PHYSIOPATHOLOGY OF PITUITARY GLAND ADRENALS AND GONADS Hormones








- Slides: 56
PHYSIOPATHOLOGY OF PITUITARY GLAND, ADRENALS AND GONADS
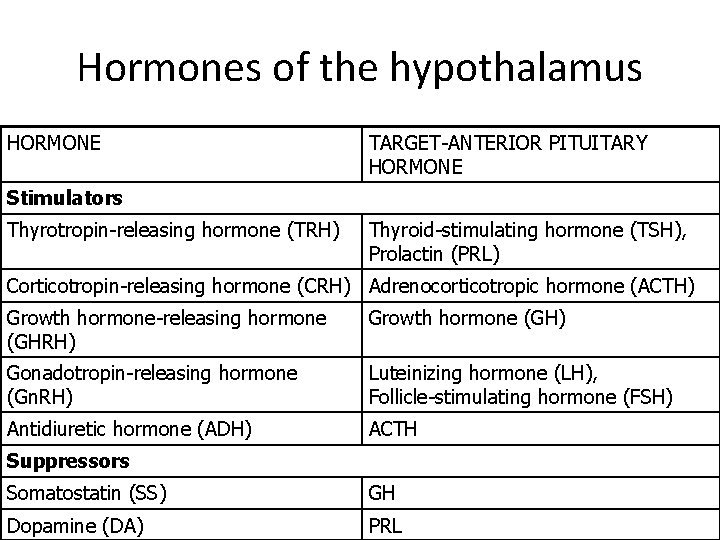
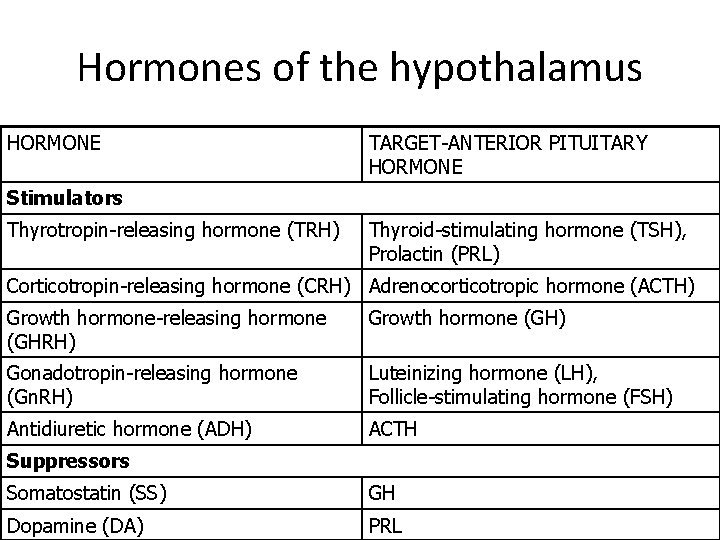
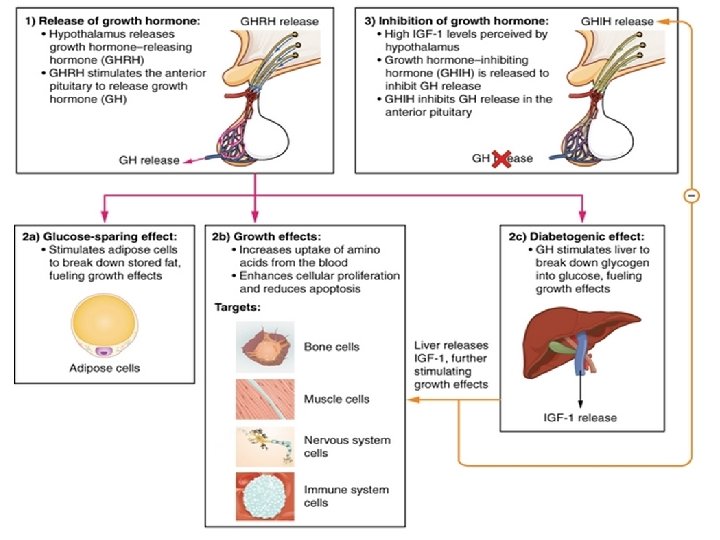
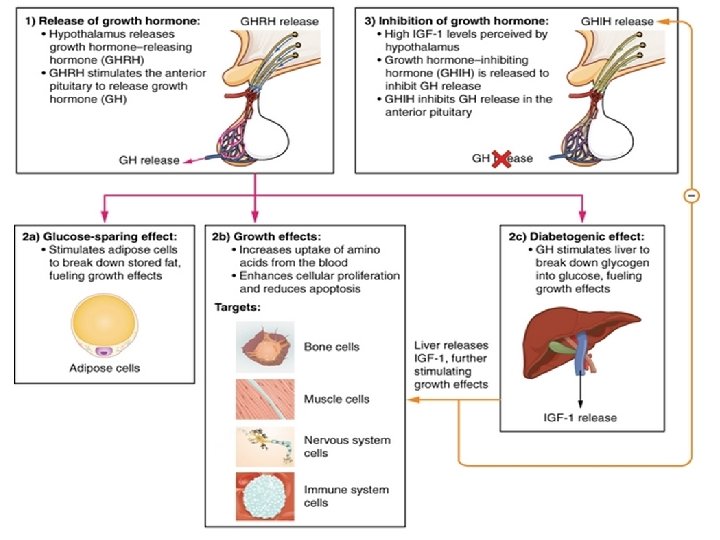
Hormones of the hypothalamus HORMONE TARGET-ANTERIOR PITUITARY HORMONE Stimulators Thyrotropin-releasing hormone (TRH) Thyroid-stimulating hormone (TSH), Prolactin (PRL) Corticotropin-releasing hormone (CRH) Adrenocorticotropic hormone (ACTH) Growth hormone-releasing hormone (GHRH) Growth hormone (GH) Gonadotropin-releasing hormone (Gn. RH) Luteinizing hormone (LH), Follicle-stimulating hormone (FSH) Antidiuretic hormone (ADH) ACTH Suppressors Somatostatin (SS) GH Dopamine (DA) PRL
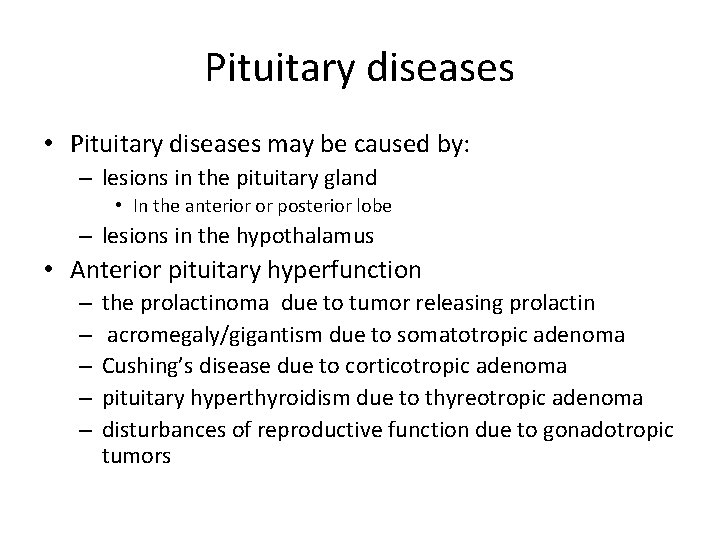
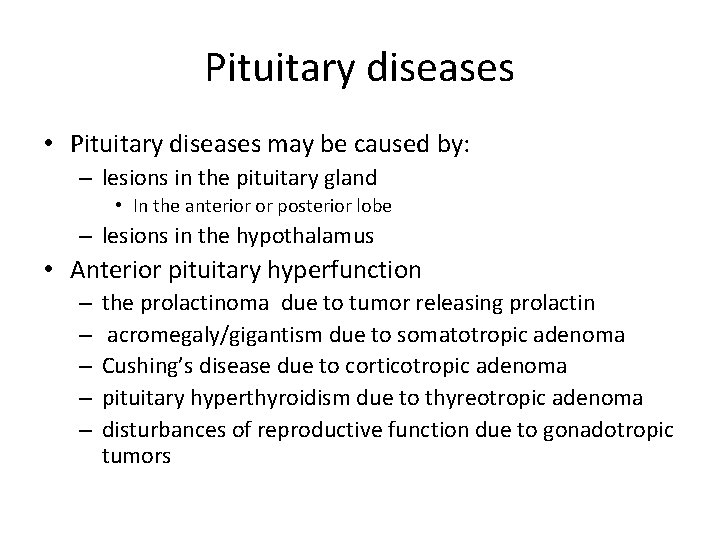
Pituitary diseases • Pituitary diseases may be caused by: – lesions in the pituitary gland • In the anterior or posterior lobe – lesions in the hypothalamus • Anterior pituitary hyperfunction – – – the prolactinoma due to tumor releasing prolactin acromegaly/gigantism due to somatotropic adenoma Cushing’s disease due to corticotropic adenoma pituitary hyperthyroidism due to thyreotropic adenoma disturbances of reproductive function due to gonadotropic tumors
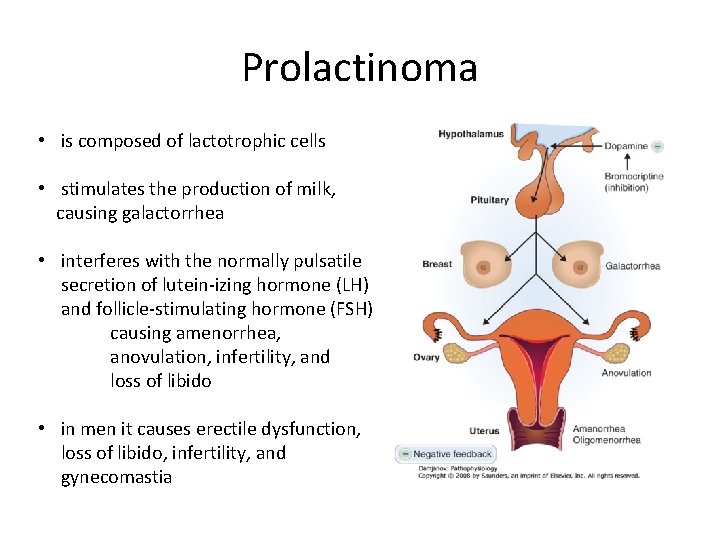
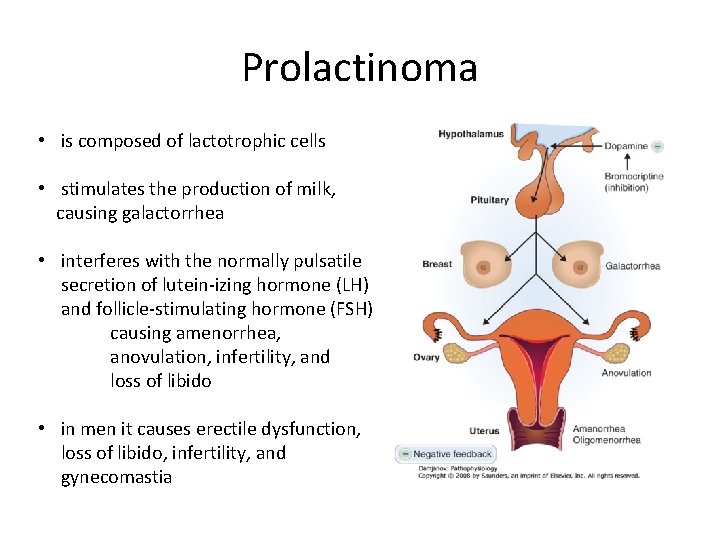
