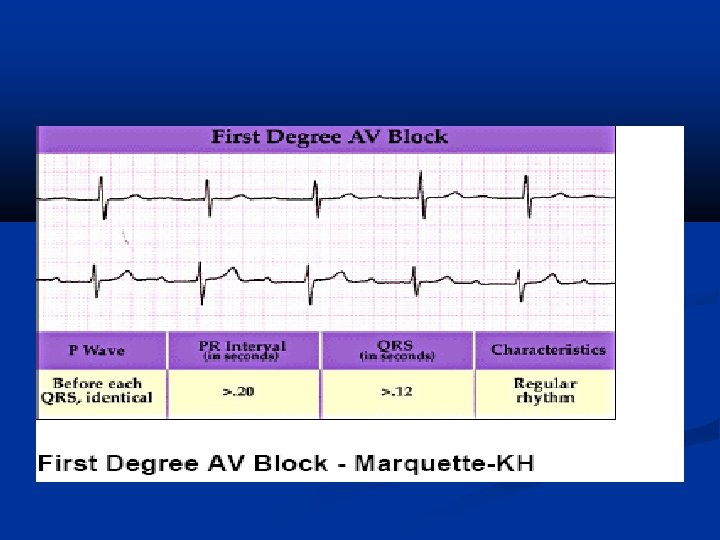
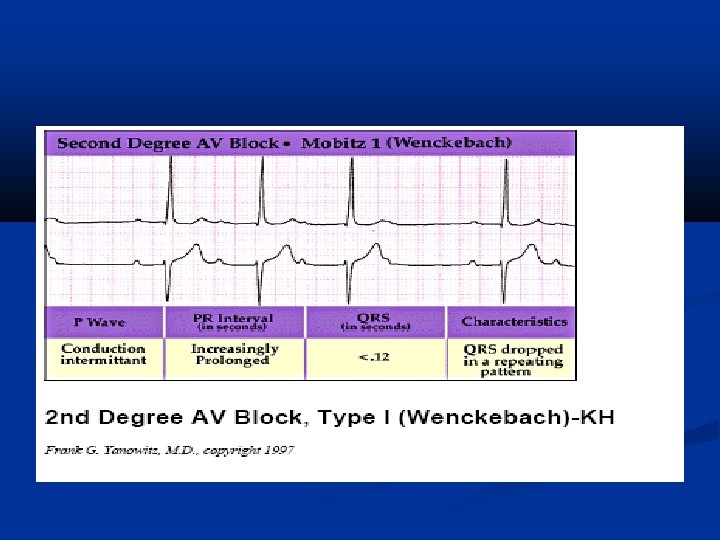
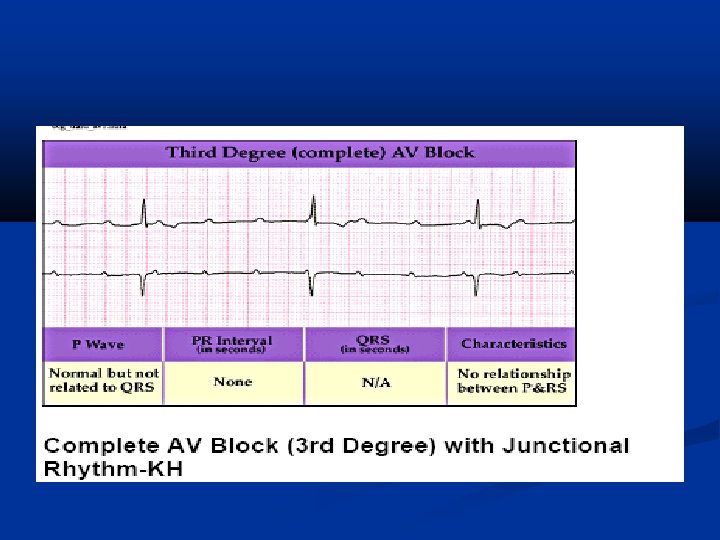
MECHANISM OF TOXICITY Inhibition of Na+/K+-ATPase pump leading to overall increase in intracellular Na+ ions and secondary increase in intracellular Ca+ levels Partly vagotonic action SA node, AV node and conduction system are involved. Form of focal toxic myocarditis [Lymphocyte infiltration of the conduction system]
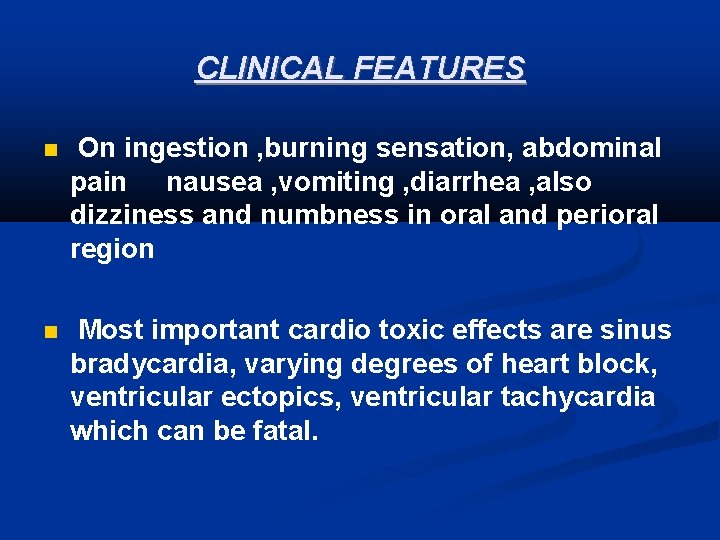
