Planning RCTs ESVS Guidelines Discussion RCTs EVAR 1


- Slides: 41
Planning RCTs ESVS Guidelines Discussion

RCTs EVAR 1 & 2 DREAM OVER ADAM CEASAR PIVOTAL OTHERS FOR r. AAA
EVAR 1 &2 1 : fit pts for OR ELECTIVE EVAR VERSUS OR 2: unfit pts for OR EVAR versus NO 38 to 41 hospitals UK, 60 yrs, 5. 5 cm, C/T scan, 1999 -2004 Target: primary outcome was mortality (operative, all-cause and AAA related). Secondary outcomes were graft-related complications and reinterventions, adverse events, renal function, health-related quality of life and costs
EVAR 1 results Follow-up 5 yrs The EVAR group did demonstrate an early Very little loss to followadvantage in terms of up (1%) AAA-related mortality, EVAR trial 1, 30 -day which was sustained for operative mortalities the first few years, but were 1. 8% and 4. 3% in the lost by the end of the EVAR and open-repair study, primarily due to groups fatal endograft ruptures there was no significant difference between the groups in terms of allcause mortality
EVAR 2 results The 30 -day operative mortality was 7. 3% in the EVAR group this group after 4 years demonstrated a significant advantage in terms of AAA-related mortality this advantage did not result in any benefit in terms of all-cause mortality
EVAR 1 & 2 conclusions EVAR offers a clear operative mortality benefit over open repair in patients fit for both procedures, but this early benefit is not translated into a longterm survival advantage. Among patients unfit for open repair, EVAR is associated with a significant long term reduction in AAA-related mortality but this does not appear to influence all-cause mortality.
DREAM 351 patients, 5 cm in diameter, suitable candidates for both techniques Target: better outcome EVAR in the first month after the procedure is sustained beyond the perioperative period.
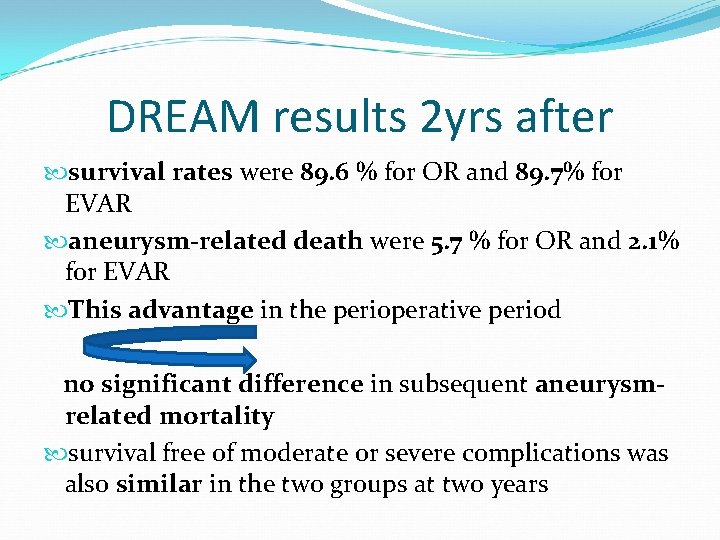
DREAM results 2 yrs after survival rates were 89. 6 % for OR and 89. 7% for EVAR aneurysm-related death were 5. 7 % for OR and 2. 1% for EVAR This advantage in the perioperative period no significant difference in subsequent aneurysmrelated mortality survival free of moderate or severe complications was also similar in the two groups at two years
DREAM conclusions The perioperative survival advantage with endovascular repair as compared with open repair is not sustained after the first postoperative year.
