Pictorial review of intracranial MRV techniques pitfalls and




- Slides: 38
Pictorial review of intracranial MRV techniques, pitfalls, and common pathologies involving the cerebral venous system Jennifer Trinh, MD Rajul Pandit, MD Mahesh R. Patel, MD Santa Clara Valley Medical Center, San Jose, CA Control #806 e. Ed. E-44
Disclosures • There are no financial disclosures.
Objectives • Know the advantages and disadvantages of two noncontrast based MR venography (MRV) techniques and their pitfalls • Review the anatomy of the cerebral venous system • Know the common sites of cerebral venous thrombosis (CVT) • Illustrate common etiologies of CVT and occlusion
Introduction • The cerebral venous system can be difficult to evaluate due to artifacts, variant anatomy, and overlapping signal intensities of venous flow. • Several MRV methods are available to image the intracranial venous system. • These methods include both non-contrast and contrast based techniques.
MRV Techniques • Two non-contrast based MRV techniques are utilized at our institution. – 2 -D time of flight (TOF) MRV is obtained with the source data in the coronal plane. – 3 -D phase contrast MRV is obtained with the source data in the sagittal plane. • Contrast-enhanced MRV is another technique that is used at other institutions. – This technique relies on the paramagnetic effect of intravenous gadolinium to shorten T 1 and provide intravascular contrast enhancement.
Signal Generation in Non-Contrast MRV • Time of Flight – TOF uses flow phenomenon for signal generation. Blood flowing into the slice is not saturated and appears bright relative to the dark (suppressed) background. A saturation band is applied above the slice to suppress inflowing arterial signal. • Phase Contrast – Spins that are moving in the same direction as a magnetic field gradient develop a phase shift that is proportional to the velocity of the spins. Bipolar gradients (two gradients with equal magnitude but opposite direction) are used to encode the velocity of the spins. – The signal in the vein depends on the velocity of the flowing blood and the velocity encoding by the technician.
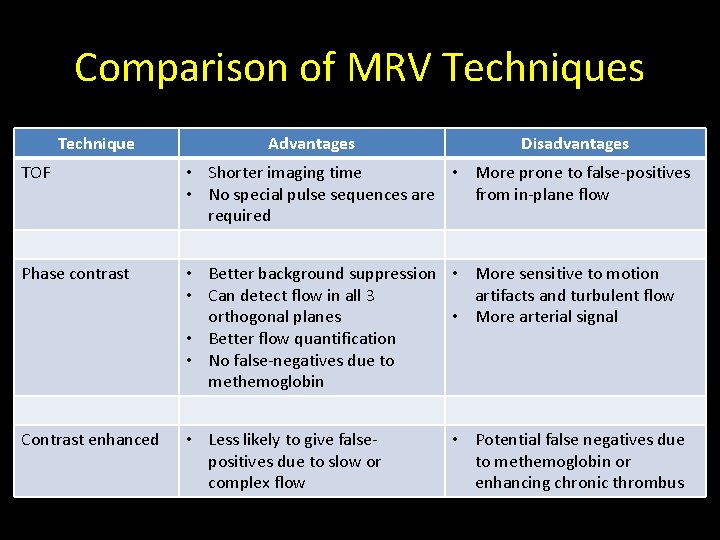
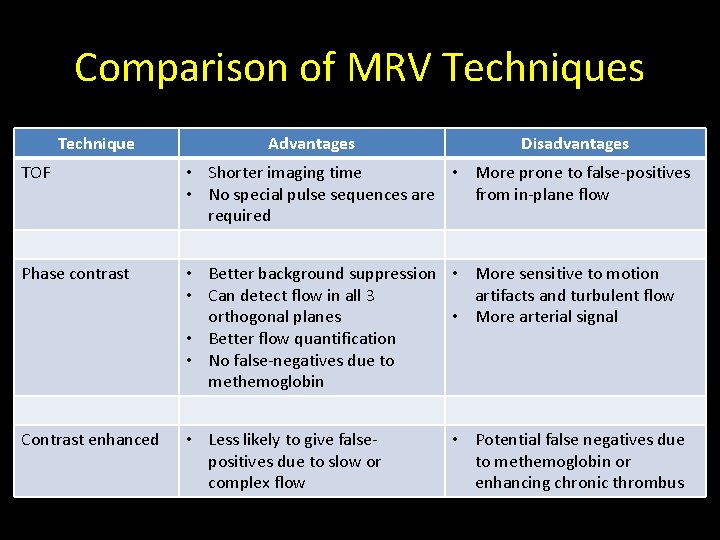
Comparison of MRV Techniques Technique Advantages Disadvantages TOF • Shorter imaging time • More prone to false-positives • No special pulse sequences are from in-plane flow required Phase contrast • Better background suppression • More sensitive to motion • Can detect flow in all 3 artifacts and turbulent flow orthogonal planes • More arterial signal • Better flow quantification • No false-negatives due to methemoglobin Contrast enhanced • Less likely to give falsepositives due to slow or complex flow • Potential false negatives due to methemoglobin or enhancing chronic thrombus
