PHYSIOLOGY REPRODUCTION The External Genitals External genitals collectively
- Slides: 48
PHYSIOLOGY REPRODUCTION
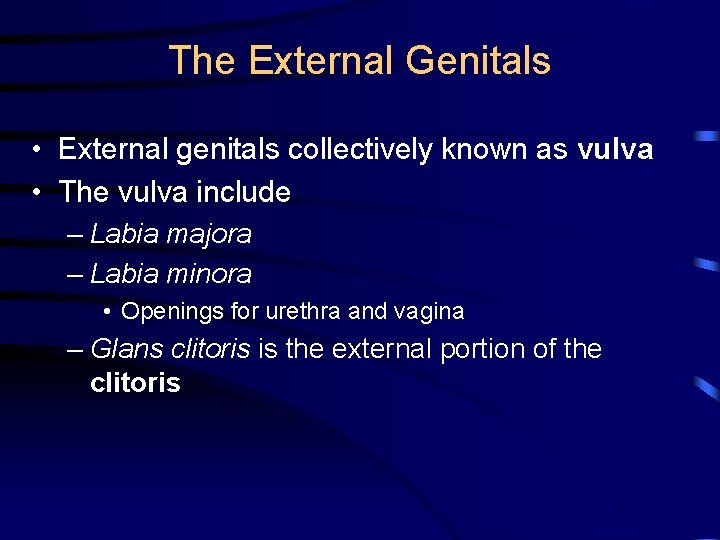
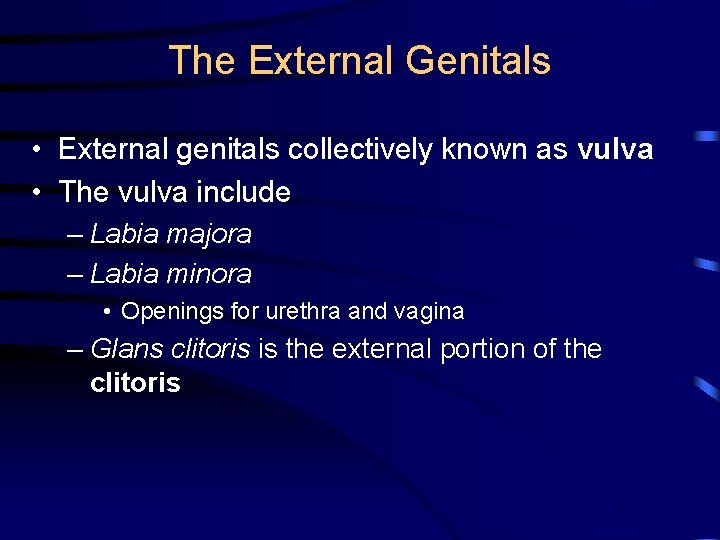
The External Genitals • External genitals collectively known as vulva • The vulva include – Labia majora – Labia minora • Openings for urethra and vagina – Glans clitoris is the external portion of the clitoris
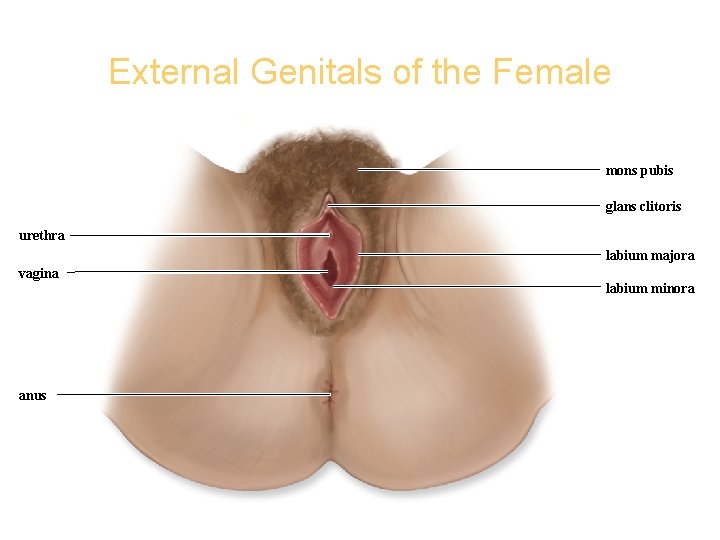
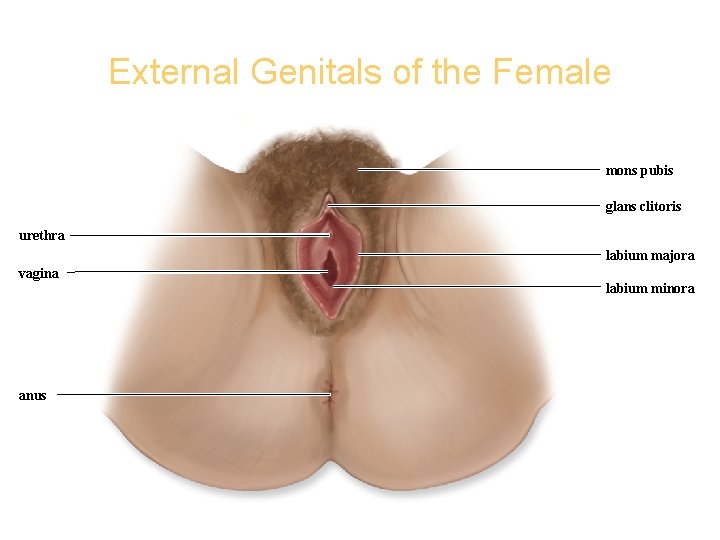
External Genitals of the Female Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. mons pubis glans clitoris urethra labium majora vagina anus labium minora
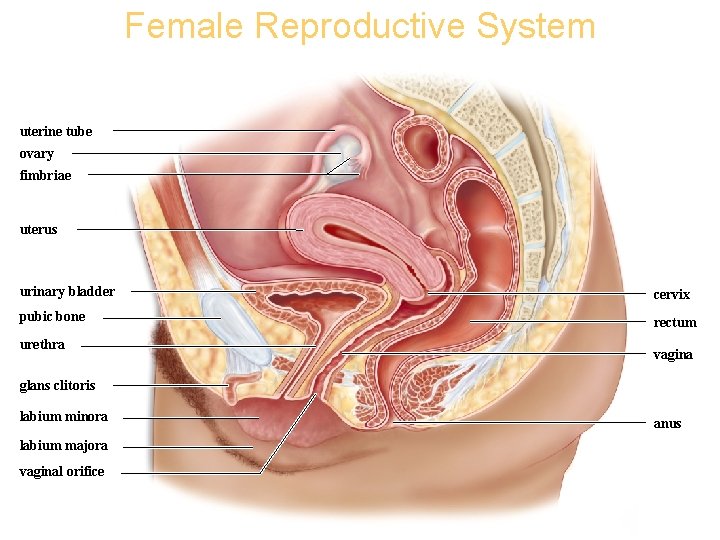
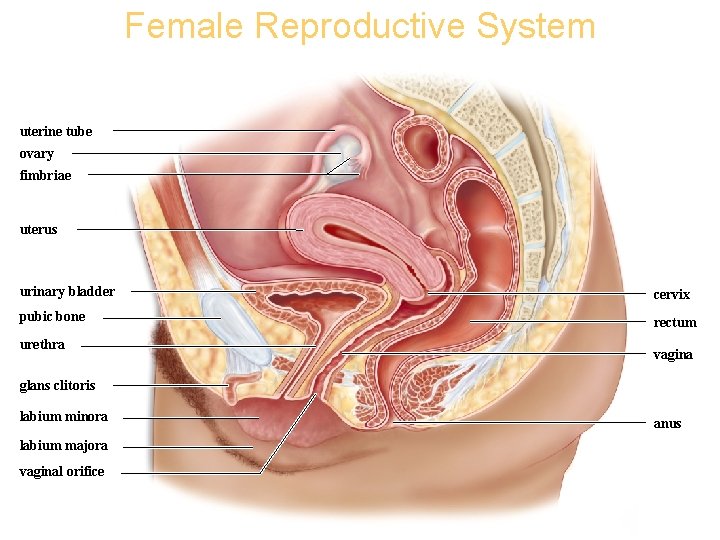
Female Reproductive System Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. uterine tube ovary fimbriae uterus urinary bladder cervix pubic bone rectum urethra vagina glans clitoris labium minora labium majora vaginal orifice anus
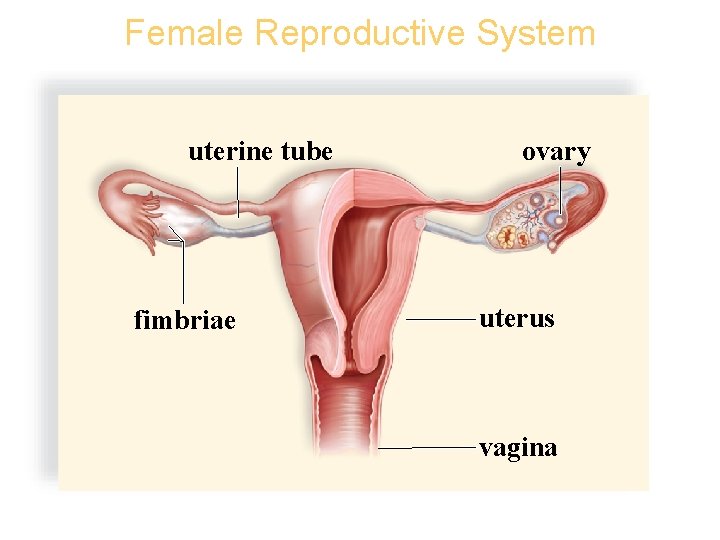
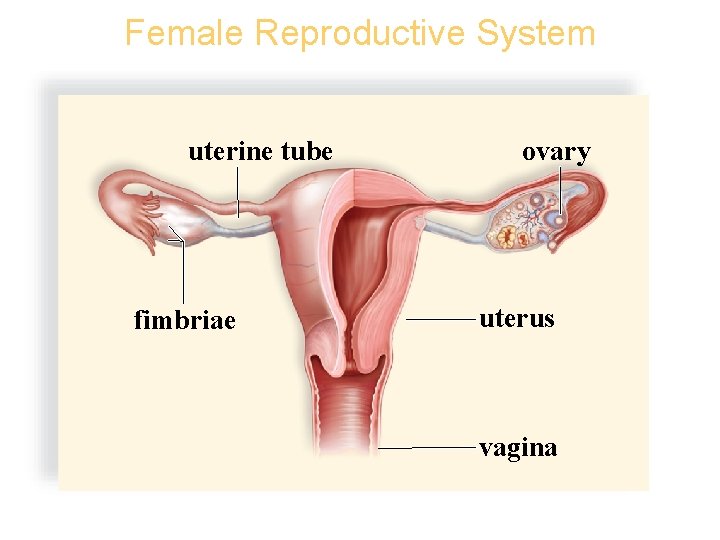
Female Reproductive System Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. uterine tube fimbriae ovary uterus vagina
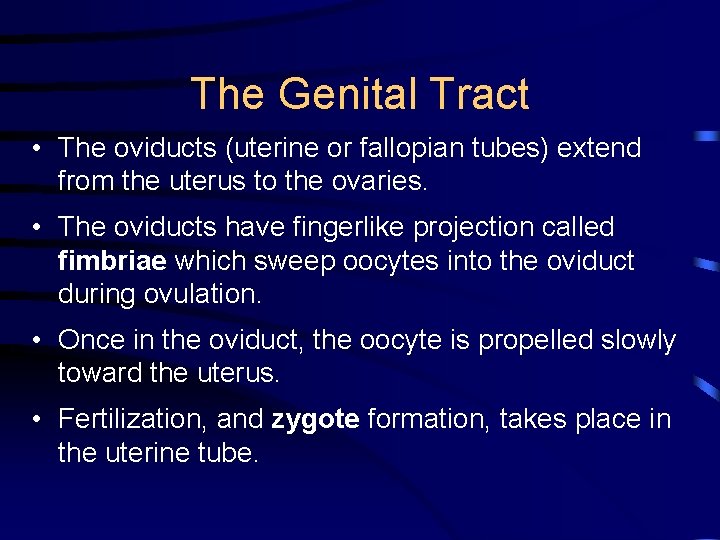
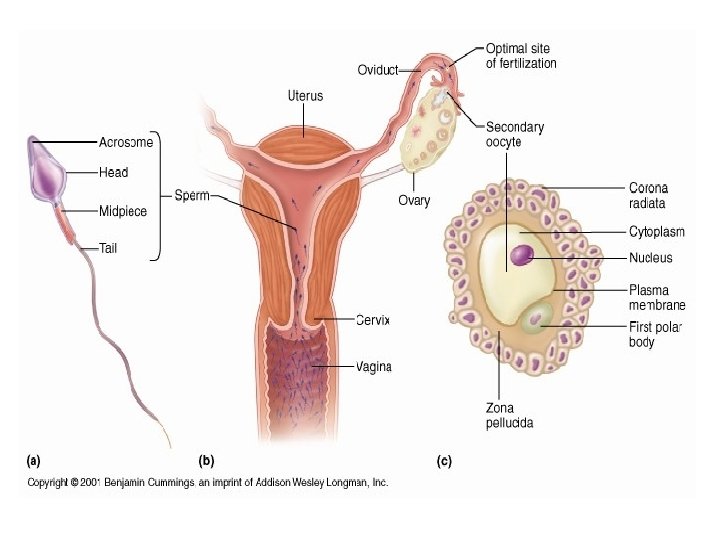
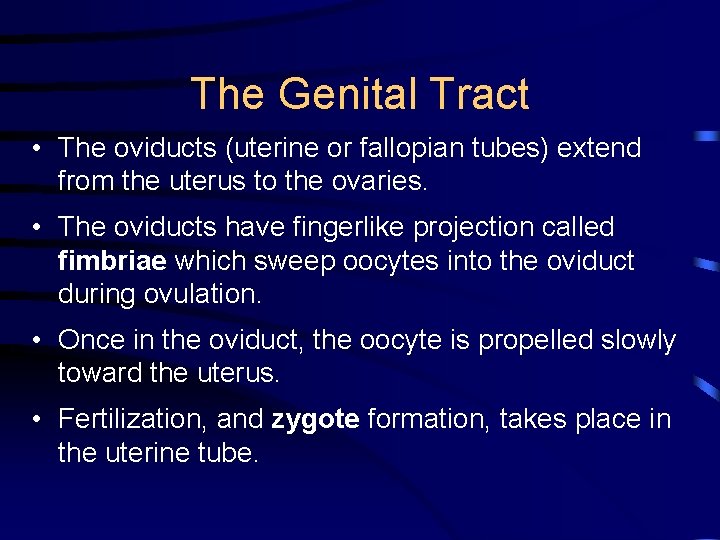
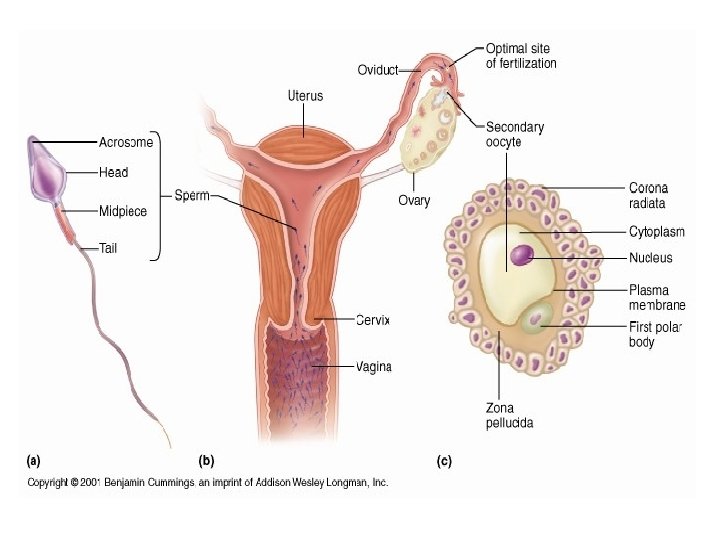
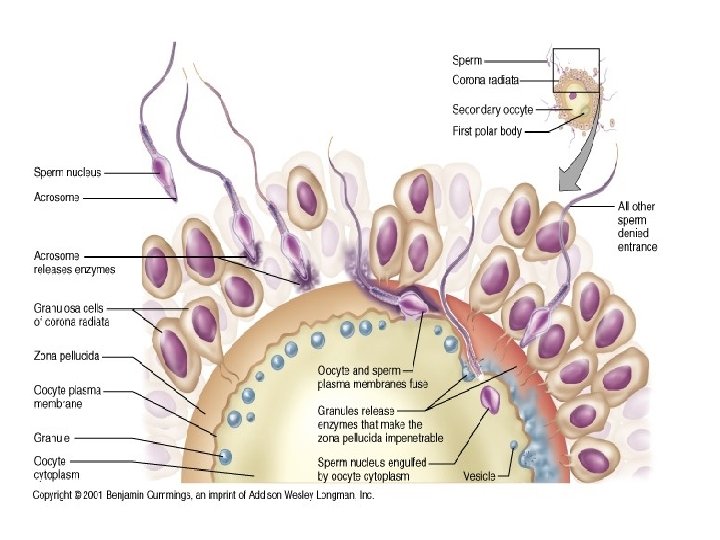
