Physiological Assessment of Coronary Artery Disease FFRIFR DR





























- Slides: 67

Physiological Assessment of Coronary Artery Disease FFR/IFR DR SURESH S Senior resident MCH CALICUT
Structure & Function of the Coronary circulation • Epicardial arteries (>400 μm in diameter) – Serve a conduit artery function, • Coronary resistance – Resistance arteries (100 to 400 μm), – Arterioles (>100 μm), . • Capillary density – Average intercapillary distance of 17 μ m

The Coronary blood flow • Oxygen extraction at rest is around 70 % • Increase in oxygen demand – Is met by increase in coronary blood flow – Dilation of microcirculation • Coronary blood flow – At rest is 250 ml/min – Stress upto 5 times
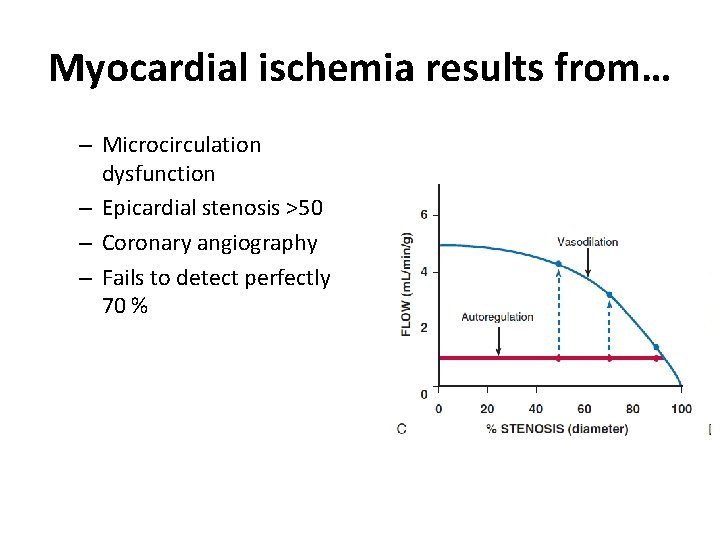
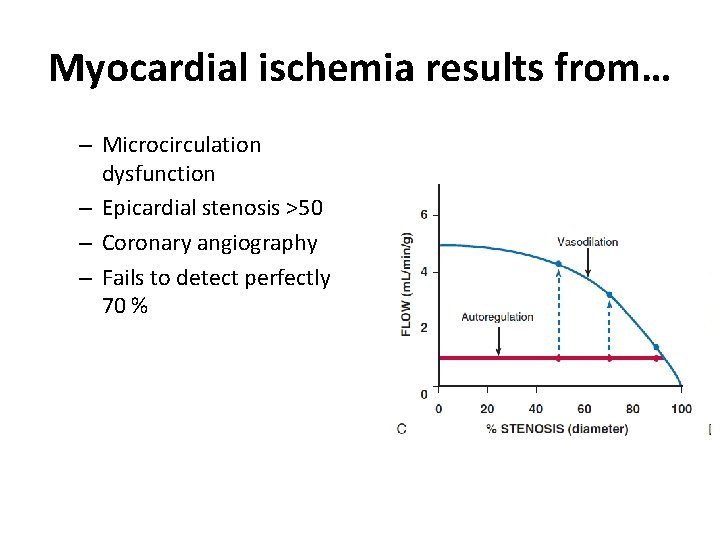
Myocardial ischemia results from… – Microcirculation dysfunction – Epicardial stenosis >50 – Coronary angiography – Fails to detect perfectly 70 %
Limitations (CAG) • Highly subjective • Intermediately severe luminal narrowing (40% -70%) cannot be accurately determined • Identification of normal and diseased vessel segments is complicated by diffuse disease • Artifacts of contrast streaming • Image foreshortening • Overlapping vessels
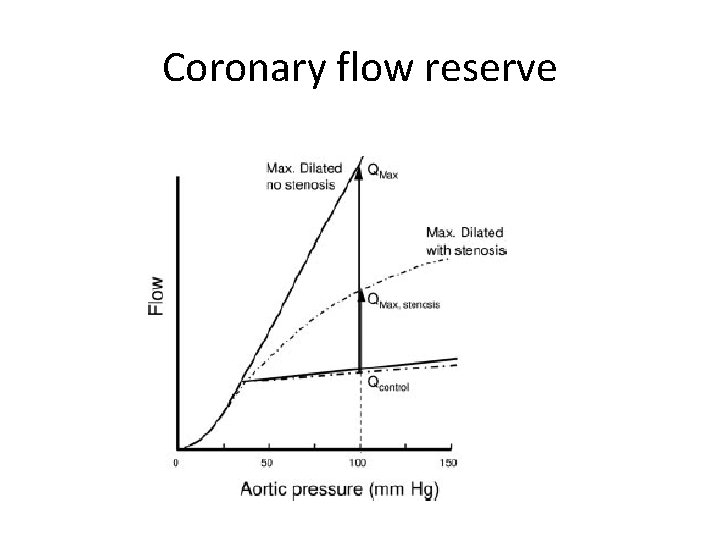
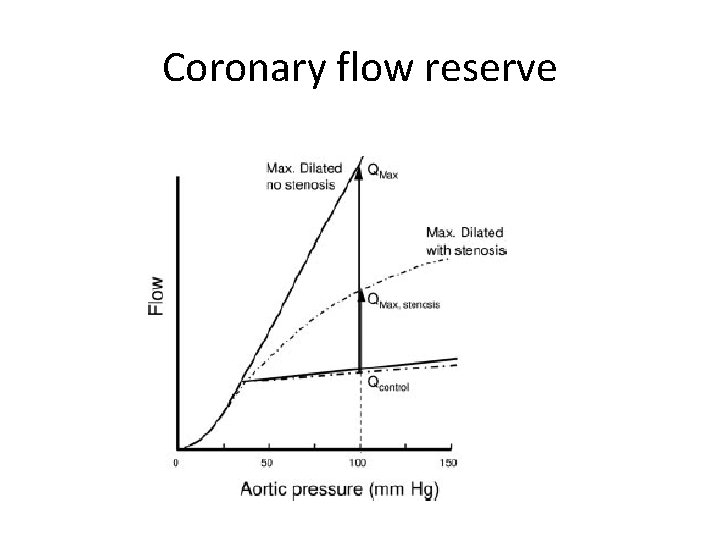
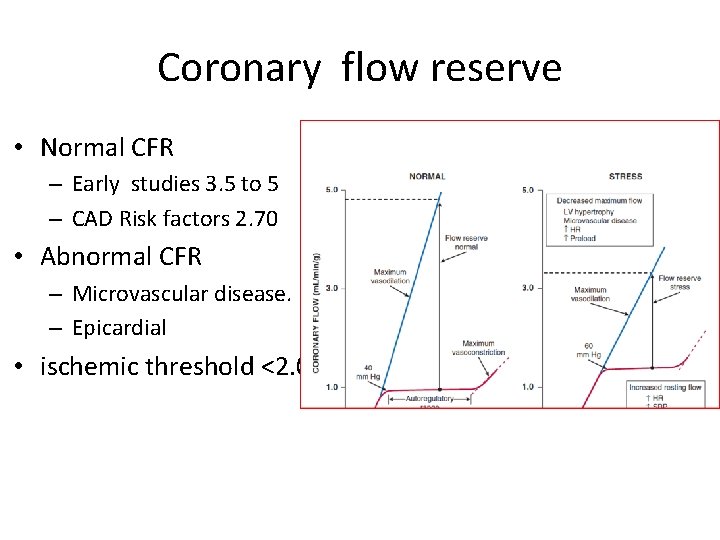
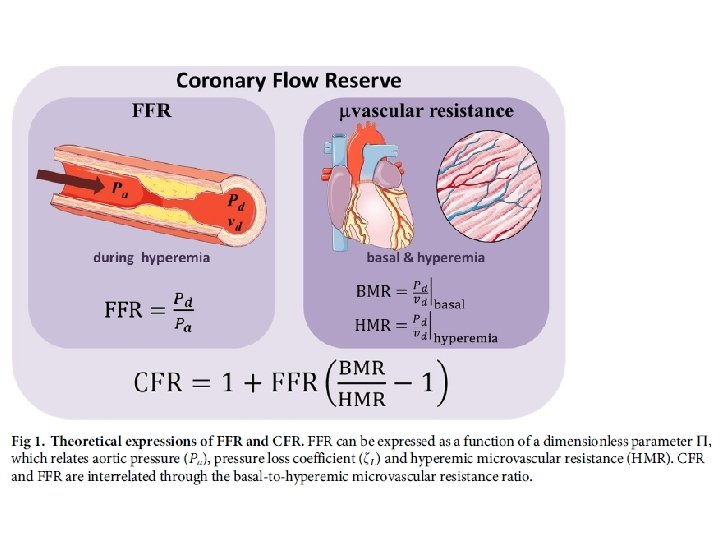
Coronary flow reserve
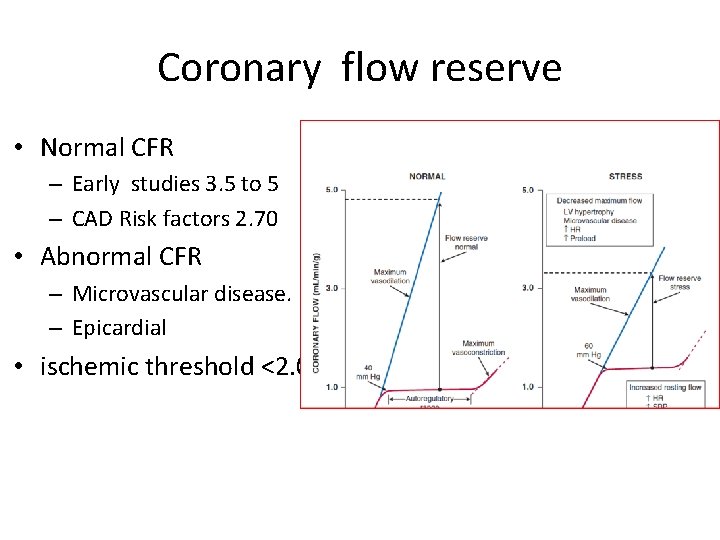
Coronary flow reserve • Normal CFR – Early studies 3. 5 to 5 – CAD Risk factors 2. 70 • Abnormal CFR – Microvascular disease. – Epicardial • ischemic threshold <2. 0.
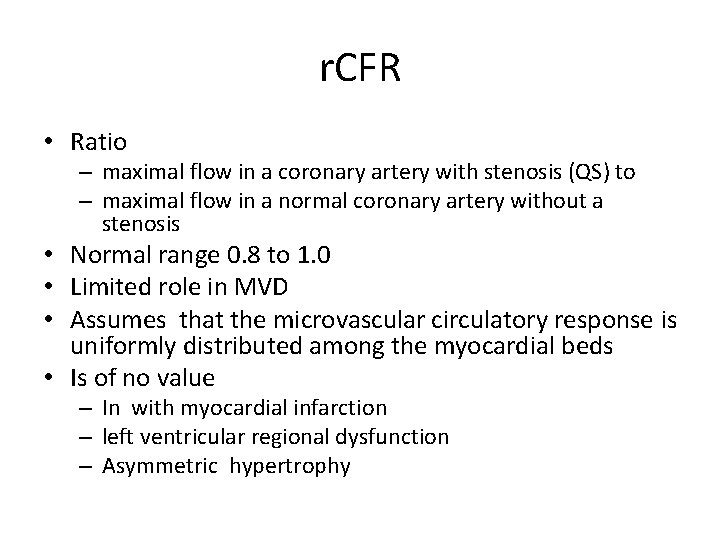
r. CFR • Ratio – maximal flow in a coronary artery with stenosis (QS) to – maximal flow in a normal coronary artery without a stenosis • Normal range 0. 8 to 1. 0 • Limited role in MVD • Assumes that the microvascular circulatory response is uniformly distributed among the myocardial beds • Is of no value – In with myocardial infarction – left ventricular regional dysfunction – Asymmetric hypertrophy
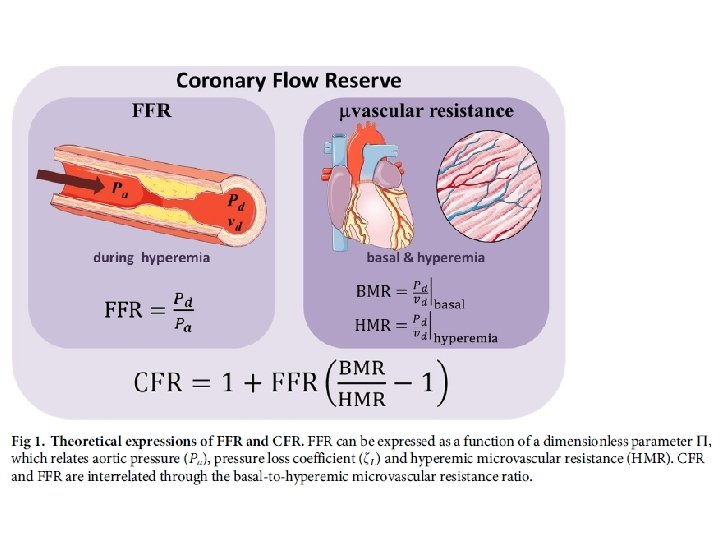