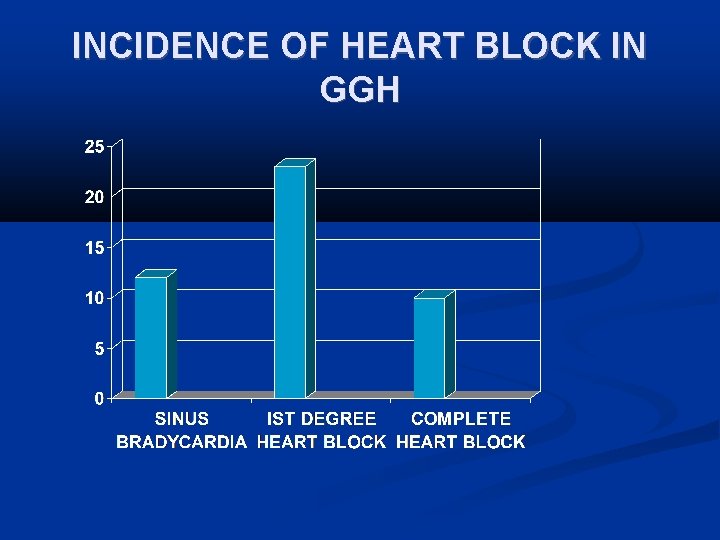
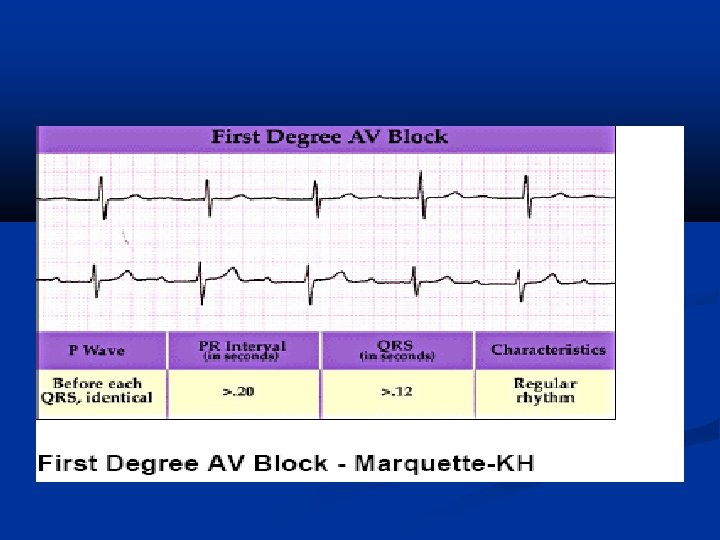
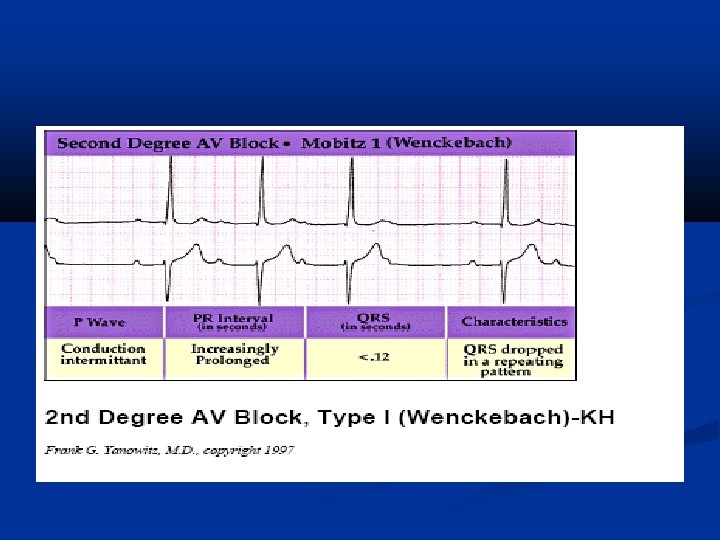
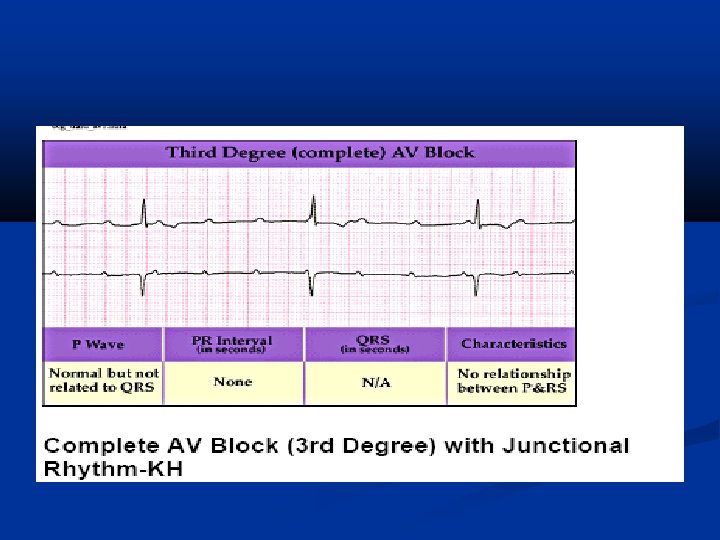
CLINICAL FEATURES On ingestion , burning sensation, abdominal pain nausea , vomiting , diarrhea , also dizziness and numbness in oral and perioral region Most important cardio toxic effects are sinus bradycardia, varying degrees of heart block, ventricular ectopics, ventricular tachycardia which can be fatal.