The Genital Tract • The oviducts (uterine or fallopian tubes) extend from the uterus to the ovaries. • The oviducts have fingerlike projection called fimbriae which sweep oocytes into the oviduct during ovulation. • Once in the oviduct, the oocyte is propelled slowly toward the uterus. • Fertilization, and zygote formation, takes place in the uterine tube.
The Genital Tract • The uterus is a thick-walled, muscular organ. – Endometrium-inner lining of the uterus-participates in the formation of the placenta • The uterine tubes join the uterus at the upper end, while at the lower end, the cervix connects with the vagina. – The vagina is a tube that lies at a 45° angle to small of the back • Mucosal lining lies in folds and can extend-especially important during birth
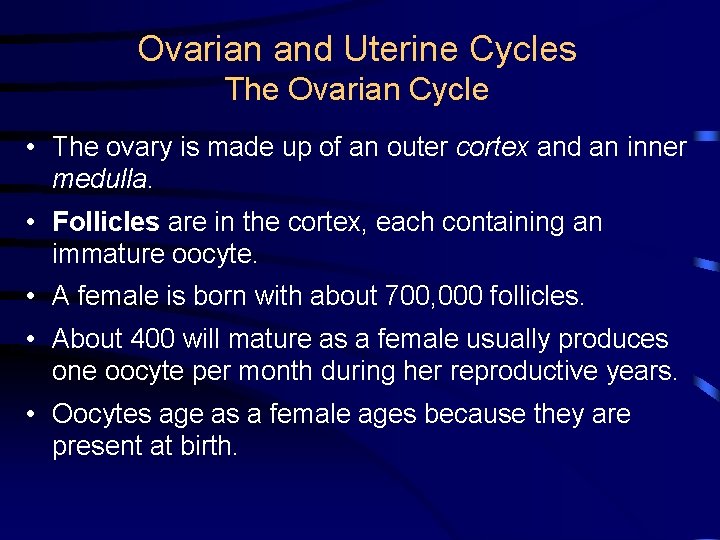
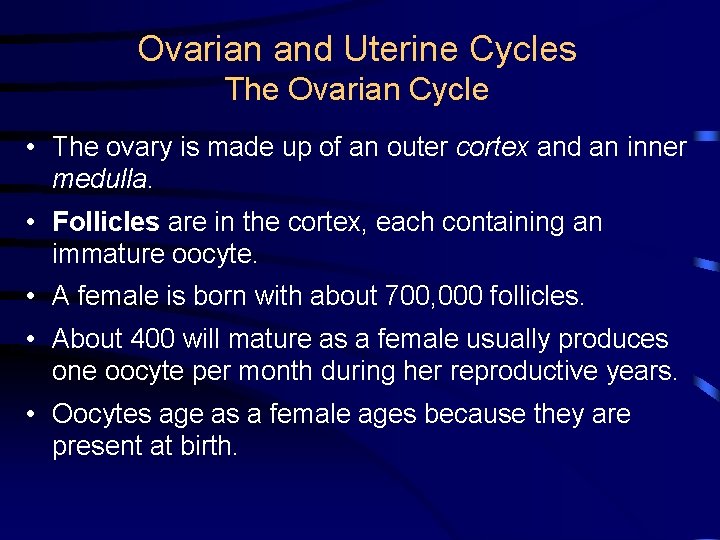
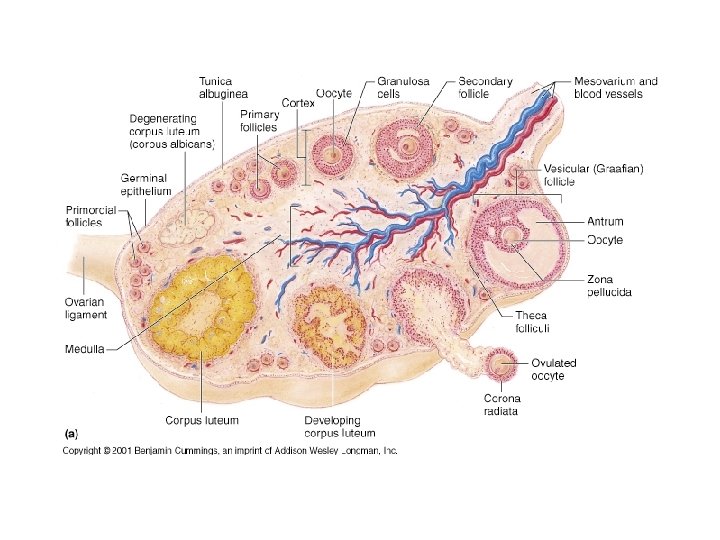
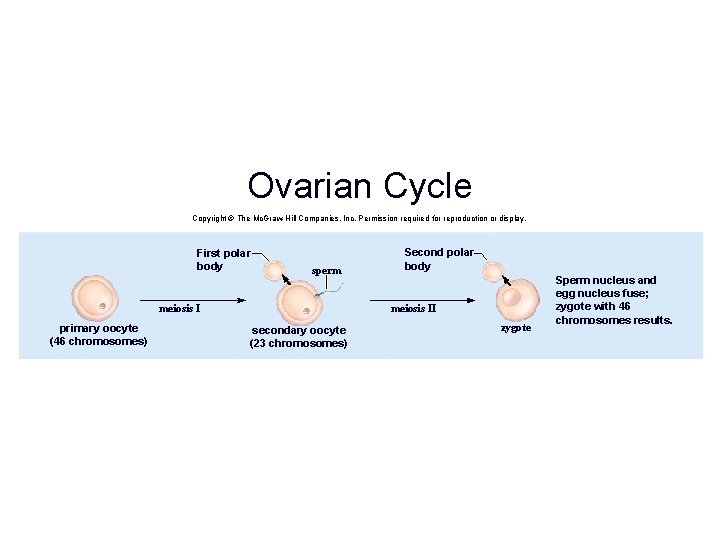
Ovarian and Uterine Cycles The Ovarian Cycle • The ovary is made up of an outer cortex and an inner medulla. • Follicles are in the cortex, each containing an immature oocyte. • A female is born with about 700, 000 follicles. • About 400 will mature as a female usually produces one oocyte per month during her reproductive years. • Oocytes age as a female ages because they are present at birth.
