PHYSIOLOGY EXTERNAL AND INTERNAL RESPIRATION EXTERNAL RESPIRATION Respiration

- Slides: 72
PHYSIOLOGY EXTERNAL AND INTERNAL RESPIRATION
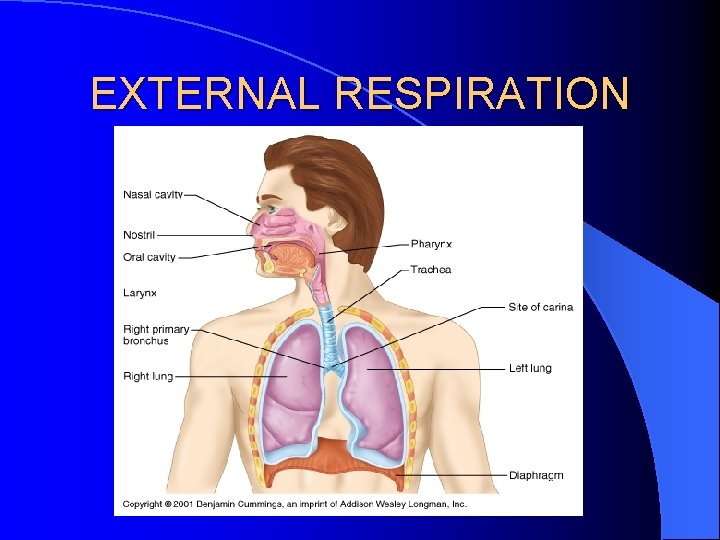
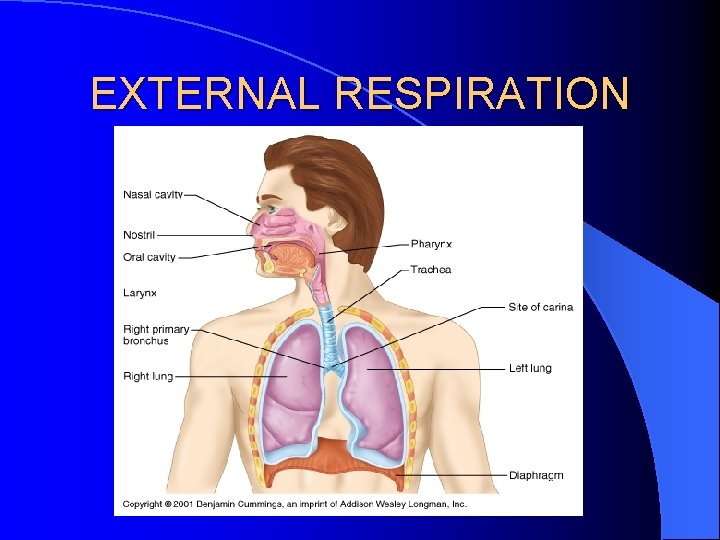
EXTERNAL RESPIRATION
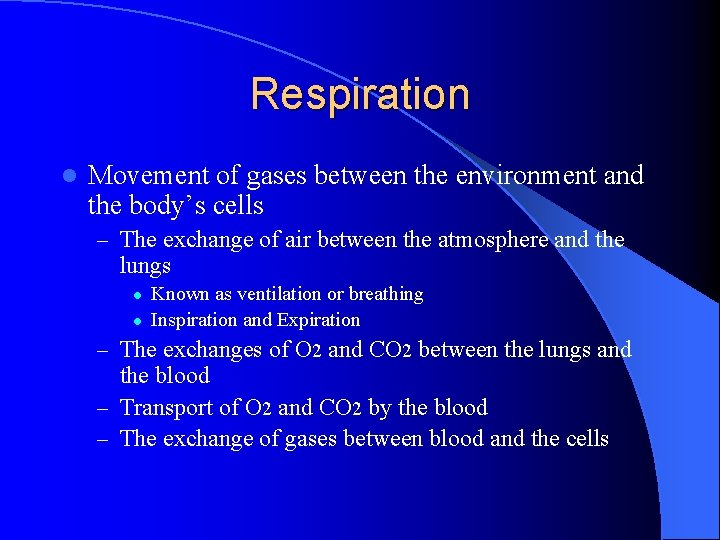
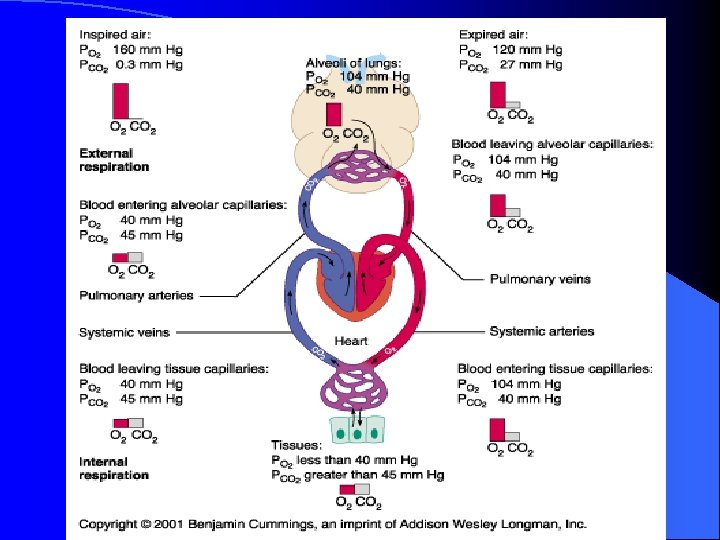
Respiration l Movement of gases between the environment and the body’s cells – The exchange of air between the atmosphere and the lungs l l Known as ventilation or breathing Inspiration and Expiration – The exchanges of O 2 and CO 2 between the lungs and the blood – Transport of O 2 and CO 2 by the blood – The exchange of gases between blood and the cells
RESPIRATION
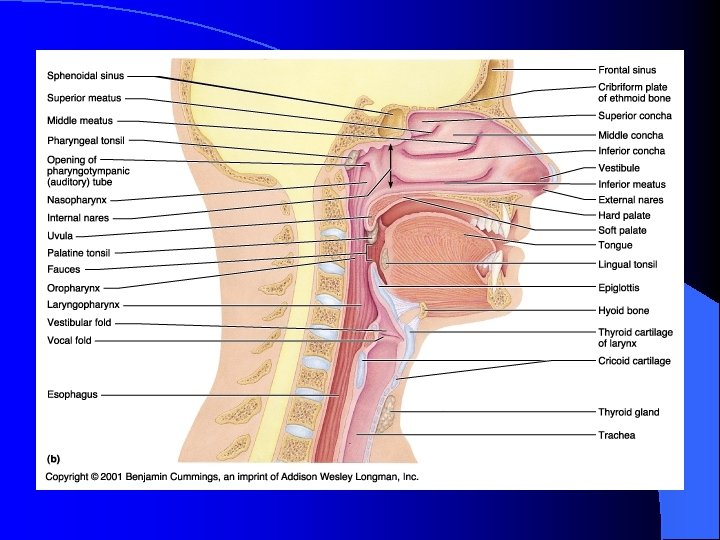
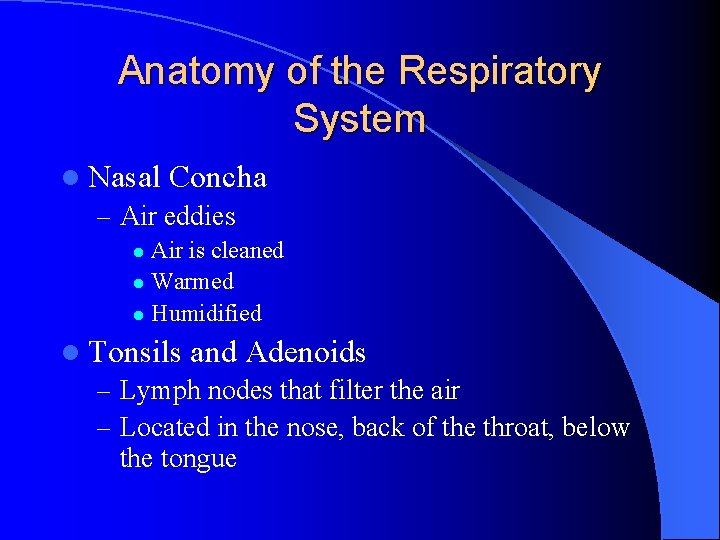
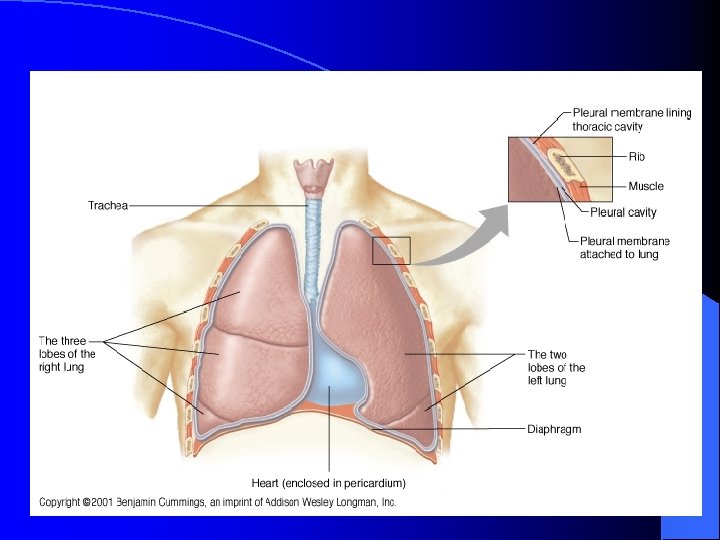
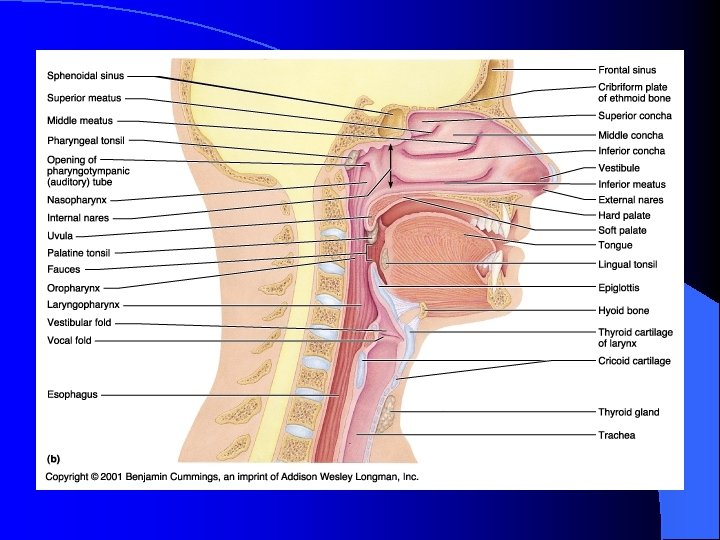
Anatomy of the Respiratory System l Nasal Concha – Air eddies Air is cleaned l Warmed l Humidified l l Tonsils and Adenoids – Lymph nodes that filter the air – Located in the nose, back of the throat, below the tongue
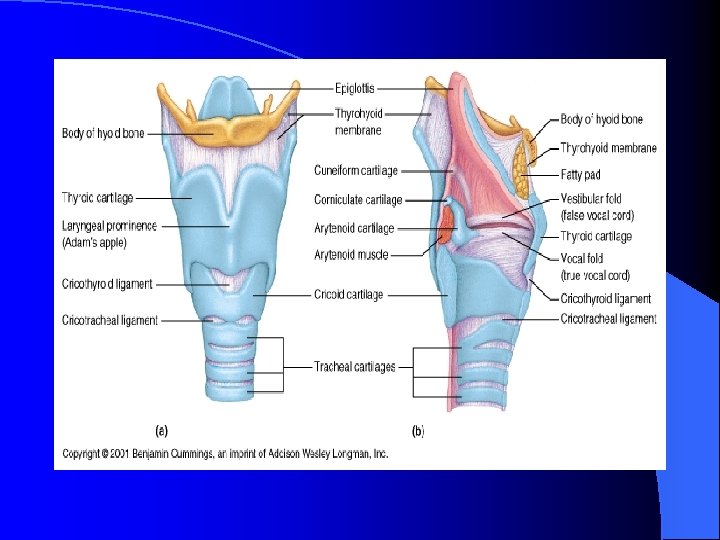
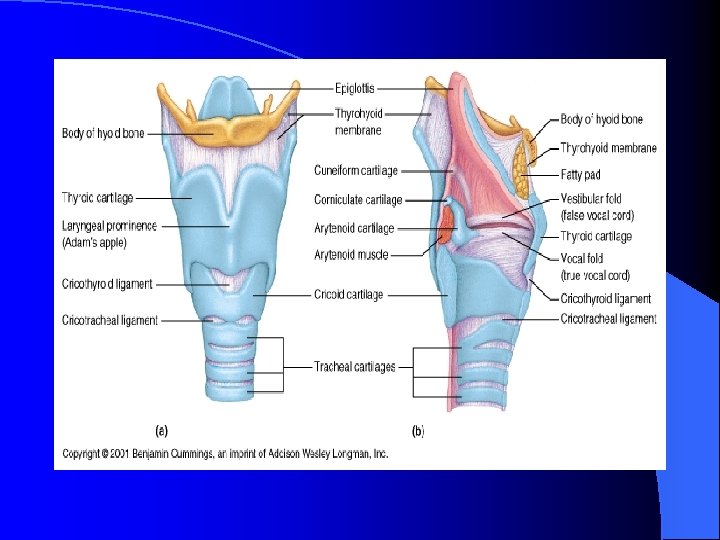
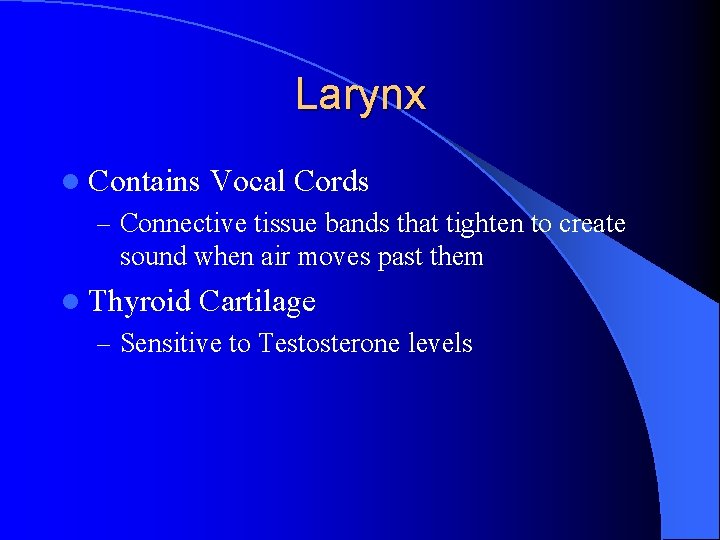
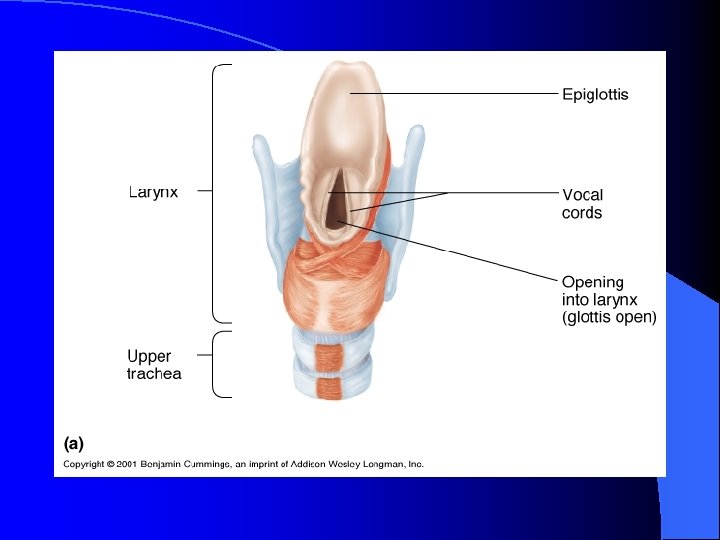
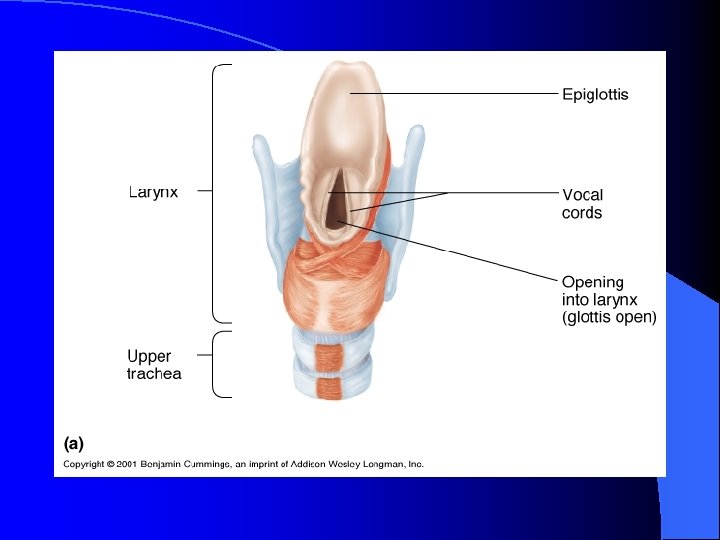
Larynx l Contains Vocal Cords – Connective tissue bands that tighten to create sound when air moves past them l Thyroid Cartilage – Sensitive to Testosterone levels
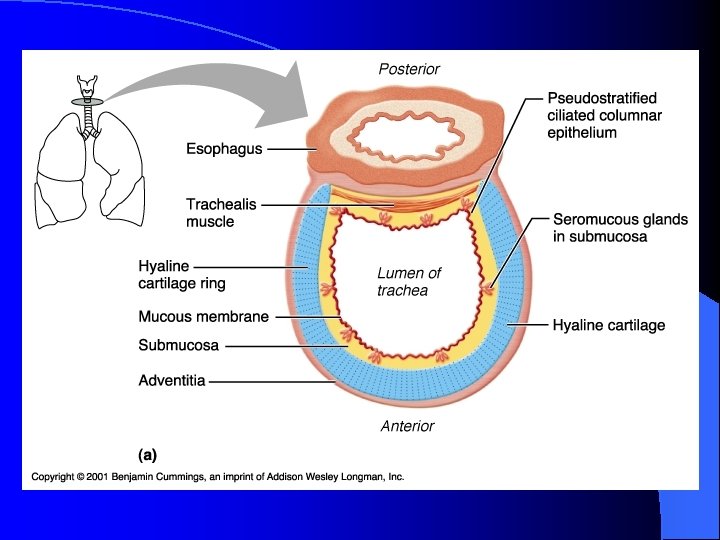
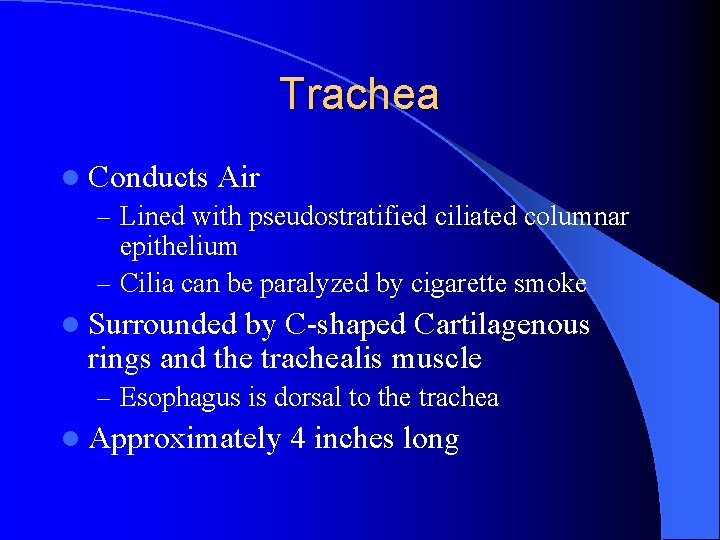
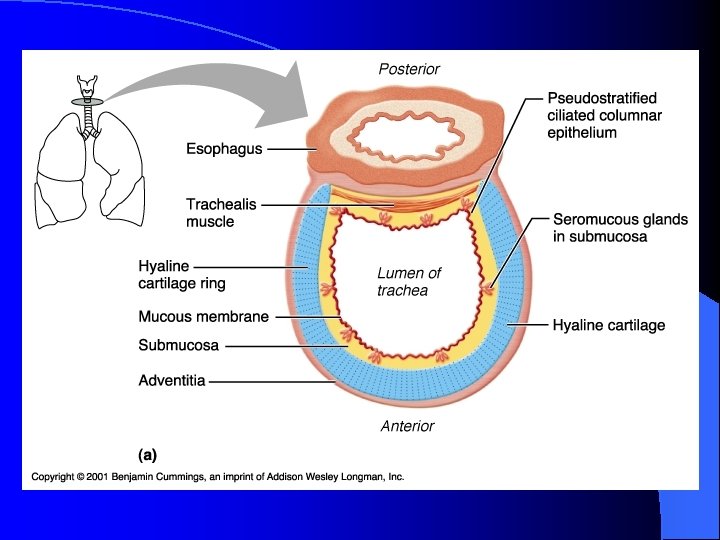
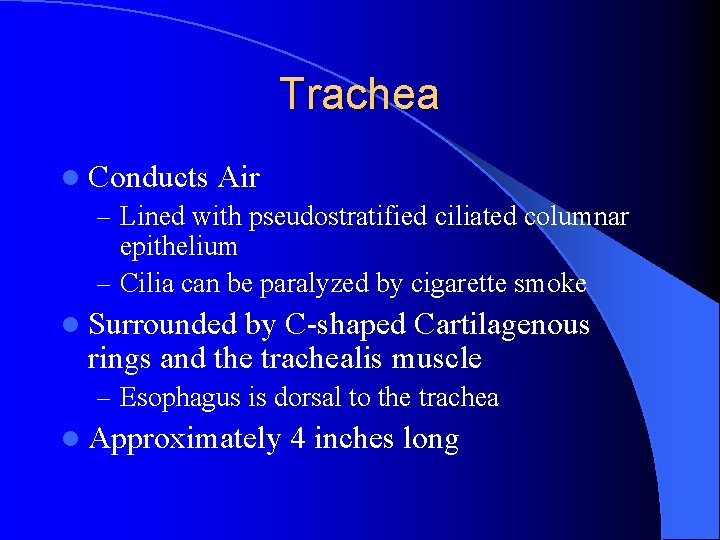