Prolactinoma • is composed of lactotrophic cells • stimulates the production of milk, causing galactorrhea • interferes with the normally pulsatile secretion of lutein izing hormone (LH) and follicle stimulating hormone (FSH) causing amenorrhea, anovulation, infertility, and loss of libido • in men it causes erectile dysfunction, loss of libido, infertility, and gynecomastia
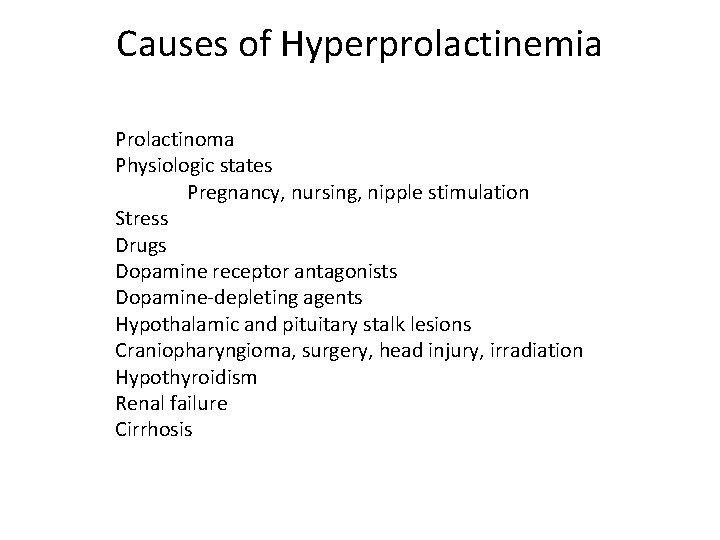
Causes of Hyperprolactinemia Prolactinoma Physiologic states Pregnancy, nursing, nipple stimulation Stress Drugs Dopamine receptor antagonists Dopamine depleting agents Hypothalamic and pituitary stalk lesions Craniopharyngioma, surgery, head injury, irradiation Hypothyroidism Renal failure Cirrhosis
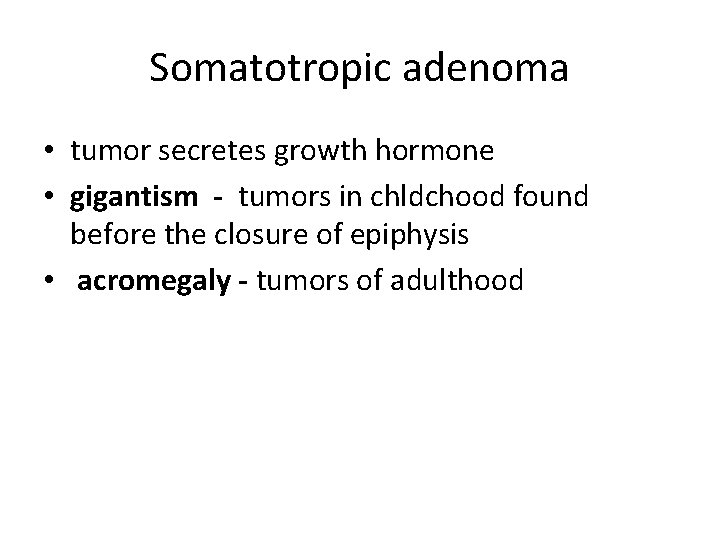
Somatotropic adenoma • tumor secretes growth hormone • gigantism - tumors in chldchood found before the closure of epiphysis • acromegaly - tumors of adulthood
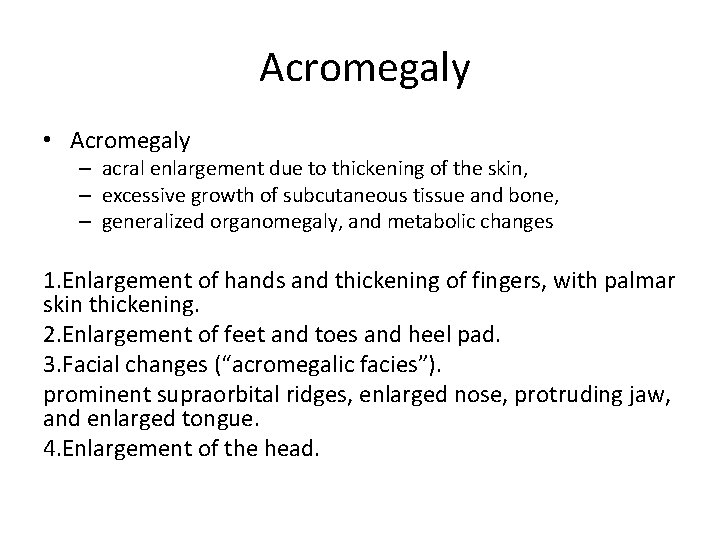
Acromegaly • Acromegaly – acral enlargement due to thickening of the skin, – excessive growth of subcutaneous tissue and bone, – generalized organomegaly, and metabolic changes 1. Enlargement of hands and thickening of fingers, with palmar skin thickening. 2. Enlargement of feet and toes and heel pad. 3. Facial changes (“acromegalic facies”). prominent supraorbital ridges, enlarged nose, protruding jaw, and enlarged tongue. 4. Enlargement of the head.

