Planning Implementing and Evaluating Your Health Promotion Programs
- Slides: 22
Planning, Implementing, and Evaluating Your Health Promotion Programs A 6 -Week Public Health Course Week 3: Assessing Our Population, Part 2
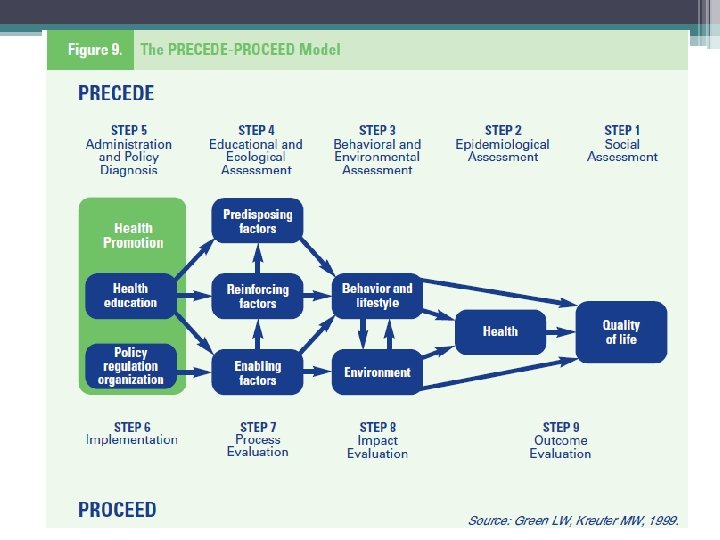
Today: • Looking ahead to the final project • Discuss epidemiological assessment and behavioral and environmental assessment • Educational and ecological assessment • Administration and policy diagnosis
Final Project • Plan ▫ When will you implement? ▫ Who will you submit it to? ▫ Keep track of your resources • 2011 National Health and Wellness Conference ▫ Poster session or presentation?
Homework • What do you know about STIs on your center? • What population and/or STI will you prioritize? Why? • What are your most important/most changeable priorities?
Homework Summary • Awesome data. Different ages and genders. Lots of Chlamydia. Interesting info about syphilis. • Numbers are too low to see a significant change. • Lots of jumping ahead! Let’s bring it back for a moment. • Important/changeable