Trachea l Conducts Air – Lined with pseudostratified ciliated columnar epithelium – Cilia can be paralyzed by cigarette smoke l Surrounded by C-shaped Cartilagenous rings and the trachealis muscle – Esophagus is dorsal to the trachea l Approximately 4 inches long
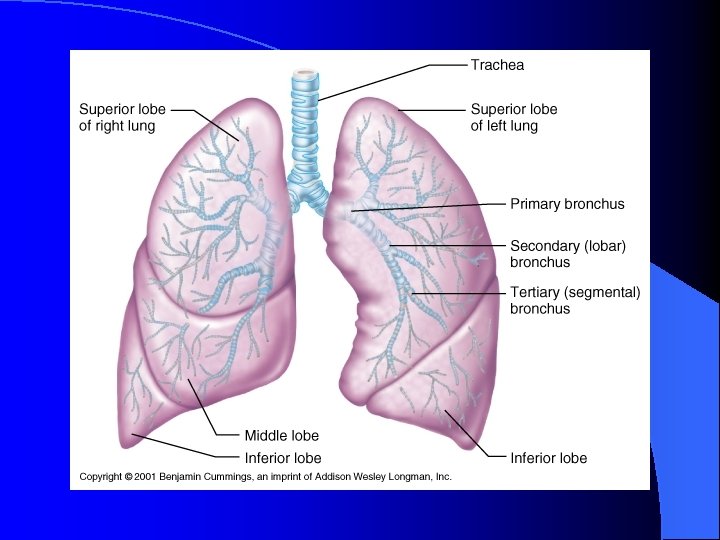
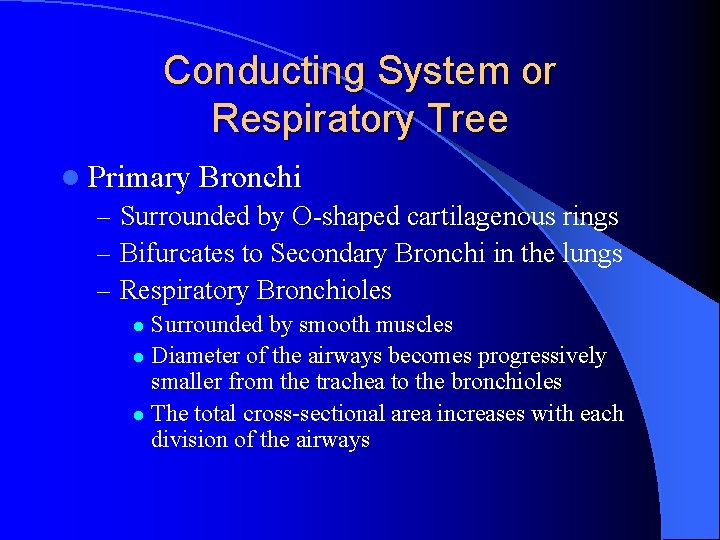
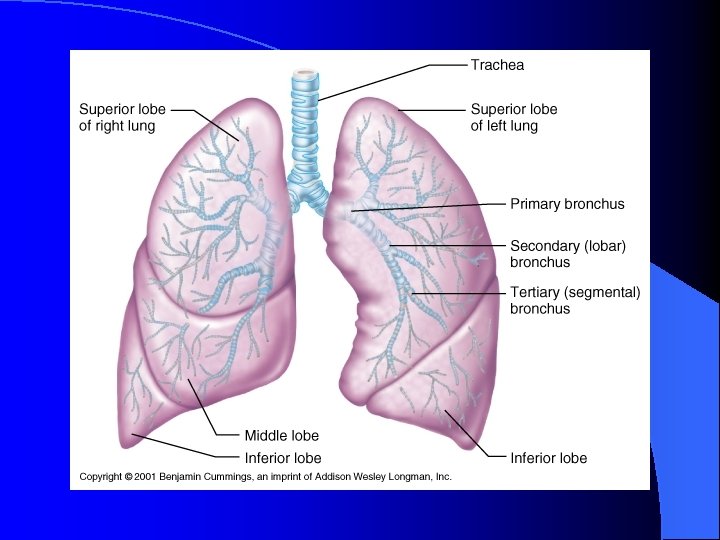
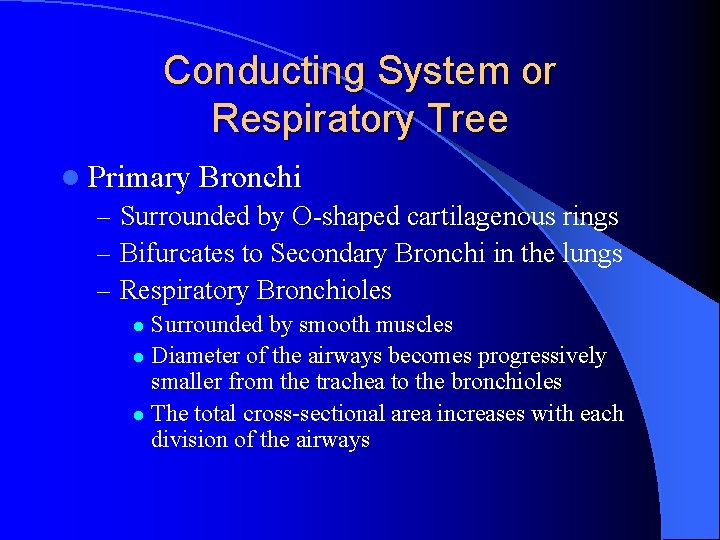
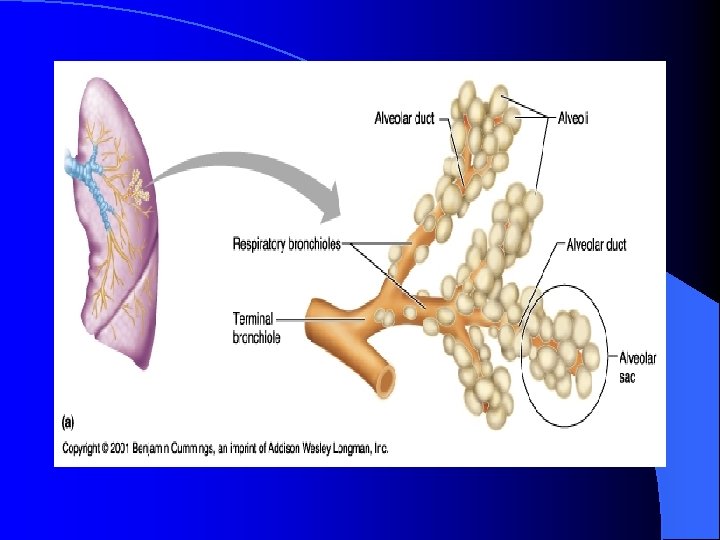
Conducting System or Respiratory Tree l Primary Bronchi – Surrounded by O-shaped cartilagenous rings – Bifurcates to Secondary Bronchi in the lungs – Respiratory Bronchioles Surrounded by smooth muscles l Diameter of the airways becomes progressively smaller from the trachea to the bronchioles l The total cross-sectional area increases with each division of the airways l
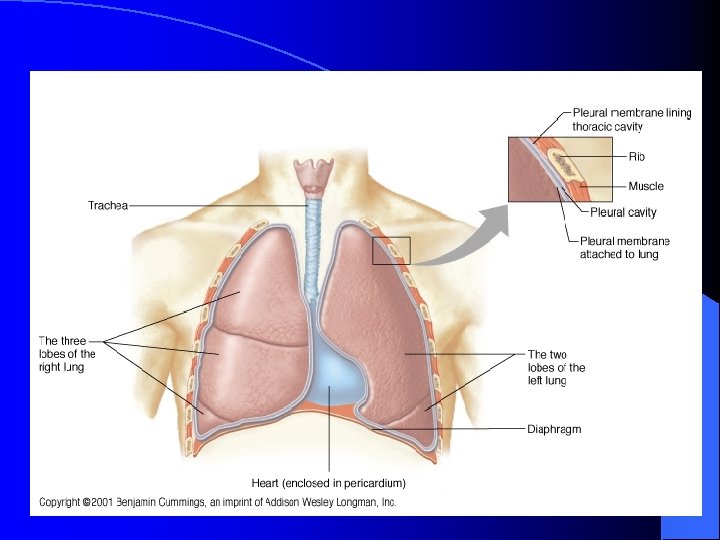
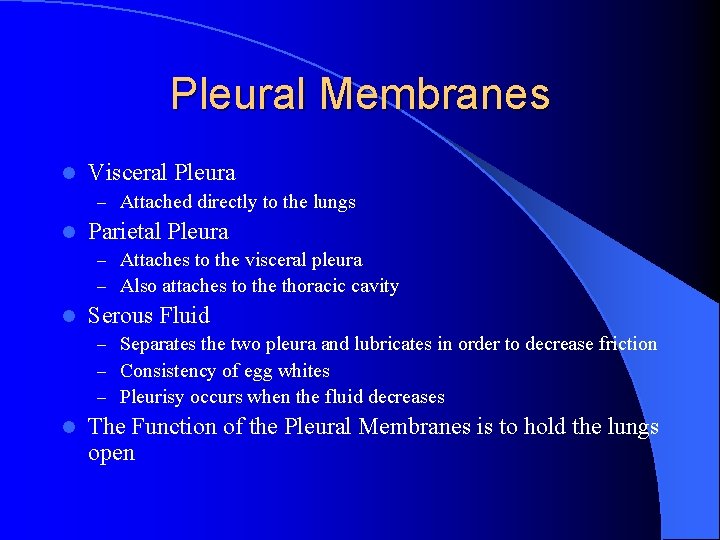
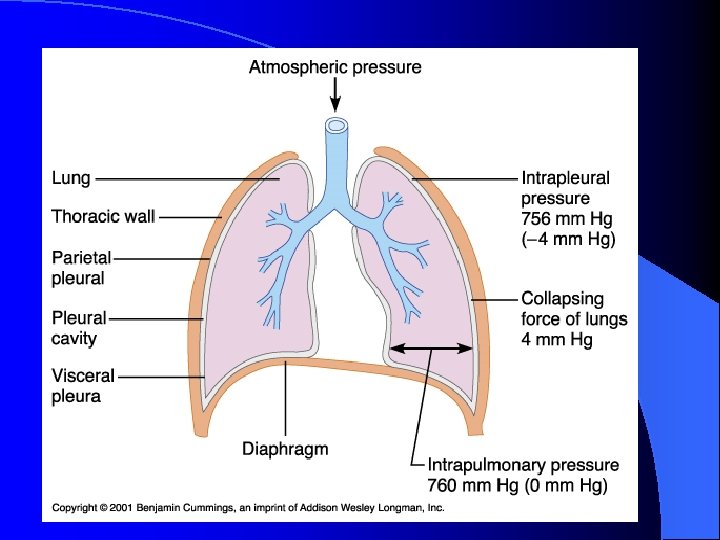
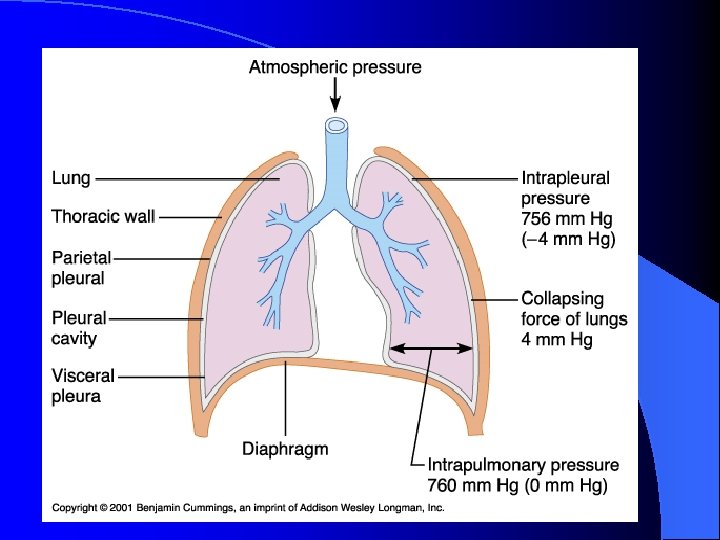
Pleural Membranes l Visceral Pleura – Attached directly to the lungs l Parietal Pleura – Attaches to the visceral pleura – Also attaches to the thoracic cavity l Serous Fluid – Separates the two pleura and lubricates in order to decrease friction – Consistency of egg whites – Pleurisy occurs when the fluid decreases l The Function of the Pleural Membranes is to hold the lungs open
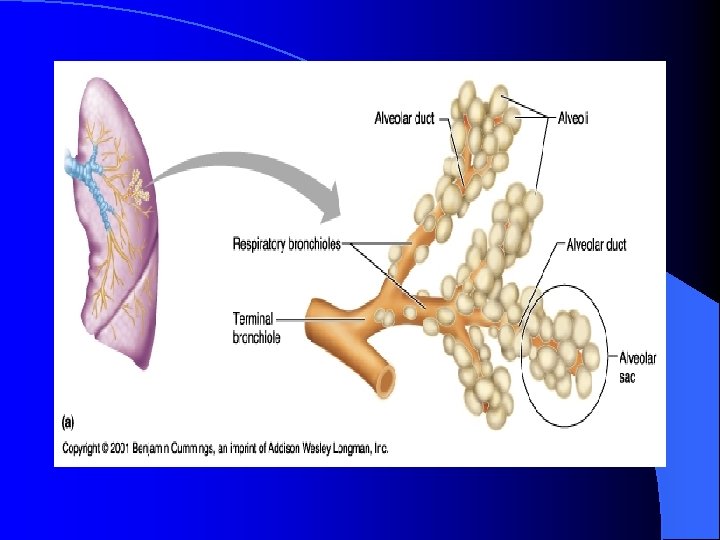
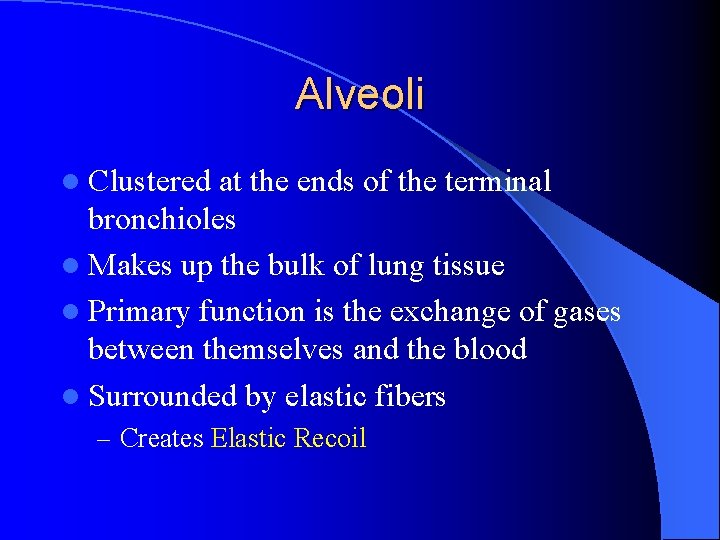
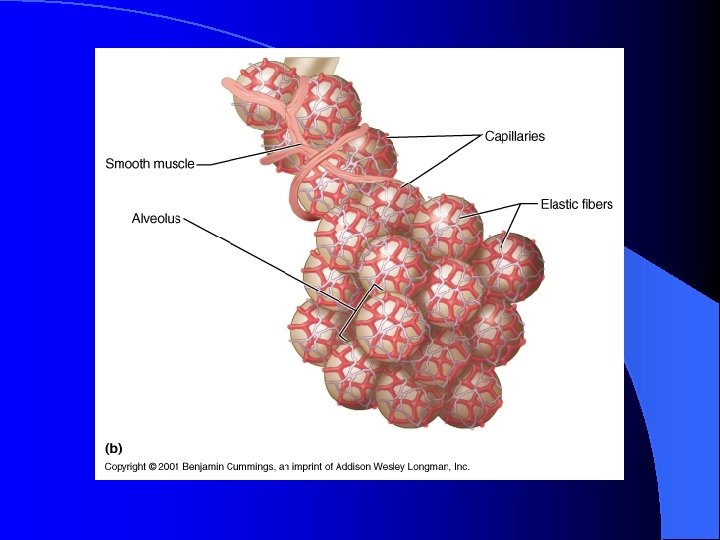
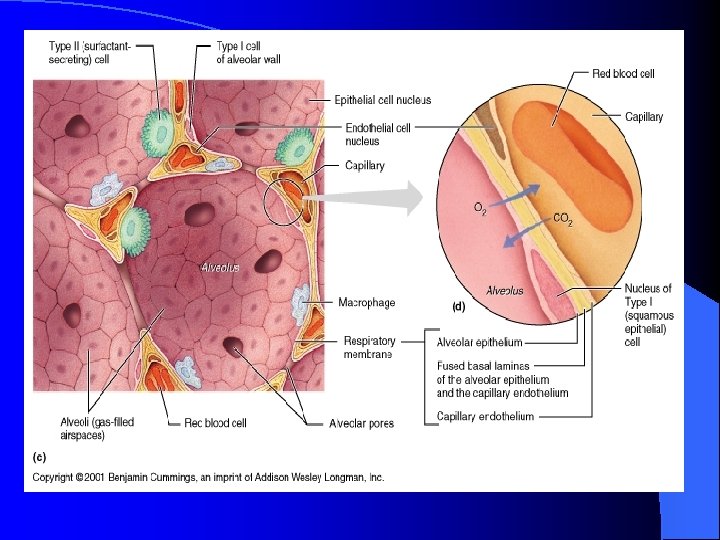