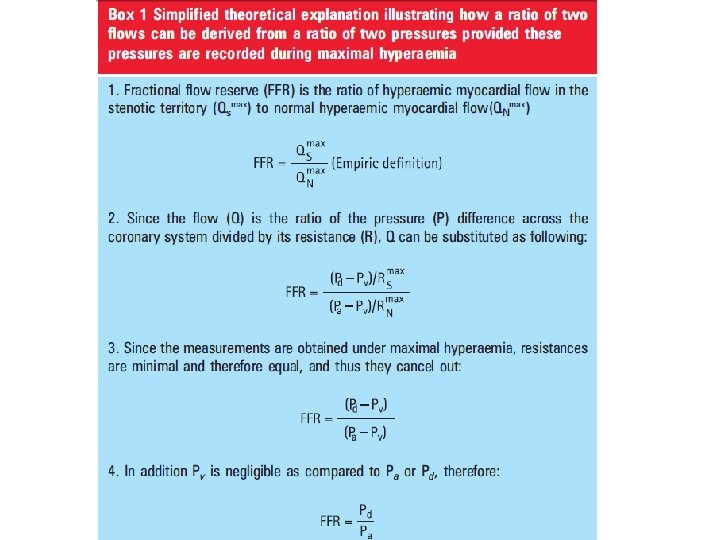
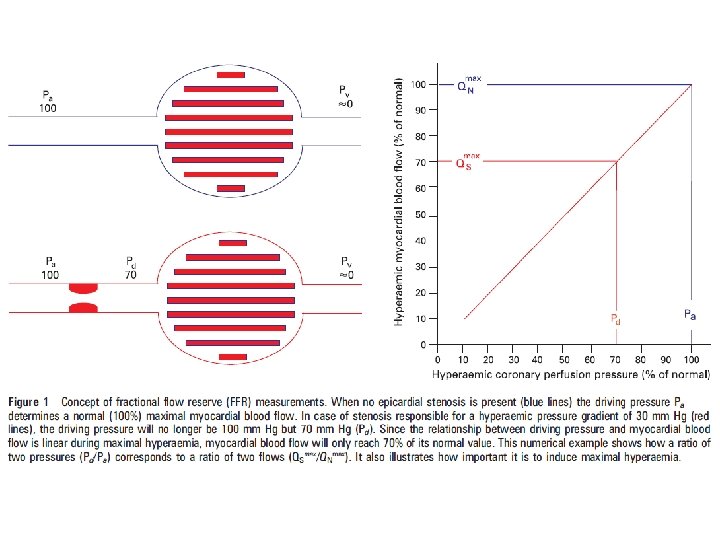

