PICOT EBP Power Point Presentation CYNTHIA ALEXANDER NU
PICOT EBP – Power. Point Presentation CYNTHIA ALEXANDER NU 522 JACKSONVILLE STATE UNIVERSITY
Introduction The development of a pressure ulcer is very high on the list of concerns for many family members when a family member is admitted into a health care facility. Interventions are initiated immediately based on the nurses’ admission assessment. One standard of care that has been utilized for immobilized patients is turning and repositioning to decrease the risks associated with pressure ulcer development.
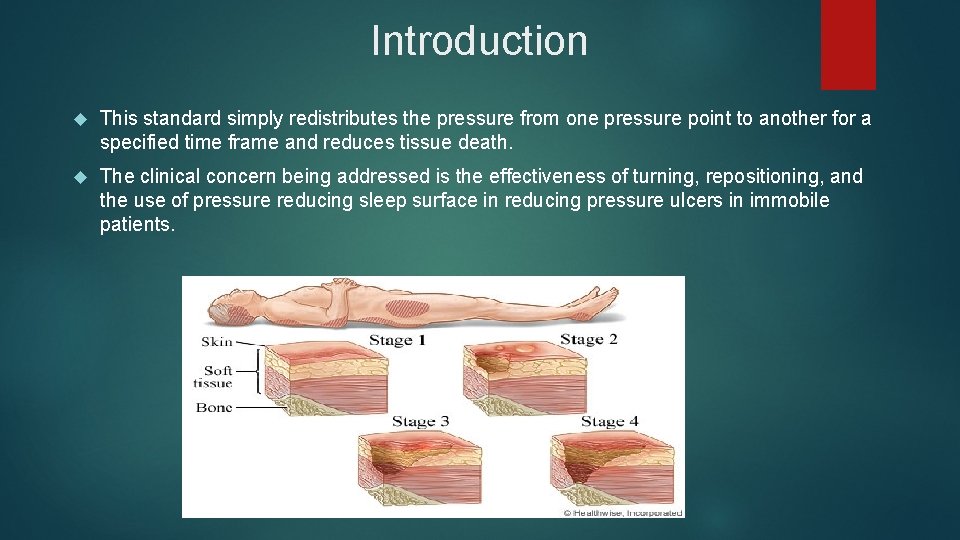
Introduction This standard simply redistributes the pressure from one pressure point to another for a specified time frame and reduces tissue death. The clinical concern being addressed is the effectiveness of turning, repositioning, and the use of pressure reducing sleep surface in reducing pressure ulcers in immobile patients.
PICOT P - Immobile patients in a health care facility I – less than every 2 hour turning, repositioning off pressure points, pressure reducing sleep surface C – Control group turned greater than every 2 hours O – Pressure ulcer development T – one week
PICOT Question Does turning less than every 2 hours, repositioning off pressure points, and use of a pressure reducing sleep surface lower the occurrence of pressure ulcers in immobile patients in one week?
Literature Review Early identification of risk factors is a key component in pressure ulcer reduction. The Braden Scale is a commonly used risk assessment tool. Once identified preventive measures should be initiated immediately to reduce those risks. According to Anders et al. , (2010) the focus on reducing pressure and increasing mobility by turning and repositioning bedridden patients has resulted in a decrease in pressure ulcers. (Anders et al. , 2010)
Literature Review The emphasis is placed on frequent position changes by turning and repositioning to relieve pressure through active movement. Reddy et al. , (2006) review concluded that no one approach could be identified as the best intervention for reducing the development of pressure ulcers. Evidence supported the use of a multisystem approach that includes moisturizing the skin, nutritional support, appropriate turning and repositioning based on the patient needs and a support surface (Reddy et al. , 2006)
Literature Review Support surfaces are important in the redistribution of pressure in immobile patients. Chou et al. , (2013) used forty-one randomized trials to evaluate support surfaces in patients admitted to acute care and long term care with increased pressure ulcer risks. The review revealed that static support surfaces are more effective than standard mattresses in the prevention of pressure ulcers in immobile patients (Chou et al. , 2013)
3 Support Surface Groups Overlays (gel or water), for low risk patients Low air loss support surfaces for medium to high risk patients Fluidized support surfaces for high risk patients (Lyder, 2003)

Support Surfaces
Literature Review In the study done by Lyder, (2003) pressure ulcers were noted to develop in as little as two hours in the absence of preventive measures. Lyder (2003) further stated that no one intervention could be expected to be effective on every patient for every situation. The use of a multiple approach system would be best. Two factors that must be taken into consideration when developing interventions are eliminating constant pressure or redistribution (Lyder, 2003)
Literature Review The use of turning and repositioning should at least be done every two hours (Lyder, 2003). Lyder (2003) also indicated that the use of an appropriate support surface is an important intervention in preventing pressure ulcers. Based on assessment the appropriate support surface should be used based on the patient’s risk factors. (Lyder, 2003)
Conclusion One goal for every health care facility should be to prevent pressure ulcers from developing in immobile patients. Initiating preventive measures once risk factors are identified is a very important function for the nurse. Preventive measure should be initiated on admission when the clinical assessment is completed and risk factors have been identified.