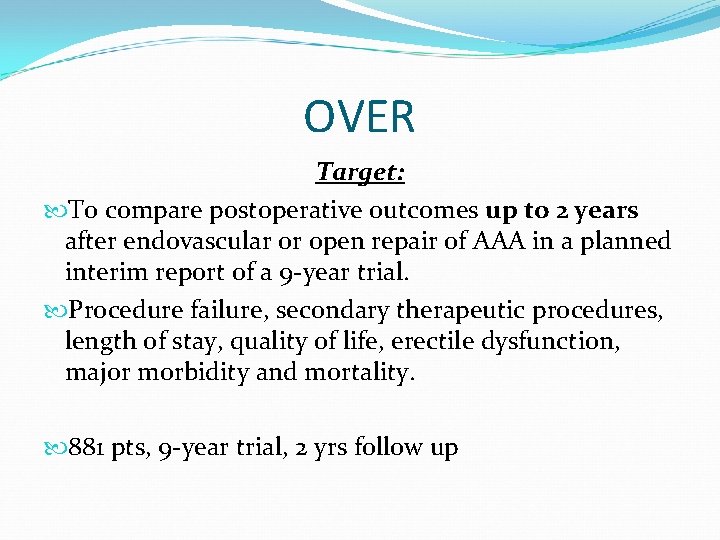
OVER Target: To compare postoperative outcomes up to 2 years after endovascular or open repair of AAA in a planned interim report of a 9 -year trial. Procedure failure, secondary therapeutic procedures, length of stay, quality of life, erectile dysfunction, major morbidity and mortality. 881 pts, 9 -year trial, 2 yrs follow up
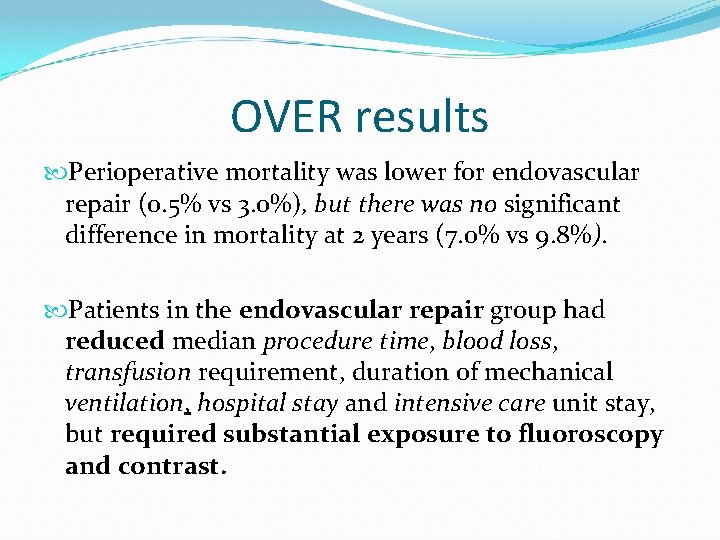
OVER results Perioperative mortality was lower for endovascular repair (0. 5% vs 3. 0%), but there was no significant difference in mortality at 2 years (7. 0% vs 9. 8%). Patients in the endovascular repair group had reduced median procedure time, blood loss, transfusion requirement, duration of mechanical ventilation, hospital stay and intensive care unit stay, but required substantial exposure to fluoroscopy and contrast.
OVER conclusions The early advantage of endovascular repair was not offset by increased morbidity or mortality in the first 2 years after repair
ADAM Target: elective surgical repair of small abdominal aortic aneurysms improves survival 50 to 79 yrs, 4. 0 to 5. 4 cm, Follow-up ranged from 3. 5 to 8. 0 years (mean, 4. 9), 569 patients were randomly assigned to immediate repair and 567 to surveillance By the end of the study, aneurysm repair had been performed in 92. 6 percent of the patients in the immediate-repair group and 61. 6 percent of those in the surveillance group.
ADAM results The rate of death from any cause, the primary outcome, was not significantly different in the two groups a low total operative mortality of 2. 7% in the immediate-repair group. no reduction in the rate of death related to abdominal aortic aneurysm in the immediate-repair group (3. 0%) as compared with the surveillance group (2. 6%). Eleven patients in the surveillance group had rupture of abdominal aortic aneurysms (0. 6% per year), resulting in seven deaths.
ADAM conclusions Survival is not improved by elective repair of abdominal aortic aneurysms smaller than 5. 5 cm, even when operative mortality is low.
