Physiology of Muscle Tendon Ligament Healing Jason R



- Slides: 45
Physiology of Muscle, Tendon & Ligament Healing Jason R. Miller, DPM, AACFAS, FAPWCA Dept. of Surgery
Purpose of Lecture • Tendon repair and tenoplasty are important aspects of podiatric surgery. • Ligament ruptures are common and repairs are often needed. • Knowledge of tendon and ligament healing allow the surgeon to make appropriate decisions concerning procedures, materials, post-op care and possible complications. • Understand the basic biology of nerves and their response to injury.
Definitions • Tendon Transfer: Detachment of a tendon of a functioning muscle at its insertion • Tendon Transposition: Rerouting without detachment to assist in other functions • Muscle-Tendon Transplantation: Detachment of a muscle tendon at both the origin and insertion to a new location with the NV structures intact. • Tendon Suspension: Tendon supports a structure
Tendon Anatomy • Very strong, stronger than muscle for size • As strong as bone with a failing point similar to steel! • Can transmit force through ability to glide • Passive component of the musculotendinous unit in light of their incredible influence on the foot.
Tendon Histology • 30% Collagen, 2% Elastin, 68% Water • Bulk is supplied by reticulin • 70% Type I collagen
Ligament Histology • 33% Composition: 90% Type I collagen, Elastin, Glycosaminoglycans. 67% Water
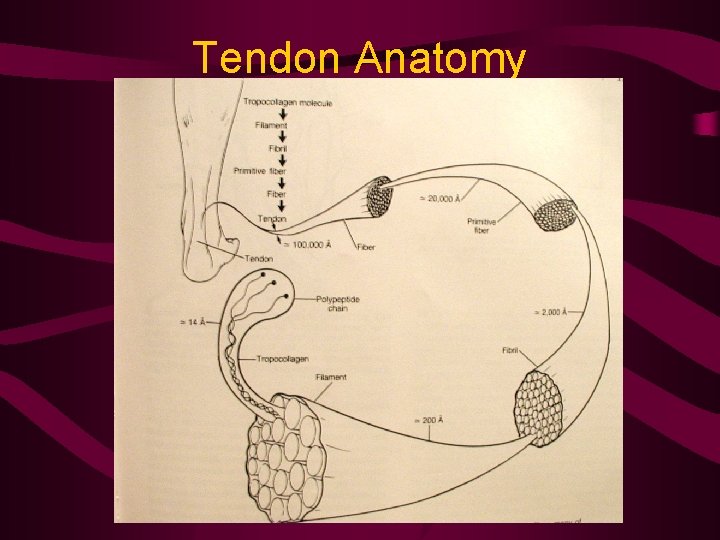
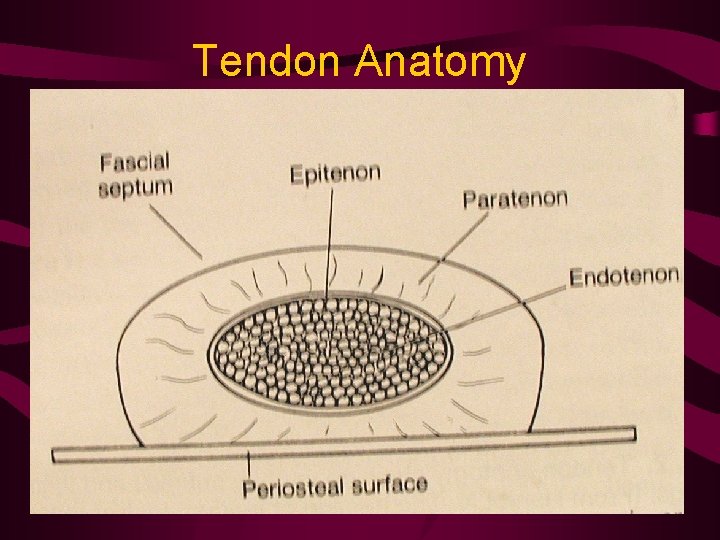
Anatomy of the Tendon • Tropocollagen – the most basic molecular unit of tendon • 3 Coverings: – Endotenon- fascicles are surrounded by this areolar CT, contains BV, L, N, and FB. – Epitenon- Fascicles bound together by this 1 -2 cell fibroblastic & synovial layer – Paratenon- loose areolar layer continuous with the epitenon & perimysium, straight.