Conclusion Review of the research data indicates that using appropriate assessments, turning and repositioning, and the appropriate sleep surfaces are essential components in reducing the occurrence of pressure ulcers in immobile patients.
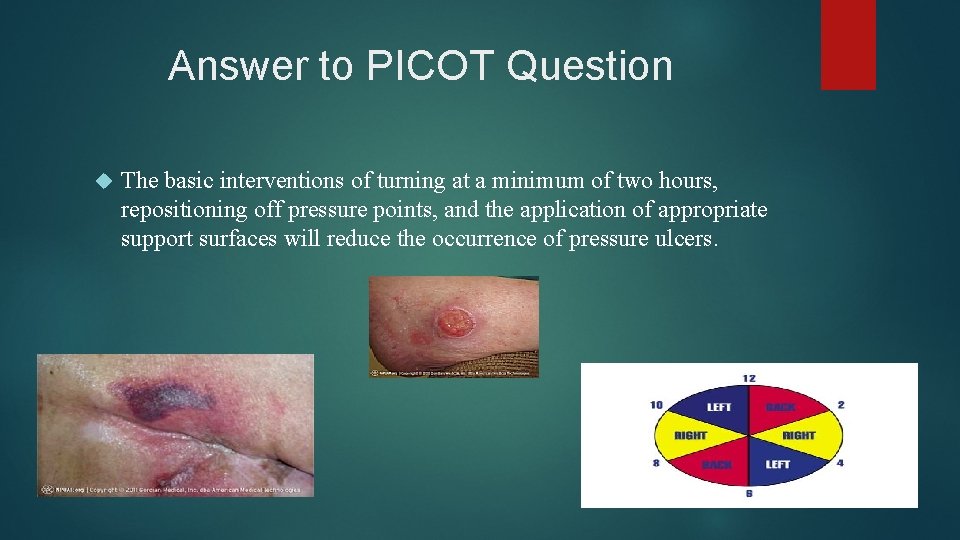
Answer to PICOT Question The basic interventions of turning at a minimum of two hours, repositioning off pressure points, and the application of appropriate support surfaces will reduce the occurrence of pressure ulcers.
Plan Training with the nurses is essential for the success of the pressure ulcer prevention plan. Assess each patient for risk factors on admission using the Braden Scale. Assess each patient for the appropriate frequency for turning and repositioning. Initiate a turning schedule.
Plan Review nutritional status and order supplements as needed. Update Care Plan with appropriate interventions for staff to follow. Failure to address these other factors could decrease the effectiveness of the two hour turning schedule, repositioning off pressure points, and the use of support surfaces.
References Anders, J. , Heinemann, A. , Leffmann, C. , Leutenegger, M. , Profener, F. , and von Renteln Kruse, W. (2010). Decubitus Ulcers: Pathophysiology and Primary Prevention. Deutsches Arzteblatt International. 107(21) 371 -382. doi: 10. 3238/arztebl. 2010. 0371. Baranoski, S. and Ayello, E. (2012) Wound Care Essentials. Practice Principles. Third Edition. Philadelphia, PA: Lippincott Wilkens & Williams. Chou, R. , Dana, T. , Bougatsos, C. , Blazina, I. , Starmer, A. , Reitel, K. , and Buckley, D. (2013). Pressure Ulcer Risk Assessment and Prevention: A Systematic Comparative Effectiveness Review. Annals of Internal Medicine. 159(1) 28 -38. doi: 10. 7326/0003 -4819 -159 -1 -20130702000006.
References Lyder, C. (2003). Pressure Ulcer Prevention and Management. The Journal of the American Medical Association. 289(2) 223 -226. doi: 10. 1001/jama 289. 2. 223. Reddy, M. , Gill, S. , and Rochon, P. (2006). Preventing Pressure Ulcers: A Systematic Review. JAMA. 296(8) 974 – 984.
- Slides: 19