PLAN Gallbladder Topography Segments Bile or gall path





PLAN Gallbladder Topography Segments Bile (or gall) path Extrahepatic bile ducts The common bile duct, types Innervation, blood supply Conclusion
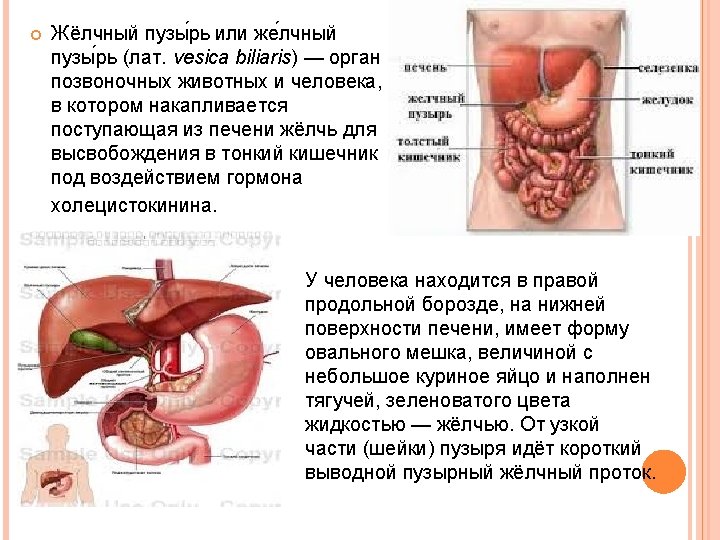
Gall bladder or gall bladder (lat. Vesica biliaris) - the body of vertebrate animals and humans, which builds coming from the liver to release bile into the small intestine under the influence of the hormone cholecystokinin. The man is in the right of the longitudinal groove on the bottom surface of the liver, has an oval shape of the bag, the size of a small hen's egg and filled with viscous, greenish liquid - bile. From the narrow part (neck) there is a short leadbladder cystic bile duct. At the transition to the neck of the bladder cystic bile duct sphincter located Lyutkensa regulating the flow of bile from the gallbladder into the cystic bile duct and back. The cystic bile duct in the liver is connected to the gate of hepatic duct. Through the merger of these two ducts forms the common bile duct, and then teaming up with the main pancreatic duct and through the sphincter of Oddi, which opens into the duodenum in the major duodenal papilla.
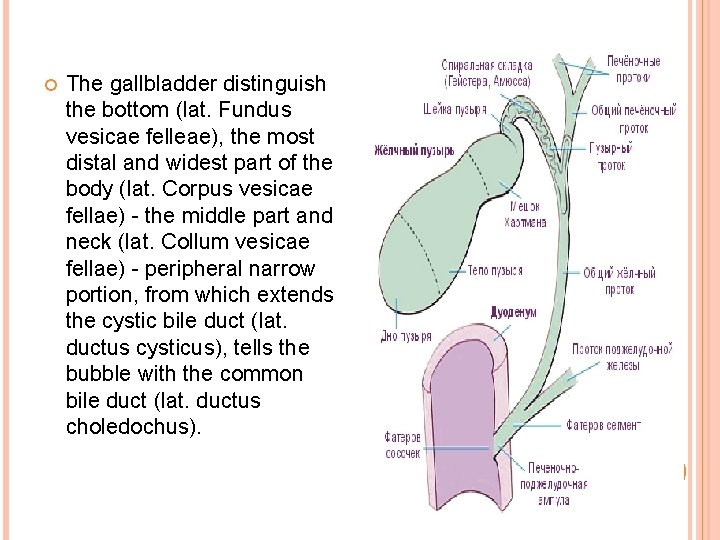
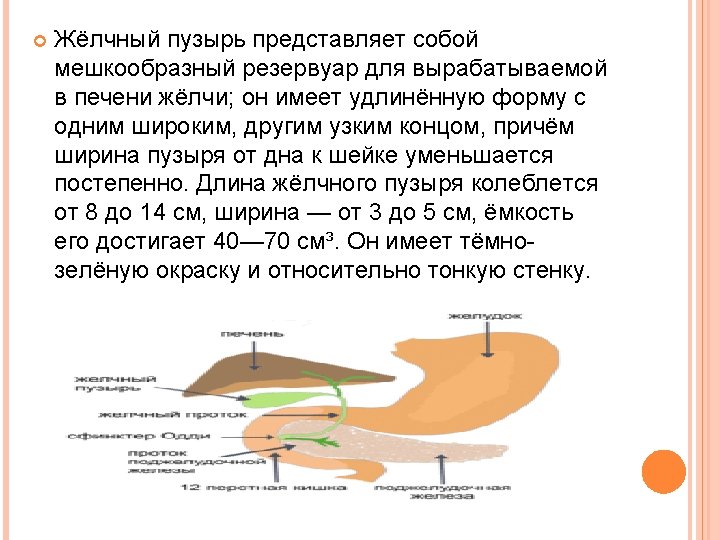
The gallbladder distinguish the bottom (lat. Fundus vesicae felleae), the most distal and widest part of the body (lat. Corpus vesicae fellae) - the middle part and neck (lat. Collum vesicae fellae) - peripheral narrow portion, from which extends the cystic bile duct (lat. ductus cysticus), tells the bubble with the common bile duct (lat. ductus choledochus).
