Physiology of digestive system General physiology Prof Dr
- Slides: 26
Physiology of digestive system General physiology Prof. Dr. Majida Alqayim
Digestive system : 1 - Tract 2 - Accessory organs Liver, gall bladder , and pancrease • Digestion : is the mechanical and chemical breaking down of food into smaller components that can be easily absorbed. Fundamental processes that take place in the GIT are for digestion : • Motility: Contractions of smooth muscle in the wall of the tube that crush, mix and propel its contents • Secretion: Delivery of enzymes, mucus, ions and the like into the lumen, and hormones into blood. Absorption: Transport of water, ions and nutrients from the lumen, across the epithelium and into blood.
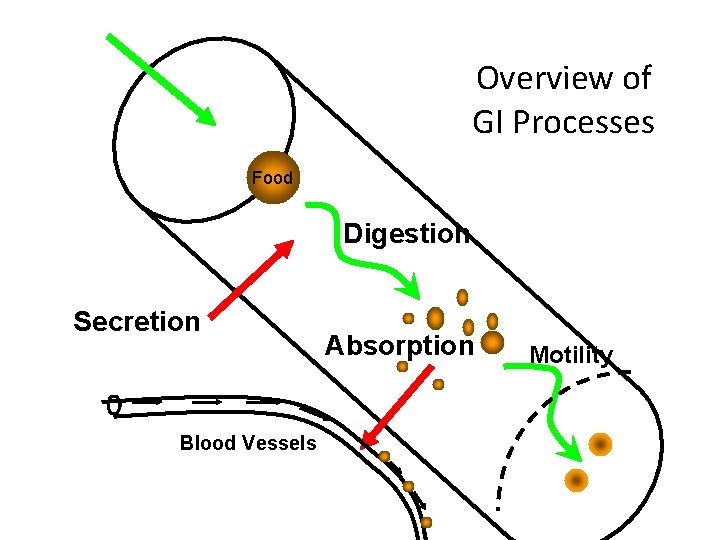
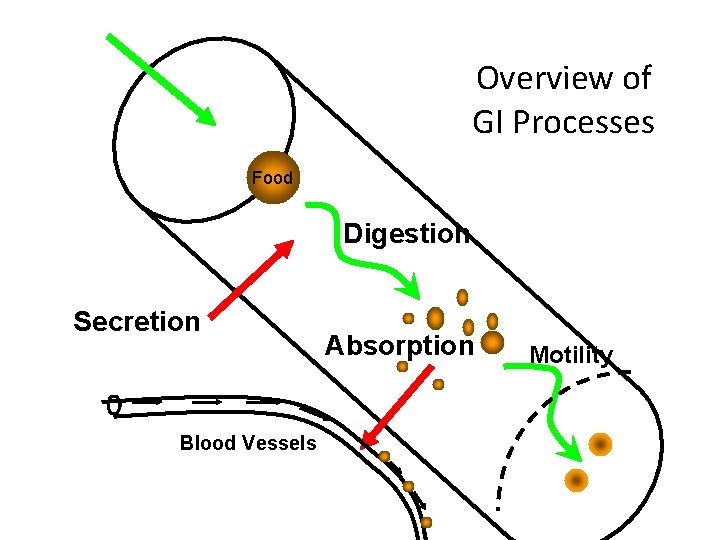
Overview of GI Processes Food Digestion Secretion Blood Vessels Absorption Motility
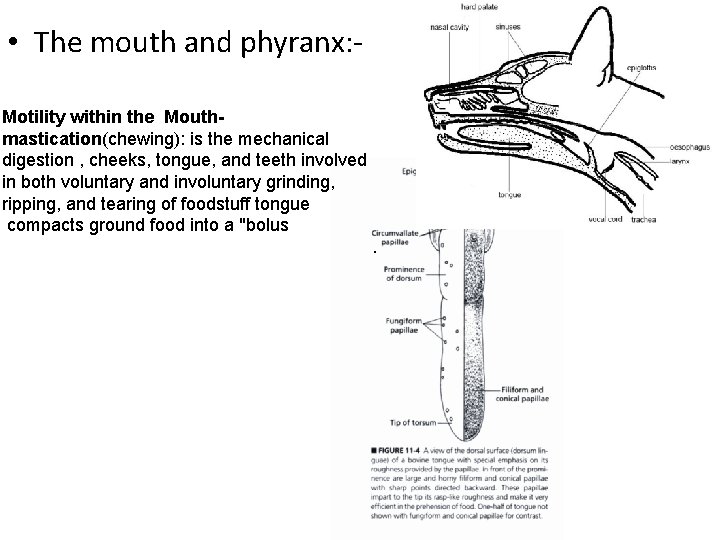
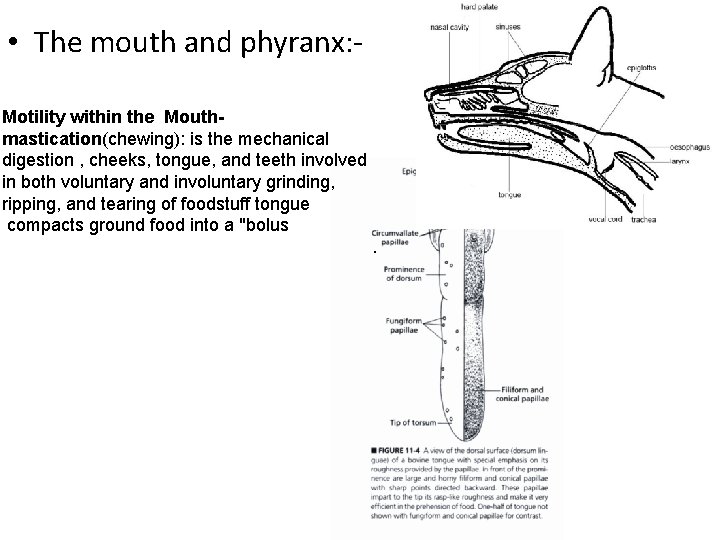
• The mouth and phyranx: Motility within the Mouthmastication(chewing): is the mechanical digestion , cheeks, tongue, and teeth involved in both voluntary and involuntary grinding, ripping, and tearing of foodstuff tongue compacts ground food into a "bolus.