Alveoli l Clustered at the ends of the terminal bronchioles l Makes up the bulk of lung tissue l Primary function is the exchange of gases between themselves and the blood l Surrounded by elastic fibers – Creates Elastic Recoil
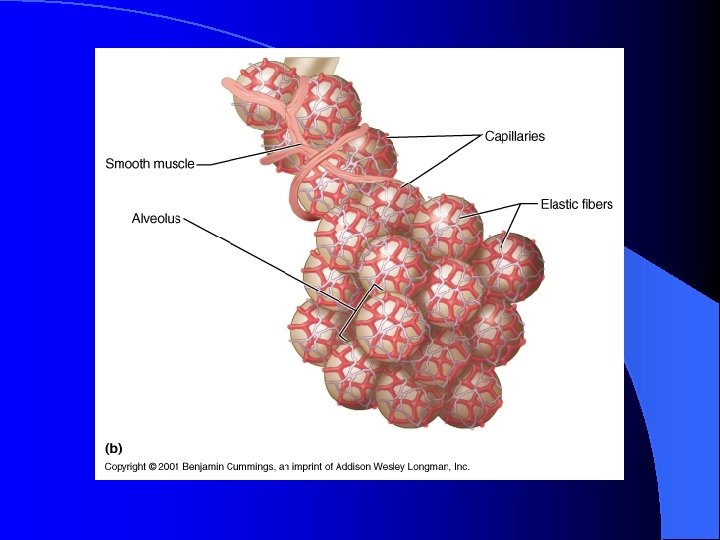
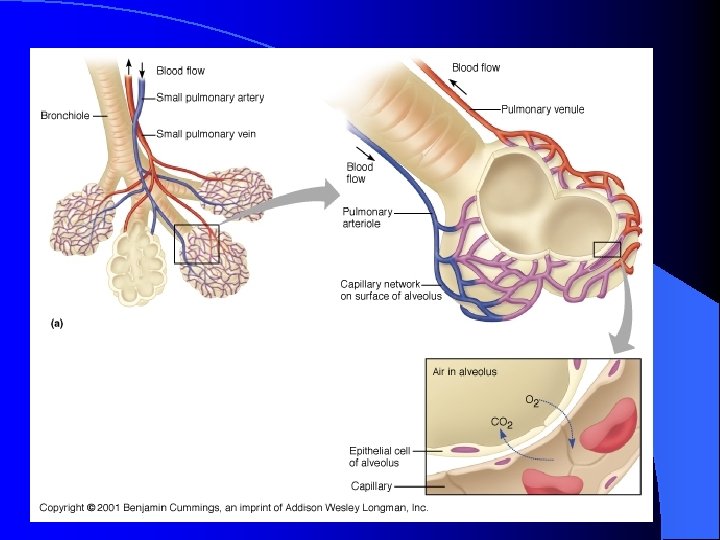
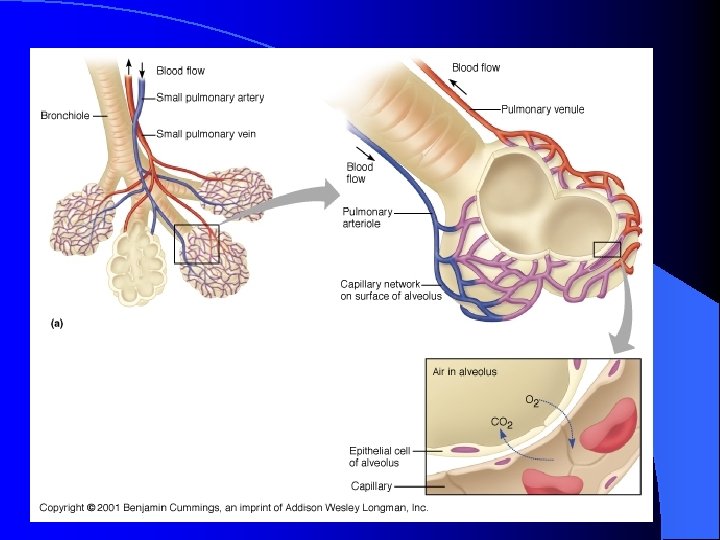
Capillaries l The alveoli are closely associated with an extensive network of capillaries – Blood vessels cover 80 -90% of the alveolar surface forming a continuous “sheet” of blood in close contact with the air-filled alveoli
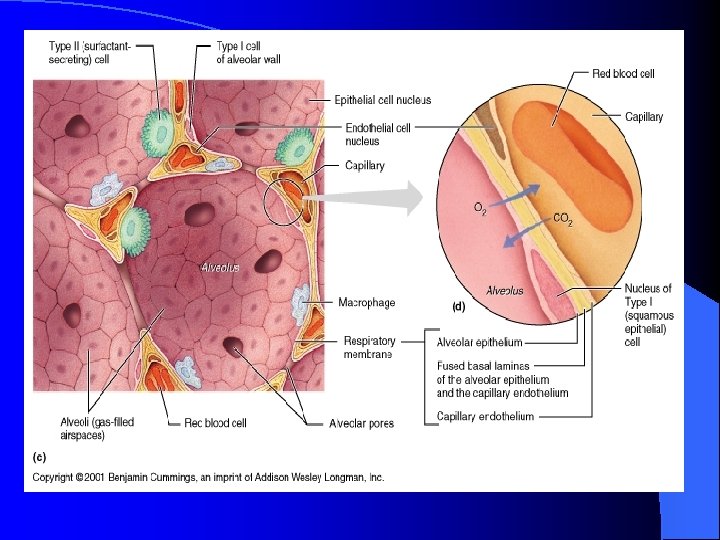
Respiratory Membrane l Consists of – The Wall of the Alveoli – The Respiratory Space This is a fluid filled space l Pneumonia may cause the space to fill with more fluid than normal l – This decreases the ability to exchange gases – The Wall of the Capillary
Gas Laws l At sea level normal atmospheric pressure is 760 mm. Hg – On top of Mt. Everest Patm = 153 mm. Hg
Dalton’s Law l The total pressure exerted by a mixture of gases is the sum of the pressures exerted by the individual gases – 78% N 2 – 21% O 2 – 1% CO 2 l Partial Pressure of gases – The pressure of a single gas in a mixture
Gas Law The total pressure of a mixture of gases, is the sum of the pressures of the individual gases (Dalton’s Law) l Gases, singly or in a mixture, move from areas of higher pressure to areas of lower pressure l If the volume of a container of gas changes, the pressure of the gas will change in an inverse manner (Boyle’s Law) l