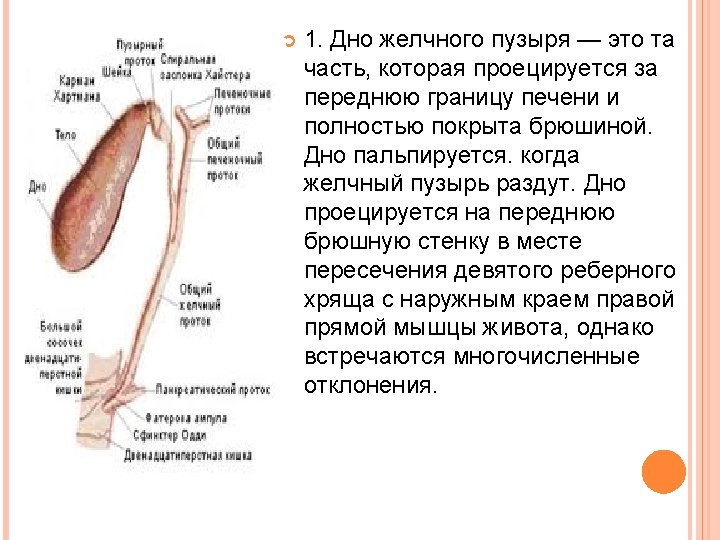
1. The bottom of the gallbladder - this is the part that is projected on the front border of the liver and is completely covered by peritoneum. Bottom palpable. when the gall bladder is inflated. The bottom is projected onto the anterior abdominal wall at the intersection of the ninth rib cartilage to the outer edge of the right rectus abdominis, but there are numerous deviations.
2. The body of the gallbladder located on the back and away from the bottom of its diameter progressively decreases. The body is covered with peritoneum not completely, it connects it with the lower surface of the liver. Thus, the lower surface is covered with gall bladder peritoneum, whereas the upper part is in contact with the lower surface of the liver, from which it is separated by a layer of loose connective tissue. Through it pass the blood and lymph vessels, nerves, and sometimes extra hepatic ducts. When cholecystectomy surgeon to divide the loose connective tissue, which will operate with minimal blood loss. At various pathological processes of the space between the liver and bladder obliterated. It is often injured liver parenchyma, which leads to bleeding. 3. Funnel - a third of the gall bladder, which follows the body. Its diameter is gradually reduced. This segment of the bladder is completely covered by peritoneum.
Gall bladder consists of a layer of high cylindrical epithelial cells, thin fibromuscular layer comprised of longitudinal, circular and oblique muscle fibers and fibrous tissue overlying the mucosa. The gall bladder has no submucosa and muscular-mucous membranes. It does not contain mucous glands (sometimes can present isolated mucous glands, which number increases slightly in inflammation, these mucous glands are located almost exclusively in the neck). Fibromuscular layer is covered with a layer of loose connective tissue, through which penetrate the blood, lymph vessels and nerves. To perform subserous cholecystectomy. you must find this a pad which is a continuation of the tissue that separates the gallbladder from the liver into the hepatic bed. Funnel goes into the neck length of 15 -20 mm, forming an acute angle, open up.