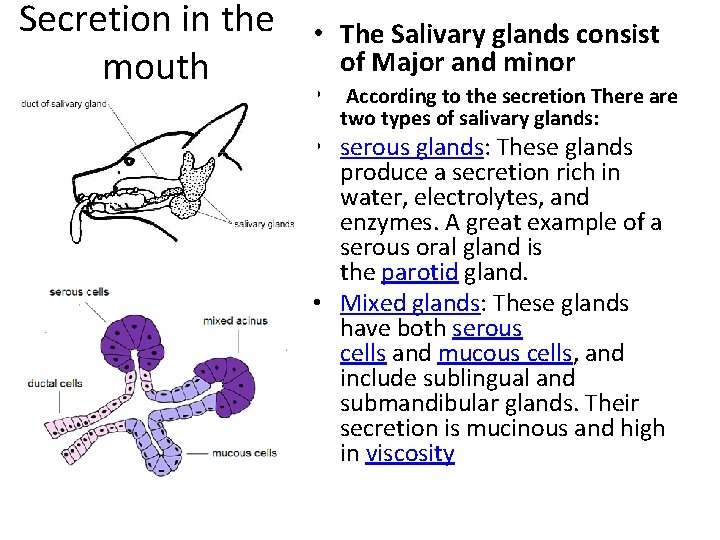
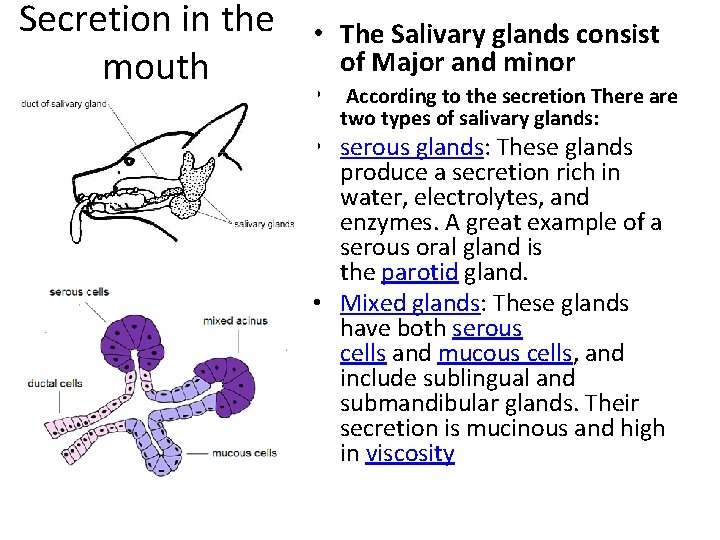
Secretion in the mouth • The Salivary glands consist of Major and minor • According to the secretion There are two types of salivary glands: • serous glands: These glands produce a secretion rich in water, electrolytes, and enzymes. A great example of a serous oral gland is the parotid gland. • Mixed glands: These glands have both serous cells and mucous cells, and include sublingual and submandibular glands. Their secretion is mucinous and high in viscosity
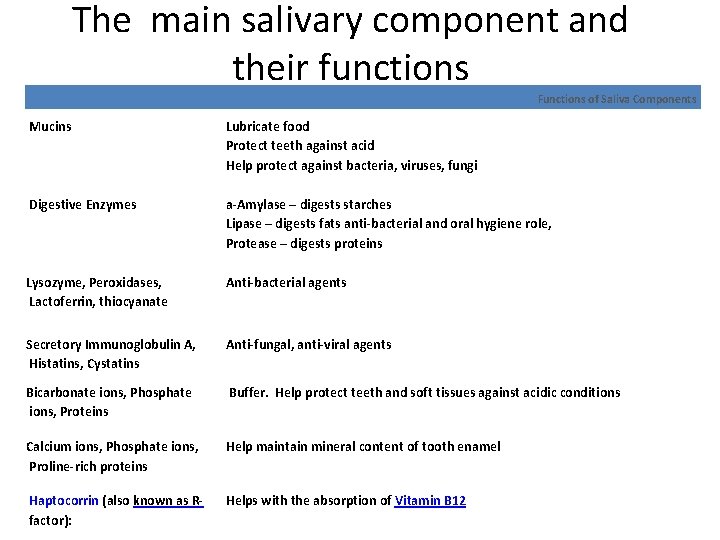
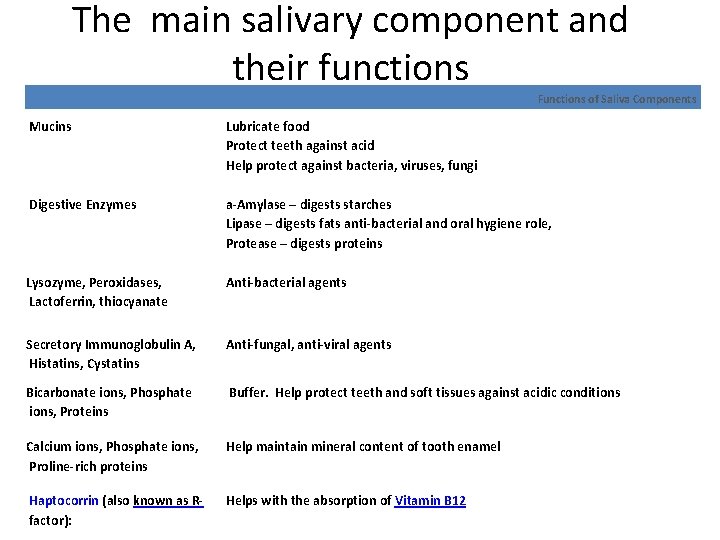
The main salivary component and their functions Functions of Saliva Components Mucins Lubricate food Protect teeth against acid Help protect against bacteria, viruses, fungi Digestive Enzymes a-Amylase – digests starches Lipase – digests fats anti-bacterial and oral hygiene role, Protease – digests proteins Lysozyme, Peroxidases, Lactoferrin, thiocyanate Anti-bacterial agents Secretory Immunoglobulin A, Histatins, Cystatins Anti-fungal, anti-viral agents Bicarbonate ions, Phosphate ions, Proteins Buffer. Help protect teeth and soft tissues against acidic conditions Calcium ions, Phosphate ions, Proline-rich proteins Help maintain mineral content of tooth enamel Haptocorrin (also known as Rfactor): Helps with the absorption of Vitamin B 12
Functions of the stomach q. Mechanical digestion q. Secreation of acid(HCl) aid in activation of pepsinogen q. Digestion of proteins by active pepsine q. Absorbtion of water and electrloytes q. Synthesis of gastric intrinsic factor (GIF), is a glycoprotein produced by the parietal cells of the stomach. It is necessary for the absorption of vitamin B 12 (cobalamin
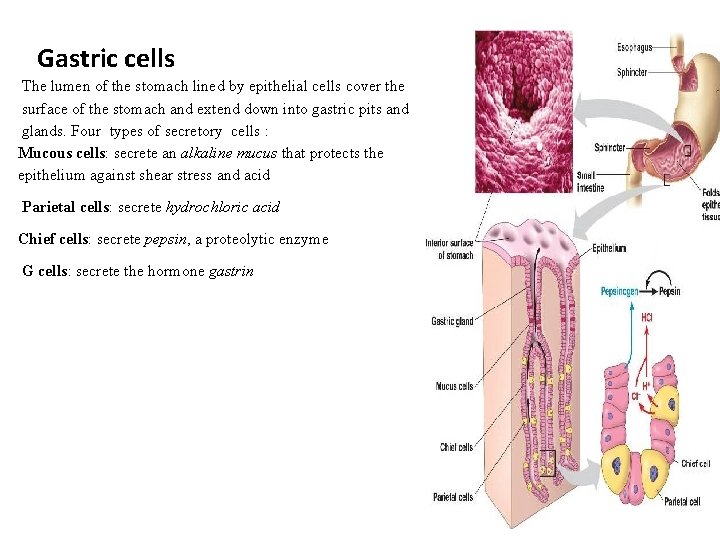
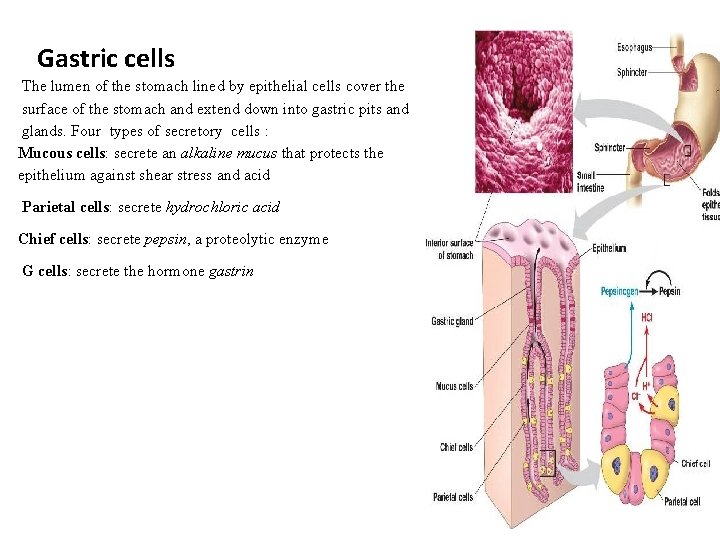
Gastric cells The lumen of the stomach lined by epithelial cells cover the surface of the stomach and extend down into gastric pits and glands. Four types of secretory cells : Mucous cells: secrete an alkaline mucus that protects the epithelium against shear stress and acid Parietal cells: secrete hydrochloric acid Chief cells: secrete pepsin, a proteolytic enzyme G cells: secrete the hormone gastrin
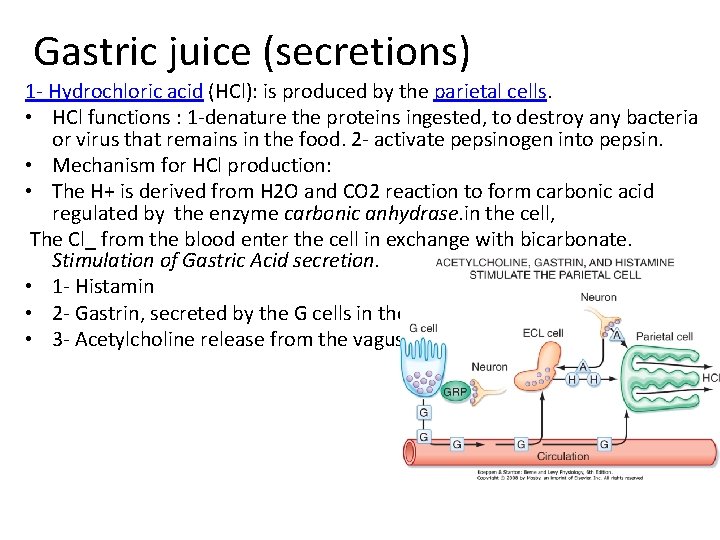
