Planned Proactive Care Modified DCIP 2016 Date Created
- Slides: 9
Planned, Proactive Care Modified DCIP 2016 Date: Created by:
The Programs • • ARI & e. Shared Care Modified DCIP/DCIP Enhanced Primary Care CCM Depression Manaaki Hauora SMS Safety in Practice I & II Falls & Frail Elderly PHO programs
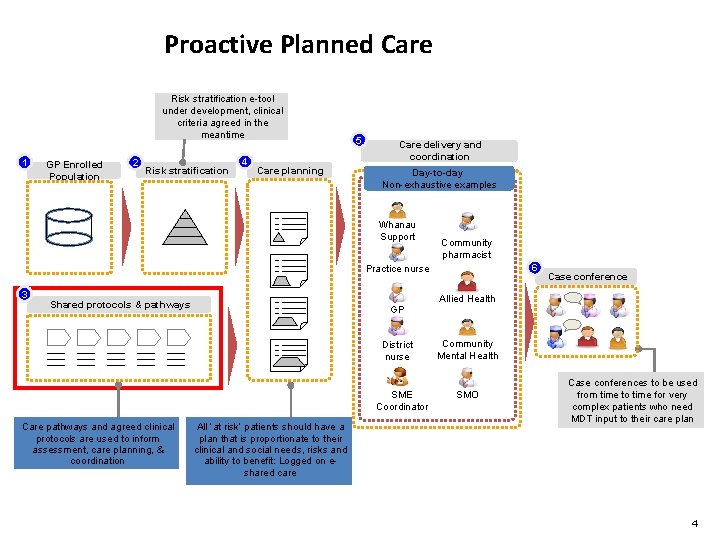
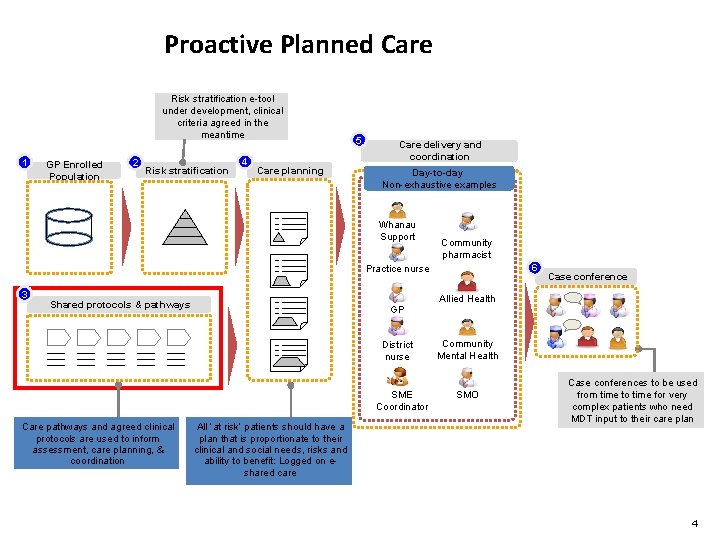
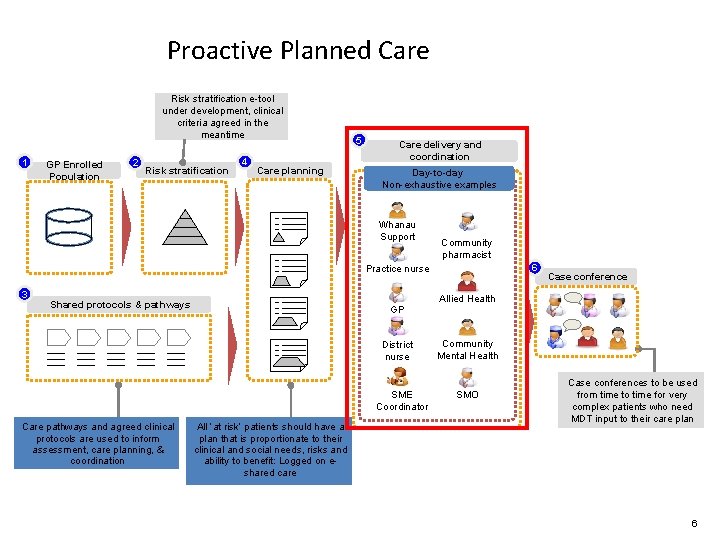
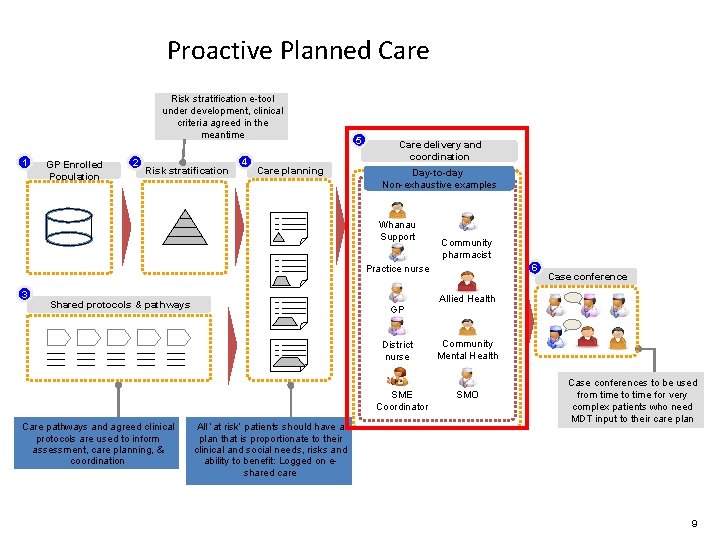
Proactive Planned Care Risk stratification e-tool under development, clinical criteria agreed in the meantime 1 GP Enrolled Population 2 Risk stratification 4 Care planning 5 Care delivery and coordination Day-to-day Non-exhaustive examples Whanau Support Community pharmacist 6 Practice nurse 3 Shared protocols & pathways GP District nurse SME Coordinator Care pathways and agreed clinical protocols are used to inform assessment, care planning, & coordination All ‘at risk’ patients should have a plan that is proportionate to their clinical and social needs, risks and ability to benefit: Logged on eshared care Case