Pituitary Gland PITUITARY GLAND In the 16 th





- Slides: 29
Pituitary Gland
PITUITARY GLAND In the 16 th century, Vesalus named this endocrine gland ‘pituitary’, because ‘pituita’ meant phlegm or mucus. It was believed that the gland channeled mucus to the nose.

Why pituitary is called the master gland: • It is referred to as the master gland because it produces the tropic hormones, that controls the functions of other endocrine glands of the body(eg. TSH) and many other body functions, like it also stimulates growth. • The pituitary gland senses the body’s needs and sends signals to different organs and glands throughout the body to regulate their function and maintain an appropriate environment. • It secretes a variety of hormones into the bloodstream which act as messengers to transmit information from the pituitary gland to distant cells, regulating their activity. • Through secretion of its hormones, the gland controls metabolism, growth, sexual maturation, reproduction, blood pressure and many other vital physical functions and processes. in one word, it helps to maintain the overall homeostasis of the body.
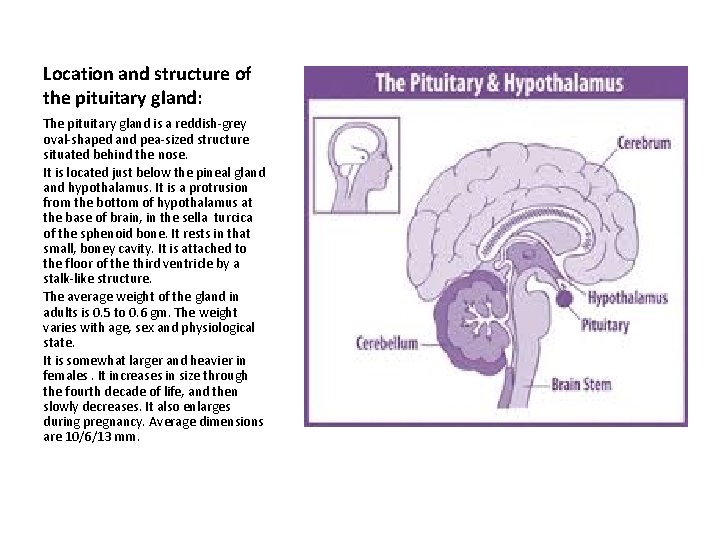
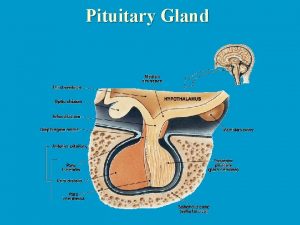
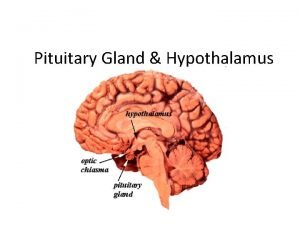
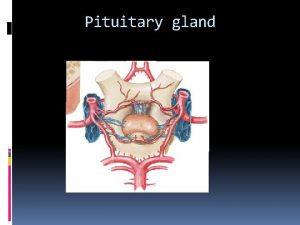
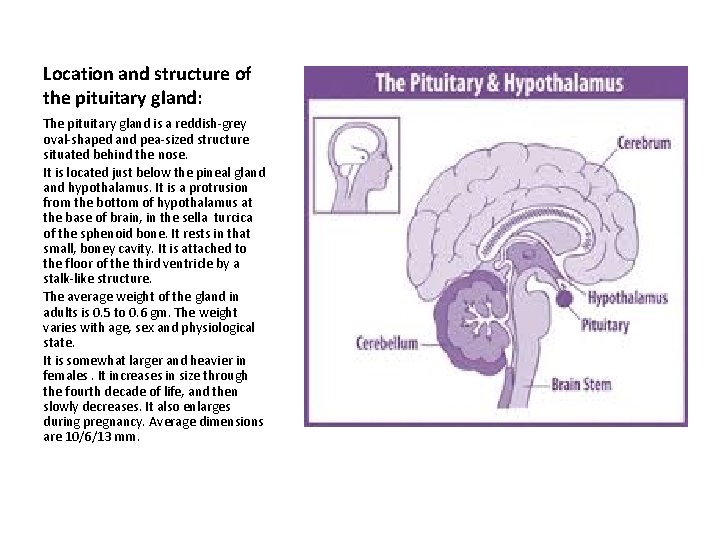
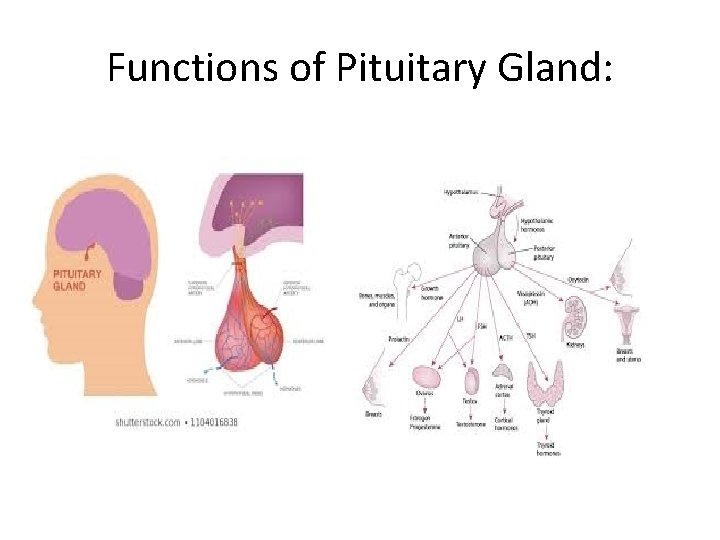