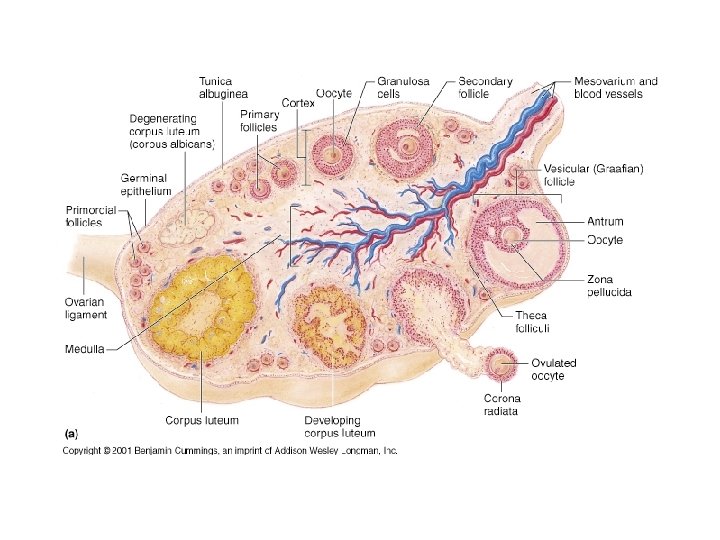
Ovarian and Uterine Cycles The Ovarian Cycle • The ovary is made up of an outer cortex and an inner medulla. • Follicles are in the cortex, each containing an immature oocyte. • A female is born with about 700, 000 follicles. • About 400 will mature as a female usually produces one oocyte per month during her reproductive years. • Oocytes age as a female ages because they are present at birth.
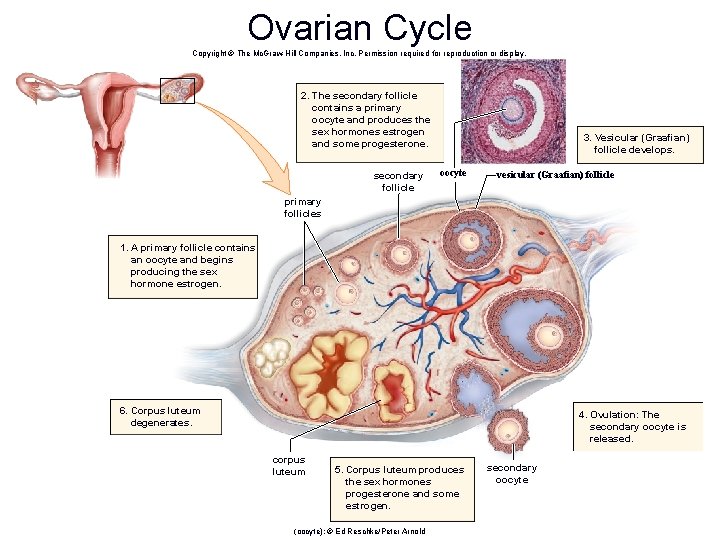
The Ovarian Cycle • The ovarian cycle occurs as a follicle changes from a primary to secondary to a vesicular follicle. • Epithelial cells of a primary follicle surround a primary oocyte. • Pools of follicular fluid surround the oocyte in a secondary follicle. • In a vesicular follicle, a fluid-filled cavity balloons out on the surface of the ovary.
The Ovarian Cycle • The ovarian cycle occurs as a follicle changes from a primary to secondary to a vesicular follicle. • Epithelial cells of a primary follicle surround a primary oocyte. • Pools of follicular fluid surround the oocyte in a secondary follicle. • In a vesicular follicle, a fluid-filled cavity balloons out on the surface of the ovary.
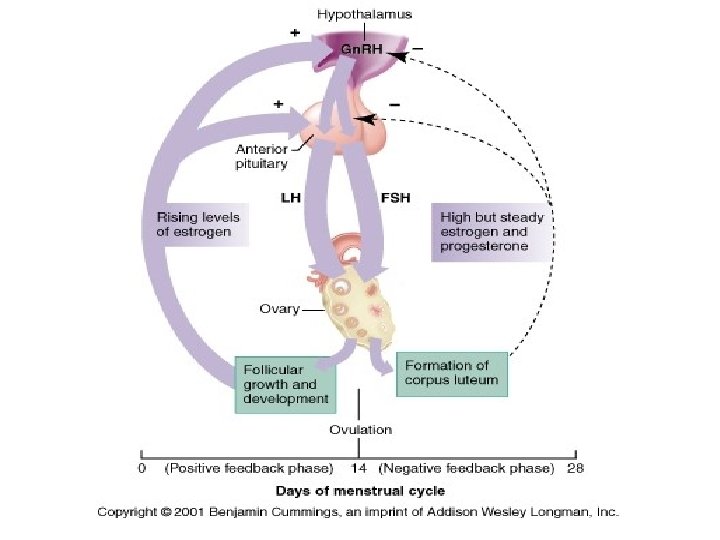
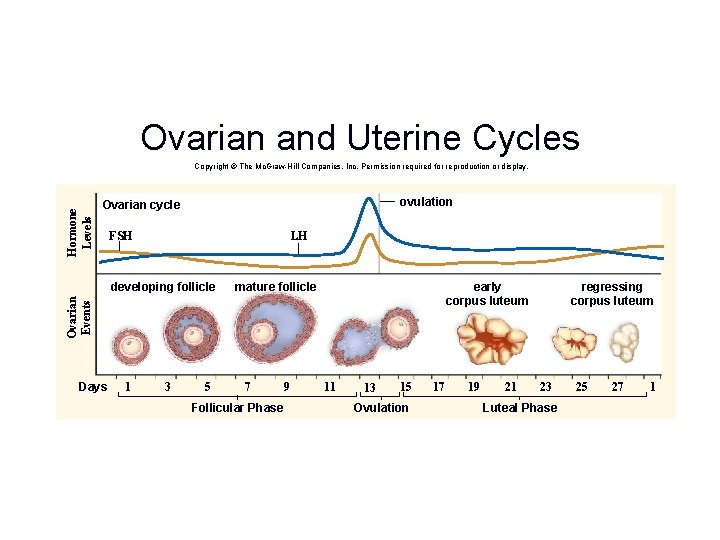
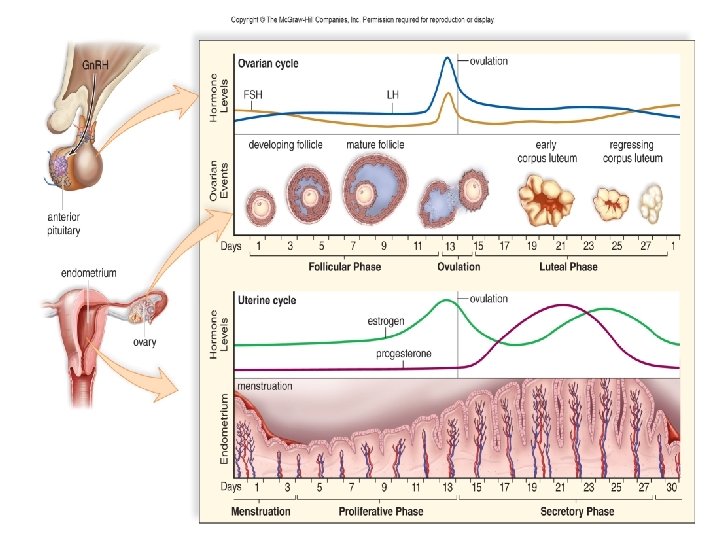
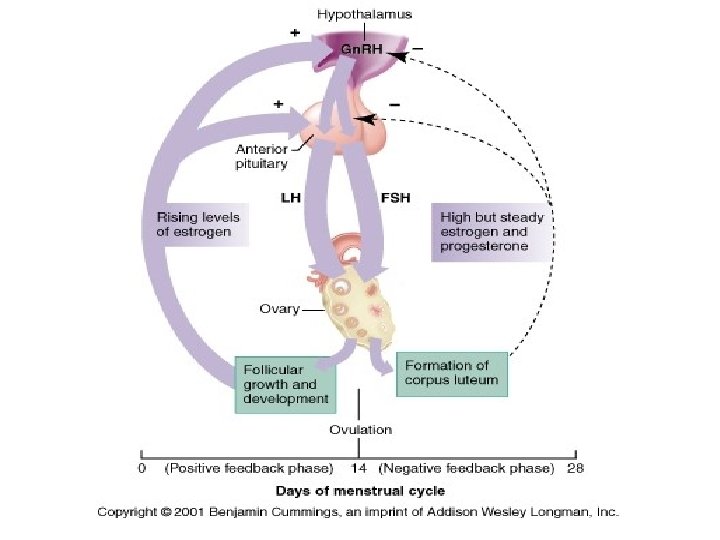
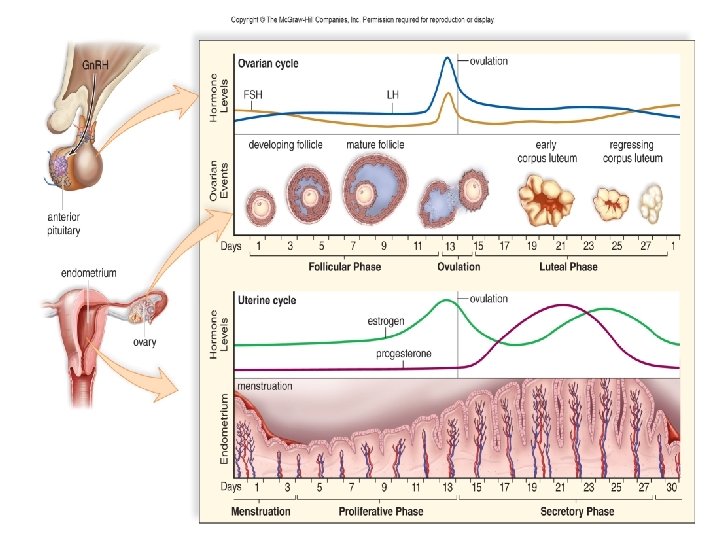
Phases of the Ovarian Cycle • Two phases of ovarian cycle – Follicular phase and luteal phase • Follicular phase – FSH promotes development of the follicle in the ovary – The ovary secretes estrogen and progesterone. – As estrogen levels rise, it exerts negative feedback control on anterior pituitary secretion of FSH. – The follicular phase comes to an end.
