Physio Lecture 7 Introduction to Cardiovascular Physiology Prof
![Membrane potential and critical equations EK = -60 LOG ([Ki]/[Ko]) = -94 mv ENa Membrane potential and critical equations EK = -60 LOG ([Ki]/[Ko]) = -94 mv ENa](https://slidetodoc.com/presentation_image/5f5b22e2c4668f92936dd9540d5433c5/image-8.jpg)
- Slides: 51
Physio Lecture 7 – Introduction to Cardiovascular Physiology Prof. dr. Željko Dujić
MAIN FUNCTIONS OF THE CIRCULATORY SYSTEM -Transport and distribute essential substances to the tissues (most important to the vital organs – brain and heart). -Remove metabolic byproducts. -Adjustment of oxygen and nutrient supply in different physiologic states. -Regulation of body temperature. - Humoral communication by maintaining tissue perfusion.
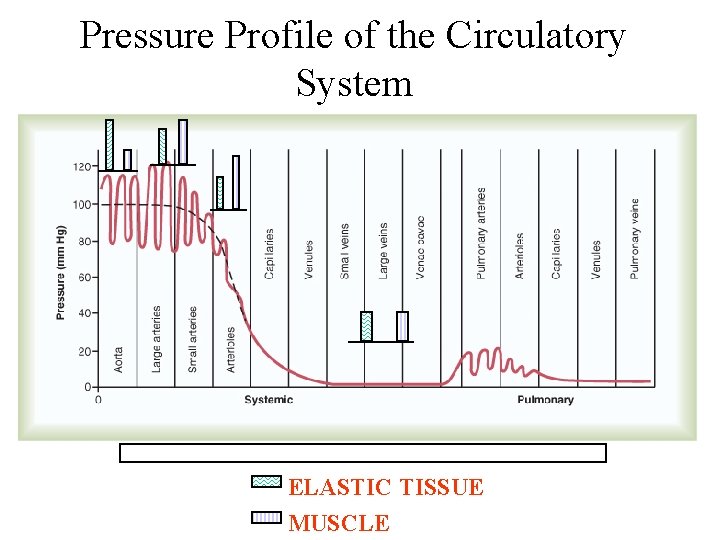
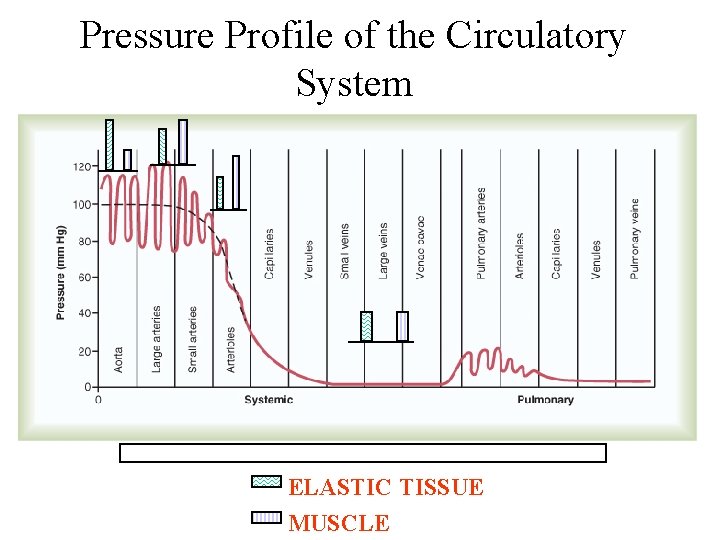
Pressure Profile of the Circulatory System ELASTIC TISSUE MUSCLE
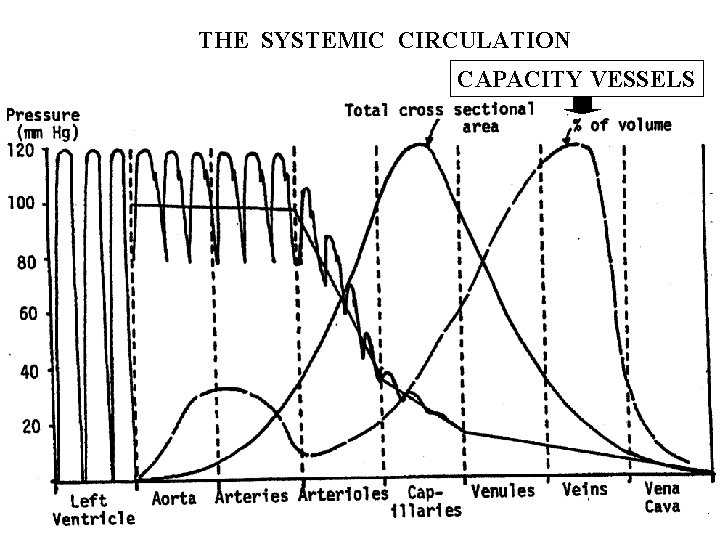
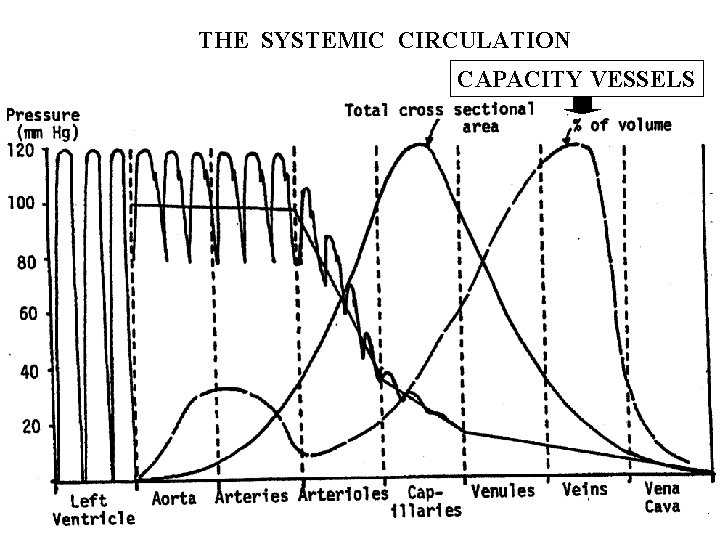
THE SYSTEMIC CIRCULATION CAPACITY VESSELS
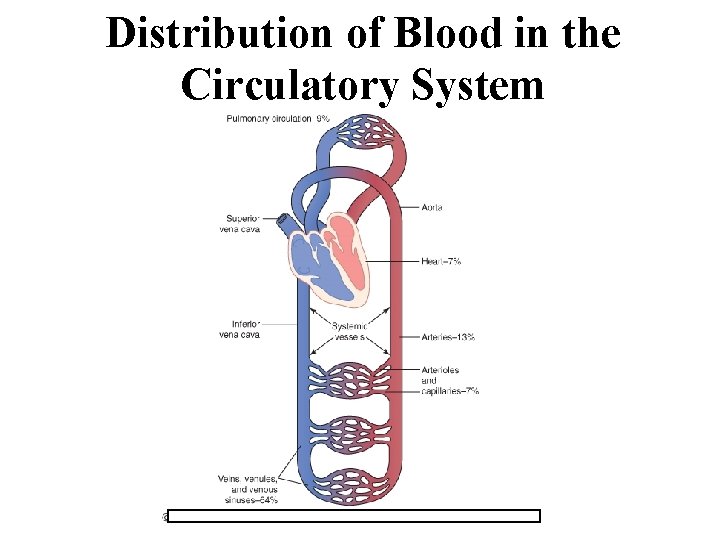
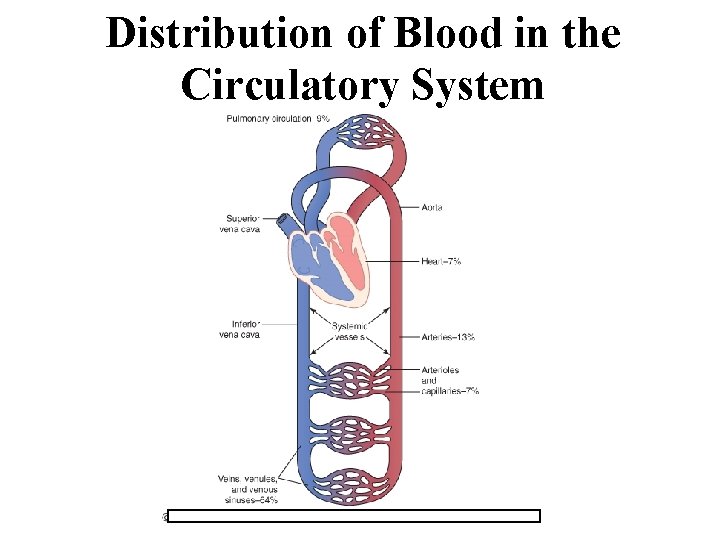
Distribution of Blood in the Circulatory System
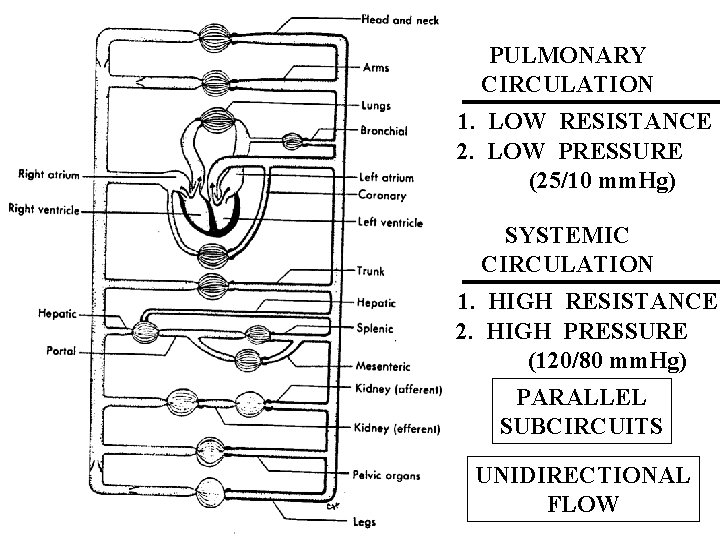
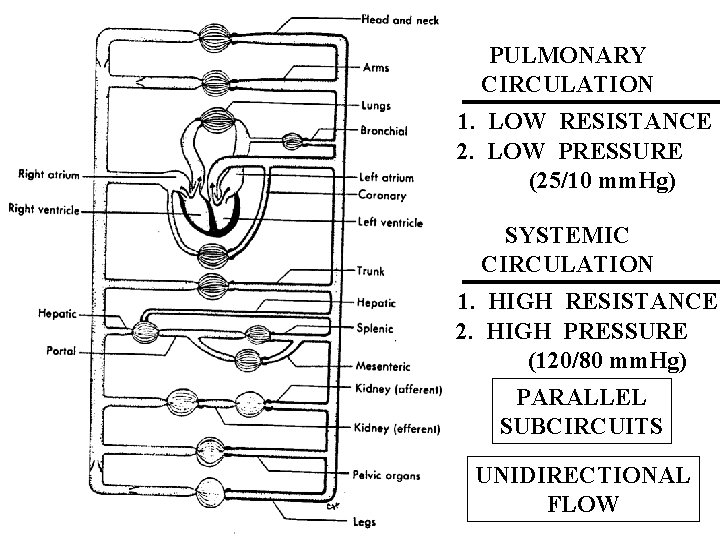