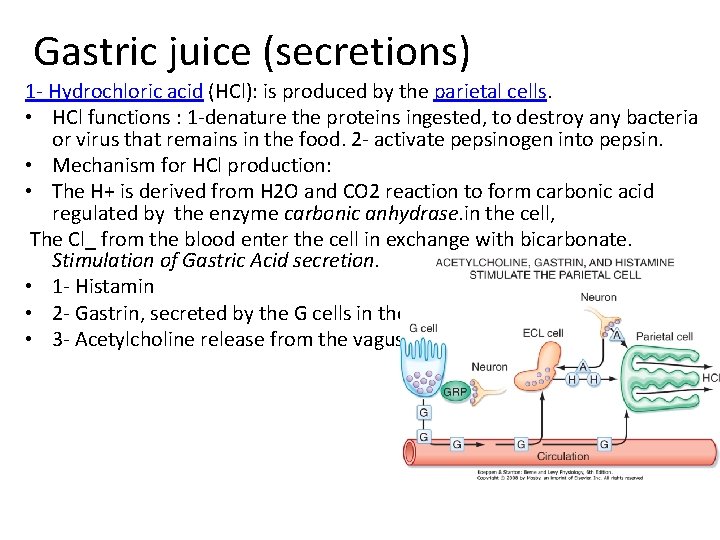
Gastric juice (secretions) 1 - Hydrochloric acid (HCl): is produced by the parietal cells. • HCl functions : 1 -denature the proteins ingested, to destroy any bacteria or virus that remains in the food. 2 - activate pepsinogen into pepsin. • Mechanism for HCl production: • The H+ is derived from H 2 O and CO 2 reaction to form carbonic acid regulated by the enzyme carbonic anhydrase. in the cell, The Cl_ from the blood enter the cell in exchange with bicarbonate. Stimulation of Gastric Acid secretion. • 1 - Histamin • 2 - Gastrin, secreted by the G cells in the antrum of the stomach • 3 - Acetylcholine release from the vagus nerve
Gastric juice 2 - Pepsin It is produced by the chief cells in its inactive form pepsinogen. Pepsinogen is then activated by the stomach acid into its active form, pepsin. Pepsin breaks down the protein in the food into smaller particles, such as amino acids. 3 - Intrinsic factor (IF): Intrinsic factor is produced by the parietal cells binds Vitamin B 12, creating a Vit. B 12 -IF complex. This complex is then absorbed at the terminal portion of the ileum. 4 - Mucin: Mucin and bicarbonate secreted by mucous cells, to protect the lininig of the stomach 5 - Gastrin: Gastrin is an endocrine hormone produced by the "G • cells and therefore enters the bloodstream and eventually returns to the stomach where it stimulates parietal cells to produce hydrochloric acid (HCl) and Intrinsic factor (IF). 6 - Gastric Lipase: Gastric lipase is an acidic lipase secreted chief • cells in the fundic mucosa in the stomach.
Intestinal functions q. Chemical digestion by digestive enzymes: § Pancreatic secretion § Intestinal secretion § Biliary secretion q. Mixing the chime with digestive enzymes via contraction of the muscle walls, is the force that propels matter through the small intestine. It is a slow process, allowing the food matter to mix with the digestive juices. q. Absorption q. Immunology
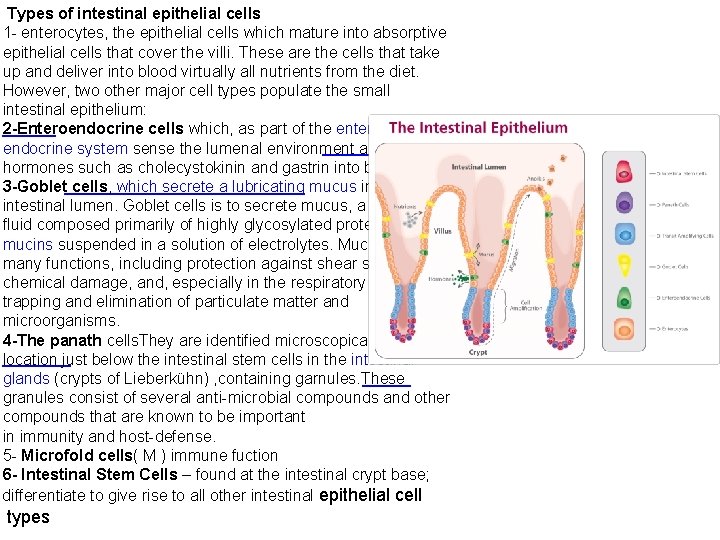
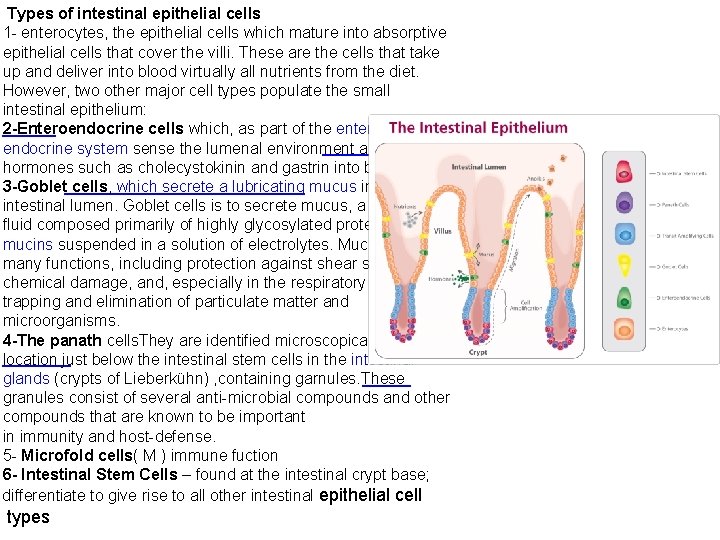
