Pithed rat simulation Anaesthetized cat simulation Experiment I

- Slides: 53
大綱 實驗一:Pithed rat simulation 實驗二:Anaesthetized cat simulation 骨骼肌及心血管系統概述
Experiment I Pithed Rat Simulation
Introduction & aim Rat. CVS is a simulation of a pithed rat experimental preparation for investigating the actions of drugs on the heart and cardiovascular system. "Pithing" refers to the destruction of spinal cord pathways, severing all the nerve connections between the brain and the cardiovascular system. This greatly simplifies the interpretation of experimental results by removing the central baroreceptor reflexes. Rat. CVS allows you to observe the pharmacological effects of a variety of different drugs on the cardiovascular system by displaying the traces of blood pressure, left ventricular pressure, venous pressure, heart rate and contractile force on a simulated chart recorder.
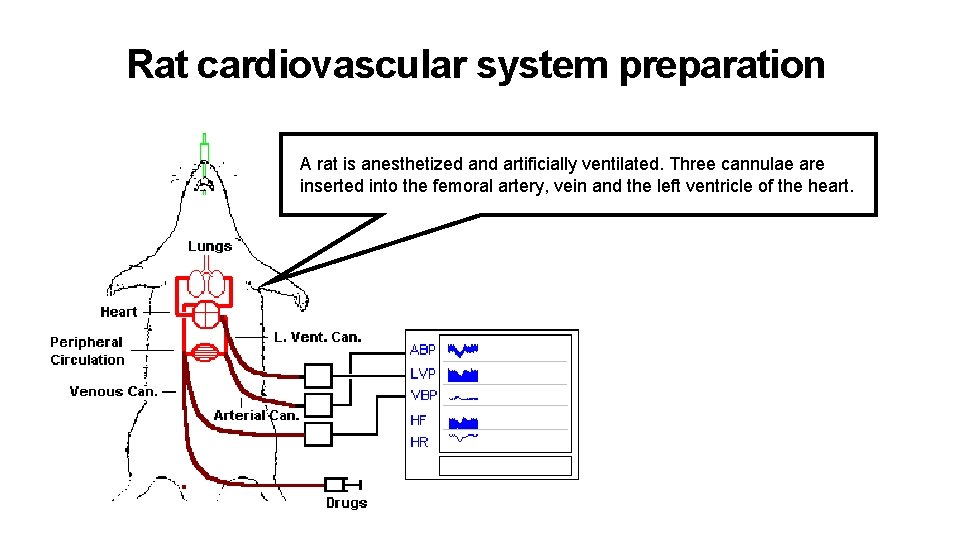
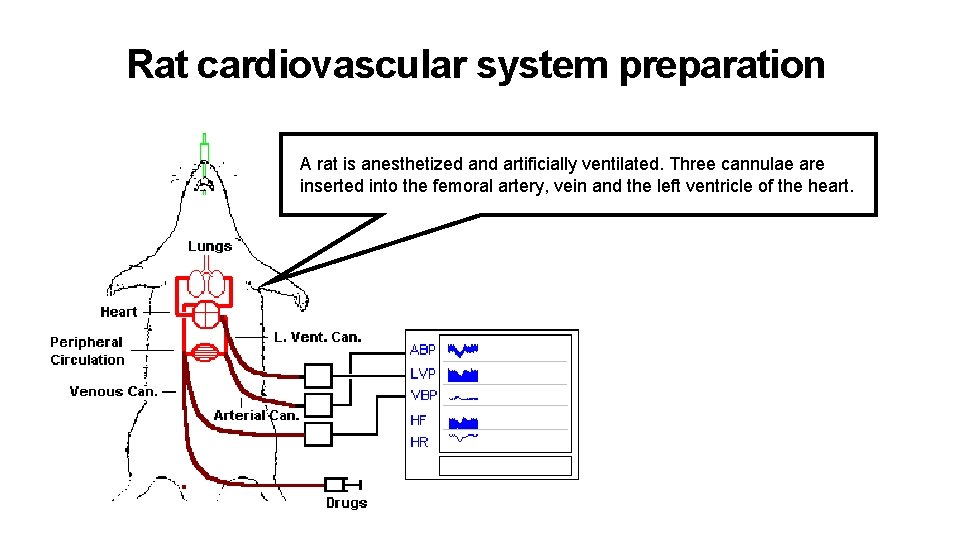
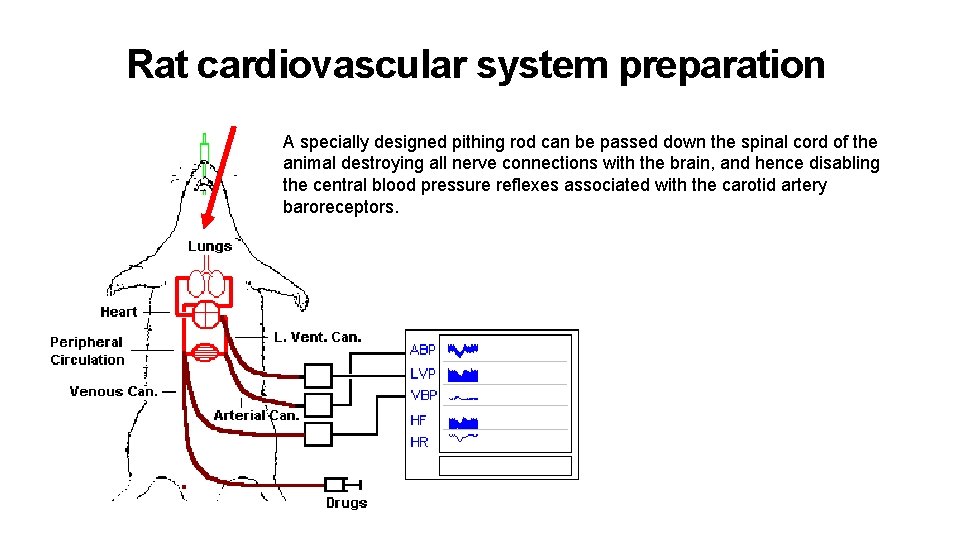
Rat cardiovascular system preparation A rat is anesthetized and artificially ventilated. Three cannulae are inserted into the femoral artery, vein and the left ventricle of the heart.
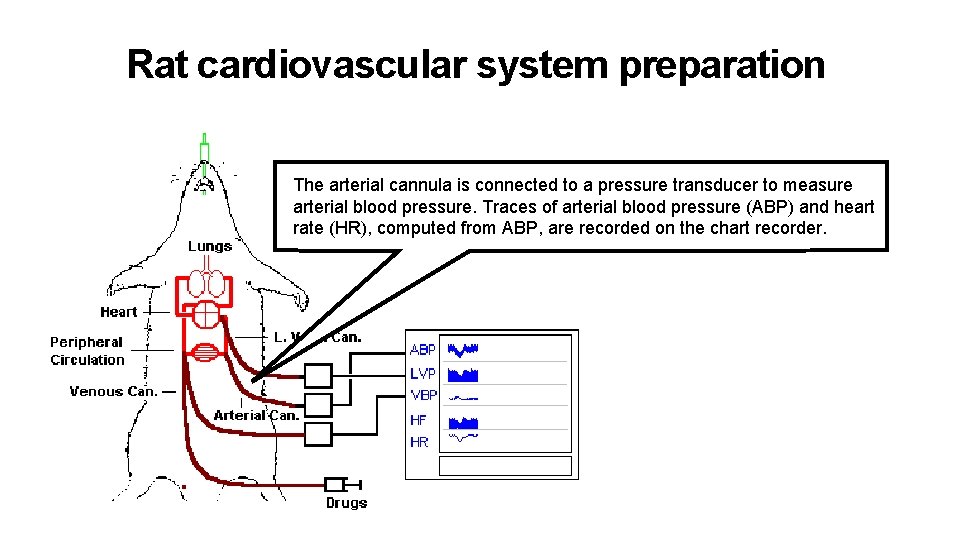
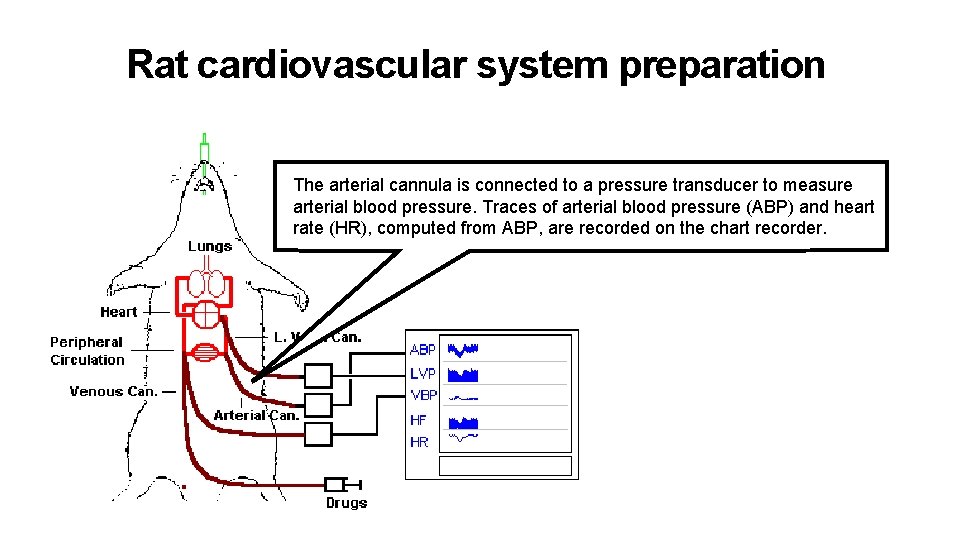
Rat cardiovascular system preparation The arterial cannula is connected to a pressure transducer to measure arterial blood pressure. Traces of arterial blood pressure (ABP) and heart rate (HR), computed from ABP, are recorded on the chart recorder.
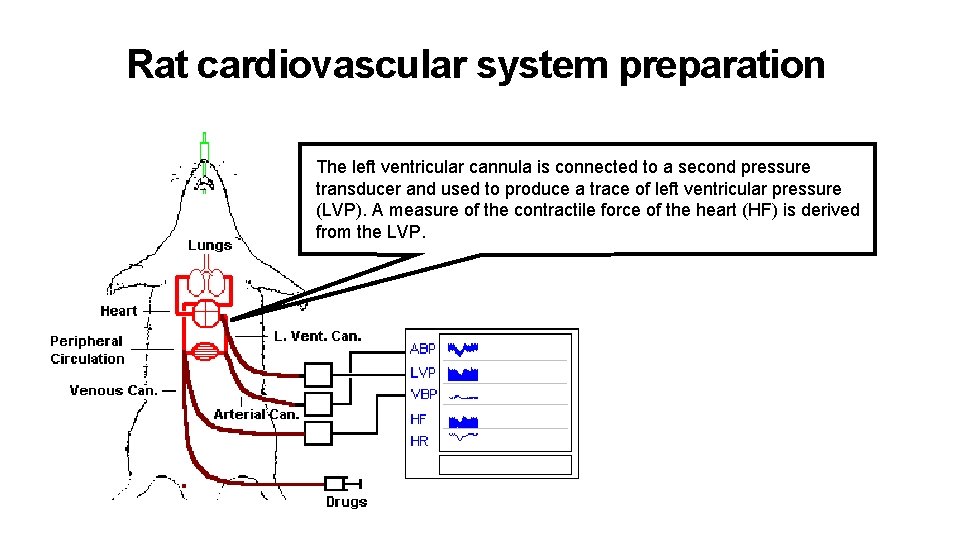
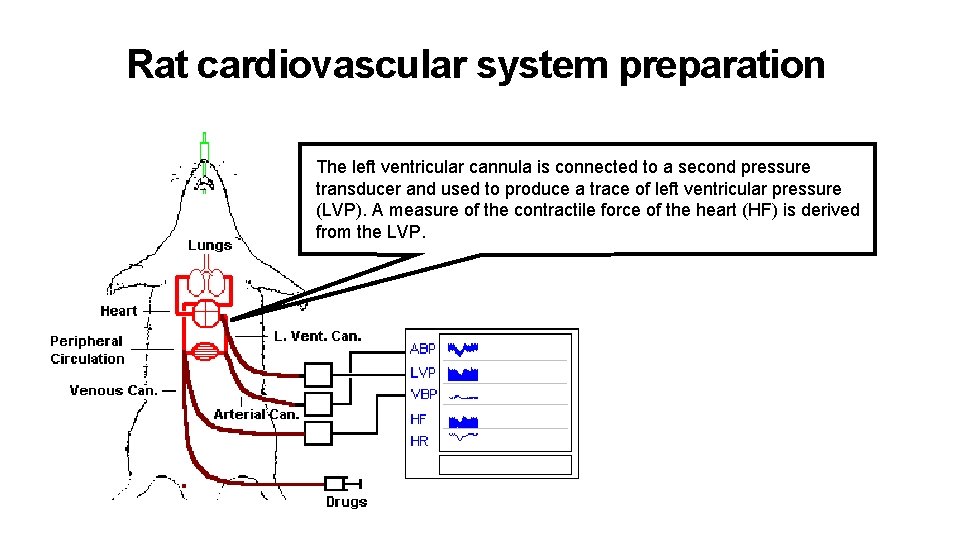
Rat cardiovascular system preparation The left ventricular cannula is connected to a second pressure transducer and used to produce a trace of left ventricular pressure (LVP). A measure of the contractile force of the heart (HF) is derived from the LVP.
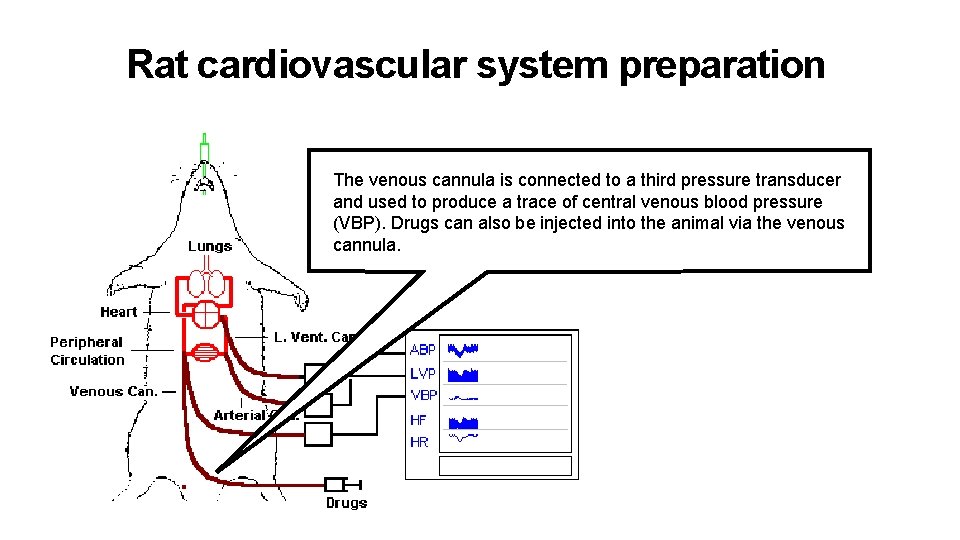
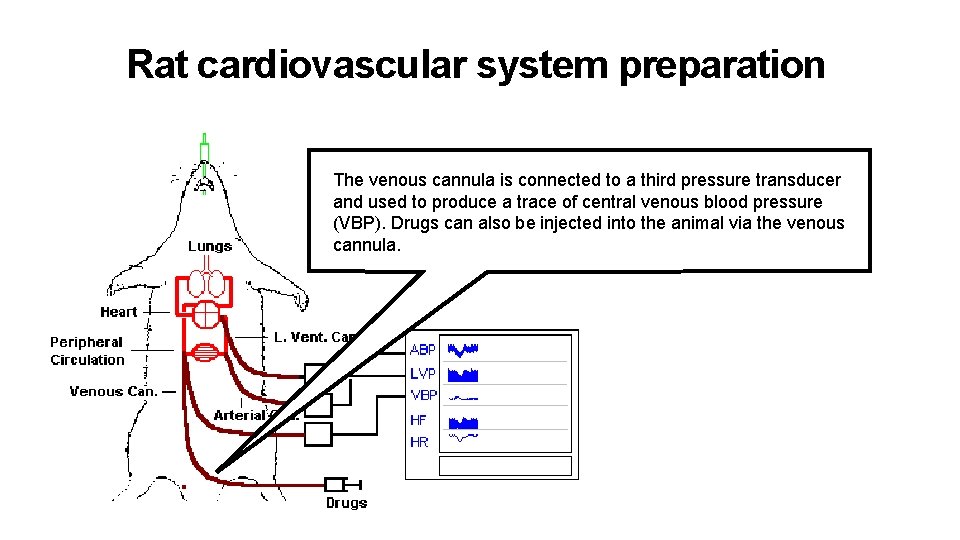
Rat cardiovascular system preparation The venous cannula is connected to a third pressure transducer and used to produce a trace of central venous blood pressure (VBP). Drugs can also be injected into the animal via the venous cannula.
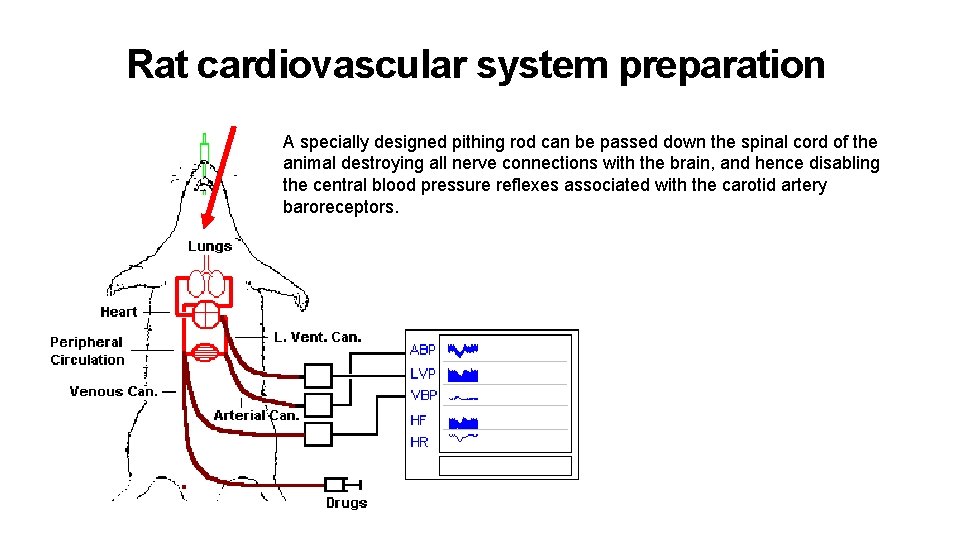
Rat cardiovascular system preparation A specially designed pithing rod can be passed down the spinal cord of the animal destroying all nerve connections with the brain, and hence disabling the central blood pressure reflexes associated with the carotid artery baroreceptors.