PULMONARY CIRCULATION 1. LOW RESISTANCE 2. LOW PRESSURE (25/10 mm. Hg) SYSTEMIC CIRCULATION 1. HIGH RESISTANCE 2. HIGH PRESSURE (120/80 mm. Hg) PARALLEL SUBCIRCUITS UNIDIRECTIONAL FLOW
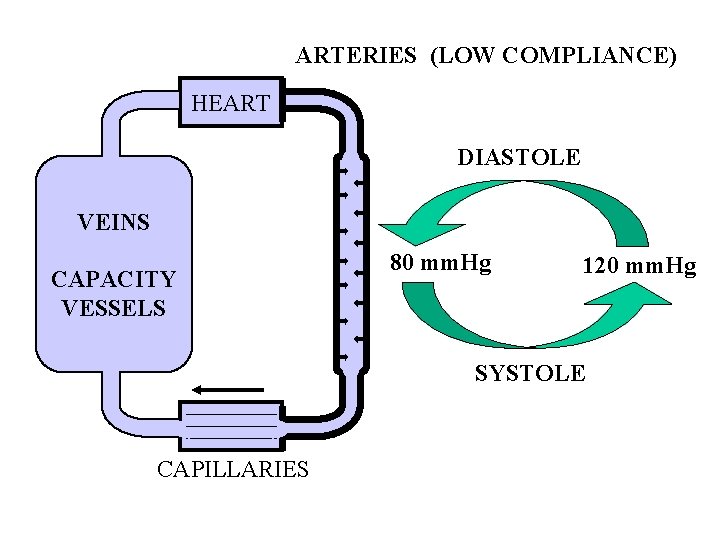
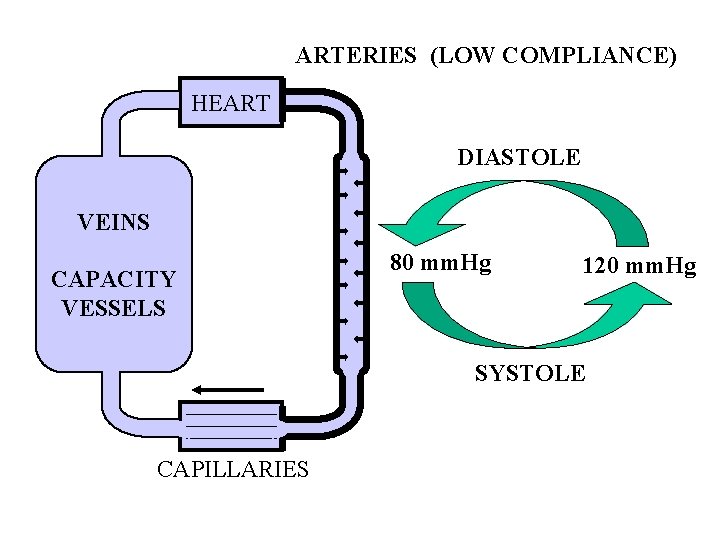
ARTERIES (LOW COMPLIANCE) HEART DIASTOLE VEINS CAPACITY VESSELS 80 mm. Hg 120 mm. Hg SYSTOLE CAPILLARIES
![Membrane potential and critical equations EK 60 LOG KiKo 94 mv ENa Membrane potential and critical equations EK = -60 LOG ([Ki]/[Ko]) = -94 mv ENa](https://slidetodoc.com/presentation_image/5f5b22e2c4668f92936dd9540d5433c5/image-8.jpg)
Membrane potential and critical equations EK = -60 LOG ([Ki]/[Ko]) = -94 mv ENa = -60 LOG ([Nai]/[Nao]) = +70 mv Em = RT/F ln PK (K+)o + PNa(Na+)o + PCl(Cl-)i PK (K+)I + PNa(Na+)i + PCl(Cl-)o
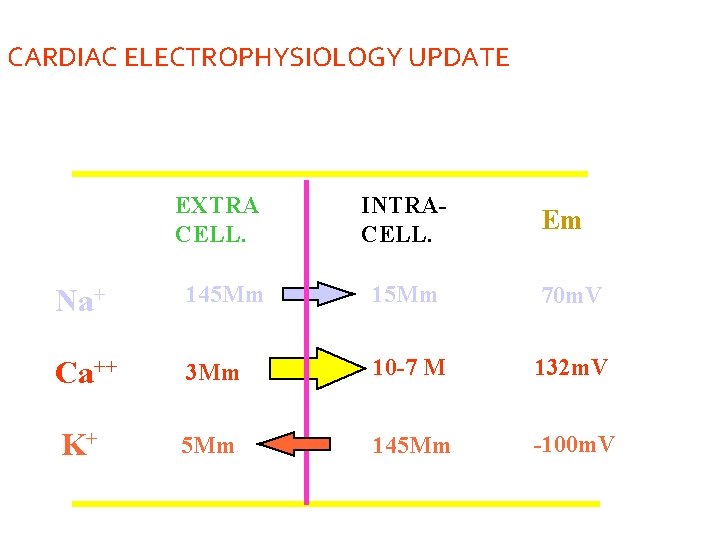
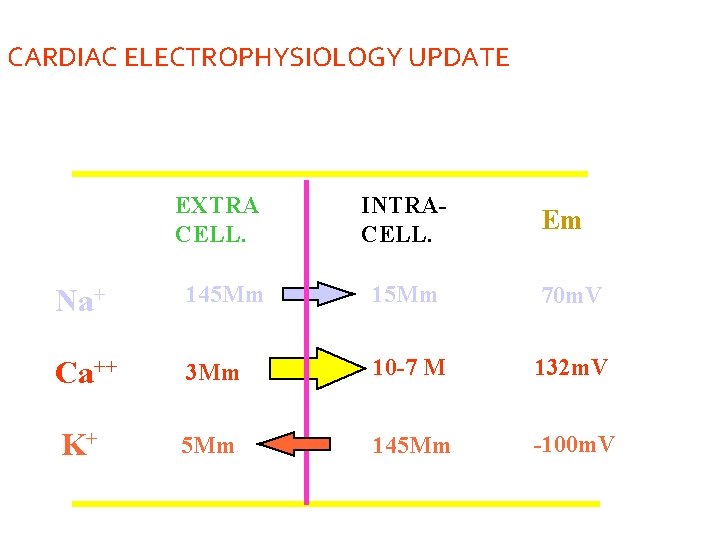
CARDIAC ELECTROPHYSIOLOGY UPDATE EXTRA CELL. INTRACELL. Em Na+ 145 Mm 15 Mm 70 m. V Ca++ 3 Mm 10 -7 M 132 m. V K+ 5 Mm 145 Mm -100 m. V
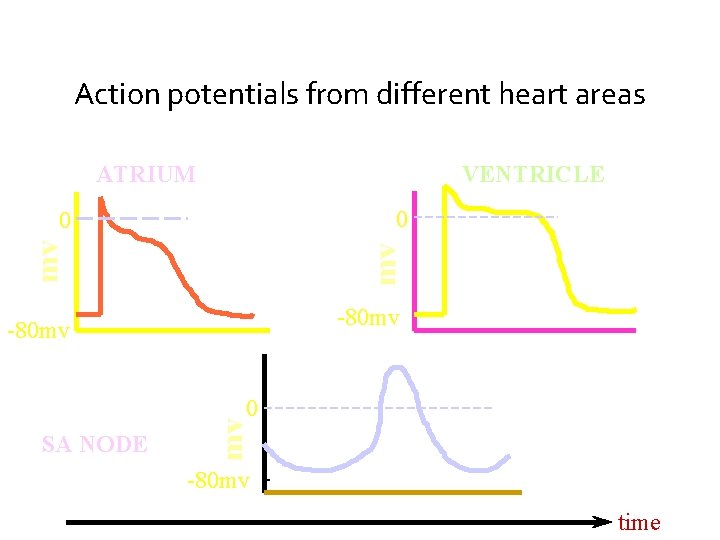
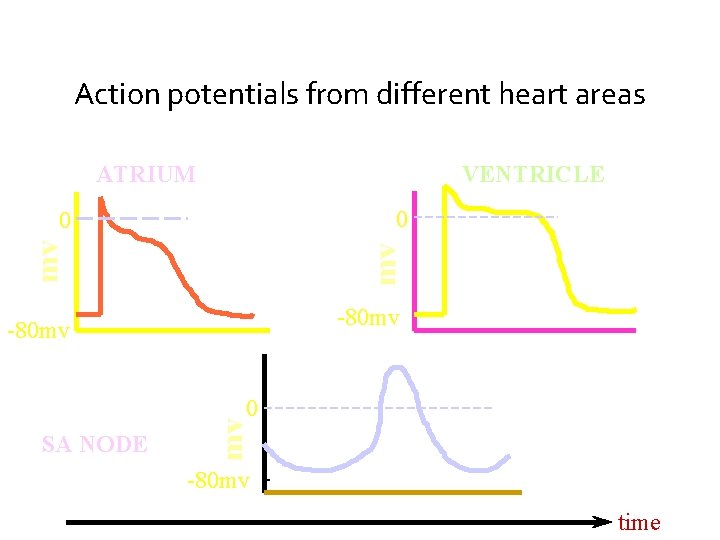
Action potentials from different heart areas ATRIUM VENTRICLE 0 mv mv 0 -80 mv SA NODE mv 0 -80 mv time
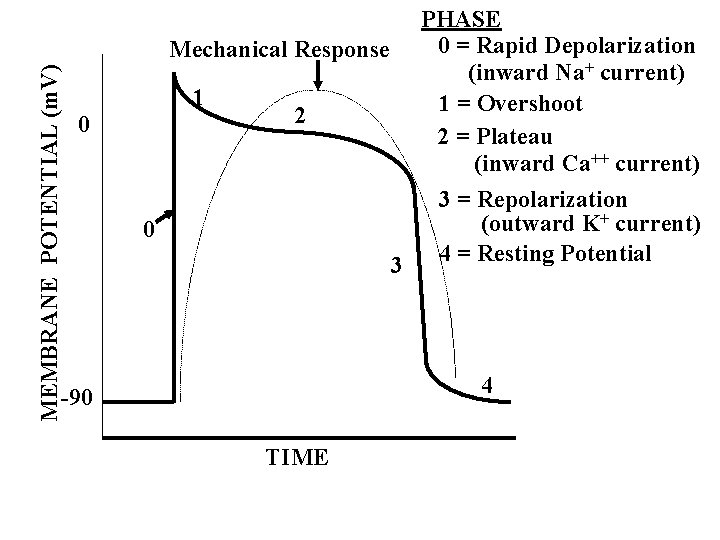
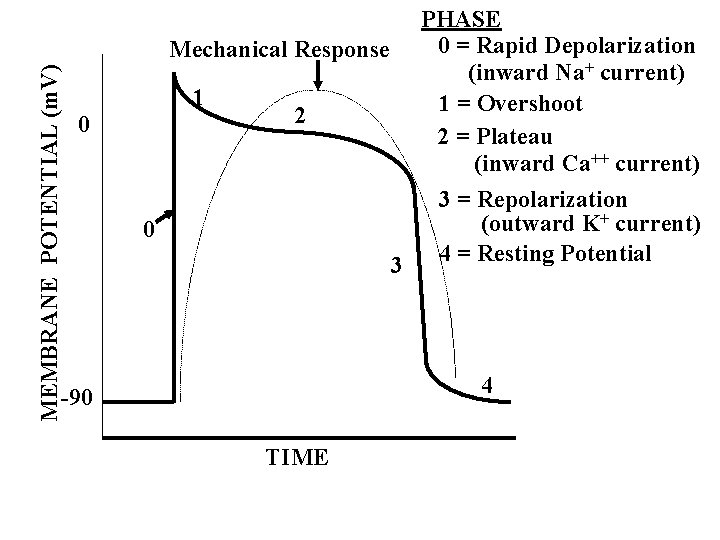
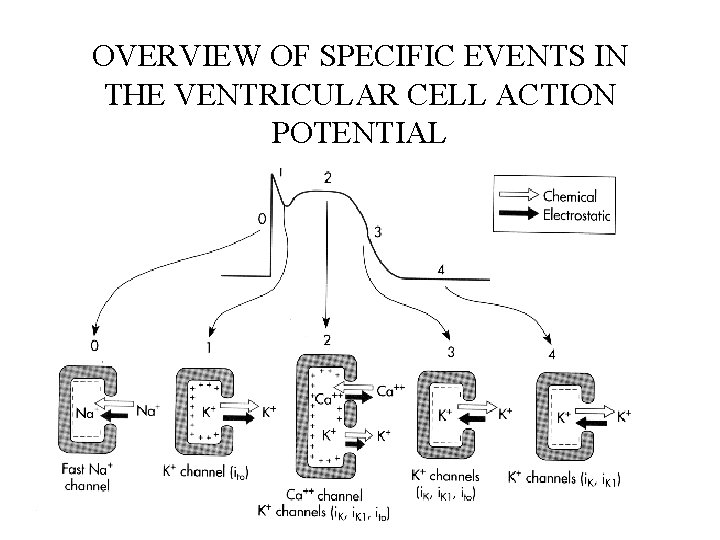