Dalton’s Law l To find the partial pressure of any one gas in a sample of air, multiply the atmospheric Pressure (Patm) by the gas’s relative contribution (%) to Patm. – Partial pressure of an atmospheric gas = l Patm X % of gas in atmosphere – Partial pressure of oxygen = 760 mm. Hg X 21% l PO 2 = 760 X 0. 21 = 160 mm. Hg
Gases Move from High Pressure to Low Pressure l Air flow occurs whenever there is a pressure gradient
Boyle’s Law l The pressure exerted by a gas or mixture of gases in a sealed container is created by the collisions of moving gas molecules with the walls of the container and with each other. – P 1 V 1 = P 2 V 2 l An increase in volume will create a decrease in pressure and a decrease in volume will create an increase in pressure
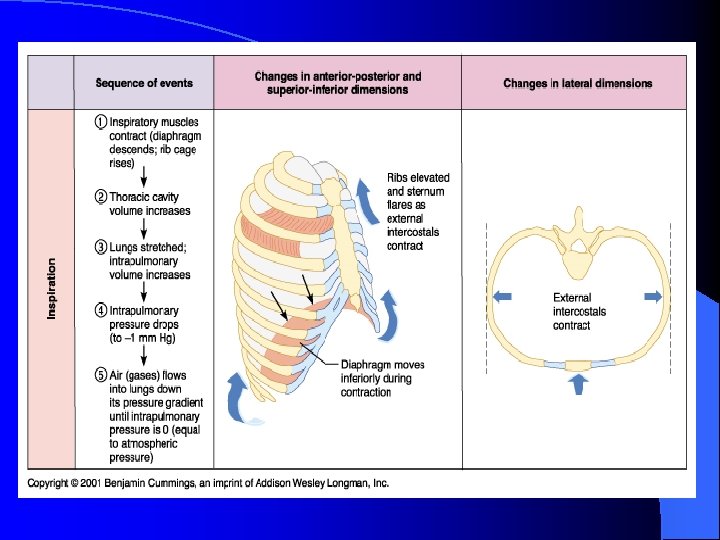
Boyle’s Law l Changes in the volume of the chest cavity during ventilation cause pressure gradients that create air flow – When the chest volume increases, the alveolar pressure falls, and air flows into the respiratory system l When the chest volume decreases, the alveolar pressure rises, and air flows out into the atmosphere
Alveoli Composed of a single layer of epithelium called Type I cells l Type II alveolar cells l – Secretes surfactant – Surfactant decreases the surface tension of the water within the alveoli – Coats the inside of the alveoli – Cortisol causes the maturation of the type II cells in the fetal stage of development l Dust Cells – Phagocytes
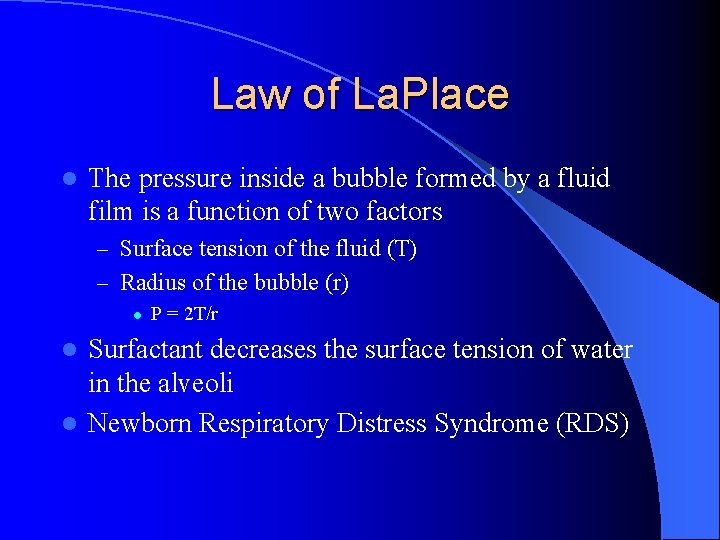
Law of La. Place l The pressure inside a bubble formed by a fluid film is a function of two factors – Surface tension of the fluid (T) – Radius of the bubble (r) l P = 2 T/r Surfactant decreases the surface tension of water in the alveoli l Newborn Respiratory Distress Syndrome (RDS) l
