PICU Analgesia Sedation Algorithm for Endotracheally Intubated Patients
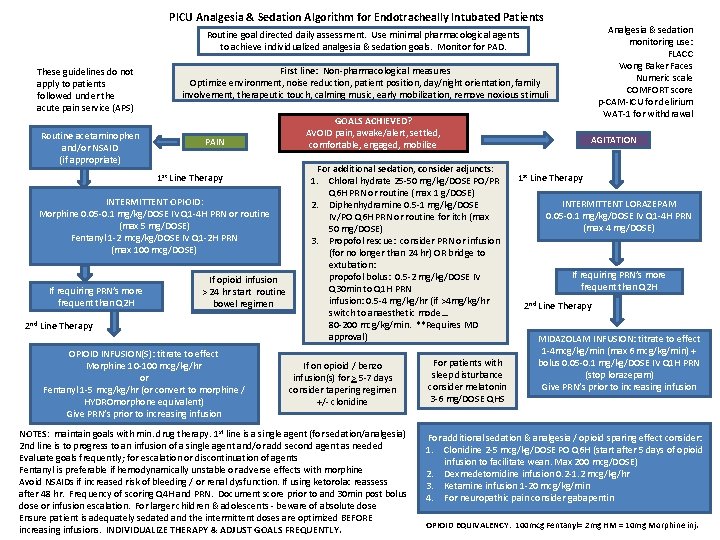
PICU Analgesia & Sedation Algorithm for Endotracheally Intubated Patients Analgesia & sedation monitoring use: FLACC Wong Baker Faces Numeric scale COMFORT score p-CAM-ICU for delirium WAT-1 for withdrawal Routine goal directed daily assessment. Use minimal pharmacological agents to achieve individualized analgesia & sedation goals. Monitor for PAD. These guidelines do not apply to patients followed under the acute pain service (APS) Routine acetaminophen and/or NSAID (if appropriate) First line: Non-pharmacological measures Optimize environment, noise reduction, patient position, day/night orientation, family involvement, therapeutic touch, calming music, early mobilization, remove noxious stimuli PAIN 1 st Line Therapy INTERMITTENT OPIOID: Morphine 0. 05 -0. 1 mg/kg/DOSE IV IV Q 1 -4 H PRN or or routine (max 5 5 mg/DOSE) Fentanyl 1 -2 mcg/kg/DOSE IV IV Q 1 -2 H PRN (max 100 mcg/DOSE) If If requiring PRN’s more frequent than Q 2 H If If opioid infusion >> 24 24 hr hr start routine bowel regimen 2 nd Line Therapy OPIOID INFUSION(S): titrate to effect Morphine 10 -100 mcg/kg/hr or Fentanyl 1 -5 mcg/kg/hr (or convert to morphine / HYDROmorphone equivalent) Give PRN’s prior to increasing infusion GOALS ACHIEVED? AVOID pain, awake/alert, settled, comfortable, engaged, mobilize For additional sedation, consider adjuncts: 1. Chloral hydrate 25 -50 mg/kg/DOSE PO/PR Q 6 H PRN or routine (max 1 g/DOSE) 2. Diphenhydramine 0. 5 -1 mg/kg/DOSE IV/PO Q 6 H PRN or routine for itch (max 50 mg/DOSE) 3. Propofol rescue: consider PRN or infusion (for no longer than 24 hr) OR bridge to extubation: propofol bolus: 0. 5 -2 mg/kg/DOSE IV Q 30 min to Q 1 H PRN infusion: 0. 5 -4 mg/kg/hr (if >4 mg/kg/hr switch to anaesthetic mode… 80 -200 mcg/kg/min. **Requires MD approval) If on opioid / benzo infusion(s) for > 5 -7 days consider tapering regimen +/- clonidine NOTES: maintain goals with min. drug therapy. 1 st line is a single agent (for sedation/analgesia) 2 nd line is to progress to an infusion of a single agent and/or add second agent as needed Evaluate goals frequently; for escalation or discontinuation of agents Fentanyl is preferable if hemodynamically unstable or adverse effects with morphine Avoid NSAIDs if increased risk of bleeding / or renal dysfunction. If using ketorolac reassess after 48 hr. Frequency of scoring Q 4 H and PRN. Document score prior to and 30 min post bolus dose or infusion escalation. For larger children & adolescents - beware of absolute dose Ensure patient is adequately sedated and the intermittent doses are optimized BEFORE increasing infusions. INDIVIDUALIZE THERAPY & ADJUST GOALS FREQUENTLY. For patients with sleep disturbance consider melatonin 3 -6 mg/DOSE QHS AGITATION 1 st Line Therapy INTERMITTENT LORAZEPAM 0. 05 -0. 1 mg/kg/DOSE IV Q 1 -4 H PRN (max 4 mg/DOSE) If requiring PRN’s more frequent than Q 2 H 2 nd Line Therapy MIDAZOLAM INFUSION: titrate to effect 1 -4 mcg/kg/min (max 6 mcg/kg/min) + bolus 0. 