MEMBRANE POTENTIAL (m. V) 0 PHASE 0 = Rapid Depolarization Mechanical Response (inward Na+ current) 1 1 = Overshoot 2 2 = Plateau (inward Ca++ current) 3 = Repolarization + current) (outward K 0 4 = Resting Potential 3 4 -90 TIME
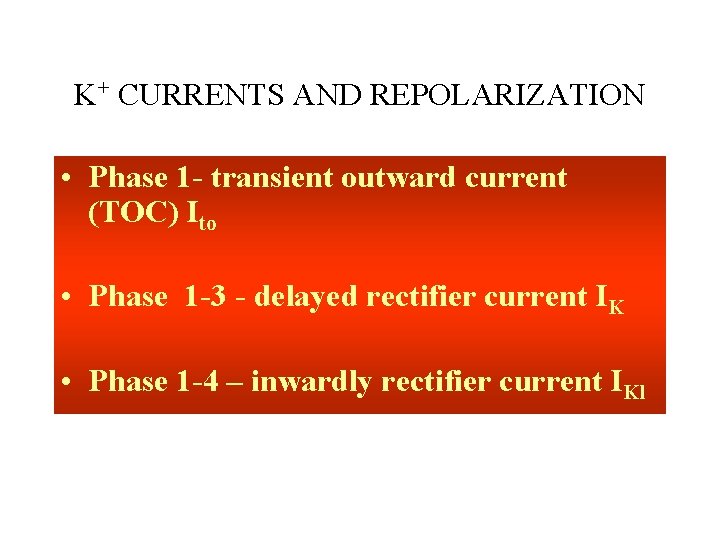
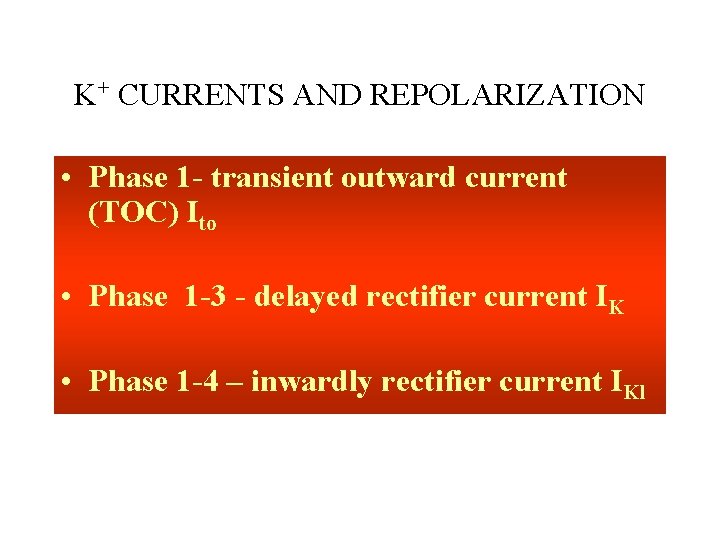
K+ CURRENTS AND REPOLARIZATION • Phase 1 - transient outward current (TOC) Ito • Phase 1 -3 - delayed rectifier current IK • Phase 1 -4 – inwardly rectifier current IKl
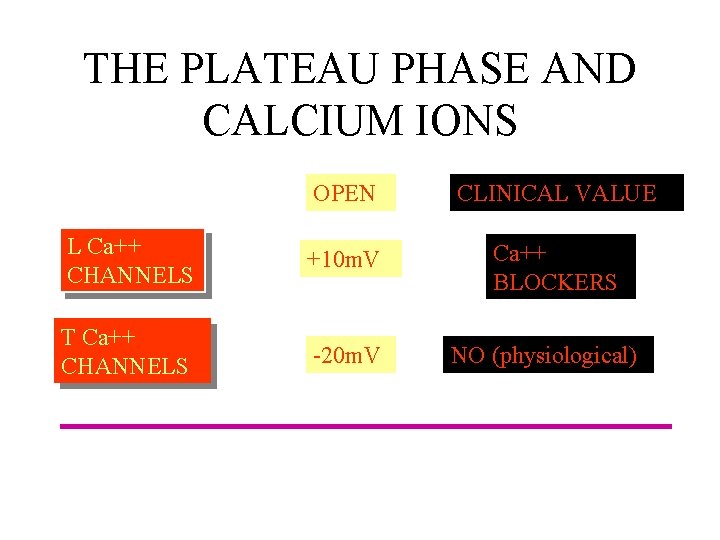
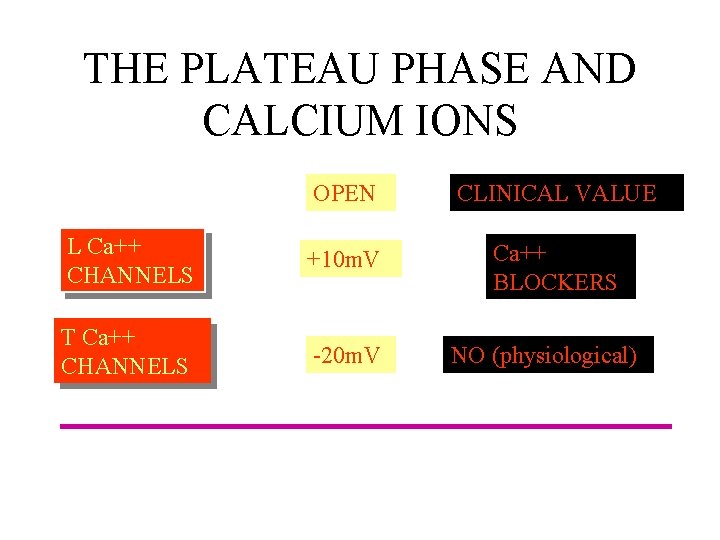
THE PLATEAU PHASE AND CALCIUM IONS OPEN CLINICAL VALUE L Ca++ CHANNELS +10 m. V Ca++ BLOCKERS T Ca++ CHANNELS -20 m. V NO (physiological)
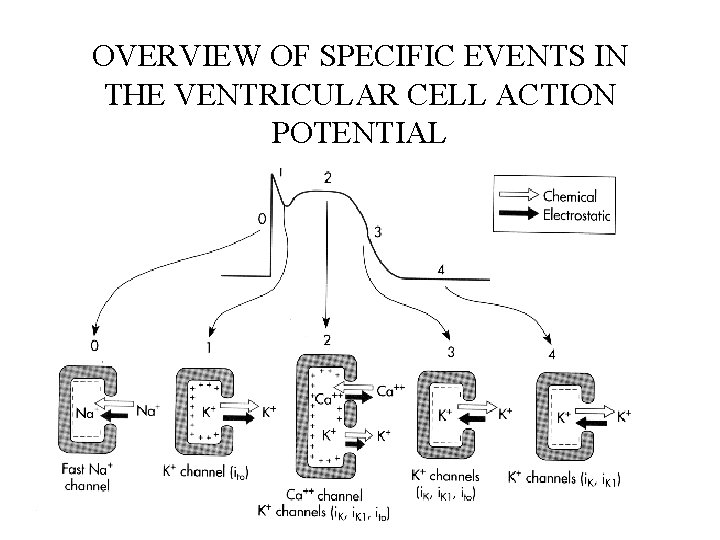
OVERVIEW OF SPECIFIC EVENTS IN THE VENTRICULAR CELL ACTION POTENTIAL
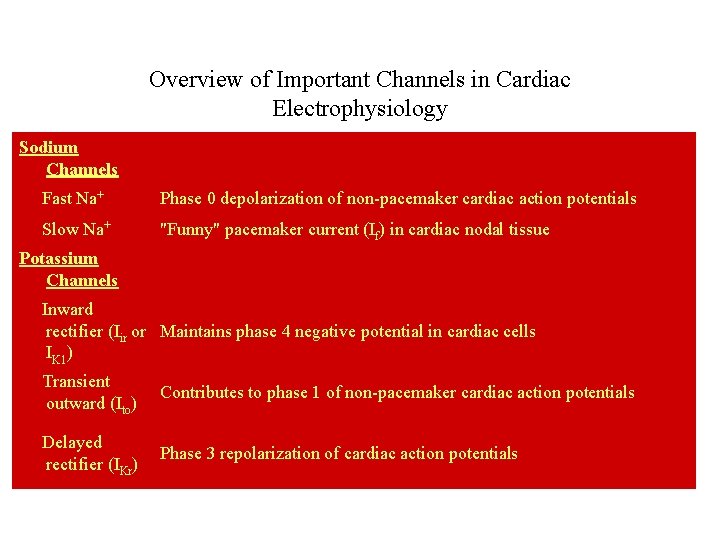
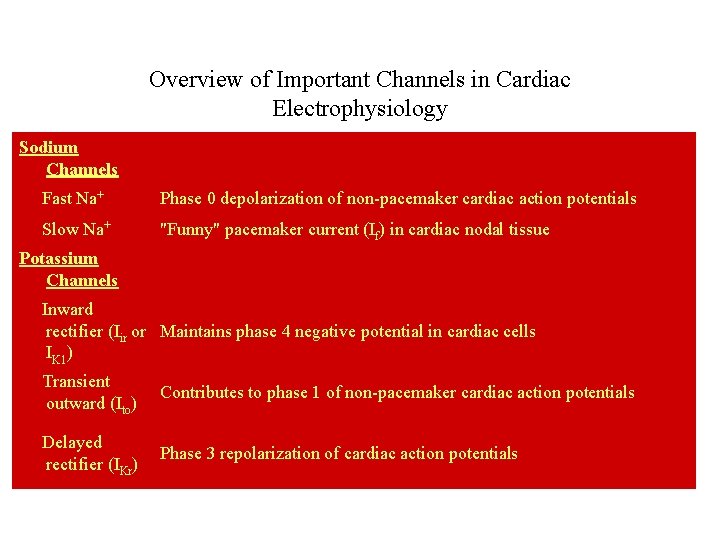
Overview of Important Channels in Cardiac Electrophysiology Sodium Channels Fast Na+ Phase 0 depolarization of non-pacemaker cardiac action potentials Slow Na+ "Funny" pacemaker current (If) in cardiac nodal tissue Potassium Channels Inward rectifier (Iir or Maintains phase 4 negative potential in cardiac cells IK 1) Transient outward (Ito) Contributes to phase 1 of non-pacemaker cardiac action potentials Delayed rectifier (IKr) Phase 3 repolarization of cardiac action potentials