What can you change? - Behavioral - Condom use with new/casual partners - Response to peer and partner pressure (condom communication and negotiation skills) - Intent to avoid risky sexual behaviors - # of partners - Frequency of sex - Delay sexual activity in virgins (by a little bit) - Females apply condoms to male partners - Environmental - Accessible condoms - Patrol of areas where students “hook up”
What can’t you change? • Students having premarital sex • Much harder to change condom use in “main” partners—need to define main partners
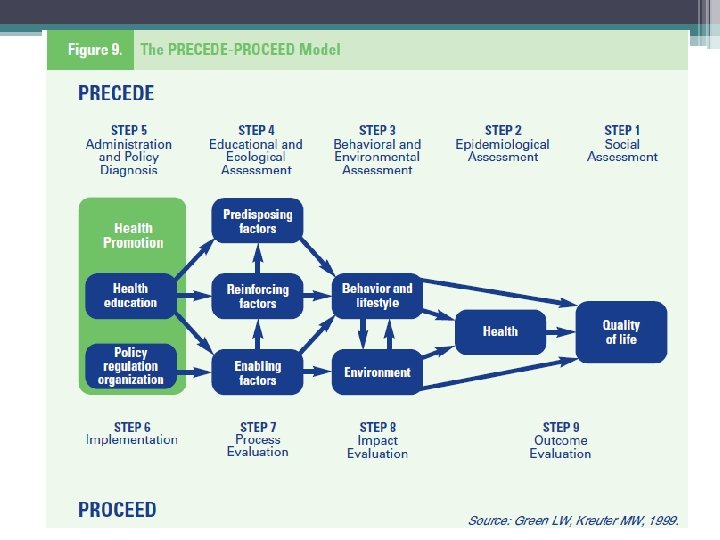
Educational and Ecological Assessment “Identifies preceding and reinforcing factors that must be in place to initiate and sustain change. ” • Become the targets/objectives of your program • Helps planners untangle the complex forces shaping health-related behavior and environmental conditions • Must consider all factors
Three Parts • Predisposing—motivate or provide a reason for behavior; knowledge, attitudes, cultural beliefs, and readiness to change • Enabling—enable persons to act on their predispositions; available resources, supportive policies, assistance, and services • Reinforcing—(after a behavior has been initiated) encourage repetition or persistence of behaviors by providing awards or incentives (social support, praise, reassurance, and symptom relief)