Location and structure of the pituitary gland: The pituitary gland is a reddish-grey oval-shaped and pea-sized structure situated behind the nose. It is located just below the pineal gland hypothalamus. It is a protrusion from the bottom of hypothalamus at the base of brain, in the sella turcica of the sphenoid bone. It rests in that small, boney cavity. It is attached to the floor of the third ventricle by a stalk-like structure. The average weight of the gland in adults is 0. 5 to 0. 6 gm. The weight varies with age, sex and physiological state. It is somewhat larger and heavier in females. It increases in size through the fourth decade of life, and then slowly decreases. It also enlarges during pregnancy. Average dimensions are 10/6/13 mm.
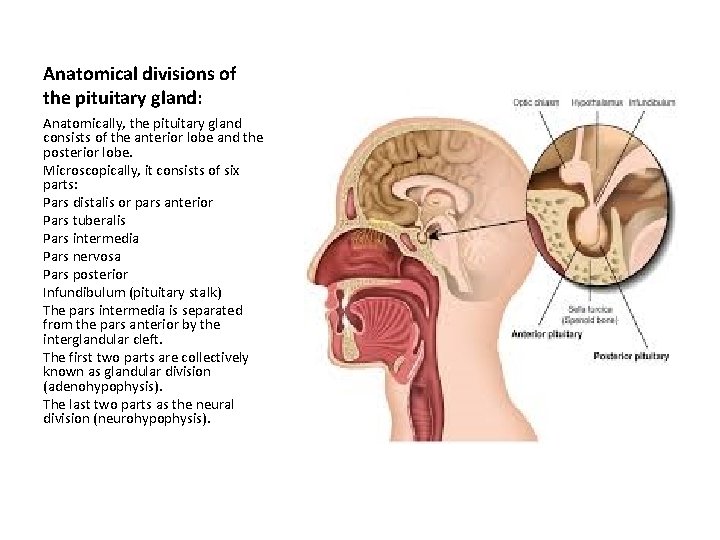
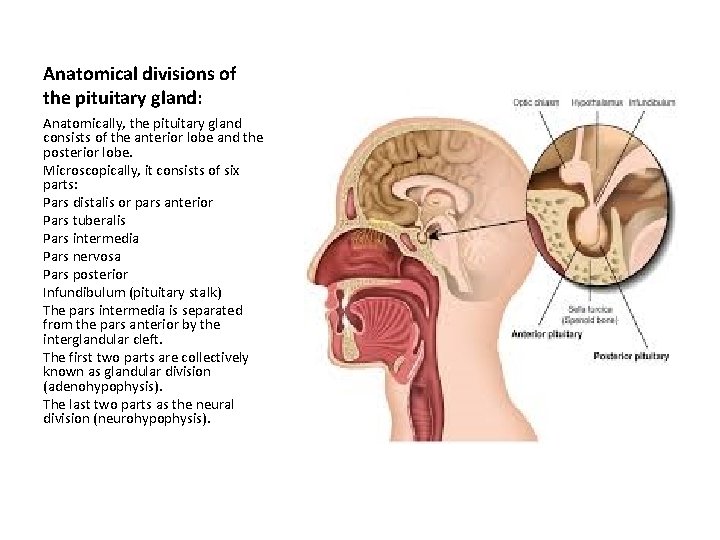
Anatomical divisions of the pituitary gland: Anatomically, the pituitary gland consists of the anterior lobe and the posterior lobe. Microscopically, it consists of six parts: Pars distalis or pars anterior Pars tuberalis Pars intermedia Pars nervosa Pars posterior Infundibulum (pituitary stalk) The pars intermedia is separated from the pars anterior by the interglandular cleft. The first two parts are collectively known as glandular division (adenohypophysis). The last two parts as the neural division (neurohypophysis).