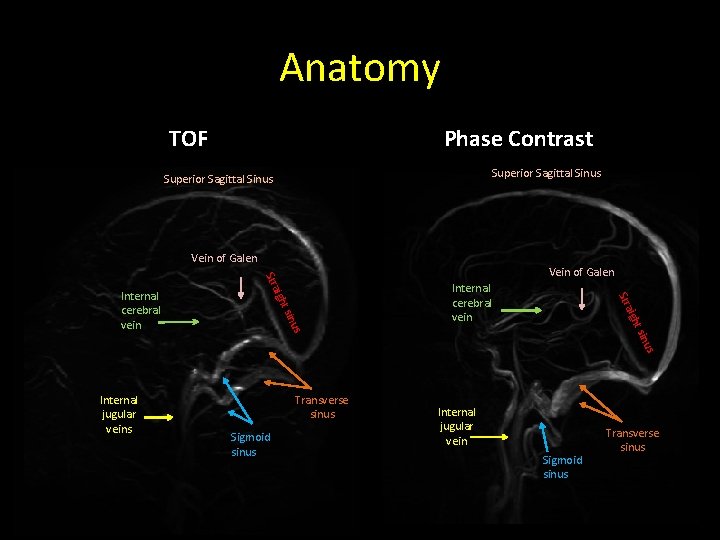
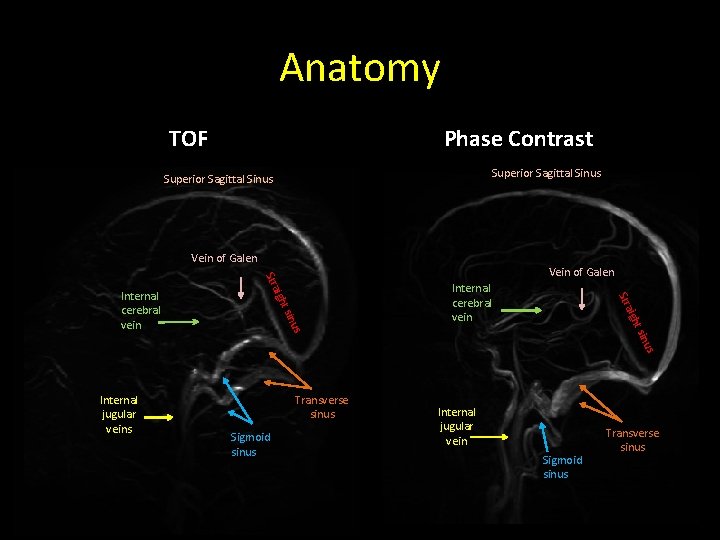
Anatomy TOF Phase Contrast Superior Sagittal Sinus Vein of Galen Stra Internal cerebral vein t si h aig Str nus t si igh Internal cerebral vein Vein of Galen nus Internal jugular veins Transverse sinus Sigmoid sinus Internal jugular vein Sigmoid sinus Transverse sinus
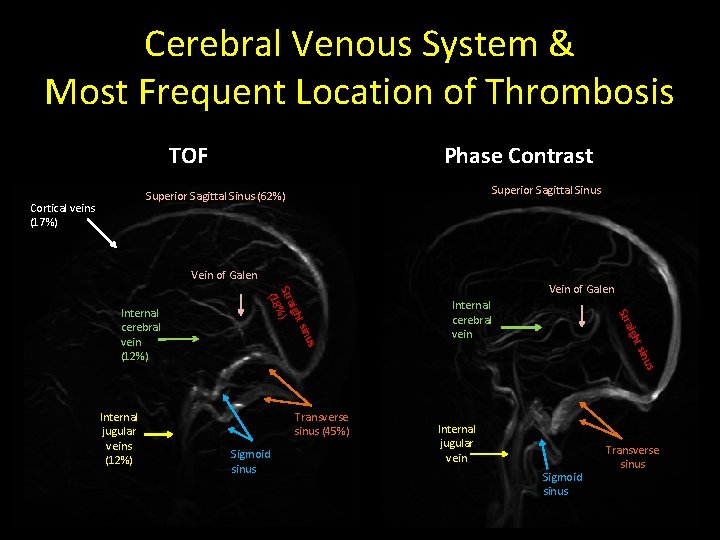
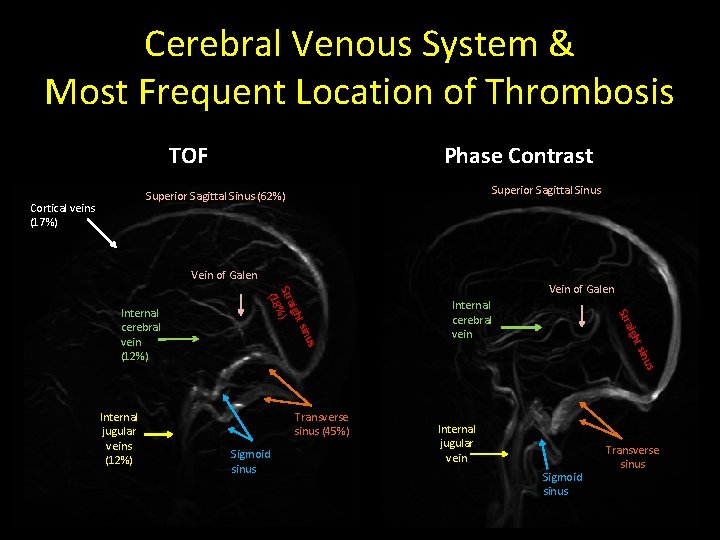
Cerebral Venous System & Most Frequent Location of Thrombosis TOF Phase Contrast Superior Sagittal Sinus (62%) Cortical veins (17%) Vein of Galen t si h aig Str Internal cerebral vein nus Internal jugular veins (12%) t si igh Stra ) % (18 Internal cerebral vein (12%) Vein of Galen Transverse sinus (45%) Sigmoid sinus Internal jugular vein Sigmoid sinus Transverse sinus

ARTIFACTS
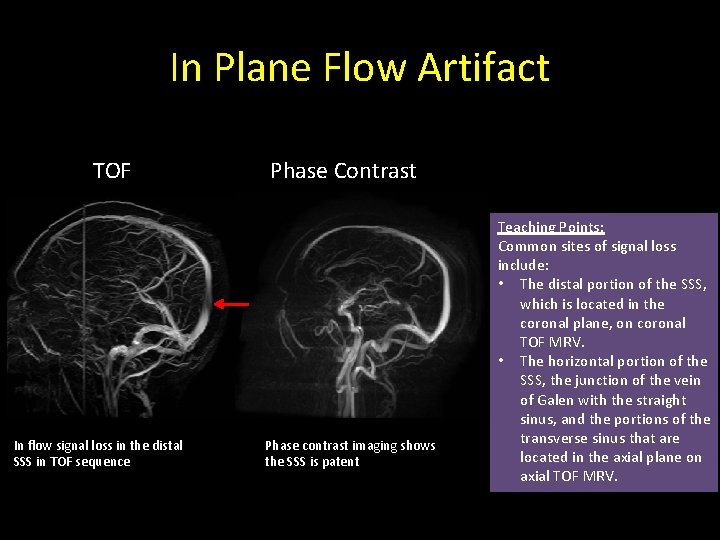
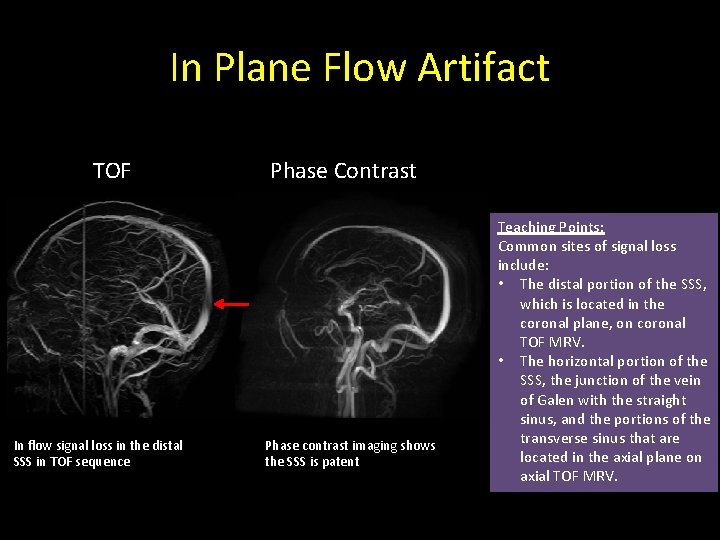
In Plane Flow Artifact TOF In flow signal loss in the distal SSS in TOF sequence Phase Contrast Phase contrast imaging shows the SSS is patent Teaching Points: Common sites of signal loss include: • The distal portion of the SSS, which is located in the coronal plane, on coronal TOF MRV. • The horizontal portion of the SSS, the junction of the vein of Galen with the straight sinus, and the portions of the transverse sinus that are located in the axial plane on axial TOF MRV.
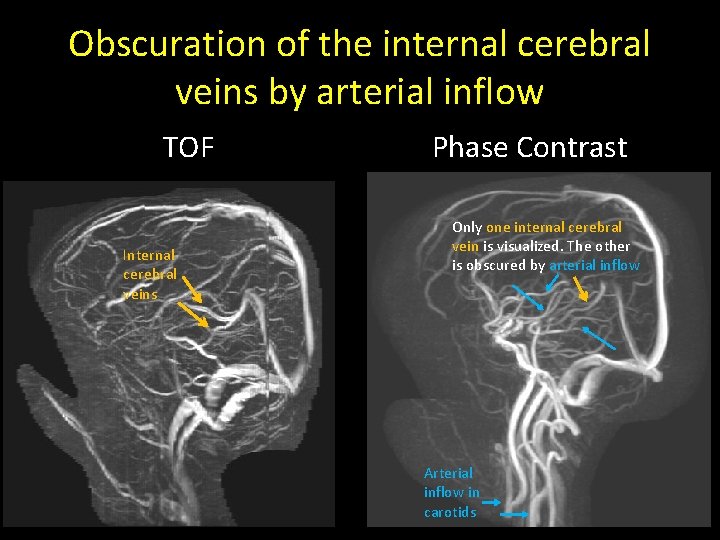
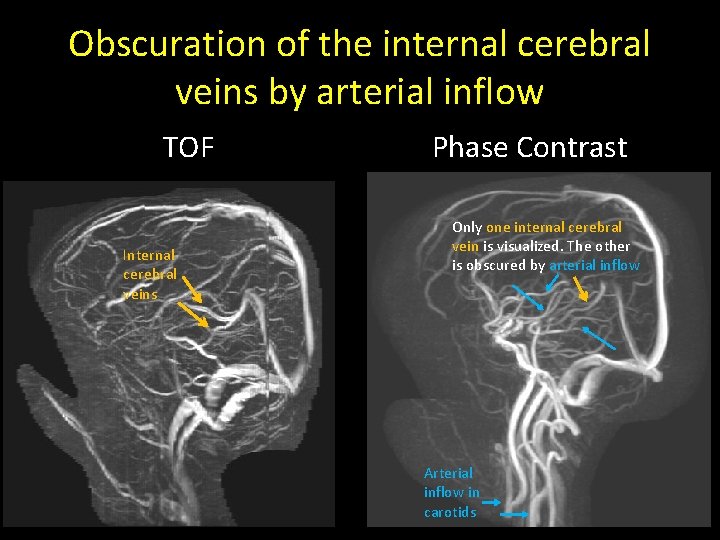
Obscuration of the internal cerebral veins by arterial inflow TOF Internal cerebral veins Phase Contrast Only one internal cerebral vein is visualized. The other is obscured by arterial inflow Arterial inflow in carotids
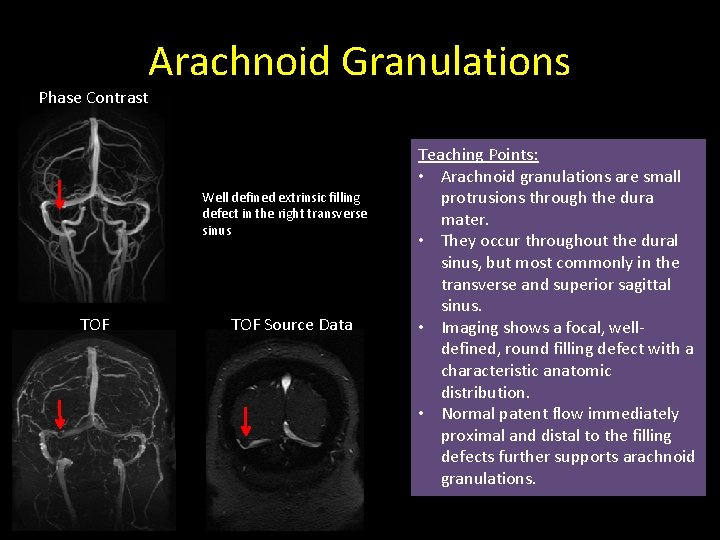
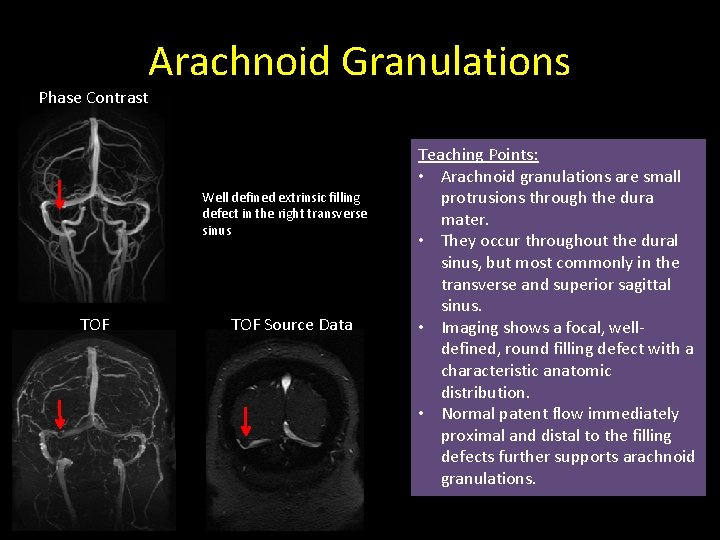
Phase Contrast Arachnoid Granulations Well defined extrinsic filling defect in the right transverse sinus TOF Source Data Teaching Points: • Arachnoid granulations are small protrusions through the dura mater. • They occur throughout the dural sinus, but most commonly in the transverse and superior sagittal sinus. • Imaging shows a focal, welldefined, round filling defect with a characteristic anatomic distribution. • Normal patent flow immediately proximal and distal to the filling defects further supports arachnoid granulations.