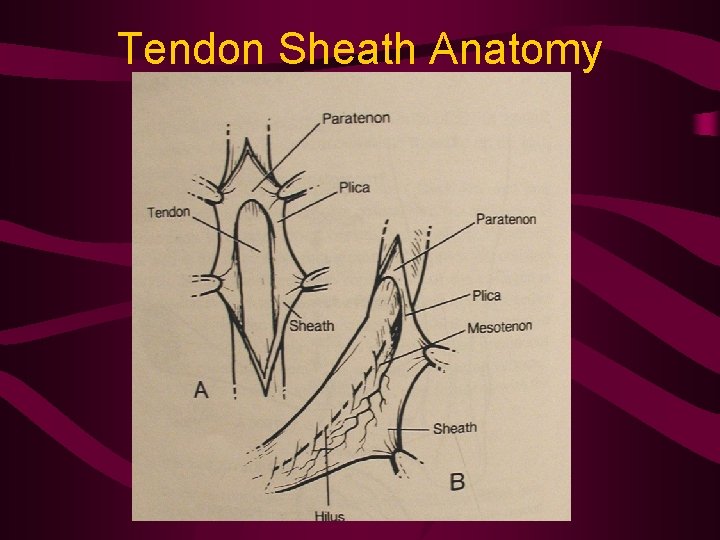
Anatomy of the Tendon • Tendon/Synovial Sheath: acts like a pulley when tendon has an angled course. • Peritenon- term applied collectively to all CT structures associated with a tendon incl para-, meso-, epi-, and endotenon.
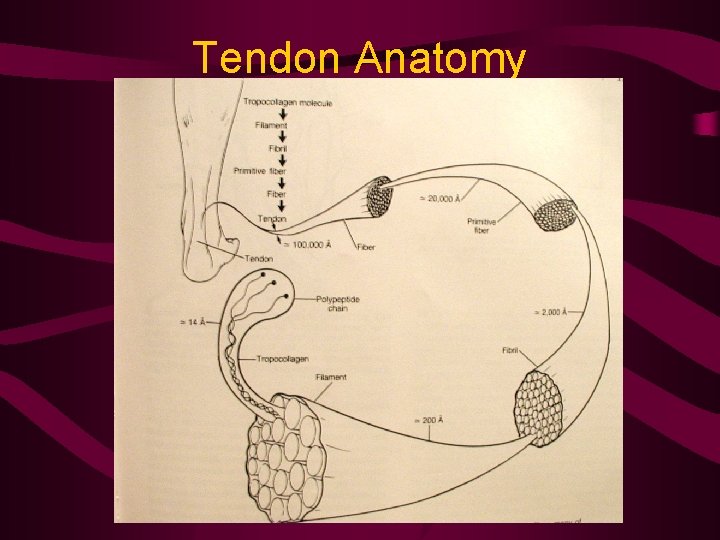
Tendon Anatomy
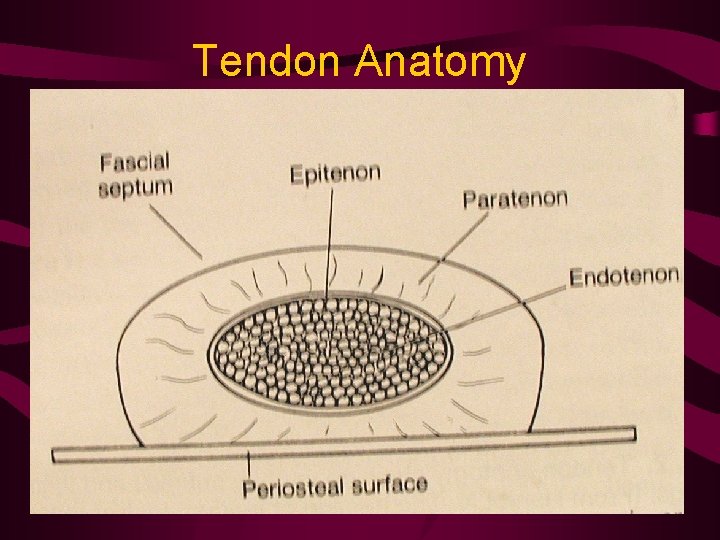
Tendon Anatomy
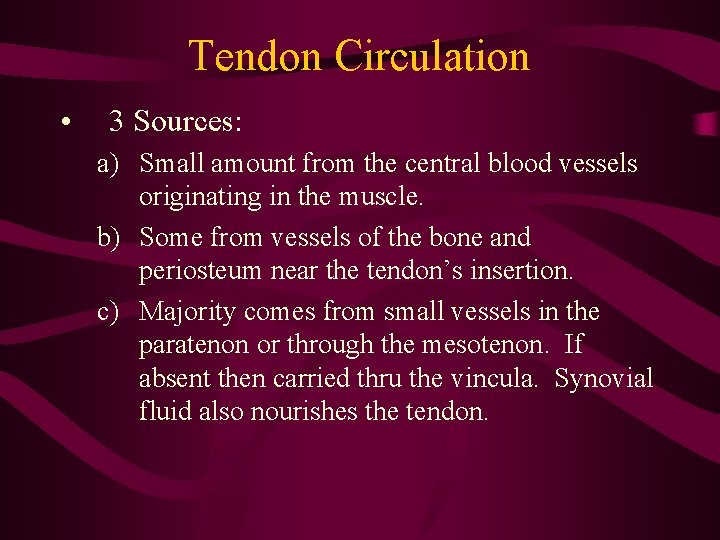
Tendon Circulation • 3 Sources: a) Small amount from the central blood vessels originating in the muscle. b) Some from vessels of the bone and periosteum near the tendon’s insertion. c) Majority comes from small vessels in the paratenon or through the mesotenon. If absent then carried thru the vincula. Synovial fluid also nourishes the tendon.