Air Flow l Flow = changes in P / R – P = Pressure – R = Resistance to Flow l Air flow in response to a pressure gradient l The flow decreases as the resistance to flow increases
Pressure in the System l Alveolar Pressure – Pressure in the air spaces of the lungs l Intrapleural Pressure – Pressure in the pleural fluid l Intrapulmonary Pressure – Pressure within the lungs as a whole l Atmospheric Pressure – Pressure in the atmosphere due to a column of air up to the stratosphere
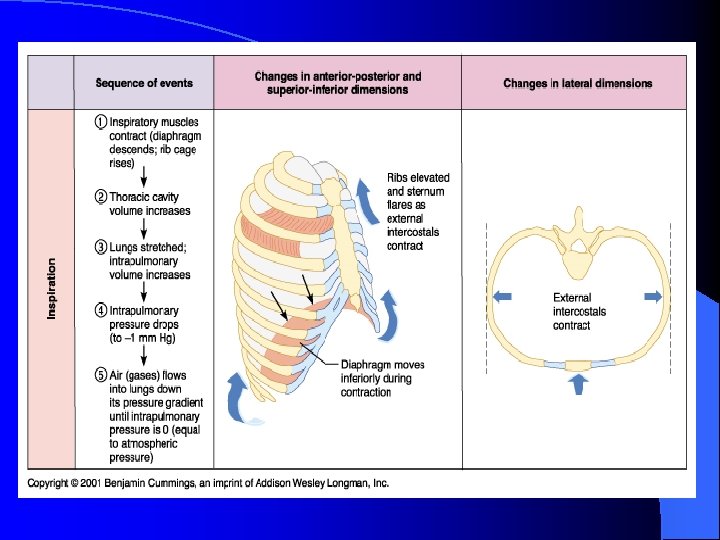
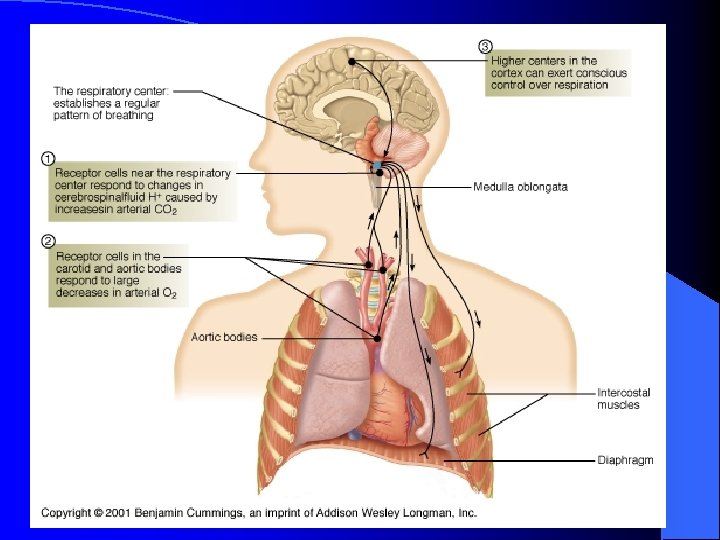
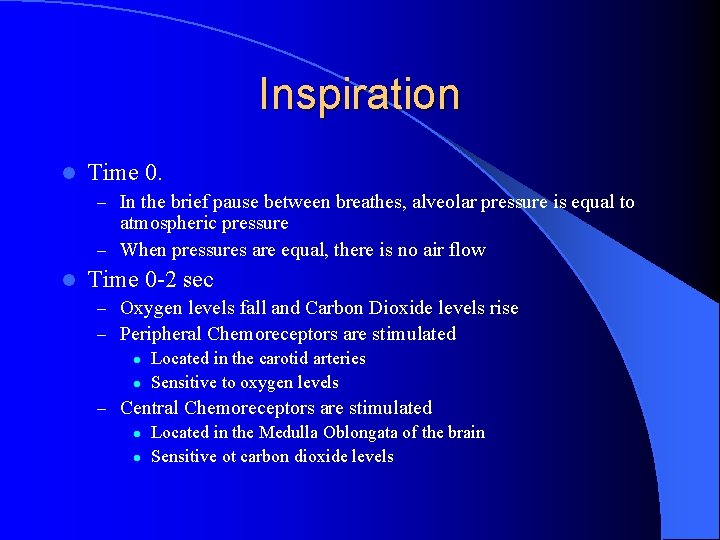
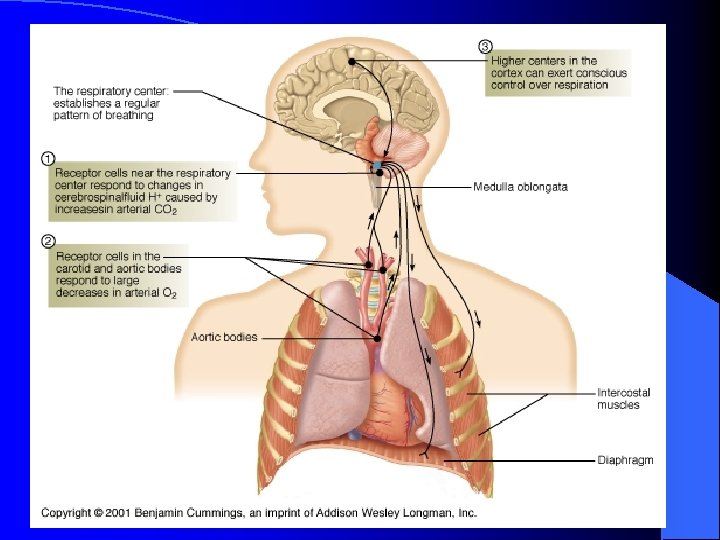
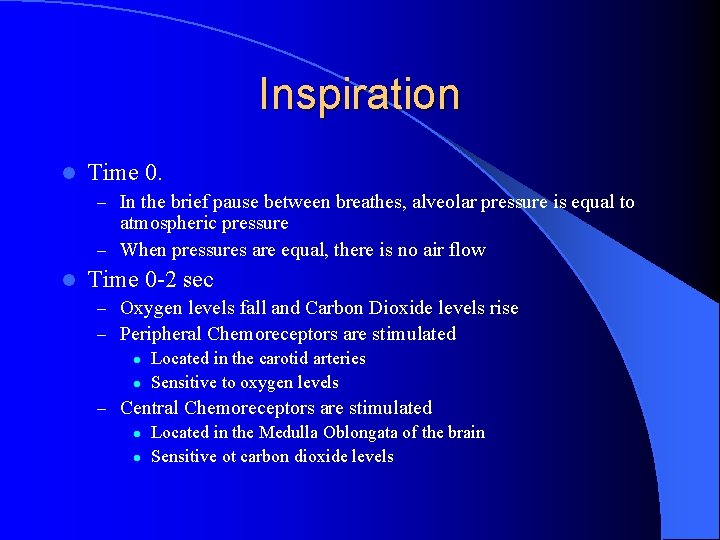
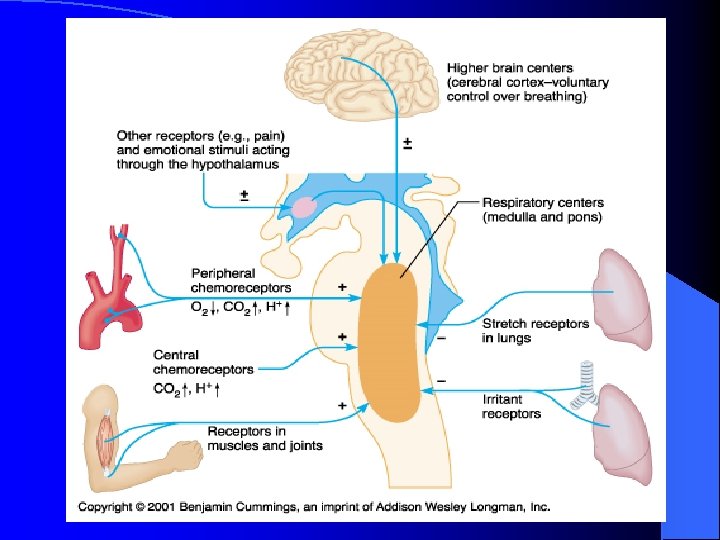
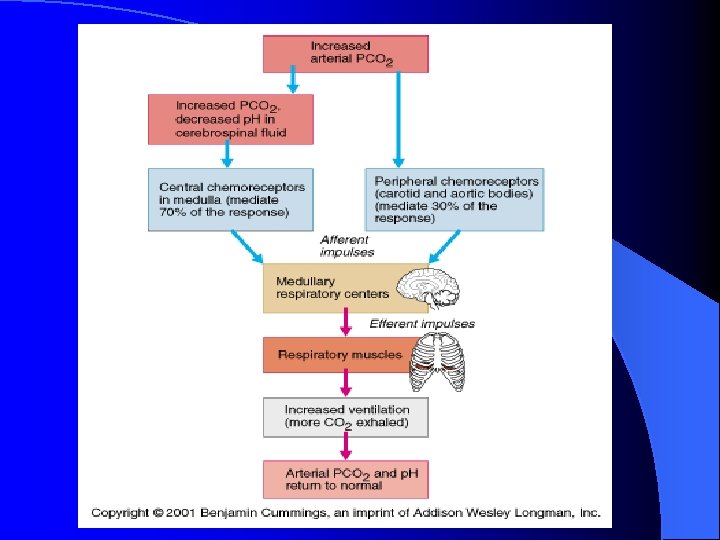
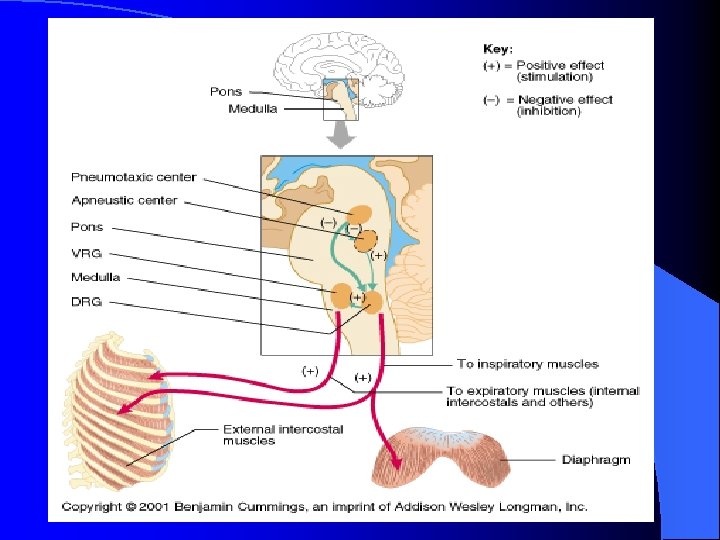
Inspiration l Time 0. – In the brief pause between breathes, alveolar pressure is equal to atmospheric pressure – When pressures are equal, there is no air flow l Time 0 -2 sec – Oxygen levels fall and Carbon Dioxide levels rise – Peripheral Chemoreceptors are stimulated l Located in the carotid arteries l Sensitive to oxygen levels – Central Chemoreceptors are stimulated l Located in the Medulla Oblongata of the brain l Sensitive ot carbon dioxide levels
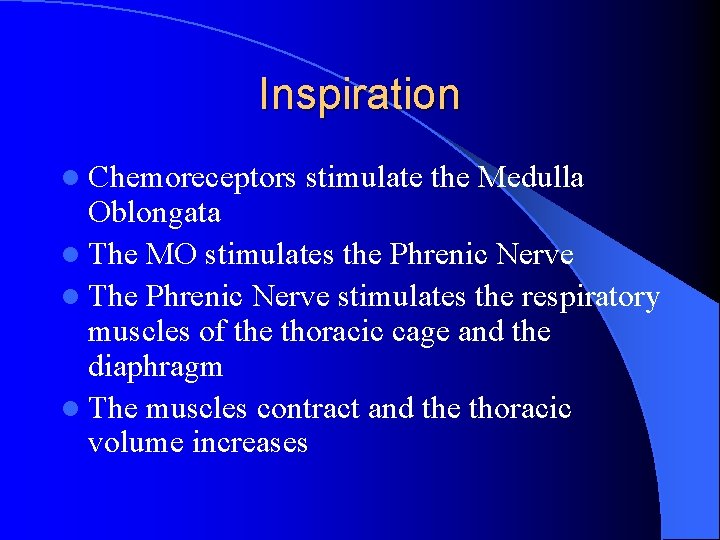
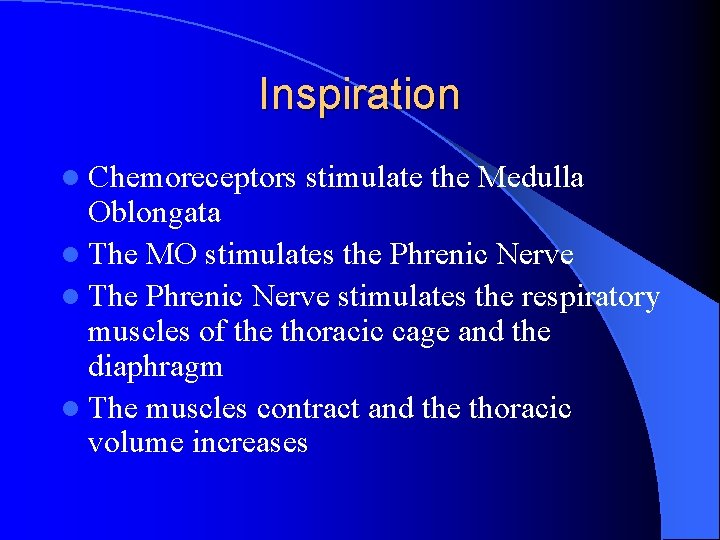
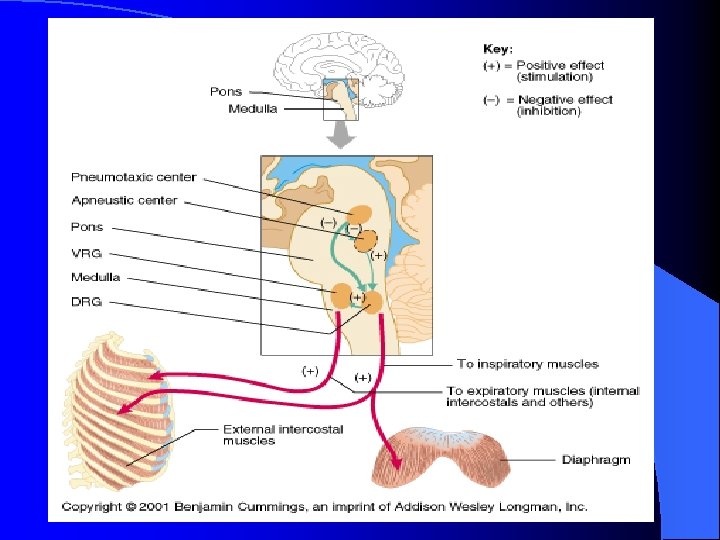
