Physiology of the Female Reproductive System Dr Matinnia


- Slides: 21
Physiology of the Female Reproductive System Dr. Matinnia
Physiological Stages • • • Neonatal period: birth---4 weeks Childhood: 4 weeks----12 years Puberty: 12 years---18 years Sexual maturation: 18 year---50 year Perimenopause: decline of ovarian function (40 years)----1 year postmenopause • Postmenopause:
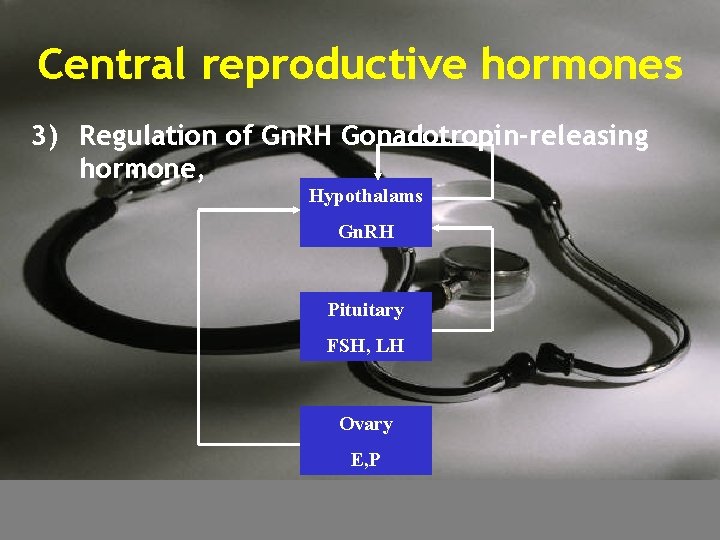
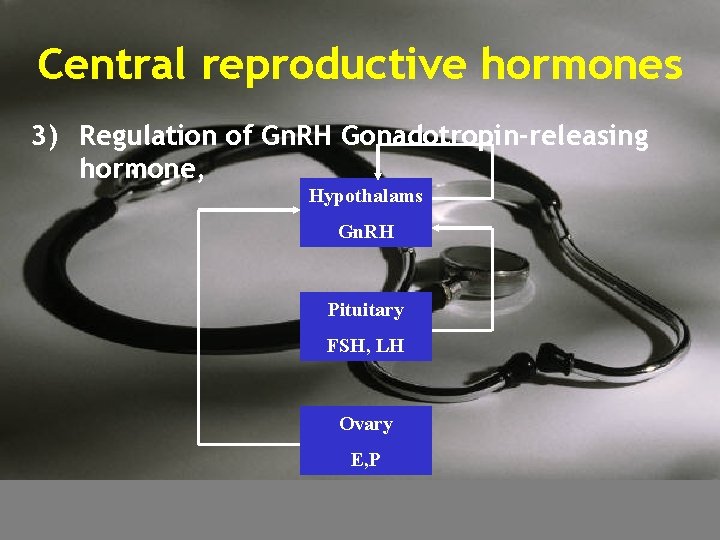
Central reproductive hormones 3) Regulation of Gn. RH Gonadotropin-releasing hormone, Hypothalams Gn. RH Pituitary FSH, LH Ovary E, P
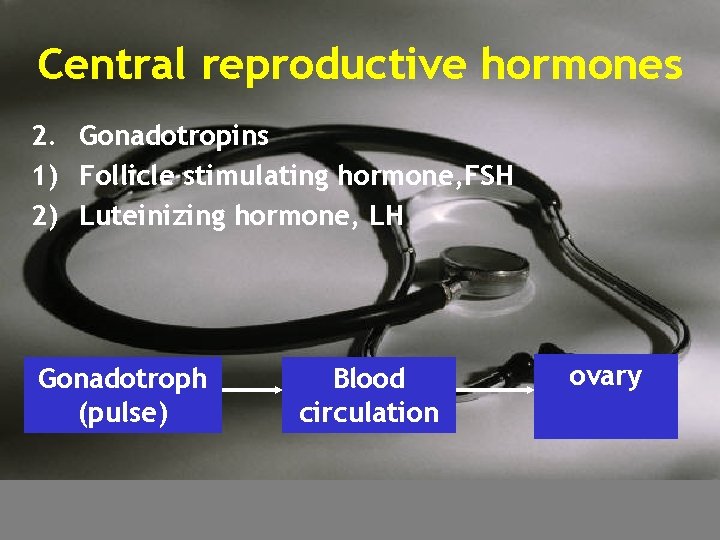
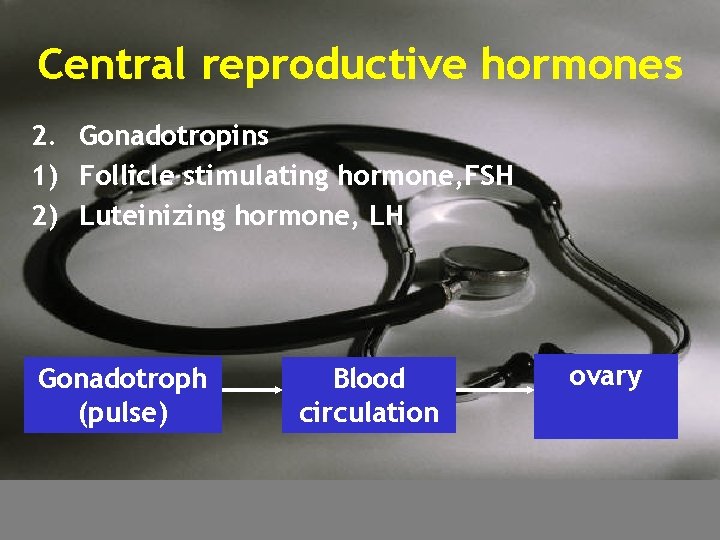