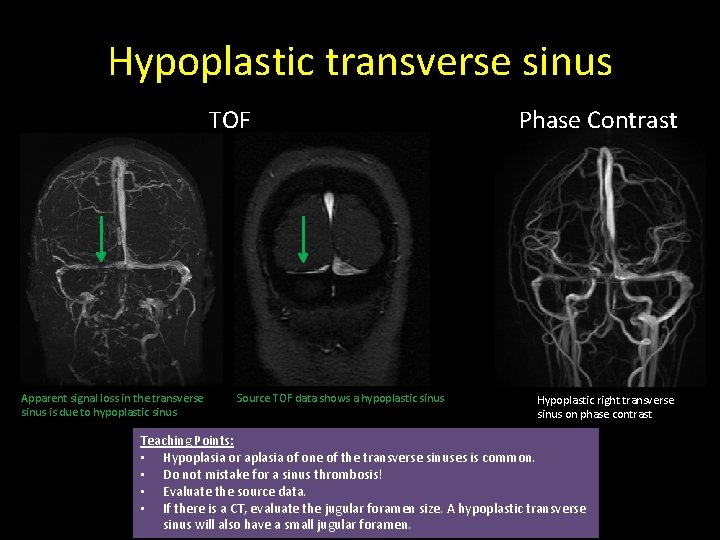
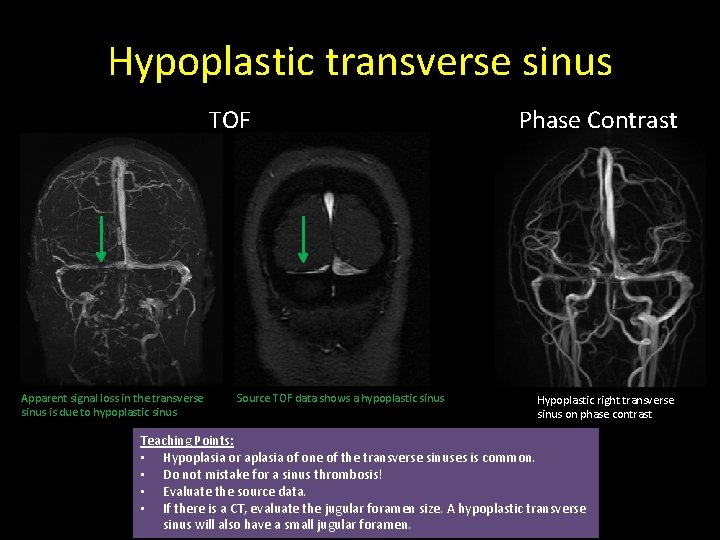
Hypoplastic transverse sinus TOF Apparent signal loss in the transverse sinus is due to hypoplastic sinus Source TOF data shows a hypoplastic sinus Phase Contrast Hypoplastic right transverse sinus on phase contrast Teaching Points: • Hypoplasia or aplasia of one of the transverse sinuses is common. • Do not mistake for a sinus thrombosis! • Evaluate the source data. • If there is a CT, evaluate the jugular foramen size. A hypoplastic transverse sinus will also have a small jugular foramen.

PATHOLOGIES
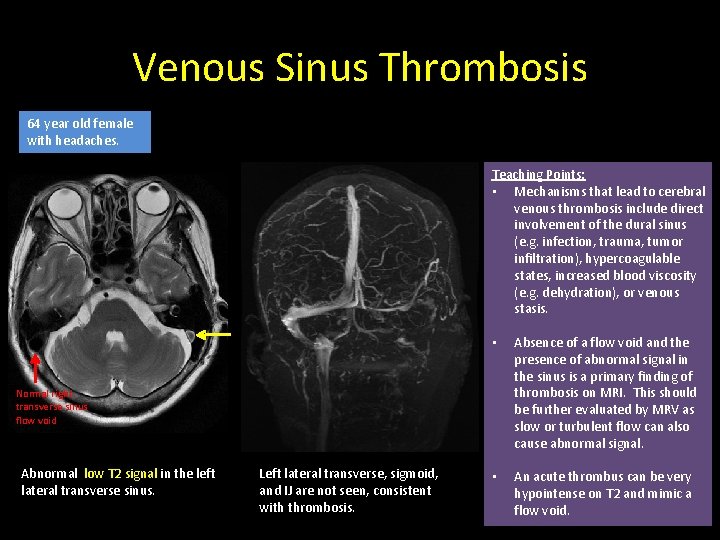
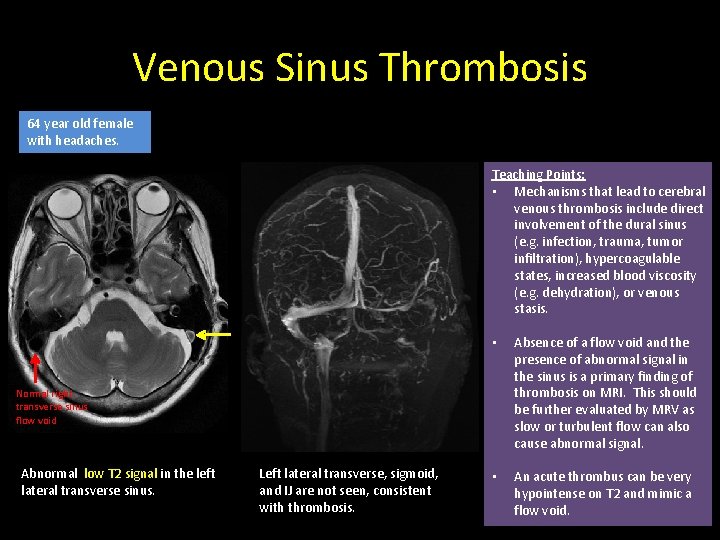
Venous Sinus Thrombosis 64 year old female with headaches. Teaching Points: • Mechanisms that lead to cerebral venous thrombosis include direct involvement of the dural sinus (e. g. infection, trauma, tumor infiltration), hypercoagulable states, increased blood viscosity (e. g. dehydration), or venous stasis. • Absence of a flow void and the presence of abnormal signal in the sinus is a primary finding of thrombosis on MRI. This should be further evaluated by MRV as slow or turbulent flow can also cause abnormal signal. • An acute thrombus can be very hypointense on T 2 and mimic a flow void. Normal right transverse sinus flow void Abnormal low T 2 signal in the left lateral transverse sinus. Left lateral transverse, sigmoid, and IJ are not seen, consistent with thrombosis.
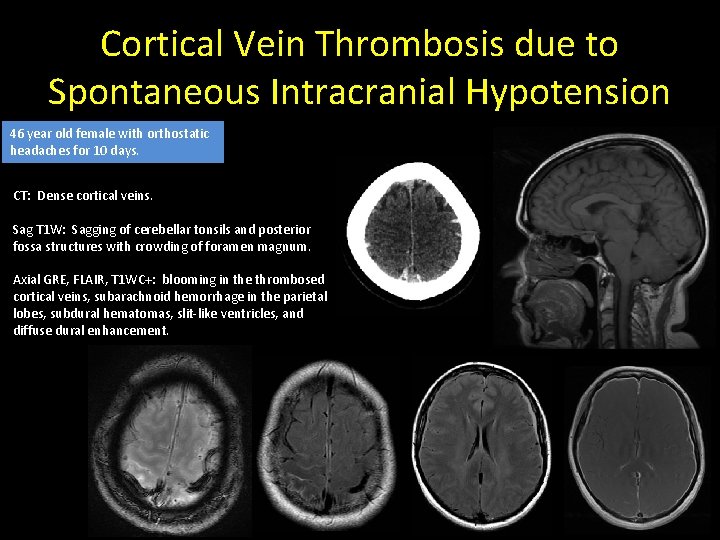
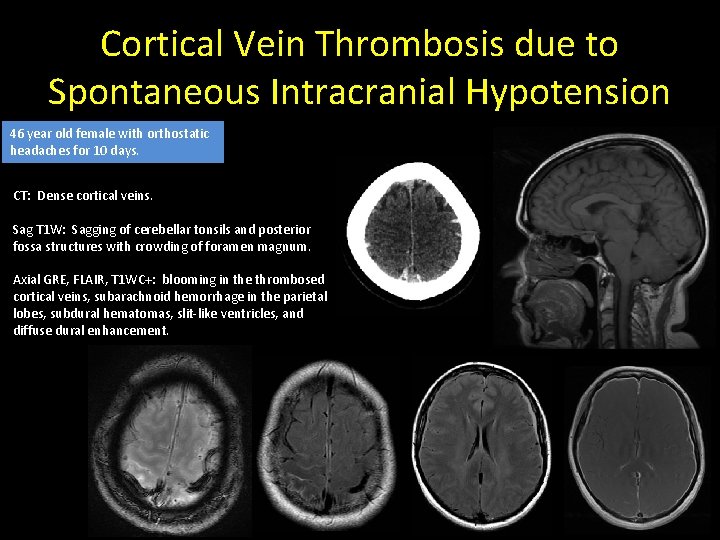
Cortical Vein Thrombosis due to Spontaneous Intracranial Hypotension 46 year old female with orthostatic headaches for 10 days. CT: Dense cortical veins. Sag T 1 W: Sagging of cerebellar tonsils and posterior fossa structures with crowding of foramen magnum. Axial GRE, FLAIR, T 1 WC+: blooming in the thrombosed cortical veins, subarachnoid hemorrhage in the parietal lobes, subdural hematomas, slit-like ventricles, and diffuse dural enhancement.