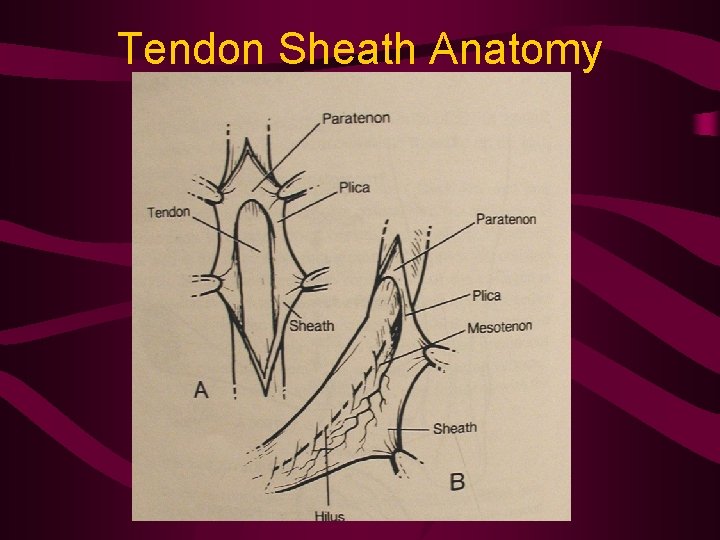
Tendon Sheath Anatomy
Tendon Innervation • Afferent supply only • Source in musculotendinous junction and external local nerves. • Golgi tendon organs: monitor increases in tension rather than length.
Tendon Attachment to Bone • Attach at 90° angles to bone in 4 layers: 1. 2. 3. 4. Tendon collagen fibers Fibrocartilage Bone Sharpey’s fibers – originate in bone and end in perisoteum.

Tendon Healing • 4 Stages – Stage 1: Severed ends joined by fibroblastic splint. At the end of this stage, the repair site is in its weakest state with serous material & granulation tissue (Zone of degeneration) 1 week
Tendon Healing • Stage 2: Increase in paratenon vascularity and collagen proliferation. 2 weeks • Stage 3: Collagen forms longitudinally, increases strength. Controlled passive motion is beneficial to decrease fibrous adhesions. 3 weeks
Tendon Healing • Stage 4: Fibers align, increasing strength further. Swelling and vascularity reduce. AROM can be performed. 4 weeks

Tendon Healing • Healing can be augmented by: – Early mobilization – US – Elec. Stim. – Growth factors
Tendon Lengthening • Muscle strength will be reduced by one grade (Polio Foundation) once healed. • Transfers will equally degrade muscle strength.
Tendon Suture • Surgilon®: Non absorbable, non reactive. Increased strength during end of Stage 1. • Stainless steel: Strongest, least reactive. Should be removed, can tear thru tendon. • Silk: Old school surgeons. • Tevdek®/Ticron®: Nonabsorbable braided polyester, resists gapping at 3 weeks better than nylon or polypropylene.
Tendon Suture • Vicryl®/Dexon®: Absorbable polygalactic acid/polyglycolic acid strong enough to keep repair intact. • Ethibond®: Strong, Non absorbable braided polyester. Good choice.
Methods of Tendon Repair • Bunnell end to end: Strong, but restricts tissue. • Double right angle: Quick, for small tendons. • Lateral trap: Tightly pulls edges of tendon together w/o damaging central microcirculation
Methods of Tendon Repair • Chicago: Simple X stitch • Robertson: Best method of anastomosis for tendons of differing sizes. • Interlace: Method for attaching small to large tendons. • Herringbone stitch & insertion: Method for grafting one tendon into center of another.