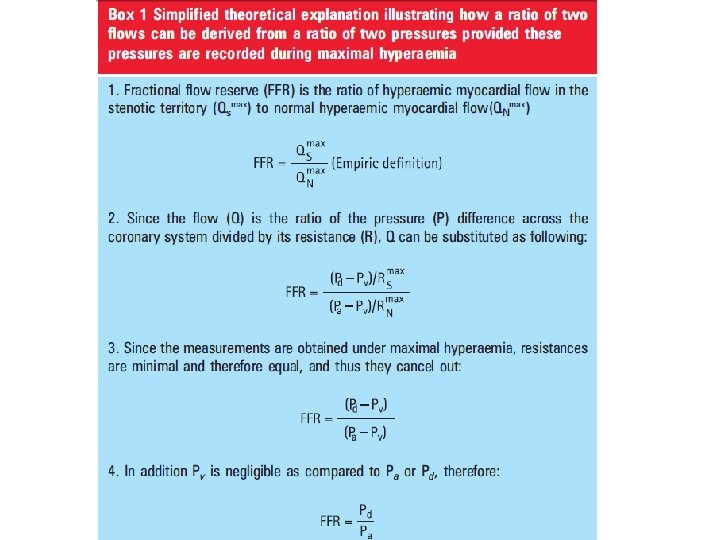
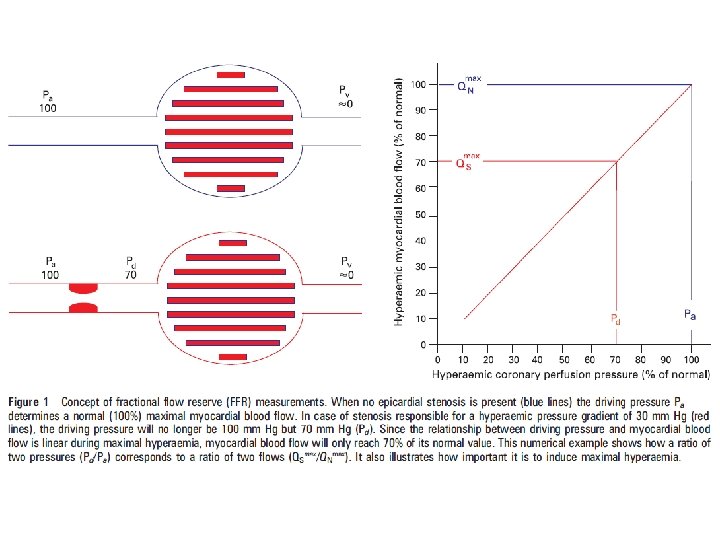
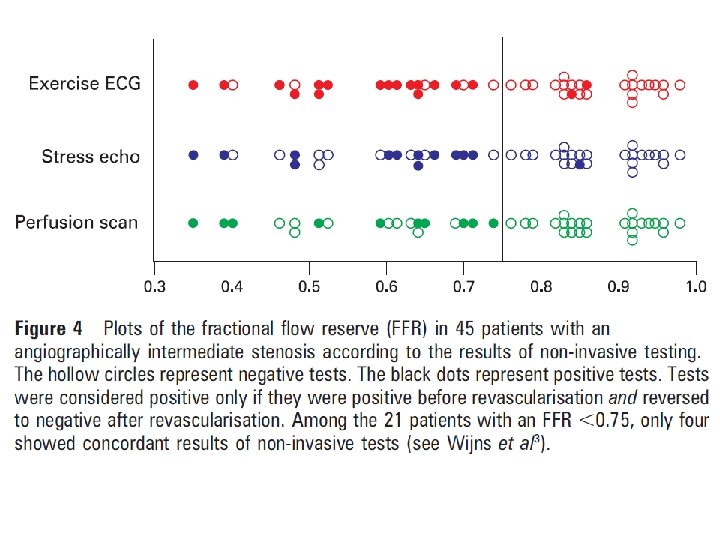
FFR • Normal value 1 • An FFR value of 0. 6 means the maximum myocardial flow across the stenosis is only 60% of what it should be without the stenosis • An FFR <0. 75 is associated with inducible ischemia (specificity, 100%), • An FFR a value >0. 80 indicates absence of inducible ischemia in the majority of patients (sensitivity, 90%).