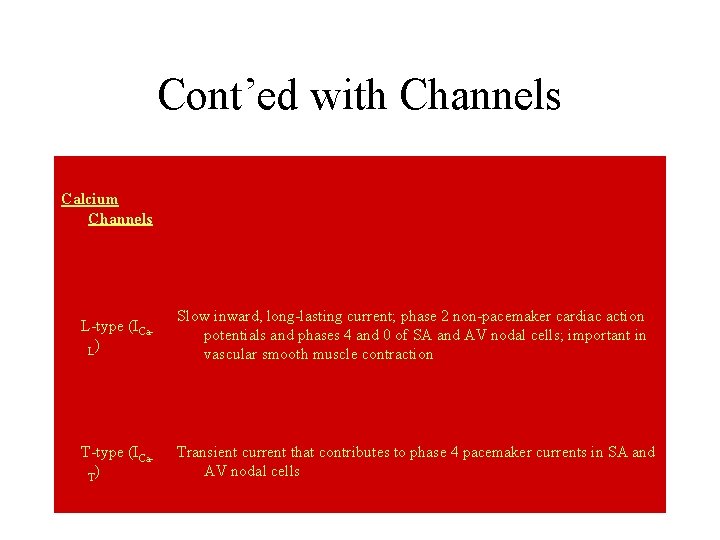
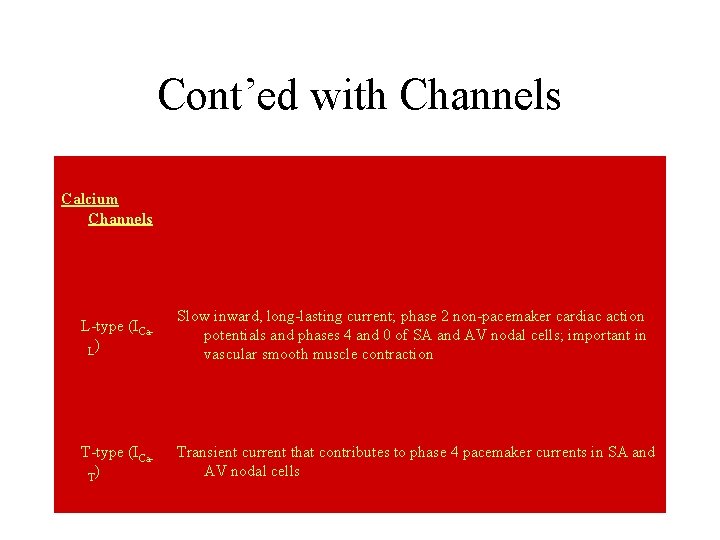
Cont’ed with Channels Calcium Channels L-type (ICa. L) Slow inward, long-lasting current; phase 2 non-pacemaker cardiac action potentials and phases 4 and 0 of SA and AV nodal cells; important in vascular smooth muscle contraction T-type (ICa. T) Transient current that contributes to phase 4 pacemaker currents in SA and AV nodal cells
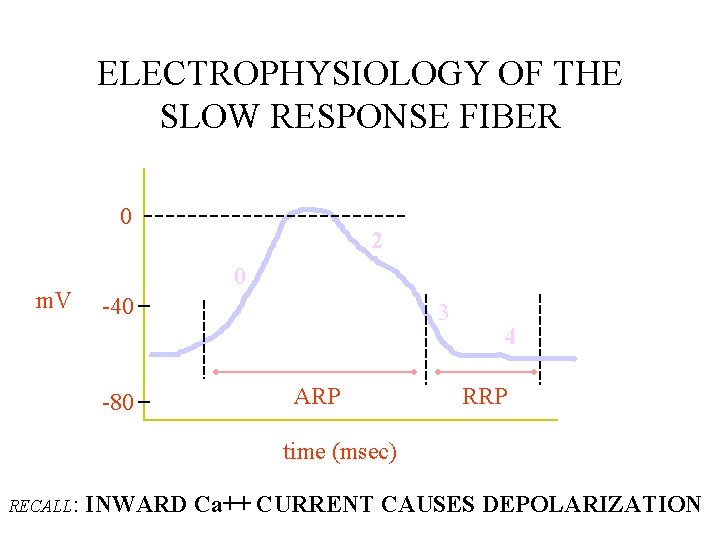
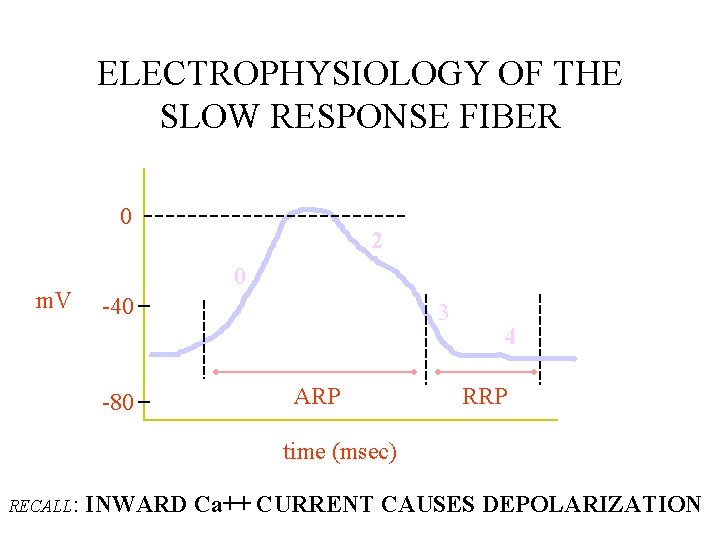
ELECTROPHYSIOLOGY OF THE SLOW RESPONSE FIBER 0 m. V 2 0 -40 -80 3 ARP 4 RRP time (msec) RECALL: INWARD Ca++ CURRENT CAUSES DEPOLARIZATION
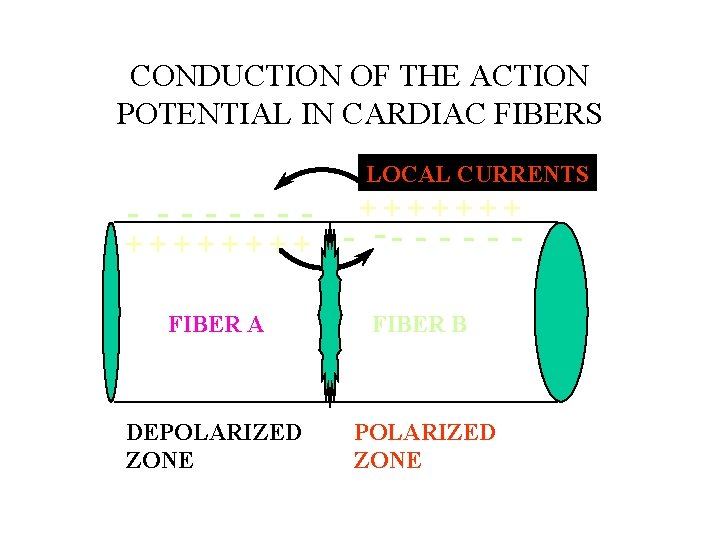
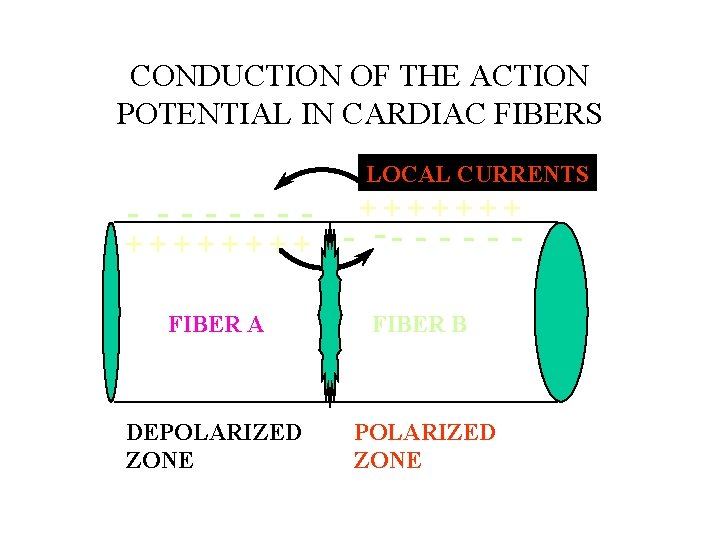
CONDUCTION OF THE ACTION POTENTIAL IN CARDIAC FIBERS LOCAL CURRENTS - ------+++++++ - -- - - FIBER A FIBER B DEPOLARIZED ZONE
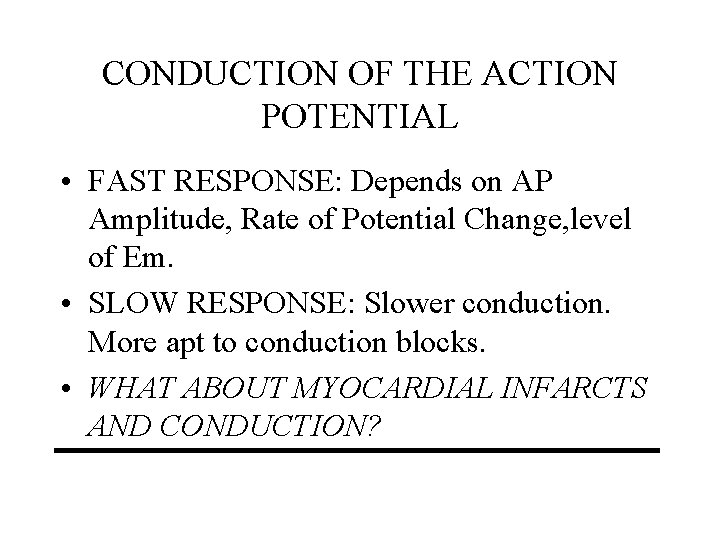
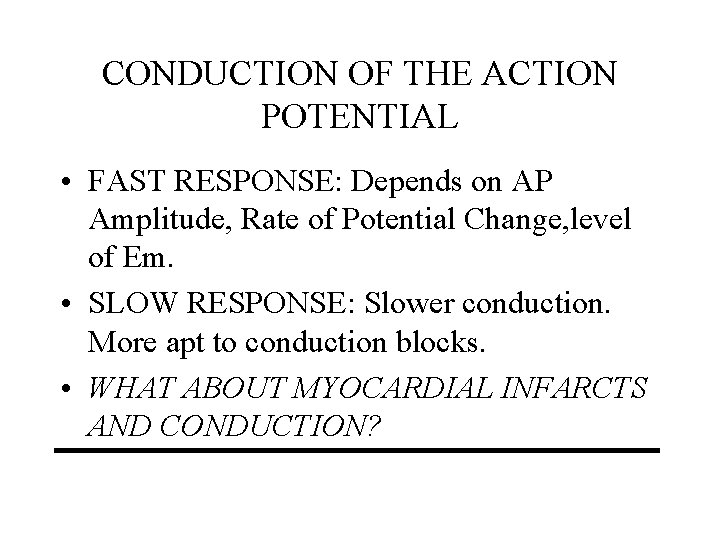
CONDUCTION OF THE ACTION POTENTIAL • FAST RESPONSE: Depends on AP Amplitude, Rate of Potential Change, level of Em. • SLOW RESPONSE: Slower conduction. More apt to conduction blocks. • WHAT ABOUT MYOCARDIAL INFARCTS AND CONDUCTION?
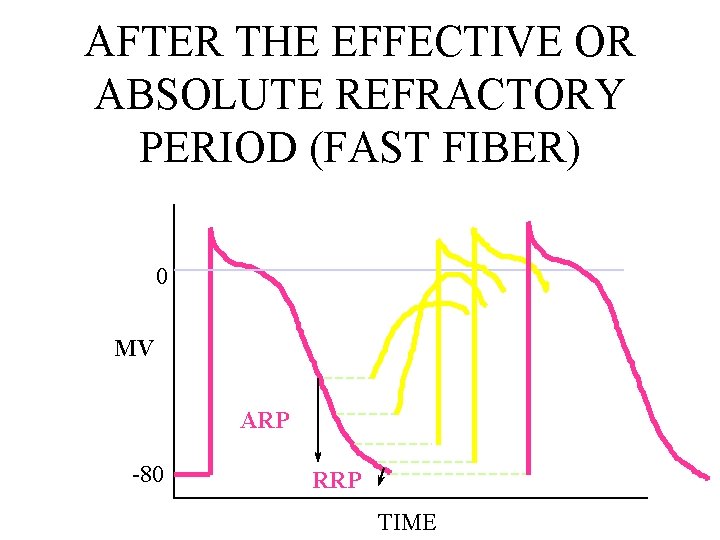
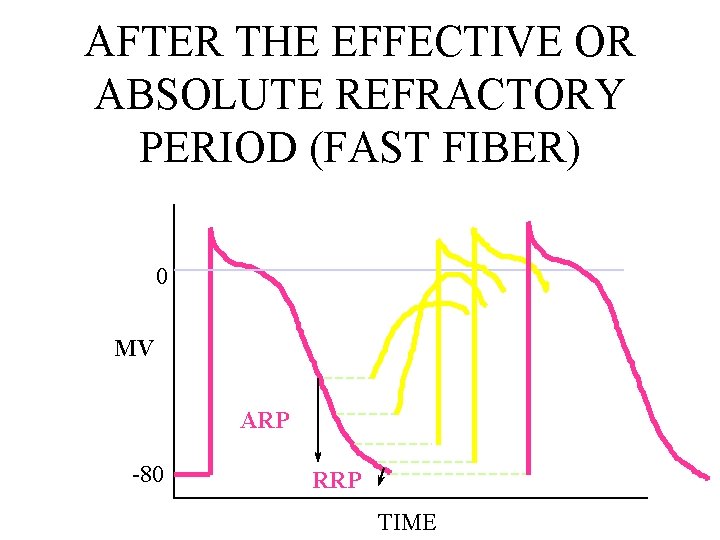
AFTER THE EFFECTIVE OR ABSOLUTE REFRACTORY PERIOD (FAST FIBER) 0 MV ARP -80 RRP TIME