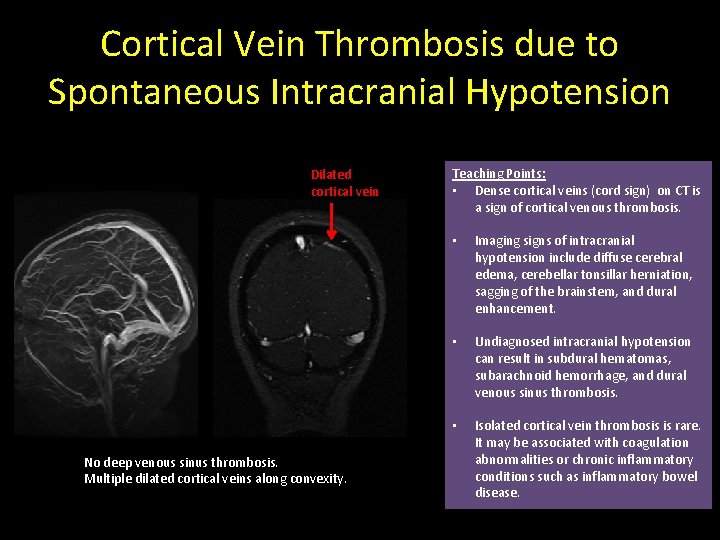
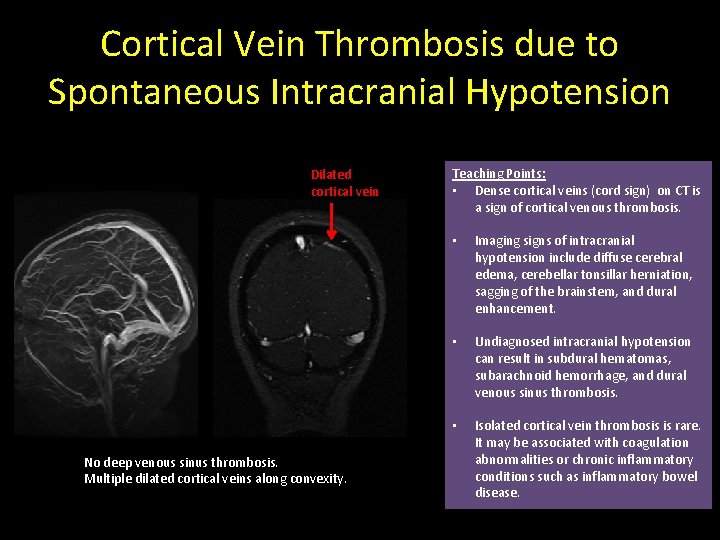
Cortical Vein Thrombosis due to Spontaneous Intracranial Hypotension Dilated cortical vein No deep venous sinus thrombosis. Multiple dilated cortical veins along convexity. Teaching Points: • Dense cortical veins (cord sign) on CT is a sign of cortical venous thrombosis. • Imaging signs of intracranial hypotension include diffuse cerebral edema, cerebellar tonsillar herniation, sagging of the brainstem, and dural enhancement. • Undiagnosed intracranial hypotension can result in subdural hematomas, subarachnoid hemorrhage, and dural venous sinus thrombosis. • Isolated cortical vein thrombosis is rare. It may be associated with coagulation abnormalities or chronic inflammatory conditions such as inflammatory bowel disease.
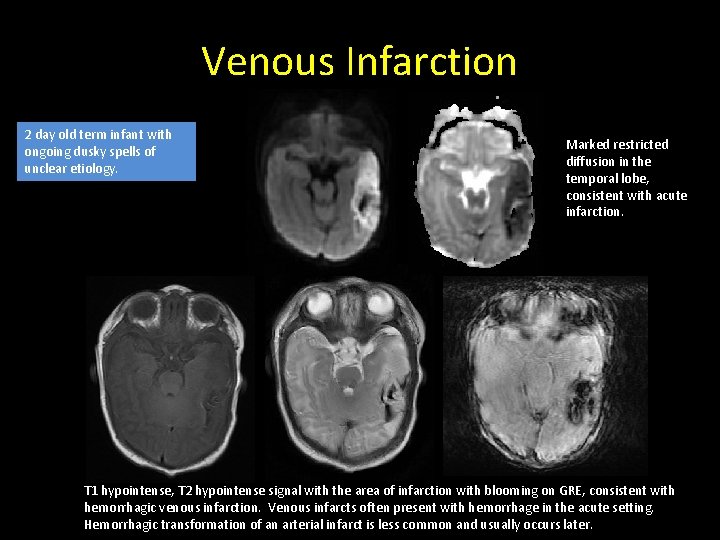
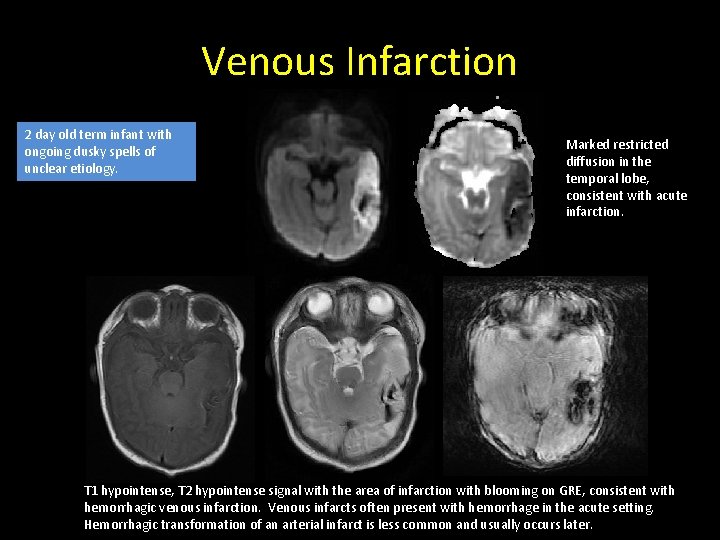
Venous Infarction 2 day old term infant with ongoing dusky spells of unclear etiology. Marked restricted diffusion in the temporal lobe, consistent with acute infarction. T 1 hypointense, T 2 hypointense signal with the area of infarction with blooming on GRE, consistent with hemorrhagic venous infarction. Venous infarcts often present with hemorrhage in the acute setting. Hemorrhagic transformation of an arterial infarct is less common and usually occurs later.
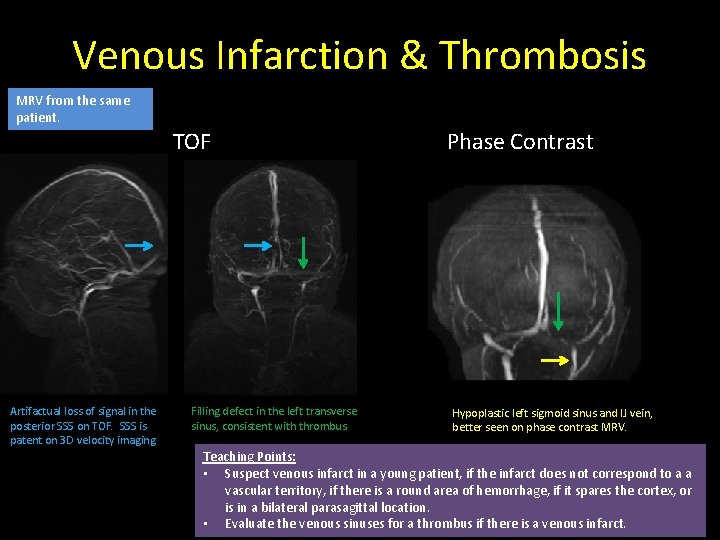
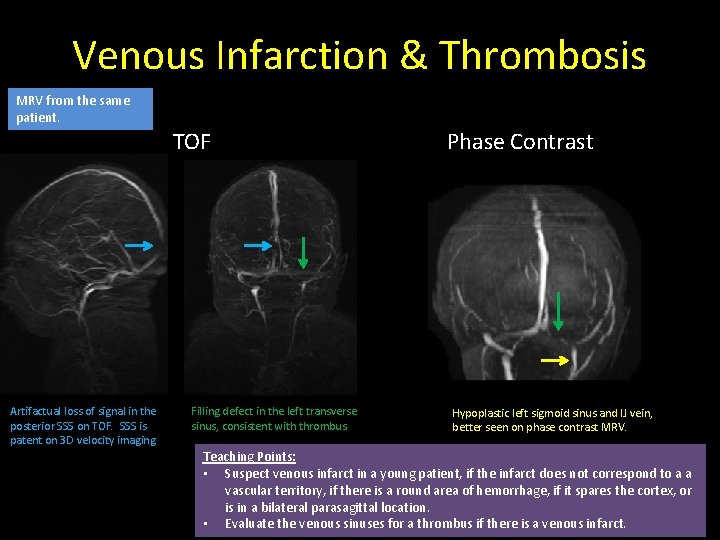
Venous Infarction & Thrombosis MRV from the same patient. Artifactual loss of signal in the posterior SSS on TOF. SSS is patent on 3 D velocity imaging. TOF Filling defect in the left transverse sinus, consistent with thrombus. Phase Contrast Hypoplastic left sigmoid sinus and IJ vein, better seen on phase contrast MRV. Teaching Points: • Suspect venous infarct in a young patient, if the infarct does not correspond to a a vascular territory, if there is a round area of hemorrhage, if it spares the cortex, or is in a bilateral parasagittal location. • Evaluate the venous sinuses for a thrombus if there is a venous infarct.