Development of the pituitary gland: • • • The pituitary body develops from two outgrowths. The posterior lobe develops from a small outgrowth of hypothalamic tissue, while the anterior lobe develops from an outgrowth of the ‘Rathke’s Pouch’ or the embryonic tissue that eventually develops into the roof of the mouth. The Rathke’s pouch grows upwards from the primitive buccal cavity or ectoderm and meets with a similar neural downgrowth from the floor of the third ventricle. The stalk of the Rathke’s pouch disappears, but that of the neural downgrowth from the hypothalamus ( from which the pituitary gland develops) persists and forms the pituitary stalk or infundibulum. From the anterior wall of Rathke’s pouch develops the pars anterior. From the top arises the pars tuberalis. From the posterior wall develops the pars intermedia. The original cavity of the Rathke’s pouch forms the interglandular cleft. The anterior lobe consists of pars anterior and pars tuberalis. The posterior lobe consists of pars posterior and pars intermedia. These two lobes fuse during the course of embryological development to form the pituitary gland.
Anatomy of the anterior pituitary gland: • • The fleshy, glandular anterior pituitary is distinct from the neural composition of the posterior pituitary. The anterior pituitary begins as part of the same embryonic tissue (Rathke’s pouch) that eventually develops into the roof of the mouth. During the course of development, it pinches off and migrates upward to assume its position next to the posterior pituitary. Since it is actually the anterior pituitary that releases the tropic hormones, the anterior pituitary actually qualifies as the master gland. The anterior pituitary is composed of multiple parts: Pars distalis: This is the distal part that comprises the majority of the anterior pituitary; it is where most pituitary hormone production occurs. Pars tuberalis: This is the tubular part that forms a sheath that extends up from the pars distalis and wraps around the pituitary stalk. Its function is poorly understood. Pars intermedia: This is the intermediate part that sits between the pars distalis and the posterior pituitary and is often very small in humans.
Anatomy of the anterior pituitary gland: • • • • It consists of column or masses of epithelioid cells with numerous blood sinuses. Schonemann in 1982 first recorded the diversity of cell types in the anterior pituitary gland. The different pituitary hormones are liberated by separate cell types. Chromophobes: These are cells with minimal /no hormonal content. The chromophobes represent degranulated chromophils, which are of two typesacidophils and basophils. They have degranulated and thereby are depleted of hormone. Some chromophobes represent the stem cells that have not yet differentiated into hormone-producing cells. Acidophil cells: Cells contain polypeptide hormone: Somatotropes- producing growth hormone Lactotropes- producing prolactin Basophil cells: Cells containing glycoprotein hormones: Thyrotropes- producing TSH Gonadotropes- producing LH or FSH Corticotropes- producing ACTH
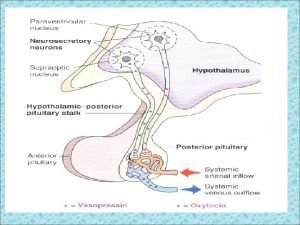
Anatomy of the posterior pituitary gland: • • Despite its name, the posterior pituitary gland is not a true gland; rather, it is largely a collection of axonal projections from the hypothalamus that terminate behind the anterior pituitary gland. It develops from a small outgrowth of hypothalamic tissue that eventually comes to dangle from the hypothalamus at the end of the pituitary stalk. The posterior pituitary consists mainly of neuronal projections ( axons ) extending from the supraoptic and paraventricular nuclei of the hypothalamus. These axons release peptide hormones into the capillaries of the hypophyseal circulation. These are then stored in neurosecretory vesicles (Herring bodies) before being secreted by the posterior pituitary into the systemic bloodstream. The posterior pituitary is derived from the hypothalamus and is distinct from the more fleshy, vascularized anterior lobe. The posterior pituitary is composed of two parts: The pars nervosa, also called the neural lobe or posterior lobe, constitutes the majority of the posterior pituitary and is the storage site of oxytocin and vasopressin. The infundibular stalk, also known as the infundibulum or pituitary stalk, bridges the hypothalamic and hypophyseal systems.