Phases of the Ovarian Cycle • Two phases of ovarian cycle • Luteal phase – LH promotes corpus luteum development, which secretes progesterone and some estrogen. – As blood progesterone levels rise, it exerts feedback control over the anterior pituitary secretion of LH. – The corpus luteum begins to degenerate. – The low progesterone and estrogen levels cause menstruation to begin.
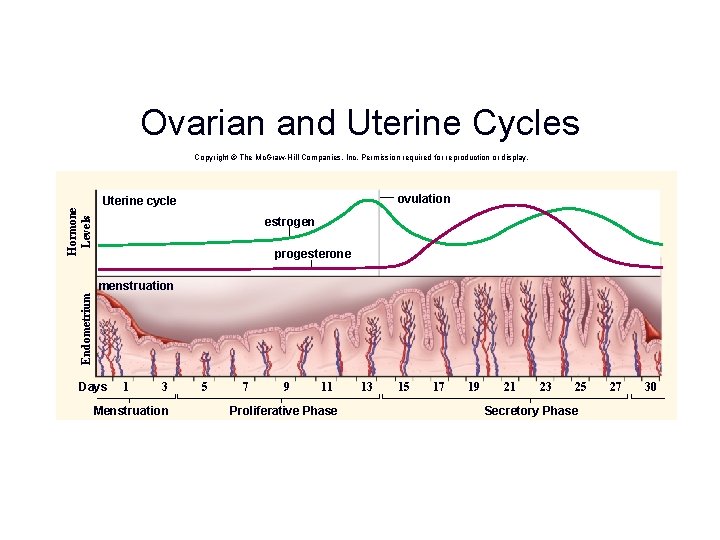
The Uterine Cycle • Estrogen and progesterone (sex hormones) affect the endometrium, causing the uterus to undergo a cyclical series of events known as the uterine cycle • 28 day cycles are divided as follows: • Days 1 to 5, low levels of sex hormones cause the endometrium to disintegrate and its blood vessels to rupture – On day one of the cycle, blood and tissues pass out of vagina during menstruation
The Uterine Cycle • Days 6 to 13, increased estrogen production by a new ovarian follicle causes the endometrium to thicken and become vascular and glandular • This is called the proliferative phase • Day 14 of 28 day cycle, ovulation usually occurs
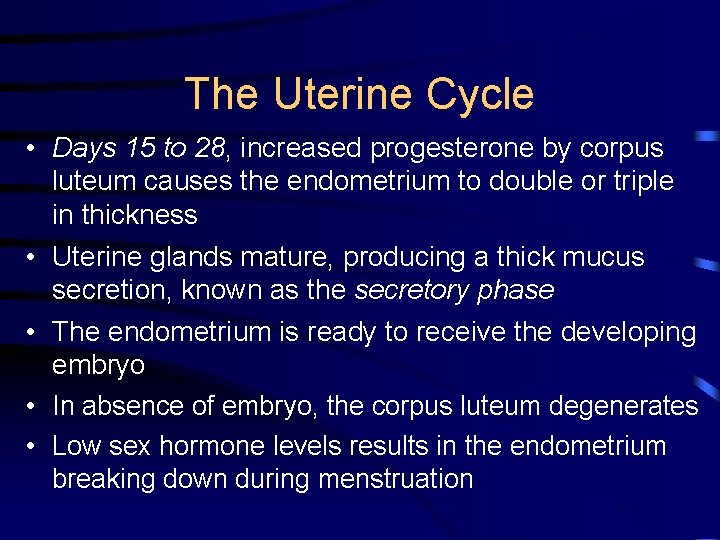
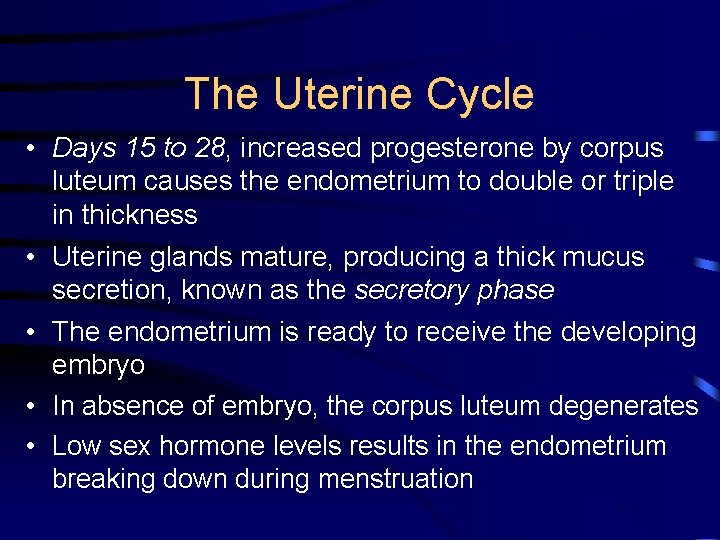
The Uterine Cycle • Days 15 to 28, increased progesterone by corpus luteum causes the endometrium to double or triple in thickness • Uterine glands mature, producing a thick mucus secretion, known as the secretory phase • The endometrium is ready to receive the developing embryo • In absence of embryo, the corpus luteum degenerates • Low sex hormone levels results in the endometrium breaking down during menstruation
The Uterine Cycle • Estrogen and progesterone – Both have effects other than those in the ovarian and uterine cycles. – Estrogen • Maintains female secondary sex characteristics – Breast development, axillary and pubic hair, subcutaneous fat deposition – Wider pelvis – Progesterone • Also needed for breast development
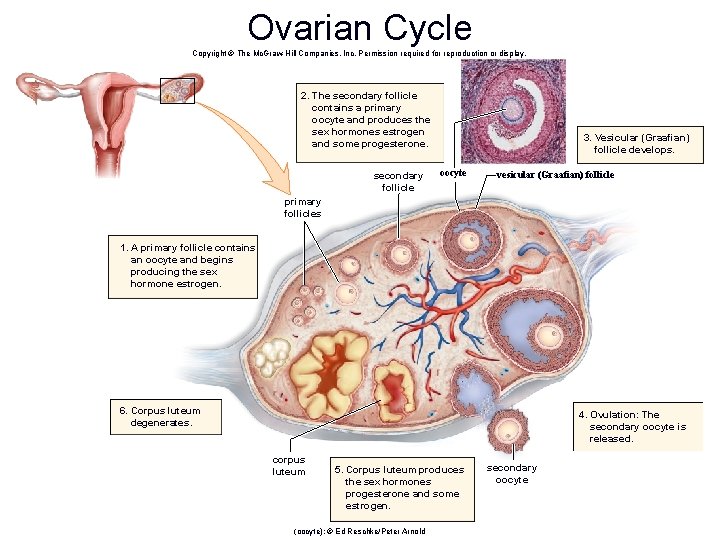
Ovarian Cycle Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. 2. The secondary follicle contains a primary oocyte and produces the sex hormones estrogen and some progesterone. secondary follicle 3. Vesicular (Graafian) follicle develops. oocyte vesicular (Graafian) follicle primary follicles 1. A primary follicle contains an oocyte and begins producing the sex hormone estrogen. 6. Corpus luteum degenerates. 4. Ovulation: The secondary oocyte is released. corpus luteum 5. Corpus luteum produces the sex hormones progesterone and some estrogen. (oocyte): © Ed Reschke/Peter Arnold secondary oocyte
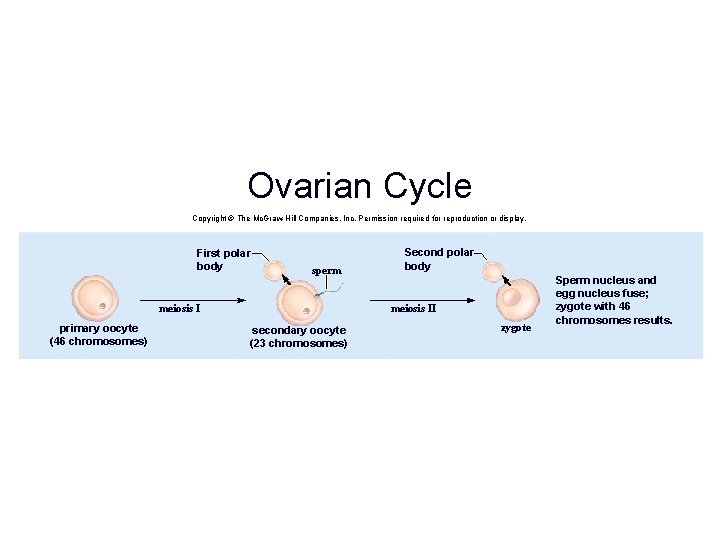
Ovarian Cycle Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. First polar body sperm meiosis I primary oocyte (46 chromosomes) Second polar body meiosis II secondary oocyte (23 chromosomes) zygote Sperm nucleus and egg nucleus fuse; zygote with 46 chromosomes results.