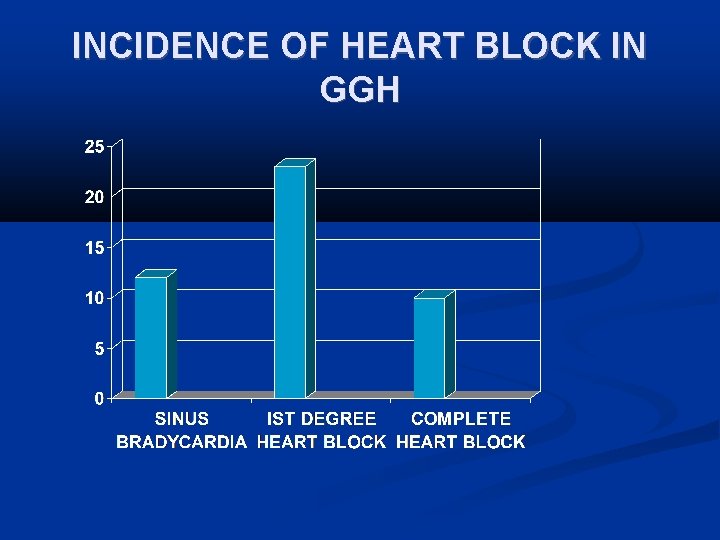
INCIDENCE OF HEART BLOCK IN GGH
Acute hemolysis occurs due to inhalation of oleander blossoms. Dermal route of exposure can cause local irritation and inflammation, unconsciousness and convulsions. Hyperkalemia occurs due to acute toxicity. Hypoxia and metabolic acidosis are potential complications
MONITORING Rate Pulse rate E. C. G Serum potassium Blood urea Serum creatinine Arterial blood gas analysis
MANAGEMENT If patient arrives within 4 hrs of ingestion, and the patient has no convulsions and fully conscious, perform gastric lavage. Take care of ABC and stabilize Activated charcoal and cholestyramine to decrease absorption. Treatment of hyperkalemia and arrhythmias Fab fragments
MANAGEMENT OF CARDIOTOXICITY Atropine 0. 6 mg , Orciprenaline 10 mg to maintain HR around 80/mt. T-wave inversion and ST depression due to toxic myocarditis corrected over a period of 3 -4 hrs with the above regimen. Sodium bicarbonate 50 ml iv 6 th hourly if ABG shows acidosis.
Monitor heart rhythm for at least 5 days. If the heart rate persists below 30/mt after all these regimen put the patient on temporary pacemaker. Do not treat asymptomatic Ventricular premature beats, if symptomatic use lignocaine 1 mg/kg iv every 5 -10 minutes.
Forced alkaline diuresis has no role in the . management. Peritoneal dialysis, hemodialysis, hemoperfusion do not increase the elimination of cardiac glycosides because of large volume of distribution
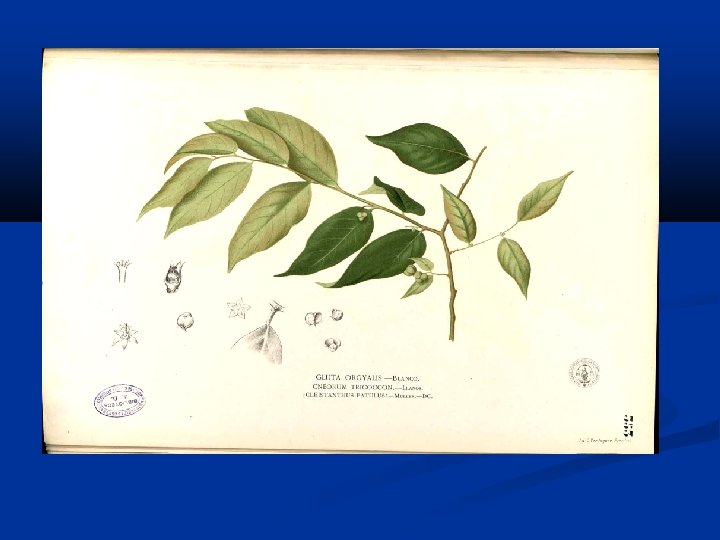
ODUVANTHALAI POISONING Cleistanthus collinus Second most common suicidal plant poison in rural south India after oleander poisoning. Poison preferred by young women.
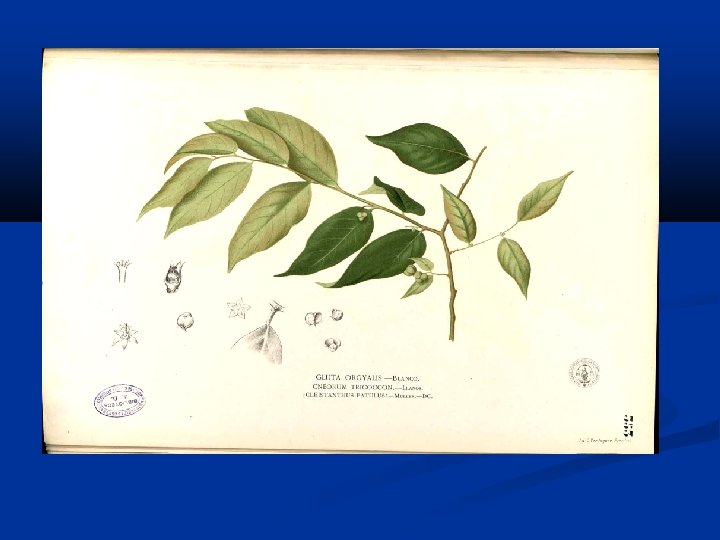
Pathogenesis Cleistanthus collinus is an extremely toxic plant poison. It is known by various names in different parts of India viz. , Oduvanthalai / Nillipalai in Tamilnadu and Pondicherry, Kadishe in Andhra pradesh, Karlajuri in West Bengal and Garari in the Hindi speaking belt. All parts of the plant are poisonous. Cleistanthin A and B are the toxins of Cleistanthus collinus They are diphyllin glycosides which produce cardiac arrhythmias, urinary potassium wasting, hypoxia, metabolic acidosis and hypotension.
MECHANISM OF TOXICITY Inhibition of Na+K+ATPase The cause of hypokalemia remains enigmatic.