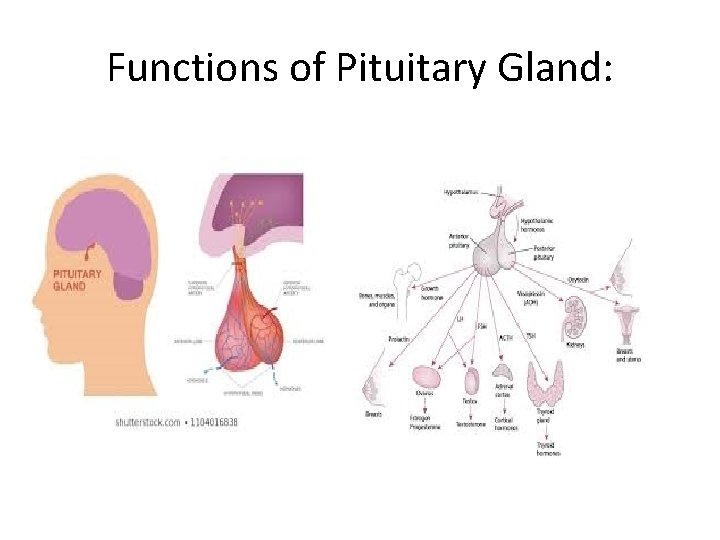
Functions of Pituitary Gland:
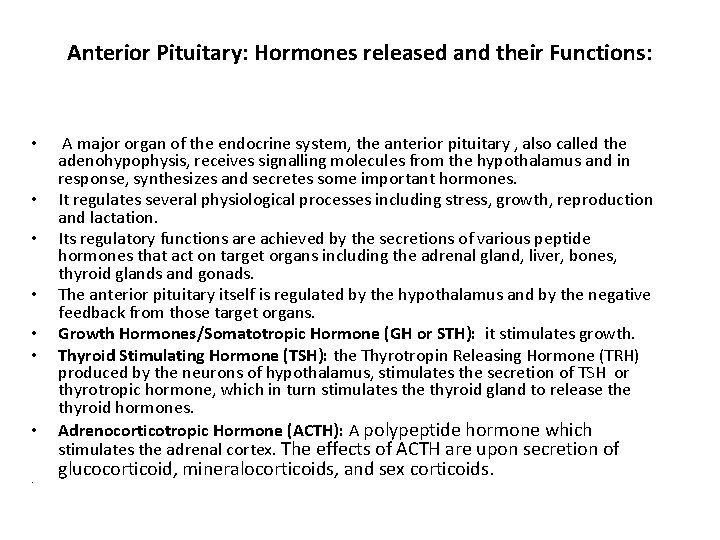
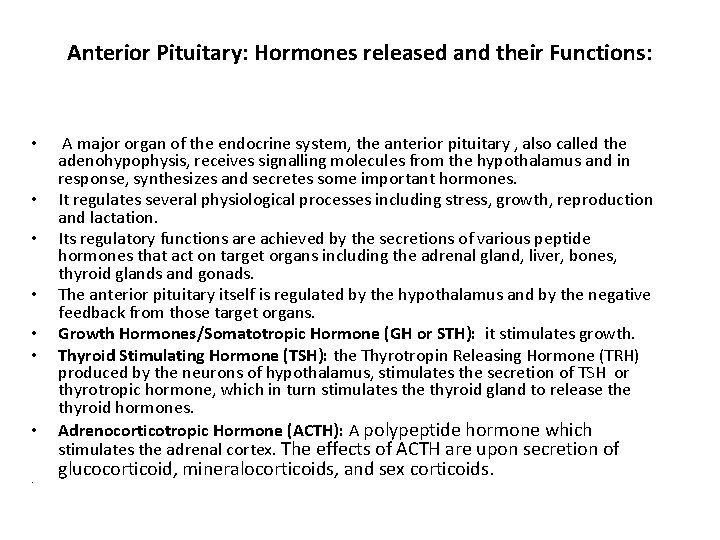
Anterior Pituitary: Hormones released and their Functions: • • A major organ of the endocrine system, the anterior pituitary , also called the adenohypophysis, receives signalling molecules from the hypothalamus and in response, synthesizes and secretes some important hormones. It regulates several physiological processes including stress, growth, reproduction and lactation. Its regulatory functions are achieved by the secretions of various peptide hormones that act on target organs including the adrenal gland, liver, bones, thyroid glands and gonads. The anterior pituitary itself is regulated by the hypothalamus and by the negative feedback from those target organs. Growth Hormones/Somatotropic Hormone (GH or STH): it stimulates growth. Thyroid Stimulating Hormone (TSH): the Thyrotropin Releasing Hormone (TRH) produced by the neurons of hypothalamus, stimulates the secretion of TSH or thyrotropic hormone, which in turn stimulates the thyroid gland to release thyroid hormones. Adrenocorticotropic Hormone (ACTH): A polypeptide hormone which stimulates the adrenal cortex. The effects of ACTH are upon secretion of glucocorticoid, mineralocorticoids, and sex corticoids.