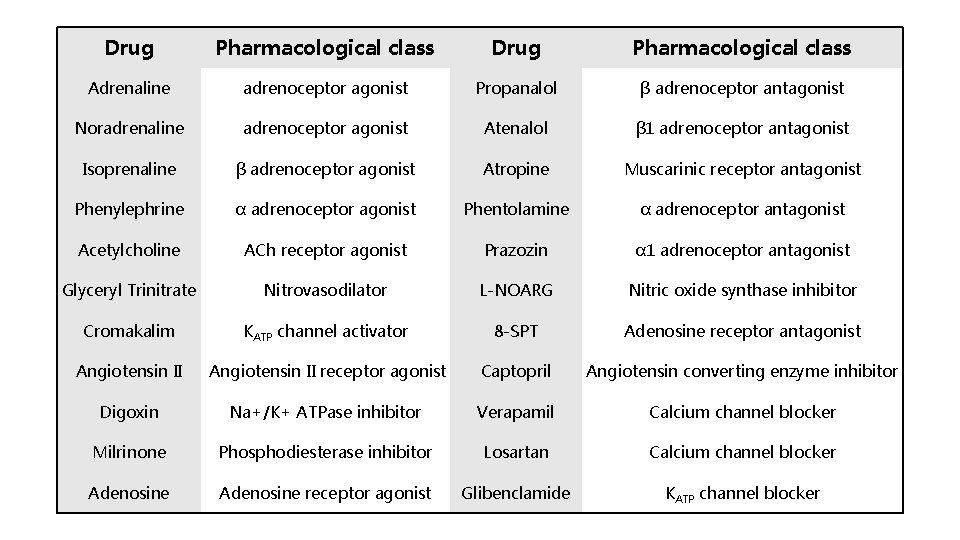
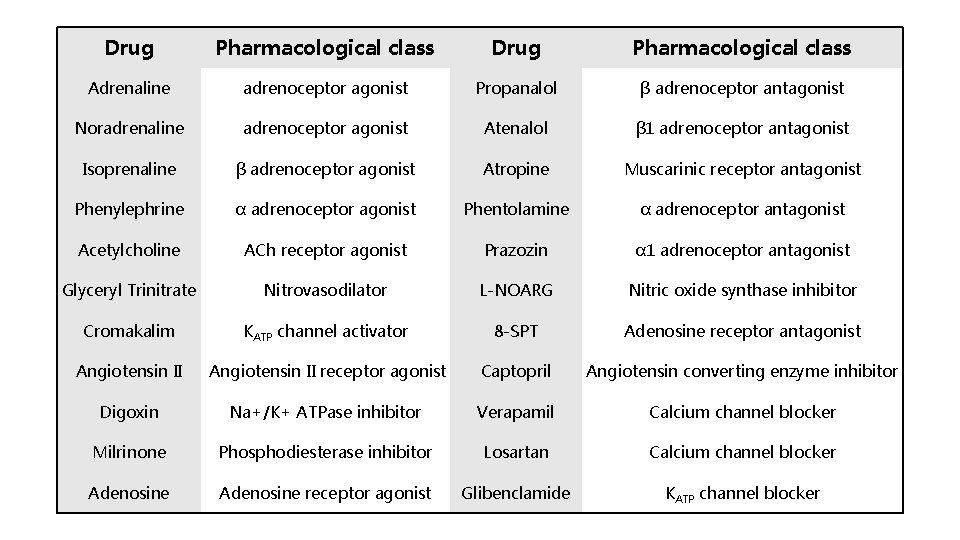
Drug Pharmacological class Adrenaline adrenoceptor agonist Propanalol β adrenoceptor antagonist Noradrenaline adrenoceptor agonist Atenalol β 1 adrenoceptor antagonist Isoprenaline β adrenoceptor agonist Atropine Muscarinic receptor antagonist Phenylephrine α adrenoceptor agonist Phentolamine α adrenoceptor antagonist Acetylcholine ACh receptor agonist Prazozin α 1 adrenoceptor antagonist Glyceryl Trinitrate Nitrovasodilator L-NOARG Nitric oxide synthase inhibitor Cromakalim KATP channel activator 8 -SPT Adenosine receptor antagonist Angiotensin II receptor agonist Captopril Angiotensin converting enzyme inhibitor Digoxin Na+/K+ ATPase inhibitor Verapamil Calcium channel blocker Milrinone Phosphodiesterase inhibitor Losartan Calcium channel blocker Adenosine receptor agonist Glibenclamide KATP channel blocker

Experiment II Anaesthetized Cat Simulation
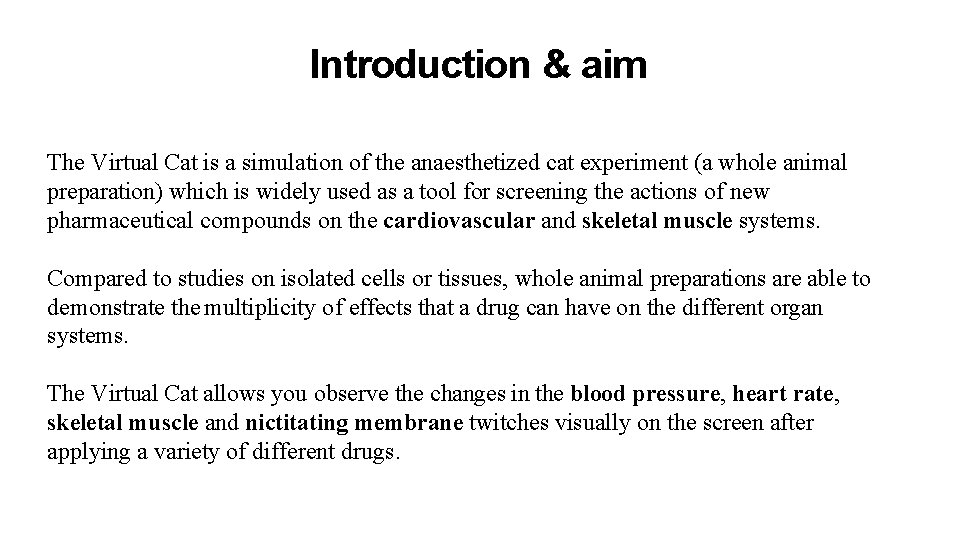
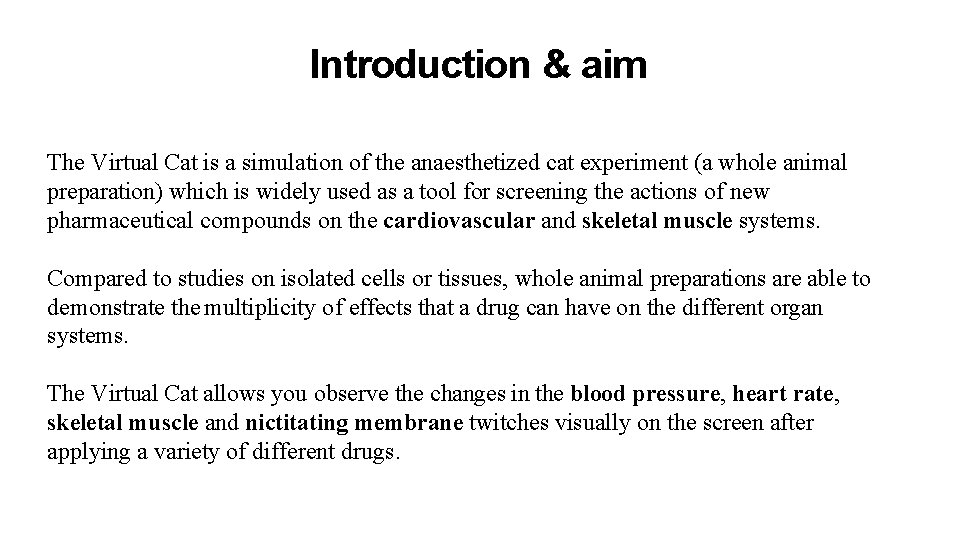
Introduction & aim The Virtual Cat is a simulation of the anaesthetized cat experiment (a whole animal preparation) which is widely used as a tool for screening the actions of new pharmaceutical compounds on the cardiovascular and skeletal muscle systems. Compared to studies on isolated cells or tissues, whole animal preparations are able to demonstrate the multiplicity of effects that a drug can have on the different organ systems. The Virtual Cat allows you observe the changes in the blood pressure, heart rate, skeletal muscle and nictitating membrane twitches visually on the screen after applying a variety of different drugs.
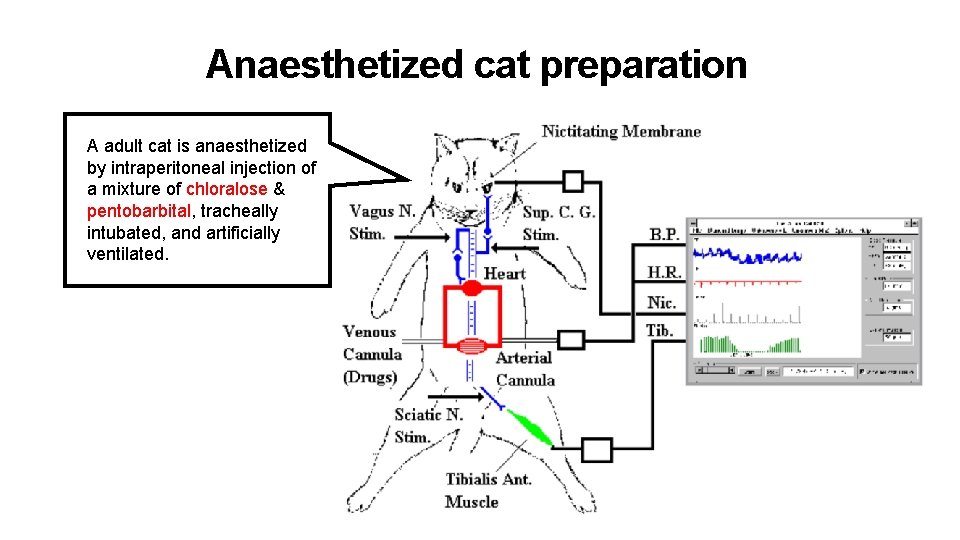
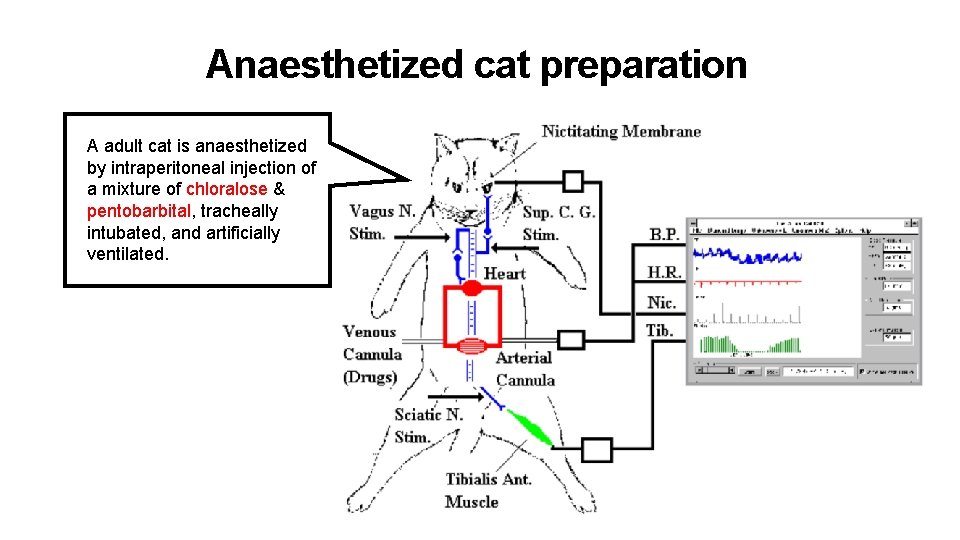
Anaesthetized cat preparation A adult cat is anaesthetized by intraperitoneal injection of a mixture of chloralose & pentobarbital, tracheally intubated, and artificially ventilated.
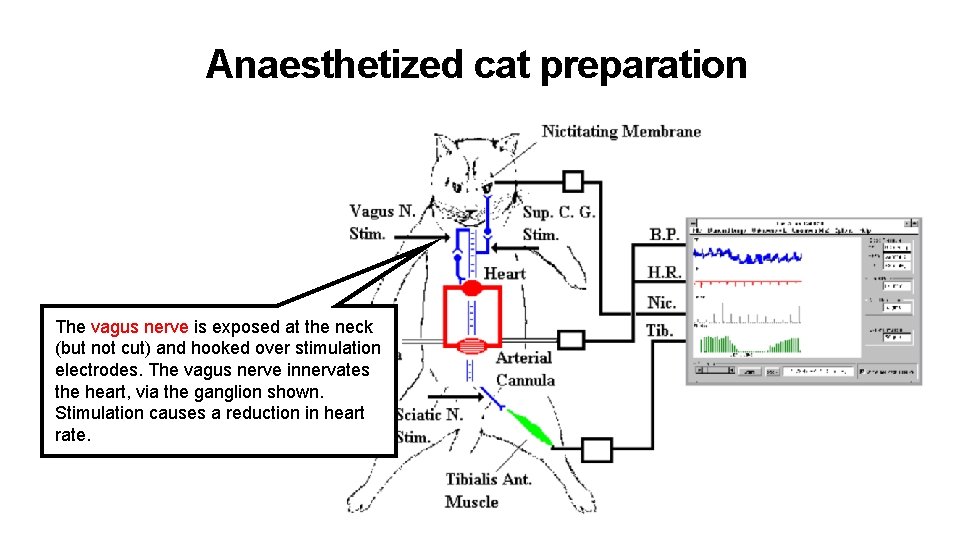
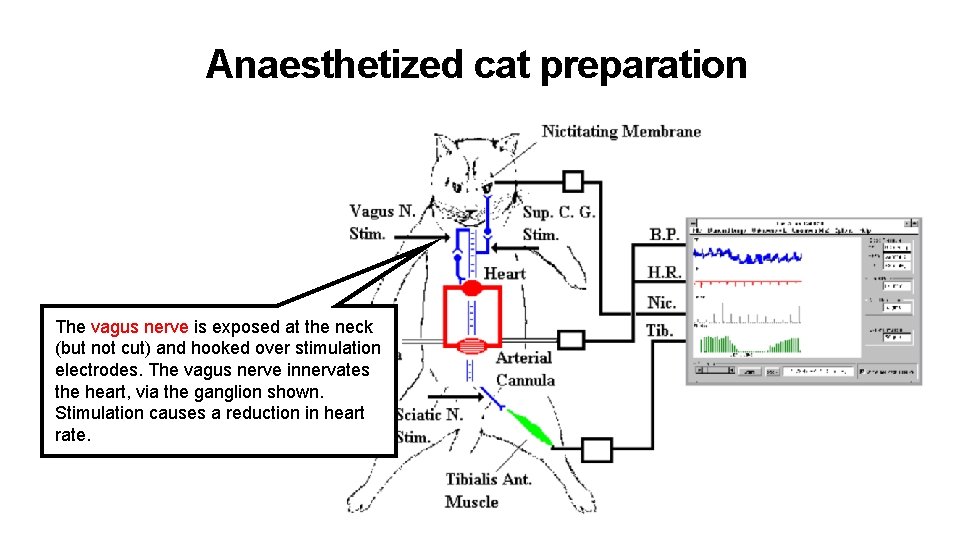
Anaesthetized cat preparation The vagus nerve is exposed at the neck (but not cut) and hooked over stimulation electrodes. The vagus nerve innervates the heart, via the ganglion shown. Stimulation causes a reduction in heart rate.
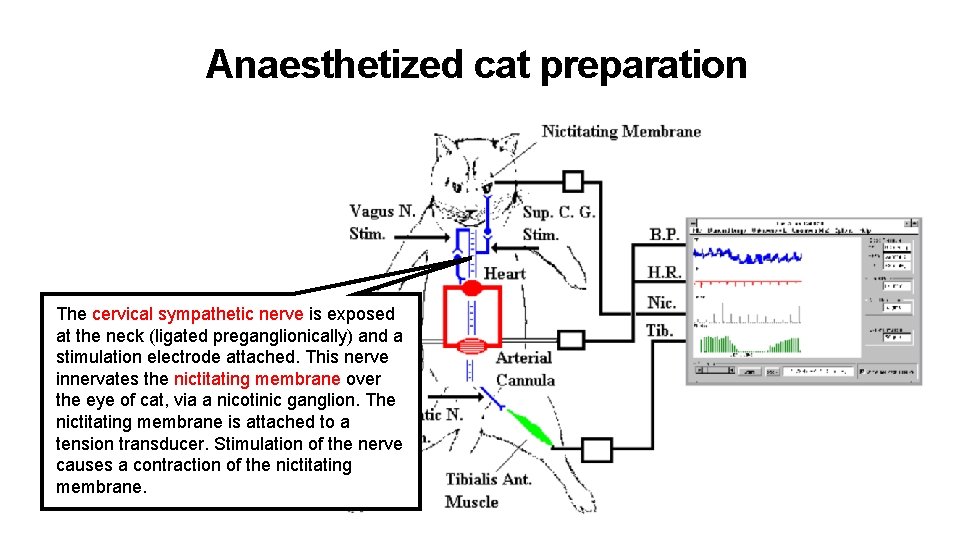
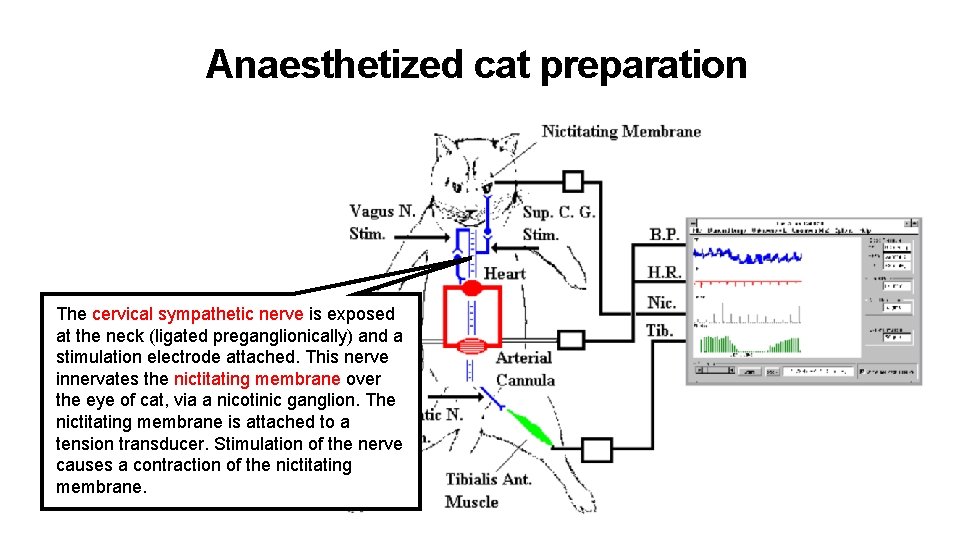
Anaesthetized cat preparation The cervical sympathetic nerve is exposed at the neck (ligated preganglionically) and a stimulation electrode attached. This nerve innervates the nictitating membrane over the eye of cat, via a nicotinic ganglion. The nictitating membrane is attached to a tension transducer. Stimulation of the nerve causes a contraction of the nictitating membrane.
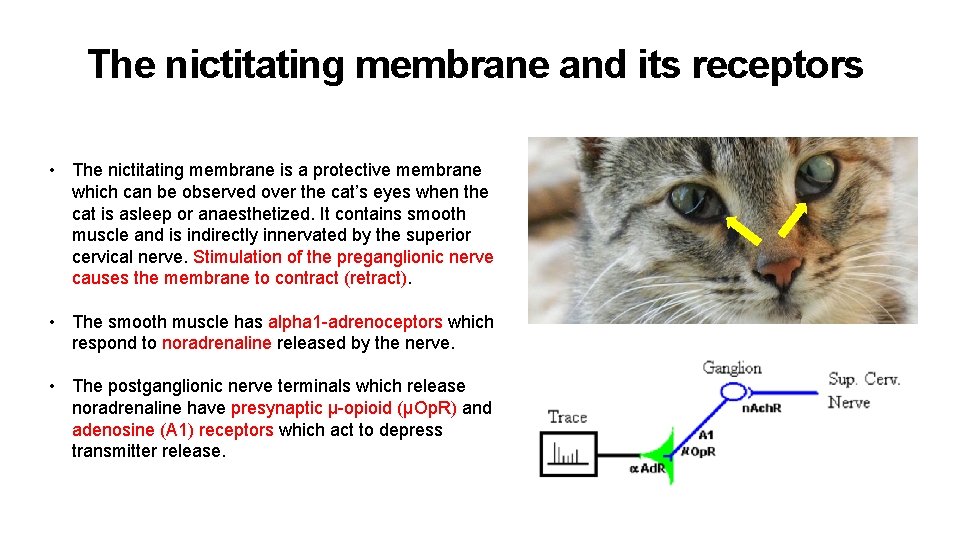
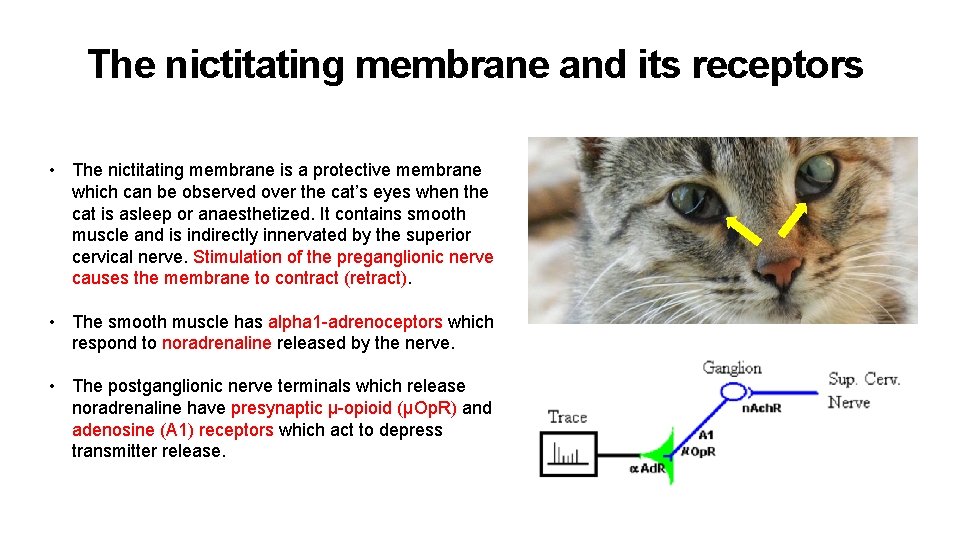
The nictitating membrane and its receptors • The nictitating membrane is a protective membrane which can be observed over the cat’s eyes when the cat is asleep or anaesthetized. It contains smooth muscle and is indirectly innervated by the superior cervical nerve. Stimulation of the preganglionic nerve causes the membrane to contract (retract). • The smooth muscle has alpha 1 -adrenoceptors which respond to noradrenaline released by the nerve. • The postganglionic nerve terminals which release noradrenaline have presynaptic μ-opioid (μOp. R) and adenosine (A 1) receptors which act to depress transmitter release.