Pathogenesis Hypokalemic metabolic acidosis, hypotension and hypoxia have been described in this poisoning. Cases have been reported where d. RTA, distributive shock and ARDS identified in patients, explaining the above findings
CLINICAL FEATURES ECG abnormalities : Bradycardia, Varying degrees of heart Blocks Hypokalemia : Severe hypokalaemia Severe non anion gap metabolic acidosis Increased urinary K+ excretion Increased urine anion gap
MONITIORING E. C. G Serum potassium Heart rate Blood pressure Respiratory rate QTc –USEFUL PROGNOSTIC INDEX
Management Correct hypokalemia by i. v KCL AT A RATE OF NOT MORE THAN 40 meq/l Bradycardia corrected with atropine 0. 6 mg/Orciprenaline 10 mg. If the heart rate is less than 30/mt, temporary Trans venous pacing may be instituted
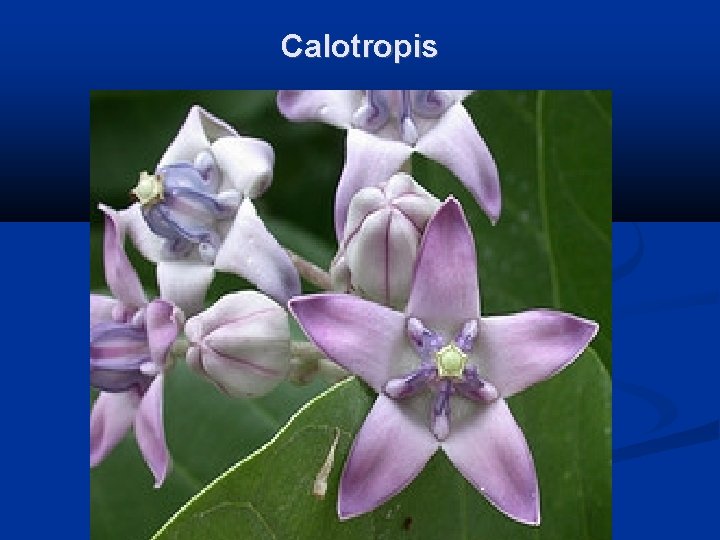
Calotropis is used as a traditional medicinal plant with unique properties Traditionally alotropis is used alone or with other medicinals to treat common disease such as fevers, rheumatism, indigestion, cough, cold, eczema, asthma, elephantiasis, nausea, vomiting, diarrhea According to Ayurveda, dried whole plant is a good tonic, expectorant, , and anthelmintic. The dried root bark is a substitute for ipecacuanha. The powdered root used in asthama, bronchitis, and dyspepsia.
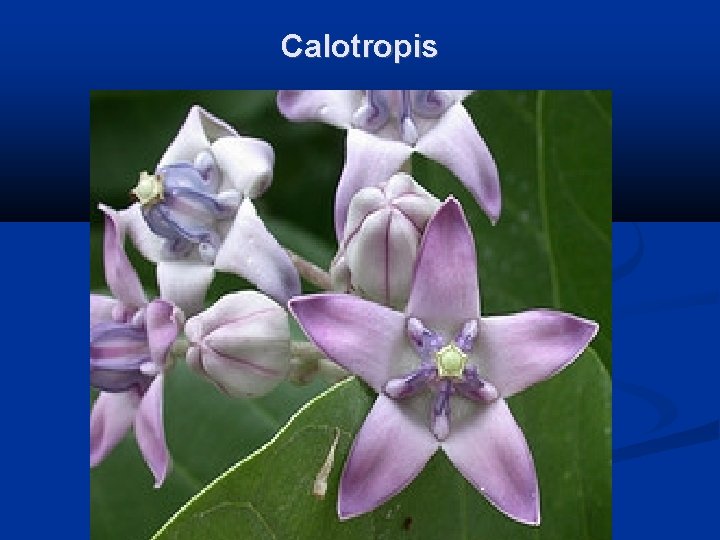
Calotropis
Toxicity Signs Acrid taste usually limits ingestion. Exposure of the skin or mucous membranes to the latex may result in vesicle formation. Keratoconjunctivitis will result if the cornea is exposed. Ingestion of significant quantities will result in ECG abnormalities.
Treatment Wash the exposed tissue with plenty of warm water and soap. Flush the eyes with sterile saline or water for 15 minutes. If cardiac abnormalities are seen, manage according to ECG assessment