Anterior Pituitary: Hormones released and their Functions: • • Prolactin: TRH also stimulates the release of prolactin from anterior pituitary, which facilitates milk production in the lactating mother. Endorphins: They consist of a large group of peptides. The word endorphin comes from the words “endogenous, ” meaning from within the body, and “morphine, ” which is an opiate pain reliever. In other words, endorphins got their name because they are natural pain relievers. Since endorphins act on the opiate receptors in our brains, they reduce pain and boost pleasure, resulting in a feeling of well-being. Endorphins are released in response to pain or stress, but they’re also released during other activities, like eating, exercise, or sex. Gonadotropins: Gonadotropin-releasing Hormone (Gn. RH), a peptide hormone synthesized and released from the Gn. RH neurons of the hypothalamus, is responsible for the synthesis and release of the gonadotropic hormones, or gonadotropins, that regulate the gametogenic and the steroidogenic functions of the male and female. In other words, they act on the gonads (testes and ovaries) to increase the production of the sex hormones and stimulate the production of the germ cells, either sperm or ova. Follicle Stimulating Hormone(FSH) and the Luteinizing Hormone (LH) are the main gonadotropins. Human Chorionic Gonadotropin is a gonadotropin that is only produced during pregnancy by the placenta.
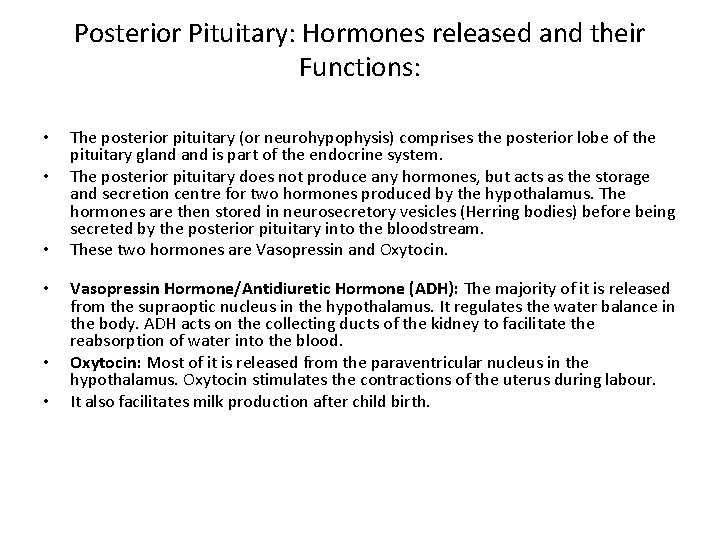
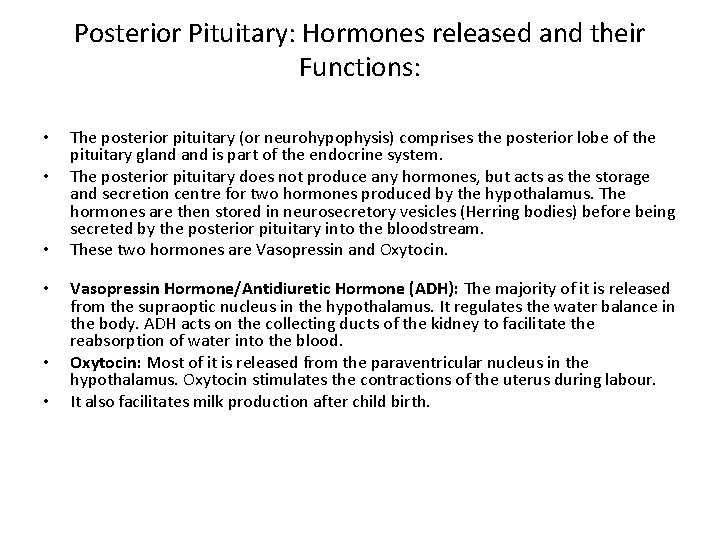
Posterior Pituitary: Hormones released and their Functions: • • • The posterior pituitary (or neurohypophysis) comprises the posterior lobe of the pituitary gland is part of the endocrine system. The posterior pituitary does not produce any hormones, but acts as the storage and secretion centre for two hormones produced by the hypothalamus. The hormones are then stored in neurosecretory vesicles (Herring bodies) before being secreted by the posterior pituitary into the bloodstream. These two hormones are Vasopressin and Oxytocin. Vasopressin Hormone/Antidiuretic Hormone (ADH): The majority of it is released from the supraoptic nucleus in the hypothalamus. It regulates the water balance in the body. ADH acts on the collecting ducts of the kidney to facilitate the reabsorption of water into the blood. Oxytocin: Most of it is released from the paraventricular nucleus in the hypothalamus. Oxytocin stimulates the contractions of the uterus during labour. It also facilitates milk production after child birth.