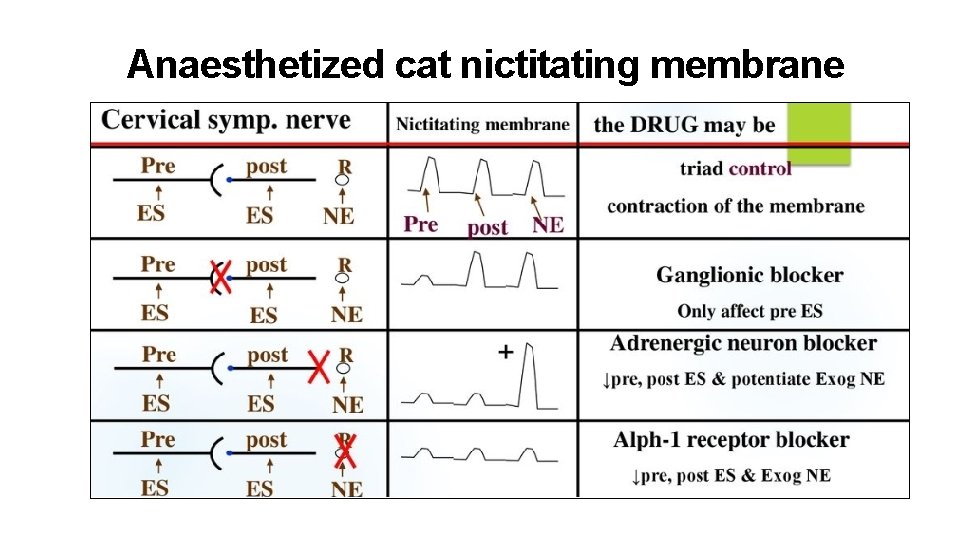
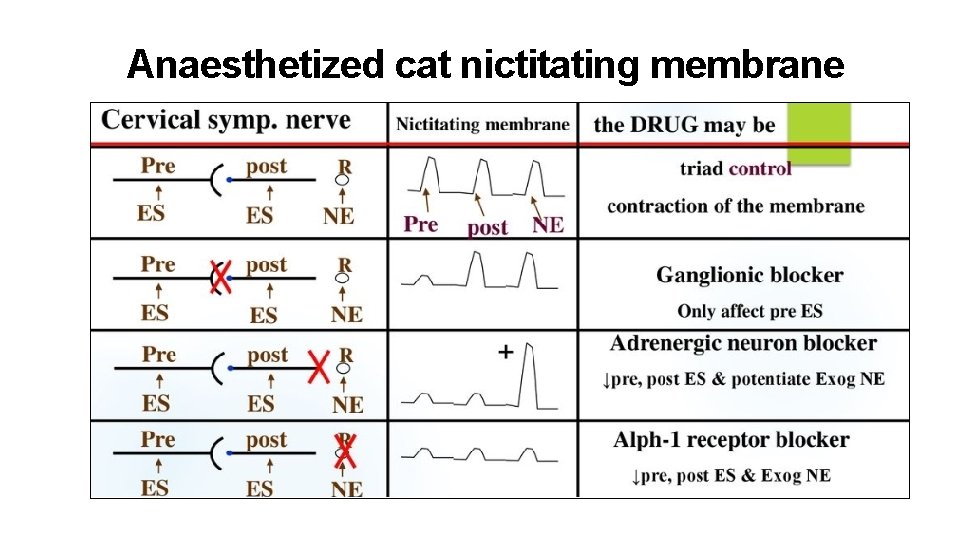
Anaesthetized cat nictitating membrane
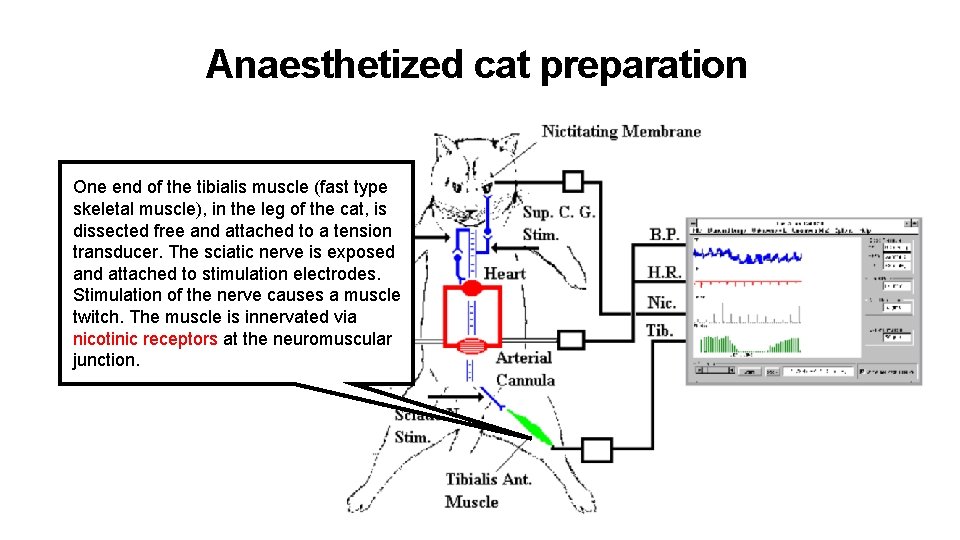
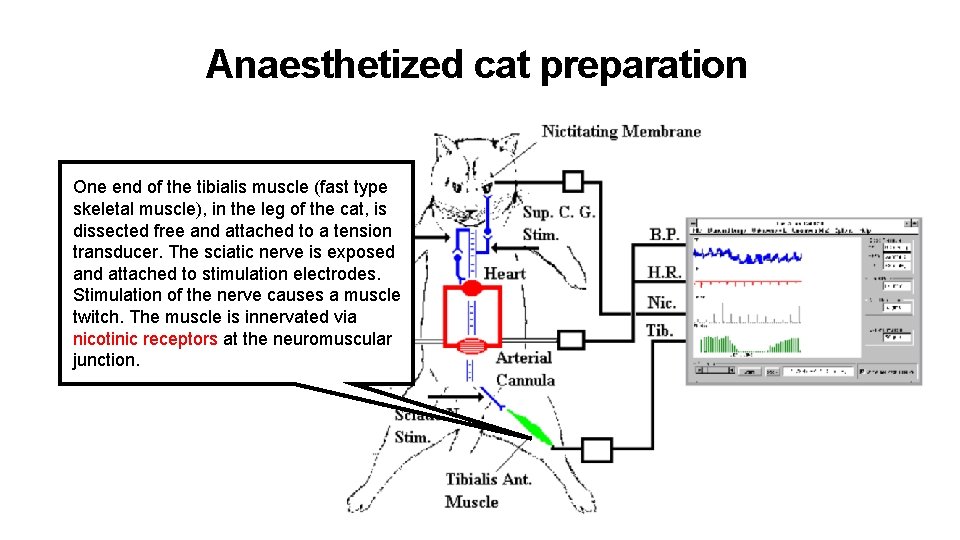
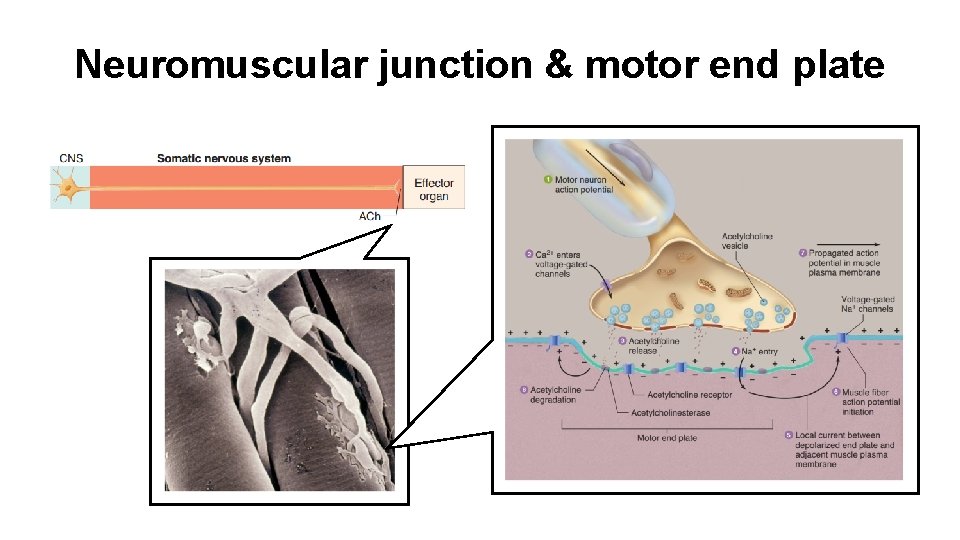
Anaesthetized cat preparation One end of the tibialis muscle (fast type skeletal muscle), in the leg of the cat, is dissected free and attached to a tension transducer. The sciatic nerve is exposed and attached to stimulation electrodes. Stimulation of the nerve causes a muscle twitch. The muscle is innervated via nicotinic receptors at the neuromuscular junction.
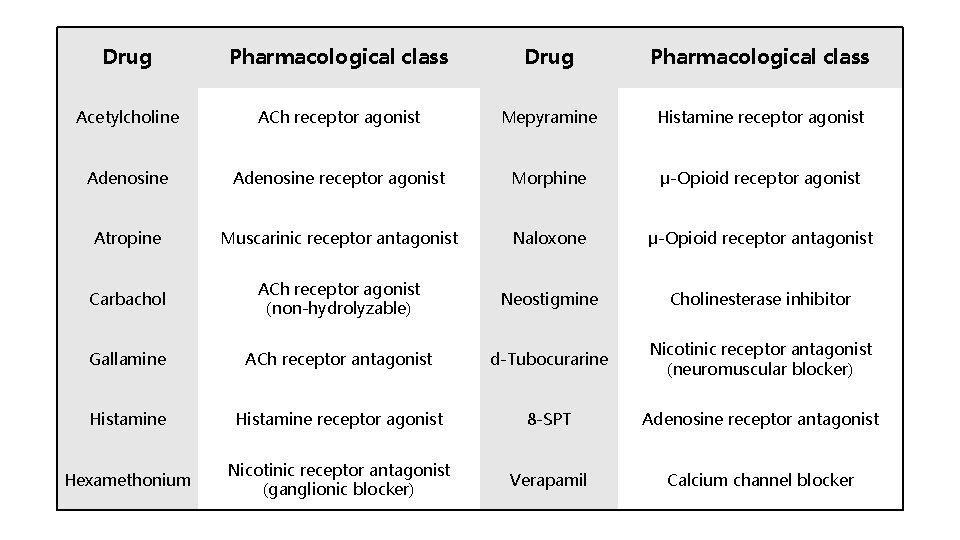
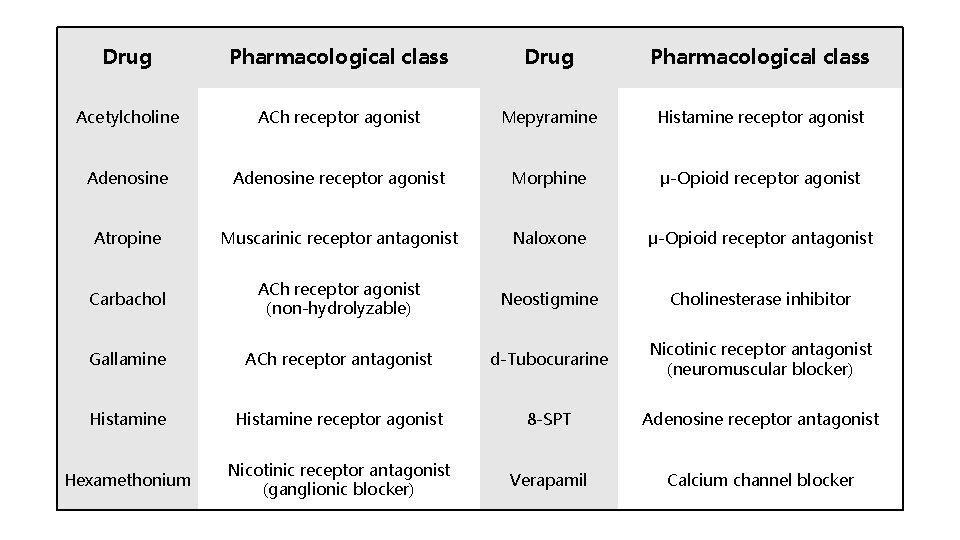
Drug Pharmacological class Acetylcholine ACh receptor agonist Mepyramine Histamine receptor agonist Adenosine receptor agonist Morphine μ-Opioid receptor agonist Atropine Muscarinic receptor antagonist Naloxone μ-Opioid receptor antagonist Carbachol ACh receptor agonist (non-hydrolyzable) Neostigmine Cholinesterase inhibitor Gallamine ACh receptor antagonist d-Tubocurarine Nicotinic receptor antagonist (neuromuscular blocker) Histamine receptor agonist 8 -SPT Adenosine receptor antagonist Hexamethonium Nicotinic receptor antagonist (ganglionic blocker) Verapamil Calcium channel blocker
Overview Skeletal muscle and cardiovascular systems
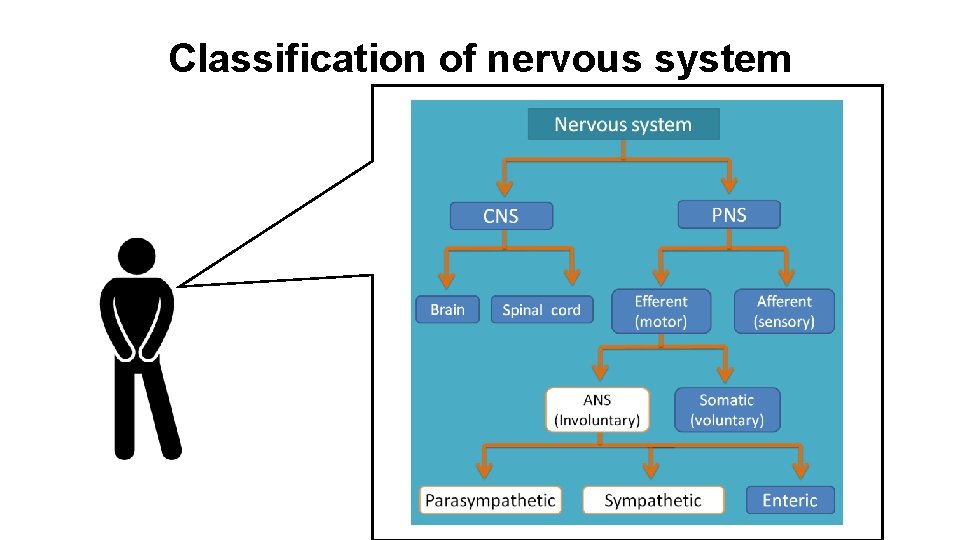
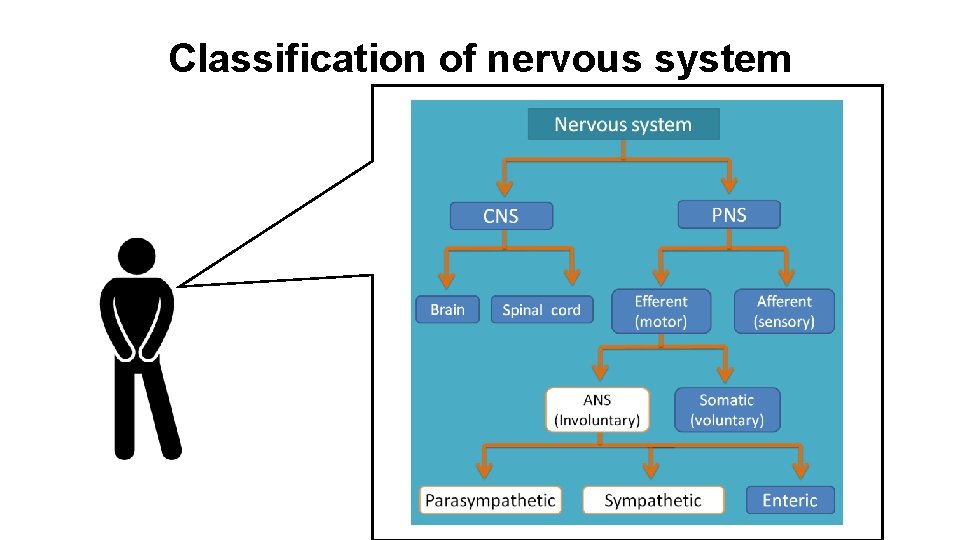
Classification of nervous system
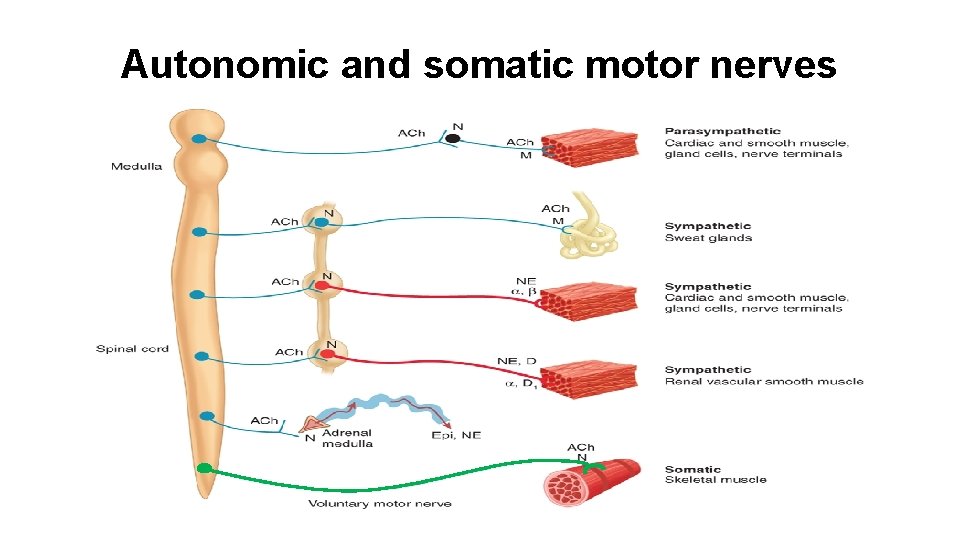
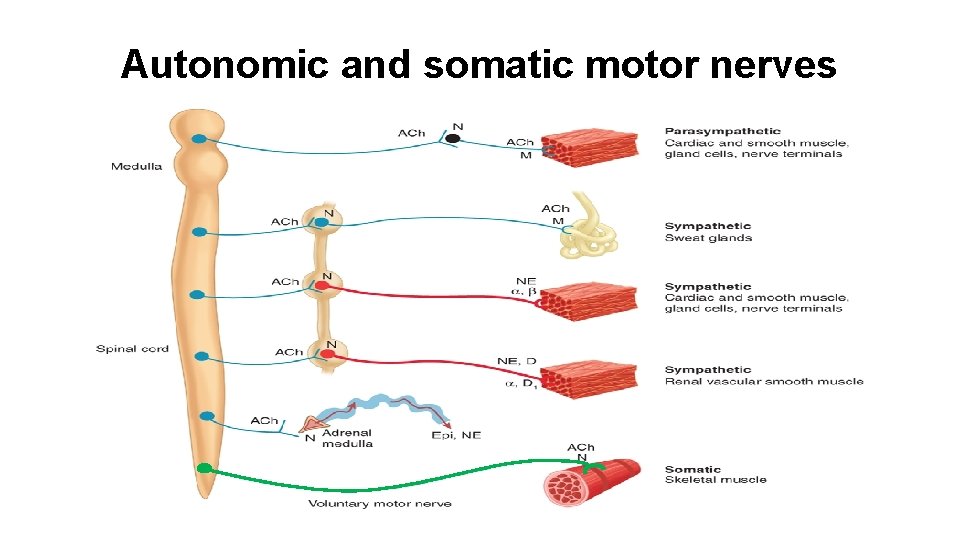
Autonomic and somatic motor nerves
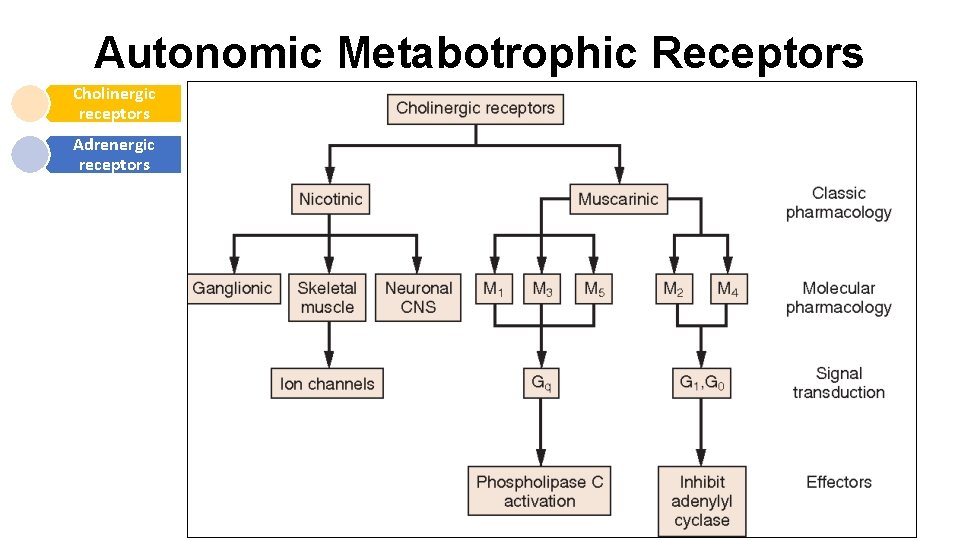
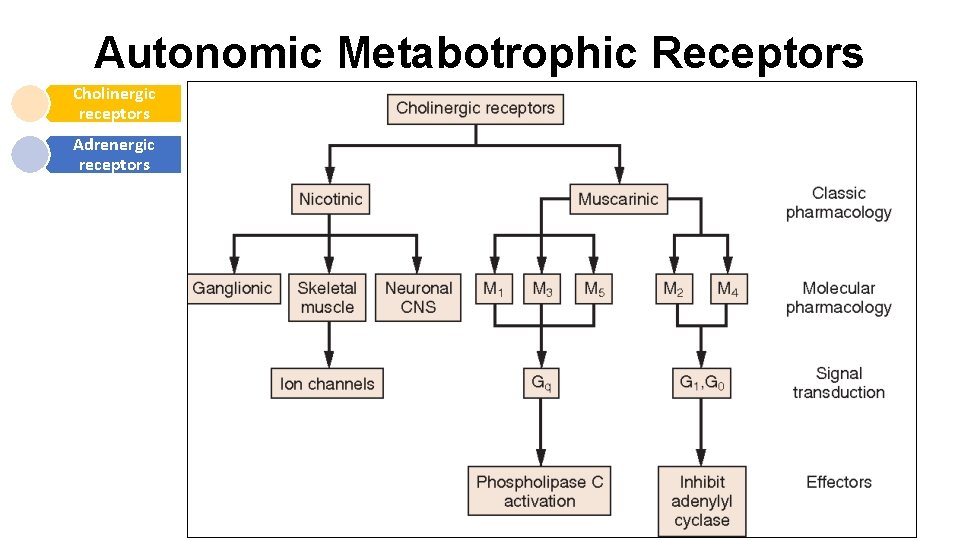
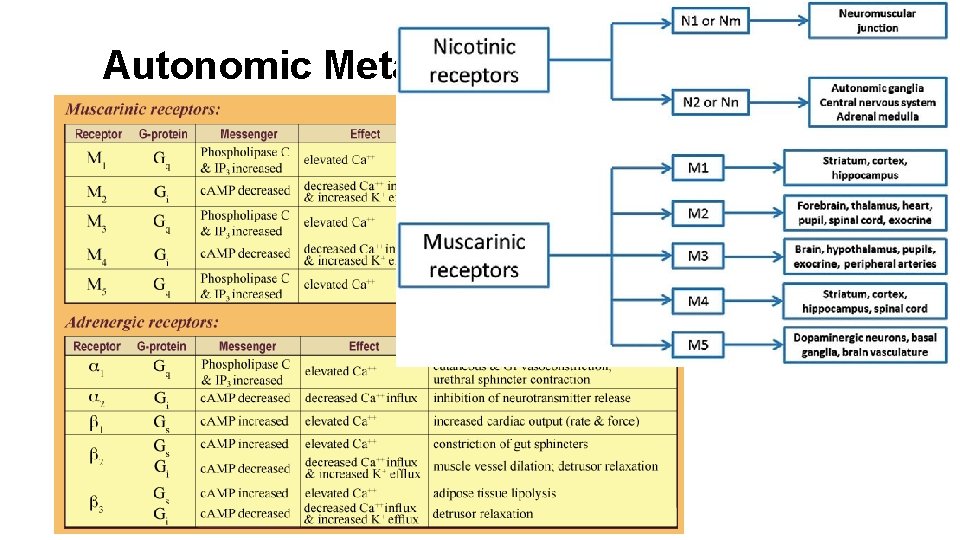
Autonomic Metabotrophic Receptors Cholinergic receptors Adrenergic receptors
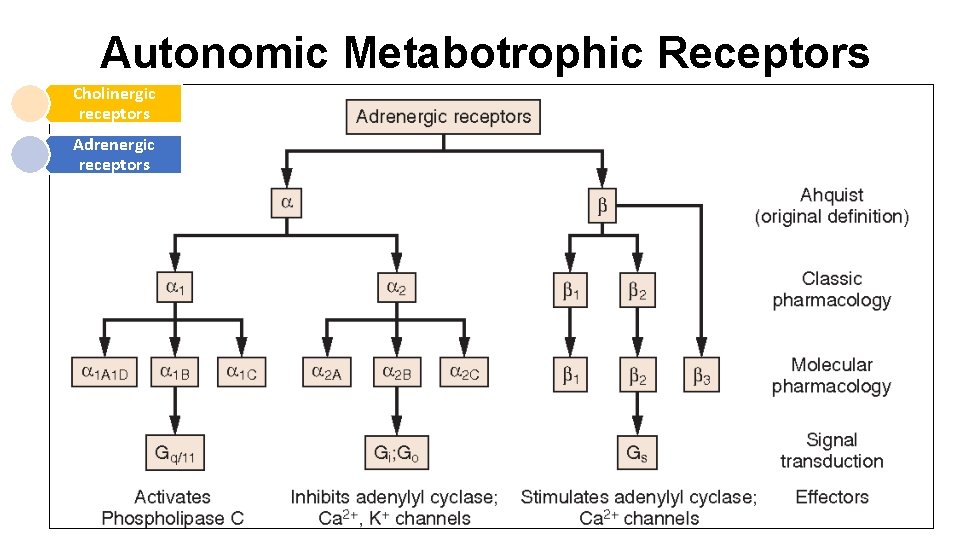
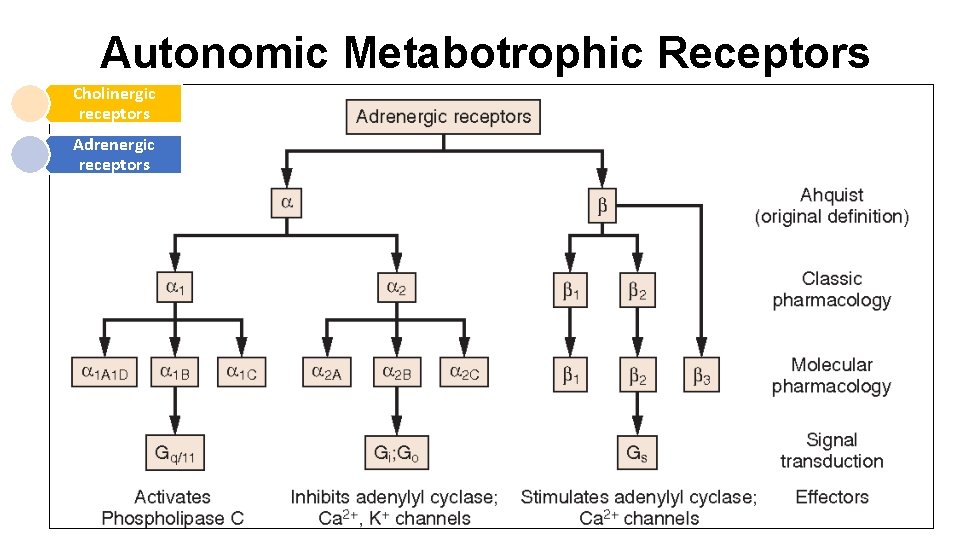