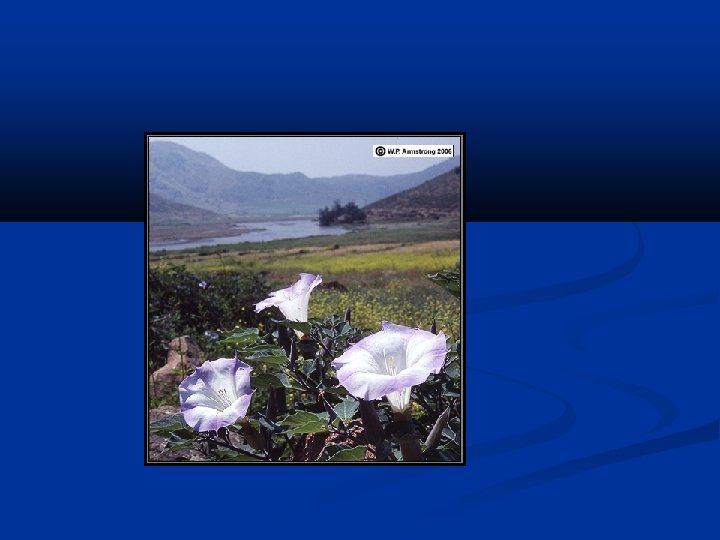
AUTONOMIC NERVOUS SYSTEM TOXINS DATURA STRAMONIUM ATROPA BELLADONA HYOSCYAMUS NIGER
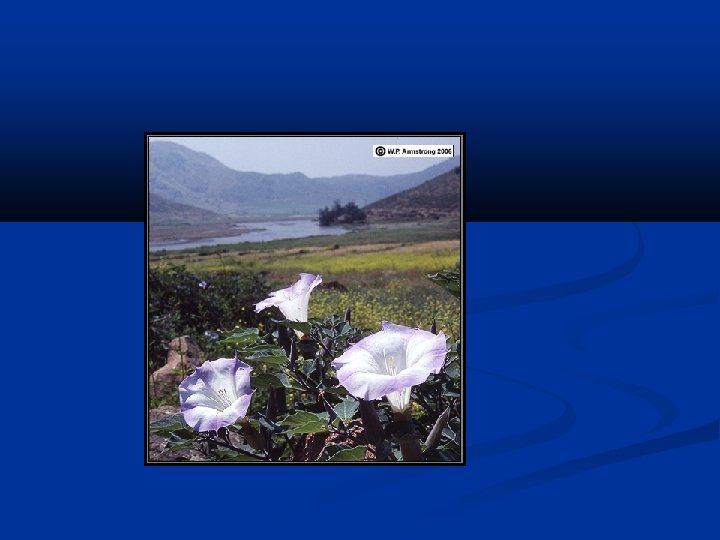
DATURA STRAMONIUM All parts of the plant are poisonous. Seeds are considered to be the most noxious. The alkaloids are scopalamine and hyoscyamine or atropine both have anticholinergic effects. Mostly accidental ingestion by children. Also used to induce hallucinations. Contact with leaves/flowers-dermatitis
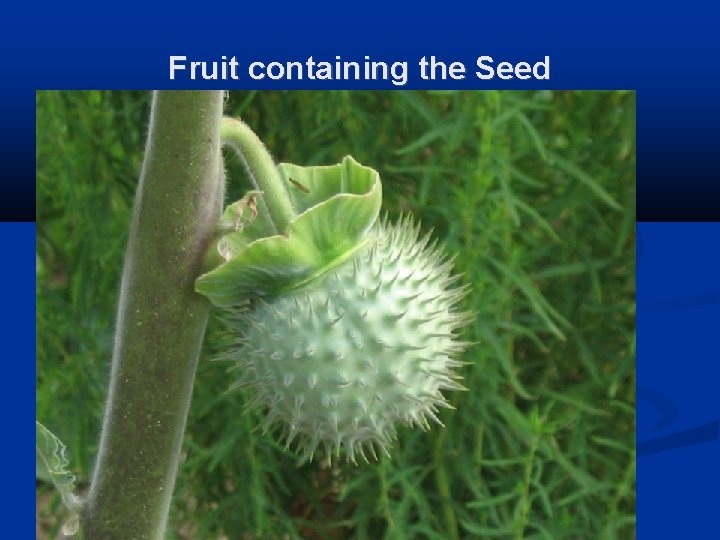
Fruit containing the Seed
CLINICAL FEATURES DATURA PERIPHERAL ANTICHOLINERGIC CENTRAL ANTICHOLINERGIC
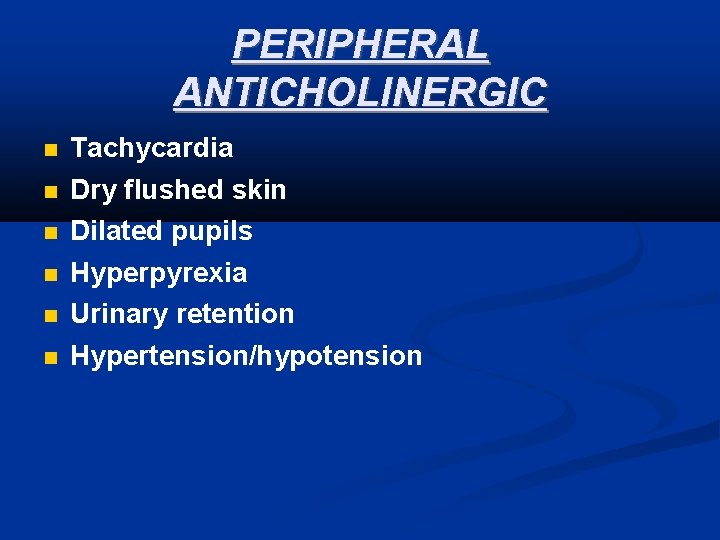
PERIPHERAL ANTICHOLINERGIC Tachycardia Dry flushed skin Dilated pupils Hyperpyrexia Urinary retention Hypertension/hypotension
CENTRAL ANTICHOLINERGIC Disorientation Agitation Muscle in coordination Ataxia Visual/auditory hallucinations Severe toxicity can result in seizures, respiratory Failure & cardiovascular collapse.
Investigations Detection of Atropine by Radio immuno assay Gas chromatography Mass spectrometry Thin layer chromatography Liquid chromatography
MANAGEMENT Supportive care Airway Circulation Gastric lavage (due to inhibition of peristalsis, seeds may remain in stomach for up to 24 hrs). Activated charcoal-50 g every 4 hrs and magnesium sulphate 30 g every 4 hrs
MANAGEMENT Hypotension: IVF, Dopamine Convulsions & agitation: : IV Diazepam 10 20 mg over 30 -60 minutes not to exceed 3 mg/kg over 24 hrs Not to use chlorpromazine for controlling agitation, Hyperactivity, disorientation Severe Hyperthermia: Sedation, Paralysis and active cooling Careful use of physostigmine to counteract CNS anticholinergic syndrome.