Central reproductive hormones 2. Gonadotropins 1) Follicle stimulating hormone, FSH 2) Luteinizing hormone, LH Gonadotroph (pulse) Blood circulation ovary
The Ovarian cycle • Function of ovary 1. Reproduction development and maturation of follicle; ovulation 2. Endocrine estrogens, progesterone, testosterone
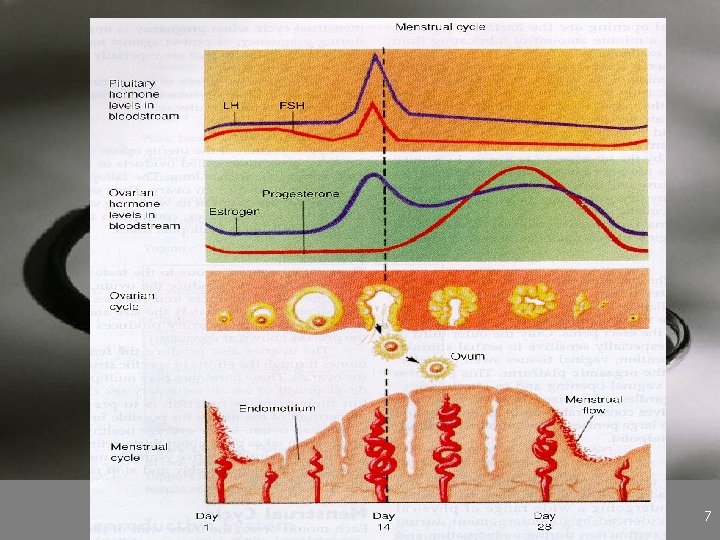
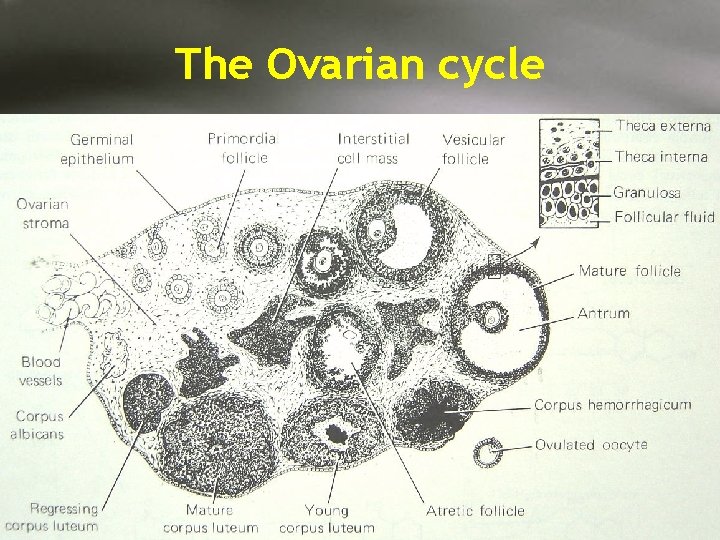
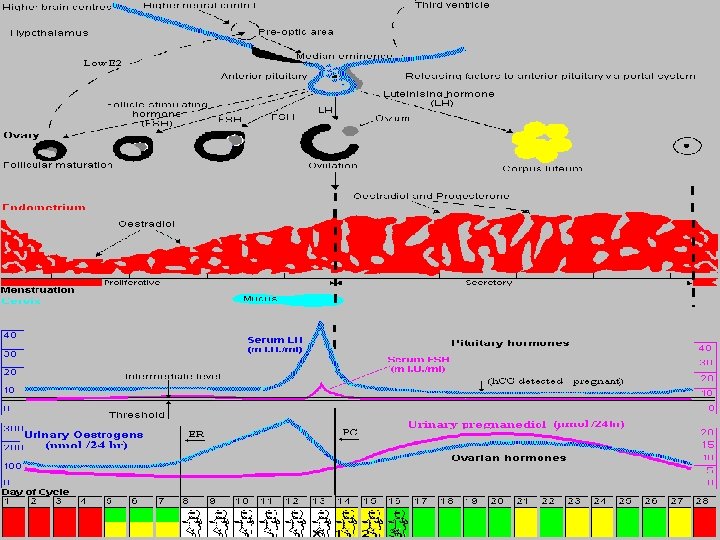
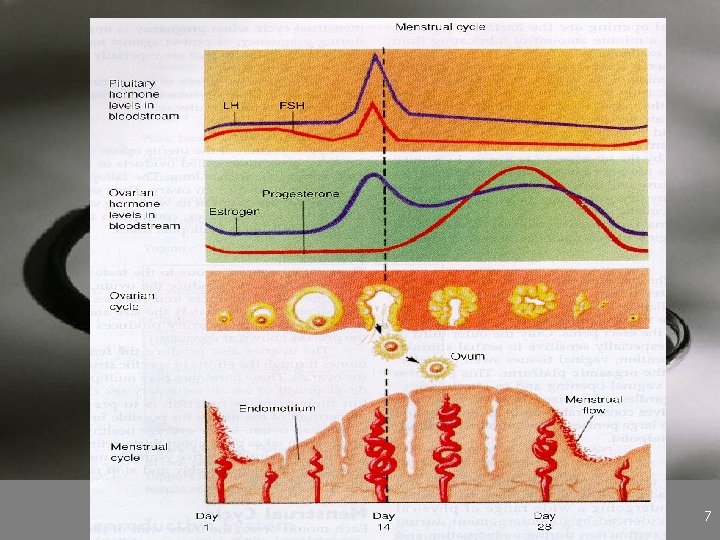
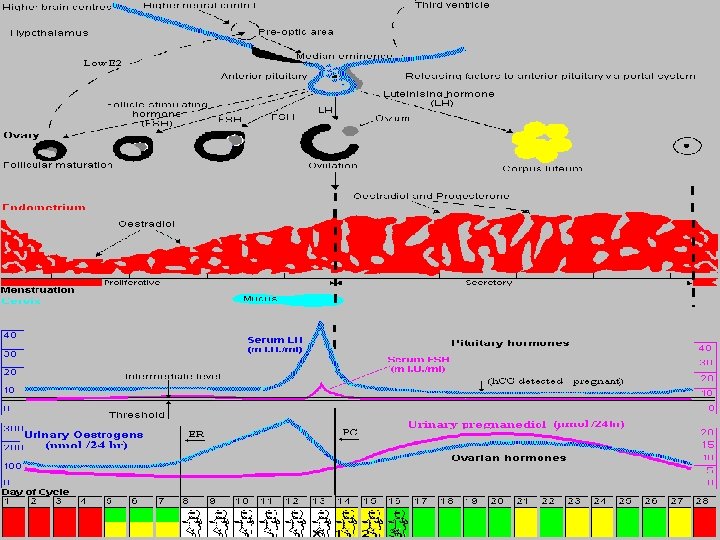
The Ovarian cycle • Cyclic changes of ovary The development and maturation of follicle 1. Follicular phase: day 1 to follicle mature (14 days) 2. Ovulation Phase 3. Luteal Phase
UNIT 3: FEMALE REPRODUCTIVE SYSTEM 7
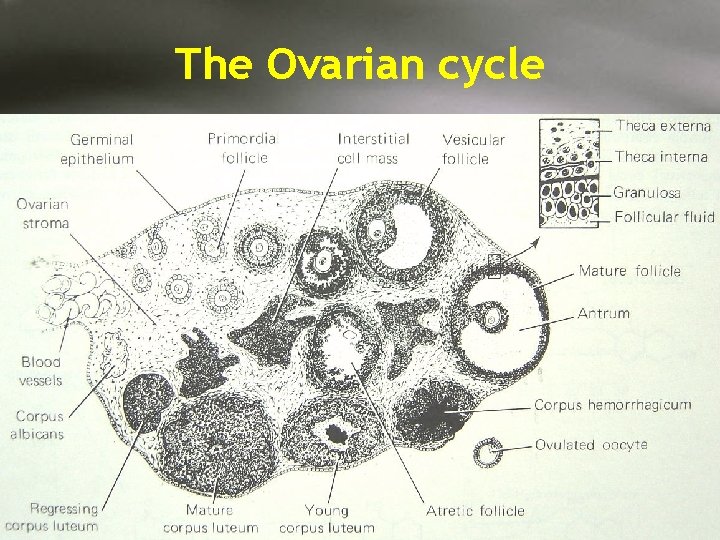