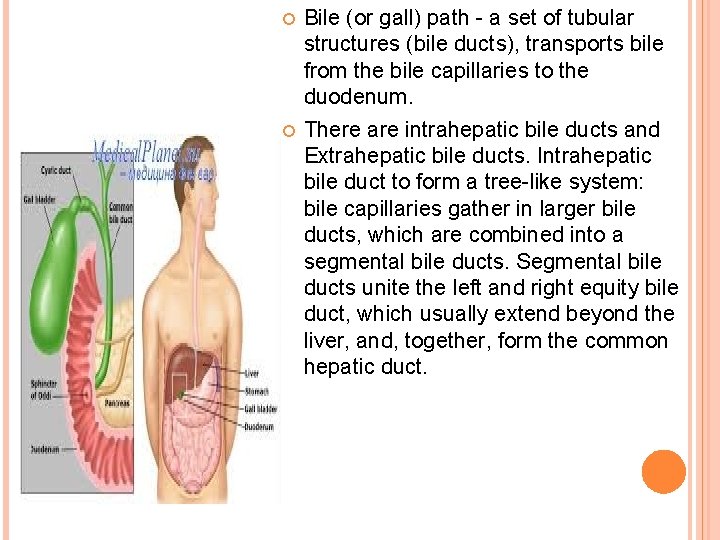
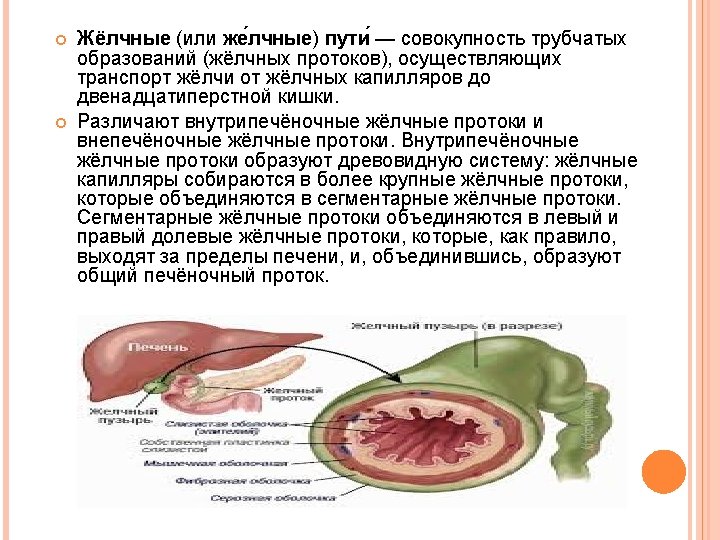
Bile (or gall) path - a set of tubular structures (bile ducts), transports bile from the bile capillaries to the duodenum. There are intrahepatic bile ducts and Extrahepatic bile ducts. Intrahepatic bile duct to form a tree-like system: bile capillaries gather in larger bile ducts, which are combined into a segmental bile ducts. Segmental bile ducts unite the left and right equity bile duct, which usually extend beyond the liver, and, together, form the common hepatic duct.
Extrahepatic bile ducts are three: the common hepatic duct, ductus hepaticus communis, cystic duct, ductus cysticus, and the common bile duct, ductus choledochus (biliaris). Common hepatic duct, ductus hepaticus communis, is formed in the gate of the liver as a result of the merger of the right and left hepatic ducts, ductus hepaticus dexter et sinister, past the same manner described above intrahepatic ducts, after a part of hepato-duodenal ligament, common hepatic duct connects with cystic duct coming from the gallbladder; thus arises the common bile duct, ductus choledochus. The cystic duct connects the gallbladder to the hepatic duct. When you merge it with the common hepatic duct forms the common bile duct. Cystic duct length of 4 -6 cm, sometimes it can reach 10 -12 cm. The flow can be short PLP completely absent. The proximal diameter is typically 2 -2. 5 mm, which is slightly less than its distal diameter, which is about 3 mm. Outside, it seems uneven and twisted, especially in the proximal half of the two-thirds of the PLP, because of the presence within the duct valves heister (Heister). Valves heister are crescent shaped and arranged in alternating sequence, which gives the impression of a continuous spiral. Actually, the valves are separated from each other. Heister valves regulate the flow of bile between the gallbladder and bile ducts. The cystic duct is usually connected to the hepatic duct at an acute angle in the upper half of the hepatic ligament, mostly on the right edge of the hepatic duct, forming a vesico-hepatic angle.