Autonomic Metabotrophic Receptors Cholinergic receptors Adrenergic receptors
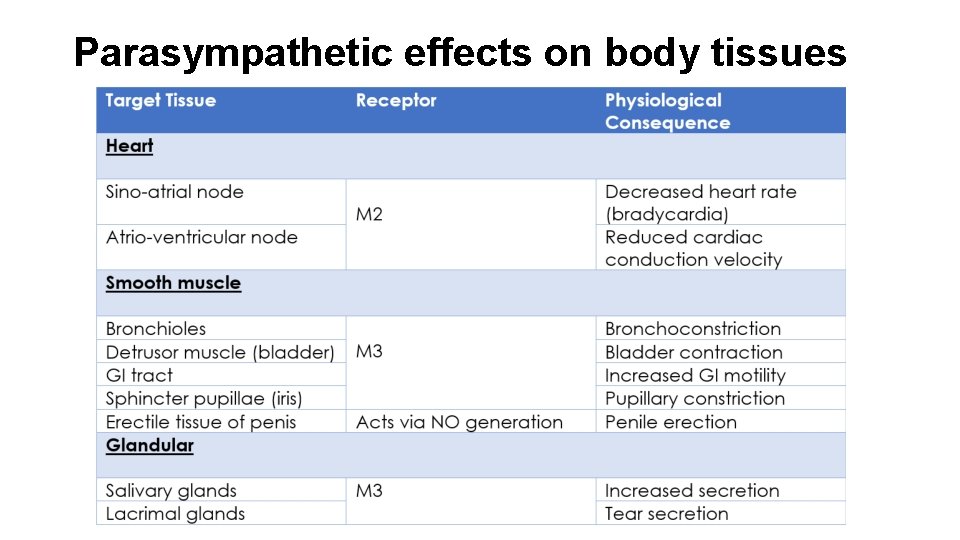
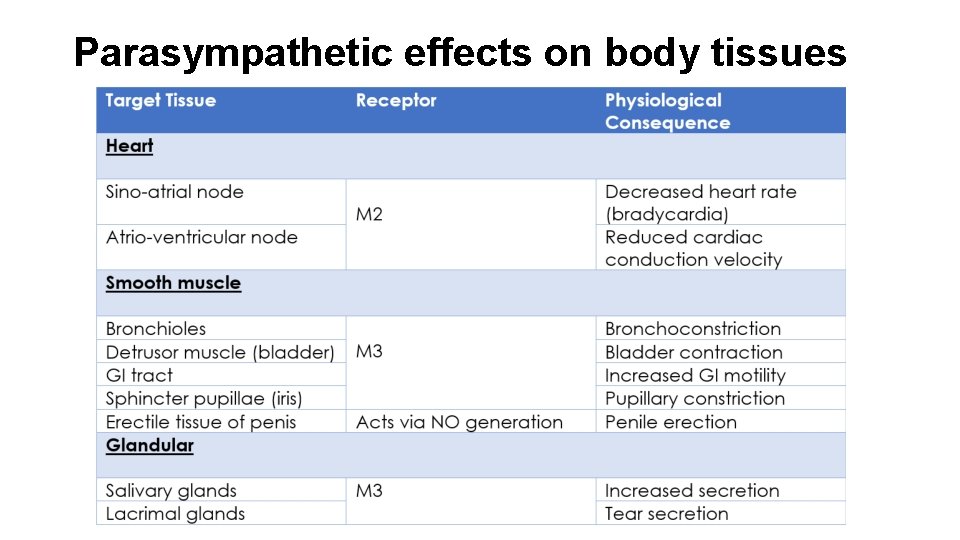
Parasympathetic effects on body tissues
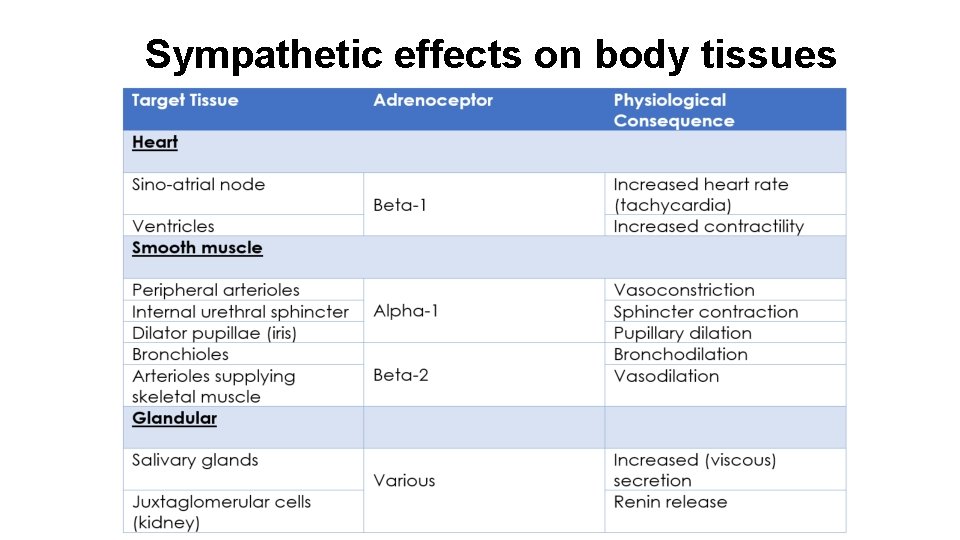
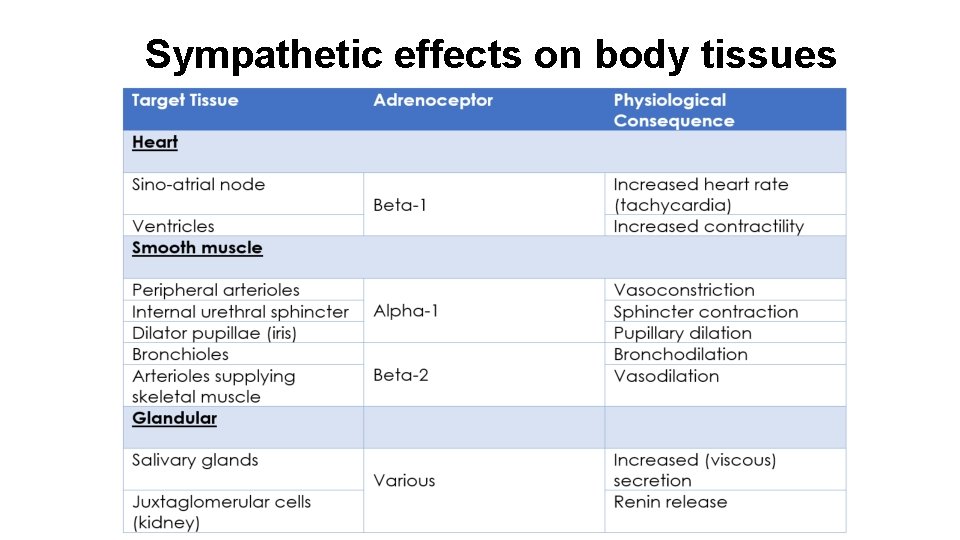
Sympathetic effects on body tissues
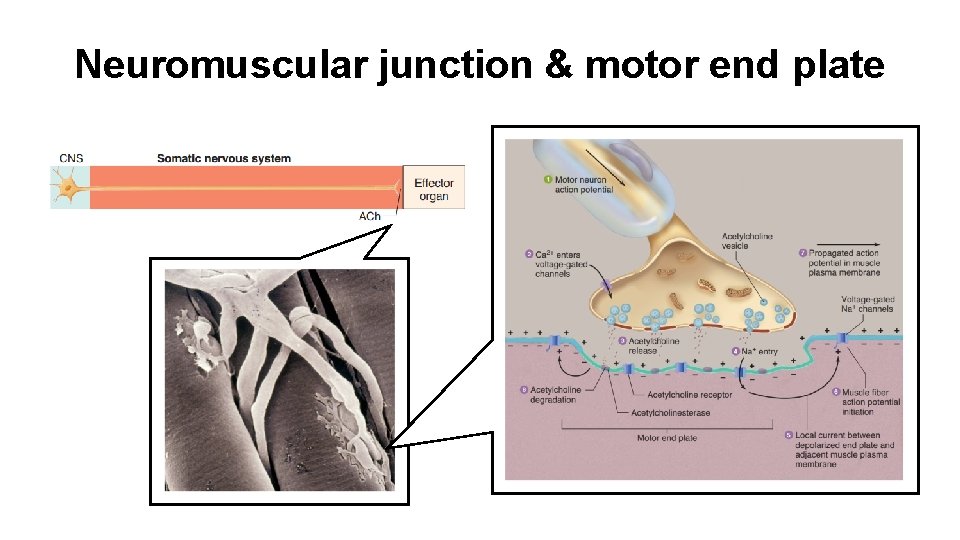
Neuromuscular junction & motor end plate
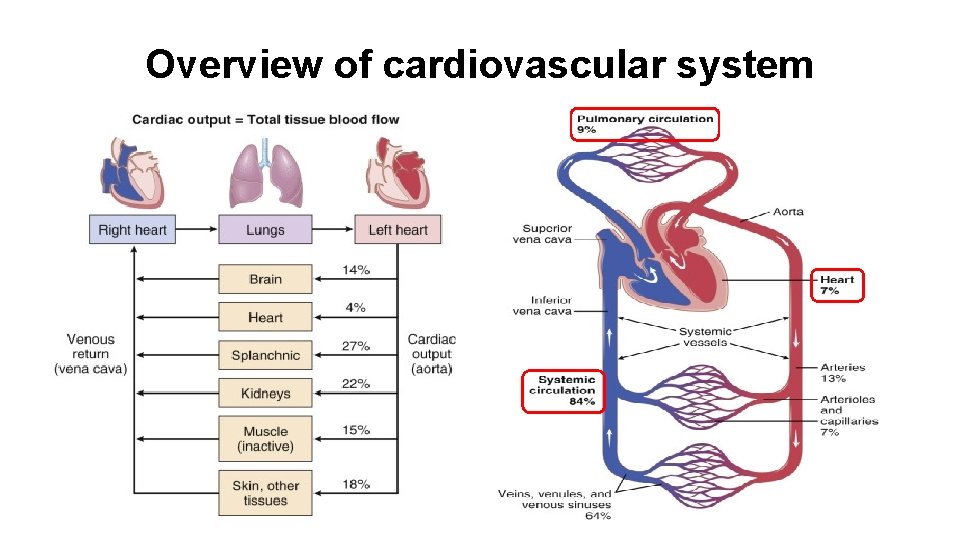
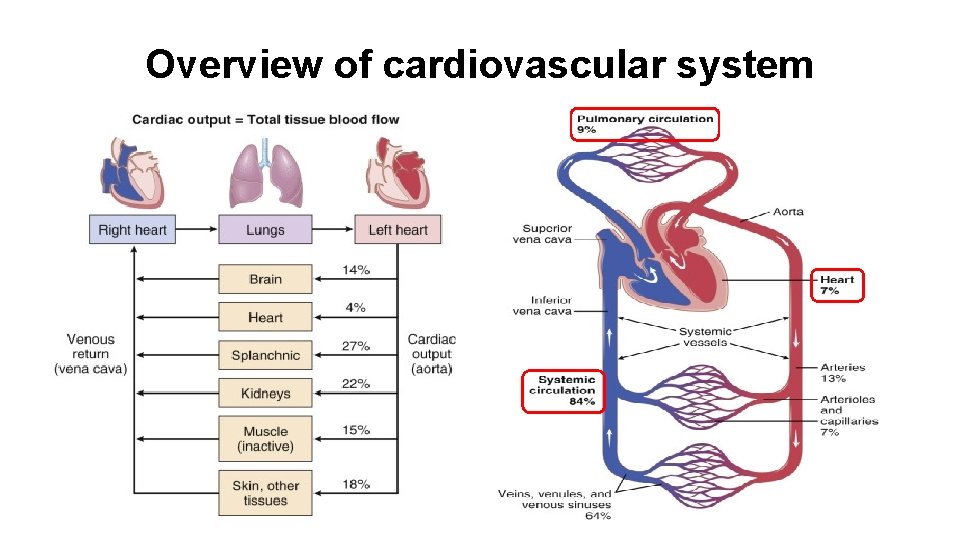
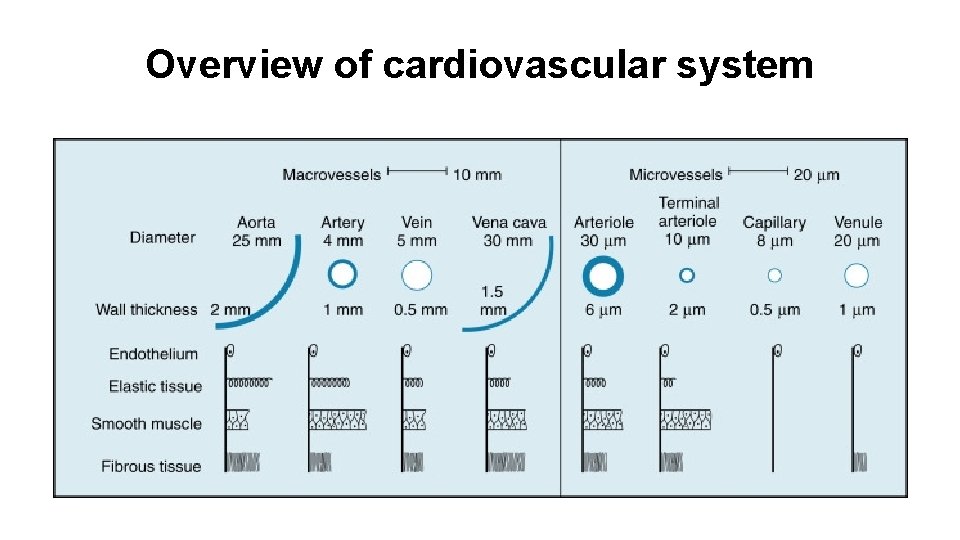
Overview of cardiovascular system
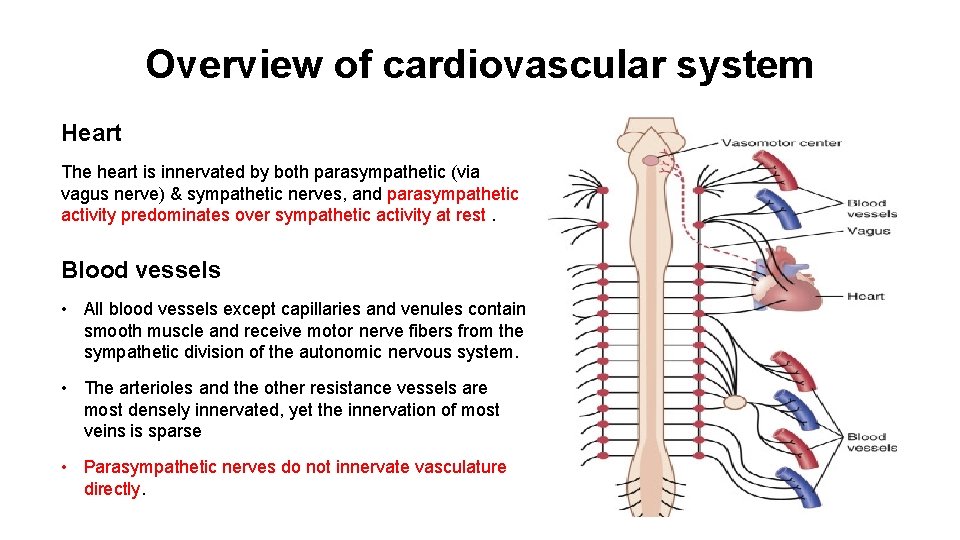
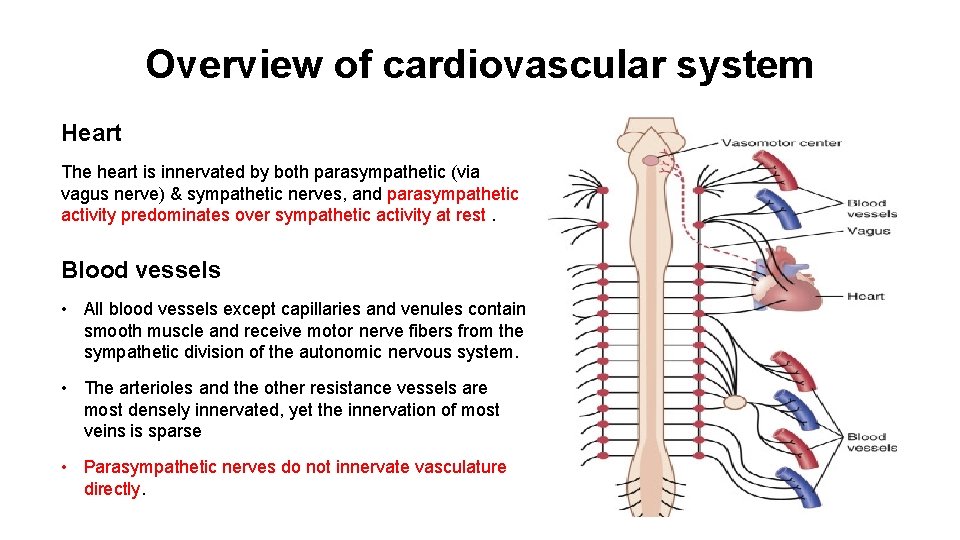
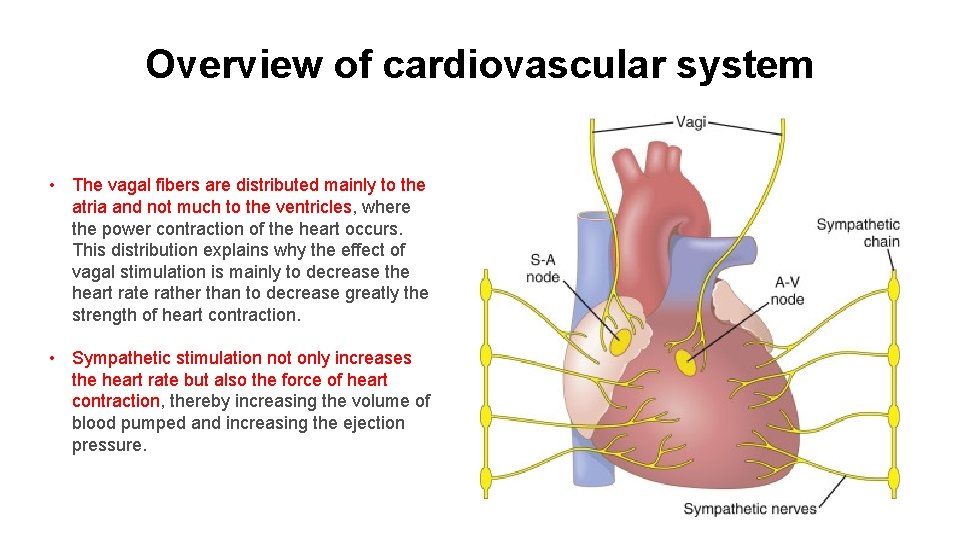
Overview of cardiovascular system Heart The heart is innervated by both parasympathetic (via vagus nerve) & sympathetic nerves, and parasympathetic activity predominates over sympathetic activity at rest. Blood vessels • All blood vessels except capillaries and venules contain smooth muscle and receive motor nerve fibers from the sympathetic division of the autonomic nervous system. • The arterioles and the other resistance vessels are most densely innervated, yet the innervation of most veins is sparse • Parasympathetic nerves do not innervate vasculature directly.
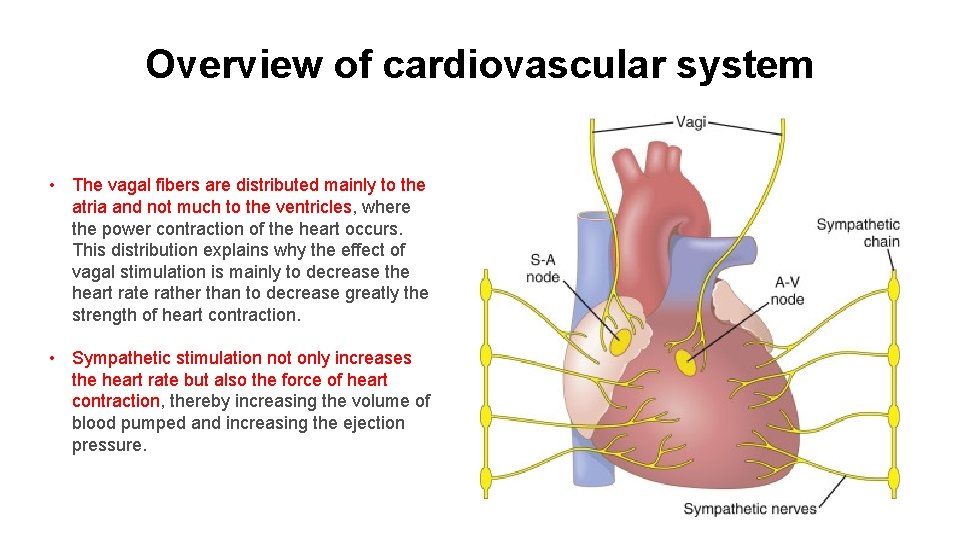
Overview of cardiovascular system • The vagal fibers are distributed mainly to the atria and not much to the ventricles, where the power contraction of the heart occurs. This distribution explains why the effect of vagal stimulation is mainly to decrease the heart rate rather than to decrease greatly the strength of heart contraction. • Sympathetic stimulation not only increases the heart rate but also the force of heart contraction, thereby increasing the volume of blood pumped and increasing the ejection pressure.
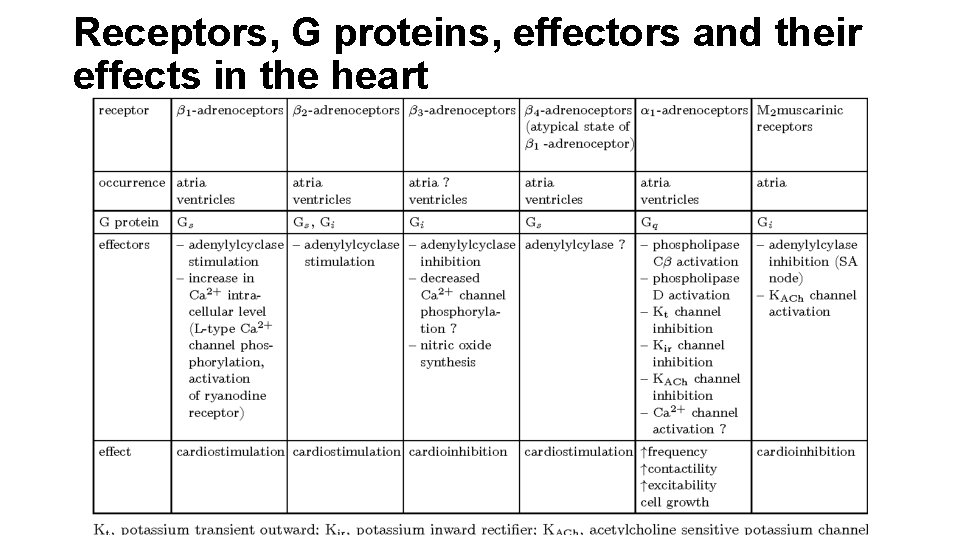
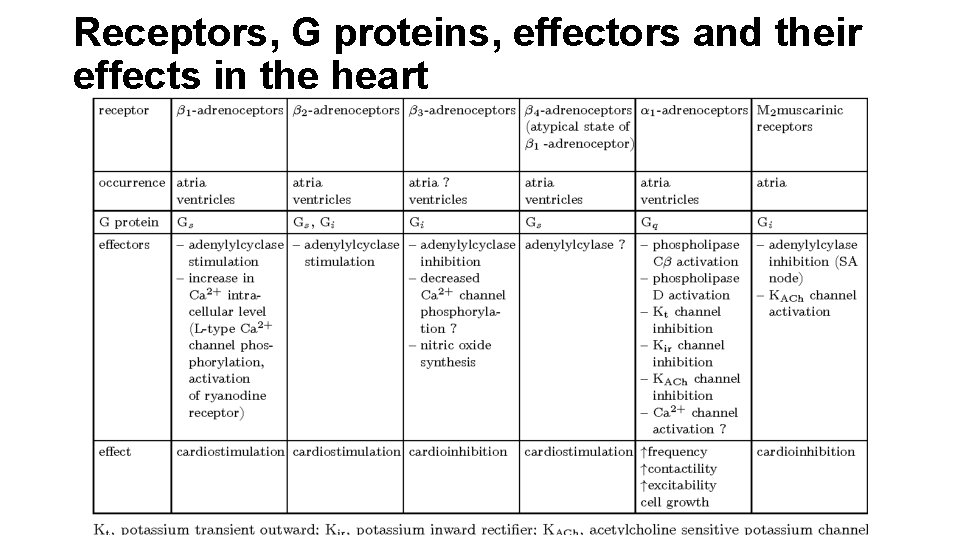