conference Allied Health Community Mental Health SMO Case conferences to be used from time to time for very complex patients who need MDT input to their care plan 4
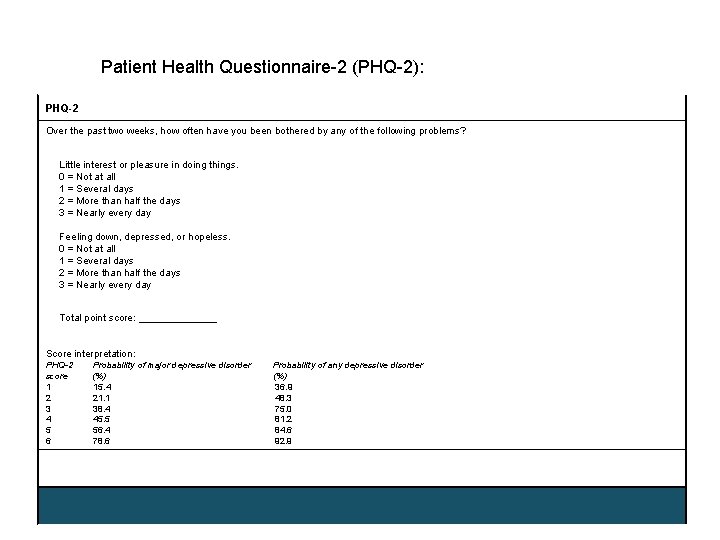
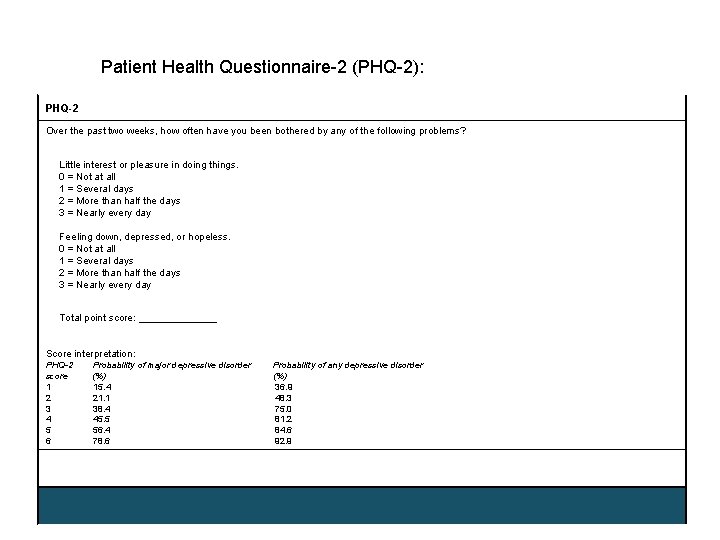
Patient Health Questionnaire-2 (PHQ-2): PHQ-2 Over the past two weeks, how often have you been bothered by any of the following problems? Little interest or pleasure in doing things. 0 = Not at all 1 = Several days 2 = More than half the days 3 = Nearly every day Feeling down, depressed, or hopeless. 0 = Not at all 1 = Several days 2 = More than half the days 3 = Nearly every day Total point score: _______ Score interpretation: PHQ-2 score 1 2 3 4 5 6 Probability of major depressive disorder (%) 15. 4 21. 1 38. 4 45. 5 56. 4 78. 6 Probability of any depressive disorder (%) 36. 9 48. 3 75. 0 81. 2 84. 6 92. 9
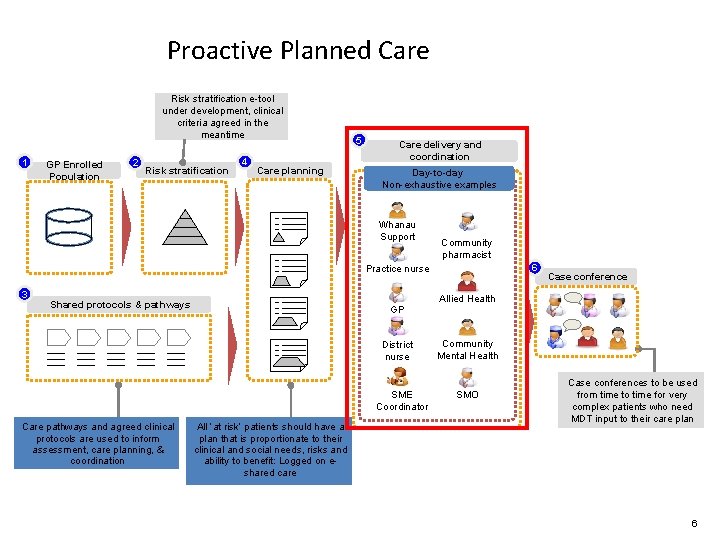
Proactive Planned Care Risk stratification e-tool under development, clinical criteria agreed in the meantime 1 GP Enrolled Population 2 Risk stratification 4 Care planning 5 Care