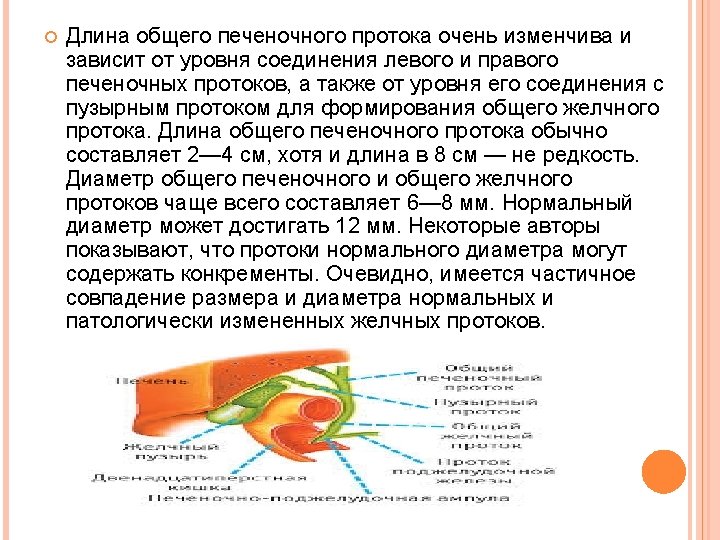
The cystic duct can enter the common bile duct perpendicularly. Sometimes it is parallel to the hepatic duct and is connected with it behind the initial portion of the duodenum, in the pancreas and even papillary PLP near it, forming a parallel connection. Sometimes it is connected to the hepatic duct in front of the PLP behind him, he enters the duct on the left side of PLP on the front wall. This rotation in relation to the hepatic duct was called spiral seam. Such fusion may cause liver syndrome Mirizzi. Occasionally the cystic duct empties into the right PLP left hepatic duct. Bile ducts originate in the liver as bile ducts and who get the bile secreted by liver cells. Interconnected, they form all channels of larger diameter forming the right and left hepatic ducts extending respectively from the right and left liver lobes. Typically, leaving the liver ducts are connected and form the common hepatic duct. Right hepatic duct is usually greater in the liver than the left.
The length of the common hepatic duct is very variable and depends on the level of the compound of left and right hepatic ducts, and the level of its connection to the cystic duct to form the common bile duct. The length of the common hepatic duct is generally 2 -4 cm, although the length is 8 cm - not uncommon. The diameter of the common hepatic and common bile ducts often is 6 -8 mm. Normal diameter up to 12 mm. Some authors suggest that the normal diameter ducts may contain concretions. Obviously, there is an overlap between the size and diameter of normal and pathological changes of the bile ducts.
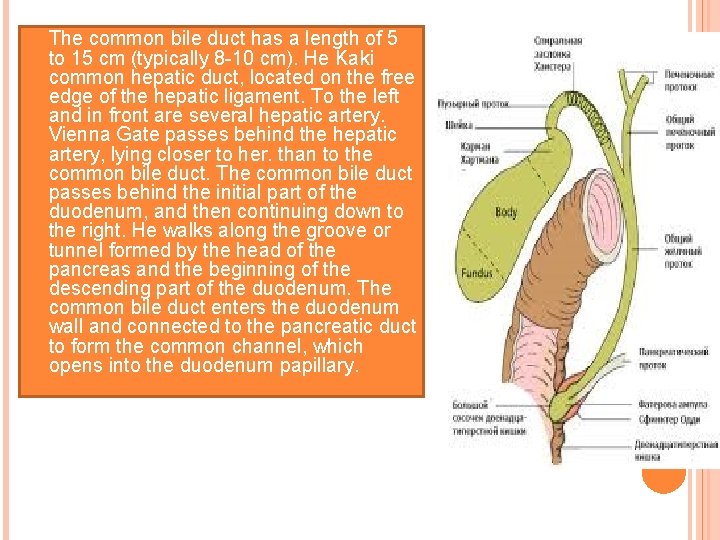
The common bile duct has a length of 5 to 15 cm (typically 8 -10 cm). He Kaki common hepatic duct, located on the free edge of the hepatic ligament. To the left and in front are several hepatic artery. Vienna Gate passes behind the hepatic artery, lying closer to her. than to the common bile duct. The common bile duct passes behind the initial part of the duodenum, and then continuing down to the right. He walks along the groove or tunnel formed by the head of the pancreas and the beginning of the descending part of the duodenum. The common bile duct enters the duodenum wall and connected to the pancreatic duct to form the common channel, which opens into the duodenum papillary.