The Ovarian cycle
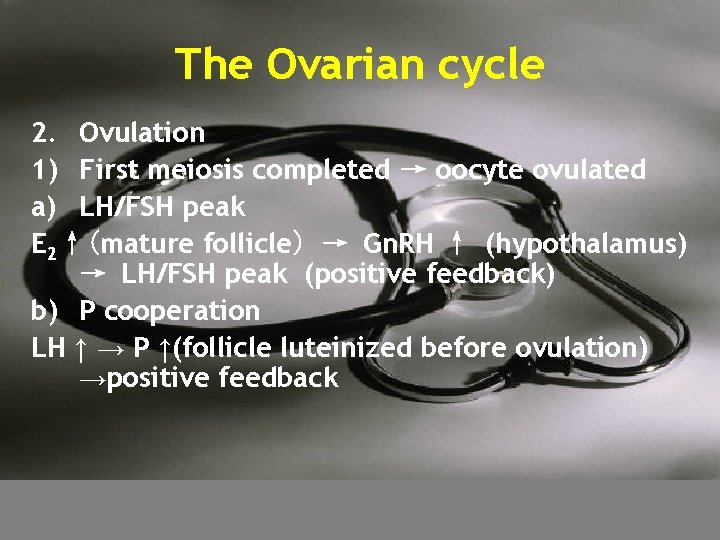
The Ovarian cycle 2. Ovulation 1) First meiosis completed → oocyte ovulated a) LH/FSH peak E 2↑(mature follicle) → Gn. RH ↑ (hypothalamus) → LH/FSH peak (positive feedback) b) P cooperation LH ↑ → P ↑(follicle luteinized before ovulation) →positive feedback
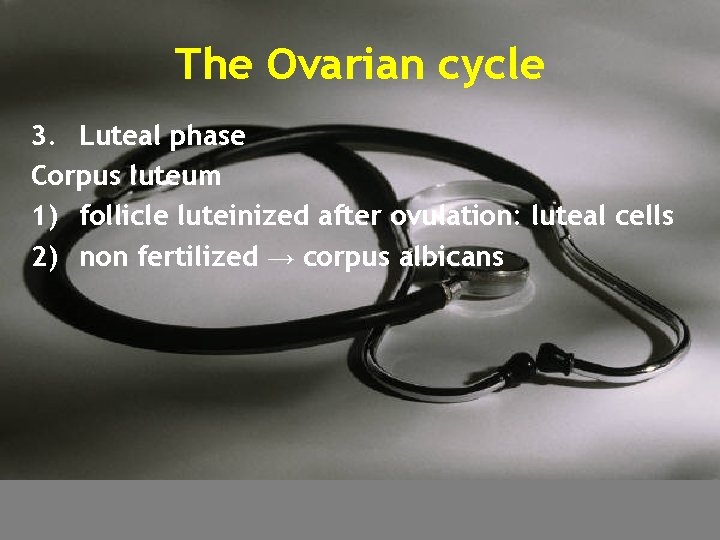
The Ovarian cycle 3. Luteal phase Corpus luteum 1) follicle luteinized after ovulation: luteal cells 2) non fertilized → corpus albicans

The Ovarian cycle • sex hormones secreted by ovary 1. Composition Estrogen, progesterone, testosterone
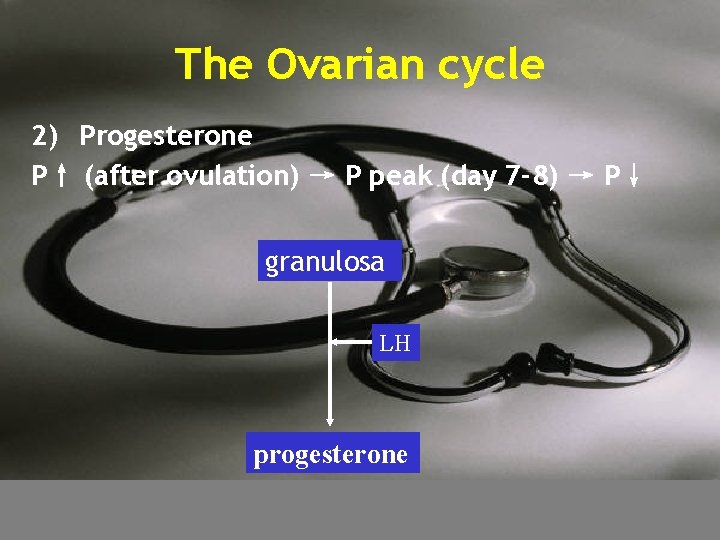
The Ovarian cycle 2) Progesterone P↑ (after ovulation) → P peak (day 7 -8) → P↓ granulosa LH progesterone