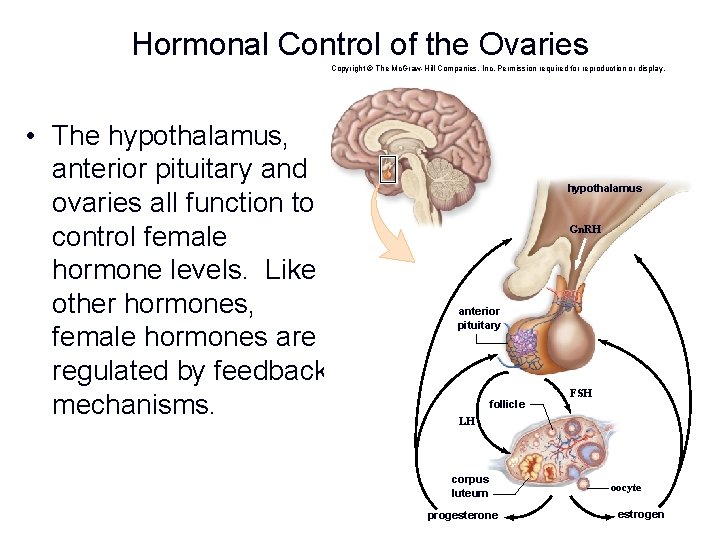
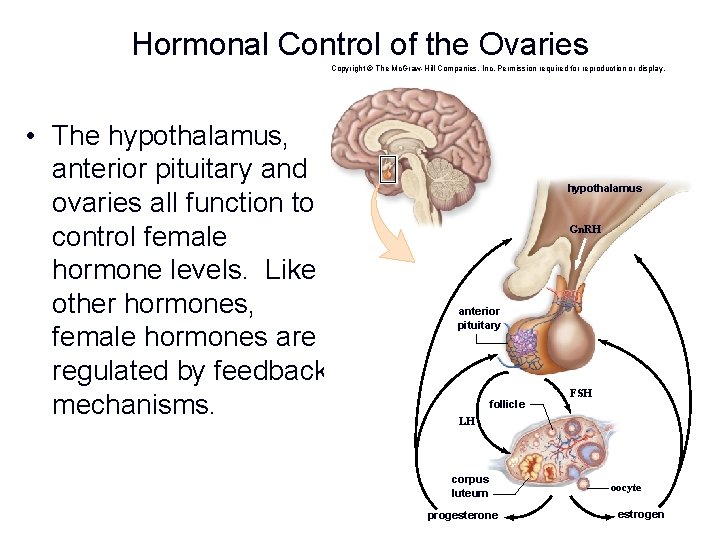
Hormonal Control of the Ovaries Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. • The hypothalamus, anterior pituitary and ovaries all function to control female hormone levels. Like other hormones, female hormones are regulated by feedback mechanisms. hypothalamus Gn. RH anterior pituitary follicle FSH LH corpus luteum progesterone oocyte estrogen
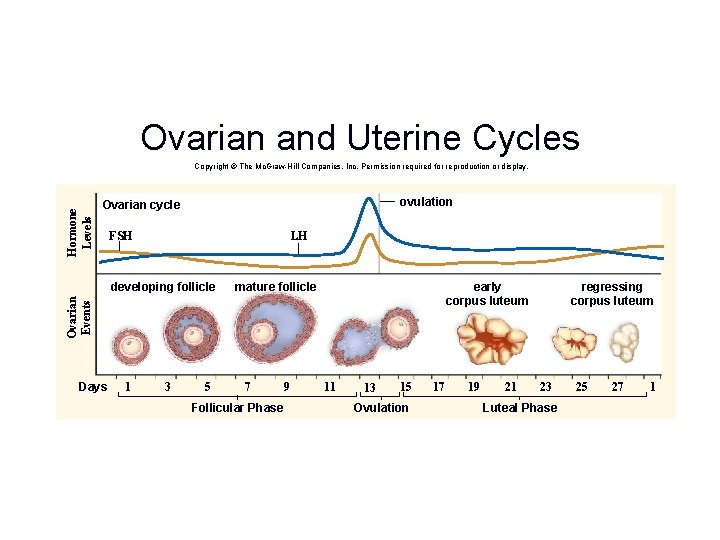
Ovarian and Uterine Cycles Hormone Levels Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. ovulation Ovarian cycle FSH LH mature follicle early corpus luteum Ovarian Events developing follicle Days 1 3 5 7 Follicular Phase 9 11 13 15 Ovulation 17 19 21 regressing corpus luteum 23 Luteal Phase 25 27 1
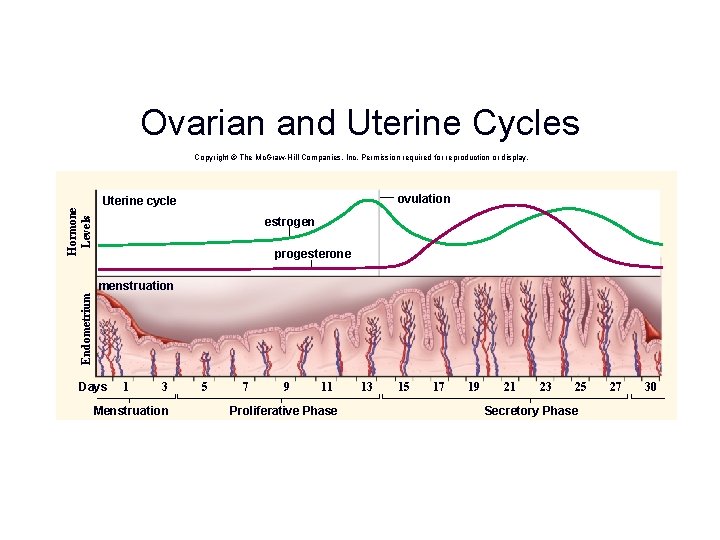
Ovarian and Uterine Cycles Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. ovulation Hormone Levels Uterine cycle estrogen progesterone Endometrium menstruation Days 1 3 Menstruation 5 7 9 11 Proliferative Phase 13 15 17 19 21 23 25 Secretory Phase 27 30
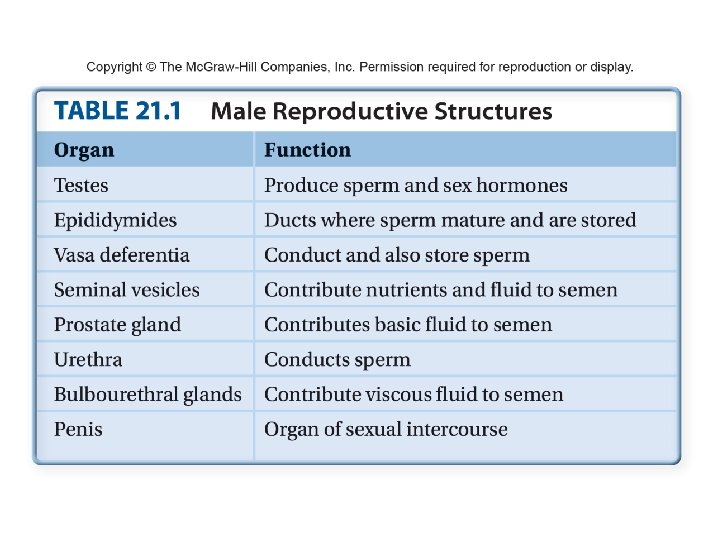
Male Reproductive System • Organisms that utilize sexual reproduction must produce gametes. – Haploid sex cells united in fertilization • This system is different in males and females, unlike other organ systems.
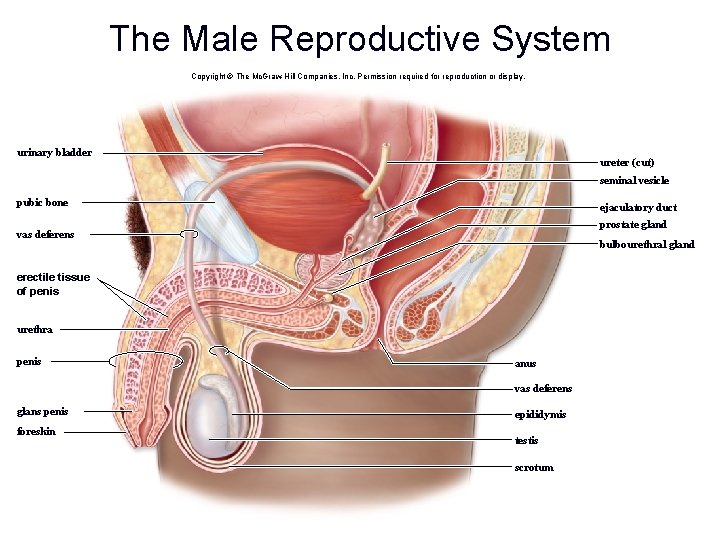
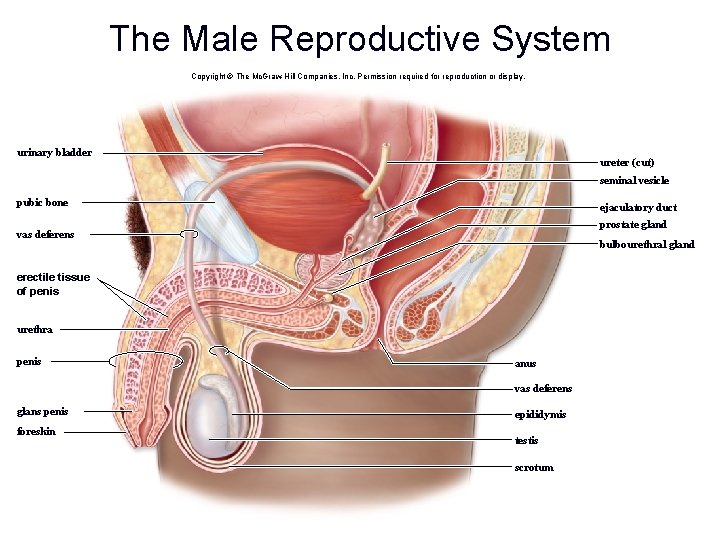
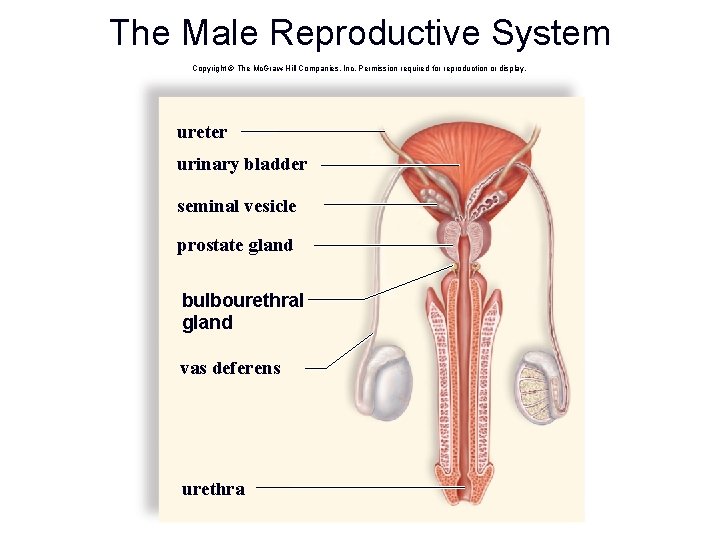
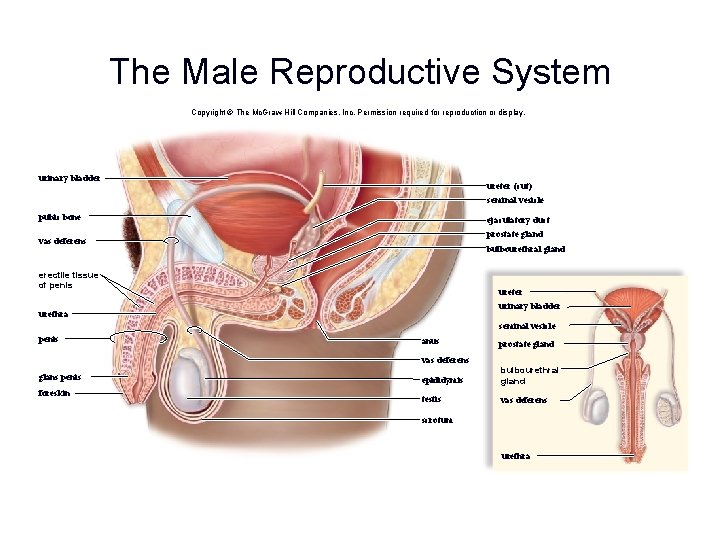