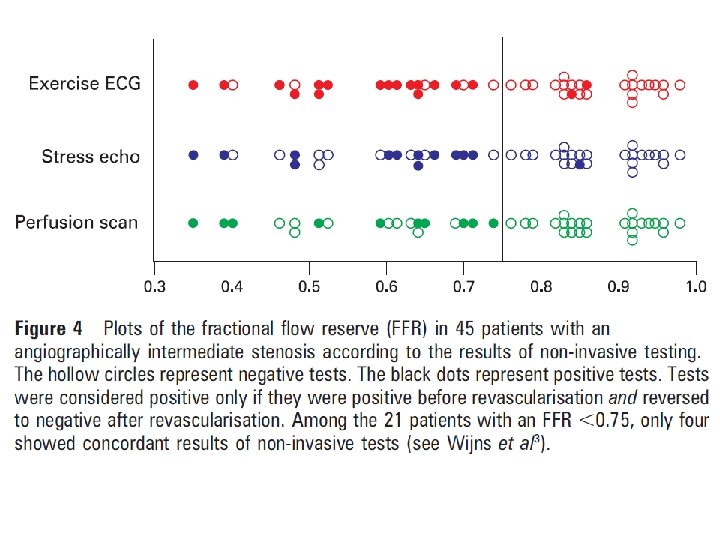

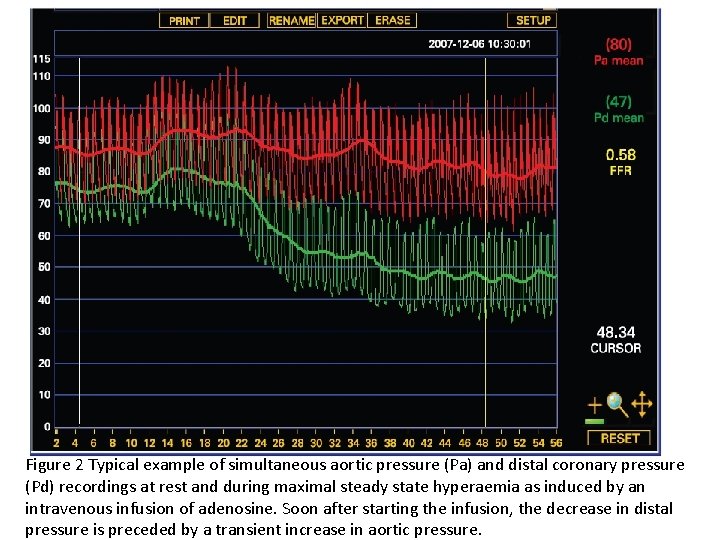
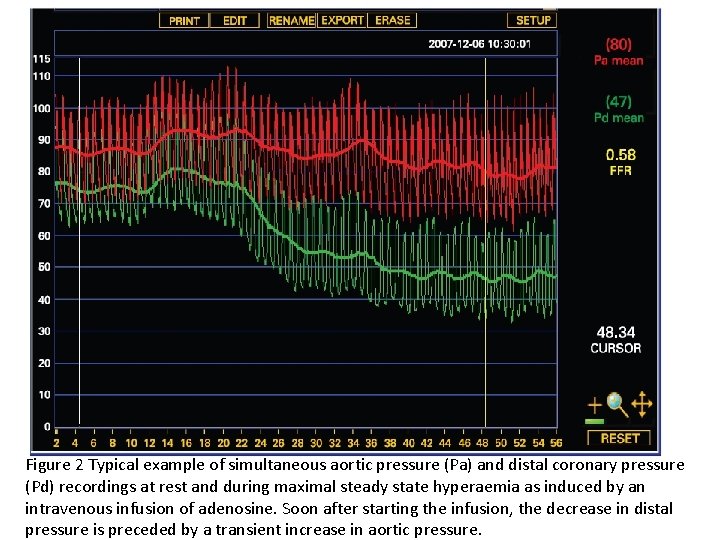
Figure 2 Typical example of simultaneous aortic pressure (Pa) and distal coronary pressure (Pd) recordings at rest and during maximal steady state hyperaemia as induced by an intravenous infusion of adenosine. Soon after starting the infusion, the decrease in distal pressure is preceded by a transient increase in aortic pressure.

FFR - advantages • Human studies did not show significant changes in FFR with changes in – heart rate, – blood pressure, – contractility. • FFR has a high reproducibility • Low intra-individual variability • FFR, unlike CFR, is independent of – gender and – CAD risk factors • It varies less with common doses of adenosine than does CFR
FFR- TECHNIQUE Catheter • Diagnostic catheters can not be used to measure FFR pressure measurements can be inaccurate & the wire manipulation is met with friction due to smaller internal diameters compared to guide catheters. • The main advantage of using guide catheters is that PCI is immediately possible if required. • Guide catheter with Side holes should not be used – It can create a false gradient between the side holes & the tip of the guide catheter creating a false Positive FFR. – Pharmacological vasodilatory agents may be flushed into the aorta instead of the coronary artery.
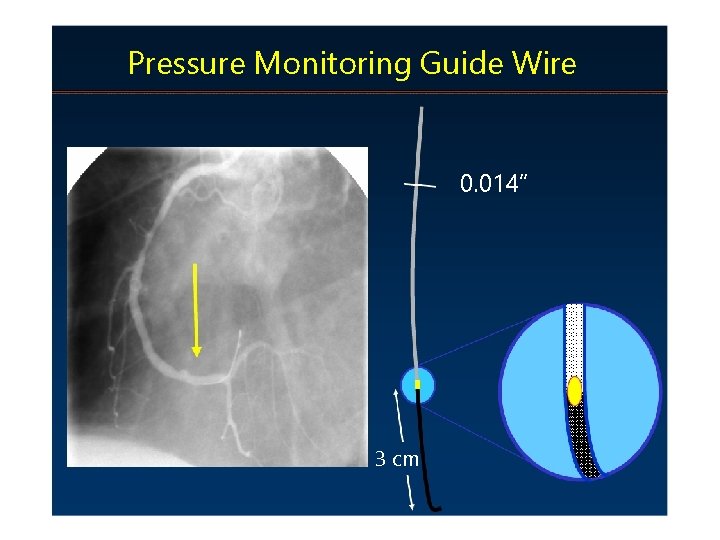
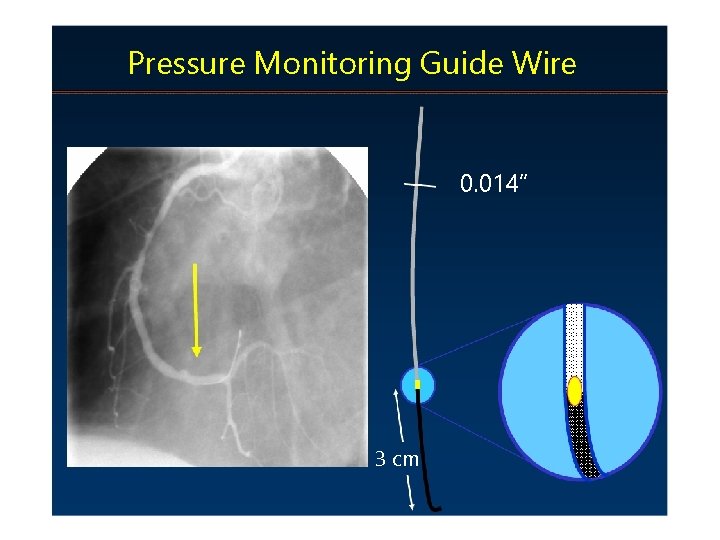
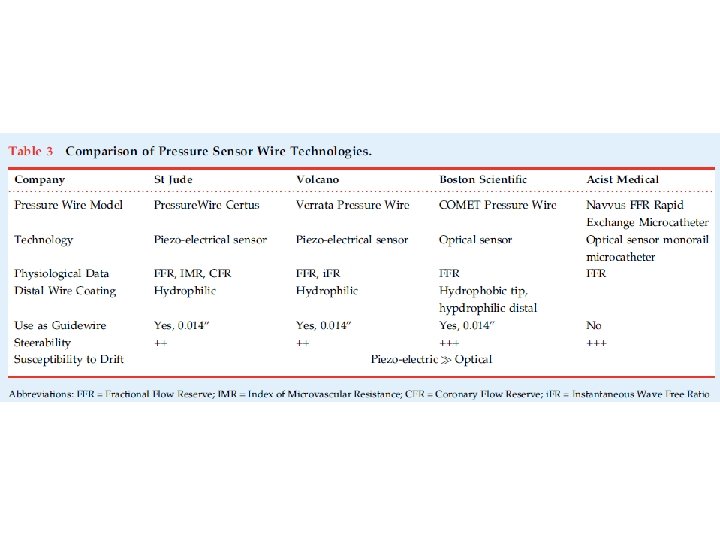
Pressure Monitoring Guide Wire 0. 014” 3 cm

Pressure Measurement Step 1: Zero the Pressure System to the Atmosphere Step 2: Insert the Pressure Sensor Guide Wire Into the Guide and Equalize the 2 Pressures Step 3: Advance the Pressure Wire Sensor Distal to the Region of Interest Step 4: Induce Maximal Hyperemia Step 5: Wire Pullback to Check for Signal Drift
Key Points of Performance of Fractional Flow Reserve (FFR) Measurements Patient preparation • Routinely obtain informed consent for FFR prior to every diagnostic coronary angiogram. • Medication for FFR identical to PCI. • Use a large calibre access in the femoral or cubital vein for peripheral adenosine application. • Beta-blockers do not need to be interrupted. • Caffeine >1 hour prior to FFR measurement has no clinically-relevant effect. • Theophylline should be interrupted 12 hours prior to FFR.