Receptors, G proteins, effectors and their effects in the heart
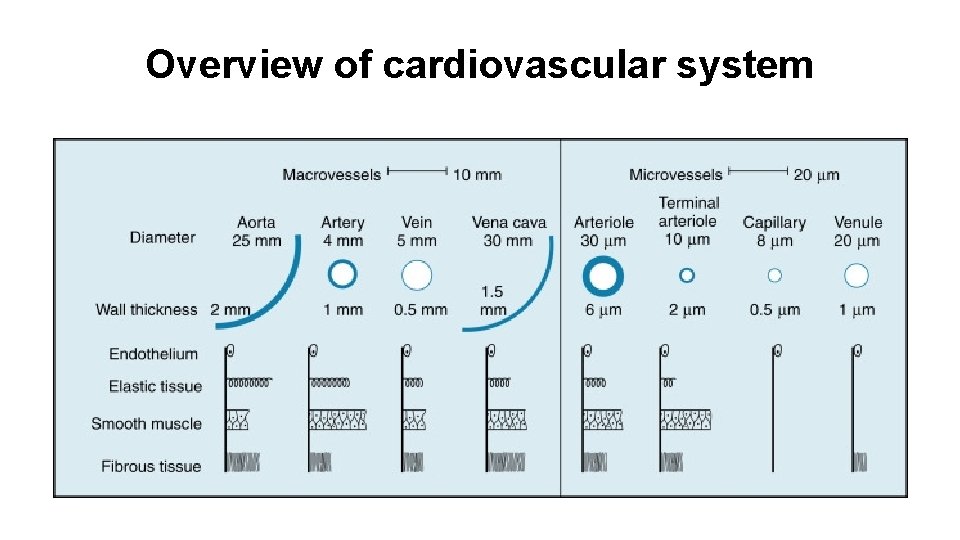
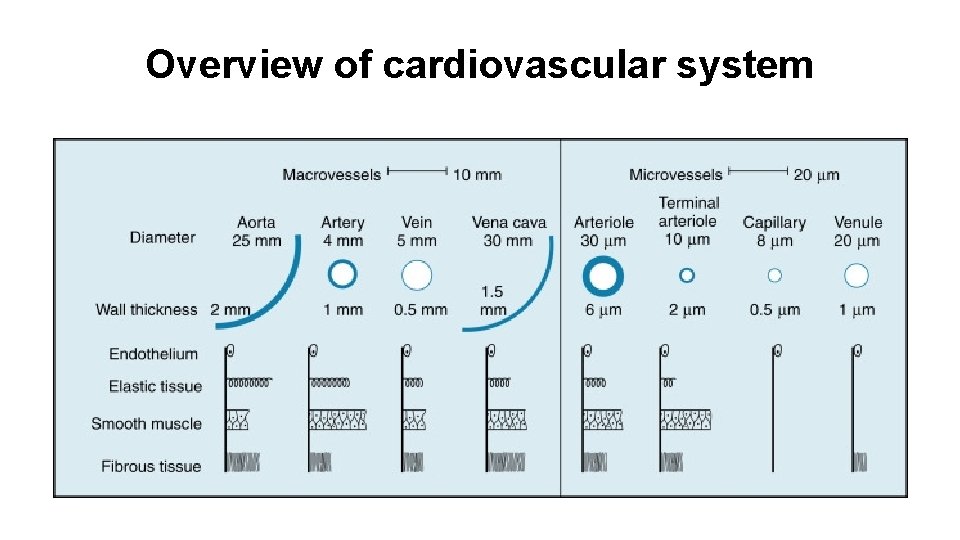
Overview of cardiovascular system
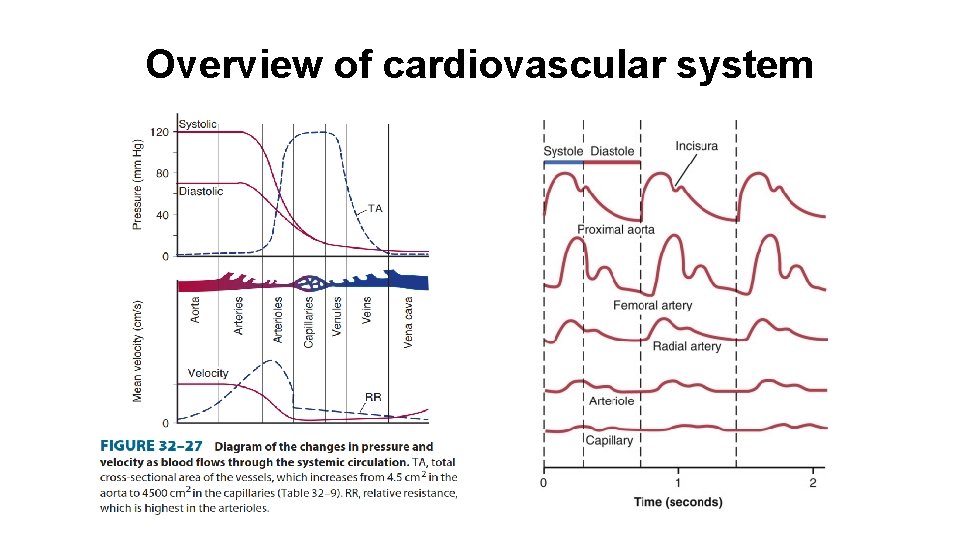
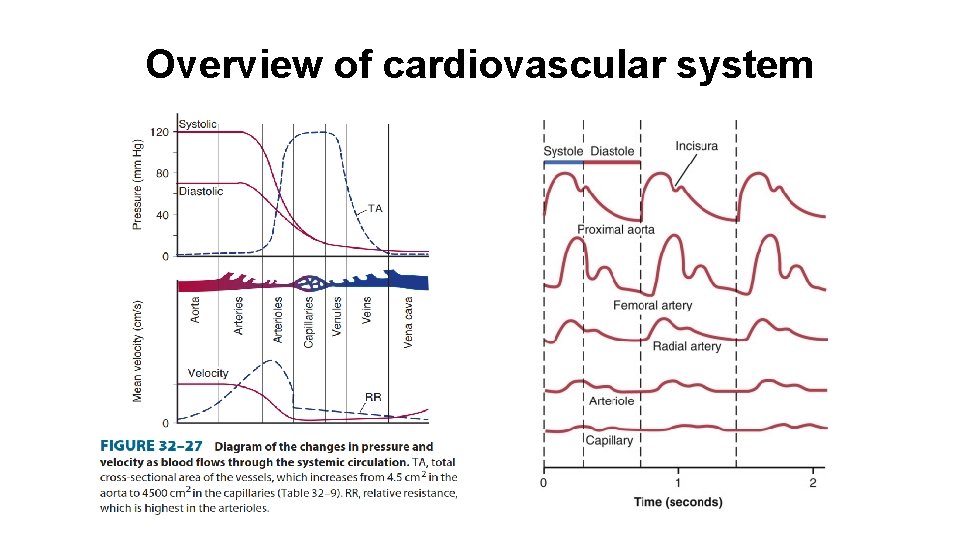
Overview of cardiovascular system
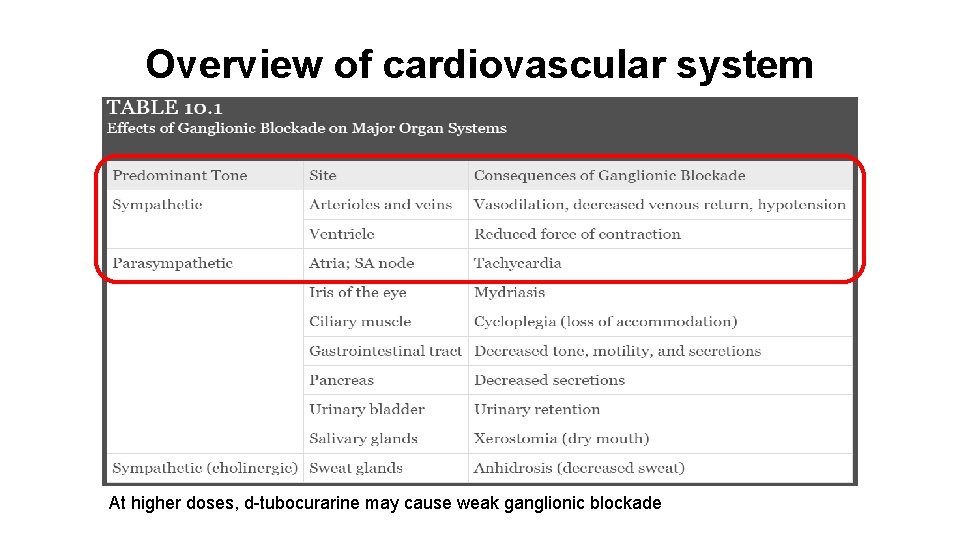
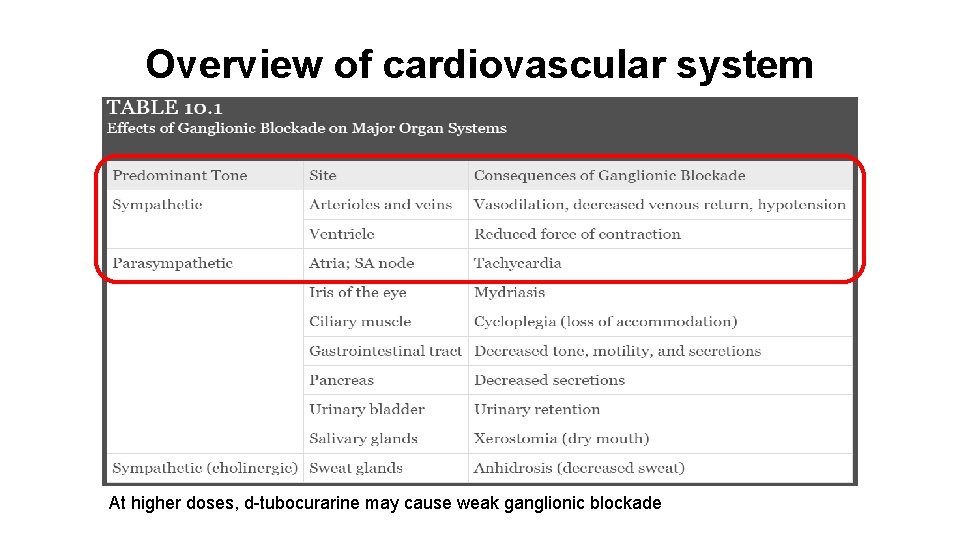
Overview of cardiovascular system At higher doses, d-tubocurarine may cause weak ganglionic blockade
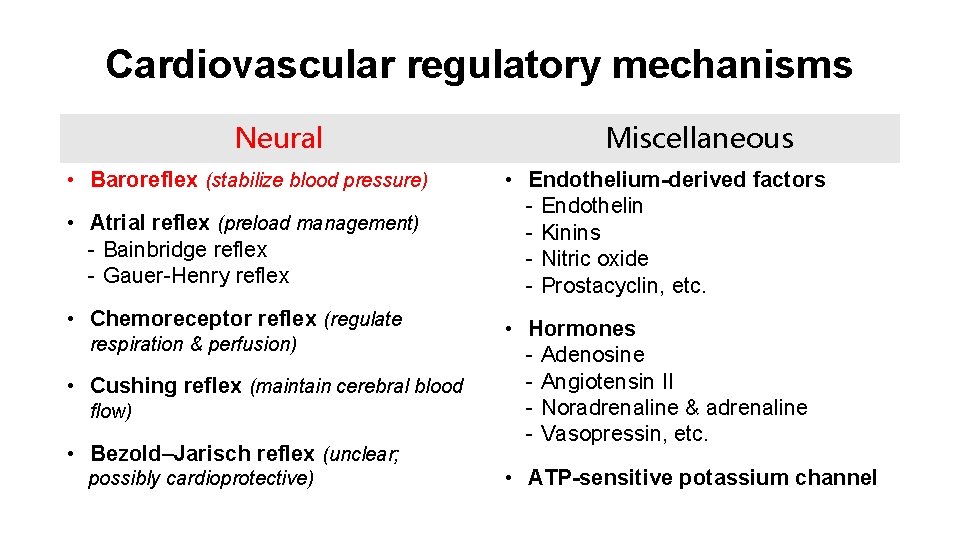
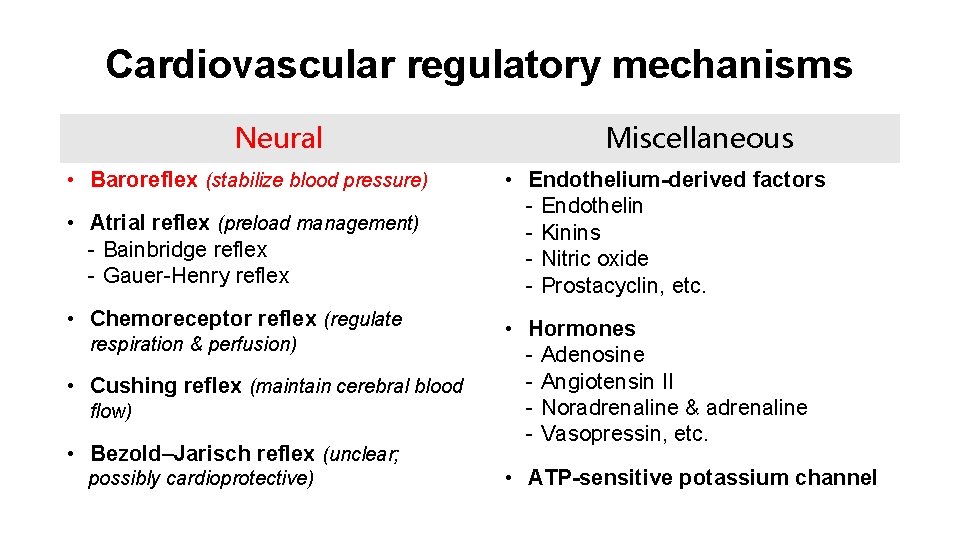
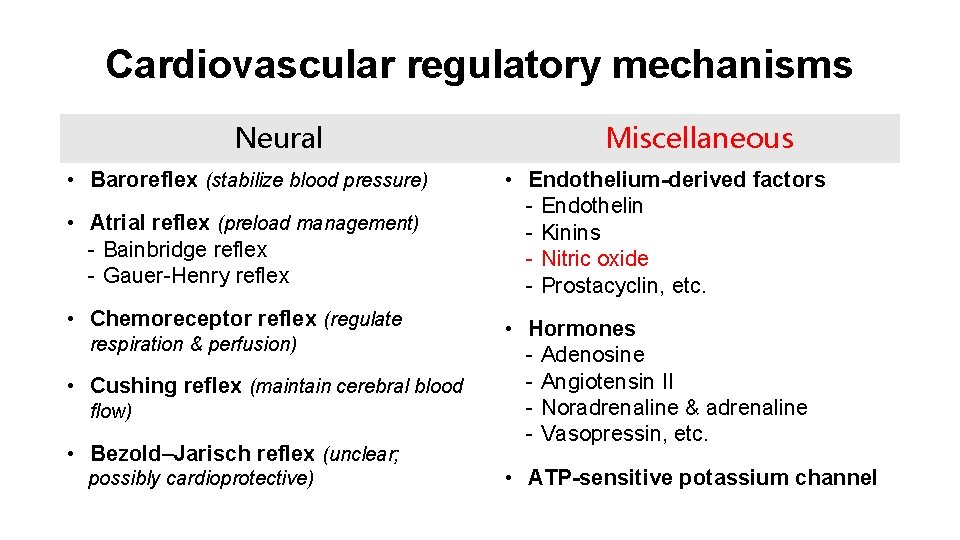
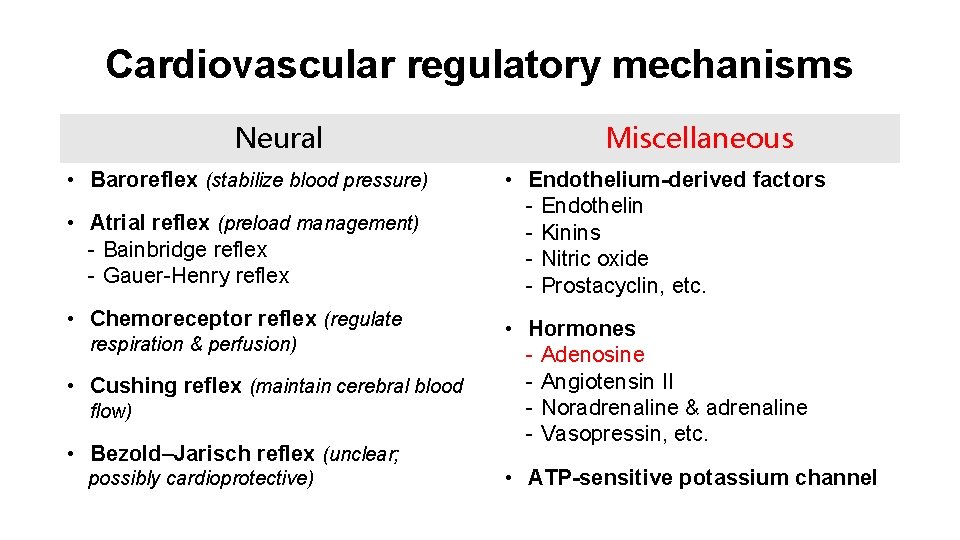
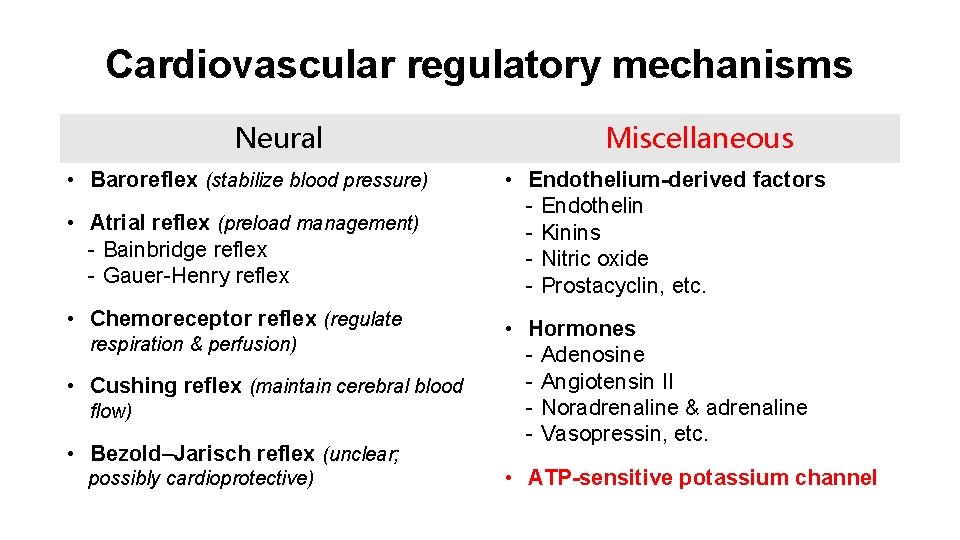
Cardiovascular regulatory mechanisms Neural • Baroreflex (stabilize blood pressure) • Atrial reflex (preload management) - Bainbridge reflex - Gauer-Henry reflex • Chemoreceptor reflex (regulate respiration & perfusion) • Cushing reflex (maintain cerebral blood flow) • Bezold–Jarisch reflex (unclear; possibly cardioprotective) Miscellaneous • Endothelium-derived factors - Endothelin - Kinins - Nitric oxide - Prostacyclin, etc. • Hormones - Adenosine - Angiotensin II - Noradrenaline & adrenaline - Vasopressin, etc. • ATP-sensitive potassium channel
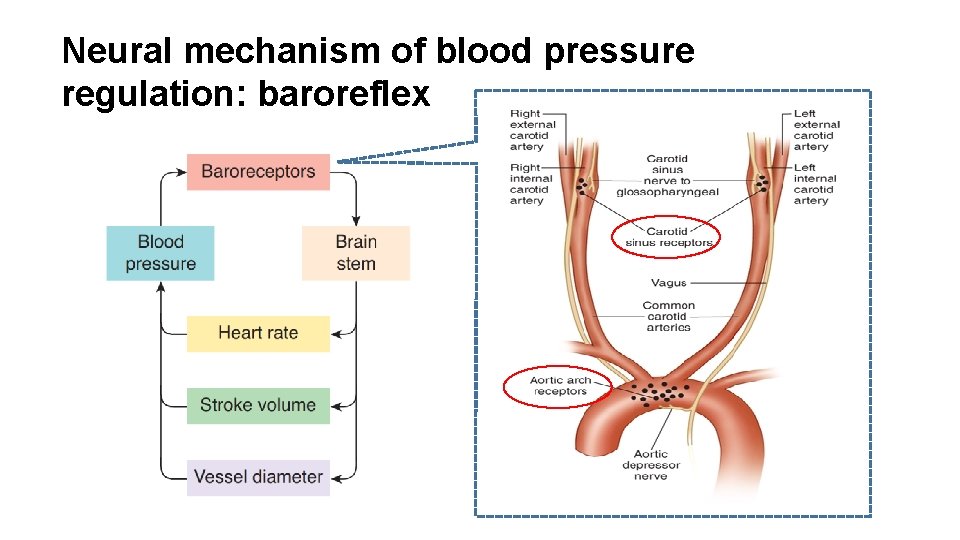
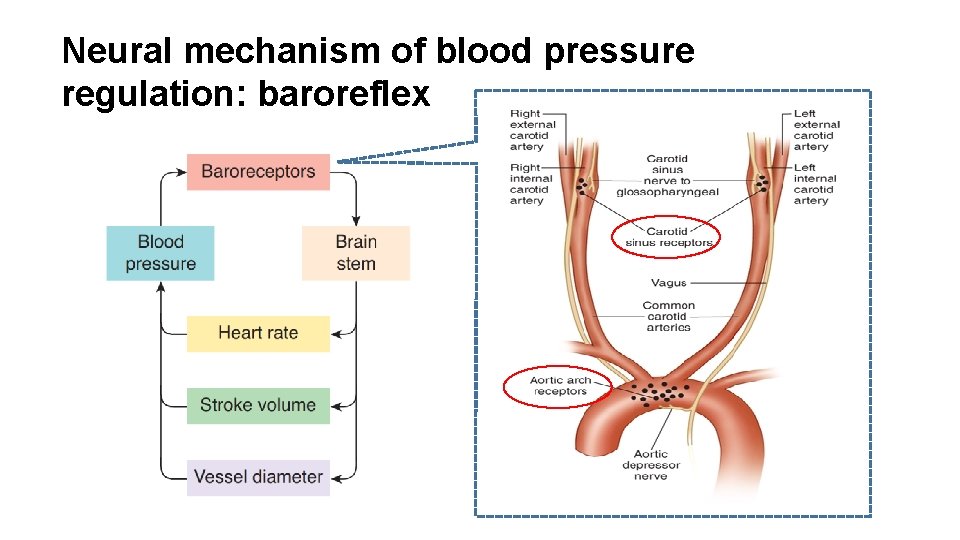
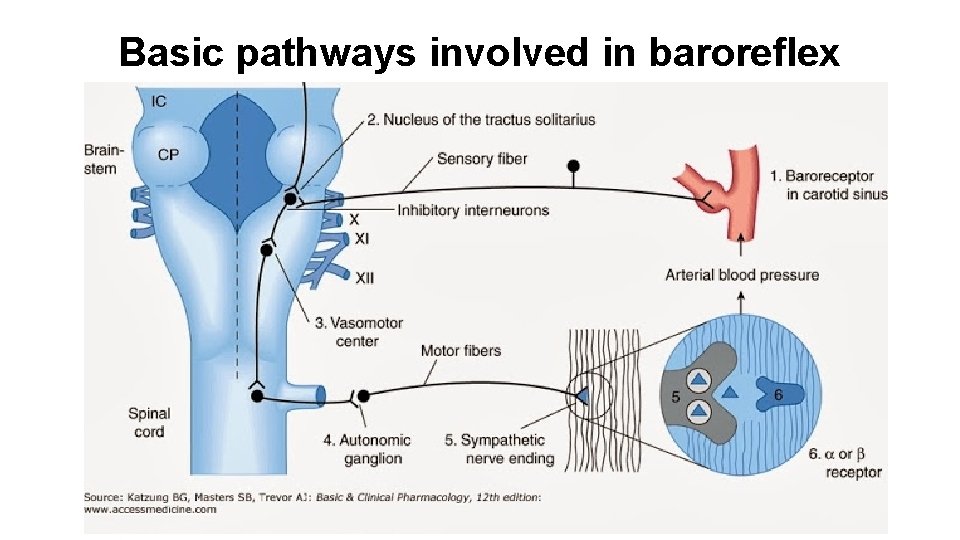
Neural mechanism of blood pressure regulation: baroreflex
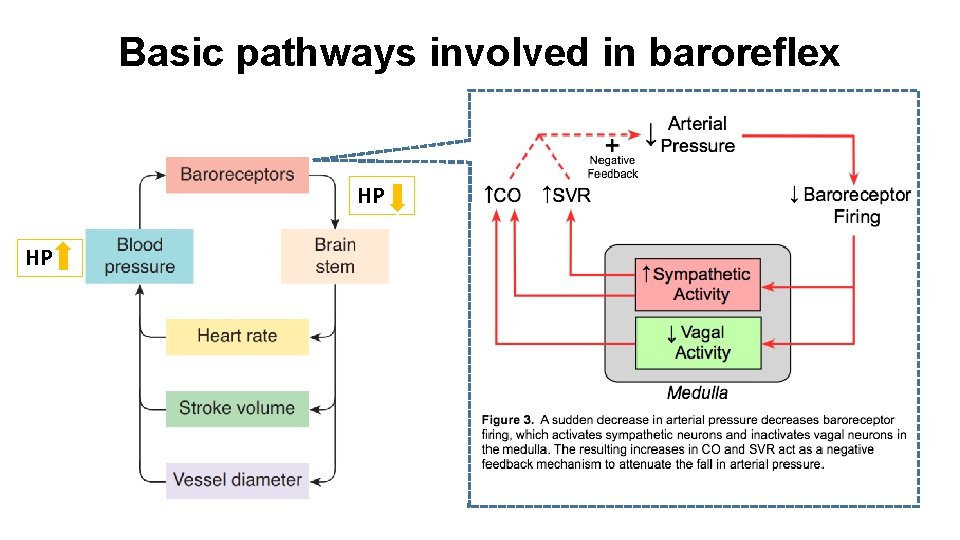
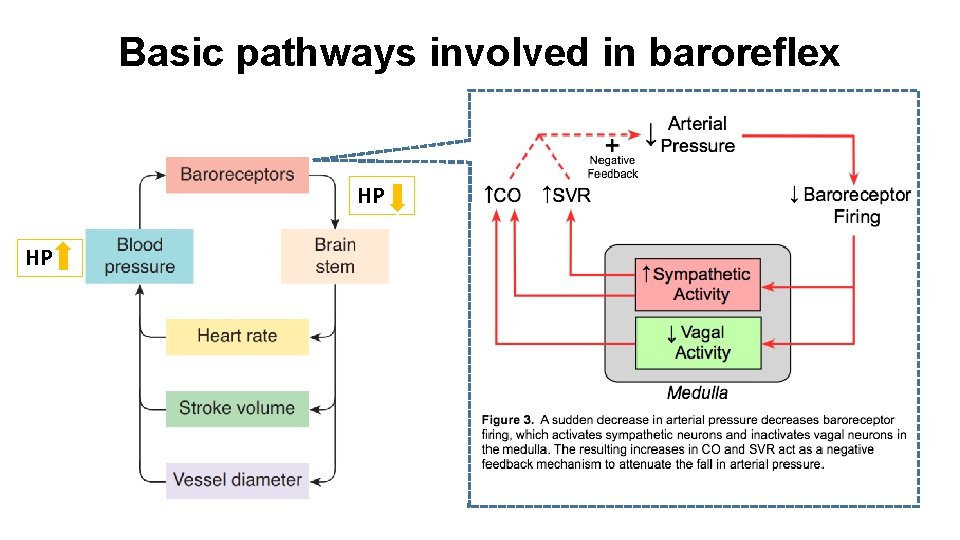
Basic pathways involved in baroreflex HP HP
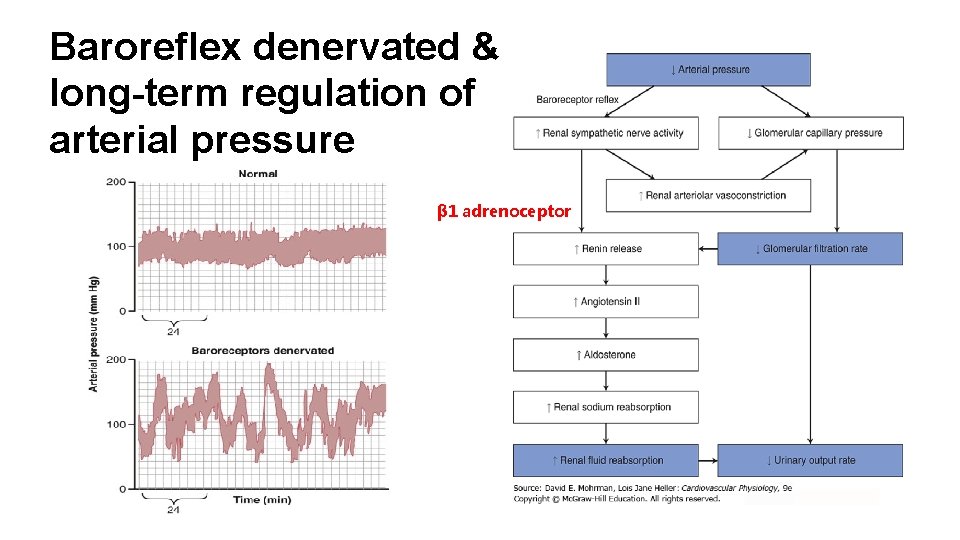
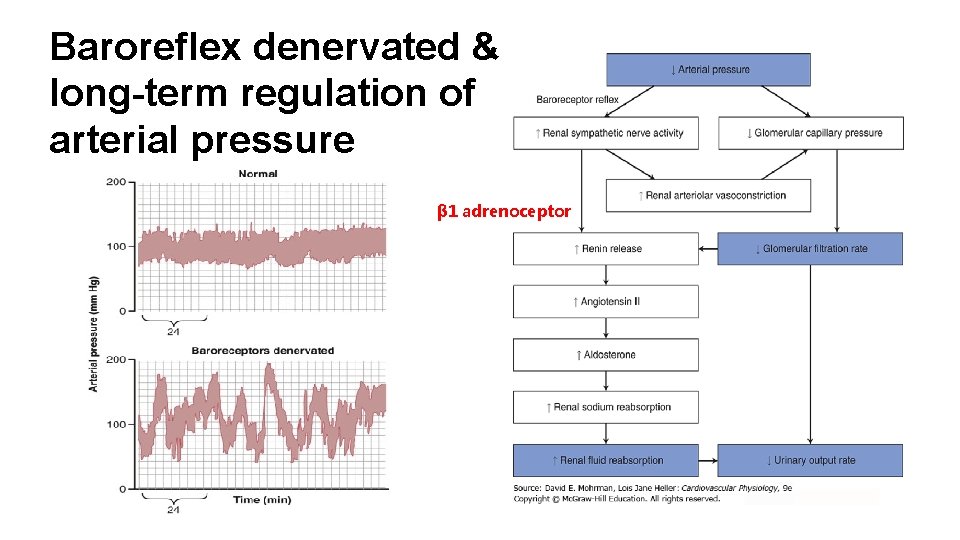
Baroreflex denervated & long-term regulation of arterial pressure β 1 adrenoceptor
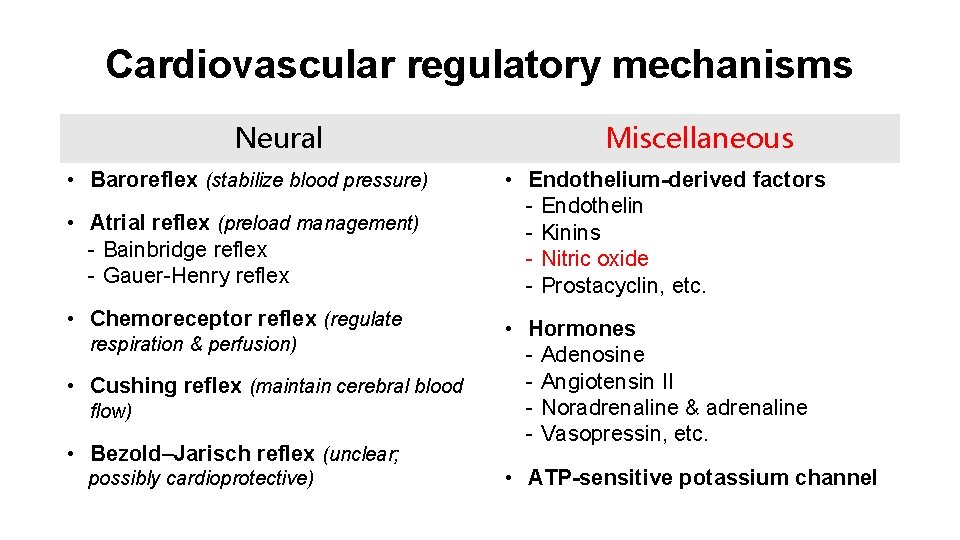