Types of intestinal epithelial cells 1 - enterocytes, the epithelial cells which mature into absorptive epithelial cells that cover the villi. These are the cells that take up and deliver into blood virtually all nutrients from the diet. However, two other major cell types populate the small intestinal epithelium: 2 -Enteroendocrine cells which, as part of the enteric endocrine system sense the lumenal environment and secrete hormones such as cholecystokinin and gastrin into blood. 3 -Goblet cells, which secrete a lubricating mucus into the intestinal lumen. Goblet cells is to secrete mucus, a viscous fluid composed primarily of highly glycosylated proteins called mucins suspended in a solution of electrolytes. Mucus serves many functions, including protection against shear stress and chemical damage, and, especially in the respiratory tree, trapping and elimination of particulate matter and microorganisms. 4 -The panath cells. They are identified microscopically by their location just below the intestinal stem cells in the intestinal glands (crypts of Lieberkühn) , containing garnules. These granules consist of several anti-microbial compounds and other compounds that are known to be important in immunity and host-defense. 5 - Microfold cells( M ) immune fuction 6 - Intestinal Stem Cells – found at the intestinal crypt base; differentiate to give rise to all other intestinal epithelial cell types
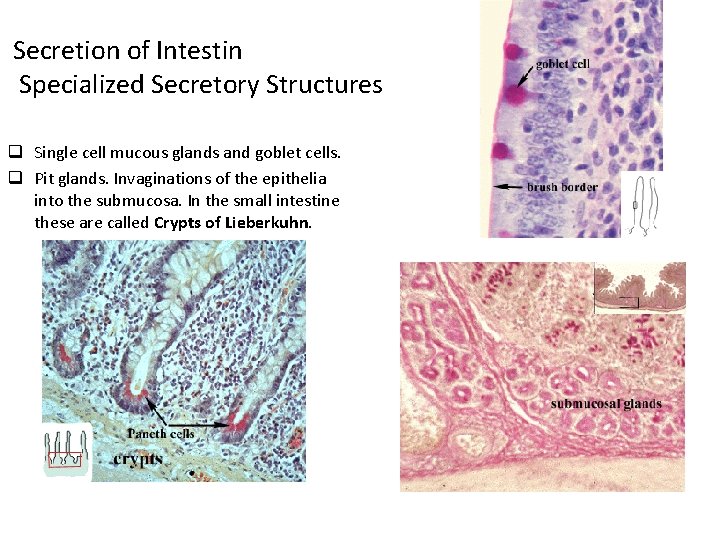
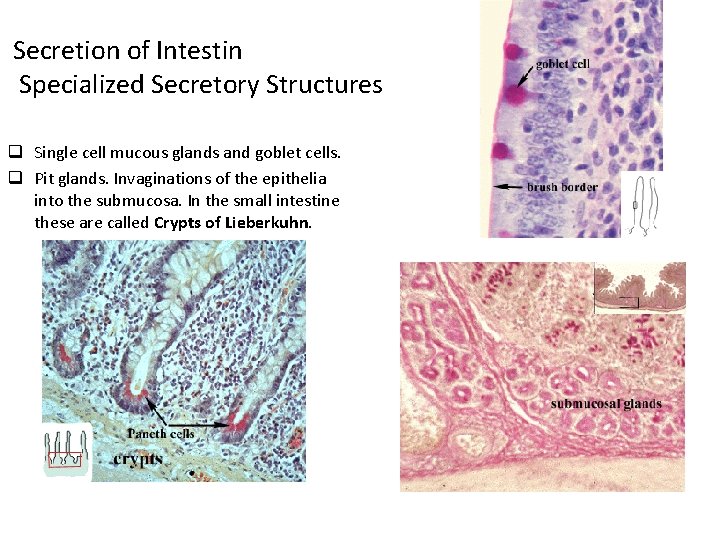
Secretion of Intestin Specialized Secretory Structures q Single cell mucous glands and goblet cells. q Pit glands. Invaginations of the epithelia into the submucosa. In the small intestine these are called Crypts of Lieberkuhn.
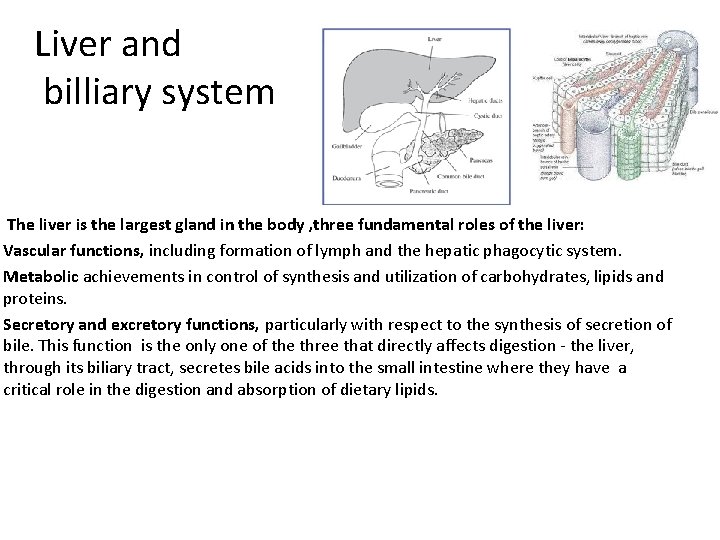
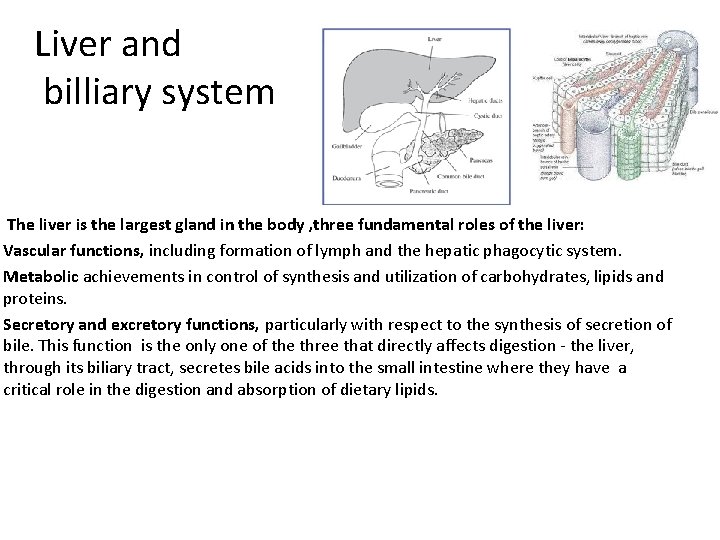
Liver and billiary system The liver is the largest gland in the body , three fundamental roles of the liver: Vascular functions, including formation of lymph and the hepatic phagocytic system. Metabolic achievements in control of synthesis and utilization of carbohydrates, lipids and proteins. Secretory and excretory functions, particularly with respect to the synthesis of secretion of bile. This function is the only one of the three that directly affects digestion - the liver, through its biliary tract, secretes bile acids into the small intestine where they have a critical role in the digestion and absorption of dietary lipids.