Catheter selection and positioning • Use guiding catheters (at least 5 F) without side holes. • Ascertain coaxial catheter position in the coronary ostium. • Disengage guiding catheter from ostium for pressure calibration, equalisation and recording of pd/pa if there are doubts about the catheter potentially obstructing the ostium.
Calibration • Before starting FFR measurement, ensure proper zeroing of the aortic pressure. • Flush the FFR wire, lay flat when connecting/calibrating and do not move. • Before equalisation of pressures, advance the FFR wire into the coronary artery until the pressure sensor is positioned precisely at the end of the guide catheter. • Before equalisation of pressures, flush the guide catheter in order to remove the viscous contrast agent. • Before equalisation of pressures, remove the introducer and close the haemostatic valve. • Pressure curves are typically averaged across three-to-five heartbeats. Therefore, pressure equalisation requires some time, and no artefacts should occur during that time

Positioning of the FFR wire or microcatheter • Pressure sensor should be positioned in the main vessel directly downstream the most distal leasion. • A second wire, in addition to the pressure sensor, could result in artefacts, and should therefore be avoided. • Be careful of artefacts: the sensor could interact with the vessel wall, especially in cases of a narrow vessel calibre or severe tortuosity. • Viscous contrast agent in the coronary artery can affect the gradient pd/pa. • In the case of a resting gradient <0. 80, measurement under hyperaemia is not necessarily required in order to make a clinical decision.
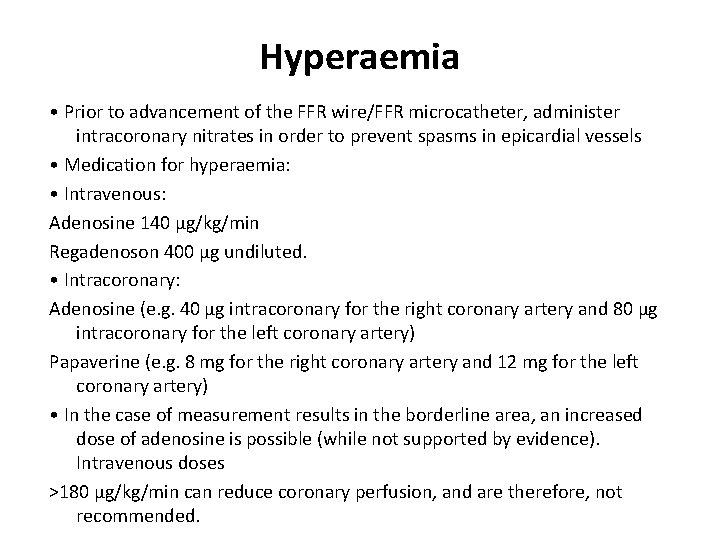
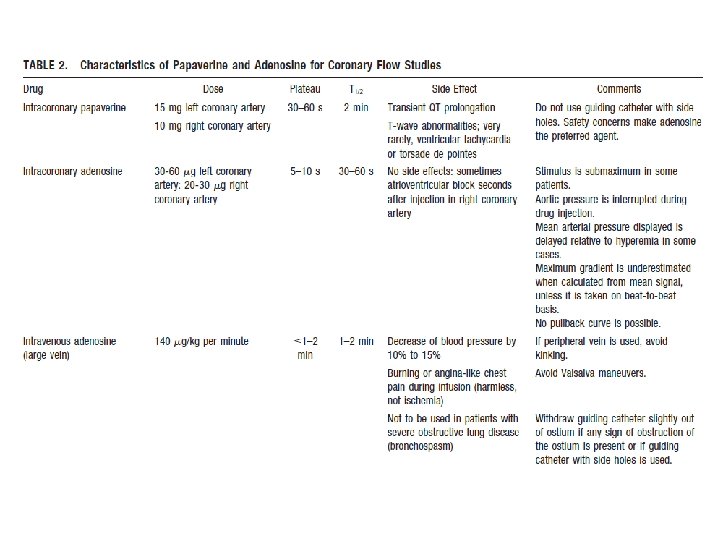
Hyperaemia • Prior to advancement of the FFR wire/FFR microcatheter, administer intracoronary nitrates in order to prevent spasms in epicardial vessels • Medication for hyperaemia: • Intravenous: Adenosine 140 μg/kg/min Regadenoson 400 μg undiluted. • Intracoronary: Adenosine (e. g. 40 μg intracoronary for the right coronary artery and 80 μg intracoronary for the left coronary artery) Papaverine (e. g. 8 mg for the right coronary artery and 12 mg for the left coronary artery) • In the case of measurement results in the borderline area, an increased dose of adenosine is possible (while not supported by evidence). Intravenous doses >180 μg/kg/min can reduce coronary perfusion, and are therefore, not recommended.