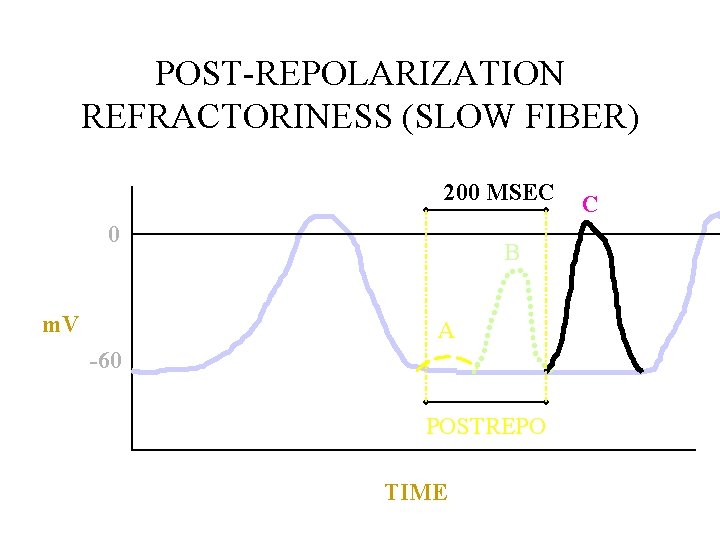
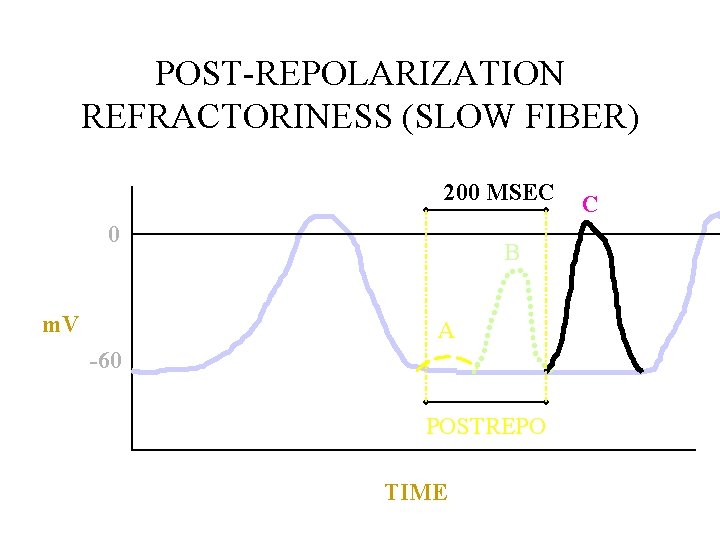
POST-REPOLARIZATION REFRACTORINESS (SLOW FIBER) 200 MSEC 0 m. V B A -60 POSTREPO TIME C
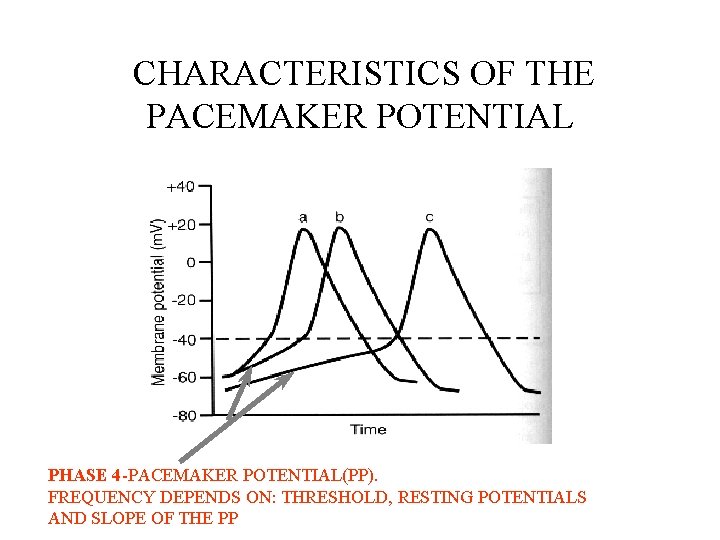
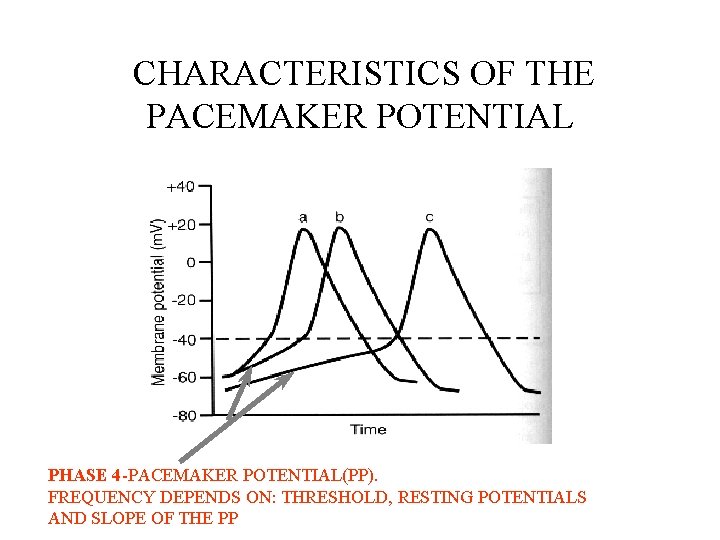
CHARACTERISTICS OF THE PACEMAKER POTENTIAL PHASE 4 -PACEMAKER POTENTIAL(PP). FREQUENCY DEPENDS ON: THRESHOLD, RESTING POTENTIALS AND SLOPE OF THE PP
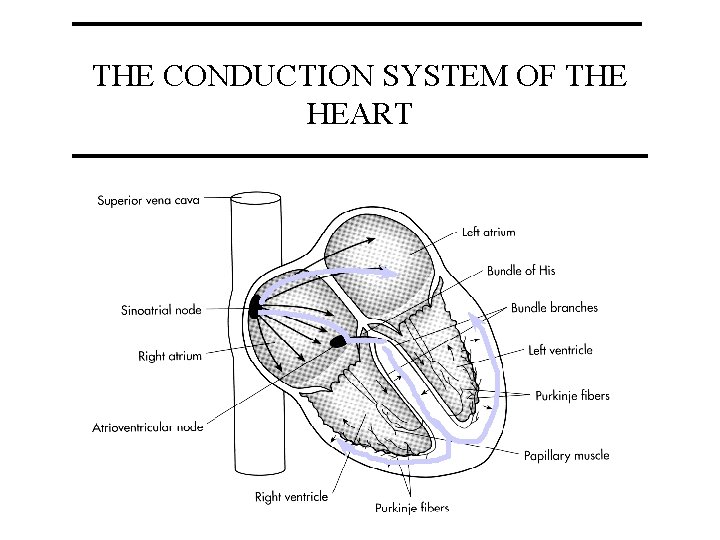
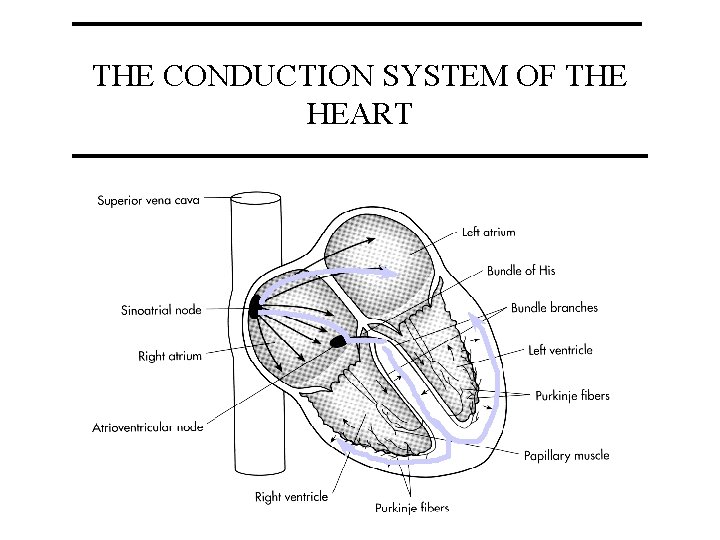
THE CONDUCTION SYSTEM OF THE HEART
PACEMAKERS (in order of their inherent rhythm) • • • Sino-atrial (SA) node (HR 60 -70) Atrio-ventricular (AV) node (HR 40) Bundle of His (HR 15 -40) Bundle branches Purkinje fibers
CARDIAC MECHANICS MAIN THEMES THE HEART AS A PUMP THE CARDIAC CYCLE CARDIAC OUTPUT
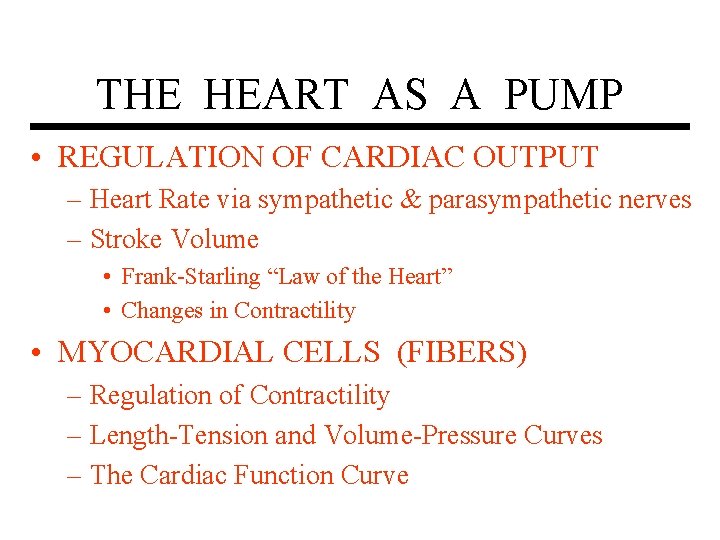
THE HEART AS A PUMP • REGULATION OF CARDIAC OUTPUT – Heart Rate via sympathetic & parasympathetic nerves – Stroke Volume • Frank-Starling “Law of the Heart” • Changes in Contractility • MYOCARDIAL CELLS (FIBERS) – Regulation of Contractility – Length-Tension and Volume-Pressure Curves – The Cardiac Function Curve
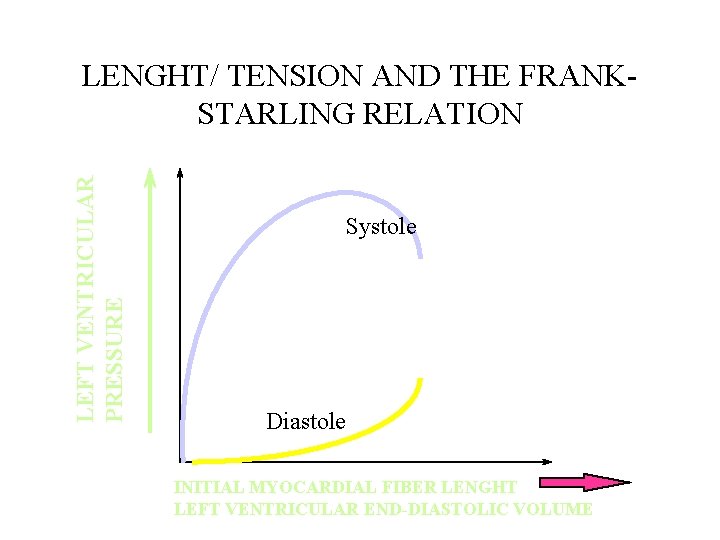
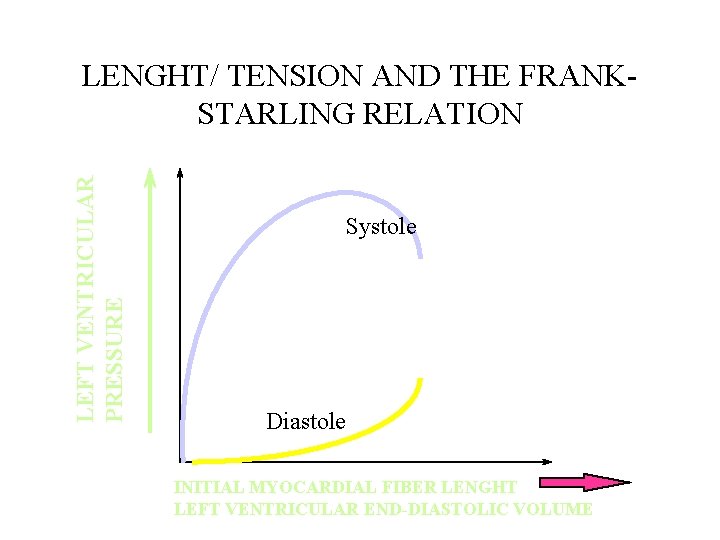
LEFT VENTRICULAR PRESSURE LENGHT/ TENSION AND THE FRANKSTARLING RELATION Systole Diastole INITIAL MYOCARDIAL FIBER LENGHT LEFT VENTRICULAR END-DIASTOLIC VOLUME