PIVOTAL 4 to 5 cm, Aneu. Rx/Talent, 1050 -patient, 525 in each group, Primary targets: aneurysm rupture AAA-related death up to 3 years Secondary targets: All-cause and AAA-related mortality in smokers vs nonsmokers; conversion to open surgical repair
PIVOTAL debate Smaller AAAs can be more favorable for EVAR as a result of suitable aortic anatomy longer necks, less angulation, less tortuosity, and longer iliac landing zones With each 1 -cm increase in diameter, anatomic suitability for EVAR decreased fivefold. increased risks of OR at a time when the patients are older and less fit for EVAR Welborn MB, Yau FS, Modrall JG, Lopez JA, Floyd S, Valentine RJ, et al. Endovascular repair of small abdominal aortic aneurysms: a paradigm shift? Vasc Endovasc Surg 2005; 39: 381 -91.
PIVOTAL early results perioperative mortality was only 0. 6%, and the 3 year rate of rupture or aneurysm-related mortality was near zero early EVAR would be of benefit in preventing rupture both appear to be safe alternatives for patients with small aneurysms of 4. 0 to 5. 0 Ouriel K, Clair DG, Kent KC, Zarins CK; Positive Impact of Endovascular Options for treating Aneurysms Early (PIVOTAL) Investigators J Vasc Surg. 2010 May; 51(5): 1081 -7. doi: 10. 1016/j. jvs. 2009. 10. 113. Epub 2010 Mar 20. Endovascular repair compared with surveillance for patients with small abdominal aortic aneurysms. . Division of Vascular Surgery, Columbia University and New. York. Presbyterian Hospital, New York, NY, USA. ourielk@nyp. org
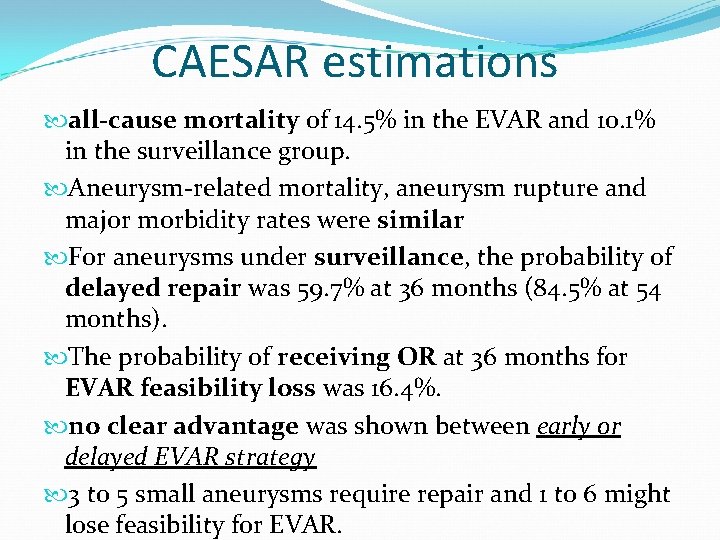
CAESAR Target : endovascular aortic aneurysm repair (EVAR) or surveillance in AAA<5. 5 cm. all-cause mortality follow-up of 32. 4 months 4. 1 -5. 4 cm, 360 patients One perioperative death after EVAR and two late ruptures (both in the surveillance group) occurred
CAESAR estimations all-cause mortality of 14. 5% in the EVAR and 10. 1% in the surveillance group. Aneurysm-related mortality, aneurysm rupture and major morbidity rates were similar For aneurysms under surveillance, the probability of delayed repair was 59. 7% at 36 months (84. 5% at 54 months). The probability of receiving OR at 36 months for EVAR feasibility loss was 16. 4%. no clear advantage was shown between early or delayed EVAR strategy 3 to 5 small aneurysms require repair and 1 to 6 might lose feasibility for EVAR.