PHYSOSTIGMINE USE To be used only if definitely known Dosage: 1 -2 mg IV slowly repeated every 10 min. should not exceed 4 mg in 30 min period Watch for seizure activity, bradycardia, heart blocks, and asystole
INDICATIONS OF PHYSOSTIGMINE Pronounced hallucinations and agitation Supraventricular arrthymias and ventricular arrthymias with hemo dynamic instability Seizures unresponsive to standard anticonvulsants
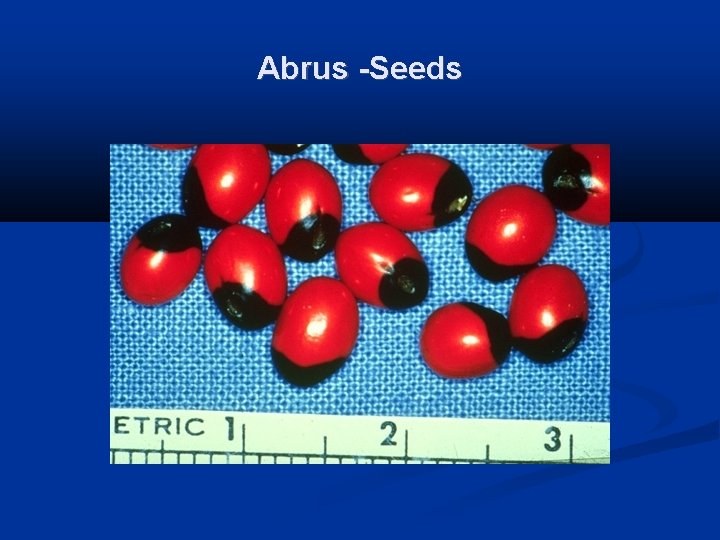
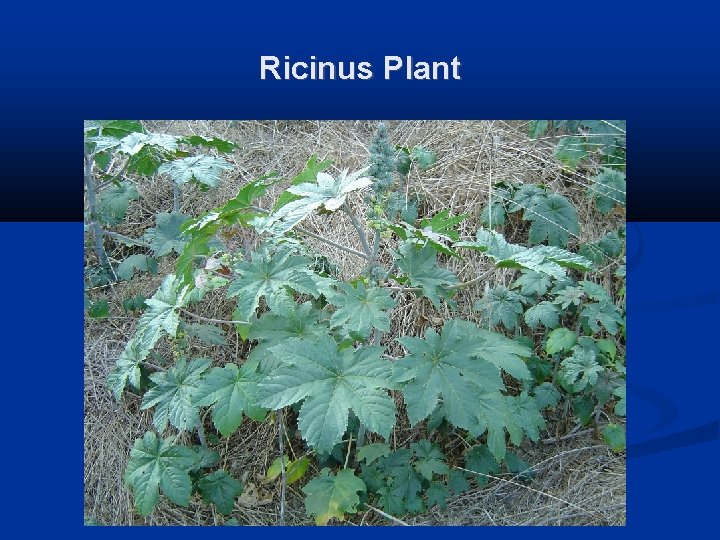
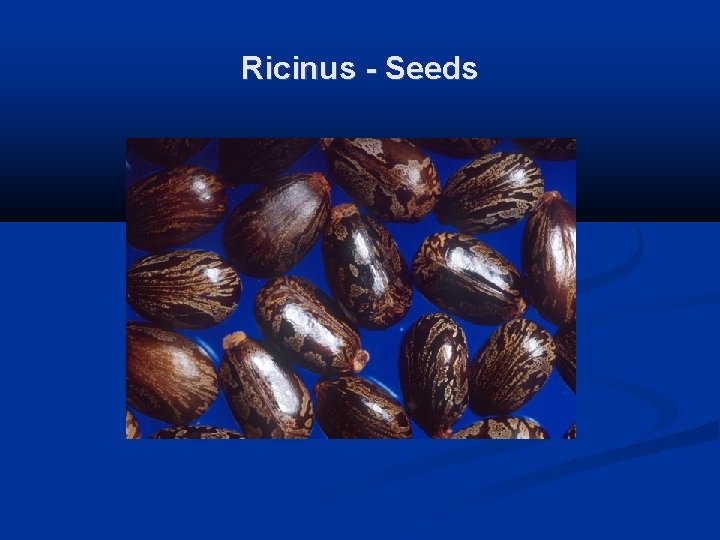
Toxalbumins (Ricin, Abrin) Both differ in appearance and taxonomy but both toxins are similar structurally and functionally Synonyms: Ricinus communis: castor bean Abrus: jequirity, Indian bead, rosaeary pea Toxic parts: All parts especially seeds
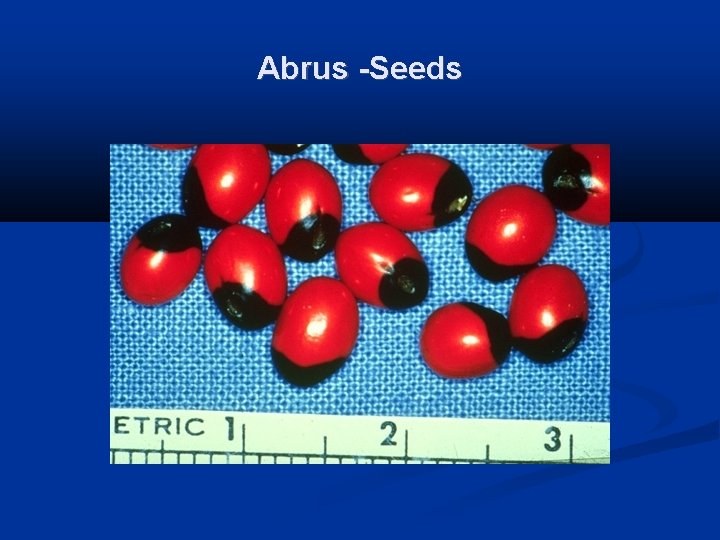
Abrus -Seeds
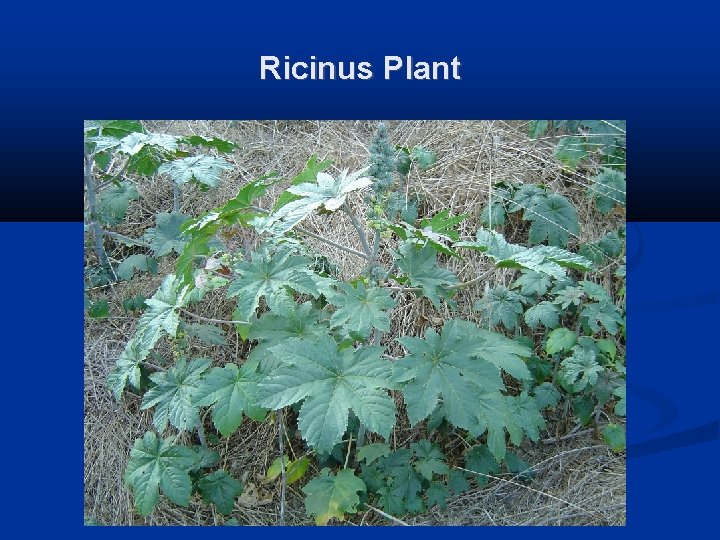
Ricinus Plant
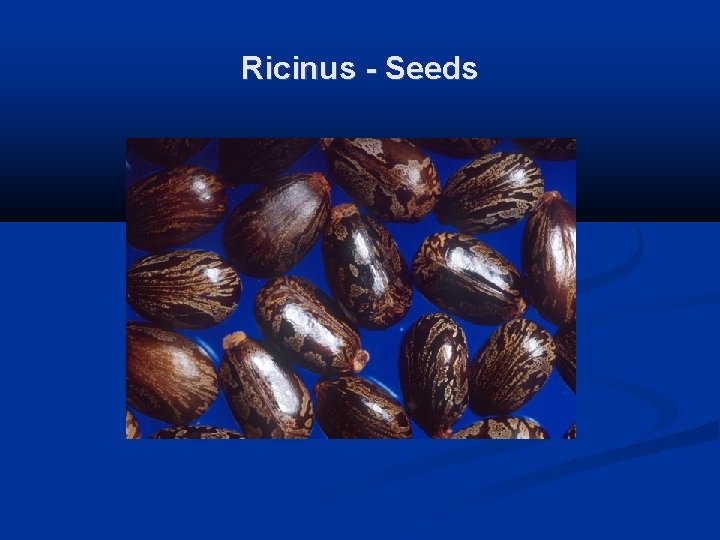
Ricinus - Seeds
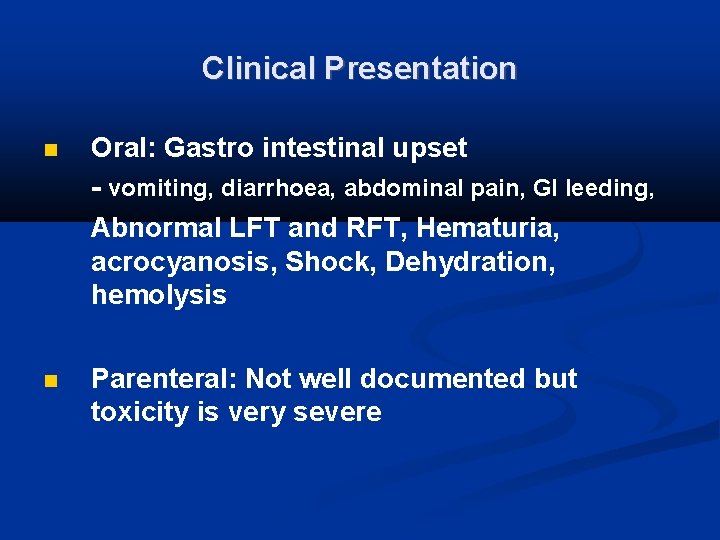
Clinical Presentation Oral: Gastro intestinal upset - vomiting, diarrhoea, abdominal pain, GI leeding, Abnormal LFT and RFT, Hematuria, acrocyanosis, Shock, Dehydration, hemolysis Parenteral: Not well documented but toxicity is very severe
Management Activated charcoal Aggressive fluid resuscitation Other supportive care Cathartics not indicated Extracorporeal elimination not useful
Mushroom Poisoning Fatalities resulting from mushroom ingestion are due to Amatoxins They are octapeptides and are heat-stable, insoluble in water, and not destroyed by drying. At least 5 subtypes of amatoxins exist; alpha and beta amatoxins are the most significant subtypes. Alpha amatoxin inhibits RNA polymerase II, which ultimately leads to cell death.