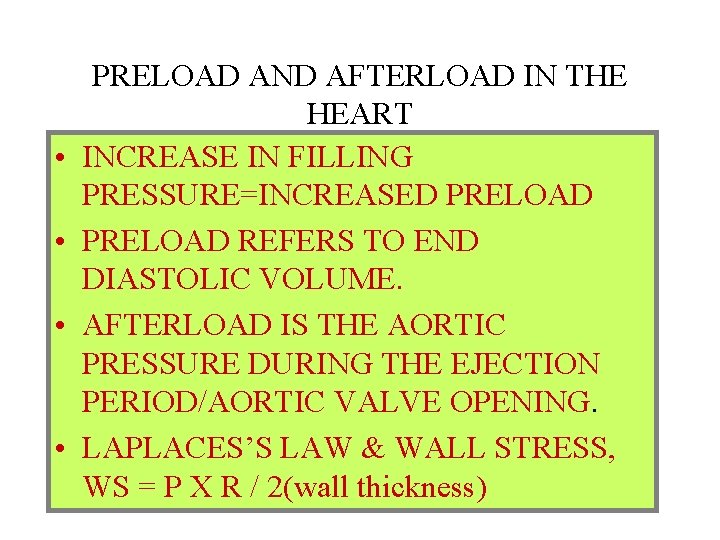
• • PRELOAD AND AFTERLOAD IN THE HEART INCREASE IN FILLING PRESSURE=INCREASED PRELOAD REFERS TO END DIASTOLIC VOLUME. AFTERLOAD IS THE AORTIC PRESSURE DURING THE EJECTION PERIOD/AORTIC VALVE OPENING. LAPLACES’S LAW & WALL STRESS, WS = P X R / 2(wall thickness)
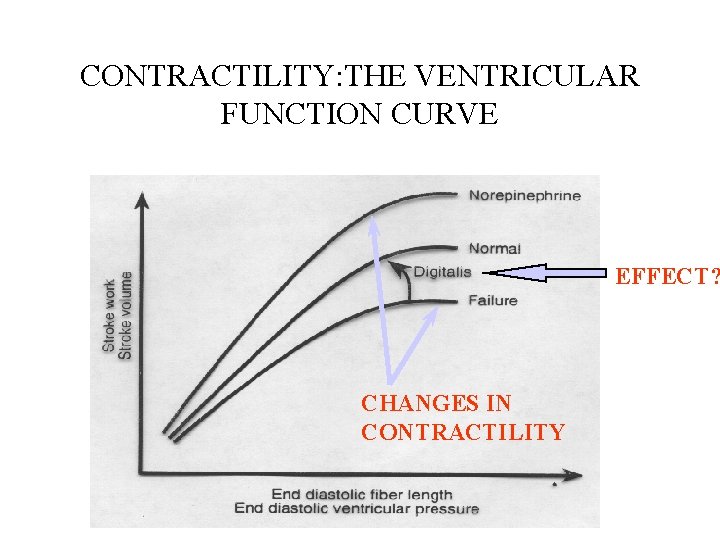
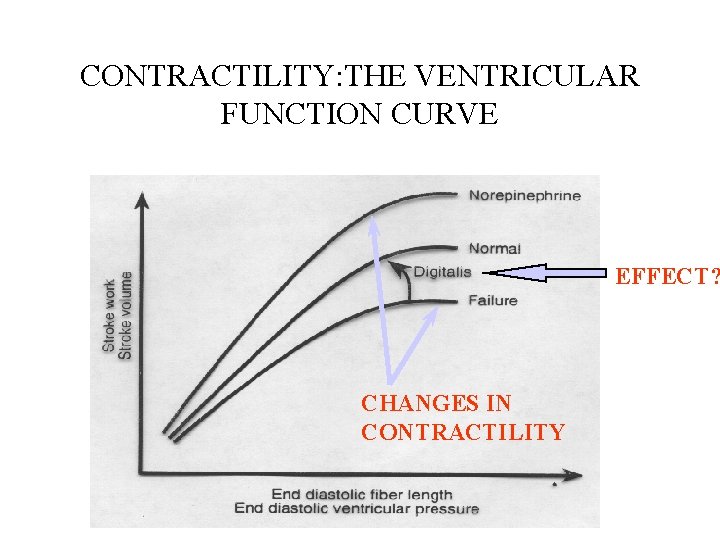
CONTRACTILITY: THE VENTRICULAR FUNCTION CURVE EFFECT? CHANGES IN CONTRACTILITY
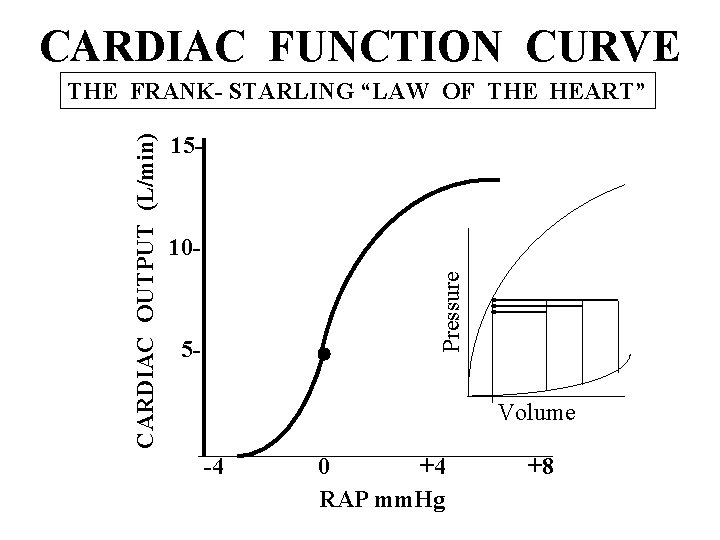
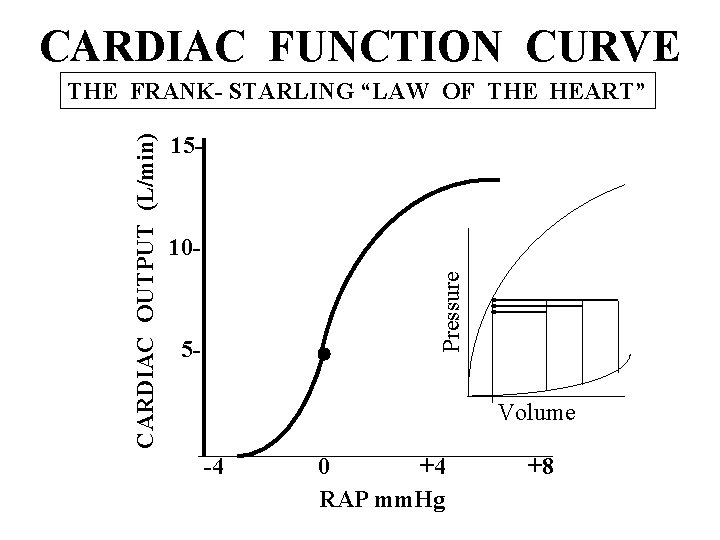
CARDIAC FUNCTION CURVE 15 - 10 Pressure CARDIAC OUTPUT (L/min) THE FRANK- STARLING “LAW OF THE HEART” 5 - Volume -4 0 +4 RAP mm. Hg +8
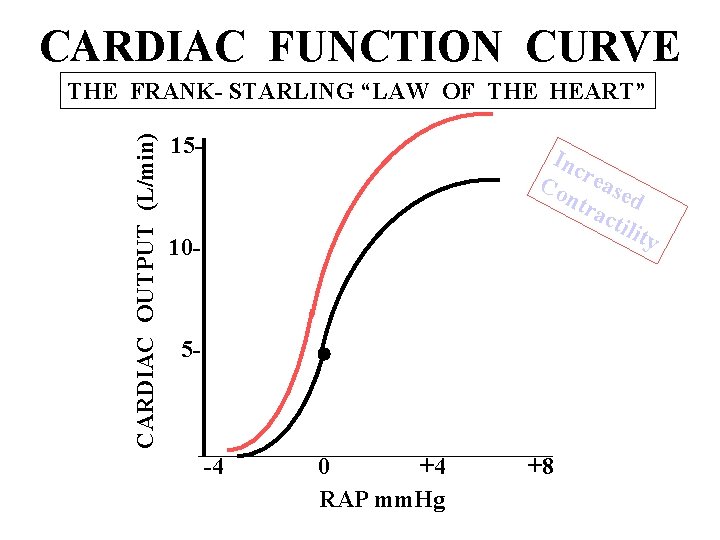
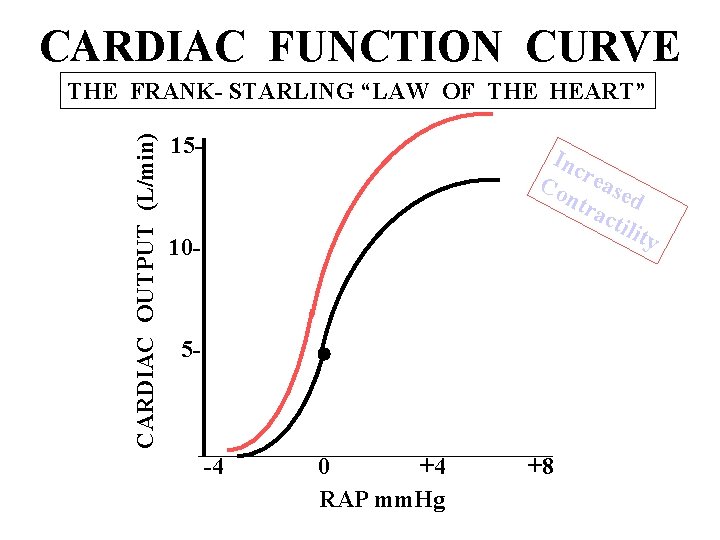
CARDIAC FUNCTION CURVE CARDIAC OUTPUT (L/min) THE FRANK- STARLING “LAW OF THE HEART” 15 - Inc Co rease ntr d act ilit y 10 - 5 - -4 0 +4 RAP mm. Hg +8
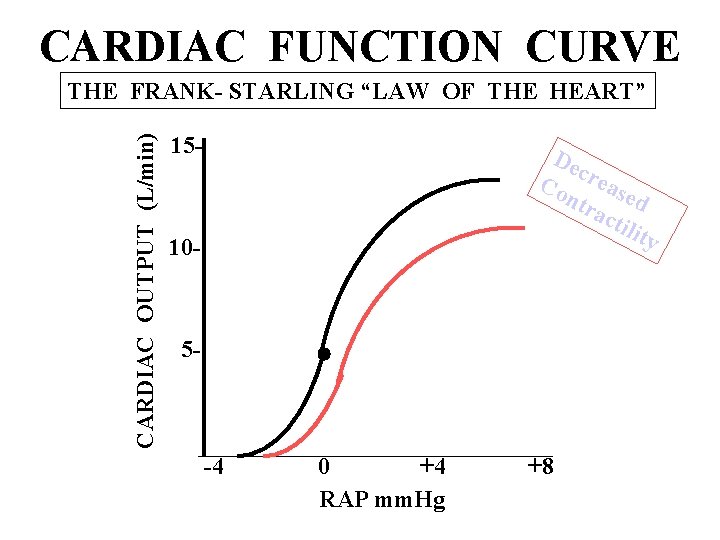
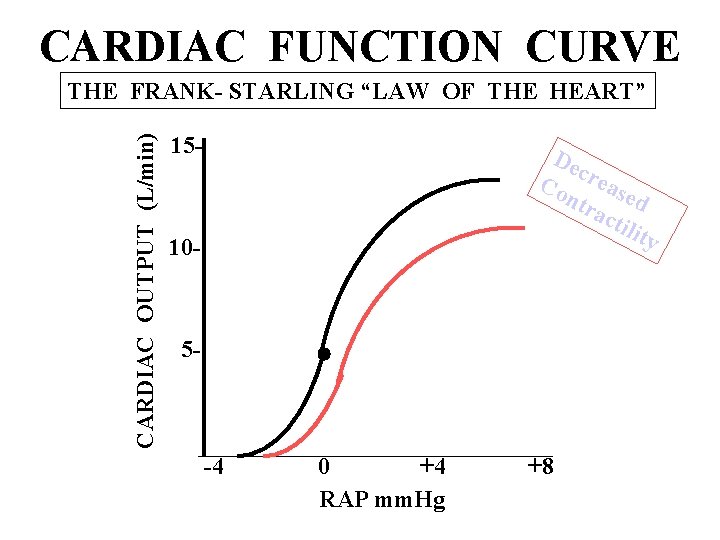
CARDIAC FUNCTION CURVE CARDIAC OUTPUT (L/min) THE FRANK- STARLING “LAW OF THE HEART” 15 - De c Co reas ntr ed act ilit y 10 - 5 - -4 0 +4 RAP mm. Hg +8
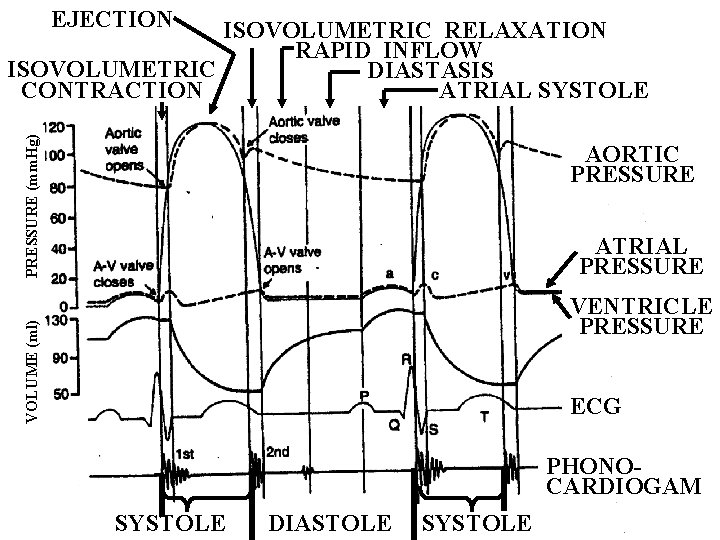
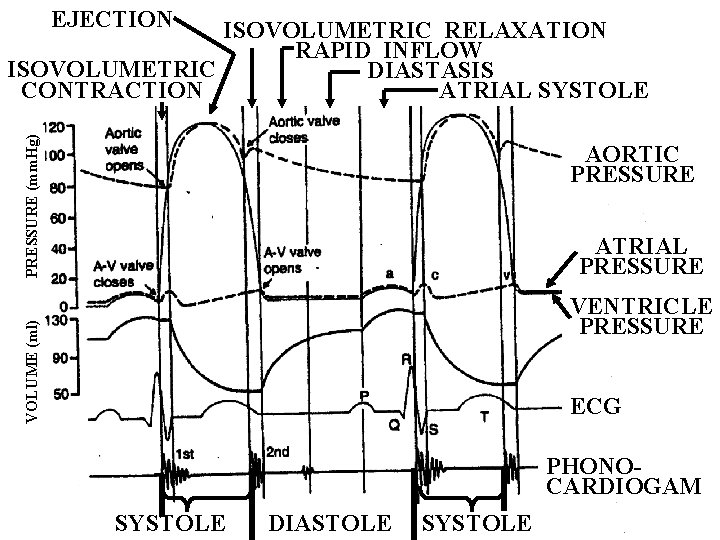