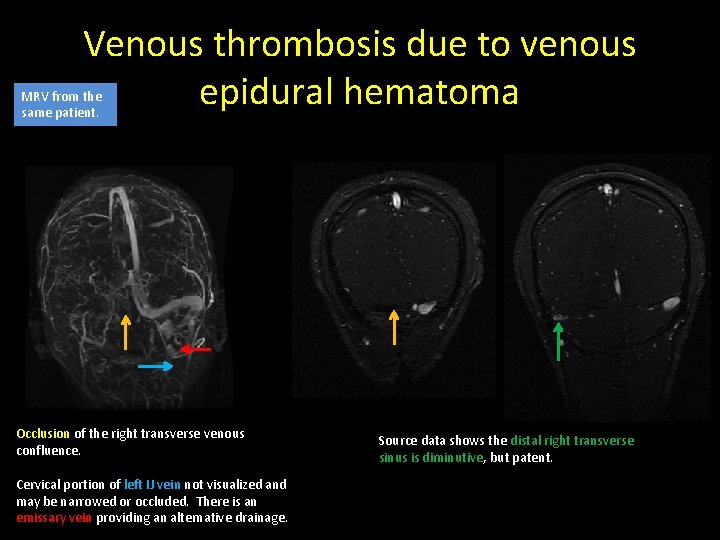
Venous thrombosis due to venous epidural hematoma 15 year old male brought in after a gang fight. Occipital fracture causing a venous epidural hematoma Probable clot in the right transverse and sigmoid sinus junction Active venous hemorrhage within the epidural hematoma Normal left venous sinuses Medial aspect of right transverse sinus not visualized and may be injured.
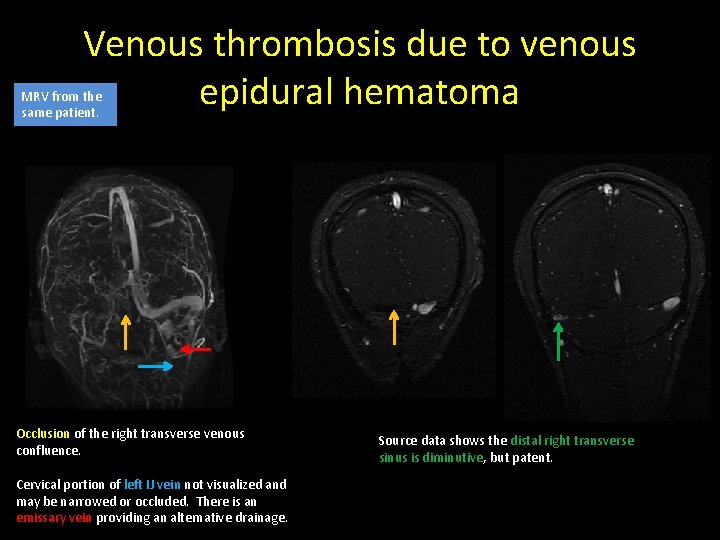
Venous thrombosis due to venous epidural hematoma MRV from the same patient. Occlusion of the right transverse venous confluence. Cervical portion of left IJ vein not visualized and may be narrowed or occluded. There is an emissary vein providing an alternative drainage. Source data shows the distal right transverse sinus is diminutive, but patent.
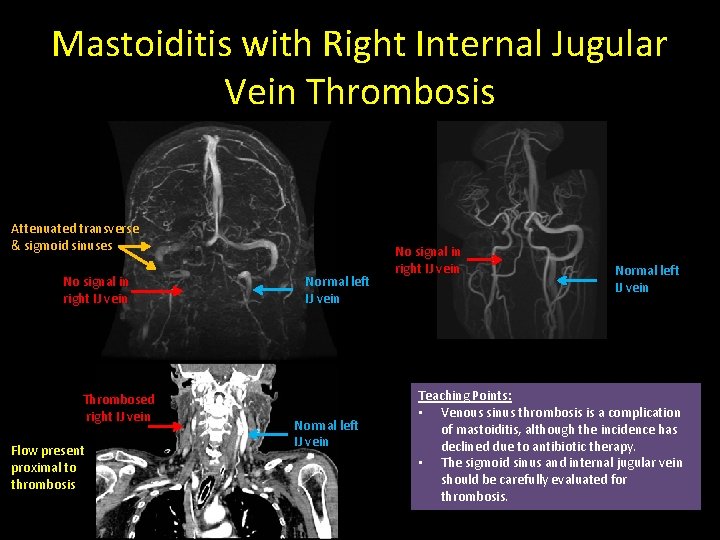
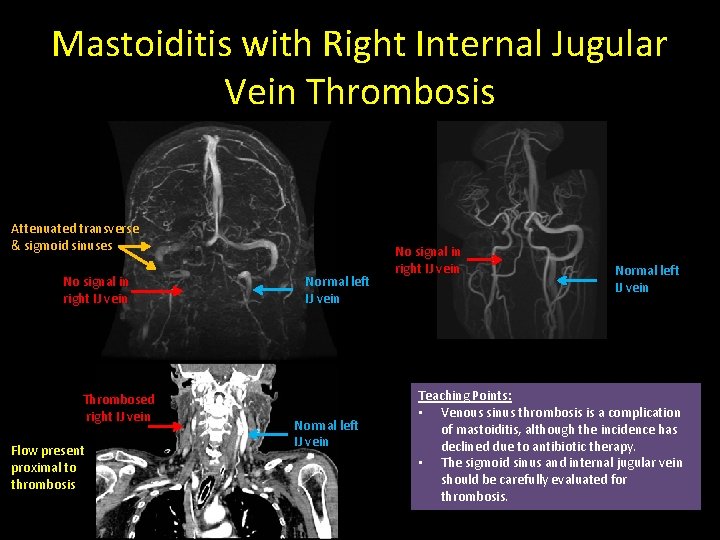
Mastoiditis with Right Internal Jugular Vein Thrombosis Attenuated transverse & sigmoid sinuses No signal in right IJ vein Thrombosed right IJ vein Flow present proximal to thrombosis Normal left IJ vein No signal in right IJ vein Normal left IJ vein Teaching Points: • Venous sinus thrombosis is a complication of mastoiditis, although the incidence has declined due to antibiotic therapy. • The sigmoid sinus and internal jugular vein should be carefully evaluated for thrombosis.

Compression from a Meningioma T 1 WC+: Homogenously enhancing left parafalcine extraaxial mass that compresses the sagittal sinus at its dural attachment. CTV: Left parafalcine meningioma compressing the sagittal sinus. Difficult to exclude focal thrombosis or invasion. Sagittal sinus around the mass is patent.
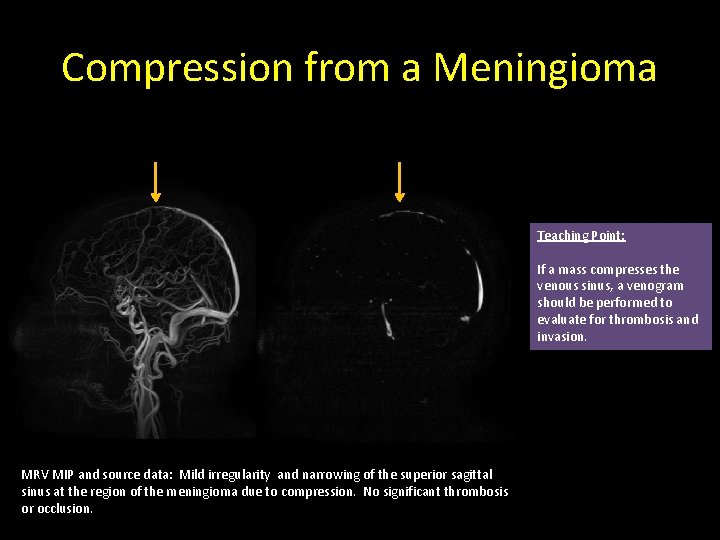
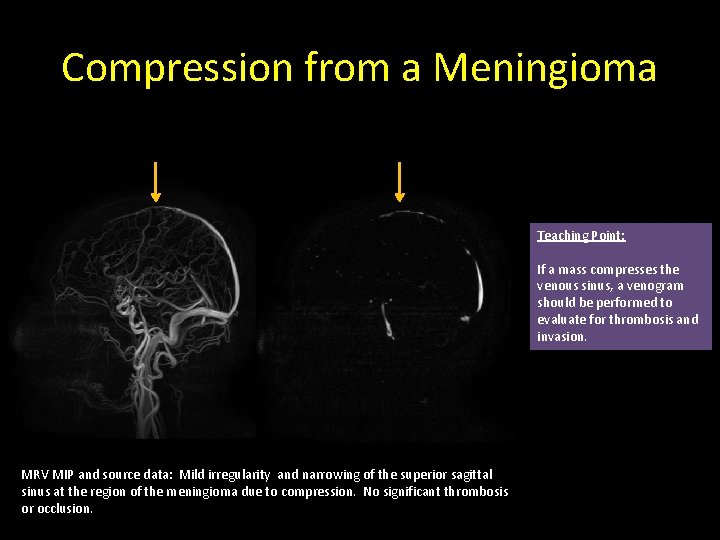
Compression from a Meningioma Teaching Point: If a mass compresses the venous sinus, a venogram should be performed to evaluate for thrombosis and invasion. MRV MIP and source data: Mild irregularity and narrowing of the superior sagittal sinus at the region of the meningioma due to compression. No significant thrombosis or occlusion.