The Male Reproductive System Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. urinary bladder ureter (cut) seminal vesicle pubic bone ejaculatory duct prostate gland vas deferens bulbourethral gland erectile tissue of penis urethra penis anus vas deferens glans penis foreskin epididymis testis scrotum
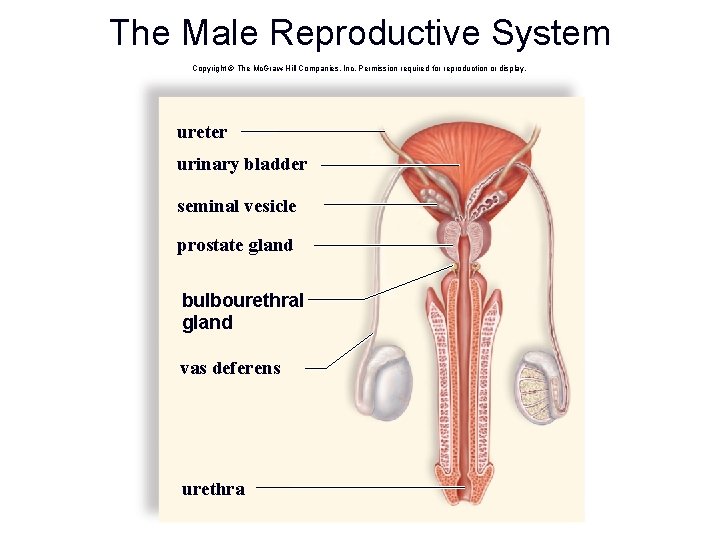
The Male Reproductive System Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. ureter urinary bladder seminal vesicle prostate gland bulbourethral gland vas deferens urethra
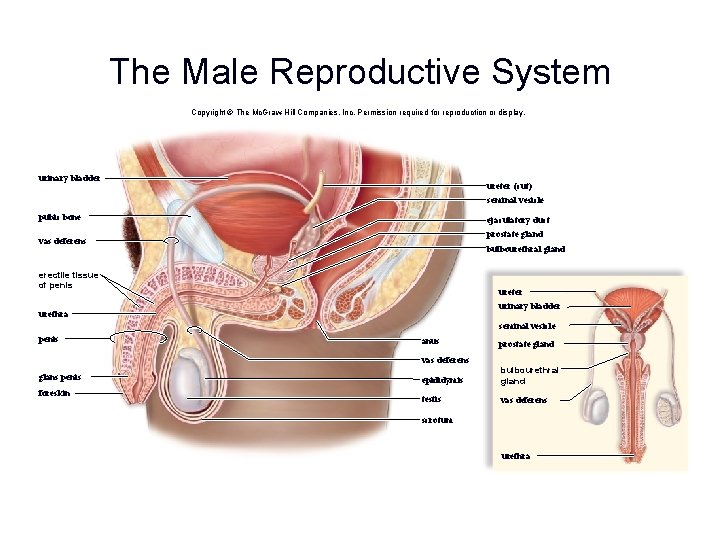
The Male Reproductive System Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. urinary bladder ureter (cut) seminal vesicle pubic bone ejaculatory duct prostate gland vas deferens bulbourethral gland erectile tissue of penis ureter urinary bladder urethra seminal vesicle penis anus prostate gland vas deferens glans penis foreskin epididymis bulbourethral gland testis vas deferens scrotum urethra
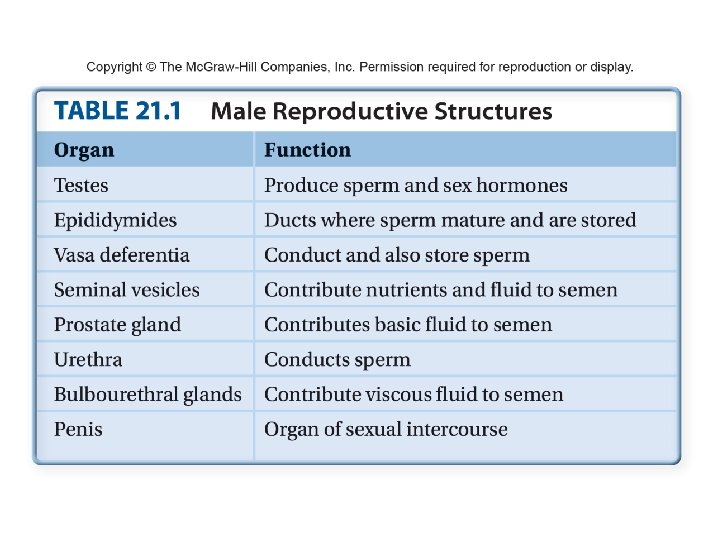
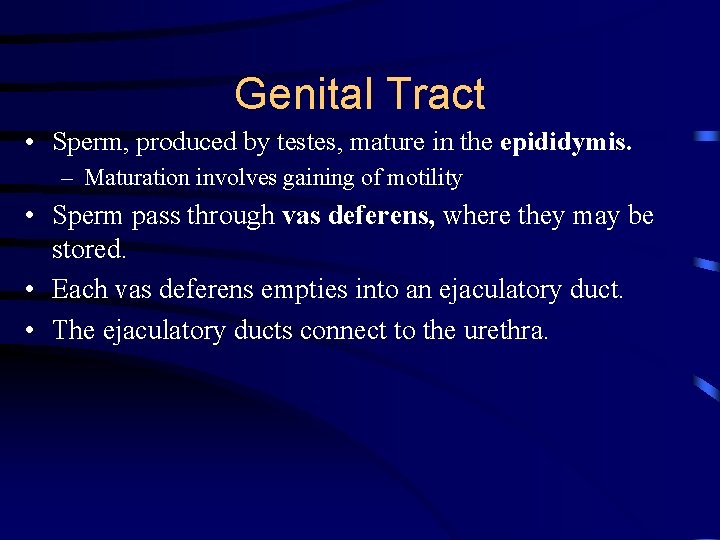
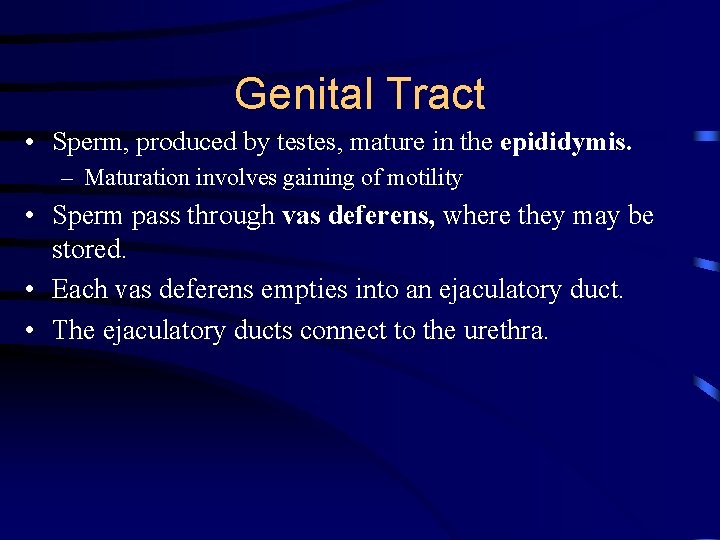
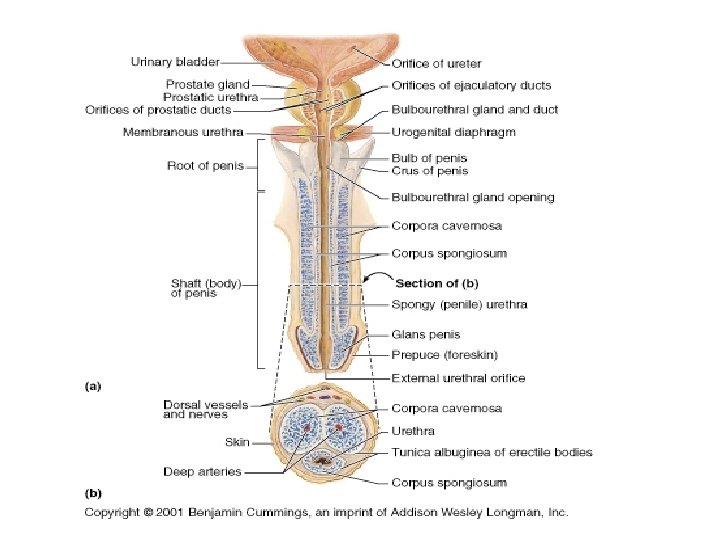
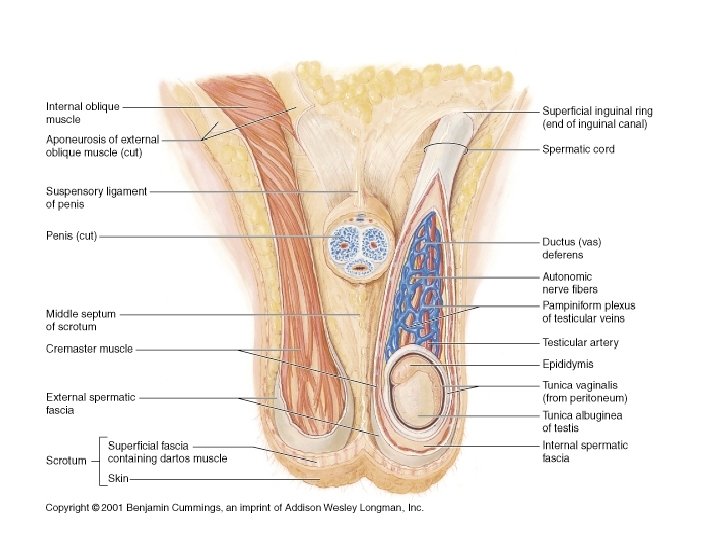
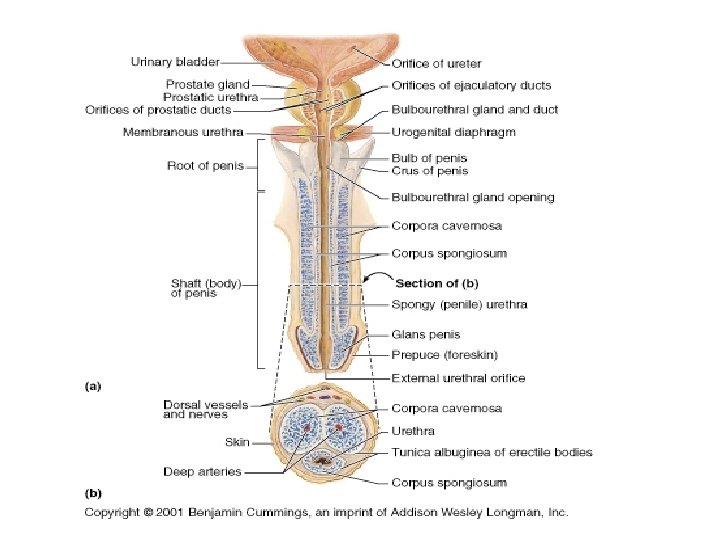
Genital Tract • Sperm, produced by testes, mature in the epididymis. – Maturation involves gaining of motility • Sperm pass through vas deferens, where they may be stored. • Each vas deferens empties into an ejaculatory duct. • The ejaculatory ducts connect to the urethra.