Acromegaly 5. Cardiomegaly organomegaly and hypertension, congestive heart failure 6. Musculoskeletal symptoms Bone overgrowth and weakening of muscle is complicated by degenerative joint disease and widespread pain. 7. Neuropathy Carpal tunnel syndrome and other peripheral nerve compression 8. Metabolic changes glucose intolerance, diabetes

Acromegaly
Causes of hypopituitarism • Invasive tumor (e. g. , brain tumor of hypothalamus, craniopharyngioma, pituitary adenoma, meningioma, chordomas, metastases) • Iatrogenic (e. g. , surgery, radiation therapy, hormonal therapy) • Infarction (e. g. , Sheehan’s postpartum syndrome, sickle cell anemia) • Injury (e. g. , head trauma) • Infection (e. g. , tuberculosis) • Immune disease (e. g. , lymphocytic hypophysitis, sarcoidosis) • Inherited (e. g. , isolated genetic pituitary hormone deficiencies, hormone receptor deficiencies) • Idiopathic
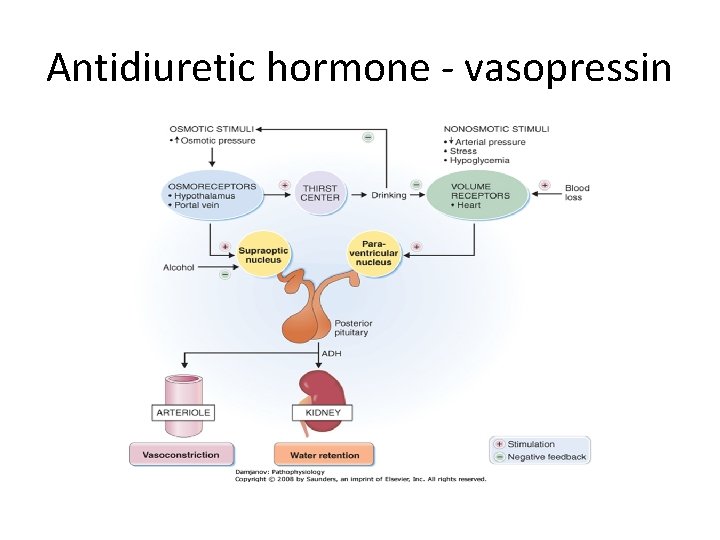
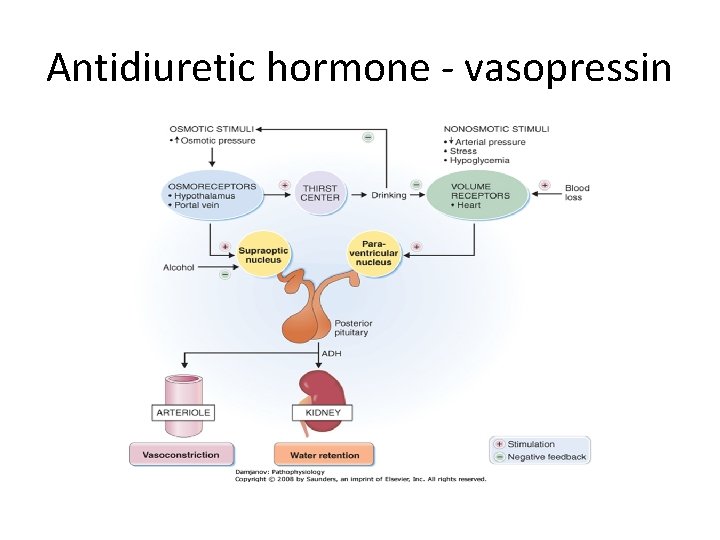
Antidiuretic hormone vasopressin
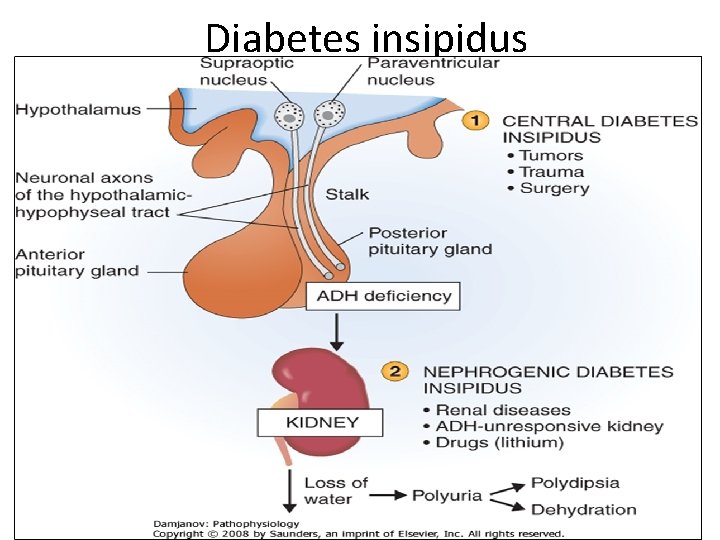
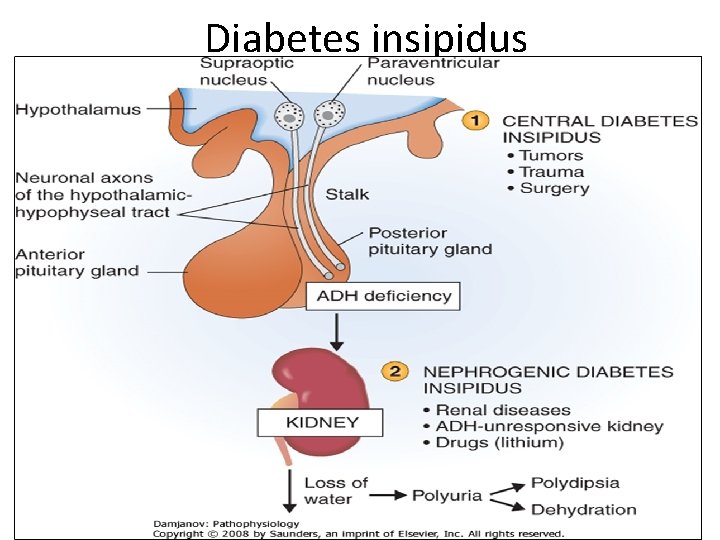
Diabetes insipidus
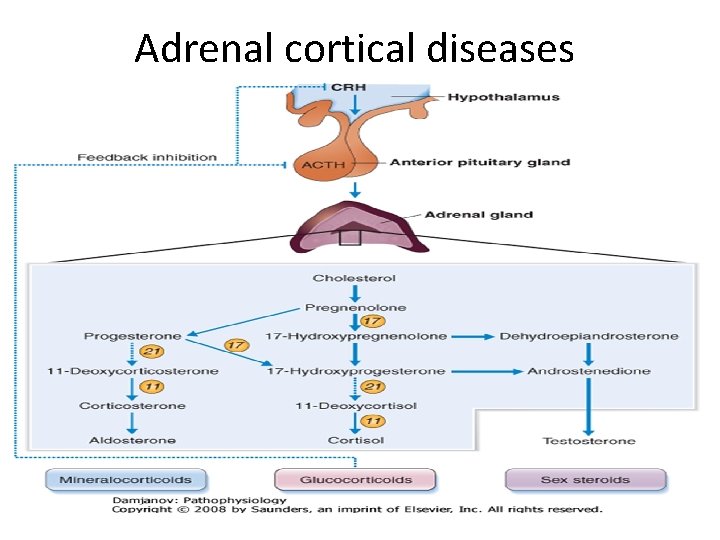
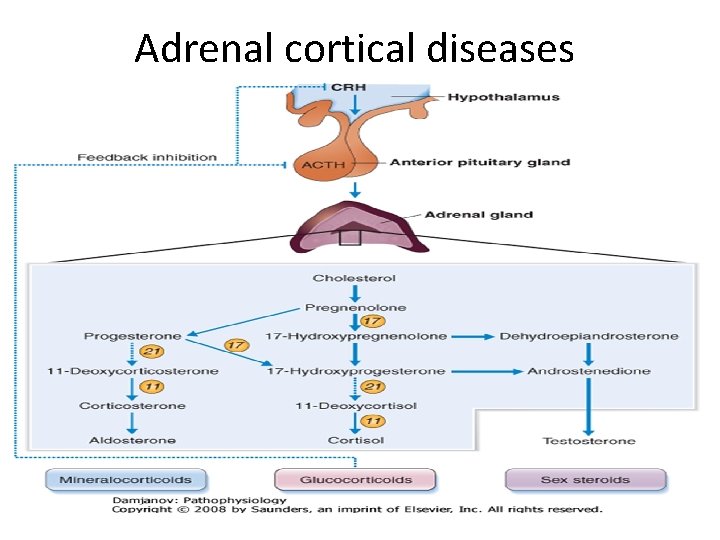
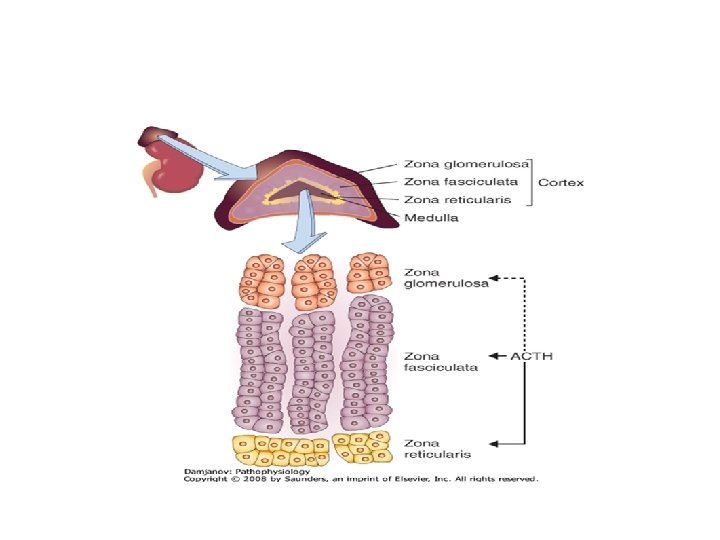
Adrenal cortical diseases
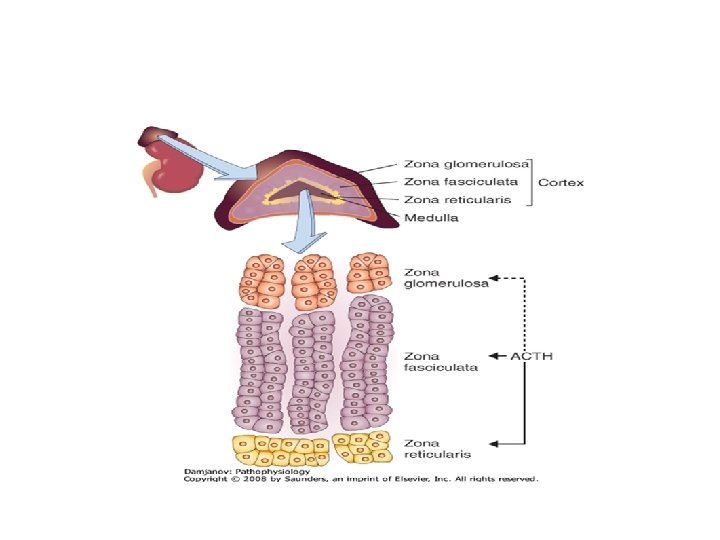
• Aldosterone • mineralocorticoid • acts on distal tubules and collecting ducts to promote uptake of Na+ in exchange for K+ or H+. • Cortisol • glucocorticoid • has anti insulin activity, decreasing glucose uptake in muscle and adipose tissue • enhances the effects of glucagons and epinephrine • Enchanced glycogenolysis and lipolysis • has anti inflammatory effects • inhibits ADH • Androgens • androstenedione, dehydroepiandrostenedione (DHEA) dehydroepiandrostenedione sulfate (DHEAS)