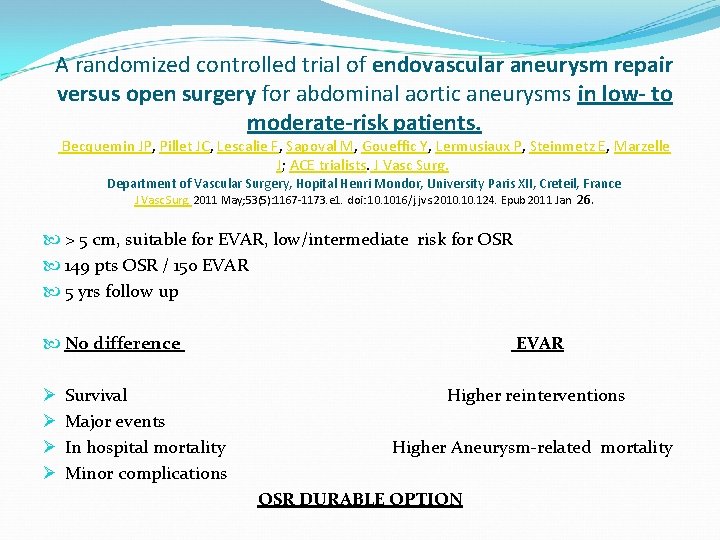
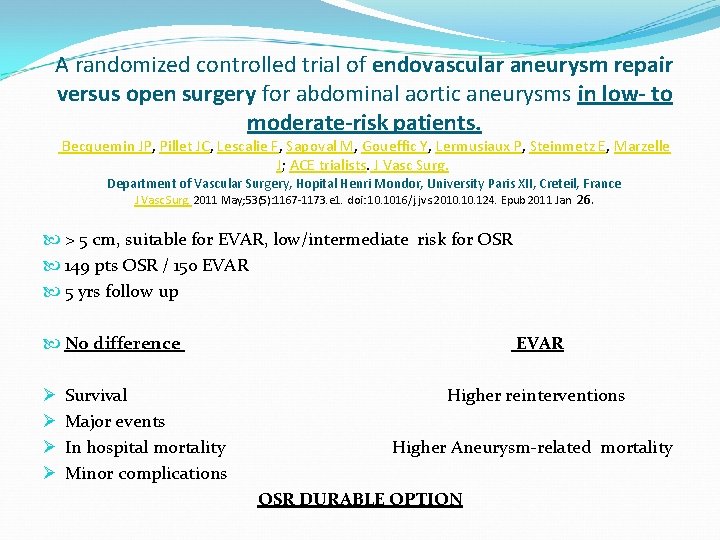
A randomized controlled trial of endovascular aneurysm repair versus open surgery for abdominal aortic aneurysms in low- to moderate-risk patients. Becquemin JP, Pillet JC, Lescalie F, Sapoval M, Goueffic Y, Lermusiaux P, Steinmetz E, Marzelle J; ACE trialists. J Vasc Surg. Department of Vascular Surgery, Hopital Henri Mondor, University Paris XII, Creteil, France J Vasc Surg. 2011 May; 53(5): 1167 -1173. e 1. doi: 10. 1016/j. jvs. 2010. 124. Epub 2011 Jan 26. > 5 cm, suitable for EVAR, low/intermediate risk for OSR 149 pts OSR / 150 EVAR 5 yrs follow up No difference Ø Ø Survival Major events In hospital mortality Minor complications EVAR Higher reinterventions Higher Aneurysm-related mortality OSR DURABLE OPTION
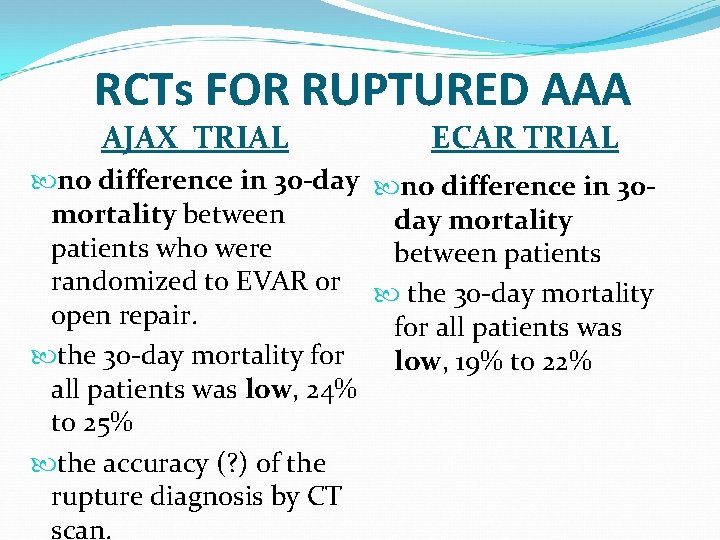
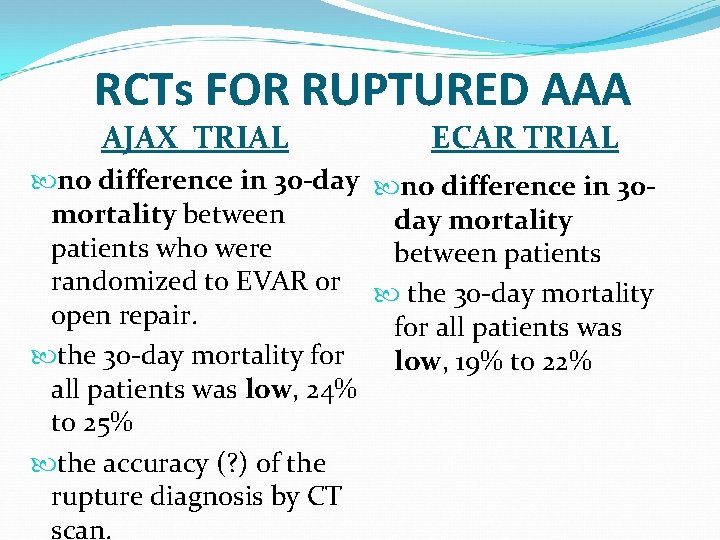
RCTs FOR RUPTURED AAA AJAX TRIAL ECAR TRIAL no difference in 30 -day no difference in 30 mortality between day mortality patients who were between patients randomized to EVAR or the 30 -day mortality open repair. for all patients was the 30 -day mortality for low, 19% to 22% all patients was low, 24% to 25% the accuracy (? ) of the rupture diagnosis by CT scan.
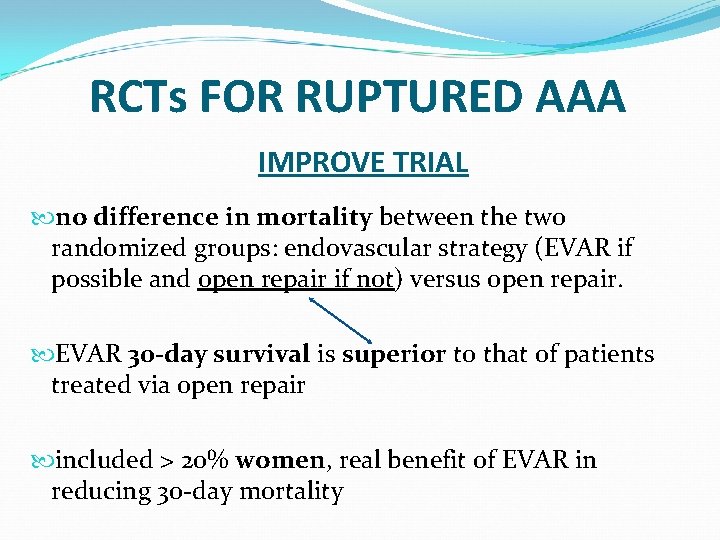
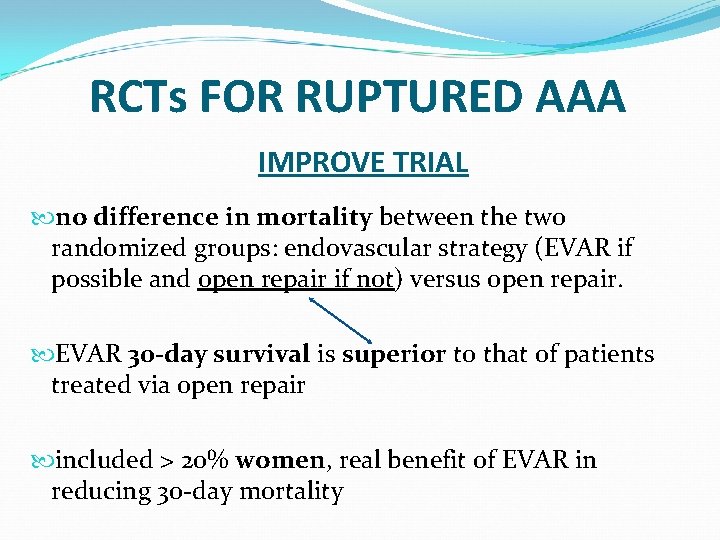