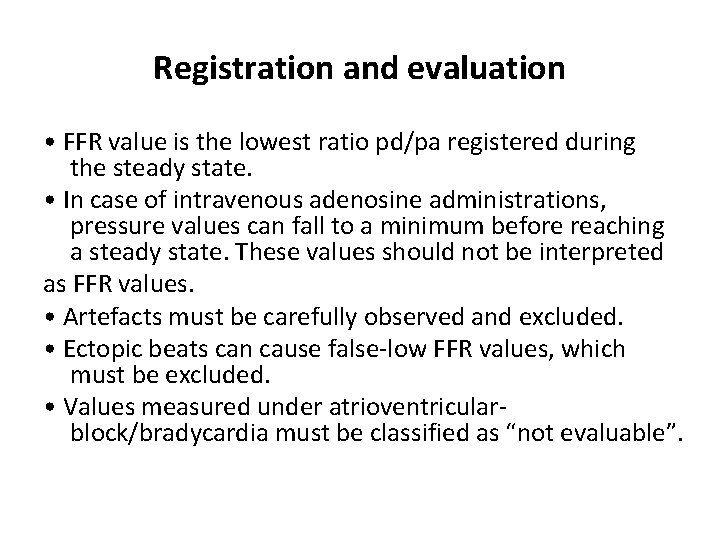
Registration and evaluation • FFR value is the lowest ratio pd/pa registered during the steady state. • In case of intravenous adenosine administrations, pressure values can fall to a minimum before reaching a steady state. These values should not be interpreted as FFR values. • Artefacts must be carefully observed and excluded. • Ectopic beats can cause false-low FFR values, which must be excluded. • Values measured under atrioventricularblock/bradycardia must be classified as “not evaluable”.
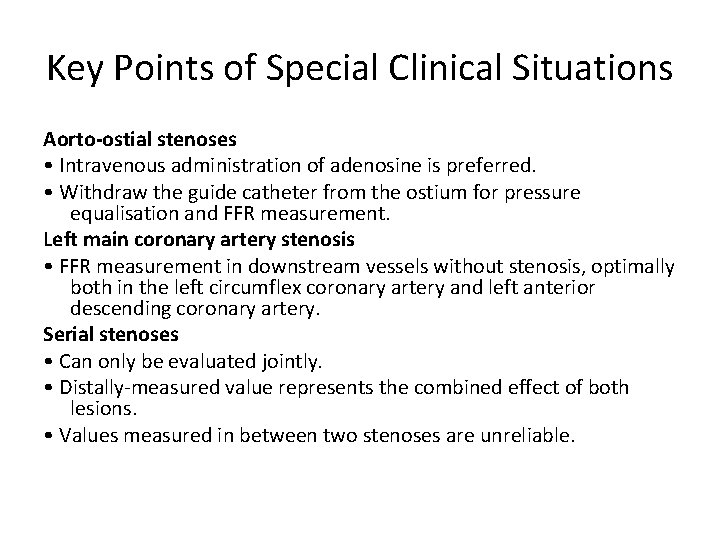
Key Points of Special Clinical Situations Aorto-ostial stenoses • Intravenous administration of adenosine is preferred. • Withdraw the guide catheter from the ostium for pressure equalisation and FFR measurement. Left main coronary artery stenosis • FFR measurement in downstream vessels without stenosis, optimally both in the left circumflex coronary artery and left anterior descending coronary artery. Serial stenoses • Can only be evaluated jointly. • Distally-measured value represents the combined effect of both lesions. • Values measured in between two stenoses are unreliable.
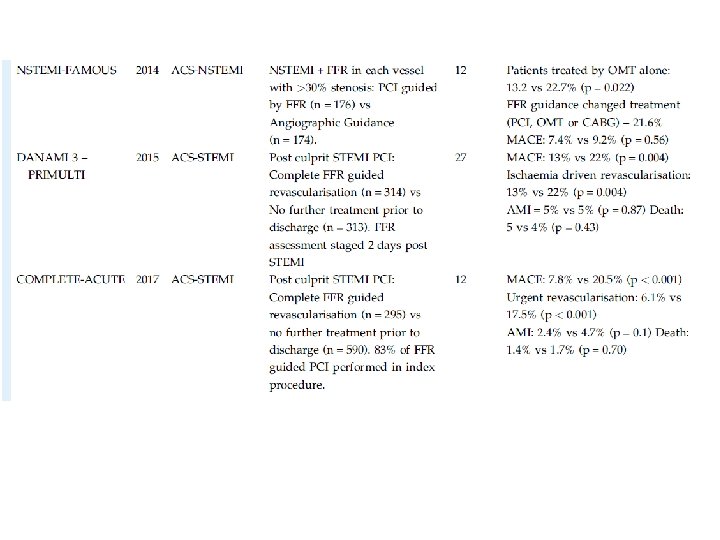
Acute coronary syndromes • In the case of STEMI, FFR measurement in the infarcted vessel is neither reasonable nor possible. In the case of NSTEMI, in the absence of a relevant thrombus load, lesions can be assessed using FFR during and after PCI • There is no established target value for FFR after PCI. • In the case of bifurcation lesion PCI, revascularisation of the side branch is not necessary if FFR is >0. 80 in the side branch
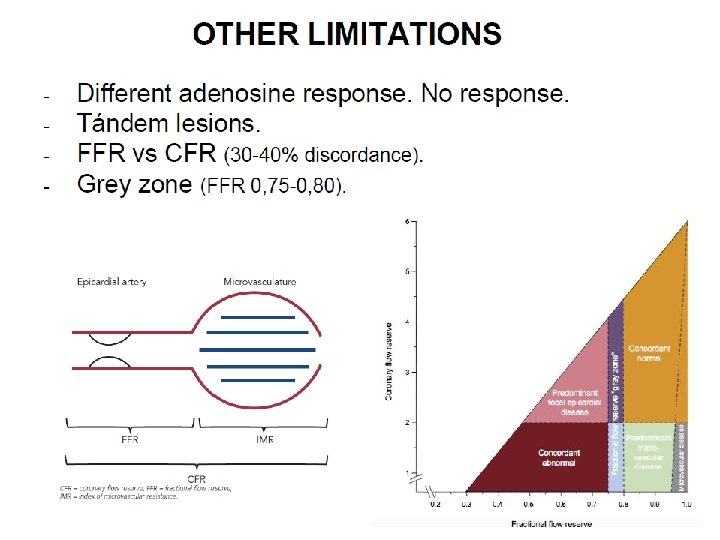
Limitations of Fractional Flow Reserve Measurements Microvascular dysfunction, • previous myocardial infarction • Left ventricular hypertrophy • diabetic microangiopathy
• certain patient groups were not included or tested in the randomised FFR studies. FAME studies, (excluded) • left main coronary artery stenosis, • recent history of STEMI • history of bypass surgery • impaired left ventricular (LV) systolic function (LV ejection fraction <30 %) • left ventricular hypertrophy (>13 mm) • there are currently no randomised, controlled outcome studies to validate FFR.
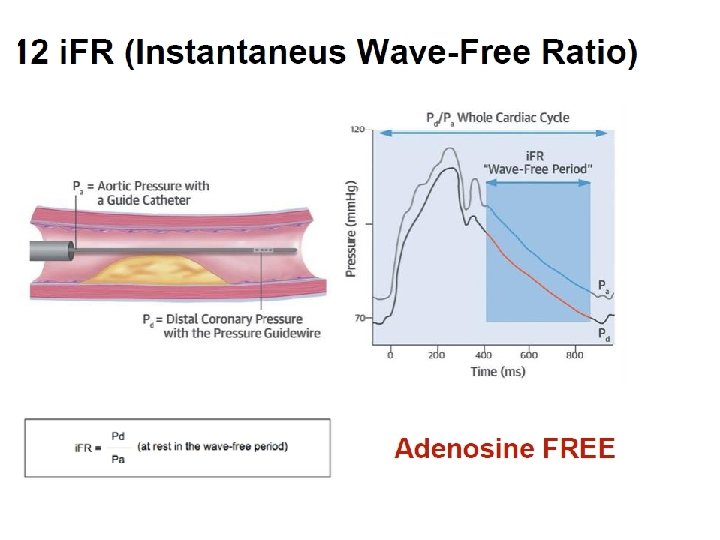
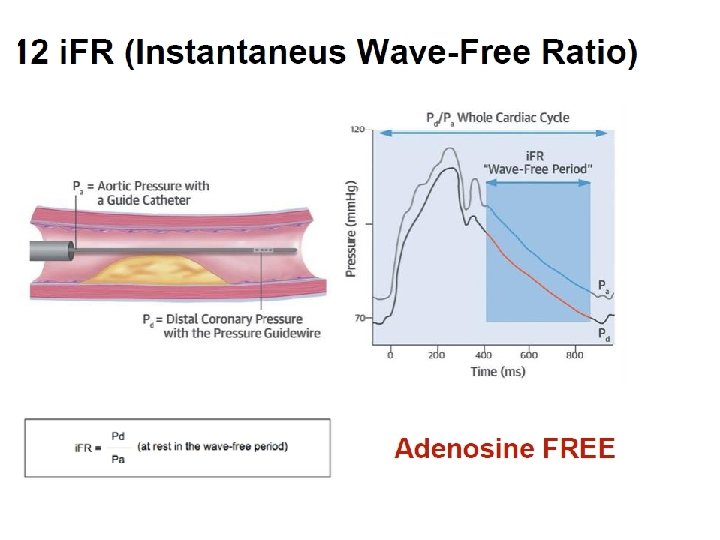
Instantaneous wave-free ratio (i. FR) • reduce the procedural time, improve cost efficiencies as well as improve patient comfort • i. FR is founded on the basis that there is a certain period in each cardiac cycle during which resistance at rest is stable (the wavefree period). • During this phase the ratio of the proximal and distal pressures are proportional to coronary flow
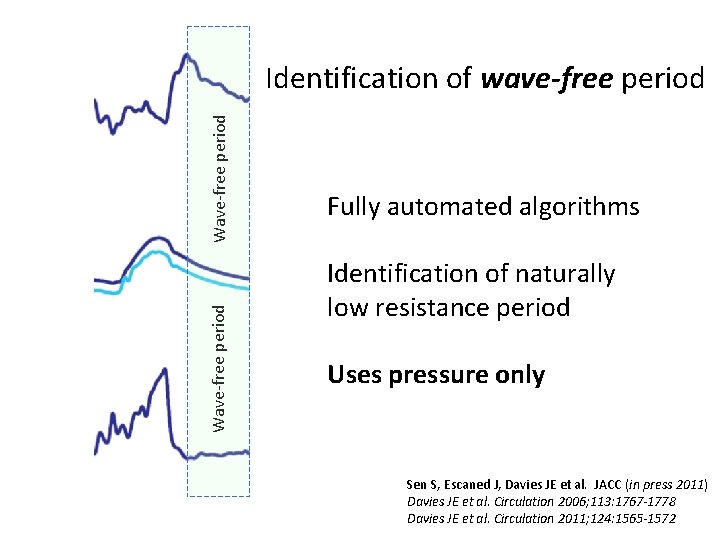
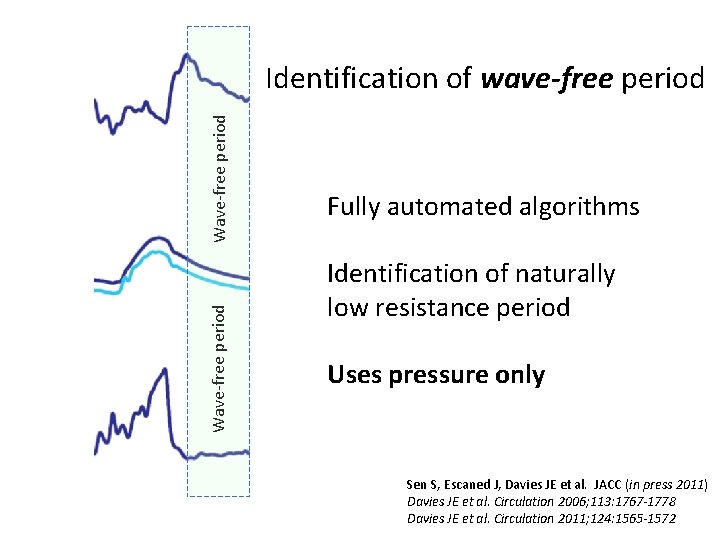
Wave-free period Identification of wave-free period Fully automated algorithms Identification of naturally low resistance period Uses pressure only Sen S, Escaned J, Davies JE et al. JACC (in press 2011) Davies JE et al. Circulation 2006; 113: 1767 -1778 Davies JE et al. Circulation 2011; 124: 1565 -1572