Adrenal cortical diseases Hypersecretion of corticosteroids may result from: 1. Hyperplasia of adrenal cortical cells 2. Benign tumors (adenomas) 3. Malignant tumors (carcinomas) 1. Conn’s syndrome – hyperaldosteronism an excess of aldosterone leads to hypertension and hypokalemia 2. Cushing’s syndrome (hypercortisolism) an excess of glucocorticoids leads to disturbances of the metabolism of carbohydrates, lipids and proteins 3. Adrenogenital syndrome an excess of androgenic hormones
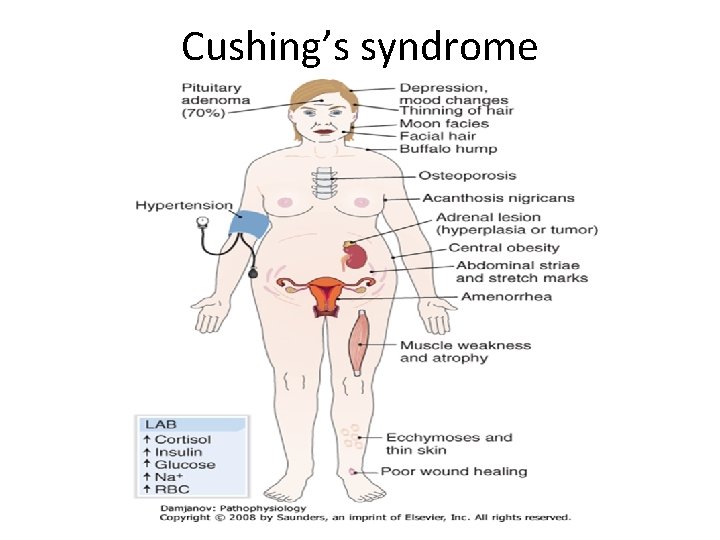
Cushing’s syndrome 1. Pituitary corticotropic adenoma (70%) 2. Adrenal cortical adenoma, carcinoma, or hyperplasia (20%) 3. Ectopic ACTH overproduction (10%) small cell lung cancer, bronchial or gastrointestinal carcinoid tumors 4. Iatrogenic (administration of glucocorticoids for immunosuppression)
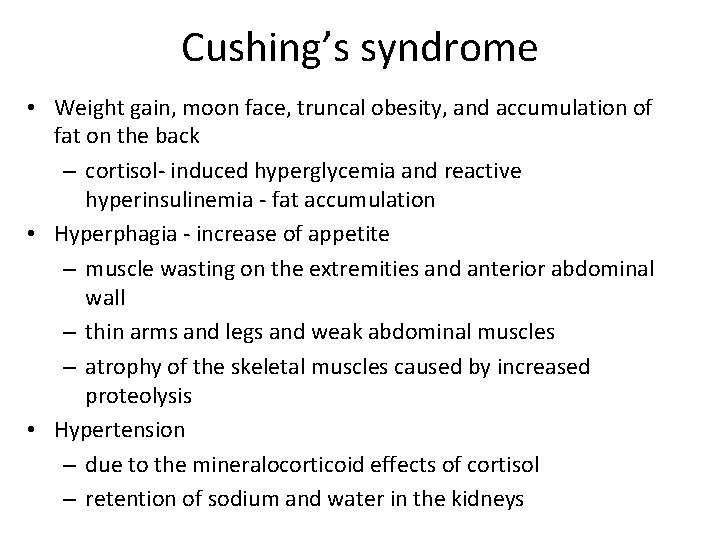
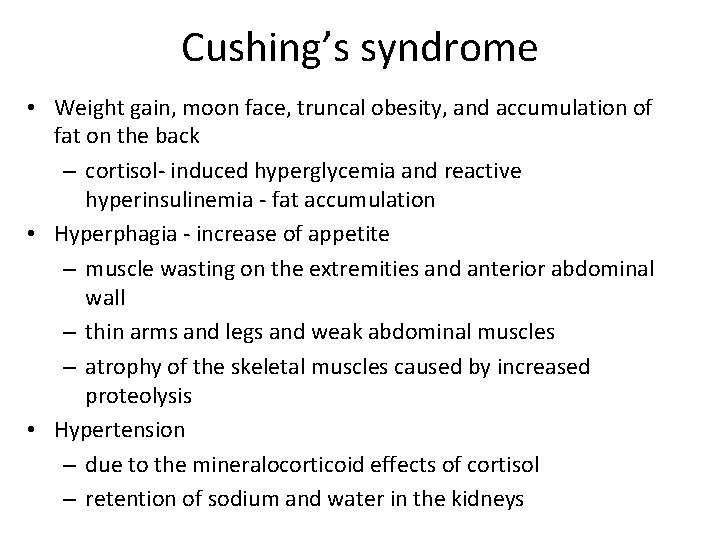
Cushing’s syndrome • Weight gain, moon face, truncal obesity, and accumulation of fat on the back – cortisol induced hyperglycemia and reactive hyperinsulinemia fat accumulation • Hyperphagia increase of appetite – muscle wasting on the extremities and anterior abdominal wall – thin arms and legs and weak abdominal muscles – atrophy of the skeletal muscles caused by increased proteolysis • Hypertension – due to the mineralocorticoid effects of cortisol – retention of sodium and water in the kidneys
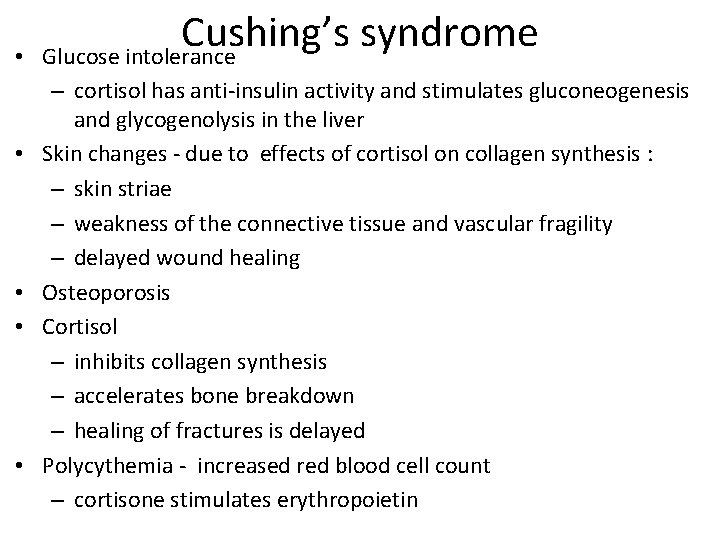
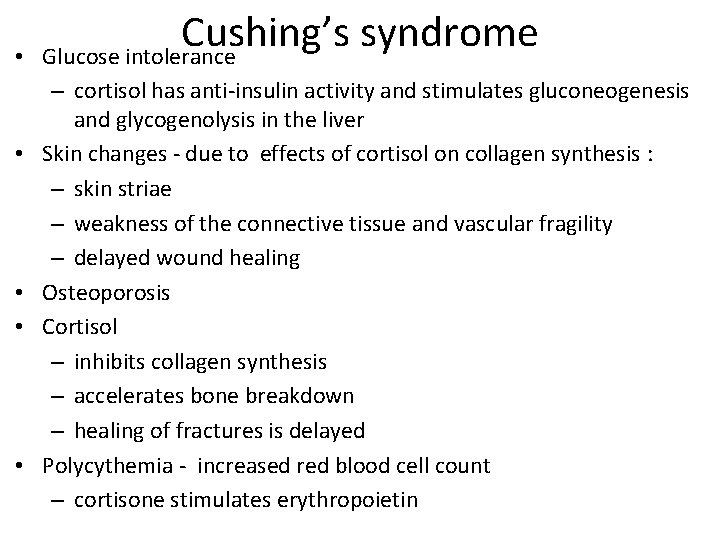
• • • Cushing’s syndrome Glucose intolerance – cortisol has anti insulin activity and stimulates gluconeogenesis and glycogenolysis in the liver Skin changes due to effects of cortisol on collagen synthesis : – skin striae – weakness of the connective tissue and vascular fragility – delayed wound healing Osteoporosis Cortisol – inhibits collagen synthesis – accelerates bone breakdown – healing of fractures is delayed Polycythemia increased red blood cell count – cortisone stimulates erythropoietin