EJECTION PRESSURE (mm. Hg) ISOVOLUMETRIC RELAXATION RAPID INFLOW ISOVOLUMETRIC DIASTASIS CONTRACTION ATRIAL SYSTOLE AORTIC PRESSURE ATRIAL PRESSURE VOLUME (ml) VENTRICLE PRESSURE ECG PHONOCARDIOGAM SYSTOLE DIASTOLE SYSTOLE
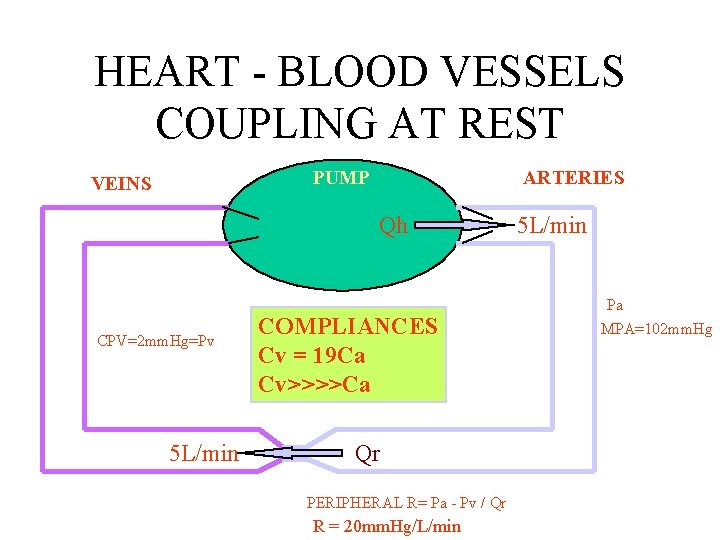
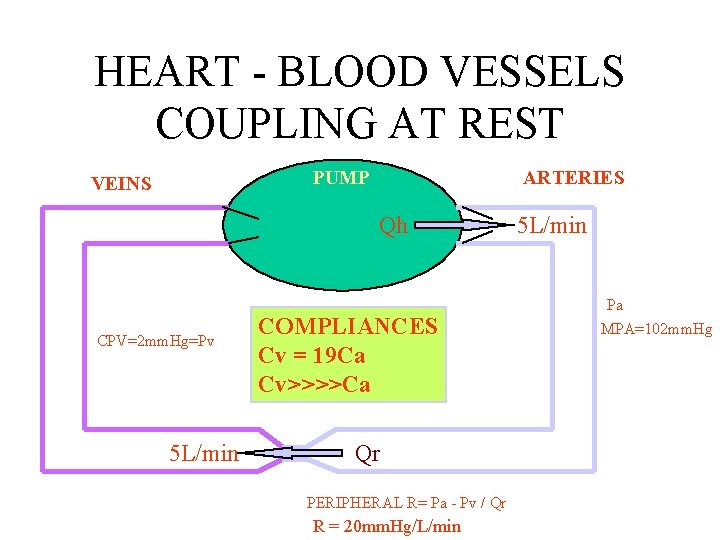
HEART - BLOOD VESSELS COUPLING AT REST PUMP VEINS ARTERIES Qh CPV=2 mm. Hg=Pv 5 L/min COMPLIANCES Cv = 19 Ca Cv>>>>Ca Qr PERIPHERAL R= Pa - Pv / Qr R = 20 mm. Hg/L/min 5 L/min Pa MPA=102 mm. Hg
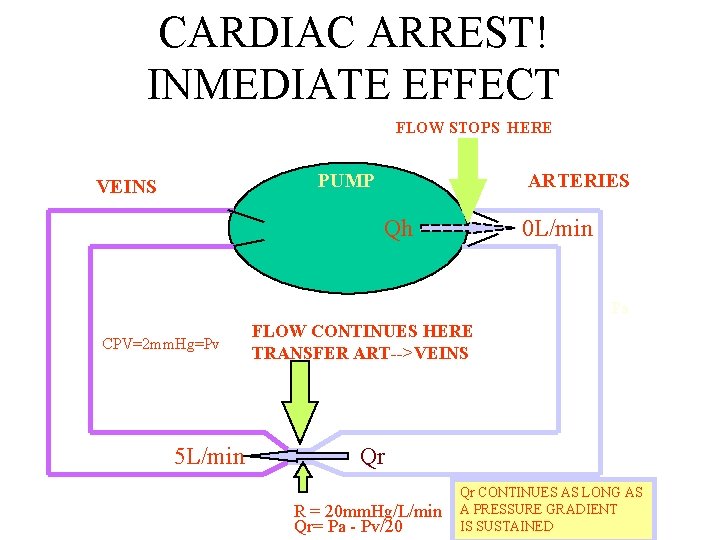
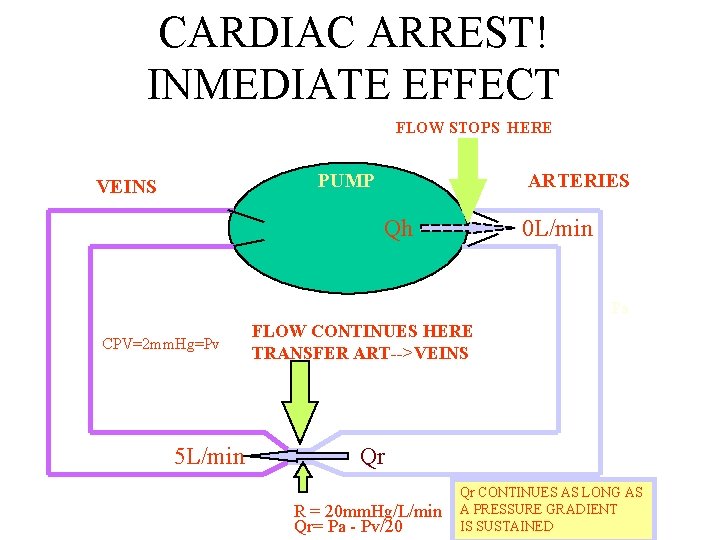
CARDIAC ARREST! INMEDIATE EFFECT FLOW STOPS HERE PUMP VEINS ARTERIES Qh 0 L/min Pa CPV=2 mm. Hg=Pv 5 L/min FLOW CONTINUES HERE TRANSFER ART-->VEINS Qr R = 20 mm. Hg/L/min Qr= Pa - Pv/20 Qr CONTINUES AS LONG AS A PRESSURE GRADIENT IS SUSTAINED
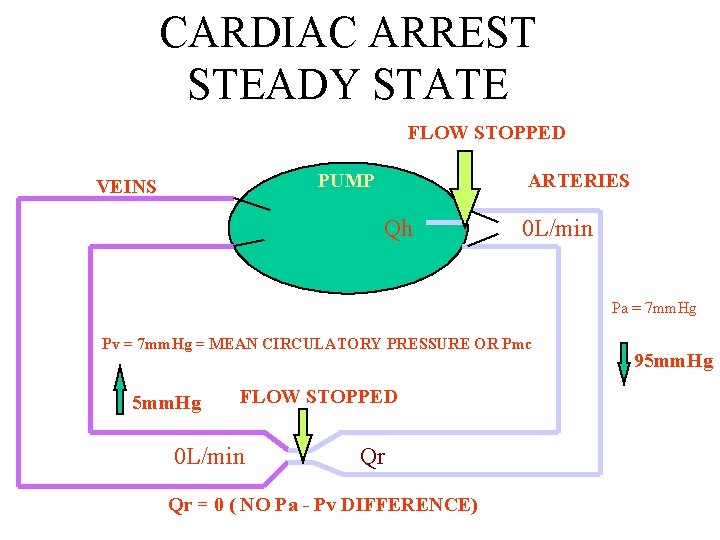
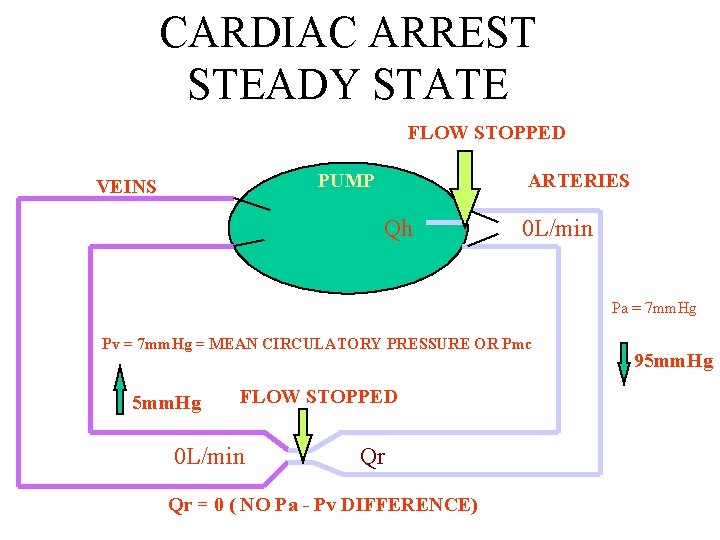
CARDIAC ARREST STEADY STATE FLOW STOPPED PUMP VEINS ARTERIES Qh 0 L/min Pa = 7 mm. Hg Pv = 7 mm. Hg = MEAN CIRCULATORY PRESSURE OR Pmc 5 mm. Hg FLOW STOPPED 0 L/min Qr Qr = 0 ( NO Pa - Pv DIFFERENCE) 95 mm. Hg
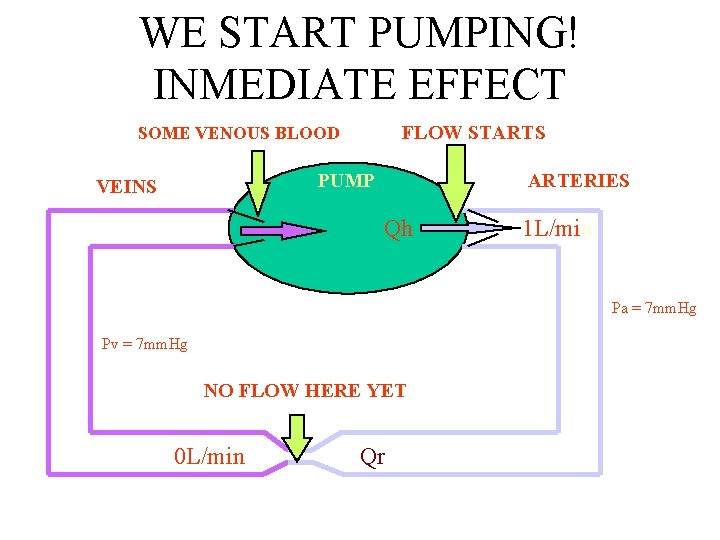
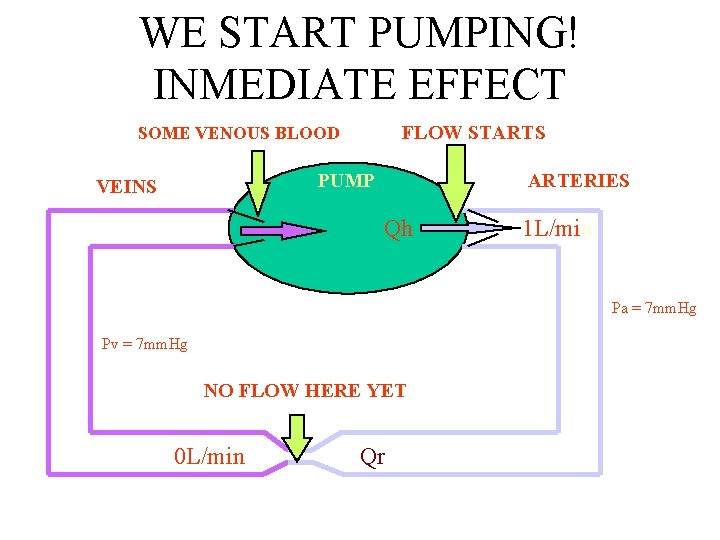
WE START PUMPING! INMEDIATE EFFECT FLOW STARTS SOME VENOUS BLOOD PUMP VEINS ARTERIES Qh 1 L/min Pa = 7 mm. Hg Pv = 7 mm. Hg NO FLOW HERE YET 0 L/min Qr