delivery and coordination Day-to-day Non-exhaustive examples Whanau Support Community pharmacist 6 Practice nurse 3 Shared protocols & pathways GP District nurse SME Coordinator Care pathways and agreed clinical protocols are used to inform assessment, care planning, & coordination All ‘at risk’ patients should have a plan that is proportionate to their clinical and social needs, risks and ability to benefit: Logged on eshared care Case conference Allied Health Community Mental Health SMO Case conferences to be used from time to time for very complex patients who need MDT input to their care plan 6
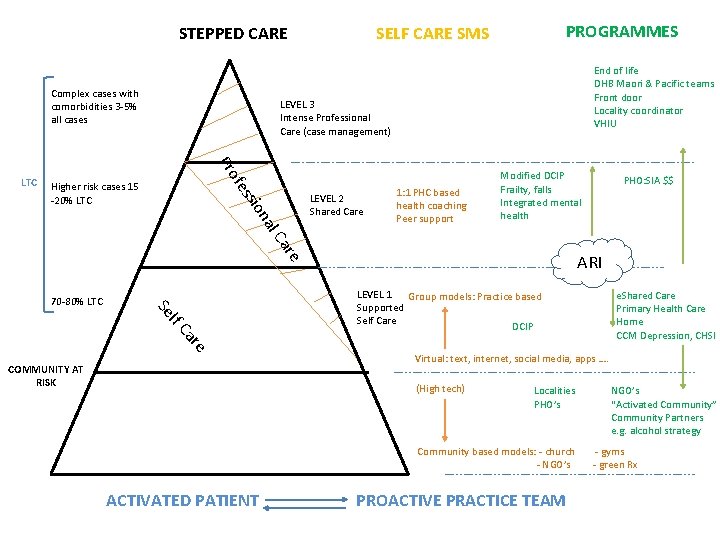
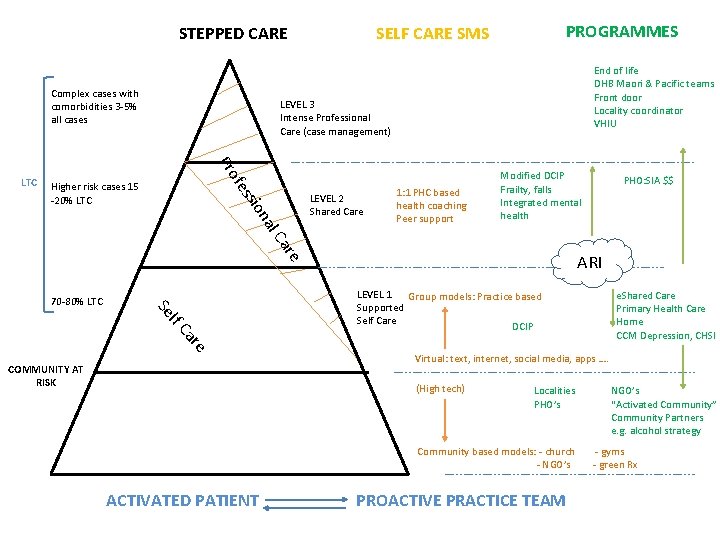
STEPPED CARE Complex cases with comorbidities 3 -5% all cases End of life DHB Maori & Pacific teams Front door Locality coordinator VHIU LEVEL 3 Intense Professional Care (case management) ssi ofe Pr LTC PROGRAMMES SELF CARE SMS Higher risk cases 15 -20% LTC al on LEVEL 2 Shared Care 1: 1 PHC based health coaching Peer support Modified DCIP Frailty, falls Integrated mental health re Ca lf Se 70 -80% LTC