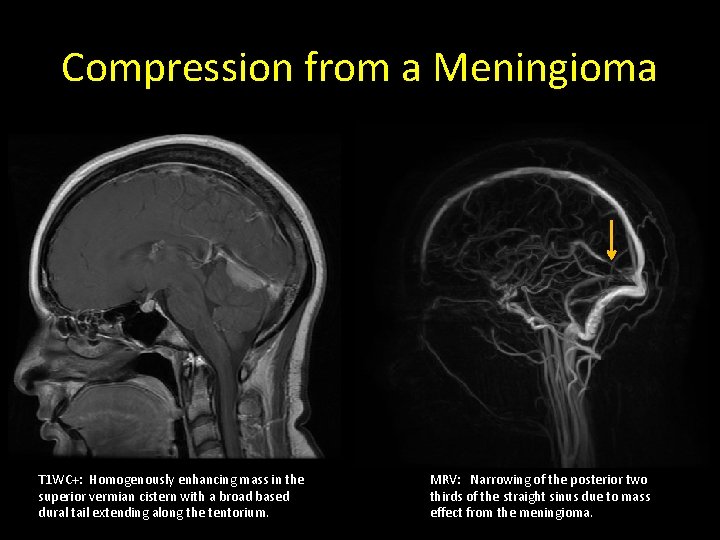
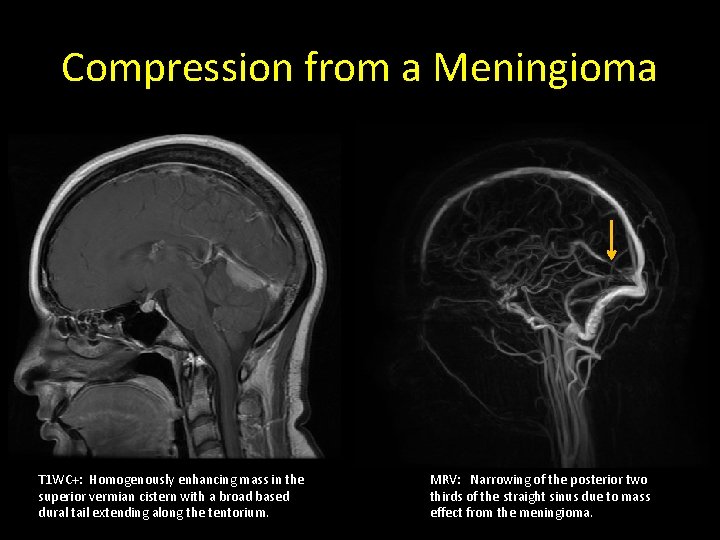
Compression from a Meningioma T 1 WC+: Homogenously enhancing mass in the superior vermian cistern with a broad based dural tail extending along the tentorium. MRV: Narrowing of the posterior two thirds of the straight sinus due to mass effect from the meningioma.
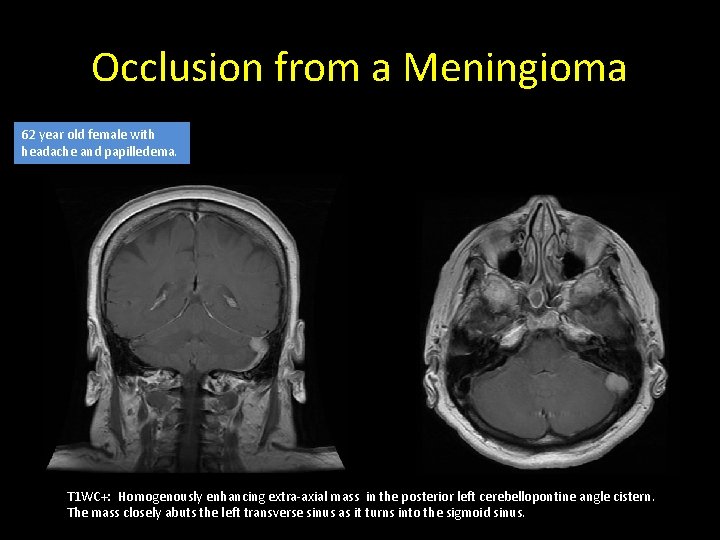
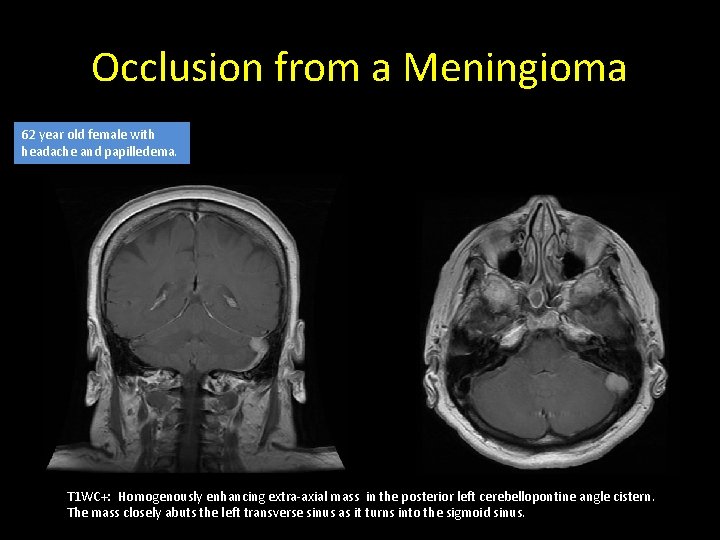
Occlusion from a Meningioma 62 year old female with headache and papilledema. T 1 WC+: Homogenously enhancing extra-axial mass in the posterior left cerebellopontine angle cistern. The mass closely abuts the left transverse sinus as it turns into the sigmoid sinus.
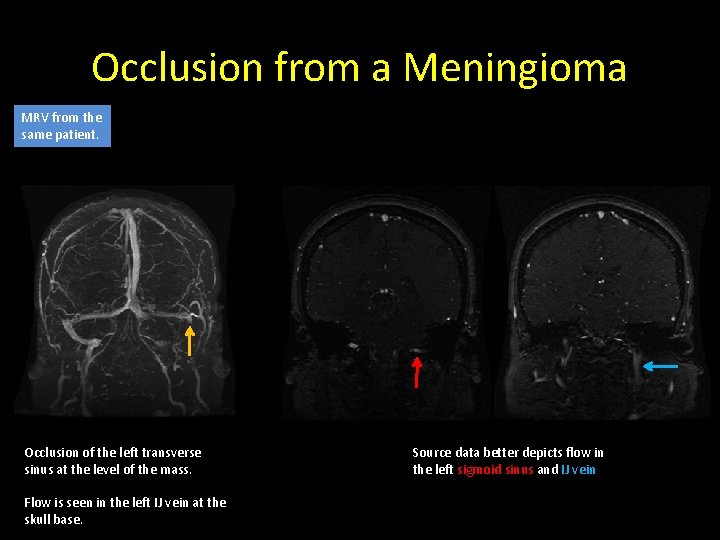
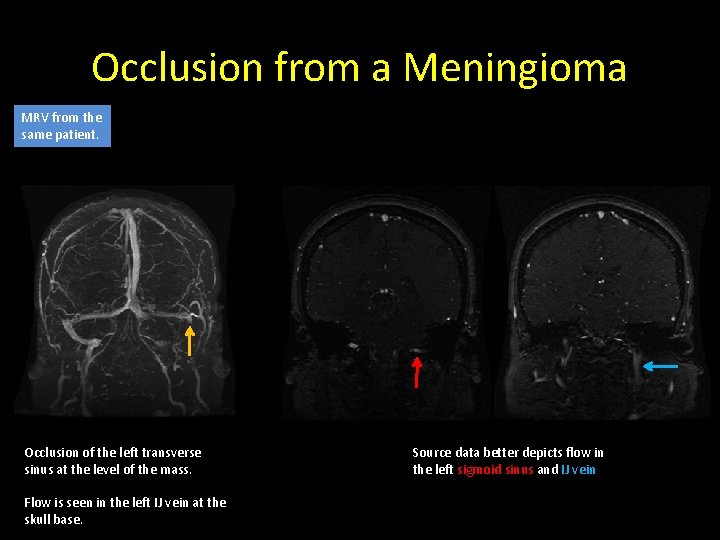
Occlusion from a Meningioma MRV from the same patient. Occlusion of the left transverse sinus at the level of the mass. Flow is seen in the left IJ vein at the skull base. Source data better depicts flow in the left sigmoid sinus and IJ vein
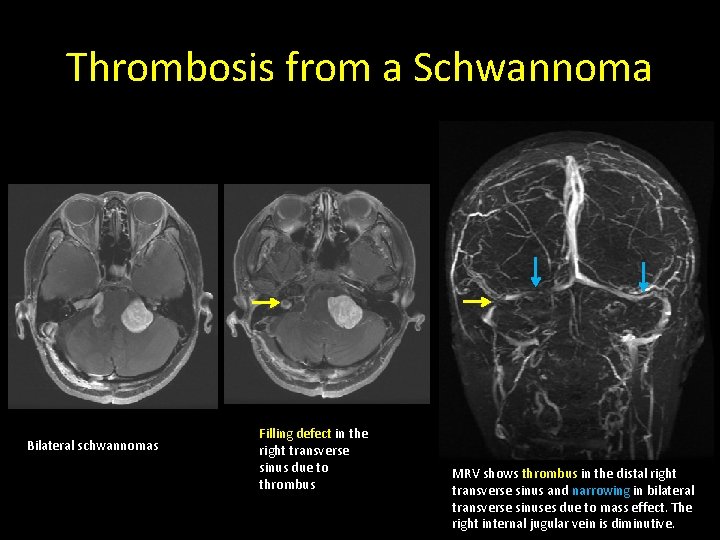
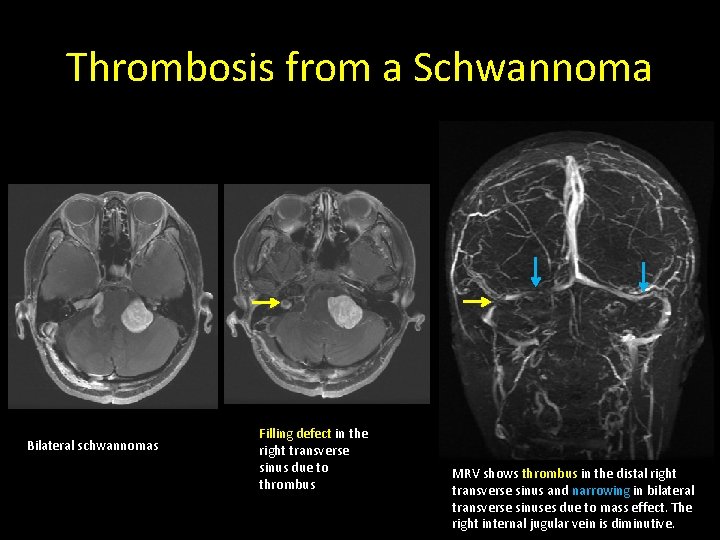
Thrombosis from a Schwannoma Bilateral schwannomas Filling defect in the right transverse sinus due to thrombus MRV shows thrombus in the distal right transverse sinus and narrowing in bilateral transverse sinuses due to mass effect. The right internal jugular vein is diminutive.