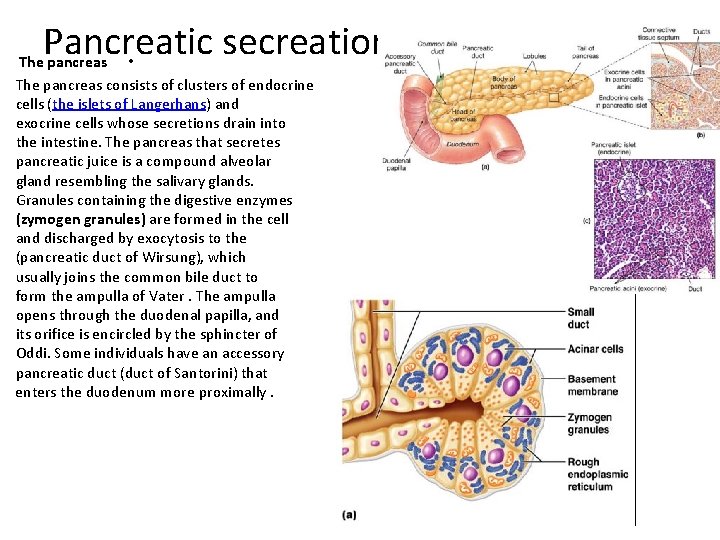
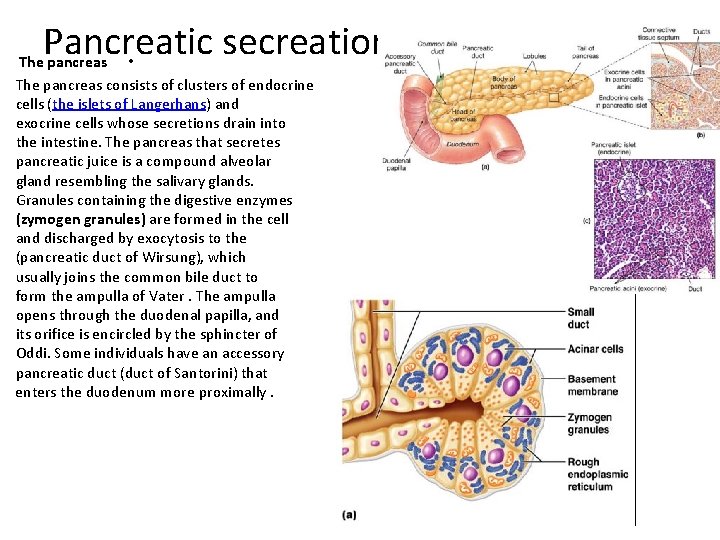
Pancreatic secreation The pancreas • The pancreas consists of clusters of endocrine cells (the islets of Langerhans) and exocrine cells whose secretions drain into the intestine. The pancreas that secretes pancreatic juice is a compound alveolar gland resembling the salivary glands. Granules containing the digestive enzymes (zymogen granules) are formed in the cell and discharged by exocytosis to the (pancreatic duct of Wirsung), which usually joins the common bile duct to form the ampulla of Vater. The ampulla opens through the duodenal papilla, and its orifice is encircled by the sphincter of Oddi. Some individuals have an accessory pancreatic duct (duct of Santorini) that enters the duodenum more proximally.
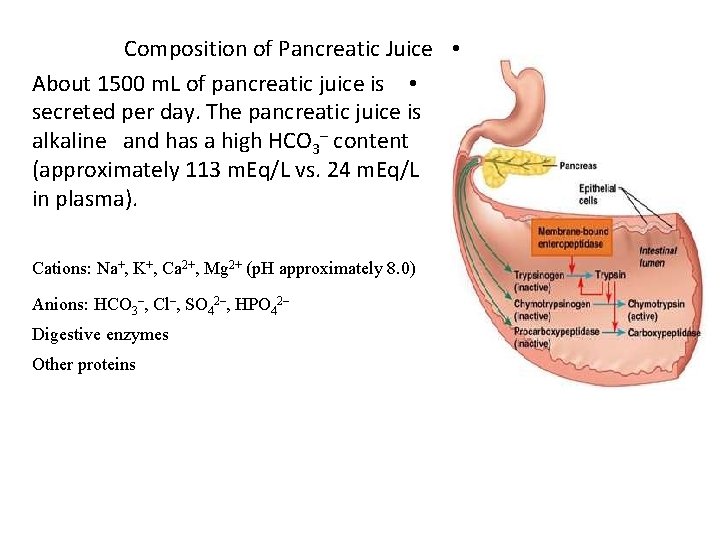
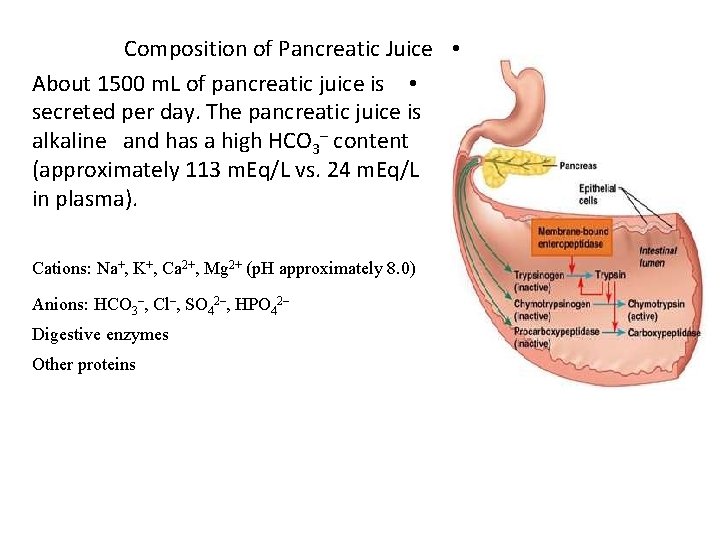
Composition of Pancreatic Juice • About 1500 m. L of pancreatic juice is • secreted per day. The pancreatic juice is alkaline and has a high HCO 3– content (approximately 113 m. Eq/L vs. 24 m. Eq/L in plasma). • Cations: Na+, K+, Ca 2+, Mg 2+ (p. H approximately 8. 0) Anions: HCO 3–, Cl–, SO 42–, HPO 42– Digestive enzymes Other proteins
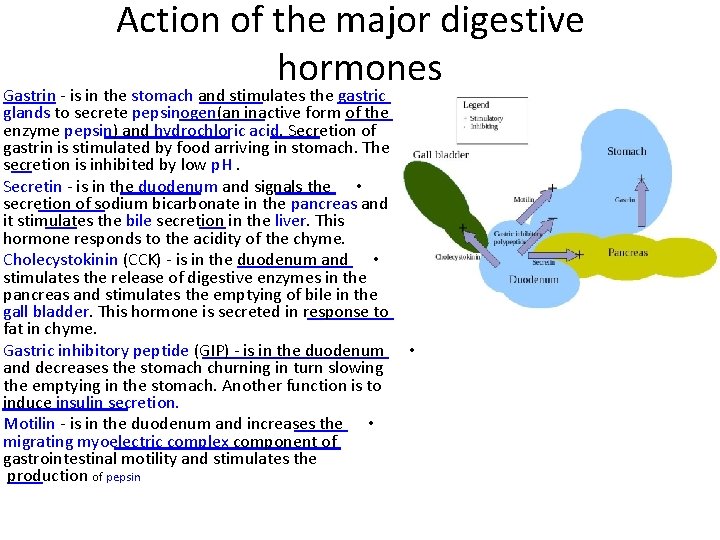
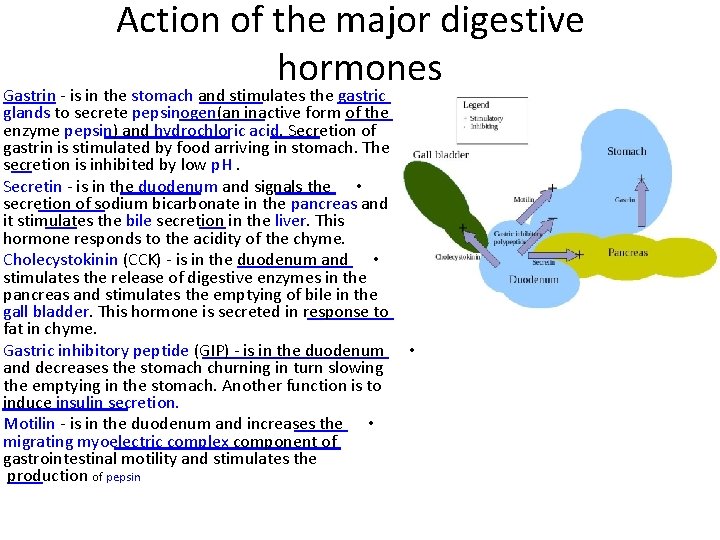
Action of the major digestive hormones Gastrin - is in the stomach and stimulates the gastric • glands to secrete pepsinogen(an inactive form of the enzyme pepsin) and hydrochloric acid. Secretion of gastrin is stimulated by food arriving in stomach. The secretion is inhibited by low p. H. Secretin - is in the duodenum and signals the • secretion of sodium bicarbonate in the pancreas and it stimulates the bile secretion in the liver. This hormone responds to the acidity of the chyme. Cholecystokinin (CCK) - is in the duodenum and • stimulates the release of digestive enzymes in the pancreas and stimulates the emptying of bile in the gall bladder. This hormone is secreted in response to fat in chyme. Gastric inhibitory peptide (GIP) - is in the duodenum • and decreases the stomach churning in turn slowing the emptying in the stomach. Another function is to induce insulin secretion. Motilin - is in the duodenum and increases the • migrating myoelectric complex component of gastrointestinal motility and stimulates the production of pepsin