re Ca COMMUNITY AT RISK ARI LEVEL 1 Group models: Practice based Supported Self Care DCIP e. Shared Care Primary Health Care Home CCM Depression, CHSI Virtual: text, internet, social media, apps …. (High tech) Localities PHO’s Community based models: - church - NGO’s ACTIVATED PATIENT PHO: SIA $$ PROACTIVE PRACTICE TEAM NGO’s “Activated Community” Community Partners e. g. alcohol strategy - gyms - green Rx
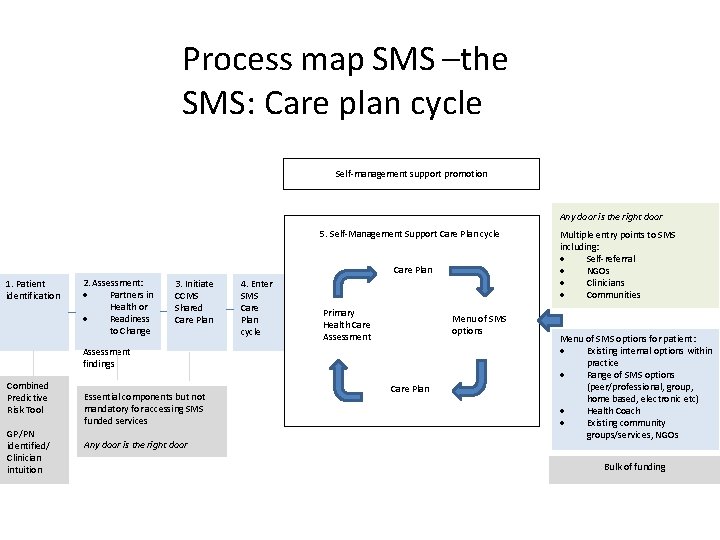
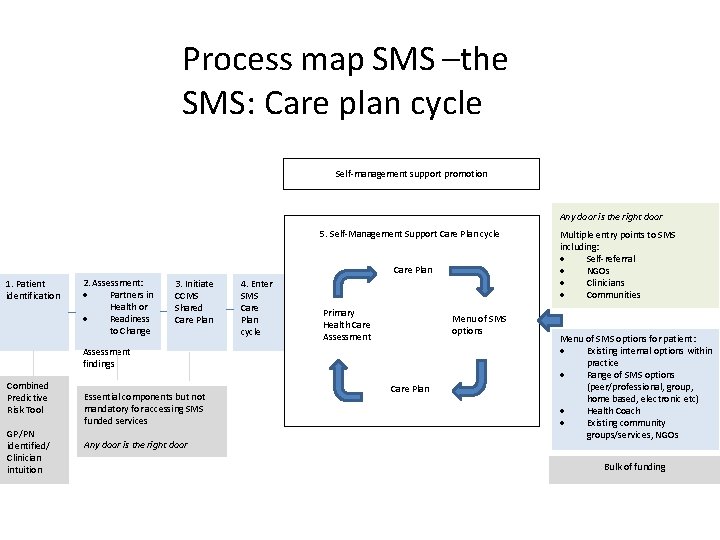
Process map SMS –the SMS: Care plan cycle Self-management support promotion Any door is the right door 5. Self-Management Support Care Plan cycle Care Plan 1. Patient identification 2. Assessment: Partners in Health or Readiness to Change 3. Initiate CCMS Shared Care Plan 4. Enter SMS Care Plan cycle Primary Health Care Assessment Menu of SMS options Assessment findings Combined Predictive Risk Tool GP/PN identified/ Clinician intuition Essential components but not mandatory for accessing SMS funded services Any door is the right door Care Plan Multiple entry points to SMS including: Self-referral NGOs Clinicians Communities Menu of SMS options for patient: Existing internal options within practice Range of SMS options (peer/professional, group, home based, electronic etc) Health Coach Existing community groups/services, NGOs Bulk of funding
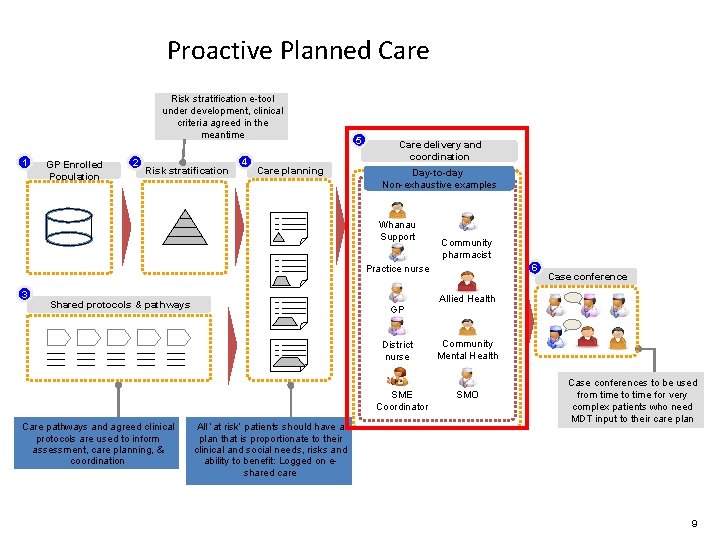
Proactive Planned Care Risk stratification e-tool under development, clinical criteria agreed in the meantime 1 GP Enrolled Population 2 Risk stratification 4 Care planning 5 Care delivery and coordination Day-to-day Non-exhaustive examples Whanau Support Community pharmacist 6 Practice nurse 3 Shared protocols & pathways GP District nurse SME Coordinator Care pathways and agreed clinical protocols are used to inform assessment, care planning, & coordination All ‘at risk’ patients should have a plan that is proportionate to their clinical and social needs, risks and ability to benefit: Logged on eshared care Case conference Allied Health Community Mental Health SMO Case conferences to be used from time to time for very complex patients who need MDT input to their care plan 9