Ovarian responses
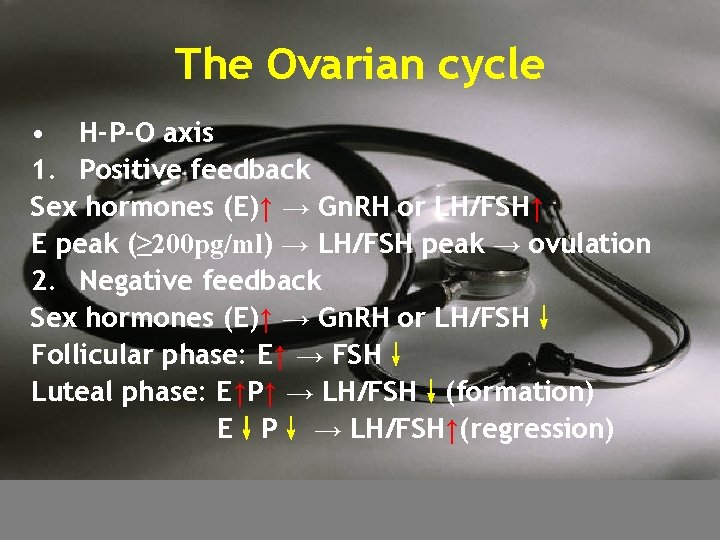
The Ovarian cycle • H-P-O axis 1. Positive feedback Sex hormones (E)↑ → Gn. RH or LH/FSH↑ E peak (≥ 200 pg/ml) → LH/FSH peak → ovulation 2. Negative feedback Sex hormones (E)↑ → Gn. RH or LH/FSH↓ Follicular phase: E↑ → FSH↓ Luteal phase: E↑P↑ → LH/FSH↓(formation) E↓P↓ → LH/FSH↑(regression)
The endometral cycle • Proliferative phase 1. E↑(mitogen)→ stroma thickens and glands become elongated → proliferative endometrium 2. Duration: 2 weeks 3. Thickness: 0. 5 mm → 5 mm
The endometral cycle • Secretory phase 1. P↑(differentiation) → secretory endometrium 2. Features stroma becomes loose and edematous blood