Cushing’s syndrome • Reproductive changes and virilization – menstrual irregularities (oligomenorrhea or amenorrhea, infertility) – signs of virilization, such as hirsutism, and an increased incidence of acne on the face and the back. – these changes are related to the androgenic effects of 17 ketosteroids. – males suffer from impotence and a loss of libido • Depression, sleep disturbances, and memory loss – Patients initially euphoric later depressed – Sleep disturbances l insomnia or lethargy – Short term memory impairement
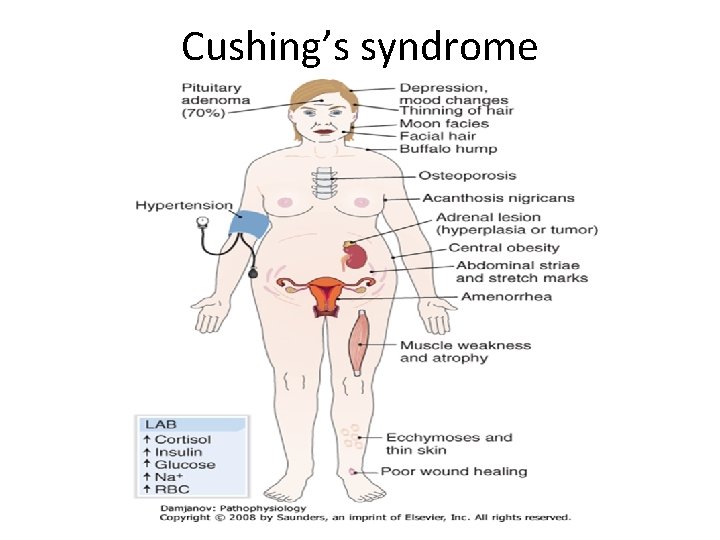
Cushing’s syndrome
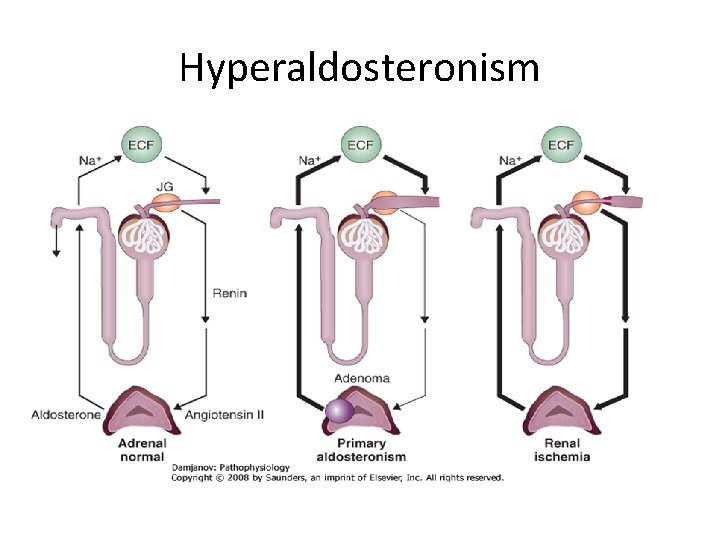
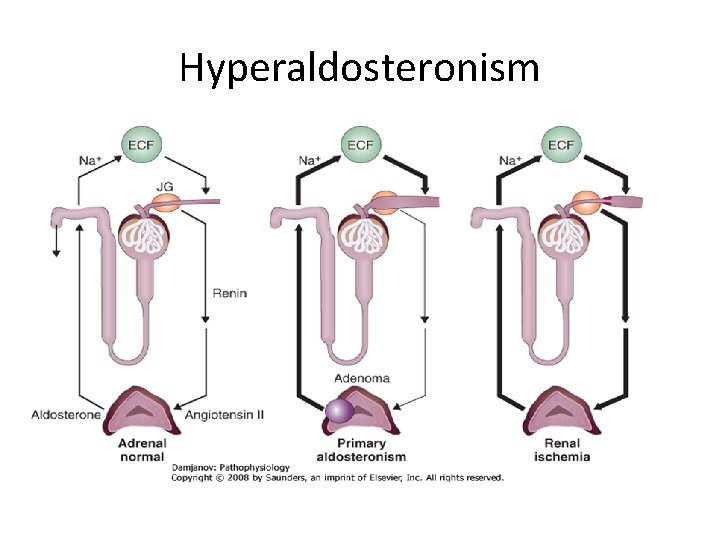
Hyperaldosteronism Two forms of hyperaldosteronism: • 1. Primary hyperaldosteronism (Conn’s syndrome). – cortical adenomas (75%) – idiopathic • 2. Secondary hyperaldosteronism. – the influence of renin angiotensin II aldosterone
Hyperaldosteronism
Hyperaldosteronism
• In primary hyperaldosteronism excess of aldosterone suppresses the secretion of renin (hyporeninemic hyperaldosteronism). • In secondary hyperaldosteronism both the renin and aldosterone levels are high (hyper reninemic hyperaldosteronism).
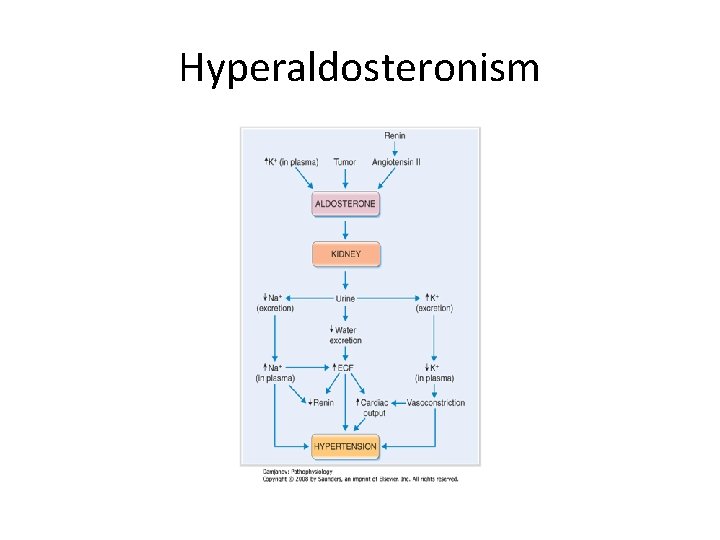
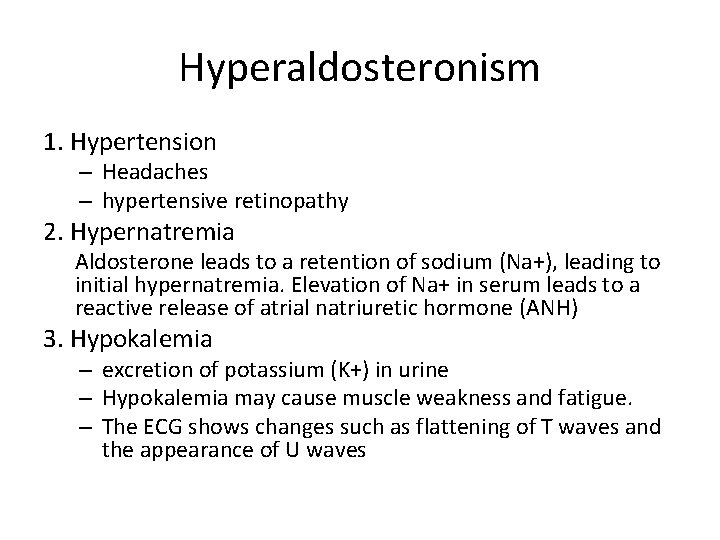
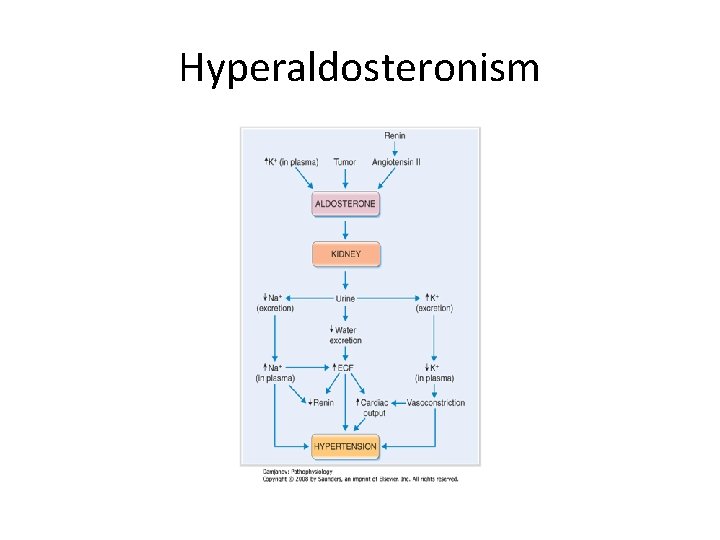
Hyperaldosteronism 1. Hypertension – Headaches – hypertensive retinopathy 2. Hypernatremia Aldosterone leads to a retention of sodium (Na+), leading to initial hypernatremia. Elevation of Na+ in serum leads to a reactive release of atrial natriuretic hormone (ANH) 3. Hypokalemia – excretion of potassium (K+) in urine – Hypokalemia may cause muscle weakness and fatigue. – The ECG shows changes such as flattening of T waves and the appearance of U waves
Hyperaldosteronism 4. Nocturnal polyuria (hypokalemic nephropathy), kidneys resistant to ADH • kidneys cannot retain the water, polyuria induces polydypsia • Loss of K+ is associated with retention of bicarbonate (HCO 3−) metabolic alkalosis 5. Metabolic alkalosis • hypokalemia, the intracellular K+ is released into the blood. • The loss of intracellular K+ is leads to intracellular influx of H+ and Na+. • The loss of H+ causes metabolic alkalosis.