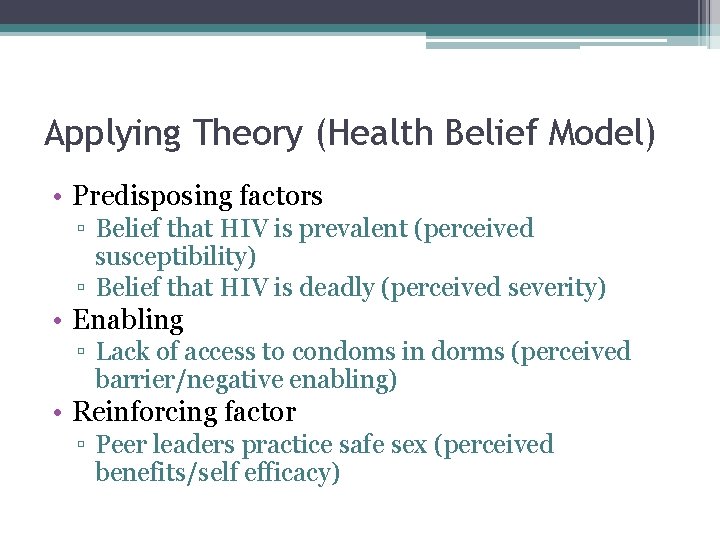
Applying Theory (Health Belief Model) • Predisposing factors ▫ Belief that HIV is prevalent (perceived susceptibility) ▫ Belief that HIV is deadly (perceived severity) • Enabling ▫ Lack of access to condoms in dorms (perceived barrier/negative enabling) • Reinforcing factor ▫ Peer leaders practice safe sex (perceived benefits/self efficacy)
Gathering Information • From students • Talk with other staff • Rely on past experience
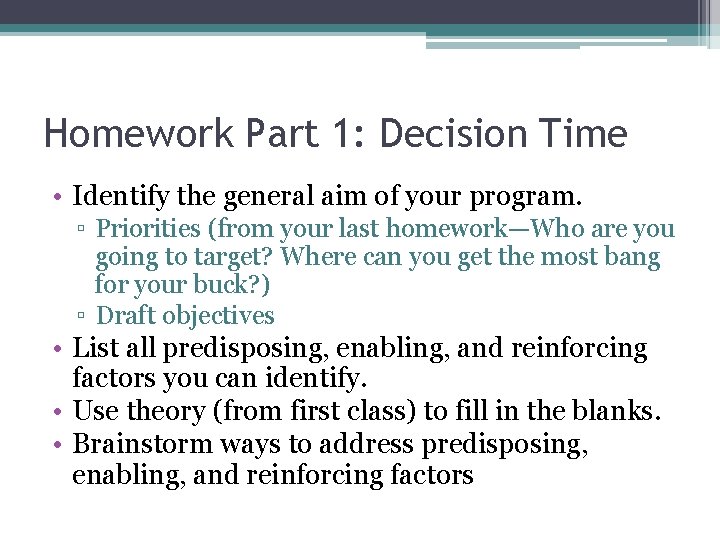
Homework Part 1: Decision Time • Identify the general aim of your program. ▫ Priorities (from your last homework—Who are you going to target? Where can you get the most bang for your buck? ) ▫ Draft objectives • List all predisposing, enabling, and reinforcing factors you can identify. • Use theory (from first class) to fill in the blanks. • Brainstorm ways to address predisposing, enabling, and reinforcing factors
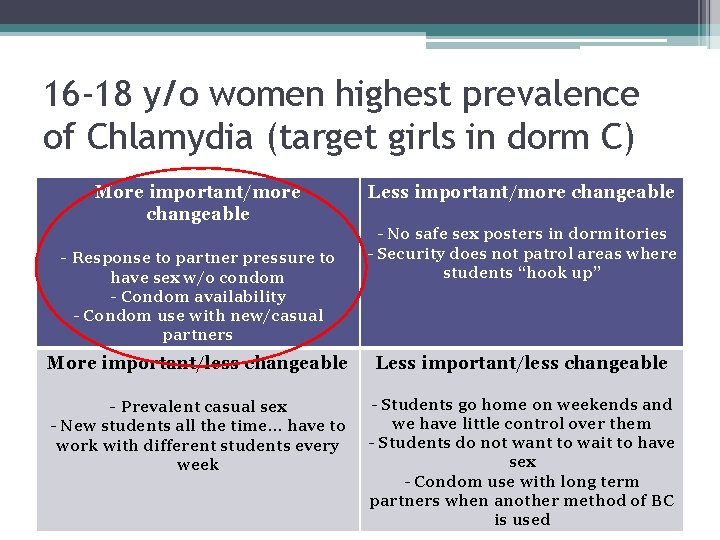
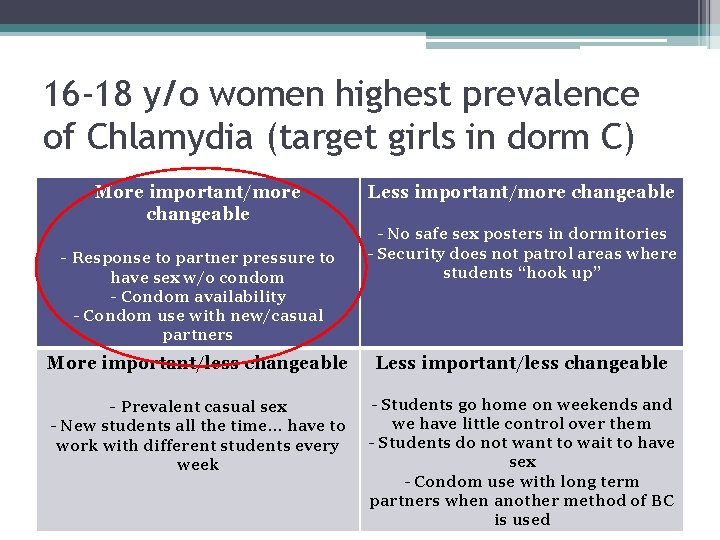