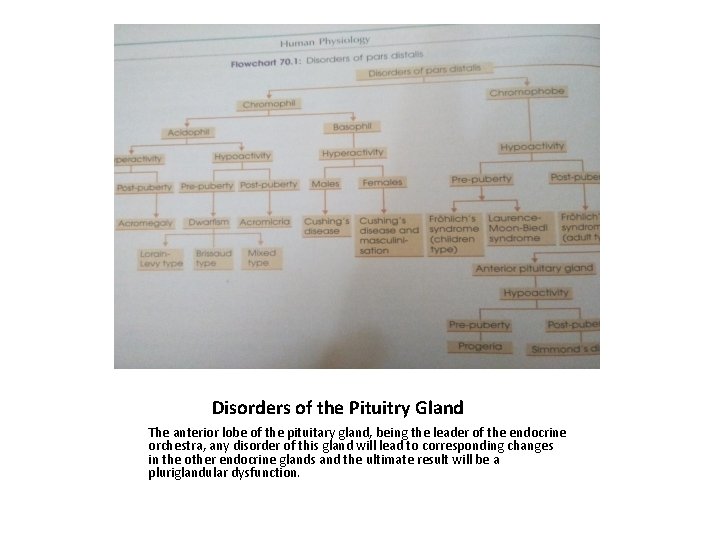
Clinical manifestations of pituitary gland disorders: • • • Lesions of the pituitary gland may affect the: Acidophil cells Basophil cells Chromophobe cells Total gland Lesions may be of two types: Hyperactive: this includes tumours, irritation, etc. Tumour of a particular type of cell will cause the signs of hyperactivity of those cells, as well as hyperactivity of other neighbouring cells (due to irritation). A hyperactive condition or hyperpituitarism may ultimately end in corresponding hypoactive state, possibly due to exhaustion and degeneration. Hypoactive (degenerative): this includes the signs of degeneration due to pressure.
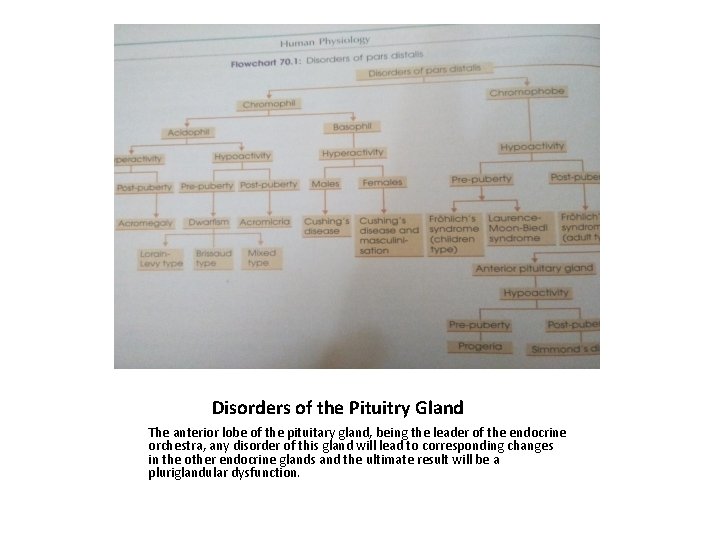
Disorders of the Pituitry Gland The anterior lobe of the pituitary gland, being the leader of the endocrine orchestra, any disorder of this gland will lead to corresponding changes in the other endocrine glands and the ultimate result will be a pluriglandular dysfunction.
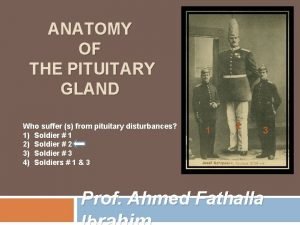
Dysfunction of Acidophil Cells: • Hyperpituitarism: • This condition usually stems from an acidophil tumour. • In the young it increases skeletal growth producing Gigantism. • Hyperpituitarism in adults leads to Acromegaly. • Hypopituitarism: • It stems from atrophy or ill-development of acidophil cells. • It produces Dwarfism in young children. • In adults this condition produces Acromicria.

Features of Acromegaly: • Skeleton: the skeletal changes lead to a gorilla-like appearance of the patient. • There is an overgrowth of the two jaws, the malar bones, the supraorbital ridges, etc. • Enlargement of hands and feet (acral parts). • There is bowing of the spine (kyphosis). • The anteroposterior diameter of the chest is increased. • Subcutaneous tissues: the subcutaneous tissues of the hand, feet, scalp, nose and lips and the skin, increase in amount, producing deep furrows. • The tongue is also enlarged. • Metabolism: blood sugar level increases leading to hyperglycaemia. • There is reduced sugar tolerance and there may be glycosuria (due to over secretion of STH and ACTH). • There is also increased BMR and increased levels of sweating.