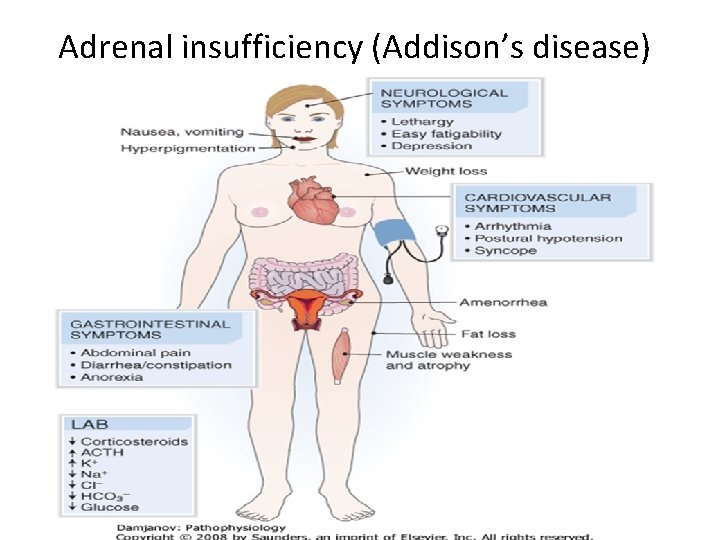
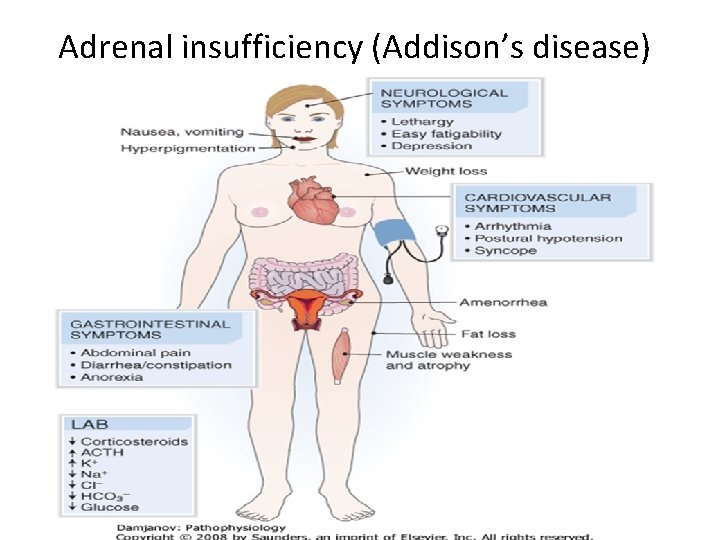
Adrenal insufficiency (Addison’s disease)
Clinical signs and symptoms 1. Weakness and easy fatigability 2. Weight loss and anorexia 3. Hyperpigmentation of the skin and mucous membranes 4. Nausea and vomiting 5. Abdominal pain 6. Diarrhea or constipation 7. Electrocardiographic changes of hyperkalemia, such as high peaked T waves and a prolonged PR interval • 8. Cardiac arrhythmia, including cardiac block • 9. Salt craving • 10. Orthostatic hypotension and syncope • •
Diseases of the Adrenal Medulla Tumors : • Neuroblastoma in childhood • tumors are composed of primitive neuroblastic precursors of adrenal medullary cells • Pheochromocytoma in adults • the tumors are composed of well differentiated cells secreting epinephrine or norepinephrine
Pheochromocytoma 1. Heart—tachycardia and stronger myocyte contraction 2. Blood vessels—vasoconstriction, but also vasodilation in some vessels 3. Kidney—renin release 4. Liver—glycogenolysis leading to hyperglycemia 5. Fat tissue—lipolysis 6. Intestine—smooth muscle cell relaxation and loss of peristalsis 7. Skin—sweating with cold and pale extremities due to constriction of peripheral arterioles
1. Hypertension Pheochromocytoma results from vasoconstriction of arterioles and increased cardiac output better venous return positive inotropic effect of catecholamines on the myocardium In about 50% of cases the hypertension is sustained 2. Sympathetic effects headache, sweating, palpitations, tachycardia, facial flushing, nausea, vomiting 3. Postural hypotensive episodes and syncope 4. increased metabolic rate fever with sweating, tachycardia, easy fatigability, weight loss 5. Hyperglycemia Catecholamines have an anti insulin effect and promote glycogenolysis hyperlipidemia lipolytic effect of catecholamines on peripheral fat stores
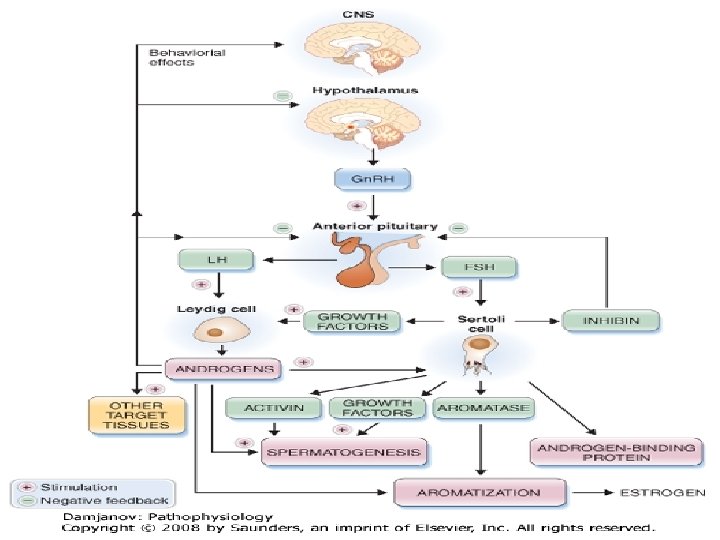
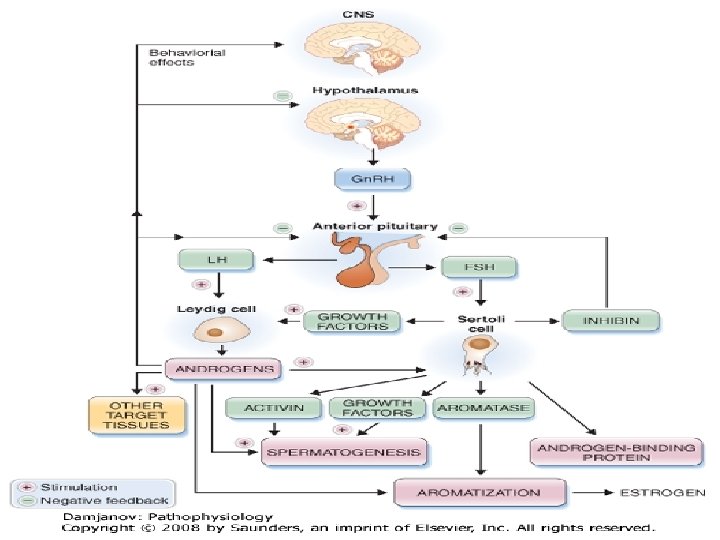
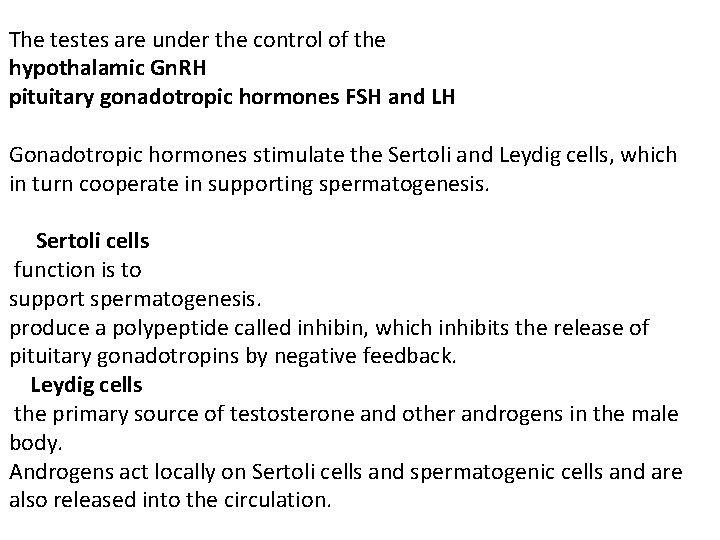
The testes are under the control of the hypothalamic Gn. RH pituitary gonadotropic hormones FSH and LH Gonadotropic hormones stimulate the Sertoli and Leydig cells, which in turn cooperate in supporting spermatogenesis. Sertoli cells function is to support spermatogenesis. produce a polypeptide called inhibin, which inhibits the release of pituitary gonadotropins by negative feedback. Leydig cells the primary source of testosterone and other androgens in the male body. Androgens act locally on Sertoli cells and spermatogenic cells and are also released into the circulation.