vessels entering the endometrium become thickened and twisted glands become contain secretory material within the lumina 3. Duration: 2 weeks 4. Thickness: 5 -6 mm
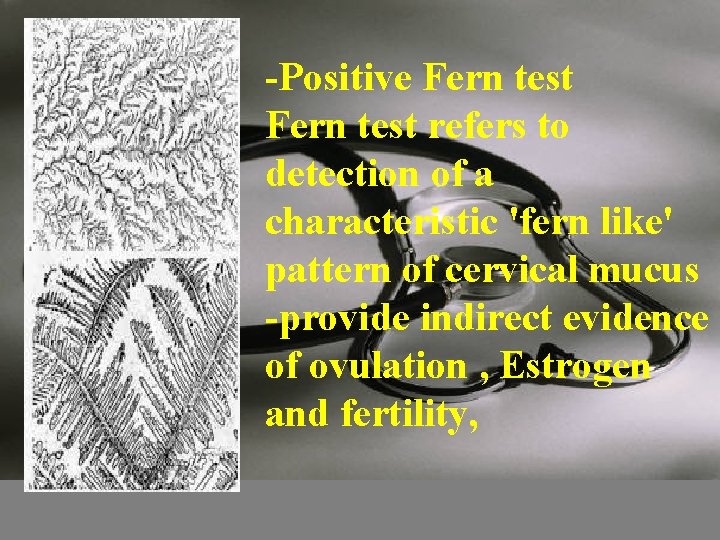
Change of Other genital organs • Cervix endocervical glands (E↑)→ mucus(thin, clear, watery) → maximal (ovulation) endocervical glands (P↑)→ mucus(thick, opaque, tenacious) • Vaginal mucosa (E↑)→ thickening and secretory changes Vaginal mucosa (P↑) → secrete↓
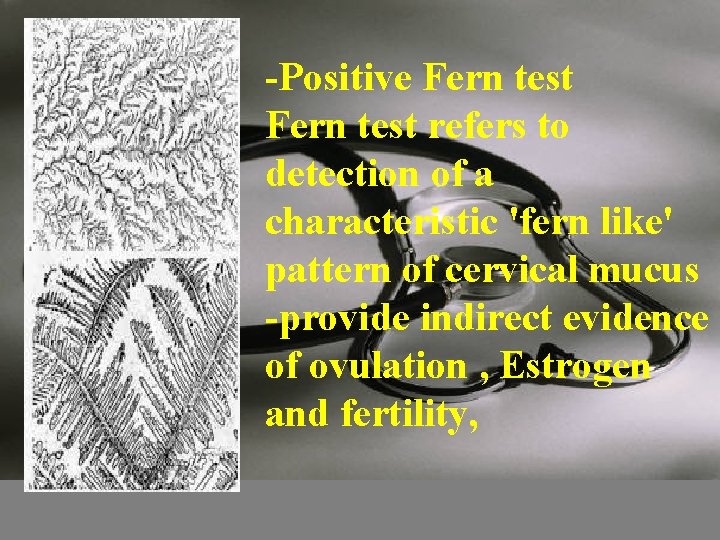
-Positive Fern test refers to detection of a characteristic 'fern like' pattern of cervical mucus -provide indirect evidence of ovulation , Estrogen and fertility,
Menstruation • • 1. 2. 3. 4. Menstruation cyclic endometrium sheds and bleeds due to cyclic ovulation Mense Endometrium is sloughed (progesterone withdrawal) Nonclotting menstrual blood mainly comes from artery (75%) Interval: 24 -35 days (28 days). duration: 2 -8 days. the first day of menstrual bleeding is consideredy by day 1 Shedding: 30 -70 ml
DYSMENORRHEA • Painful menstrual cramps • Painful menses without evidence of a physical abnormality • Believed to be normal body response to uterine contractions • Other symptoms : • Nausea, vomiting, gastrointestinal disturbances, and fainting • Prostaglandins cause forceful, frequent uterine contractions called cramps • Fibroids, polyps, IUD, PID, or endometriosis UNIT 3: FEMALE REPRODUCTIVE SYSTEM 20

END