Clinical features Initial latent and asymptomatic period of 6 -12 hours Abdominal cramping, vomiting, and profuse watery diarrhea (rice water, cholera like) occur. Leading to severe dehydration and circulatory collapse. The patient appears to have improved clinically, ongoing liver damage occurs as indicated by laboratory abnormalities (elevation of serum aminotransferase levels, prothrombin time). This stage may last as long as 2 -3 days. Hepatic and renal injury become clinically apparent and may progress to fulminant
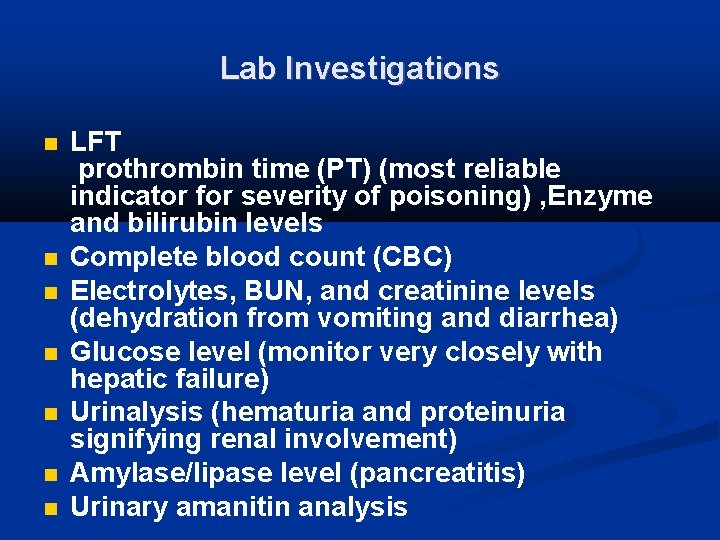
Lab Investigations LFT prothrombin time (PT) (most reliable indicator for severity of poisoning) , Enzyme and bilirubin levels Complete blood count (CBC) Electrolytes, BUN, and creatinine levels (dehydration from vomiting and diarrhea) Glucose level (monitor very closely with hepatic failure) Urinalysis (hematuria and proteinuria signifying renal involvement) Amylase/lipase level (pancreatitis) Urinary amanitin analysis
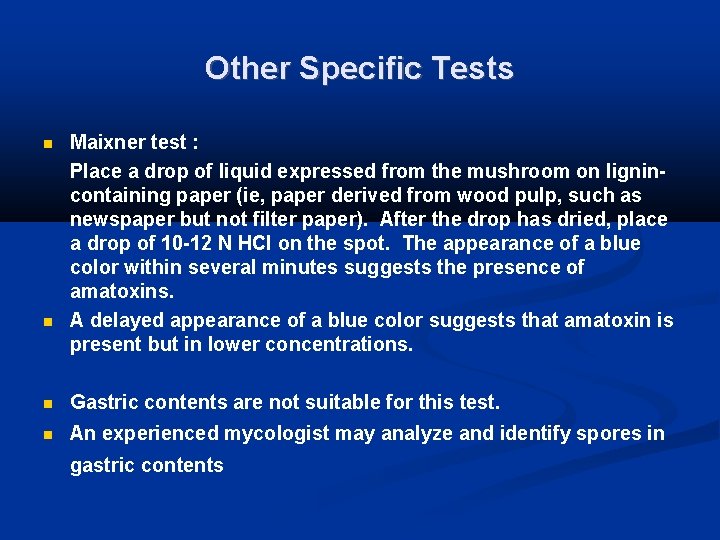
Other Specific Tests Maixner test : Place a drop of liquid expressed from the mushroom on lignincontaining paper (ie, paper derived from wood pulp, such as newspaper but not filter paper). After the drop has dried, place a drop of 10 -12 N HCl on the spot. The appearance of a blue color within several minutes suggests the presence of amatoxins. A delayed appearance of a blue color suggests that amatoxin is present but in lower concentrations. Gastric contents are not suitable for this test. An experienced mycologist may analyze and identify spores in gastric contents
Management Reduction of amatoxin absorption - Gastric lavage, Activated charcoal Aggressive management of fluid and electrolyte imbalance. Vitamin K (if coagulopathy is present) N-acetylcysteine