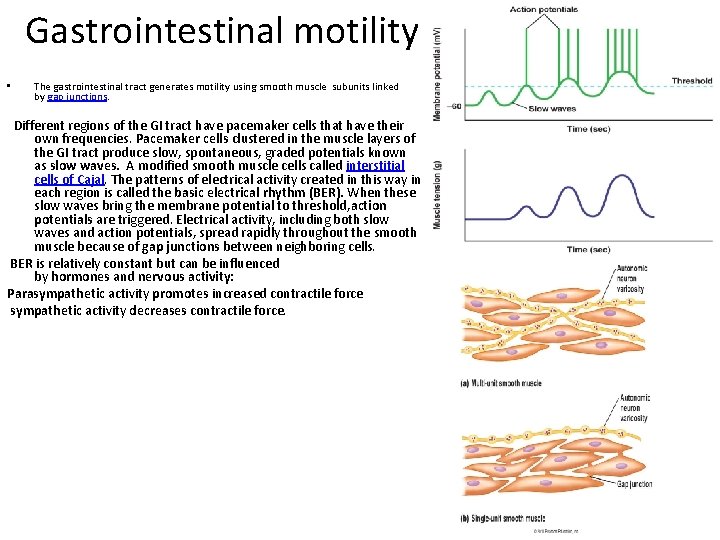
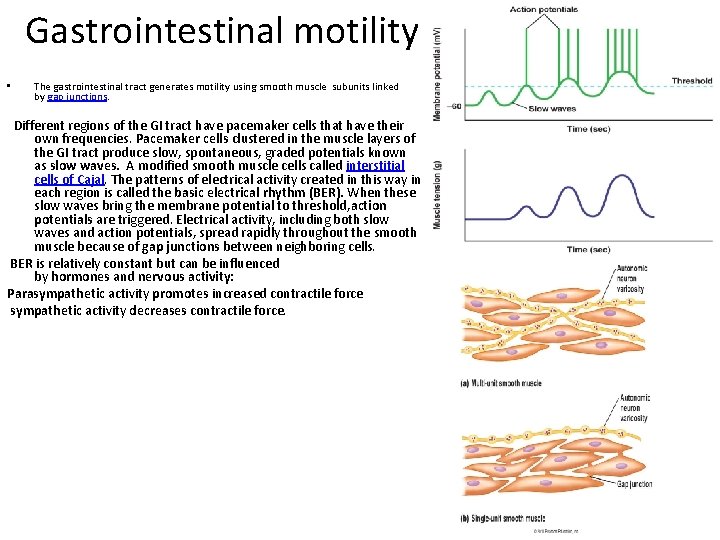
Gastrointestinal motility • The gastrointestinal tract generates motility using smooth muscle subunits linked by gap junctions. Different regions of the GI tract have pacemaker cells that have their own frequencies. Pacemaker cells clustered in the muscle layers of the GI tract produce slow, spontaneous, graded potentials known as slow waves. A modified smooth muscle cells called interstitial cells of Cajal. The patterns of electrical activity created in this way in each region is called the basic electrical rhythm (BER). When these slow waves bring the membrane potential to threshold, action potentials are triggered. Electrical activity, including both slow waves and action potentials, spread rapidly throughout the smooth muscle because of gap junctions between neighboring cells. BER is relatively constant but can be influenced by hormones and nervous activity: Parasympathetic activity promotes increased contractile force sympathetic activity decreases contractile force.
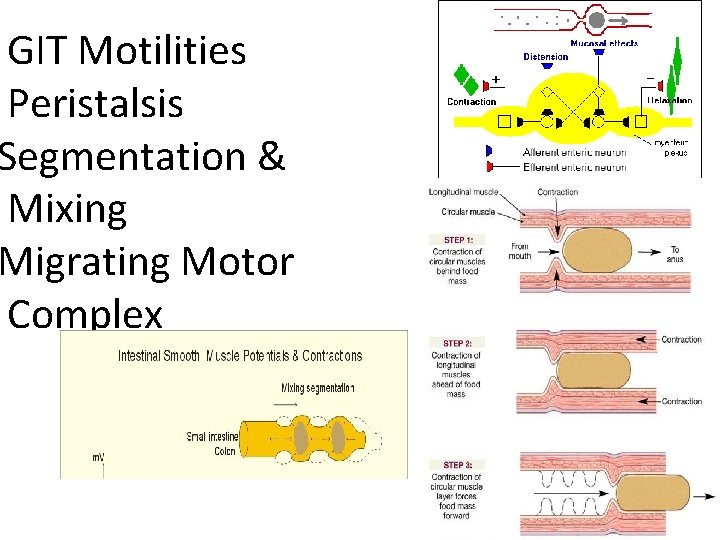
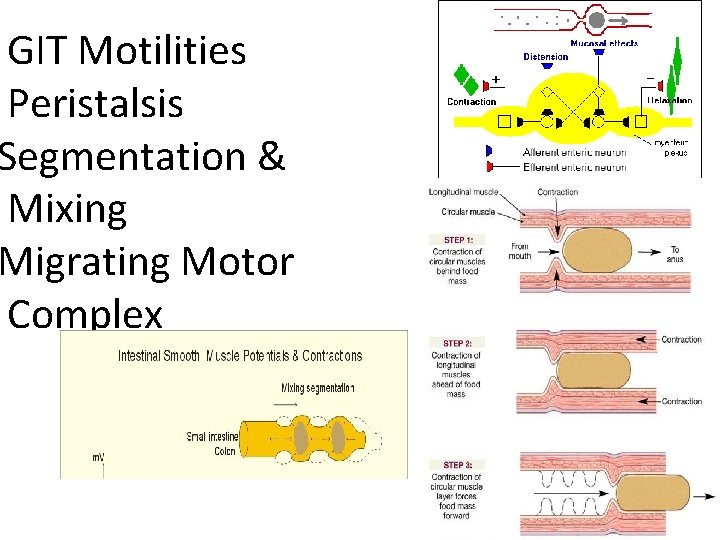
GIT Motilities Peristalsis Segmentation & Mixing Migrating Motor Complex
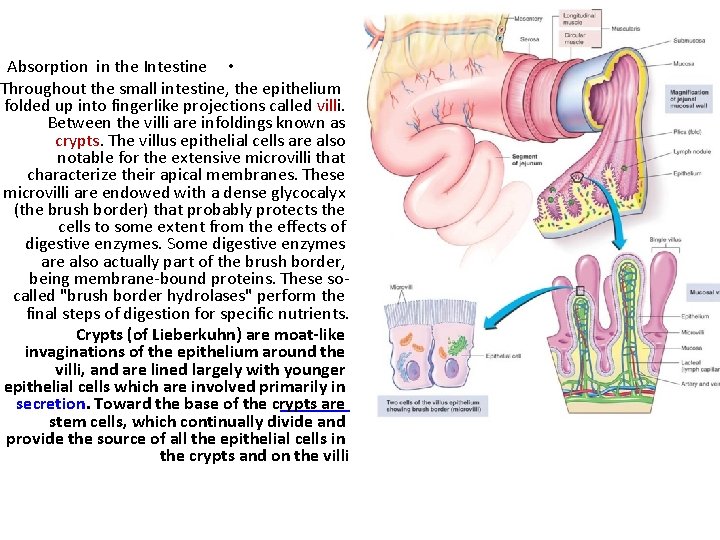
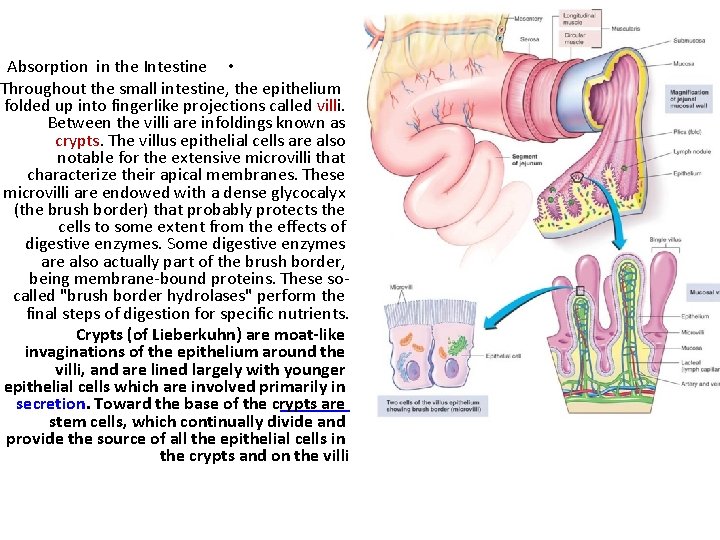
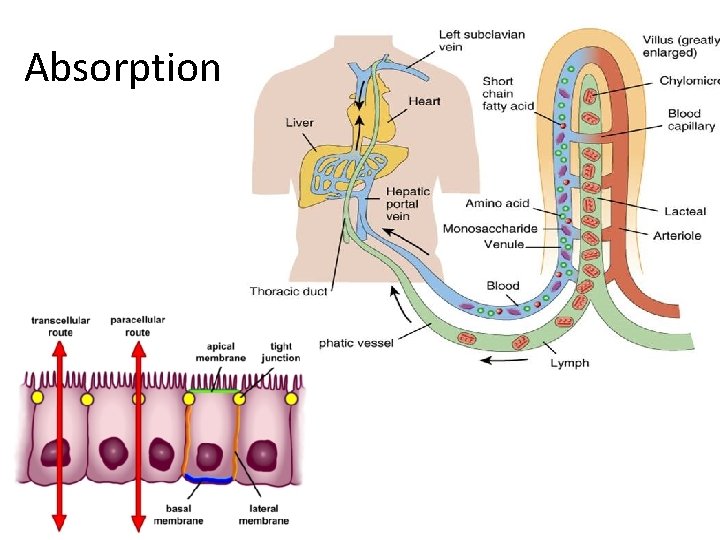
Absorption in the Intestine • Throughout the small intestine, the epithelium folded up into fingerlike projections called villi. Between the villi are infoldings known as crypts. The villus epithelial cells are also notable for the extensive microvilli that characterize their apical membranes. These microvilli are endowed with a dense glycocalyx (the brush border) that probably protects the cells to some extent from the effects of digestive enzymes. Some digestive enzymes are also actually part of the brush border, being membrane-bound proteins. These socalled "brush border hydrolases" perform the final steps of digestion for specific nutrients. Crypts (of Lieberkuhn) are moat-like invaginations of the epithelium around the villi, and are lined largely with younger epithelial cells which are involved primarily in secretion. Toward the base of the crypts are stem cells, which continually divide and provide the source of all the epithelial cells in the crypts and on the villi • •