Inspiration l Chemoreceptors stimulate the Medulla Oblongata l The MO stimulates the Phrenic Nerve l The Phrenic Nerve stimulates the respiratory muscles of the thoracic cage and the diaphragm l The muscles contract and the thoracic volume increases
Inspiration l When thoracic volume increases then alveolar pressure fall approximately 4 mm. Hg below atmospheric pressure l Air flows from high pressure to low pressure until the pressures reach equilibrium
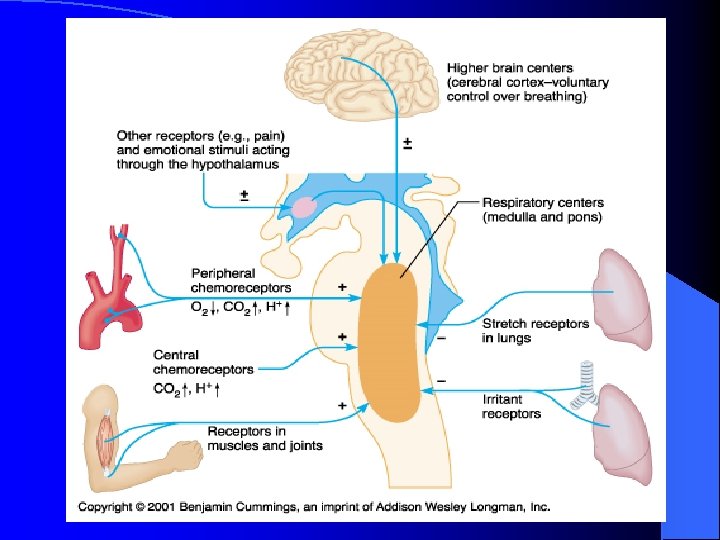
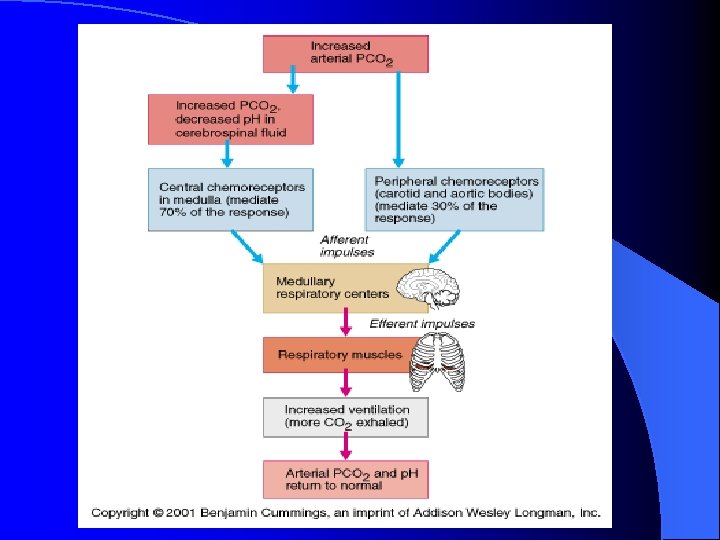
Exhalation l Time 2 -4 sec: – As lung and thoracic volumes decrease air pressure in the lungs increases until the pressures equal equilibrium – Stretch receptors in the lung tissue are stimulated – Stretch receptors send information to the MO and this stops the phrenic nerve stimulation – Respiratory muscles relax l Time 4 sec: – Elastic Recoil occurs – Alveolar pressure is now higher than atmospheric pressure due to a decrease in lung volume – Air leaves the lungs until pressures reach equilibrium
Intrapleural Pressure Changes During Ventilation l The lungs are “stuck” to the thoracic cage by the cohesive forces exerted by the fluid between the two pleural membranes l If the thoracic cage moves, the lungs move with it
Intrapleural Pressure l The pressure between the pleural membranes is normally subatmospheric l The combination of the outward pull of the thoracic cage and in inward recoil of the elastic lungs creates a subatmospheric intrapleural pressure of about -3 mm. Hg
What happens to subatmospheric intrapleural pressure if an opening is made between the sealed pleural cavity and the atmosphere?