RCTs FOR RUPTURED AAA IMPROVE TRIAL no difference in mortality between the two randomized groups: endovascular strategy (EVAR if possible and open repair if not) versus open repair. EVAR 30 -day survival is superior to that of patients treated via open repair included > 20% women, real benefit of EVAR in reducing 30 -day mortality
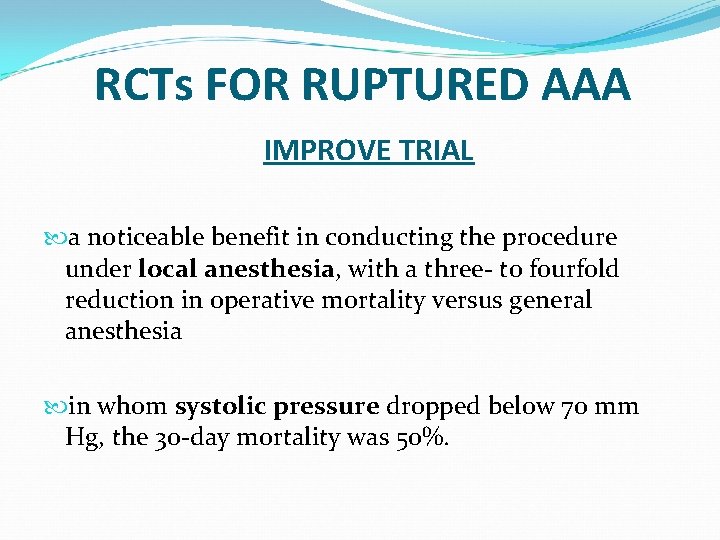
RCTs FOR RUPTURED AAA IMPROVE TRIAL a noticeable benefit in conducting the procedure under local anesthesia, with a three- to fourfold reduction in operative mortality versus general anesthesia in whom systolic pressure dropped below 70 mm Hg, the 30 -day mortality was 50%.
ESVS GUIDELINES • Randomised controlled trials, large registries and singlecenter series comparing EVAR with OR have shown that the minimally invasive approach has lower early morbidity and mortality low incidence of primary conversion to OR after EVAR, between 0. 9 and 5. 9% (1. 8% on RCTs)
Pre-operative evaluation of cardiac morbidity Regardless of the type of surgery, coronary artery disease (CAD) is the leading cause of early and late mortality after AAA repair
Cardiac disease Before the planned endovascular procedure, a detailed cardiac history should therefore be obtained, and patients should be screened for all cardiovascular risk factors. Level 2, Recommendation B. Cardiac stress testing prior to EVAR is recommended in patients with three or more clinical factors for cardiac disease. Level 2 b, Recommendation B
Pulmonary disease A recent retrospective study conducted by Jonker 293 found that patients with AAA and chronic obstructive pulmonary disease had improved outcomes after EVAR compared to those undergoing open repair. In-hospital death and major complications occurred in 30% of patients after open repair compared with 12% after EVAR. Jonker FH, Schlosser FJ, Dewan M, Huddle M, Sergi M, Dardik A, et al. Patients with abdominal aortic aneurysm and chronic obstructive pulmonary disease have improved outcomes with endovascular aneurysm repair compared with open repair. Vascular 2009 Nove. Dec; 17(6): 316 e 24.
Renal protection strategies The REMEDIAL trial suggested that the strategy of volume supplementation by sodium bicarbonate plus NAC seems to be superior to the combination of normal saline with NAC alone in preventing CIN in patients at medium to high risk Briguori C, Airoldi F, D’Andrea D, Bonizzoni E, Morici N, Focaccio A, et al. Renal insufficiency following contrast media administration trial (REMEDIAL): a randomised comparison of 3 preventive strategies. Circulation 2007 Mar 13; 115(10): 1211 e 7 [Epub 2007 Feb 19].