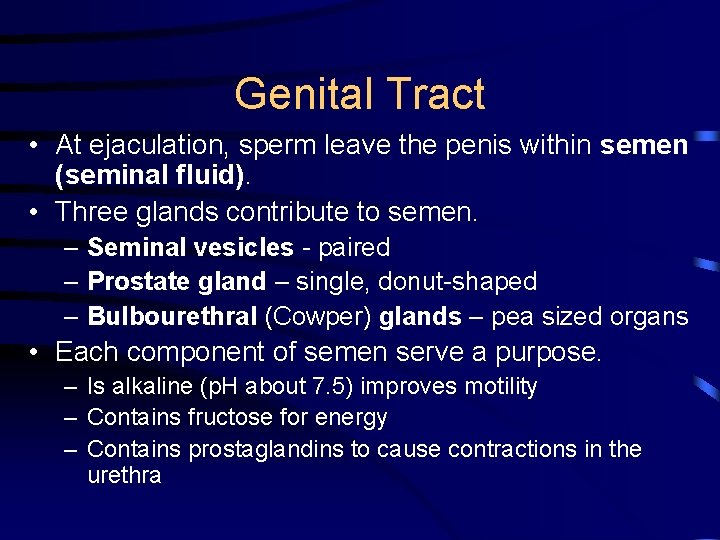
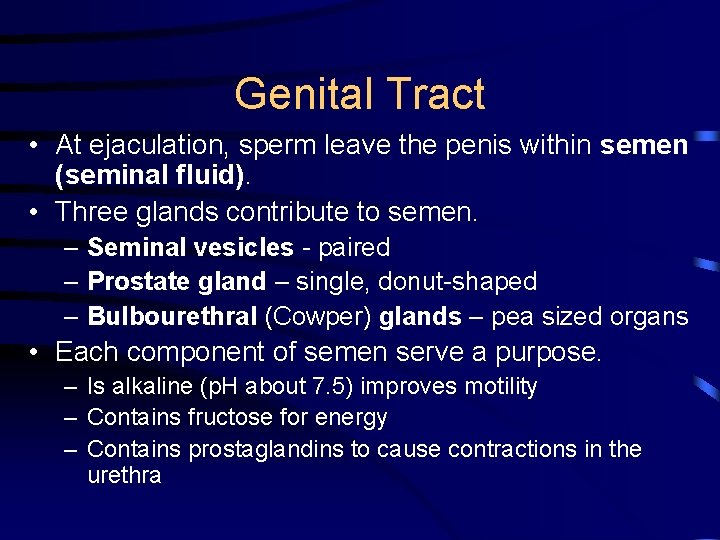
Genital Tract • At ejaculation, sperm leave the penis within semen (seminal fluid). • Three glands contribute to semen. – Seminal vesicles - paired – Prostate gland – single, donut-shaped – Bulbourethral (Cowper) glands – pea sized organs • Each component of semen serve a purpose. – Is alkaline (p. H about 7. 5) improves motility – Contains fructose for energy – Contains prostaglandins to cause contractions in the urethra
Genital Tract • The penis is the male organ of sexual intercourse. – The penis has a long shaft and an enlarged tip called the glans penis. – At birth, the glans penis is covered by a layer of skin called the foreskin. • Circumcision, the surgical removal of the foreskin
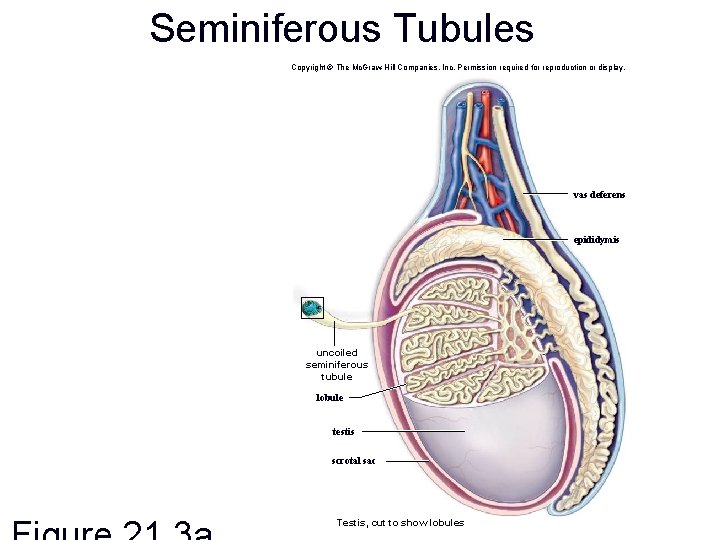
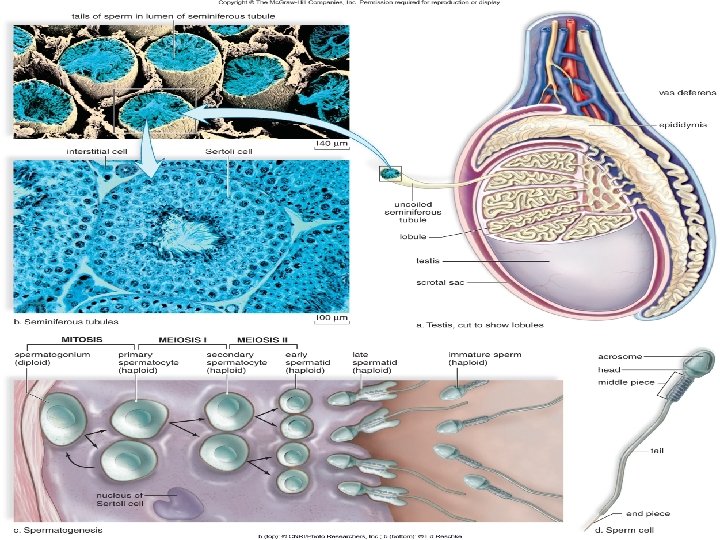
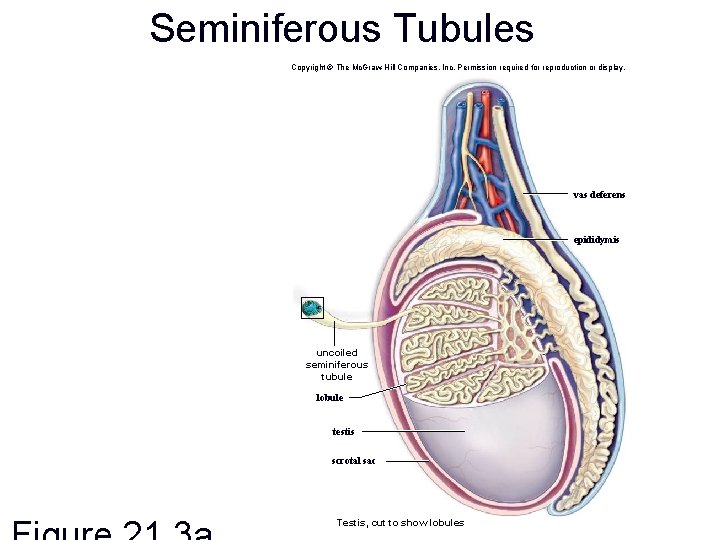
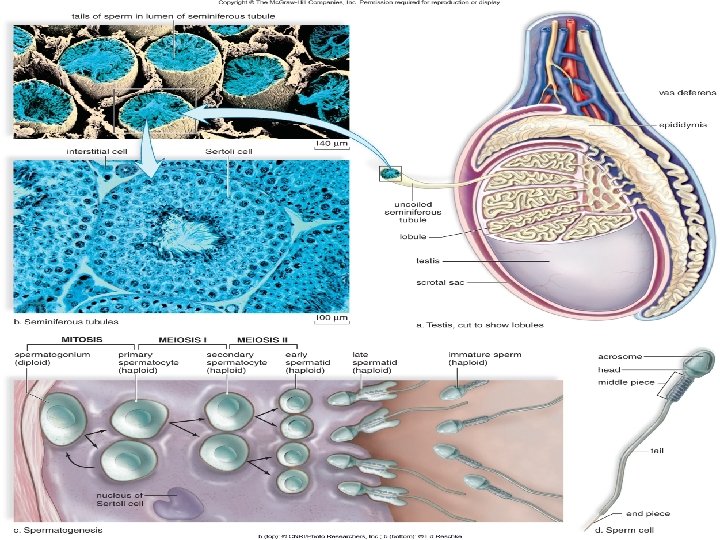
Seminiferous Tubules Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. vas deferens epididymis uncoiled seminiferous tubule lobule testis scrotal sac Testis, cut to show lobules
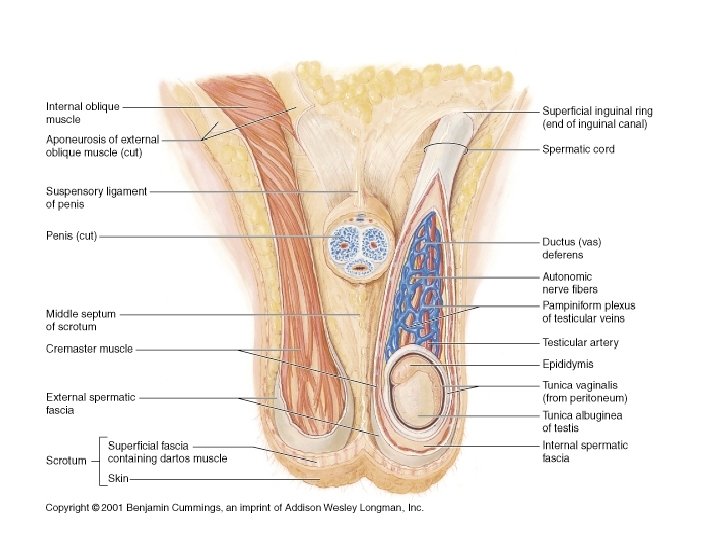
Male Gonads, the Testes • The testes – Produce sperm and male sex hormones – Located outside of the abdominal body cavity • Internal body temperature is too high for sperm production • Scrotum helps regulate temperature of the testes – Can move the testes further or closer to the body
Seminiferous Tubules • The testes are composed of compartments called lobules, each of which contains one to three tightly coiled seminiferous tubules. • Altogether, these tubules have a combined length of 250 meters. • Spermatogenesis occurs in the seminiferous tubules as viewed microscopically.
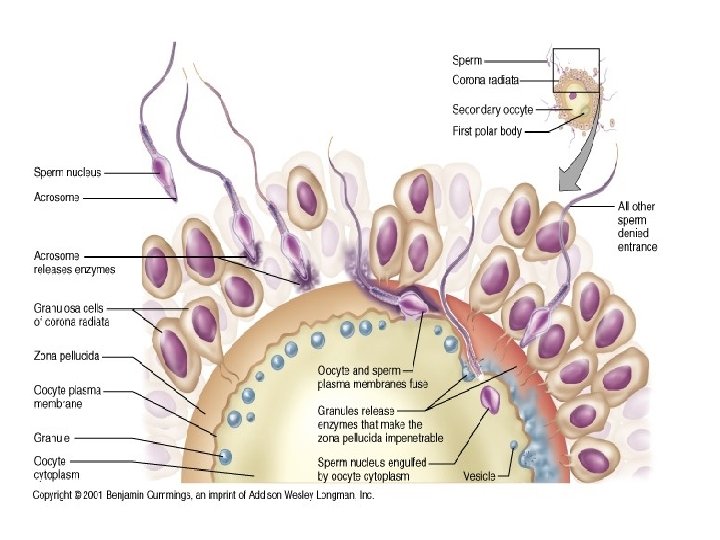
Seminiferous Tubules • Spermatogonia are the first cells produced by spermatogenesis. – They become primary spermatocytes that undergo meiosis I to produce secondary spermatocytes. – Secondary spermatocytes undergo meiosis II to produce four spermatids. – Spermatids differentiate into sperm. – Sertoli cells support, nourish, and regulate spermatogenic cells.
Interstitial Cells • Interstitial cells secrete the male sex hormones, the androgens. • These cells lie between the seminiferous tubules. • The most important androgen is testosterone.
• Erections and Orgasm in Males Spongy, erectile tissue containing distensible blood spaces extends through the penis shaft. – Sexual excitement increases blood flow to the penis causing an erection. – Sperm enters from the vasa deferentia, and glands contribute secretions to the semen. – Semen is ejaculated. – Ejaculation is followed by a refractory period. – Over 400 million sperm cells may be ejaculated.