16 -18 y/o women highest prevalence of Chlamydia (target girls in dorm C) More important/more changeable - Response to partner pressure to have sex w/o condom - Condom availability - Condom use with new/casual partners Less important/more changeable - No safe sex posters in dormitories - Security does not patrol areas where students “hook up” More important/less changeable Less important/less changeable - Prevalent casual sex - Students go home on weekends and we have little control over them - Students do not want to wait to have sex - Condom use with long term partners when another method of BC is used - New students all the time… have to work with different students every week
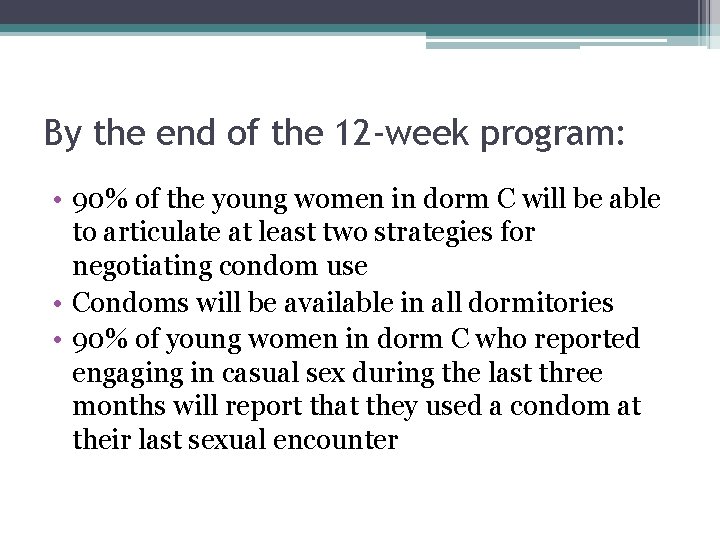
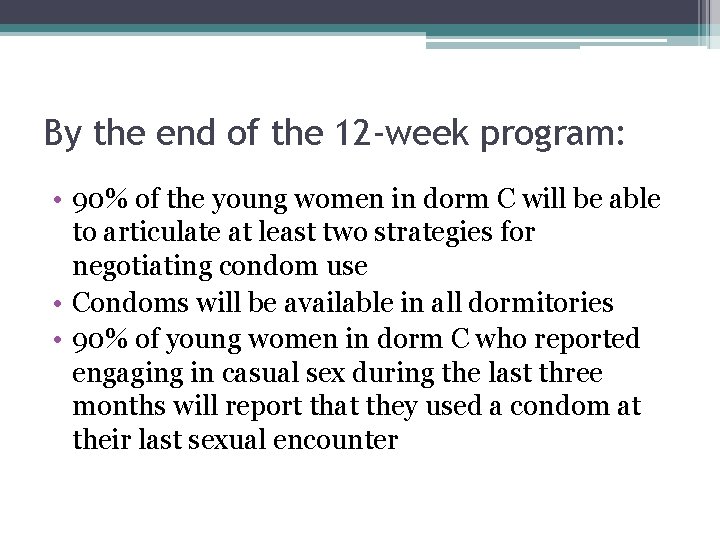
By the end of the 12 -week program: • 90% of the young women in dorm C will be able to articulate at least two strategies for negotiating condom use • Condoms will be available in all dormitories • 90% of young women in dorm C who reported engaging in casual sex during the last three months will report that they used a condom at their last sexual encounter
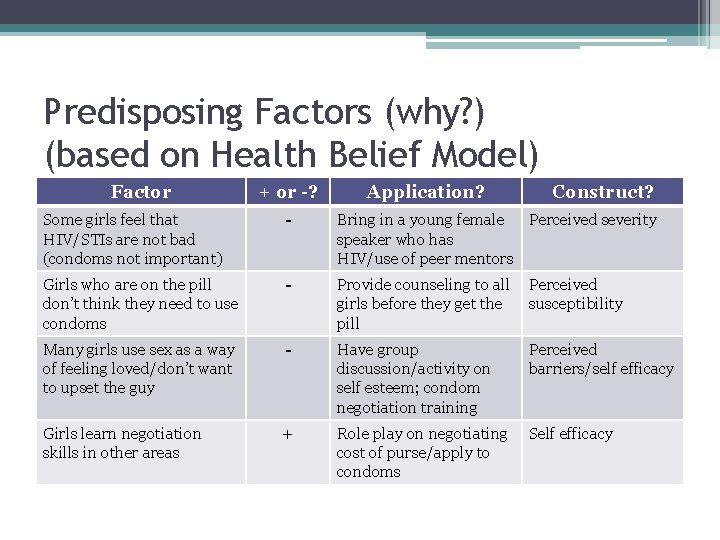
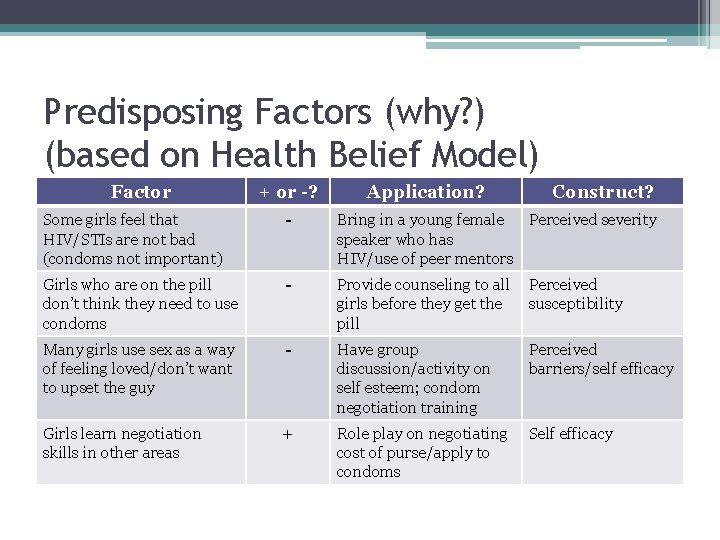