Suprarenal fixation did not seem to increase the likelihood of postoperative renal impairment. Furthermore, suprarenal fixation may be responsible for progressively significant proteinuria. Kouvelos GN, Boletis I, Papa N, Kallinteri A, Peroulis M, Matsagkas MI. Analysis of effects of fixation type on renal function after endovascular aneurysm repair. Department of Surgery, Vascular Surgery Unit, Medical School, University of Ioannina, Greece. J Endovasc Ther. 2013 Jun; 20(3): 334 -44. doi: 10. 1583/124177 MR. 1.
Graft Type The RETA Registry reported that all inhospital complications, reinterventions, conversions, and technical failure were significantly more frequent in the AUI group. Thomas SM, Beard JD, Ireland M, Ayers S, on behalf of the Vascular Society of Great Bitain and Ireland the British Society of Interventional Radiology. Results from theprospective registry of endovascular treatment of abdominal aortic aneurysm (RETA): midterm results to five years. Eur J Vasc Endovasc Surg 2005; 29: 563 e 70. Noorani A, Cooper DG, Walsh SR, Sadat U, Varty K, Boyle JR, Hayes PD. Cambridge Vascular Unit, Addenbrooke's Hospital, Cambridge University Hospitals NHS Foundation Trust, Cambridge, UK. Comparison of aortomonoiliac Endovascular aneurysm repair versus a
Type of anaesthesia The preferential use of local anaesthesia for EVAR, restricting regional anaesthesia or general anaesthesia only to those with predefined contraindications, is feasible and appears to be well tolerated. Level 3 b, Recommendation B.
Percutaneous access Percutaneous approach for EVAR may provide a less invasive aortic access and can facilitate shorter hospital stay in selected patients. Level 3, Recommendation D.

Management of accessory renal arteries Most often the occlusion of accessory renal arteries during EVAR is not associated with clinically significant signs or symptoms of renal infarct, does not contribute to any increase in endoleak rate and should not be embolised preoperatively. Level 4, Recommendation C.
Management of concomitant iliac aneurysms Preservation of flow to at least one hypogastric artery is recommended in standard risk patients. Level 2 c, Recommendation B. Hypogastric embolisation is usually preferred over simple coverage of its ostium by the endograft to prevent the risk of Type 2 endoleak, but coils should be placed as proximal as possible to spare collateral circulation. Level 4, Recommendation C.
The use of an IBD in maintaining antegrade flow to at least one hypogastric artery for aortoiliac aneurysm repair was shown to be feasible and safe in some preliminary clinical series Malina M, Dirven M, Sonesson B, Resch T, Dias N, Ivancev K. Feasibility of a branched stentgraft in common iliac artery aneurysms. J Endovasc Ther 2006; 13: 496 e 500. Tielliu IF, Bos WT, Zeebregts CJ, Prins TR, Van Den Dungen JJ, Verhoeven EL. The role of branched endografts in preserving internal iliac arteries. J Cardiovasc Surg (Torino) 2009; 50(2): 213 e 8. Ziegler P, Avgerinos ED, Umscheid T, Perdikides T, Erz K, Stelter WJ. Branched iliac bifurcation: 6 years experience with endovascular preservation of internal iliac artery flow. J Vasc Surg 2007; 46(2): 204 e 10. Verzini F, Parlani G, Romano L, De Rango P, Panuccio G, Cao P. Endovascular treatment of iliac aneurysm: concurrent comparison of side branch endograft versus hypogastric exclusion. J Vasc Surg 2009; 49(5): 1154 e 61.
Pararenal aneurysms: fenestrated grafts In case of short or diseased neck the use of endografts with fenestrations shows promising results but should be performed with appropriate training and in centers with extensive experience in EVAR. Level 3, Recommendation C.
early mortality of the procedure resulted ranging between 0% and 8. 5%, with a reintervention rate of 7. 9 -24%. Monahan TS, Schneider DB. Fenestrated and branched stent grafts for repair of complex aortic aneurysms. Semin Vasc Surg 2009; 22: 132 e 9.
Endovascular repair of ruptured AAA EVAR should be considered as a treatment option for ruptured AAA, provided that anatomy is suitable, and the centre is appropriately equipped and the team experienced in emergency endovascular aneurysm procedures. Level 2 b, Recommendation B.