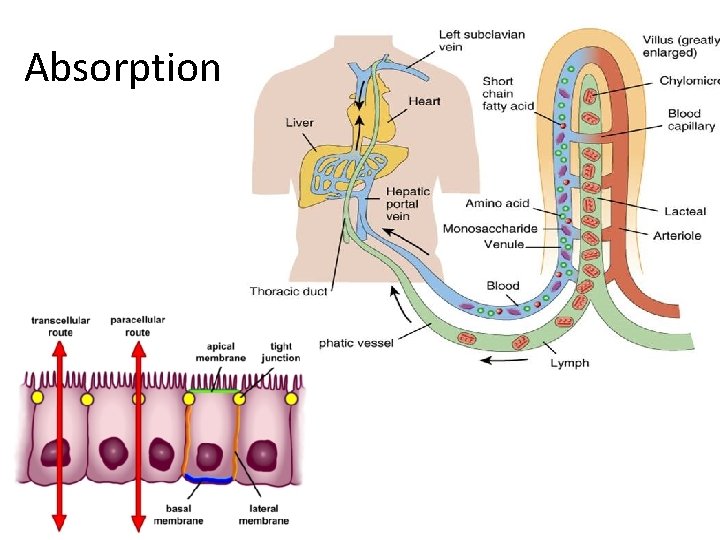
Absorption
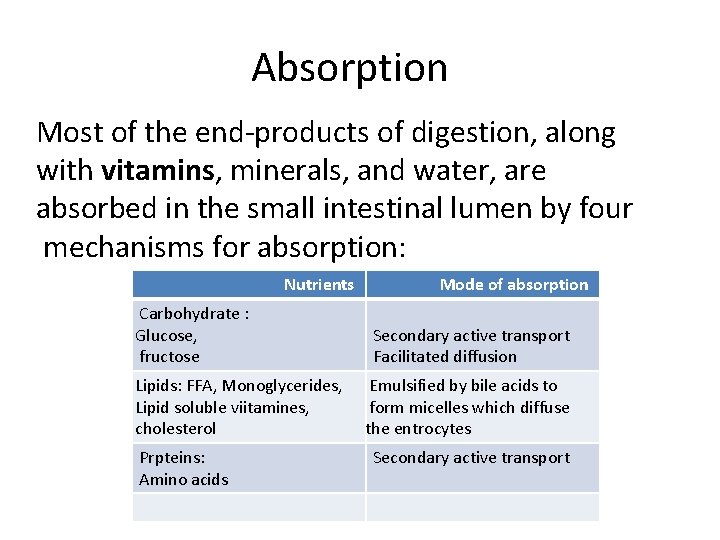
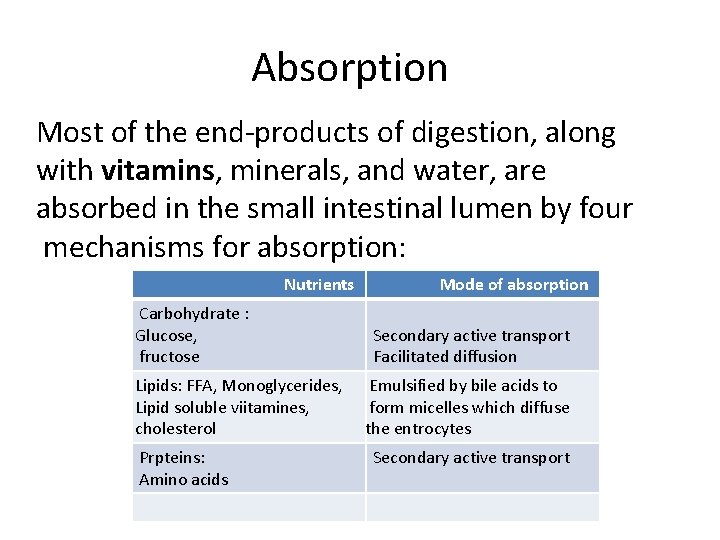
Absorption Most of the end-products of digestion, along with vitamins, minerals, and water, are absorbed in the small intestinal lumen by four mechanisms for absorption: Nutrients Carbohydrate : Glucose, fructose Lipids: FFA, Monoglycerides, Lipid soluble viitamines, cholesterol Prpteins: Amino acids Mode of absorption Secondary active transport Facilitated diffusion Emulsified by bile acids to form micelles which diffuse the entrocytes Secondary active transport
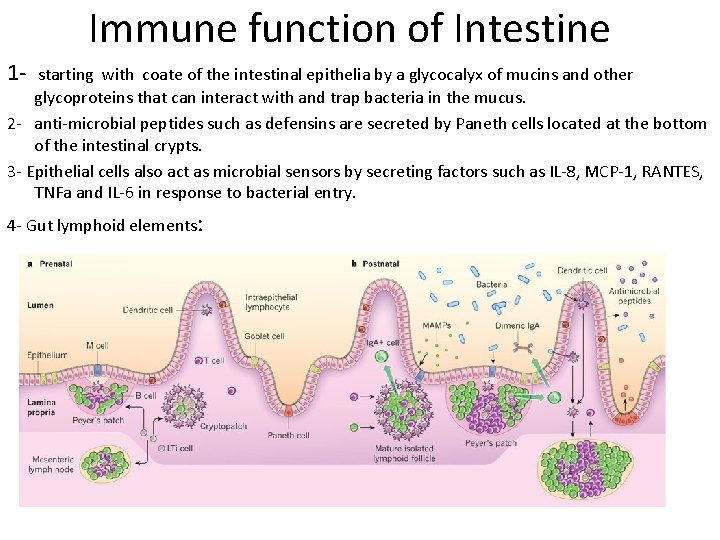
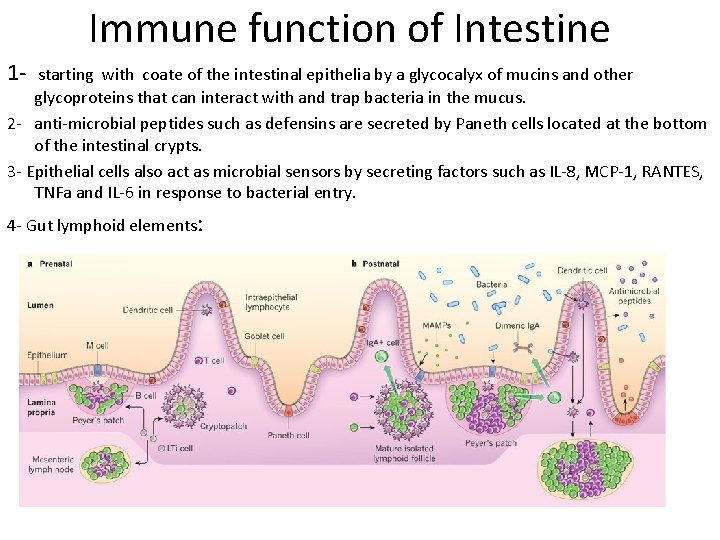
Immune function of Intestine 1 - starting with coate of the intestinal epithelia by a glycocalyx of mucins and other glycoproteins that can interact with and trap bacteria in the mucus. 2 - anti-microbial peptides such as defensins are secreted by Paneth cells located at the bottom of the intestinal crypts. 3 - Epithelial cells also act as microbial sensors by secreting factors such as IL-8, MCP-1, RANTES, TNFa and IL-6 in response to bacterial entry. 4 - Gut lymphoid elements:
Gut immune elements Peyer's Patches: These are lymphoid follicles similar in many ways to lymph nodes, located in the mucosa and extending into the submucosa of the small intestine, especially the ileum. Mucosa associated lymphoid tissue{Lamina propria lymphocytes}: These are lymphocytes scattered in the lamina propria of the mucosa. A majority of these cells are Ig. A-secreting B cells. Intraepithelial lymphocytes: These are lymphocytes that are positioned in the basolateral spaces between lumenal epithelial cells, beneath the tight junctions M or microfold cell. M cells are a specific cell type in the intestinal epithelium over lymphoid follicles that endocytose a variety of protein and peptide antigens. Instead of digesting these proteins, M cells transport them into the underlying tissue, where they are taken up by local dendritic cells and macrophages. Dendritic cells and macrophages that receive antigens from M cells present them to T cells Paneth cells, along with goblet cells, enterocytes, and enteroendocrine cells, represent the principal cell types of the epithelium of the small intestine their location just below the intestinal stem cells in the intestinal glands (crypts of Lieberkühn) they secret anti-microbial compounds and other compounds that are