Predisposing Factors (why? ) (based on Health Belief Model) Factor + or -? Application? Construct? Some girls feel that HIV/STIs are not bad (condoms not important) - Bring in a young female Perceived severity speaker who has HIV/use of peer mentors Girls who are on the pill don’t think they need to use condoms - Provide counseling to all girls before they get the pill Perceived susceptibility Many girls use sex as a way of feeling loved/don’t want to upset the guy - Have group discussion/activity on self esteem; condom negotiation training Perceived barriers/self efficacy Girls learn negotiation skills in other areas + Role play on negotiating cost of purse/apply to condoms Self efficacy
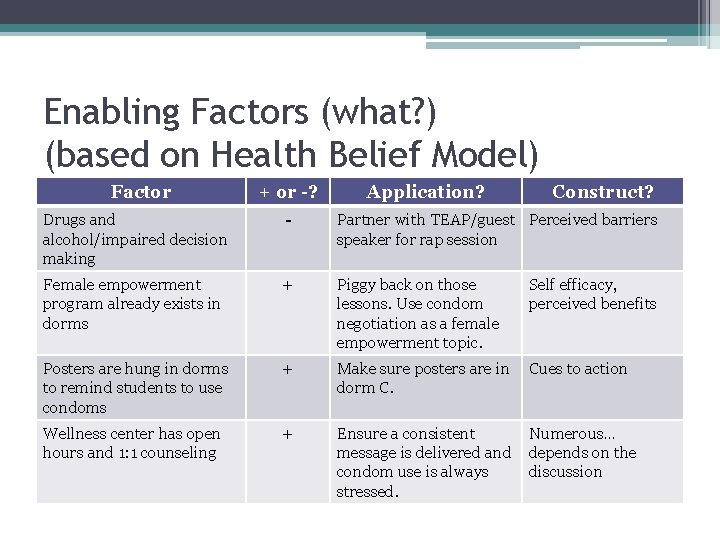
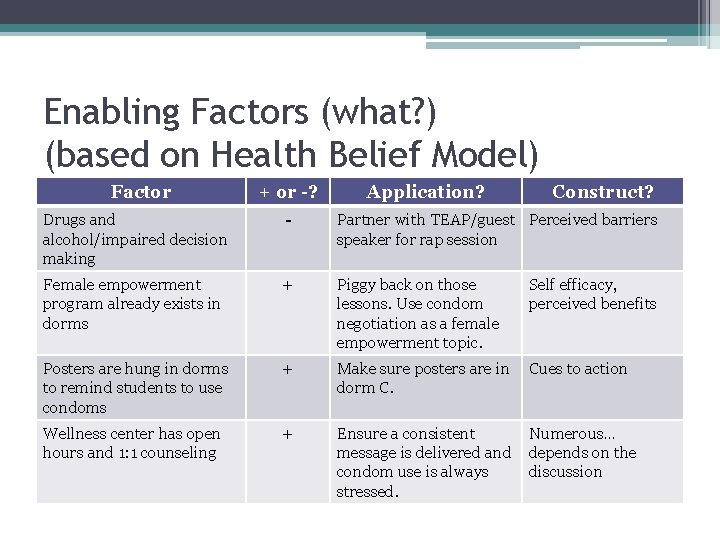
Enabling Factors (what? ) (based on Health Belief Model) Factor + or -? Application? Construct? Drugs and alcohol/impaired decision making - Partner with TEAP/guest Perceived barriers speaker for rap session Female empowerment program already exists in dorms + Piggy back on those lessons. Use condom negotiation as a female empowerment topic. Self efficacy, perceived benefits Posters are hung in dorms to remind students to use condoms + Make sure posters are in dorm C. Cues to action Wellness center has open hours and 1: 1 counseling + Ensure a consistent message is delivered and condom use is always stressed. Numerous… depends on the discussion