Instantaneouswave-free ratio (i. FR)

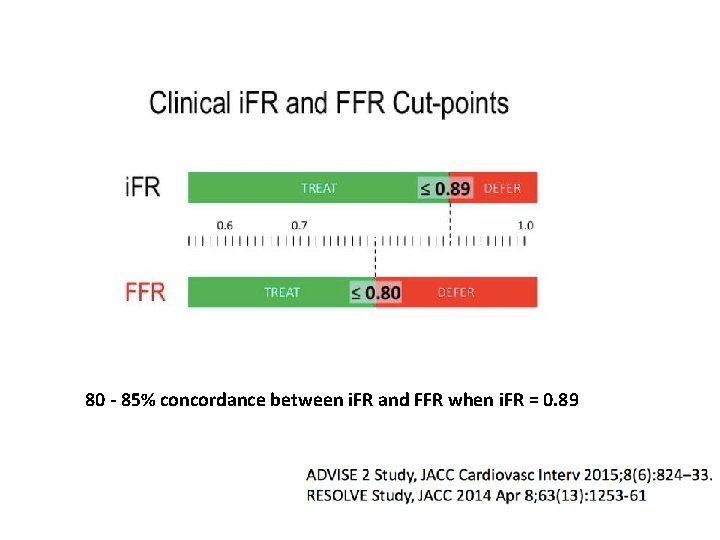
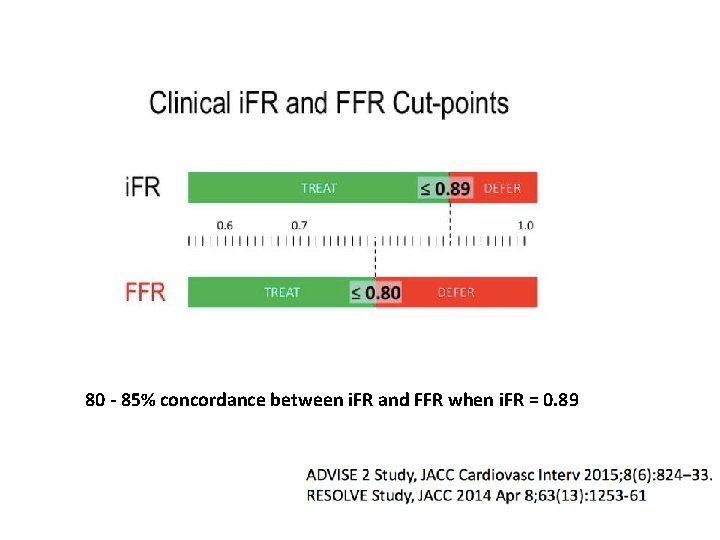
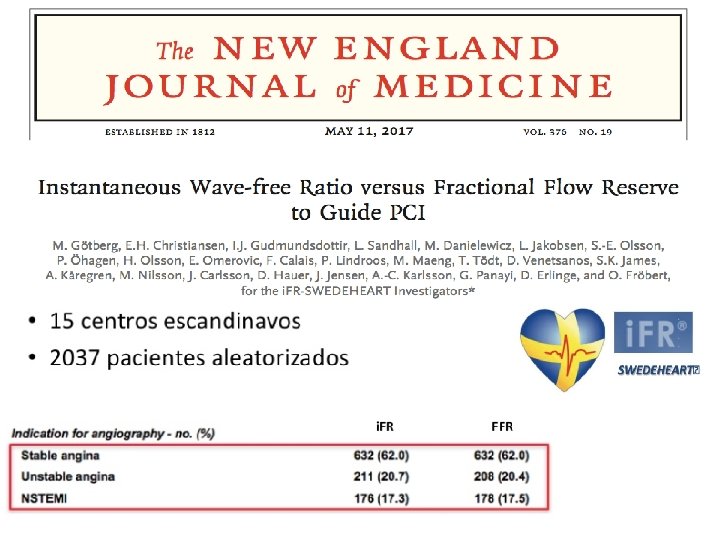
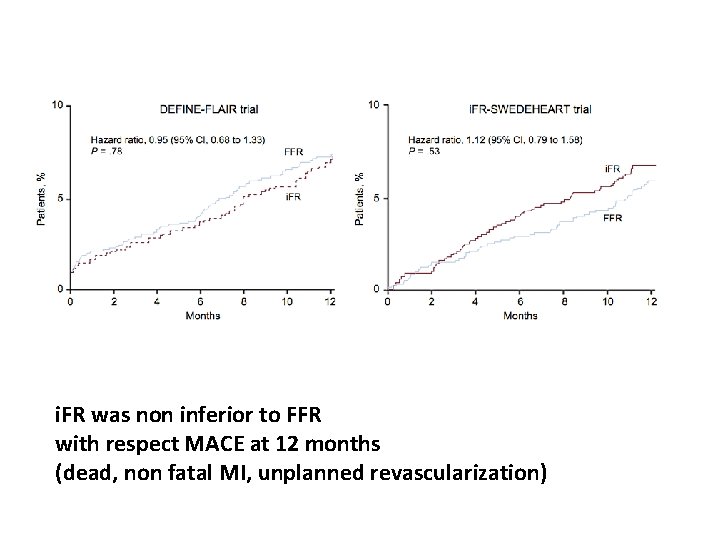
80 - 85% concordance between i. FR and FFR when i. FR = 0. 89
TRIALS