Cardiovascular regulatory mechanisms Neural • Baroreflex (stabilize blood pressure) • Atrial reflex (preload management) - Bainbridge reflex - Gauer-Henry reflex • Chemoreceptor reflex (regulate respiration & perfusion) • Cushing reflex (maintain cerebral blood flow) • Bezold–Jarisch reflex (unclear; possibly cardioprotective) Miscellaneous • Endothelium-derived factors - Endothelin - Kinins - Nitric oxide - Prostacyclin, etc. • Hormones - Adenosine - Angiotensin II - Noradrenaline & adrenaline - Vasopressin, etc. • ATP-sensitive potassium channel
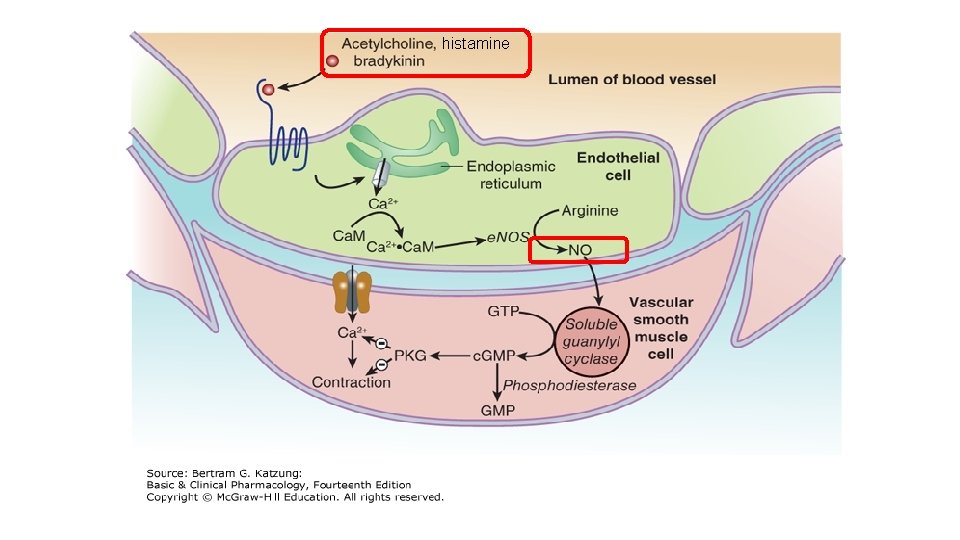
histamine
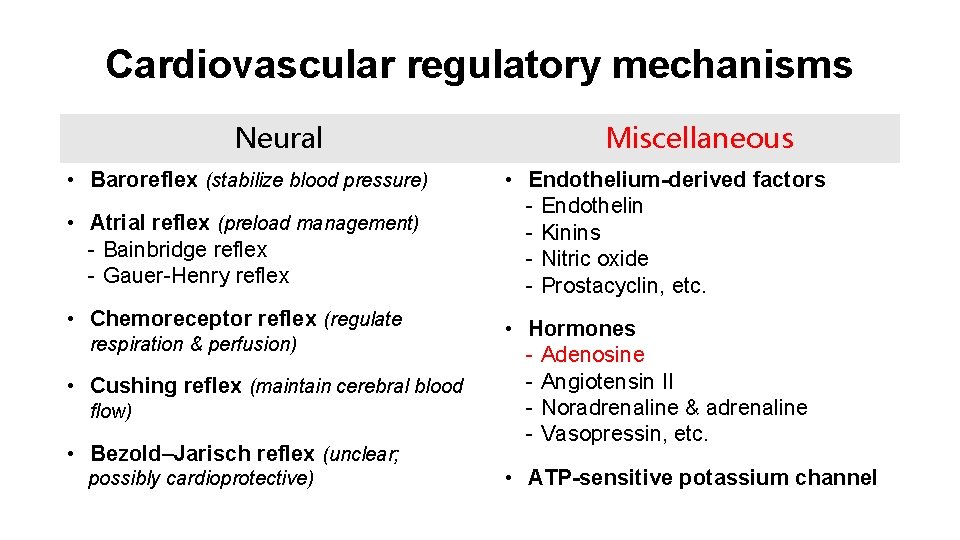
Cardiovascular regulatory mechanisms Neural • Baroreflex (stabilize blood pressure) • Atrial reflex (preload management) - Bainbridge reflex - Gauer-Henry reflex • Chemoreceptor reflex (regulate respiration & perfusion) • Cushing reflex (maintain cerebral blood flow) • Bezold–Jarisch reflex (unclear; possibly cardioprotective) Miscellaneous • Endothelium-derived factors - Endothelin - Kinins - Nitric oxide - Prostacyclin, etc. • Hormones - Adenosine - Angiotensin II - Noradrenaline & adrenaline - Vasopressin, etc. • ATP-sensitive potassium channel
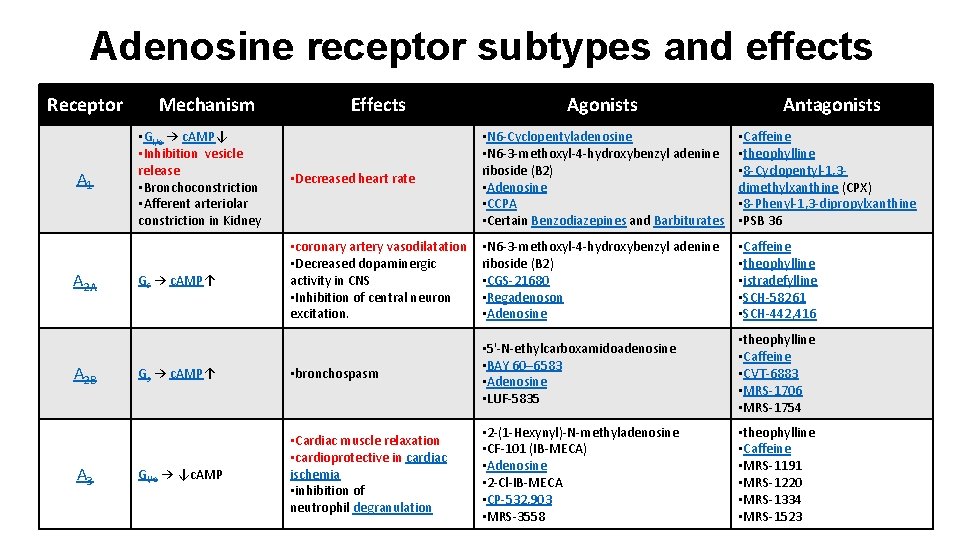
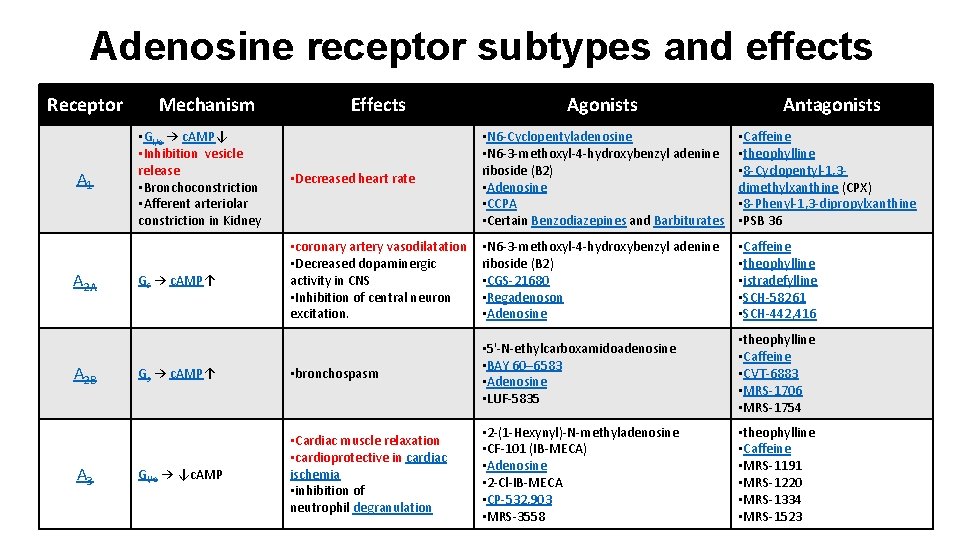
Adenosine receptor subtypes and effects Receptor A 1 A 2 A A 2 B A 3 Mechanism • Gi/o → c. AMP↓ • Inhibition vesicle release • Bronchoconstriction • Afferent arteriolar constriction in Kidney Gs → c. AMP↑ Effects Agonists Antagonists • Decreased heart rate • N 6 -Cyclopentyladenosine • N 6 -3 -methoxyl-4 -hydroxybenzyl adenine riboside (B 2) • Adenosine • CCPA • Certain Benzodiazepines and Barbiturates • Caffeine • theophylline • 8 -Cyclopentyl-1, 3 dimethylxanthine (CPX) • 8 -Phenyl-1, 3 -dipropylxanthine • PSB 36 • coronary artery vasodilatation • Decreased dopaminergic activity in CNS • Inhibition of central neuron excitation. • N 6 -3 -methoxyl-4 -hydroxybenzyl adenine riboside (B 2) • CGS-21680 • Regadenoson • Adenosine • Caffeine • theophylline • istradefylline • SCH-58261 • SCH-442, 416 Gs → c. AMP↑ • bronchospasm • 5'-N-ethylcarboxamidoadenosine • BAY 60– 6583 • Adenosine • LUF-5835 • theophylline • Caffeine • CVT-6883 • MRS-1706 • MRS-1754 Gi/o → ↓c. AMP • Cardiac muscle relaxation • cardioprotective in cardiac ischemia • inhibition of neutrophil degranulation • 2 -(1 -Hexynyl)-N-methyladenosine • CF-101 (IB-MECA) • Adenosine • 2 -Cl-IB-MECA • CP-532, 903 • MRS-3558 • theophylline • Caffeine • MRS-1191 • MRS-1220 • MRS-1334 • MRS-1523
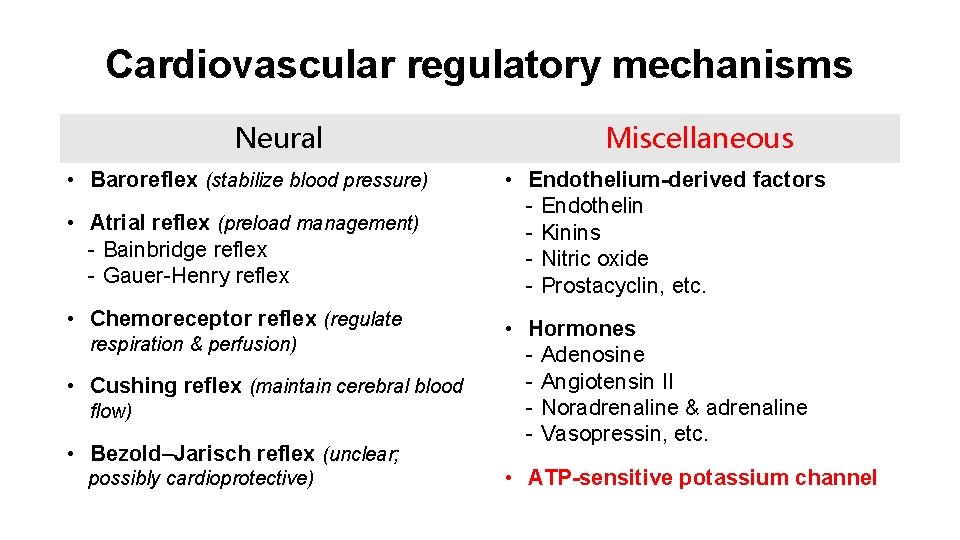
Cardiovascular regulatory mechanisms Neural • Baroreflex (stabilize blood pressure) • Atrial reflex (preload management) - Bainbridge reflex - Gauer-Henry reflex • Chemoreceptor reflex (regulate respiration & perfusion) • Cushing reflex (maintain cerebral blood flow) • Bezold–Jarisch reflex (unclear; possibly cardioprotective) Miscellaneous • Endothelium-derived factors - Endothelin - Kinins - Nitric oxide - Prostacyclin, etc. • Hormones - Adenosine - Angiotensin II - Noradrenaline & adrenaline - Vasopressin, etc. • ATP-sensitive potassium channel
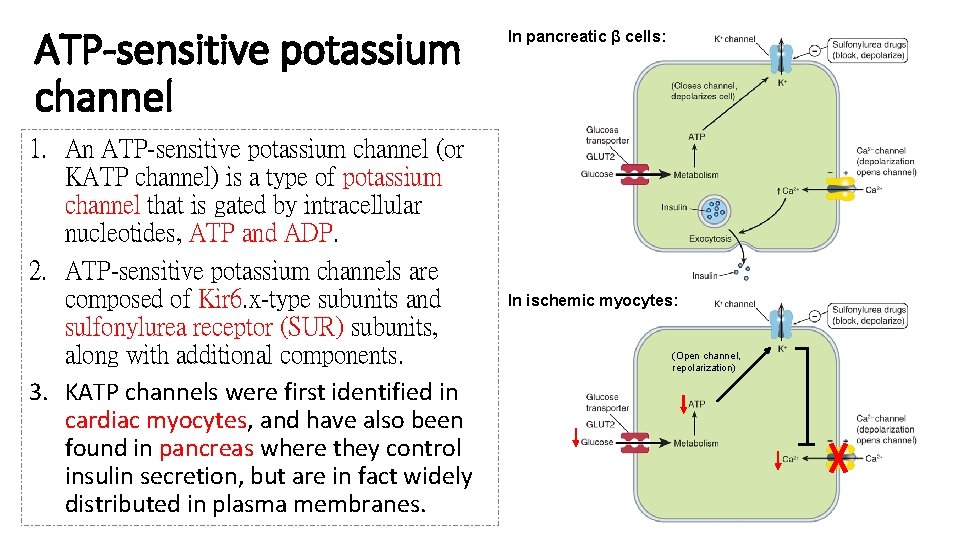
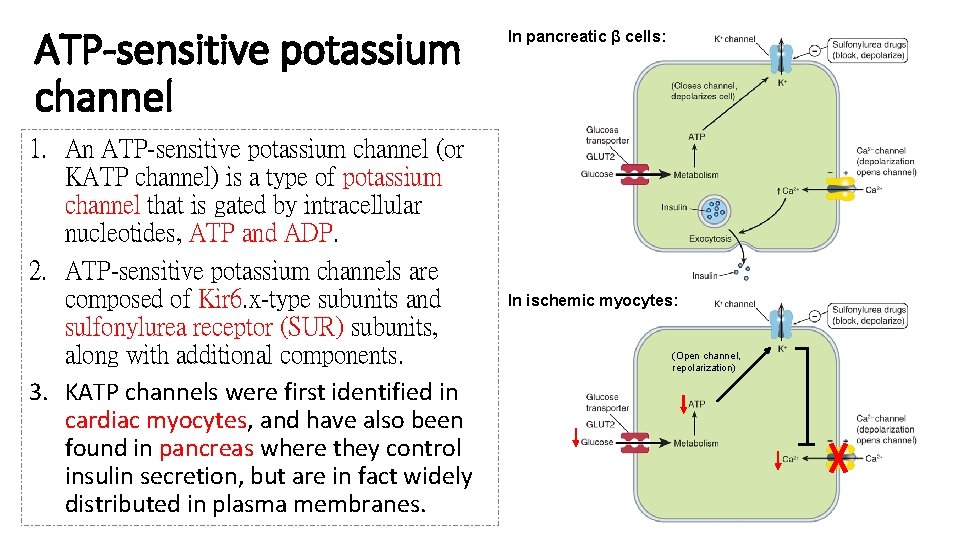
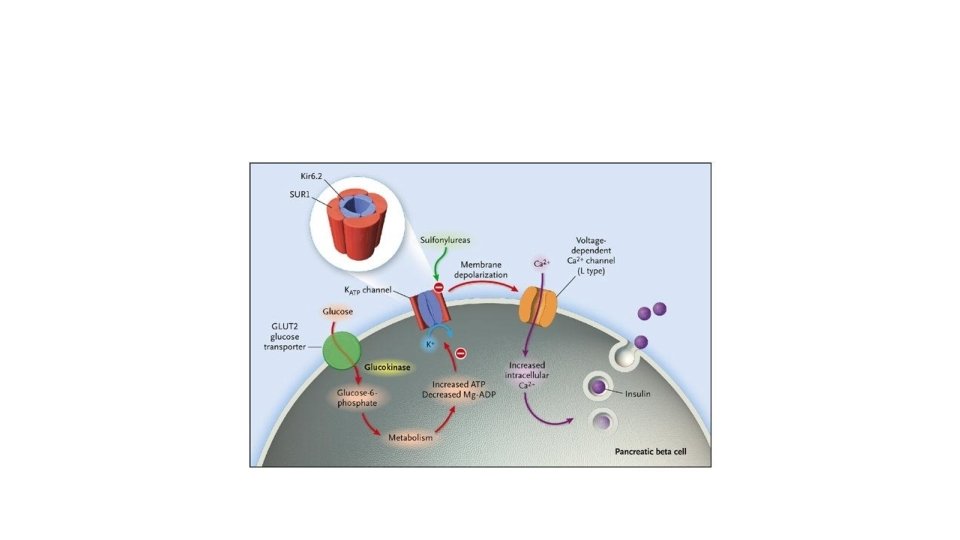
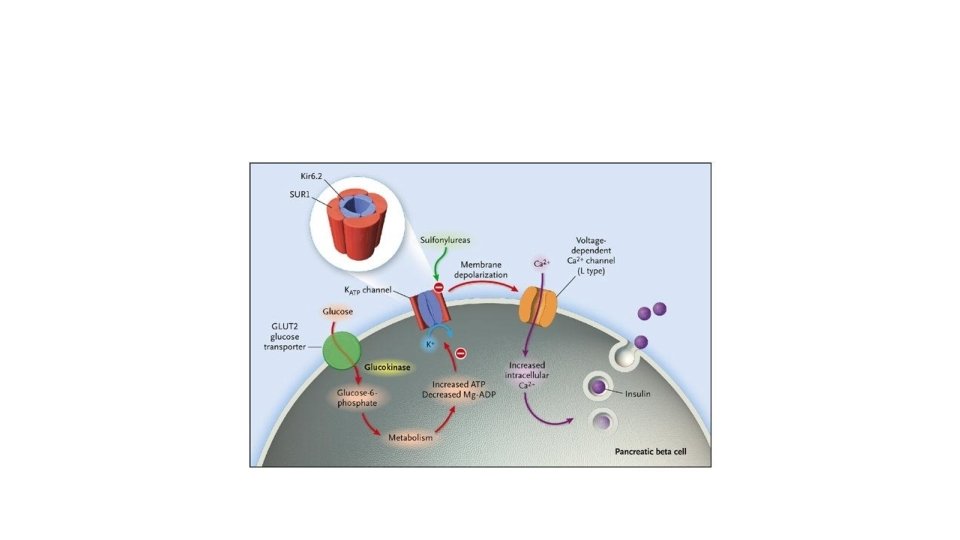
ATP-sensitive potassium channel 1. An ATP-sensitive potassium channel (or KATP channel) is a type of potassium channel that is gated by intracellular nucleotides, ATP and ADP. 2. ATP-sensitive potassium channels are composed of Kir 6. x-type subunits and sulfonylurea receptor (SUR) subunits, along with additional components. 3. KATP channels were first identified in cardiac myocytes, and have also been found in pancreas where they control insulin secretion, but are in fact widely distributed in plasma membranes. In pancreatic β cells: In ischemic myocytes: (Open channel, repolarization)