05 -0. 1 mg/kg/DOSE IV Q 1 H PRN (stop lorazepam) Give PRN’s prior to increasing infusion For additional sedation & analgesia / opioid sparing effect consider: 1. Clonidine 2 -5 mcg/kg/DOSE PO Q 6 H (start after 5 days of opioid infusion to facilitate wean. Max 200 mcg/DOSE) 2. Dexmedetomidine infusion 0. 2 -1. 2 mcg/kg/hr 3. Ketamine infusion 1 -20 mcg/kg/min 4. For neuropathic pain consider gabapentin OPIOID EQUIVALENCY: 100 mcg Fentanyl= 2 mg HM = 10 mg Morphine inj.

Opioid and Benzodiazepine Infusions Tapering Algorithm Routine goal directed daily assessment. Individualize analgesia & sedation taper. Monitor for withdrawal (WAT-1 scores done Q 4 H & PRN) LOW RISK OF WITHDRAWAL OPIOID EQUIVALENCY: 100 mcg Fentanyl= 2 mg HM = 10 mg Morphine IV >5 -7 days of continuous IV infusions HIGH cumulative dose < 5 days of continuous IV infusions Increase infusion(s) to 80% of original dose Discontinue IV infusions Continue intermittent agents PRN and consider switching to longer acting agents END POINTS any 1 of the following >3 PRN’s in 3 hours WAT-1 scores > 3 Cardiorespiratory instability and/or Ventilator dysynchrony despite PRN doses RESUME infusion(s) at 50% of original dose Adjust dose(s) to achieve GOALS WAT-1 scores < 3 on 2 separate occurrence's HIGH RISK OF WITHDRAWAL ANY 1 of ENDPOINTS met? WAT-1 scores >3 Continue to WEAN by 10 -20% Q 4 -24 H as tolerated Continue intermittent agents PRN for WAT-1 scores > 3 Tolerating wean, WAT-1 score < 3 Reduce IV infusion(s) by 50% Consider alternating if on two different infusions (ie. narcotic & benzo) Continue intermittent agents PRN *IF PATIENT IS IN WITHDRAWAL: Consider discontinuing infusion Switch to intermittent opioid & benzo (either IV or enteral) Convert to longer acting agents (hydromorphone, morphine & lorazepam) For patients with sleep disturbance consider melatonin 3 -6 mg/DOSE QHS NOTE: Length of taper will depend on number of infusion days as well as maximum doses reached to achieve analgesia & sedation targets. Dexmedetomidine may be used as a strategy to reduce narcotic infusion dose. If continued for > 7 days wean infusion by 0. 2 -0. 5 mcg/kg/hr Q 8 -24 H; then consider clonidine. If transferring to floor complete narcotic infusion order set. Administer PRN doses of opioid / or benzodiazepine to treat symptoms, based on WAT-1 scores > 3 Consider increasing background infusion by 10 -20% to achieve targets. Consider clonidine 2 -5 mcg/kg/DOSE PO/NG Q 6 H (taper over 48 hours once opioids and benzodiazepines are discontinued) Monitor for delirium using p-CAM-ICU score **IF PATIENT HAS DELIRIUM: 1. Discontinue / minimize use of opioids & benzos 2. Discontinue anticholinergic meds ie. diphenhydramine, ranitidine, dimenhydrinate, etc. 3. Institute non-drug measures: sleep hygiene, day/night activity, noise reduction, orientation 4. Consider atypical anti-psychotic (quetiapine, olanzapine, risperidone, chlorpromazine, haldol)
- Slides: 2