Microbial Life in the Digestive Tract The gastrointestinal tract contains an immensely complex ecology of microorganisms. A typical person harbors more than 500 distinct species of bacteria, representing dozens of different lifestyles and capabilities. The composition and distribution of this menagerie varies with age, state of health and diet. The gastrointestinal tract is sterile at birth, but colonization typically begins within a few hours of birth, starting in the small intestine and progressing caudally over a period of several days. In most circumstances, a "mature" microbial flora is established by 3 to 4 weeks of age. In healthy individuals the stomach and proximal small intestine contain few microorganisms, largely a result of the bacteriocidal activity of gastric acid; those that are present are aerobes and facultative anaerobes. Large intestinal epithelial cells do not produce digestive enzymes, but contain huge numbers of bacteria which have the enzymes to digest and utilize many substrates. Bacterial populations in the large intestine digest carbohydrates, proteins and lipids that escape digestion and absorption in small intestine.
Microbial Fermentation is the enzymatic decomposition and utililization of foodstuffs, particularly carbohydrates, by microbes. Fermentation takes place throughout the gastrointestinal tract of all animals, but the intensity of fermentation depends on microbe numbers, which are generally highest in the large bowel. Thus, the large intestine is quantitatively the most important site of fermention, except for species with forestomachs (ruminants). Further, there are major differences in the contribution of fermentation to energy production of different species. In carnivores like dogs and cats, and even in omnivores like humans, fermentation generates rather few calories, but in herbivores, fermentation is a way of life. In all animals, processes are attributed to the microbial flora of the large intestine or the rumen : 1 - Digestion and metabolism of carbohydrates not digested in the small intestine (e. g. cellulose, residual starch) producing VFAs : Acetic acid, Propionic acid, Beutyric acid 2 - synthesis of high quality proteins 3 - Synthesis of vitamin K and certain B vitamins