Features of Acromegaly: • • • Viscera: the organs concerned with metabolism are all enlarged, such as heart, lungs, liver, kidneys, pancreas, spleen. etc. Other endocrine glands: Thyroid: it is enlarged and hyperactive, and may cause Grave’s Disease. Adrenal Cortex: It becomes enlarged and hyperactive. Thymus: it is enlarged. Reproductive functions: the gonads may be initially hyperactive and later there may be atrophy, due to overwork and exhaustion. Almost all patients have increased production of lactogenic hormones. In males there may be diminished libido and sometimes impotency. In females there may be sterility, menstrual disturbances, lack of breast development and persistent lactation (lactorrhoea). Some other manifestations: Lantern jaw, papilloedema, rhinorrhoea, deepening of voice, visual disturbances, drowsiness and lethargy, complete amenorrhoea, cutaneous pigmentation, concomitant presence of hypertension.
Features of Gigantism: • Skeleton: increased skeletal growth produces unusually tall structures(upto 7 or 8 feet). • The muscles and viscera: they are also proportionately large in size. • Metabolism: there may be reduced sugar tolerance with hyperglycaemia, and glycosuria (due to oversecretion of STH and ACTH). • There is increased BMR and increased levels of sweating. • Changes in other glands: as seen in Acromegaly.
Features of Acromicria : • It is caused by the hypoactivity of the acidophil cells in the adult. • It is antithesis of acromegaly. • It is a very rare clinical condition. • The bones of the face, hands and feet are small. • There is loss of hair. • Loss of sexual functions.
Features of the three types of Dwarfism: • • • • 1. Lorain-Levy Type (Infantilism)- Features: Stunted growth(about 3 feet in adults). Lack of growth of sex organs and secondary sexual characteristics, whereby an adult male resembles a normal child. Intelligence is normal and age-proportional. Metabolism is normal. 2. Bissaud Type (Fat Body of Dickens)- Features: Same characteristic features as the Lorain-Levy Type. In addition, there is excessive fat deposition in the body. Round and chubby face. No beard or moustache. Sleepy and sloth-like nature. 3. Mixed Type/ Dyspituitarism- Features: The patient may be fat and hairless, have large accessory nasal sinuses, prominent supraorbital ridges and some other traits of Acromegaly. In some, dysfunction of acidophil cells may develop pressure symptoms on neighbouring structures. Such patients resemble patients of hypopituitarism, with acromegaly, or gigantism.
Dysfunction of Basophil Cells: • • • • Hyperactivity lesion: In Males: Cushing’s Disease In Females: Cushing’s Disease and Masculinisation Cushing’s disease or pituitary basophilism, is a disease founded by and named after, Harvey Cushing in 1932. It is the basophil adenoma of the pituitary gland is a primary pituitary tumour. Similar clinical changes found in adrenal tumour is called Cushing’s Syndrome. Women are affected four times more than men. Features: The signs of hyperactivity develop in this disease due to mechanical pressure on the active cells. There is excessive fat deposition over the supracondylar fossae, face ( rounded or moon face), back of the neck and abdomen. Extremities are usually spared. Fatty deposits are tender and painful. Purplish striae are found over the abdomen, thighs, etc. , due to loss of protein matrix.
Clinical signs and symptoms of Cushing’s Disease: • • • • Masculinisation, with growth of beard and moustache, etc. Asthenia and wasting of the muscles of the limbs. Obesity of the trunk but not of the limbs. In males, there is excessive hair growth (hirsutism). Osteoporosis of bones due to decalcification and loss of protein matrix. Hypertension in a few patients. Mental derangement. In males, impotence with testes atrophy. In females, amenorrhoea, sterility, etc. Hyperglycaemia and glycosuria. Retention of sodium and diminution of potassium level in the plasma. Eosinopenia, lymphocytopenia and polycythaemia. Increased excretion of 17 -oxogenic steroids and 17 -hyroxycorticosteroids.
Dysfunction of the Chromophobe Cells: • It is caused by a tumour of the inactive chromophobe cells. • Mechanical pressure on active cells produces signs of both irritation and hypoactivity. • Hence, the following effects are observed in patients: • In children: • 1. Frohlich’s Syndrome (adiposogenital dystrophy): • Stunted growth (dwarfism). • Idiotic expressions. • Sexual infantilism. • Generalized obesity. • 2. Laurence-Moon-Biedl Syndrome (often familial): • This is same as Frohlich’s Syndrome (children type). • In addition, the patients have polydactylism and retinitis pigmentosa.