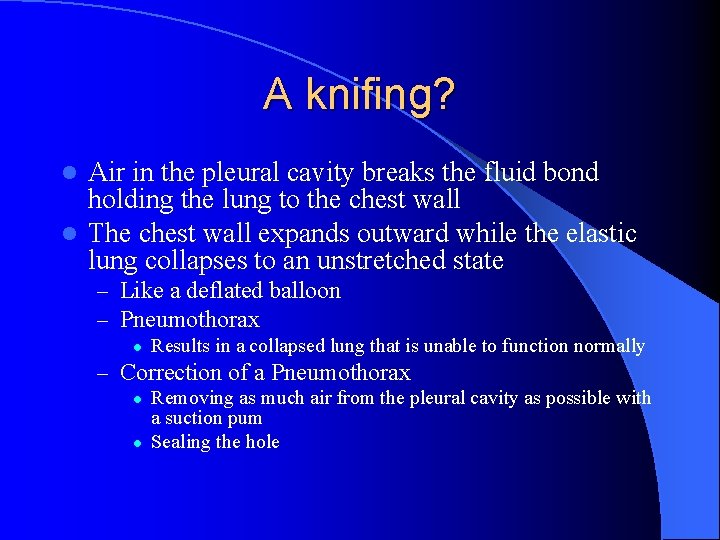
A knifing? Air in the pleural cavity breaks the fluid bond holding the lung to the chest wall l The chest wall expands outward while the elastic lung collapses to an unstretched state l – Like a deflated balloon – Pneumothorax l Results in a collapsed lung that is unable to function normally – Correction of a Pneumothorax l l Removing as much air from the pleural cavity as possible with a suction pum Sealing the hole
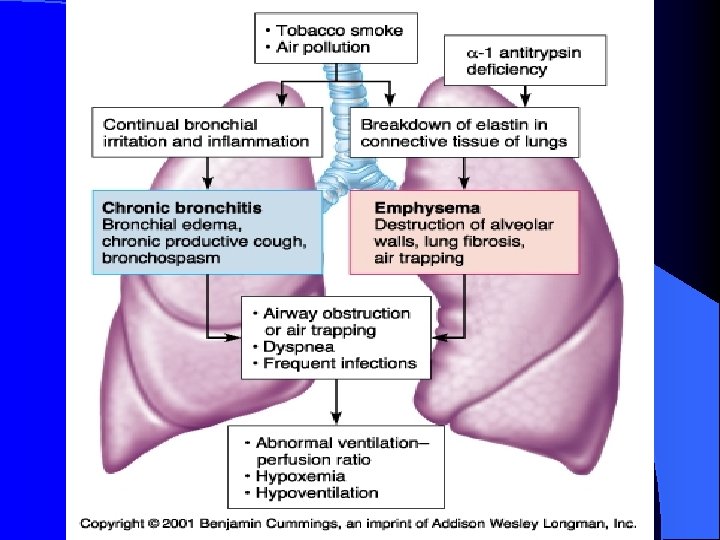
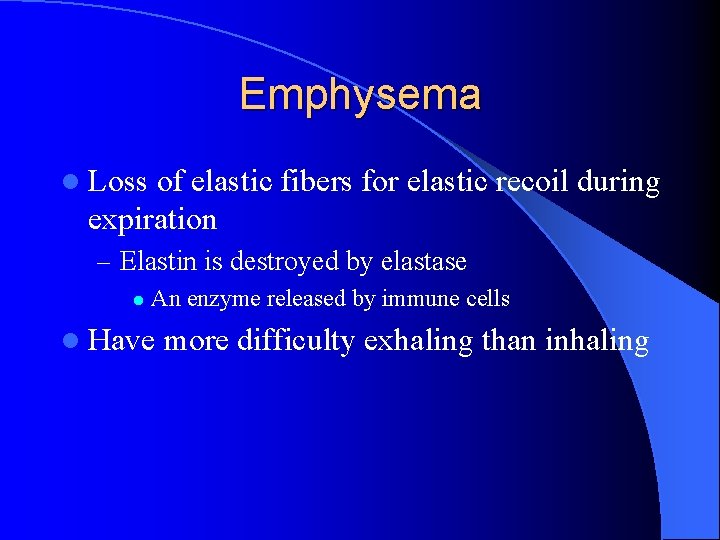
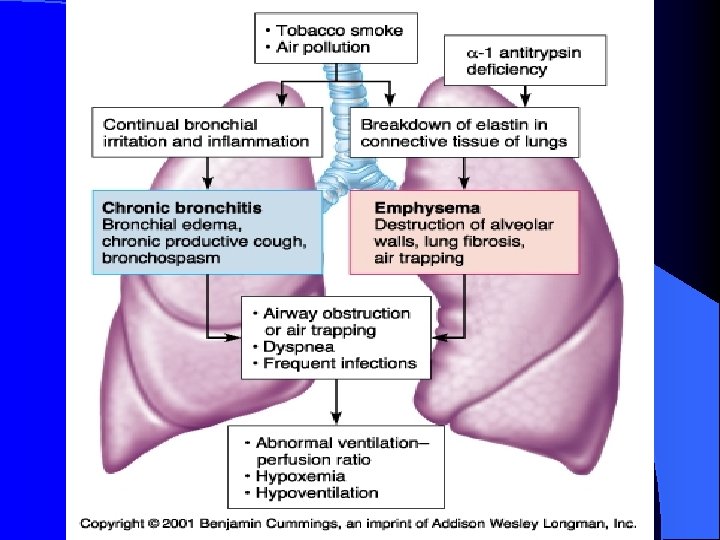
Emphysema l Loss of elastic fibers for elastic recoil during expiration – Elastin is destroyed by elastase l An enzyme released by immune cells l Have more difficulty exhaling than inhaling
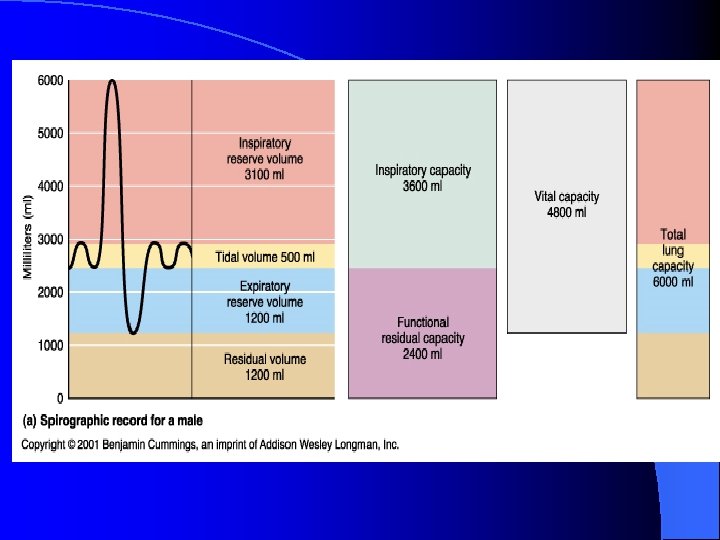
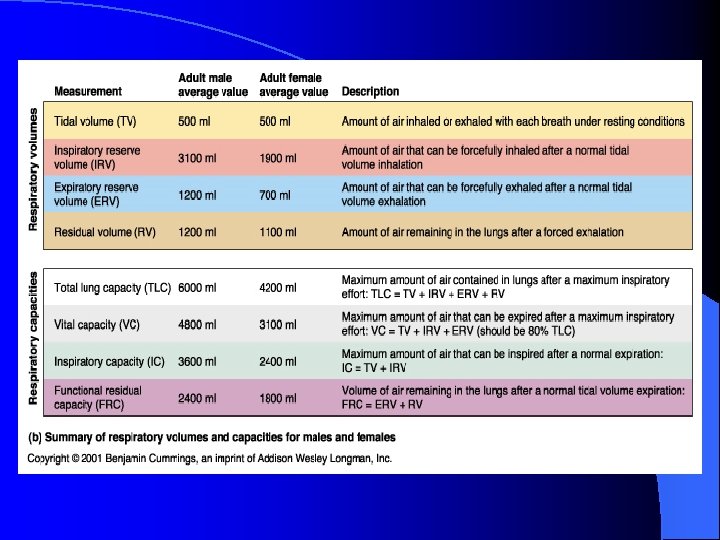
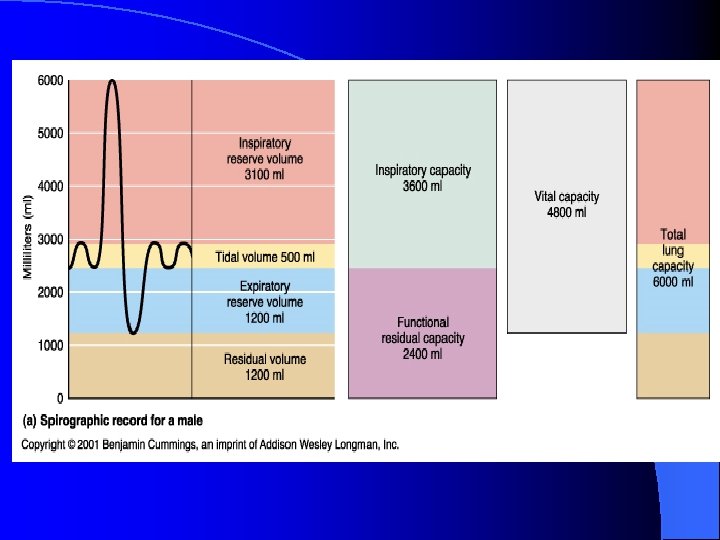
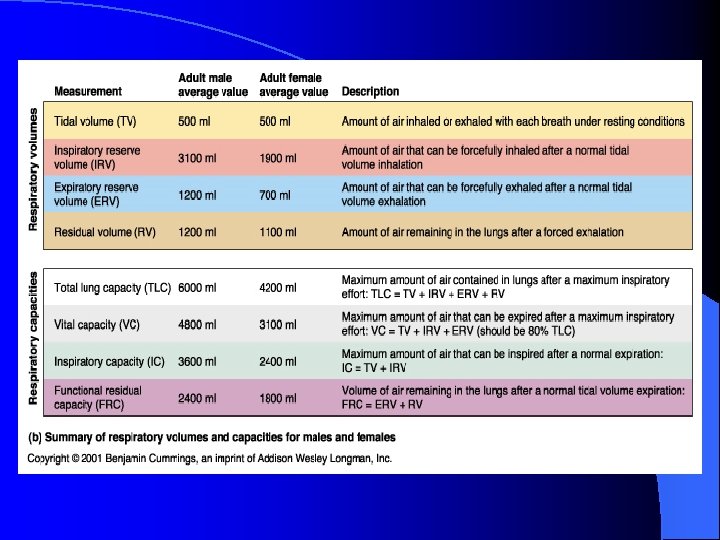
Ventilation l Lung Volumes – Use a spirometer to measure pulmonary function l Tidal Volume l Inspiratory Reserve Volume l Expiratory Reserve Volume l Residual Volume
Tidal Volume l Breathing Quietly – The volume of air that moves during a single inspiration or expiration (VT). l Average tidal volume during quiet breathing is about 350 – 500 ml of air
Inspiratory Reserve Volume (IRV) l At the end of a quiet inspiration, take in as much additional air as you possibly can – About 3000 ml in a 70 kg male
Expiratory Reserve Volume (ERV) l Stop at the end of a normal exhalation, then exhale as much air as you possibly can l This is a forceful exhalation – Average is about 1100 ml
Residual Volume (RV) l Cannot be measured direction l Even if you blow out as much air as you can, air still remains in the lungs and the airways – About 1200 ml
Lung Capacities l The sum of two or more lung volumes – Vital capacity (VC) The sum of the inspiratory reserve volume, expiratory reserve volume and tidal volume l This represents the maximum amount of air that can be voluntarily moved into or out of the respiratory system with one breath l
Total Lung Capacity l Total Lung Capacity – Vital capacity + residual volume l Functional Residual Capacity – Expiratory reserve volume + residual volume
Airway Resistance l Bronchioles are collapsible tubes l Bronchoconstriction – Increases resistance to air flow and decreases the amount of fresh air that reaches the alveoli l Histamine – Bronchoconstrictor l Bronchodilators – Decreases resistance to air flow