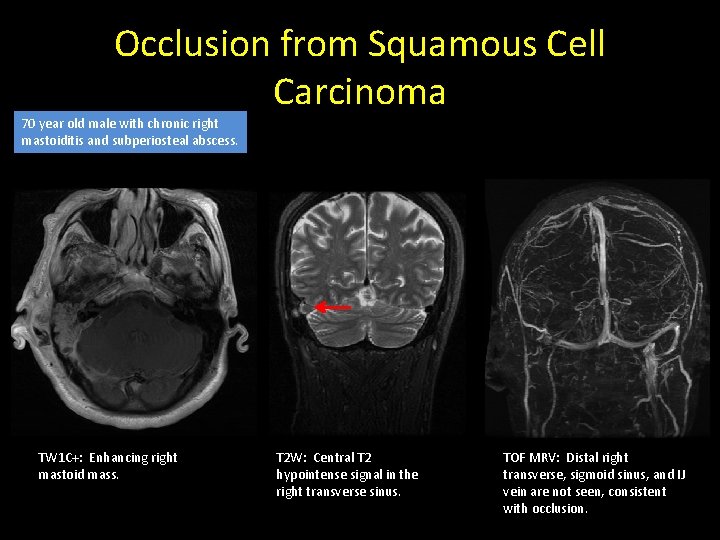
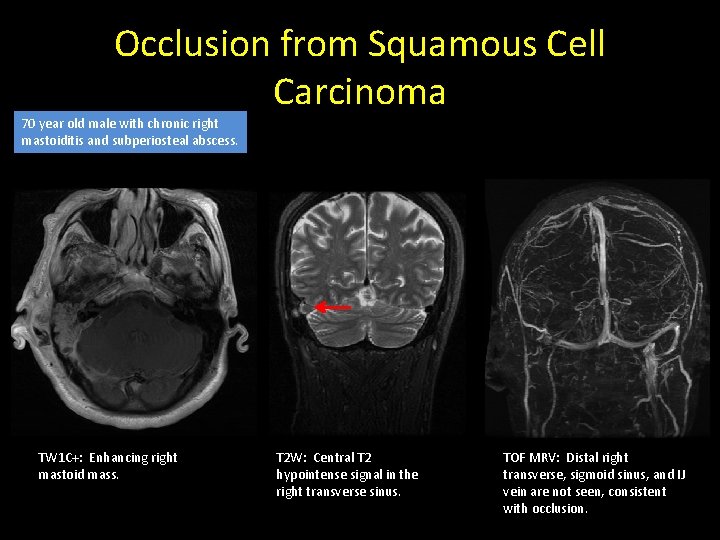
Occlusion from Squamous Cell Carcinoma 70 year old male with chronic right mastoiditis and subperiosteal abscess. TW 1 C+: Enhancing right mastoid mass. T 2 W: Central T 2 hypointense signal in the right transverse sinus. TOF MRV: Distal right transverse, sigmoid sinus, and IJ vein are not seen, consistent with occlusion.
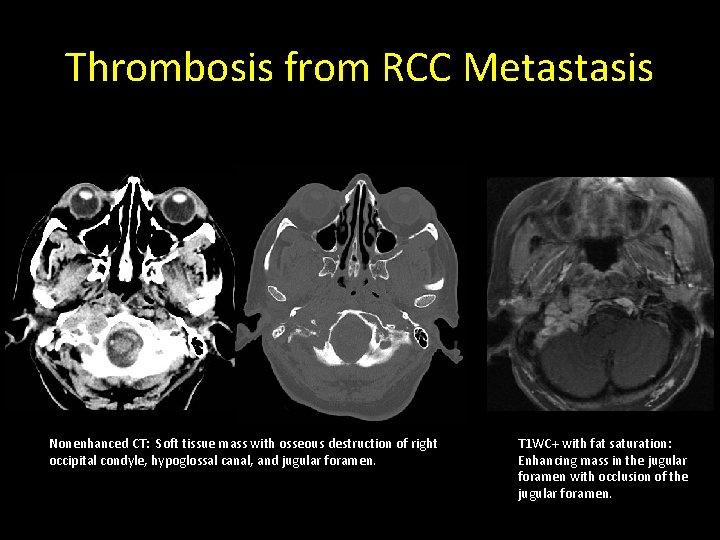
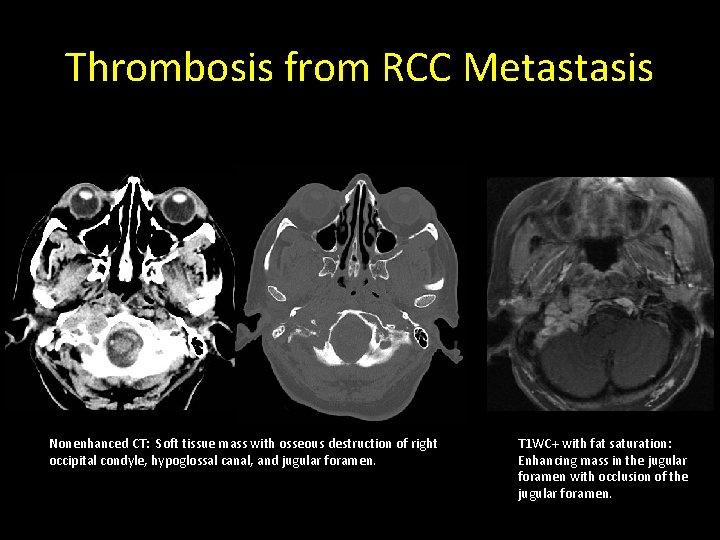
Thrombosis from RCC Metastasis Nonenhanced CT: Soft tissue mass with osseous destruction of right occipital condyle, hypoglossal canal, and jugular foramen. T 1 WC+ with fat saturation: Enhancing mass in the jugular foramen with occlusion of the jugular foramen.
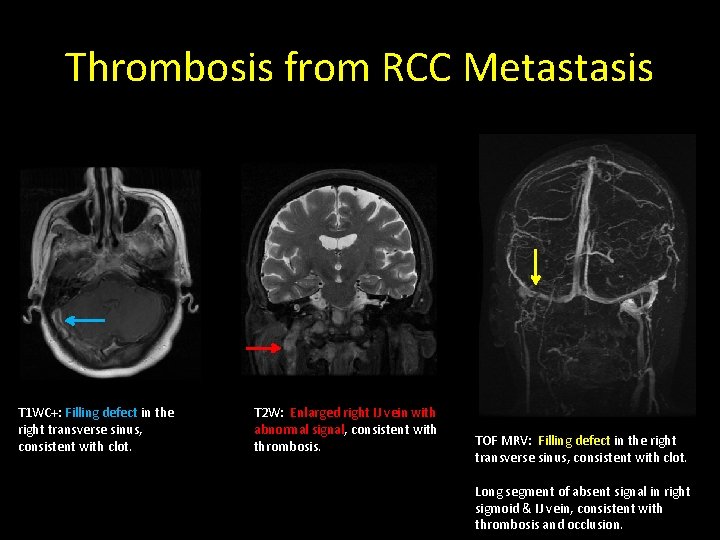
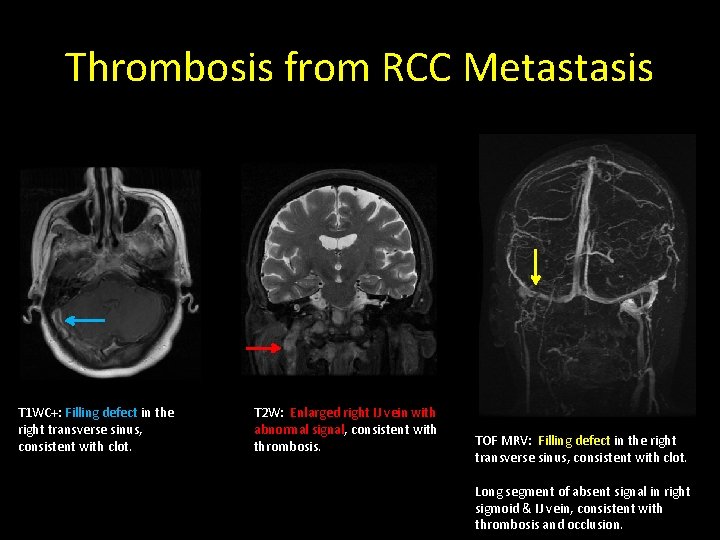
Thrombosis from RCC Metastasis T 1 WC+: Filling defect in the right transverse sinus, consistent with clot. T 2 W: Enlarged right IJ vein with abnormal signal, consistent with thrombosis. TOF MRV: Filling defect in the right transverse sinus, consistent with clot. Long segment of absent signal in right sigmoid & IJ vein, consistent with thrombosis and occlusion.