Clinical Features of Frohlich’s Syndrome- Adult Type: In Males: Adiposity of feminine distribution. Mental disposition and appearance resemble females. Degeneration of sex. Hands and feet are small and pretty, fingers are delicate and tapering. • Skin of face and body are smooth and hairless. • • • In Females: • Extreme adiposity. • Degeneration of sex.
Dysfunction of total gland: • • • Hyperactivity: Not known as pure clinical type. Often appears in mixed form. Hypoactivity: (degenerative changes). In Children: Progeria In Adults: Simmond’s disease. • Progeria: • Progeria, also known as Hutchinson-Gilford syndrome, it is an extremely rare disorder, marked by appearance of early senility. • Children generally appear normal at birth, but they age rapidly, starting in their first two years of life. • The symptoms are often seen in pituitary dwarfs.
Clinical signs and symptoms of Progeria: • • • • • Generally appear normal at birth. Slowed growth, with below average height and weight. Narrowed face, small lower jaw, thin lips, beaked nose. Loss of fat under skin and loss of muscle mass. Skeletal abnormalities and fragile bones. Delayed and abnormal tooth formation. Stiff joints. Insulin resistance. Increased risk of CVD. Chances of hearing loss. Head disproportionately large for the face. Prominent eyes and incomplete closure of eyelids. Hair loss, including loss of eyelashes and eyebrows. Thinning, spotty, wrinkled skin. Hardening and tightening of skin on the trunk and extremities. Visible veins. High –pitched voice.

Clinical signs and symptoms of Simmond’s Disease: • It is due to degeneration of the anterior lobe of the pituitary. • There is loss of weight and shrunken appearance (cachexia). • Sexual degeneration: amenorrhoea, sterility, loss of axillary and pubic hairs, impotency (in males), etc. • Asthenia: extreme weakness. • Anorexia: loss of appetite. • Low BMR. • Mental deterioration. • Atrophy of viscera: gonads, thyroid, adrenal cortex, etc. degenerate. • Anaemia. • Hypoglycaemia. • Diminished urinary excretion of 11 -oxycorticoids. 17 -oxogenic steroids and gonadotrophins. • PBI in the blood falls.
Role of the hypothalamus in controlling the actions of the pituitary gland: • • The hypothalamus controls the activity of the pituitary gland through individual releasing factors corresponding to different tropic hormones. There are RF for gonadotropins along with TRF and CRF. The hormones of the endocrine gland have inhibitory influence over both the anterior pituitary and hypothalamus in releasing the pituitary tropic hormones and hypothalamic releasing substances respectively. Thus, under normal conditions, a perfect optimal endocrine balance is maintained in the body. Commonly, tissue content of a hormone or hormone level in circulation maintains a balance between rates of synthesis and release of the hormone. Decrease in circulatory hormone levels will influence the hypothalamic nucleus to secrete releasing factor and vice versa. An increase in hypothalamic content of releasing factor represents increased synthesis and secretion of the corresponding tropic hormone in the anterior pituitary. This hormone, via circulation, influences the target gland.
 Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual Pineal gland pituitary gland
Pineal gland pituitary gland Hypophyseal fossa and pituitary gland
Hypophyseal fossa and pituitary gland Embryonic development of pituitary gland
Embryonic development of pituitary gland Dictalie
Dictalie Anterior pituitary gland
Anterior pituitary gland Hypersecretion of prolactin
Hypersecretion of prolactin Venous drainage of pituitary gland
Venous drainage of pituitary gland Hypothalamus and pituitary gland connection
Hypothalamus and pituitary gland connection Development of tongue
Development of tongue Pituitary gland hormones
Pituitary gland hormones Diaphragma sellae
Diaphragma sellae Hypothalamus
Hypothalamus Origin of posterior pituitary gland
Origin of posterior pituitary gland Dwrfism
Dwrfism Pituitary gland division
Pituitary gland division Human body organ systems
Human body organ systems Gland
Gland Exocrine glands function
Exocrine glands function What is the name
What is the name Pituitary gland disorders
Pituitary gland disorders Pituitary gland
Pituitary gland Blood supply of pituitary gland
Blood supply of pituitary gland Nerve supply to pituitary gland
Nerve supply to pituitary gland N
N Hashitoxicosis
Hashitoxicosis Hypophyseal fossa and pituitary gland
Hypophyseal fossa and pituitary gland Endocrine histology
Endocrine histology Hyposecretion of prolactin
Hyposecretion of prolactin Where is kidney pain felt diagram
Where is kidney pain felt diagram