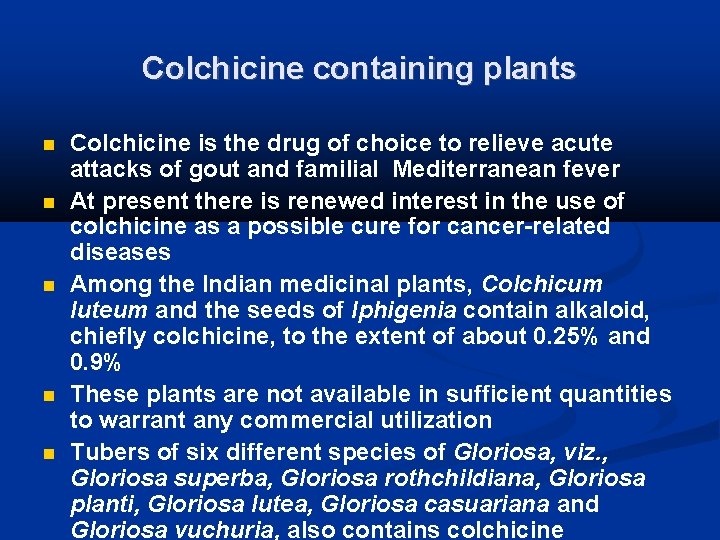
Colchicine containing plants Colchicine is the drug of choice to relieve acute attacks of gout and familial Mediterranean fever At present there is renewed interest in the use of colchicine as a possible cure for cancer-related diseases Among the Indian medicinal plants, Colchicum luteum and the seeds of Iphigenia contain alkaloid, chiefly colchicine, to the extent of about 0. 25% and 0. 9% These plants are not available in sufficient quantities to warrant any commercial utilization Tubers of six different species of Gloriosa, viz. , Gloriosa superba, Gloriosa rothchildiana, Gloriosa planti, Gloriosa lutea, Gloriosa casuariana and Gloriosa vuchuria, also contains colchicine
Colchicum luteum
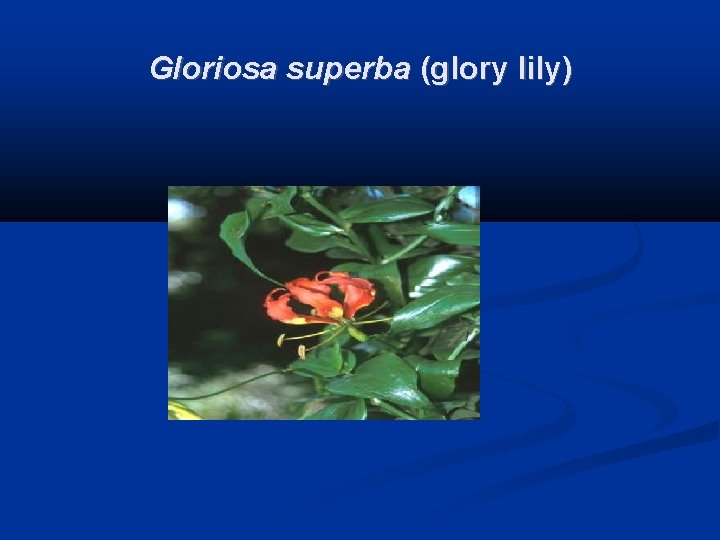
Gloriosa superba (glory lily)
Gloriosa superba (glory lily) Gloriosa superba (glory lily) poisoning has been reported from Sri Lanka and south India The plant contains the alkaloids colchicine and gloriosine. Colchicine has antimitotic properties and causes vomiting and severe diarrhoea, dehydration, haemodynamic instability, renal failure and eventually multiorgan failure. Colchicum autumnale (meadow saffron) also contains colchicine. It appears to be a rare cause of poisoning in many countries
Antibodies against colchicine have been developed in France for the management of acute poisoning with the drug form of colchicine. Animal studies have shown good efficacy. Anti-colchicine antibody fragments are not in commercial production. If they could be made available at a price affordable to local health systems, they might make a significant difference in the management of G. superba and C. autumnale poisoning.