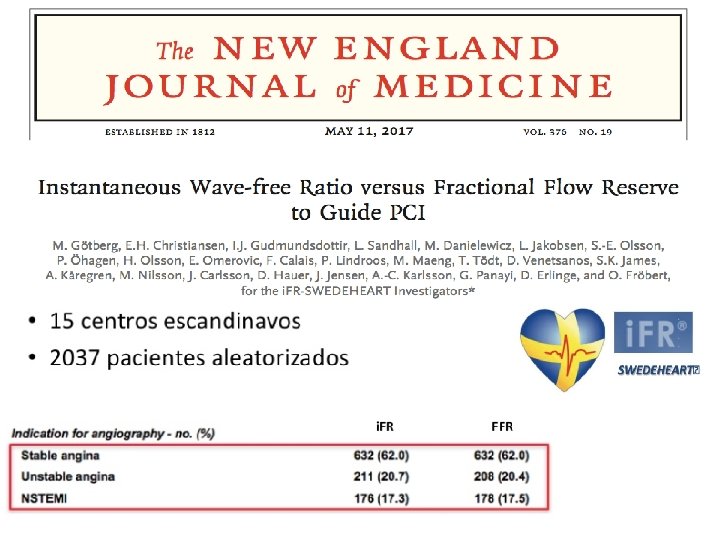
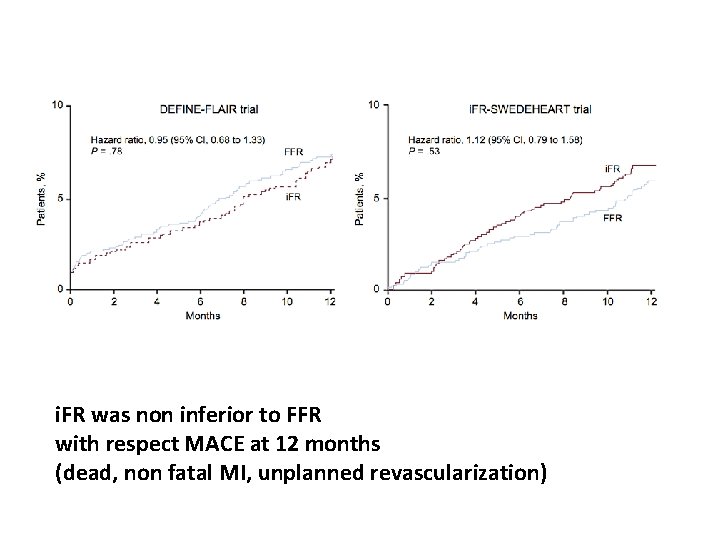
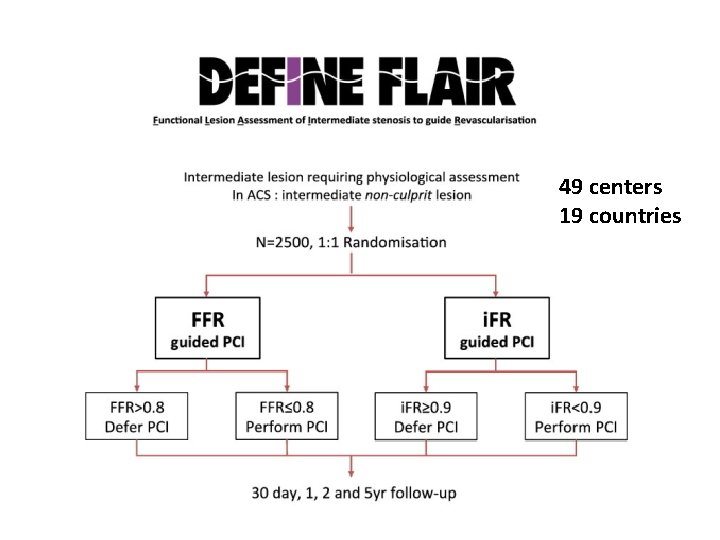
i. FR was non inferior to FFR with respect MACE at 12 months (dead, non fatal MI, unplanned revascularization)

THANK YOU
Back up slides




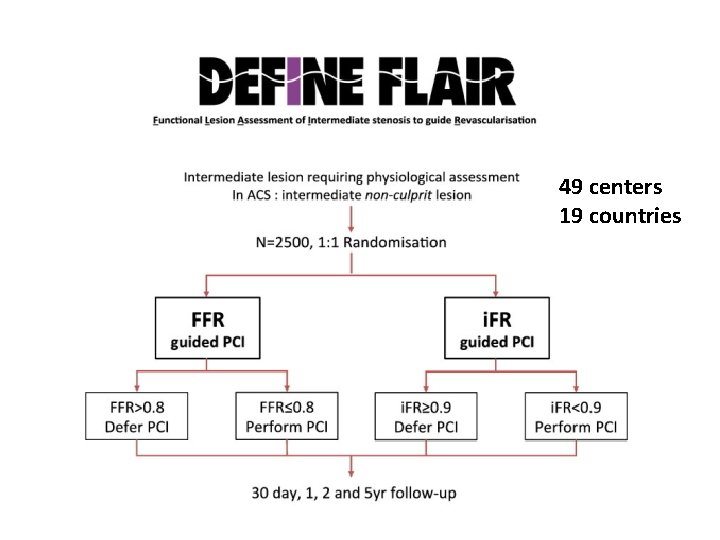
49 centers 19 countries





 Coronary artery disease
Coronary artery disease Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Good morning blood
Good morning blood Function of coronary artery
Function of coronary artery Coronary heart disease
Coronary heart disease Origin of sma
Origin of sma Communicable disease and non communicable disease
Communicable disease and non communicable disease Coronary sulcus
Coronary sulcus Heart sounds location
Heart sounds location Coronary personality
Coronary personality Right atrium
Right atrium Ali sepahdari
Ali sepahdari Cardiac plexus
Cardiac plexus What is high quality cpr
What is high quality cpr Crux cordis
Crux cordis Dipyrimadole
Dipyrimadole Great cardiac vein
Great cardiac vein Global registry of acute coronary events
Global registry of acute coronary events Ischemic heart disease classification
Ischemic heart disease classification Pk papyrus covered coronary stent system
Pk papyrus covered coronary stent system Flow of coronary circulation
Flow of coronary circulation Acute coronary syndrome
Acute coronary syndrome Unlocking of knee joint
Unlocking of knee joint Coronary blood flow
Coronary blood flow Coronary circulatory routes
Coronary circulatory routes Mesa coronary calcium score
Mesa coronary calcium score Heart disease
Heart disease Structure of blood vessels
Structure of blood vessels Heart cycle animation
Heart cycle animation Coronary circulation of heart
Coronary circulation of heart Mesa coronary calcium score
Mesa coronary calcium score Spider view cag
Spider view cag Coronary calcium score guidelines
Coronary calcium score guidelines Qfr coronary
Qfr coronary Heart veins
Heart veins Pk papyrus
Pk papyrus Glisson capsule
Glisson capsule Coronary circulation
Coronary circulation Definition of structural adaptation
Definition of structural adaptation Examples of physiological arousal
Examples of physiological arousal Why is artificial selection used
Why is artificial selection used Physiological disorders unit 14
Physiological disorders unit 14 Health and social care level 3 unit 14
Health and social care level 3 unit 14 Psychology emotions
Psychology emotions Phonetic anatomy
Phonetic anatomy Physiological buffer system
Physiological buffer system Physiological process in reading chart
Physiological process in reading chart Physiological regurgitation
Physiological regurgitation High arithmetic density
High arithmetic density Physiological perspective
Physiological perspective Physiological effects of electricity on the human body
Physiological effects of electricity on the human body Physiological factors in design
Physiological factors in design Psychological factors affecting sports performance
Psychological factors affecting sports performance Arithmetic population density
Arithmetic population density What is motivation
What is motivation Smart bristow faradic coil
Smart bristow faradic coil Unit 14 physiological disorders assignment 1
Unit 14 physiological disorders assignment 1 Formal region example
Formal region example Phosphate buffer system equation
Phosphate buffer system equation Oxygen uptake pdhpe
Oxygen uptake pdhpe Hydrophytes plants
Hydrophytes plants Physiological psychology
Physiological psychology Discontinuous variation
Discontinuous variation Physiological arousal
Physiological arousal Cannon-bard theory vs james-lange
Cannon-bard theory vs james-lange Physiological arousal
Physiological arousal Physiological density
Physiological density Cartogram world population
Cartogram world population