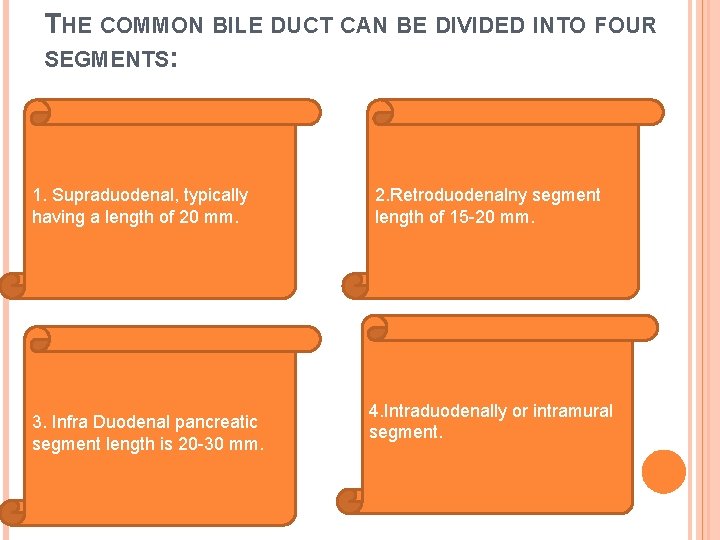
THE COMMON BILE DUCT CAN BE DIVIDED INTO FOUR SEGMENTS: 1. Supraduodenal, typically having a length of 20 mm. 3. Infra Duodenal pancreatic segment length is 20 -30 mm. 2. Retroduodenalny segment length of 15 -20 mm. 4. Intraduodenally or intramural segment.
There are three basic ways to connect the common bile and pancreatic ducts: 1. Most often, the common bile duct and pancreatic duct are joined shortly after penetration through the wall of the duodenum, forming a small common path. 2. Both streams run parallel but do not fall apart and are connected to a large duodenal papilla. Sometimes pancreatic duct may fall to 5 to 15 mm below the papilla. 3. The pancreatic duct and common bile duct are connected to a higher level in front of the wall of the duodenum, forming a long common channel. In rare cases, the compound of type 1 or 3 forms an extension called an ampoule.
The innervation of the liver, gall bladder and bile ducts - plexus hepaticus (truncus sympathicus, nn. Vagi). Blood supply: the liver - a. hepatica propria, and its branch a. cystica coming to the gallbladder and its ducts. In addition to the artery in the liver enters the gate v. portae, blood was collected from the unpaired organs in the abdominal cavity; passing system intraorgan veins, it leaves the liver through vv. hepaticae. flowing into the v. cava inferior. From the gallbladder and its ducts venous blood flowing into the portal vein. Lymph is removed from the liver and gall bladder in nodi lymphatici hepatici, phrenici superior et inferior, lumbales dextra, celiaci, gastrici, pylorici, pancreatoduodenales, anulus lymphaticus cardiae, parasternales.
CONCLUSION Guy de Chauliac (1300 -13681, a famous surgeon from Avignon (France), stated: "The good operation can not be performed without the knowledge of anatomy. " The knowledge of anatomy is very important in biliary tract surgery. Surgeons who operate on the biliary tract, faced with countless anatomical variants that are found at the gates of the liver and extrahepatic biliary structures. The surgeon should be familiar with the normal anatomy and common deviations. Before ligation and dissection of each anatomical structure must be carefully identified to avoid fatal consequences.
- Slides: 36