PARASYMPATHIC INPUT l PNS is the primary neural control of bronchioles and causes bronchoconstriction l Smooth muscle in the bronchioles have β-2 receptors that respond to epinephrine and norepi – Stimulation of β-2 receptors relaxes airway smooth muscle and results in bronchodilation l Used to treat asthma or allergies
Chronic Obstructive Pulmonary Disease (COPD) l Asthma, emphysema, chronic bronchitis

INTERNAL RESPIRATION
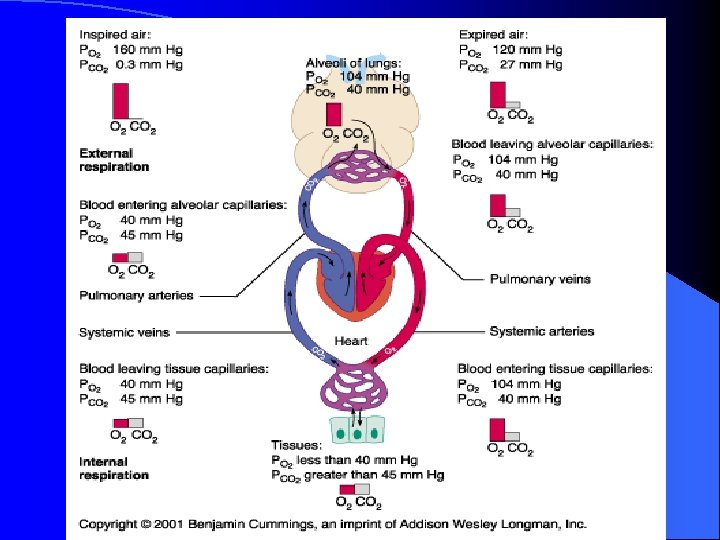
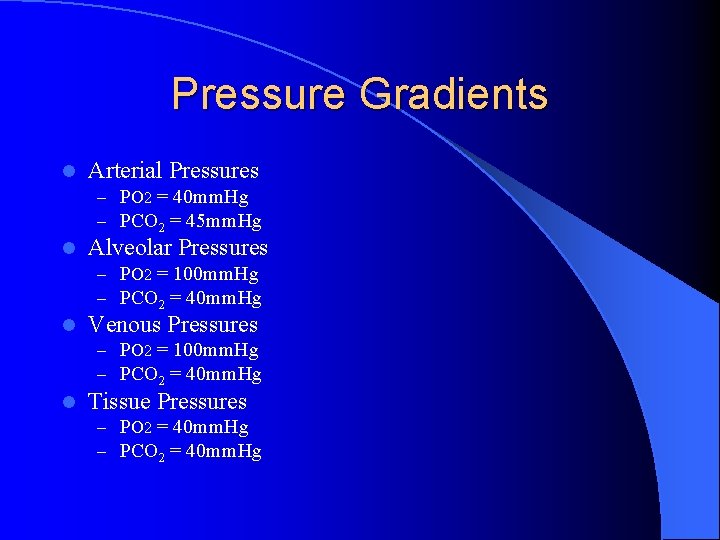
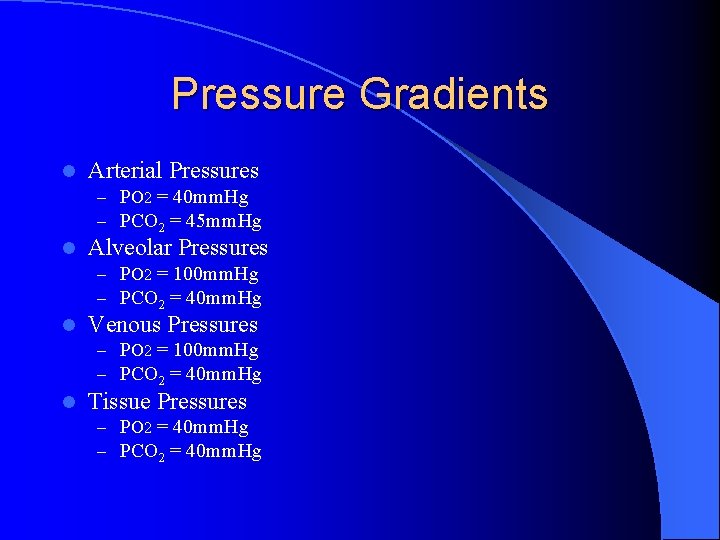
Pressure Gradients l Arterial Pressures – PO 2 = 40 mm. Hg – PCO 2 = 45 mm. Hg l Alveolar Pressures – PO 2 = 100 mm. Hg – PCO 2 = 40 mm. Hg l Venous Pressures – PO 2 = 100 mm. Hg – PCO 2 = 40 mm. Hg l Tissue Pressures – PO 2 = 40 mm. Hg – PCO 2 = 40 mm. Hg
Hemoglobin l Oxygen is transported two – Dissolved in the plasma – Bound to hemoglobin ways in the blood l Mean Corpuscular Hemoglobin – Counting the RBC’s and quantifying the amount of hemoglobin per RBC l Hemoglobin Concentration or %
Hemoglobin l One hemoglobin molecule binds up to four oxygen molecules – Percent oxygen saturation l Globin – Proteins in the hemoglobin Alpha, beta, gamma and delta types l Adults have 2 alpha and 2 bets l Fetal Hb l – Two gamma and two alpha
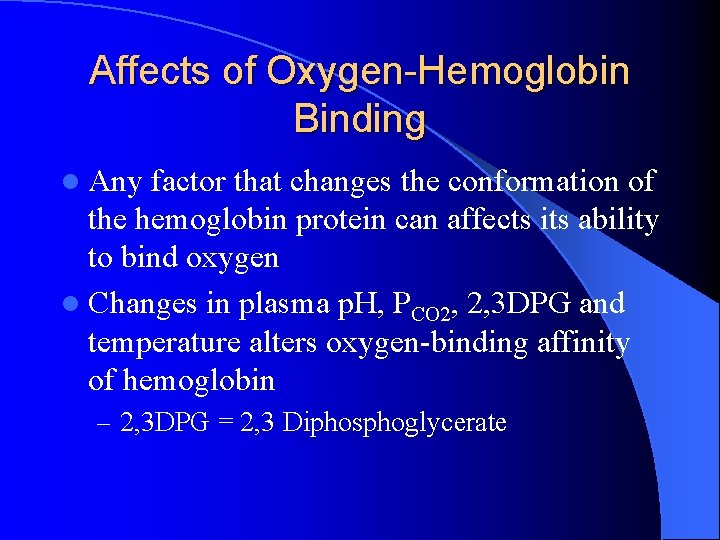
Affects of Oxygen-Hemoglobin Binding l Any factor that changes the conformation of the hemoglobin protein can affects its ability to bind oxygen l Changes in plasma p. H, PCO 2, 2, 3 DPG and temperature alters oxygen-binding affinity of hemoglobin – 2, 3 DPG = 2, 3 Diphosphoglycerate
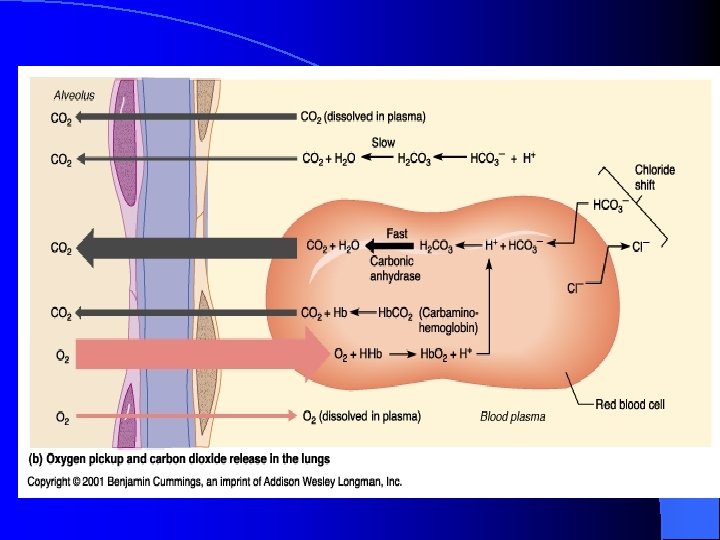
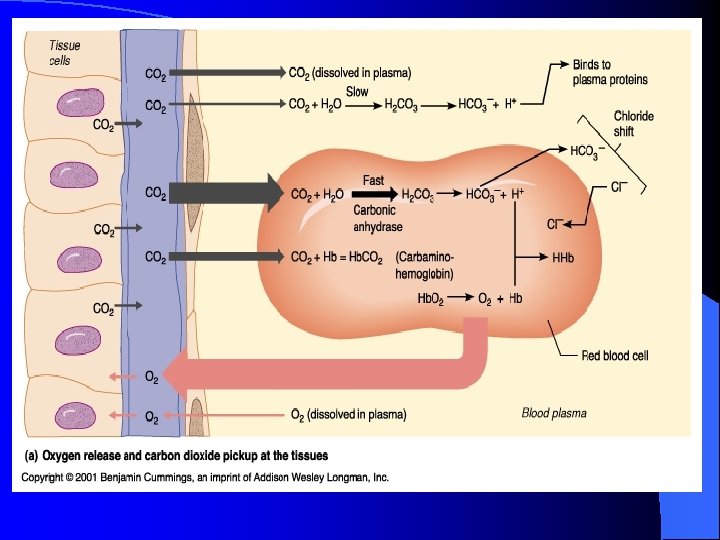
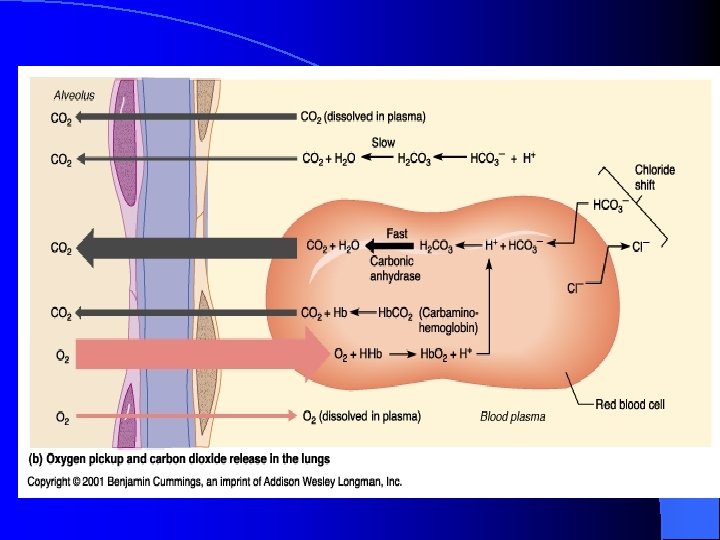
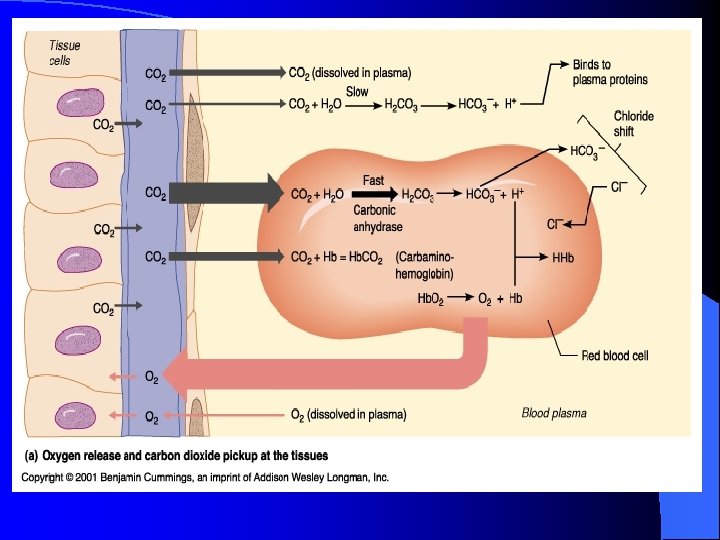
Carbon Dioxide Transportation l 7% of the CO 2 is carried by venous blood dissolved in the blood l 93% diffuses into red blood cells, – 70% is converted to bicarbonate ions HCO 3– 23% binds to hemoglobin as carbaminohemoglobin
Hydrogen Ion Transportation l Hemoglobin binds hydrogen ions – Prevents large shifts in the body’s p. H – Too many hydrogen ions in the blood may cause respiratory acidosis l This is caused by an increase in CO 2 levels in the blood
l H 2 O + CO 2 = H 2 CO 3 = H+ + HCO 3 - l. Carbonic Anyhydrase
What happens to plasma p. H during hyperventilation? How does this change in p. H affect oxygen binding at the lungs when PO 2 is decreased? How does it affect unloading of oxygen at the cells?