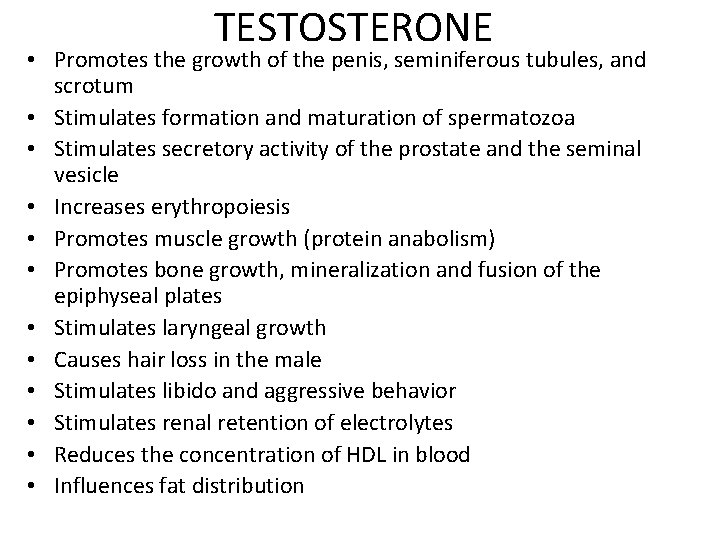
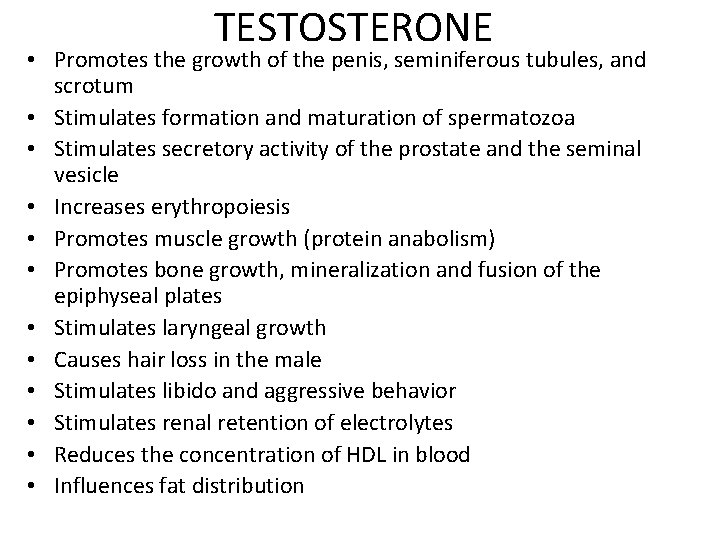
TESTOSTERONE • Promotes the growth of the penis, seminiferous tubules, and scrotum • Stimulates formation and maturation of spermatozoa • Stimulates secretory activity of the prostate and the seminal vesicle • Increases erythropoiesis • Promotes muscle growth (protein anabolism) • Promotes bone growth, mineralization and fusion of the epiphyseal plates • Stimulates laryngeal growth • Causes hair loss in the male • Stimulates libido and aggressive behavior • Stimulates renal retention of electrolytes • Reduces the concentration of HDL in blood • Influences fat distribution
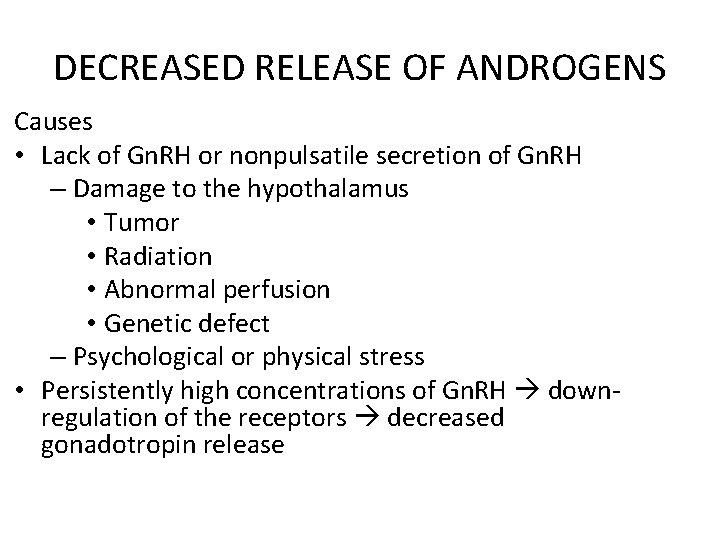
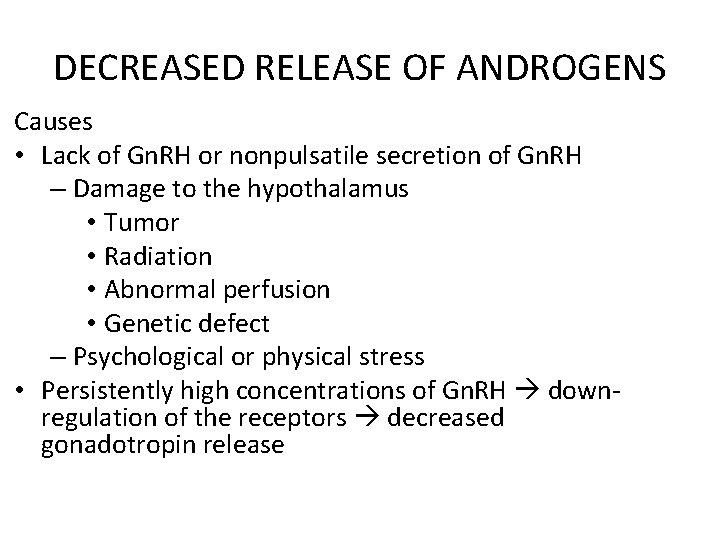
DECREASED RELEASE OF ANDROGENS Causes • Lack of Gn. RH or nonpulsatile secretion of Gn. RH – Damage to the hypothalamus • Tumor • Radiation • Abnormal perfusion • Genetic defect – Psychological or physical stress • Persistently high concentrations of Gn. RH down regulation of the receptors decreased gonadotropin release

DECREASED RELEASE OF ANDROGENS • Inhibition of gonadotropin release • Prolactin • Damage to the pituitary – Trauma – Infarct – Autoimmune disease – Tumor – Hyperplasia • Damage to the testes – Genetic defect – Severe systemic disease • Enzyme defects in hormone synthesis • Defect of testosterone receptors
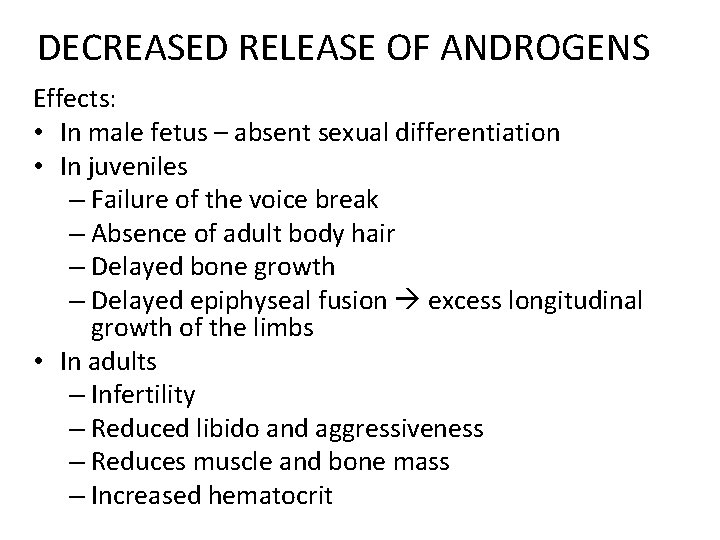
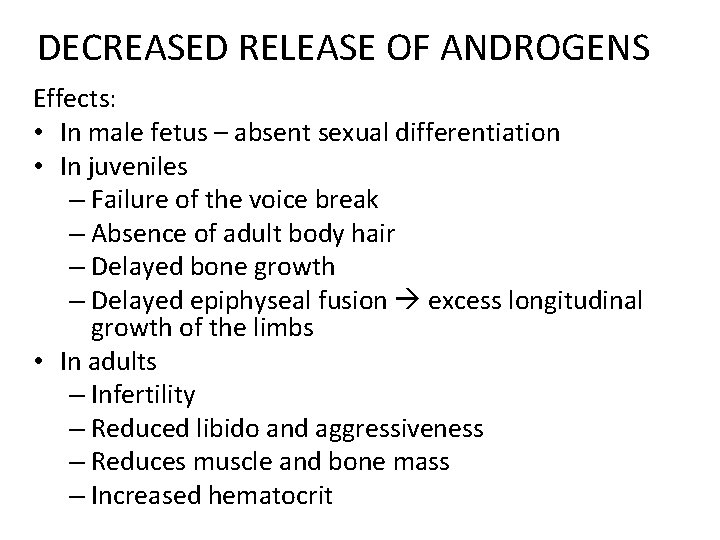
DECREASED RELEASE OF ANDROGENS Effects: • In male fetus – absent sexual differentiation • In juveniles – Failure of the voice break – Absence of adult body hair – Delayed bone growth – Delayed epiphyseal fusion excess longitudinal growth of the limbs • In adults – Infertility – Reduced libido and aggressiveness – Reduces muscle and bone mass – Increased hematocrit
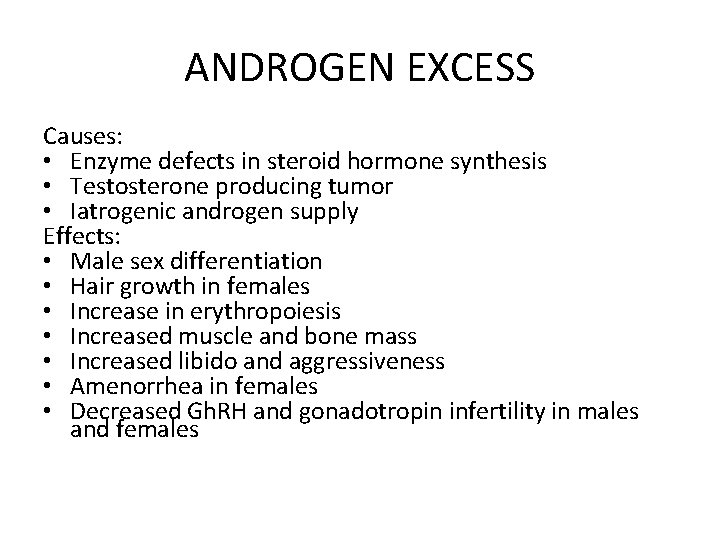
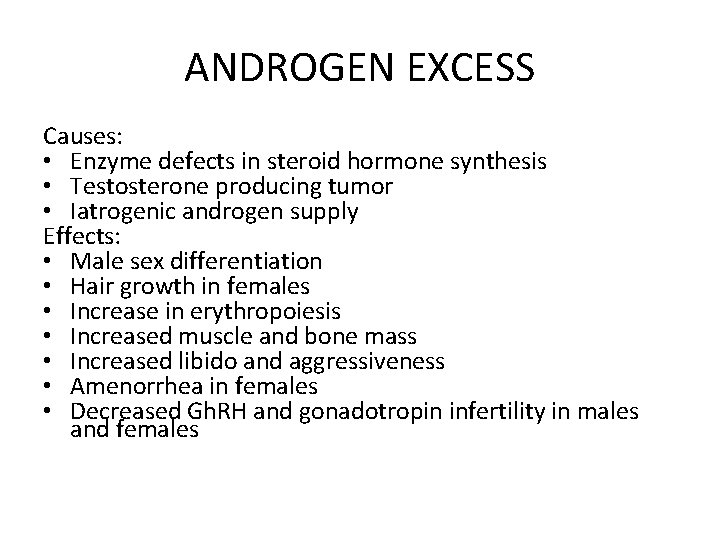
ANDROGEN EXCESS Causes: • Enzyme defects in steroid hormone synthesis • Testosterone producing tumor • Iatrogenic androgen supply Effects: • Male sex differentiation • Hair growth in females • Increase in erythropoiesis • Increased muscle and bone mass • Increased libido and aggressiveness • Amenorrhea in females • Decreased Gh. RH and gonadotropin infertility in males and females
GONADOTROPIC HORMONES IN FEMALES • LH and FSH released from the pituitary anterior lobe in pulsatile manner (every 60 to 90 minutes for 1 min. ) • Stimulated by pulsatile release of Gn. RH from the hypothalamus Effects of FSH: • Promotes the maturation of the follicles • Stimulates estrogen production in the granulosa cells of the follicles Effect of LH: • Stimulates follicle rupture and ovum discharge • Stimulates corpus luteum formation • Stimulates progesterone synthesis
• During follicular phase: • Estrogens (estrone, estradiol, estriol) stimulate release of gonadotropins – positive feedback • During luteal phase: • Progestogens (progesterone and analogs) and estrogens inhibit further release of gonadotropins (negative feedback) • Granulosa cells produce activin (promotes gonadotropin release) and inhibin (suppresses it).

Hypothalamic pituitary ovarian axis. Gonadotropin releasing hormone (Gn. RH) stimulates the pituitary, which secretes the follicle stimulating hormone (FSH) luteinizing hormone (LH). FSH and LH stimulate granulosa and theca cells to produce estrogens, progestins, androgens, inhibins, and activins, which provide negative or positive feedback to the hypothalamus or the pituitary. Inhibin inhibits the pituitary activins activate it.