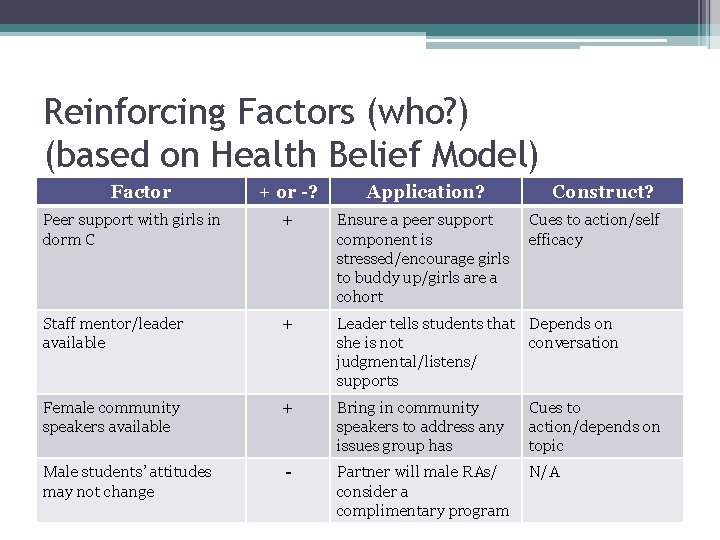
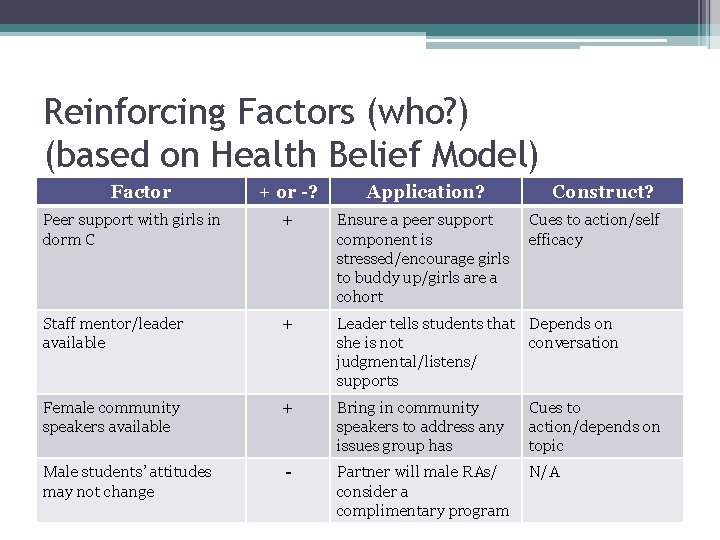
Reinforcing Factors (who? ) (based on Health Belief Model) Factor + or -? Application? Construct? Peer support with girls in dorm C + Ensure a peer support component is stressed/encourage girls to buddy up/girls are a cohort Staff mentor/leader available + Leader tells students that Depends on she is not conversation judgmental/listens/ supports Female community speakers available + Bring in community speakers to address any issues group has Cues to action/depends on topic Male students’ attitudes may not change - Partner will male RAs/ consider a complimentary program N/A Cues to action/self efficacy
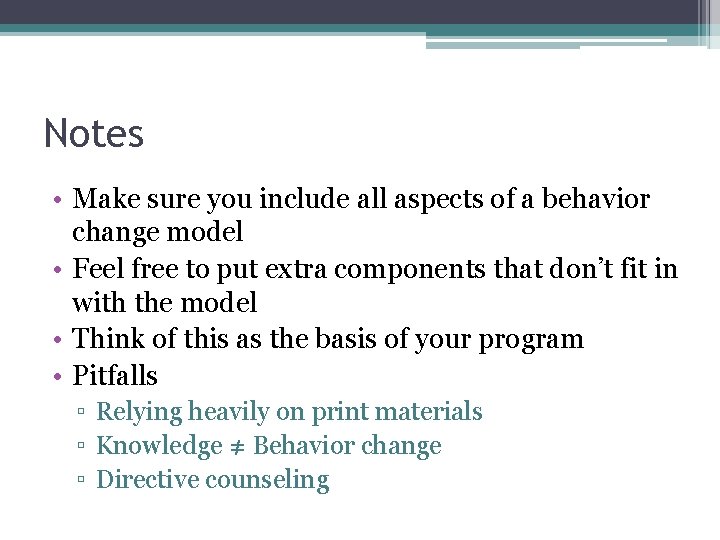
Notes • Make sure you include all aspects of a behavior change model • Feel free to put extra components that don’t fit in with the model • Think of this as the basis of your program • Pitfalls ▫ Relying heavily on print materials ▫ Knowledge ≠ Behavior change ▫ Directive counseling
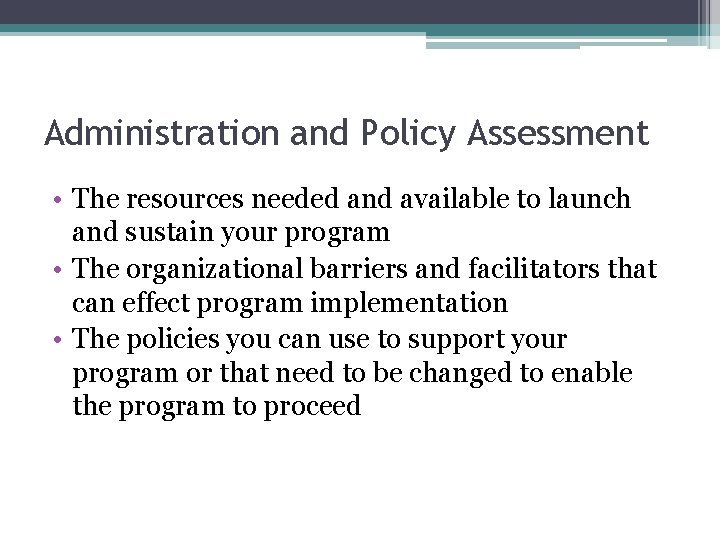
Administration and Policy Assessment • The resources needed and available to launch and sustain your program • The organizational barriers and facilitators that can effect program implementation • The policies you can use to support your program or that need to be changed to enable the program to proceed
JC’s No Sex Policy • What is the effect on STI rates? When would it be helpful and when harmful? • What is the effect of abstinence-only education? ▫ Lowest STI rate in 15 -24 y/o from states with no mandates for abstinence education ▫ States with mandates emphasizing abstinence had the highest rates ▫ States with mandates to cover (not emphasize) abstinence fell in the middle Source: Hogben, M. et al. (2010). Sexuality education policies and sexually transmitted disease rates in the USA. International Journal of STD and AIDS. 21; 293 -297.
Homework/Closing • Homework #3 due by COB on Friday • Three articles ▫ Condom Use with “Casual” and “Main” Partners: What’s in a Name? ▫ Effective Targeted and Community HIV/STD Prevention Programs (social norms/opinion leaders) ▫ Effective Approaches to Reducing Adolescent Unprotected Sex, Pregnancy, and Childbearing • Questions?