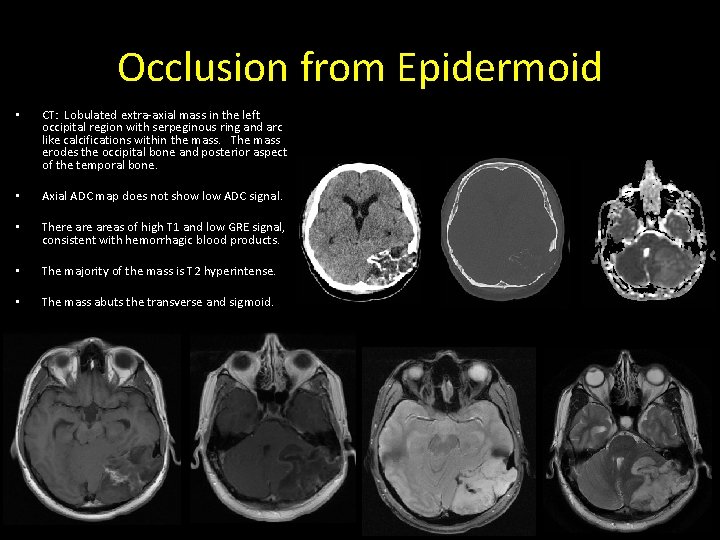
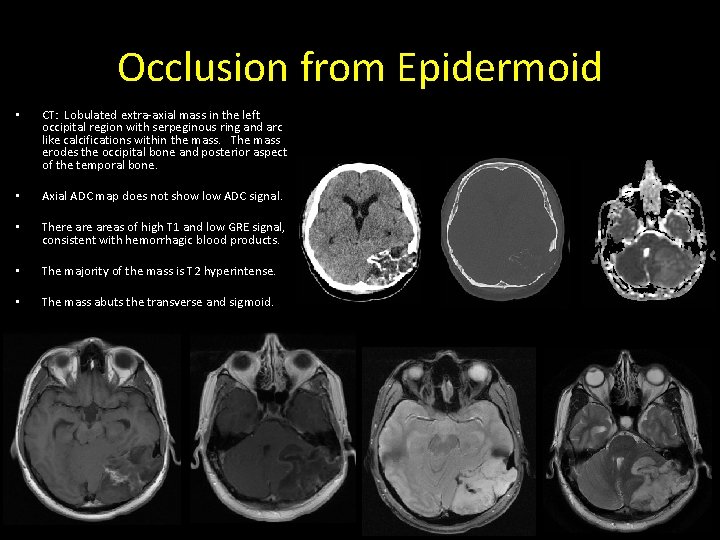
Occlusion from Epidermoid • CT: Lobulated extra-axial mass in the left occipital region with serpeginous ring and arc like calcifications within the mass. The mass erodes the occipital bone and posterior aspect of the temporal bone. • Axial ADC map does not show low ADC signal. • There areas of high T 1 and low GRE signal, consistent with hemorrhagic blood products. • The majority of the mass is T 2 hyperintense. • The mass abuts the transverse and sigmoid.
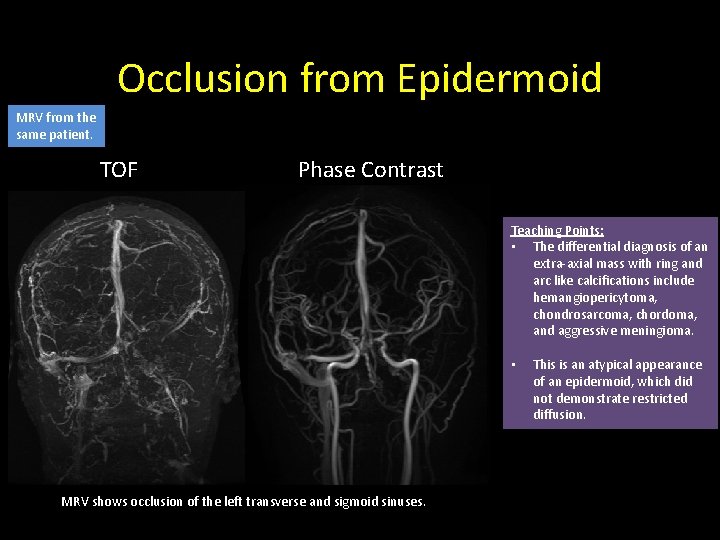
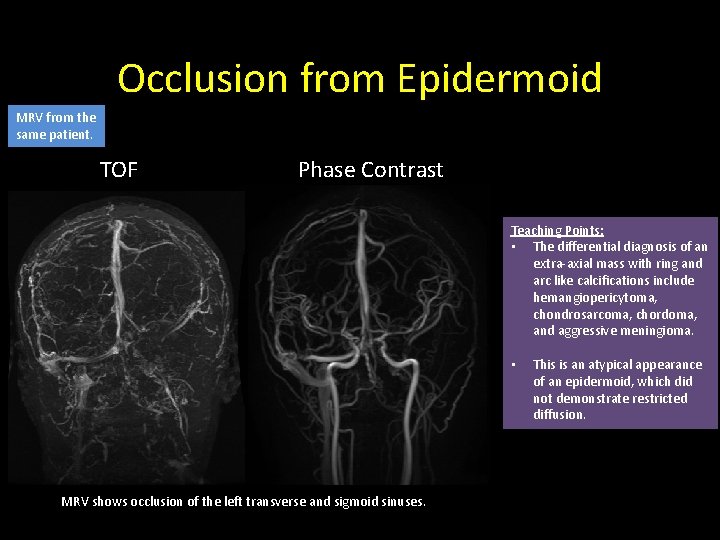
Occlusion from Epidermoid MRV from the same patient. TOF Phase Contrast Teaching Points: • The differential diagnosis of an extra-axial mass with ring and arc like calcifications include hemangiopericytoma, chondrosarcoma, chordoma, and aggressive meningioma. • MRV shows occlusion of the left transverse and sigmoid sinuses. This is an atypical appearance of an epidermoid, which did not demonstrate restricted diffusion.
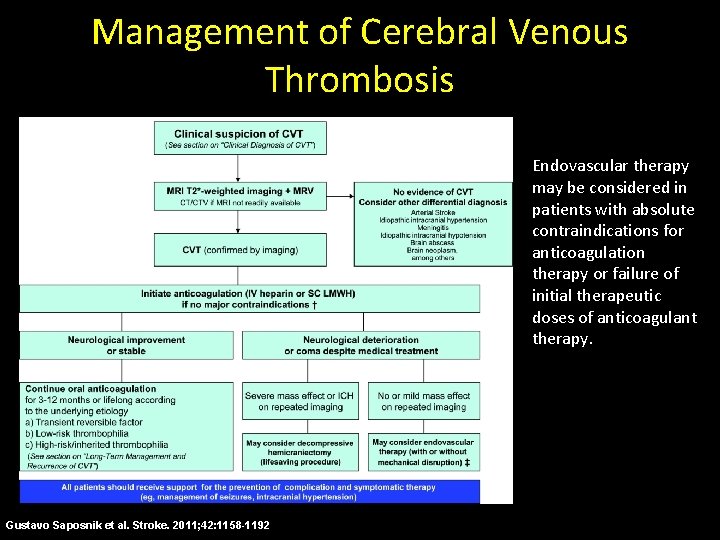
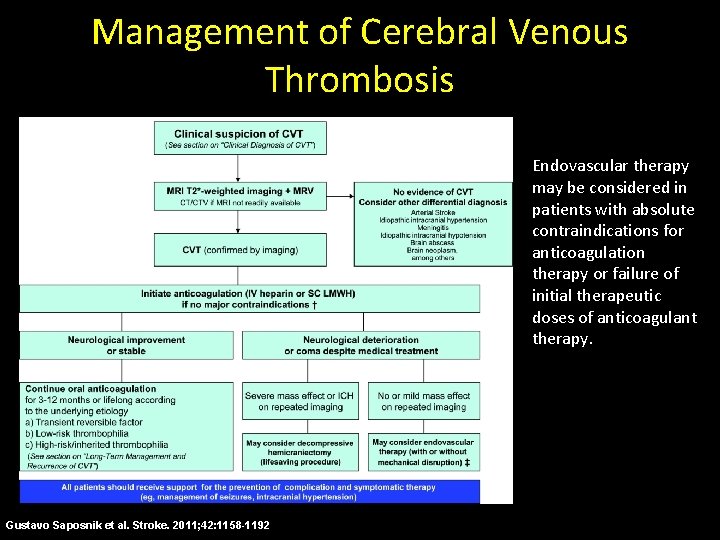
Management of Cerebral Venous Thrombosis Endovascular therapy may be considered in patients with absolute contraindications for anticoagulation therapy or failure of initial therapeutic doses of anticoagulant therapy. Gustavo Saposnik et al. Stroke. 2011; 42: 1158 -1192
Summary • Familiarity with common pitfalls of MRV will assist in the accurate interpretation and diagnosis of the intracranial venous system. • Correlating imaging findings on different MRV sequences and reviewing the source data can avoid diagnostic pitfalls associated with all imaging techniques. • Knowledge of the typical and subtle imaging features of common pathologies of the cerebral venous sinuses will lead to prompt diagnosis and treatment, which can improve prognosis.
References • • Leach JL, Fortuna RB, Jones BV, Gaskill-Shipley MF. Imaging of cerebral venous thrombosis: current techniques, spectrum of findings, and diagnostic pitfalls. Radiographics. 2006; 26 Suppl 1: S 19 -41 Poon CS, Chang JK, Swarnkar A, Johnson MH, Wasenko J. Radiologic diagnosis of cerebral venous thrombosis: pictorial review. AJR Am J Roentgenol. 2007; 189(6 Suppl): S 64 -75 Ayanzen RH, Bird CR, Keller PJ et al. Cerebral MR venography: normal anatomy and potential diagnostic pitfalls. AJNR Am J Neuroradiol 2000: 21: 74– 78 Glockner JF, Lee CU. Magnetic Resonance Venography. Appl Radiol. 2010: 39: 36 -42 Rollins N, Ison C, Booth T, Chia J. MR Venography in the Pediatric Patient. AJNR Am J Neuroradiol. 2005; 26(1): 50 -5 Carr JC, Carroll TJ (2012). Magnetic Resonance Angiography: Principles and Applications. Chicago, IL: Springer. Saposnik G, Barinagarrementeria F, Brown RD Jr, Bushnell CD, Cucchiara B, Cushman M, de. Veber G, Ferro JM, Tsai FY; American Heart Association Stroke Council and the Council on Epidemiology and Prevention. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011; 42(4): 1158 -92
Contact Information Jennifer Trinh, MD Department of Radiology Santa Clara Valley Medical Center 751 S. Bascom Ave. San Jose, CA 95125 Jennifer. trinh@hhs. sccgov. org