Securing Tendon To Bone • • • Trephine plug 3 Hole Suture Buttress & button anchor Tunnel w/ sling Screw & washer (cleated polyacetyl, Ti) STATAC, Mitek, PEBA
Objectives of Tendon Transfer • To improve motor function where weakness or imbalances exist to prevent deformity. • To eliminate deforming forces • To provide active motor power • To provide better stability • To eliminate or reduce need for bracing • To improve cosmesis
Principles of Transfer • • Do not create new imbalances Understand anatomy & physiology Correct fixed/structural deformities 1 st Perform at appropriate age Select suitable tendon Provide a mechanically efficient line of pull Perform stabilizing procedures 1 st
Principles of Transfer • • • Preserve the gliding mechanism Use atraumatic technique Preserve neurovascular supply Provide adequate muscle-tendon tension Use secure fixation techniques Appropriate post-op management
Ligamentous Healing • Treated similarly to tendon, blood supply similar without muscular blood supply • Healing stages similar • Primary repair of initial ruptures is preferred • Suture choices same as tendon.
Nerve Healing & Repair • Peripheral Nerves – Conducting axons – Insulating Schwann cells – Connective tissue matrix
Nerve Healing & Repair • Nerve fibers – Ensheathed by Schwann cells – Myelinated fibers are individually encased – Non-myelinated fibers are encased in groups • Basal lamina layer – Envelops Schwann cells – Critical role in supporting axonal regeneration by serving as a “highway”
Nerve Healing & Repair • Endoneurium – Myelinated & unmyelinated are embedded with this CT • Perineurium – Compact layer that encircles the endoneurium composed of concentric, elongated perineural cells
Nerve Healing & Repair • Perineurium – Partitions nerve fibers into fascicles • Internal Epineurium • External Epineurium – Concentric layers of CT encircling the fascicles – Contain fibroblasts, macrophages, mast cells, BVs, and fat
Nerve Healing & Repair • Seddon classification of nerve injury – 3 grades – Neurapraxia – Axonotmesis – Neurotmesis
Seddon classification • Neurapraxia - mildest grade of nerve injury – Reduction or complete blockage of conduction across a segment of nerve. – Axonal continuity is maintained – Nerve conduction is preserved proximal & distal to the lesion but not across it – Usually reversible injuries, full recovery in days to weeks.
Seddon classification • Etiologies: – Direct mechanical compression – Ischemia/PVD – Metabolic derangements – Disease or toxinscausing demyelination
Seddon classification • Axonotmesis – Interruption of the axons with preservation of the surrounding CT “highway” – Distal Wallerian degeneration of the axons occurs during a several day period – Direct e-stim will NOT give rise to nerve conduction or muscle response – Recovery can occur through axonal regeneration due to CT highway
Seddon classification • Schwann cells proliferate and form longitudinal conduits (bands of Bungner) through which axons regenerate in months. • Recovery depends on: – Extent of retrograde axonal loss – Time to regenerate & reinnervate target muscles/sensory end organs • Regenerate at 1 mm/day
Axonotmetic Injuries • Mixed sensory & motor nerves regenerate slower • Nerve complexity dictates accuracy of nerve regeneration
Seddon Classification • Neurotmesis – most severe grade – Disruption of axon, myelin, and CT “highway” components of nerve. – Recovery through regeneration cannot occur – External continuity is preserved but intrneural fibrosis occurs – Also includes complete loss of continuity – Surgery is required to remove roadblocks to healing.
Sunderland Classification • • • Created 5 grade system. Grade I – neurapraxic injury Grade II – axonotmetic injury Grade III – endonerium disrupted Grade IV – additional disruption of perineurium • Grade V – epineural continuity is disrupted (neurotmesis)
Mackinnon & Dellon • Added Grade VI – Combinations of the previous grades of injury.
Operative Decision Making • Open injury: – Lesion in continuity • Medical mgmt. with close F/U, EMG/MRN – Lesion Discontinuity • Sharp transection – end to end repair • Blunt transection – delayed repair, resect scar, graft, repair.
Operative Decision Making • Closed Injury: – Majority caused by stretch and/or compressive forces. – Hematoma may require emergent surgery (ie compartment syndrome, pseudoaneurysm) – Most injuries do not involve transection – May represent any of Seddon’s 3 grades
Summary • Guidelines will help you as a surgeon to deal with tendon, ligament, & nerve injuries. • Understanding principles will lead to more successful repairs and mgmnt.