Hormonal changes during the menstrual cycle. The surge of luteinizing hormone (LH) on day 13 leads to ovulation, a point that divides the proliferative from the secretory phase. Estrogen is the prevalent ovarian hormone during the proliferative (follicular) phase. Progesterone predominates in the secretory phase. FSH, follicle stimulating hormone.
ESTROGENS PHYSIOLOGICAL ACTION • • • Promote the development of the female sex characteristic The secondary sexual characteristics Development of the mammary glands Female fat distribution Promote bone growth and maturation and accelerate epiphyseal fusion Influence the psychological development of women Increase the coagulability of blood Raise electrolyte retention in the kidneys Increase mineralization of the bones Hydroxylation of vitamin D 3 Inhibition of parathyroid hormone (PTH)
PROGESTERONE PHYSIOLOGICAL ACTION • Promotes the maturation and secretory activity of the uterine mucosa • Decreases the contractility of the uterine muscle • Raise the body’s metabolism and temperature • Trigger hyperventilation • Reduce sensitivity to insulin in the periphery • Moderate glucocorticoid antimineralocorticoid (natriuretic) actions • Lower the production of cholesterol and the plasma concentration of HDL and LDL.
FEMALE SEX HORMONES EXCESS Causes: • Exogenous supply (contraceptive pills) • Tumors producing sex hormones – Folliculoma – Thecoma
DEFICIENCY OF GONADOTROPINS Causes: • Decreased Gn. RH release – Malnutrition – Severe systemic disease – High performance sport – Influence of neurotransmitters: norepinephrine, dopamine, serotonin, endorphins • Persistently high concentrations of Gn. RH down regulation of Gn. RH receptor
DEFICIENCY OF GONADOTROPINS • Damage to the pituitary • Displacement of the gonadotropin producing cells by tumor • Raised concentration of the sex hormones • Ovulation inhibitors • Anabolic substances with androgen action • Tumors • Androgenital syndrome • Polycystic ovaries • Prolactin excess
ADRENOGENITAL SYNDROME 21β hydroxylase deficiency impaired transformation of: – progesterone into 11 desoxycorticosterone – 17 hydroxyprogesterone into 11 desoxycortisol Effects: – Cortisol deficiency – Disinhibition of ACTH release – Stimulation of synthesis of the steroid precursors – Increased formation of androstendion and testosterone
PROLACTIN EXCESS Causes: 1. Hormone producing tumors 2. Antidopaminergic drugs 3. Renal and liver failure 4. Hypothyroidism

ESTROGENS AND PROGESTERONE DEFFICIENCY Causes: • Ovarian insufficiency – Abnormal development – Damage to the ovaries • Radiation • Chemotherapeutic agents • Inadequate follicle maturation or transformation into corpus luteum (corpus luteum insufficiency) • Enzyme defect • Resistant ovary syndrome – ovaries are refractory to gonadotropins – Defective receptor – Inactivating antibodies
DEFFICIENCY OF FEMALE SEX HORMONES EFFECTS • Infertility Progestogen deficiency • Uterine mucosa does not mature Estrogen deficiency • Phase of uterine proliferation is absent • Osteoporosis • Increased risk of atherosclerosis

EXCESS OF FEMALE SEX HORMONES EFFECTS Excess of estrogens • Thrombosis raised clotting tendency • In children – Premature sexual maturation – Accelerated growth – Premature epiphyseal fusion short stature Excess of progestogen • Natriuresis • Rise in body temperature • Hyperventilation • Insulin resistance diabetes mellitus.