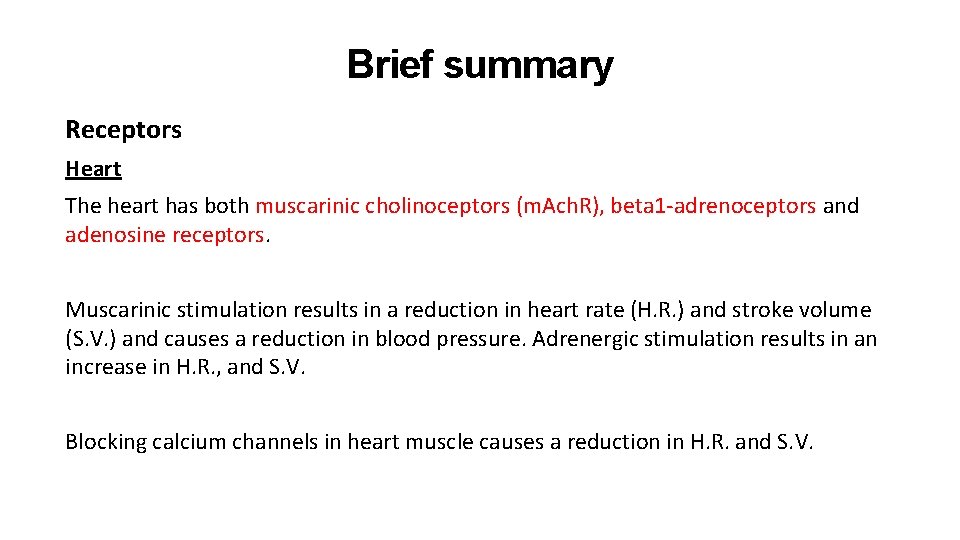
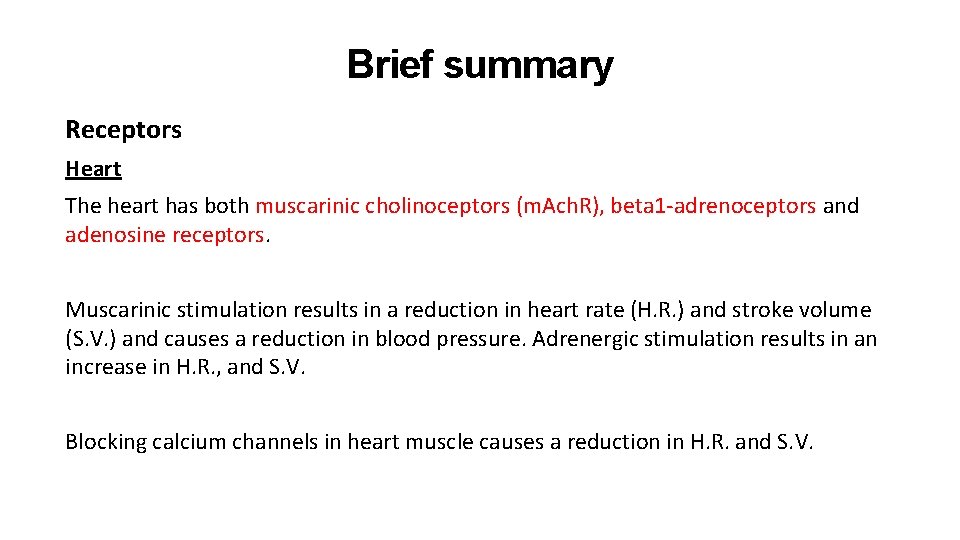
Brief summary Receptors Heart The heart has both muscarinic cholinoceptors (m. Ach. R), beta 1 -adrenoceptors and adenosine receptors. Muscarinic stimulation results in a reduction in heart rate (H. R. ) and stroke volume (S. V. ) and causes a reduction in blood pressure. Adrenergic stimulation results in an increase in H. R. , and S. V. Blocking calcium channels in heart muscle causes a reduction in H. R. and S. V.
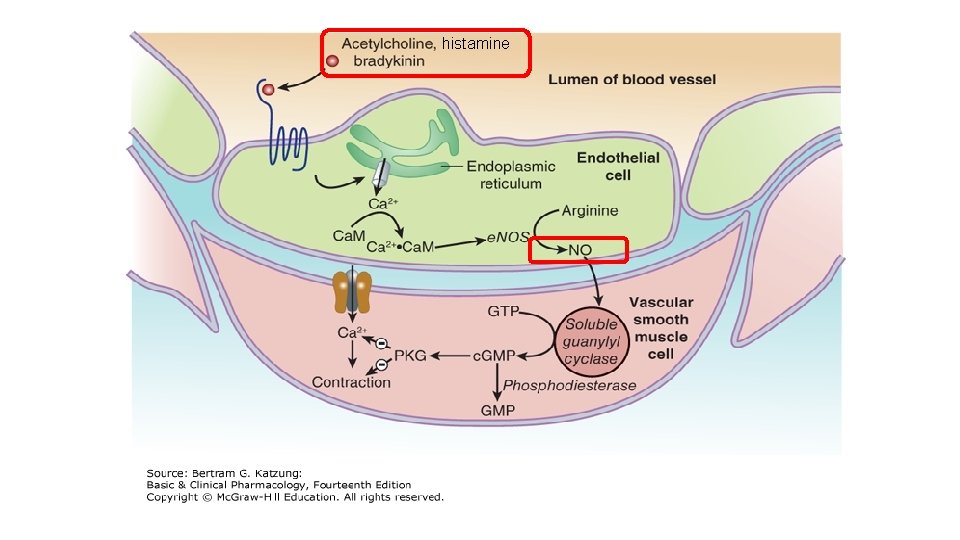
Brief summary Receptors Blood vessels • Alpha 1 -adrenoceptors on blood vessels cause vasoconstriction, increasing peripheral resistance. • Beta 2 -adrenoceptors on blood vessels cause vasodilation. • Agents which open smooth muscle potassium ion channels cause vasodilation. • Nitrovasodilators cause vasodilation by generating nitric oxide. • Angiotensin I is converted to angiotension II and causes vasoconstriction
Thanks for your attention!
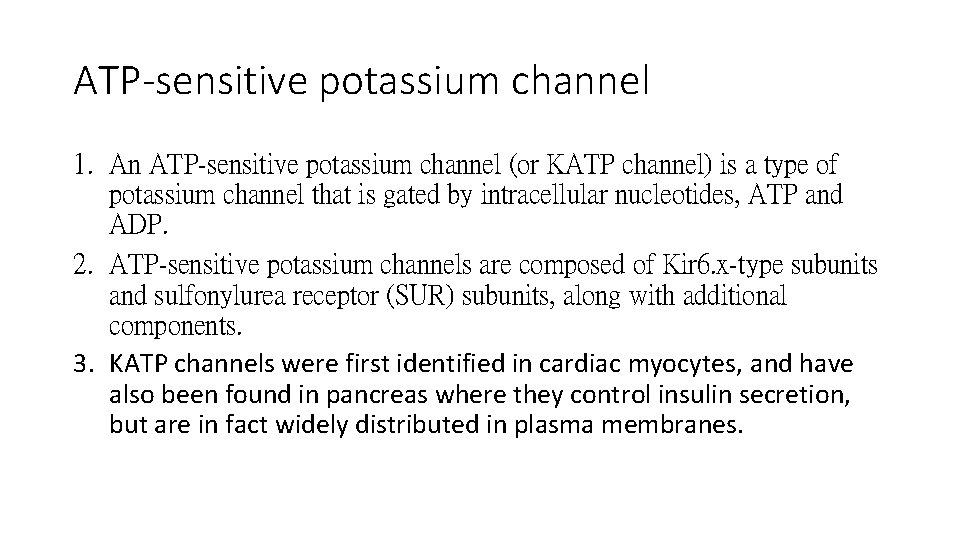
ATP-sensitive potassium channel 1. An ATP-sensitive potassium channel (or KATP channel) is a type of potassium channel that is gated by intracellular nucleotides, ATP and ADP. 2. ATP-sensitive potassium channels are composed of Kir 6. x-type subunits and sulfonylurea receptor (SUR) subunits, along with additional components. 3. KATP channels were first identified in cardiac myocytes, and have also been found in pancreas where they control insulin secretion, but are in fact widely distributed in plasma membranes.
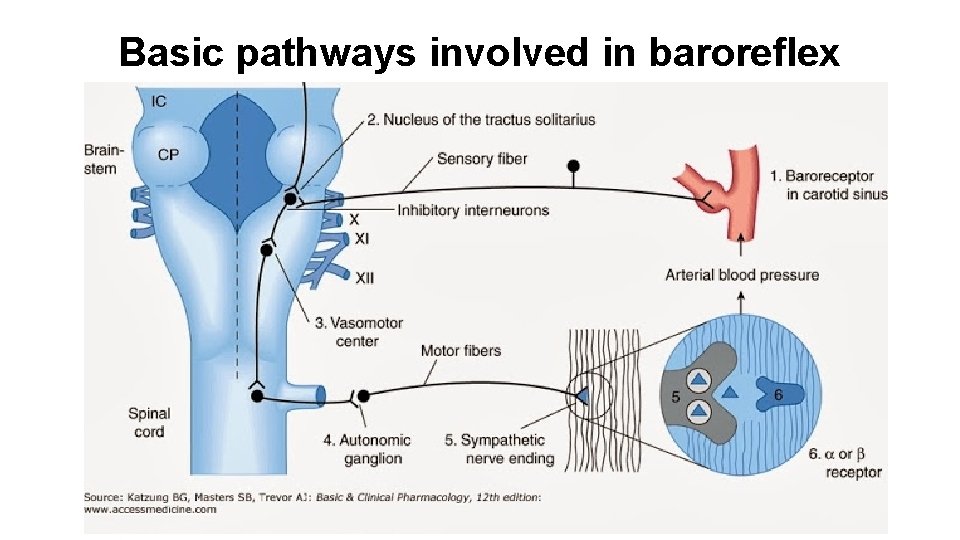
Basic pathways involved in baroreflex
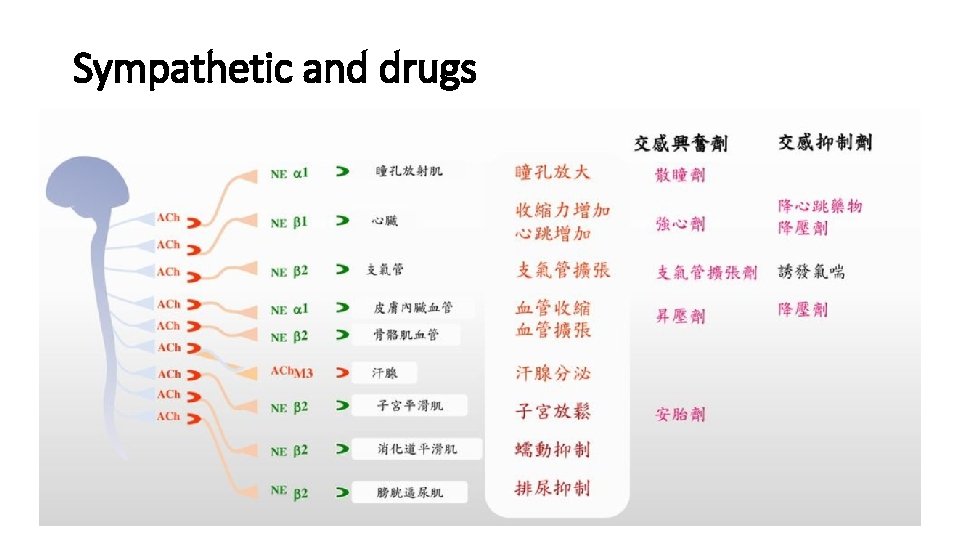
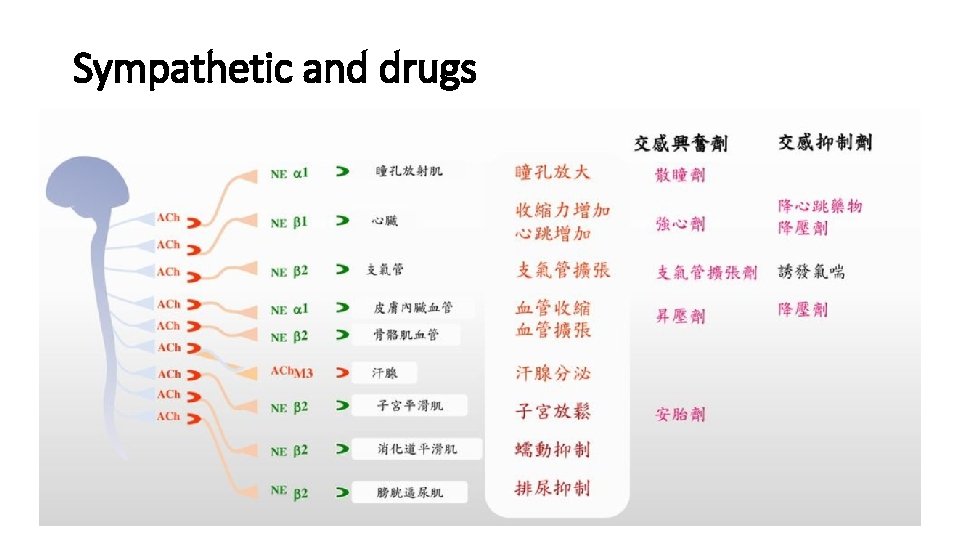
Sympathetic and drugs
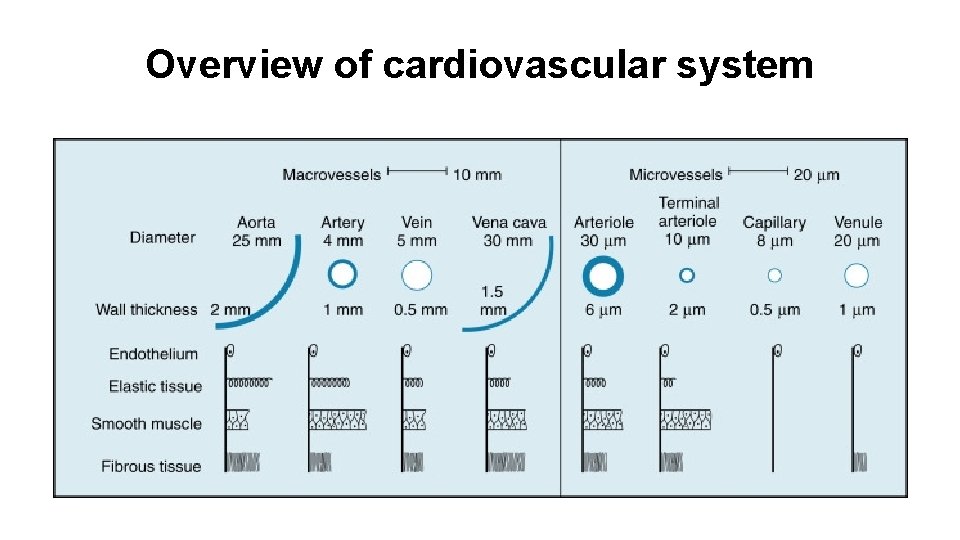
Overview of cardiovascular system
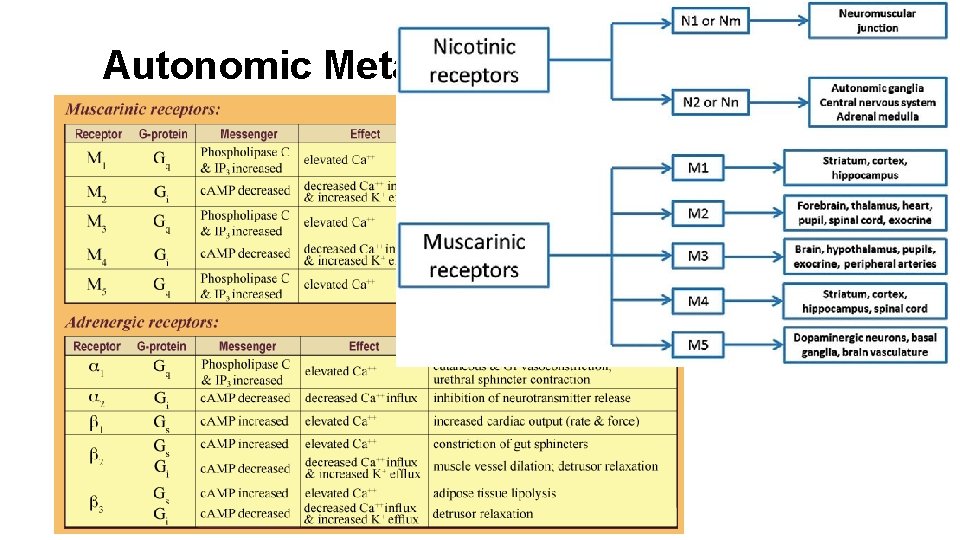
Autonomic Metabotrophic Receptors