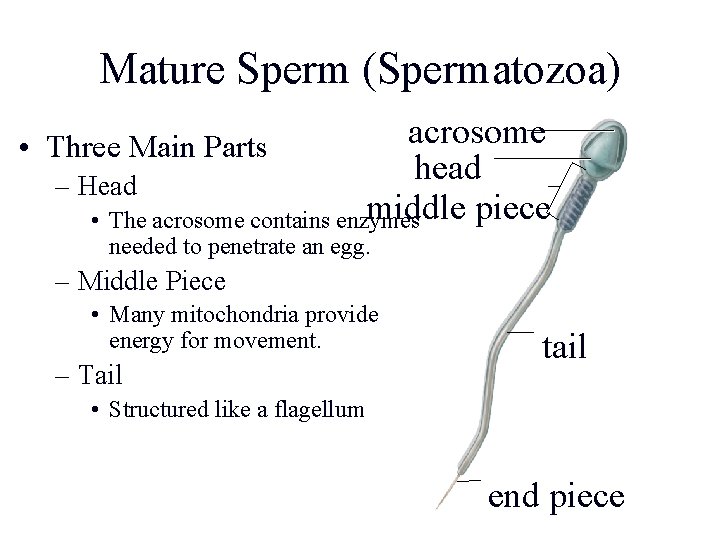
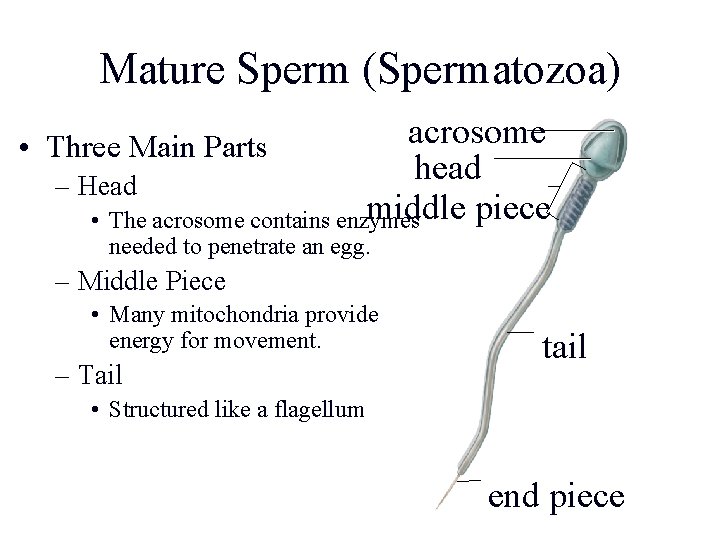
Mature Sperm (Spermatozoa) acrosome • Three Main Parts head – Head middle piece • The acrosome contains enzymes needed to penetrate an egg. – Middle Piece • Many mitochondria provide energy for movement. – Tail tail • Structured like a flagellum end piece
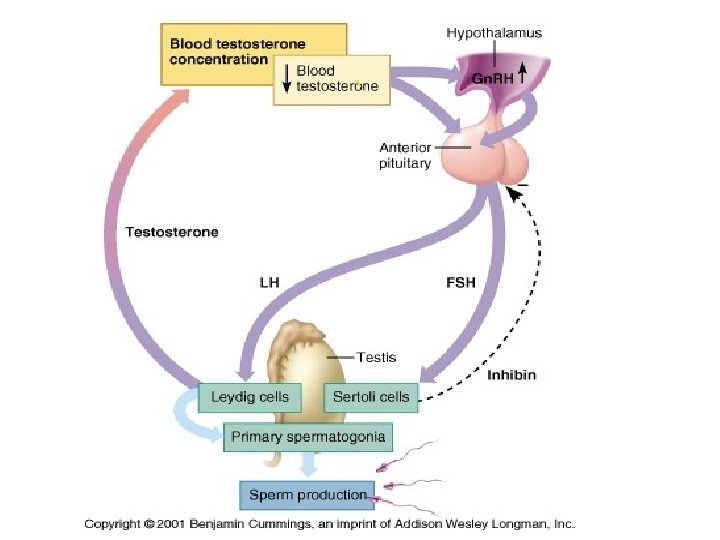
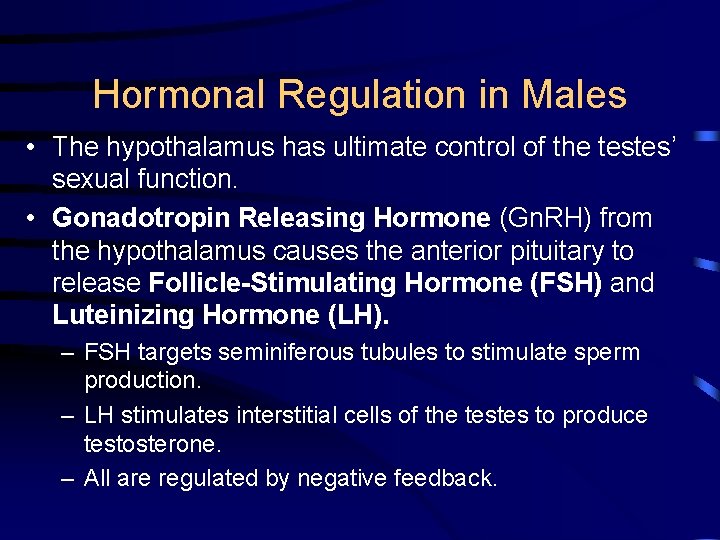
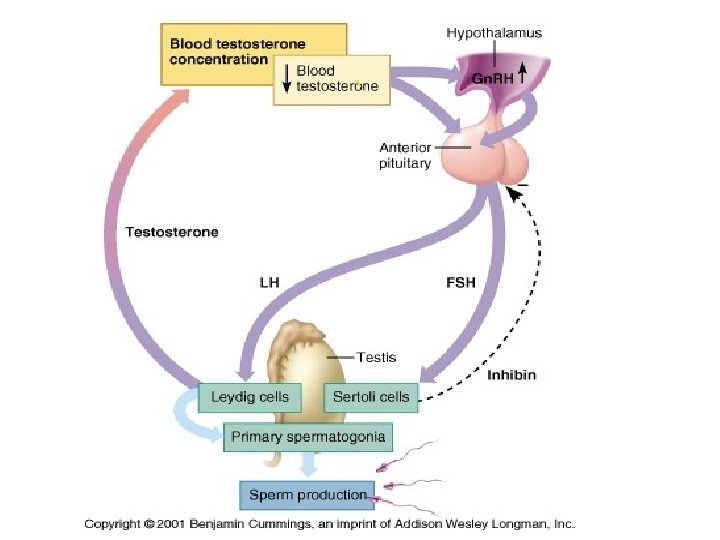
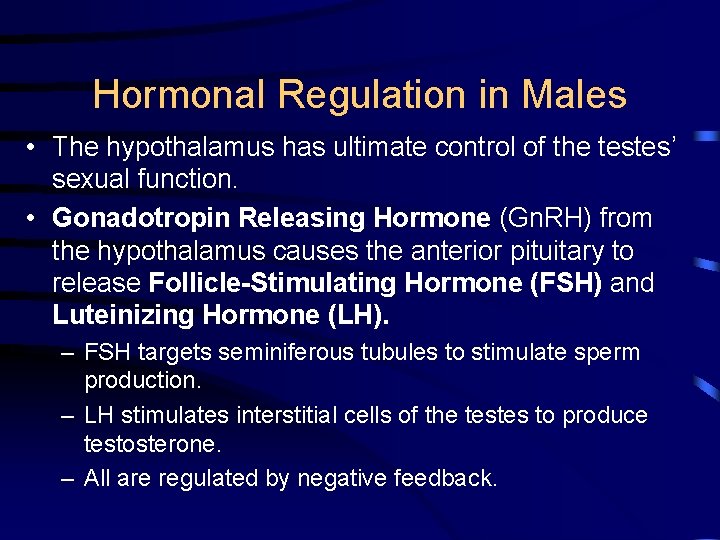
Hormonal Regulation in Males • The hypothalamus has ultimate control of the testes’ sexual function. • Gonadotropin Releasing Hormone (Gn. RH) from the hypothalamus causes the anterior pituitary to release Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH). – FSH targets seminiferous tubules to stimulate sperm production. – LH stimulates interstitial cells of the testes to produce testosterone. – All are regulated by negative feedback.
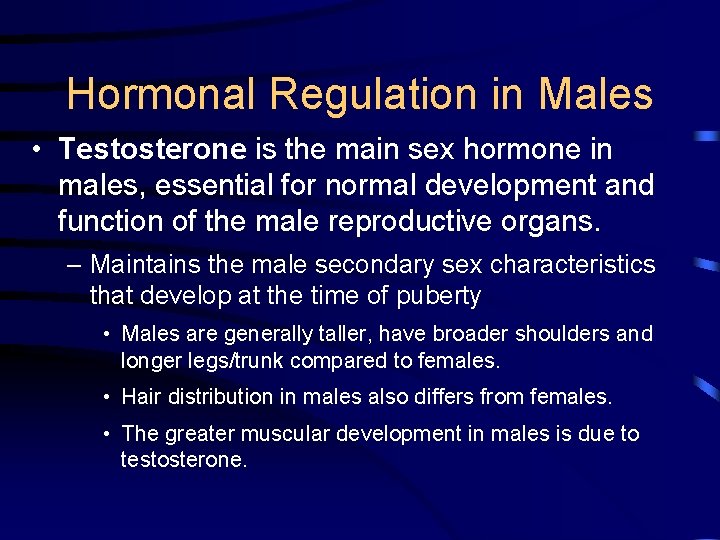
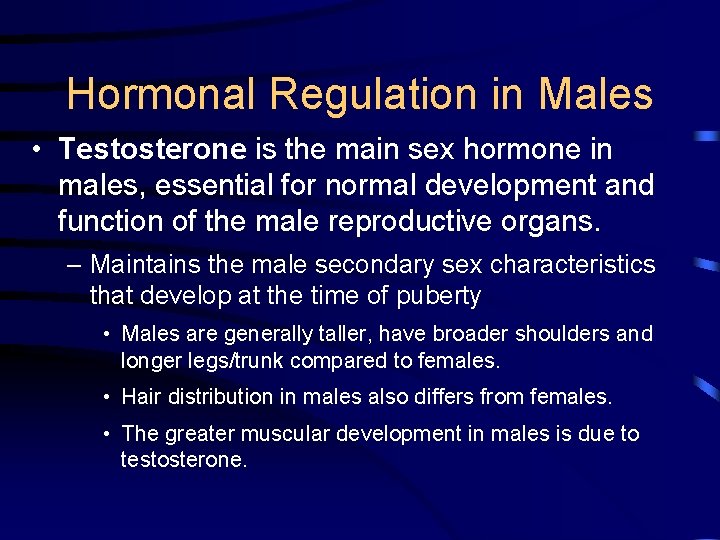
Hormonal Regulation in Males • Testosterone is the main sex hormone in males, essential for normal development and function of the male reproductive organs. – Maintains the male secondary sex characteristics that develop at the time of puberty • Males are generally taller, have broader shoulders and longer legs/trunk compared to females. • Hair distribution in males also differs from females. • The greater muscular development in males is due to testosterone.