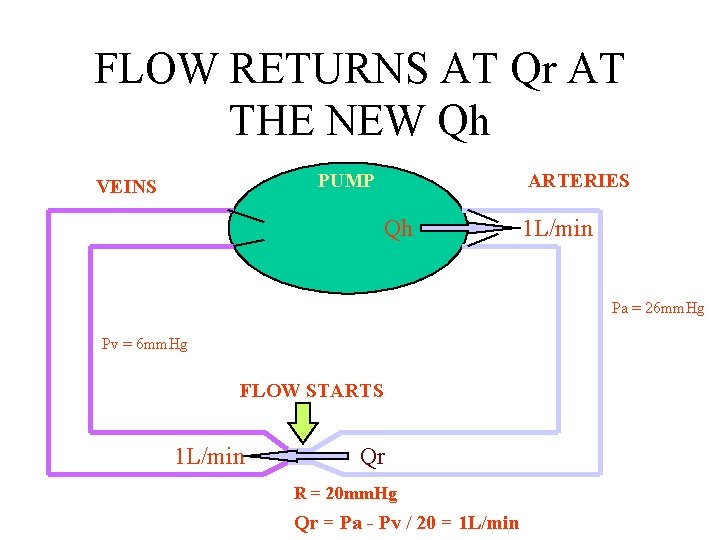
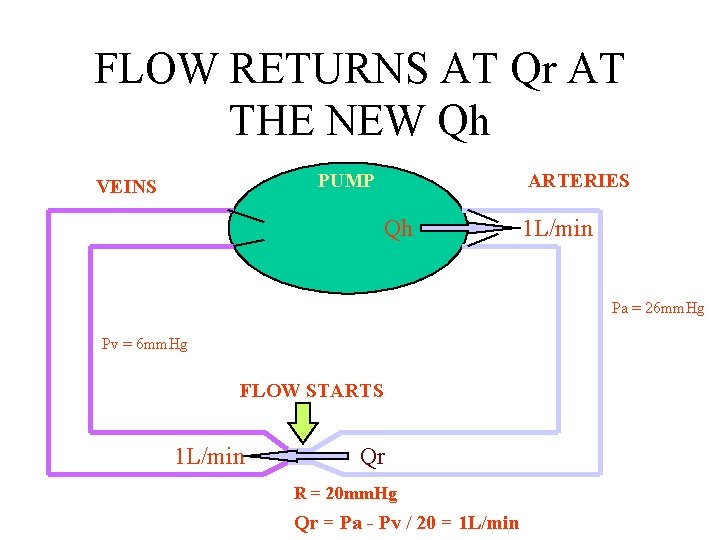
FLOW RETURNS AT Qr AT THE NEW Qh PUMP VEINS ARTERIES Qh 1 L/min Pa = 26 mm. Hg Pv = 6 mm. Hg FLOW STARTS 1 L/min Qr R = 20 mm. Hg Qr = Pa - Pv / 20 = 1 L/min
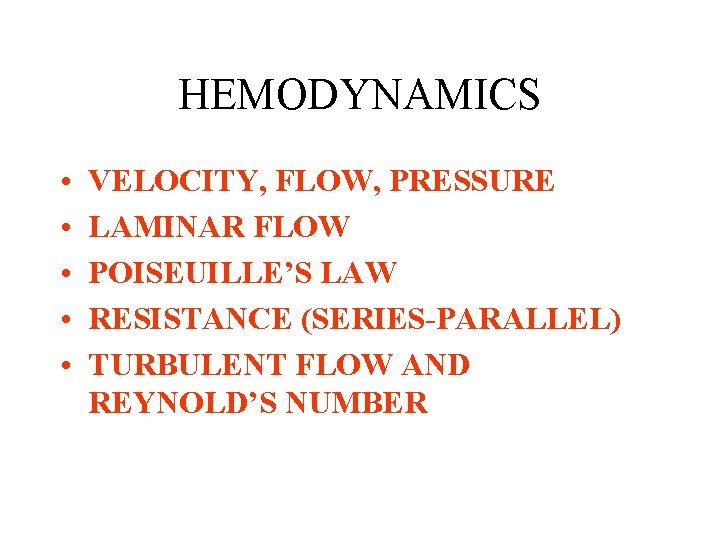
HEMODYNAMICS • • • VELOCITY, FLOW, PRESSURE LAMINAR FLOW POISEUILLE’S LAW RESISTANCE (SERIES-PARALLEL) TURBULENT FLOW AND REYNOLD’S NUMBER
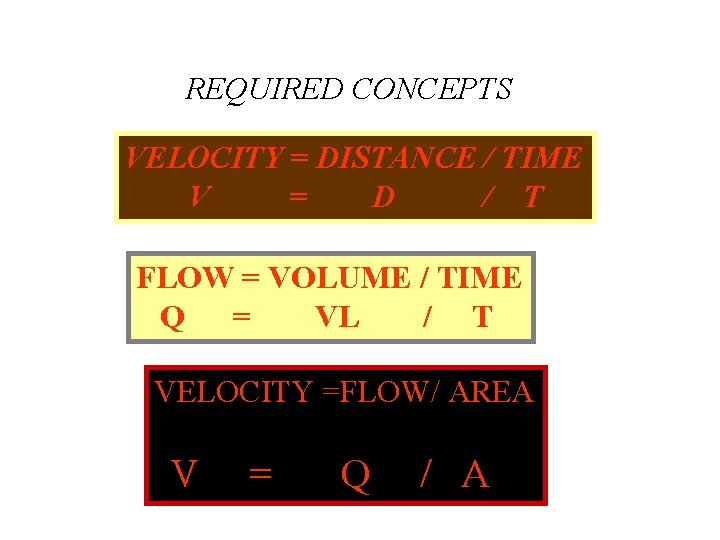
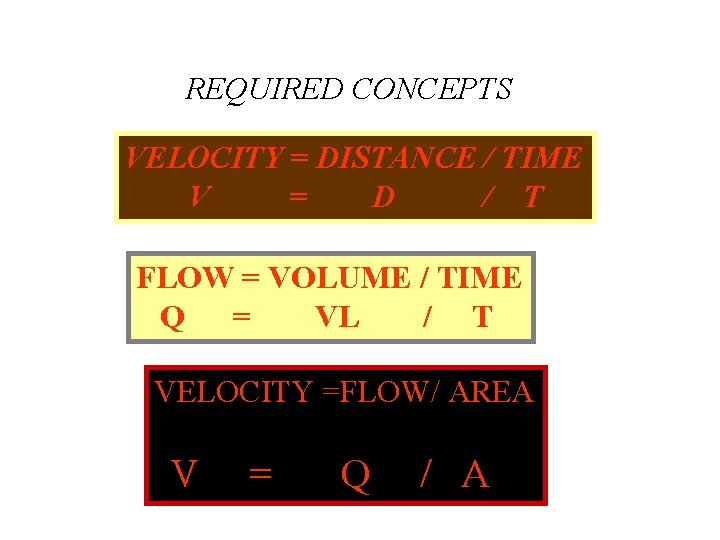
REQUIRED CONCEPTS VELOCITY = DISTANCE / TIME V = D / T FLOW = VOLUME / TIME Q = VL / T VELOCITY =FLOW/ AREA V = Q / A
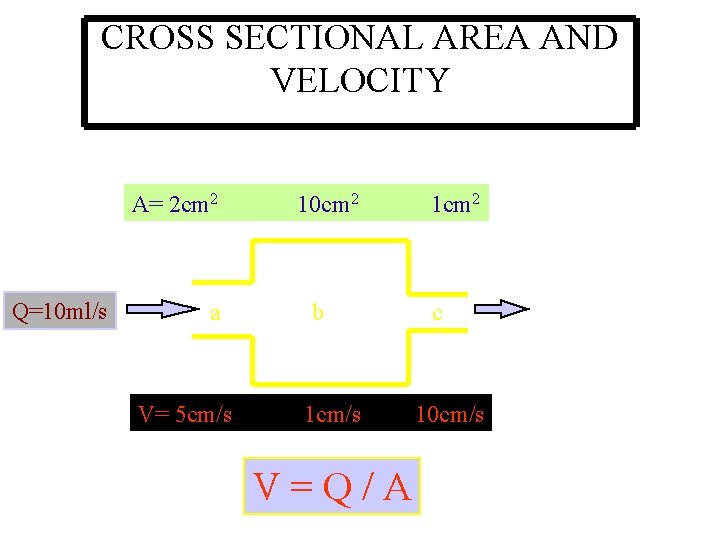
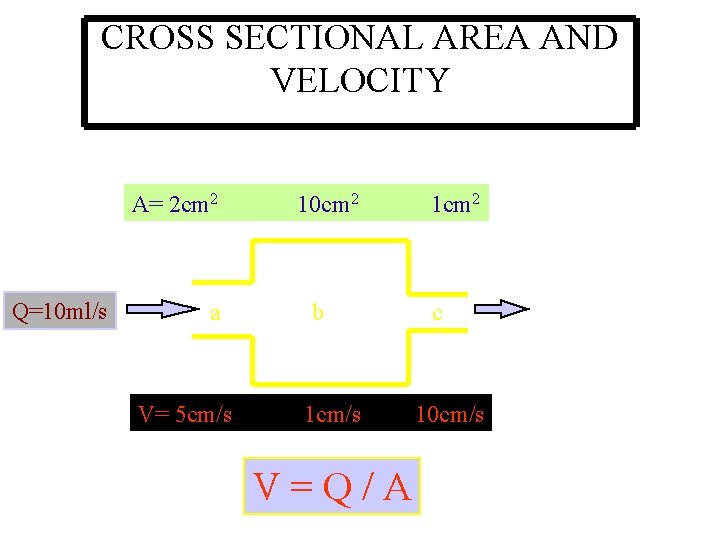
CROSS SECTIONAL AREA AND VELOCITY A= 2 cm 2 10 cm 2 1 cm 2 Q=10 ml/s a b c V= 5 cm/s 1 cm/s 10 cm/s V = Q / A
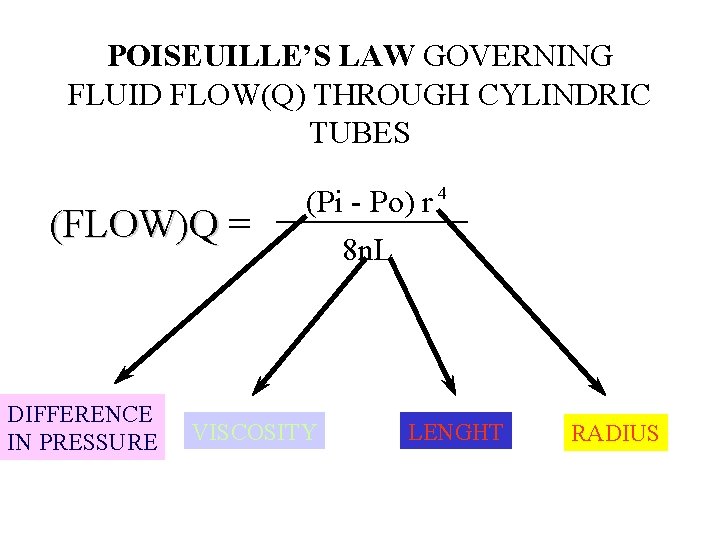
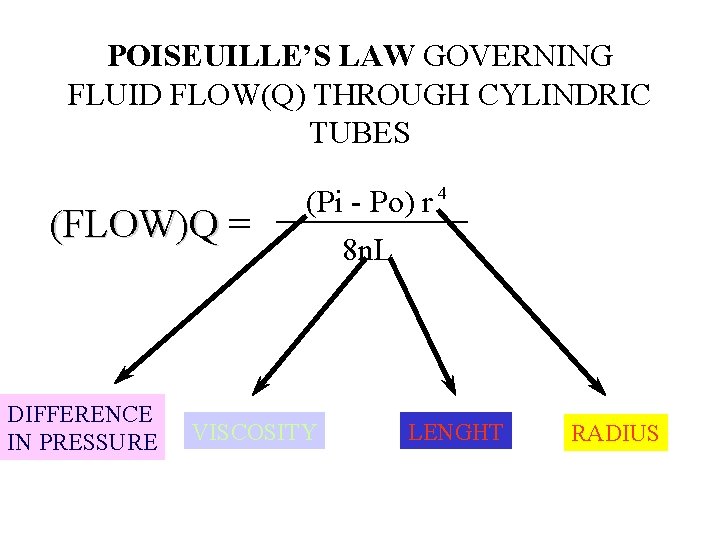
POISEUILLE’S LAW GOVERNING FLUID FLOW(Q) THROUGH CYLINDRIC TUBES (FLOW)Q = (FLOW)Q DIFFERENCE IN PRESSURE 4 (Pi - Po) r 8 n. L VISCOSITY LENGHT RADIUS
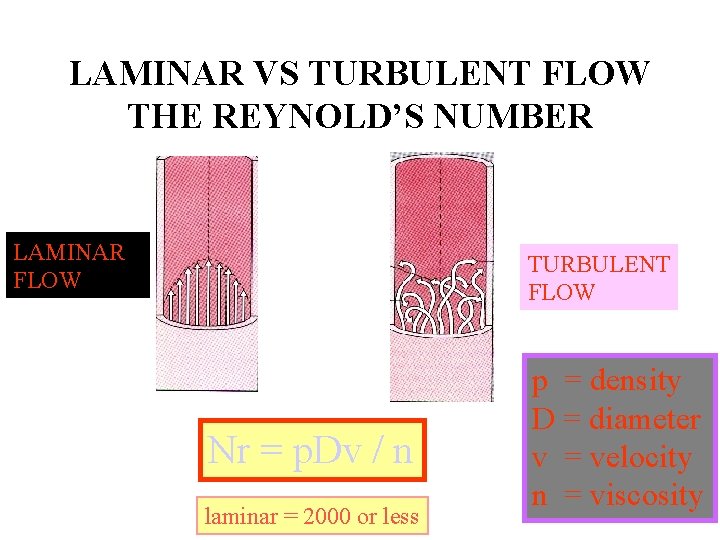
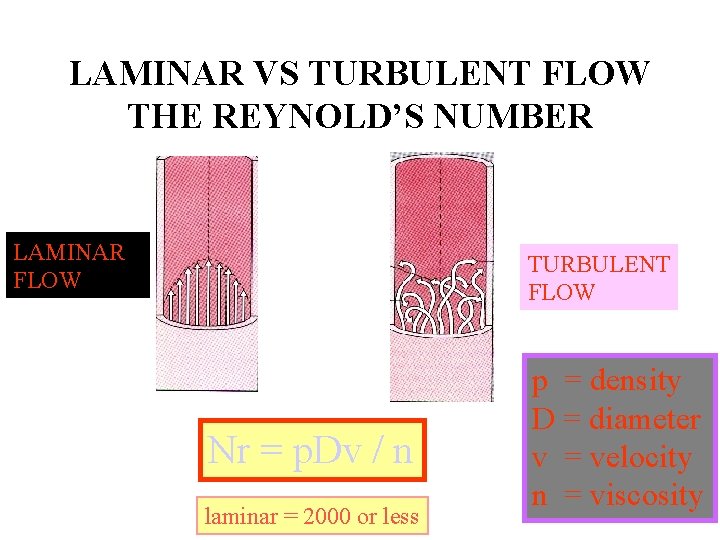
LAMINAR VS TURBULENT FLOW THE REYNOLD’S NUMBER LAMINAR FLOW TURBULENT FLOW Nr = p. Dv / n laminar = 2000 or less p = density D = diameter v = velocity n = viscosity
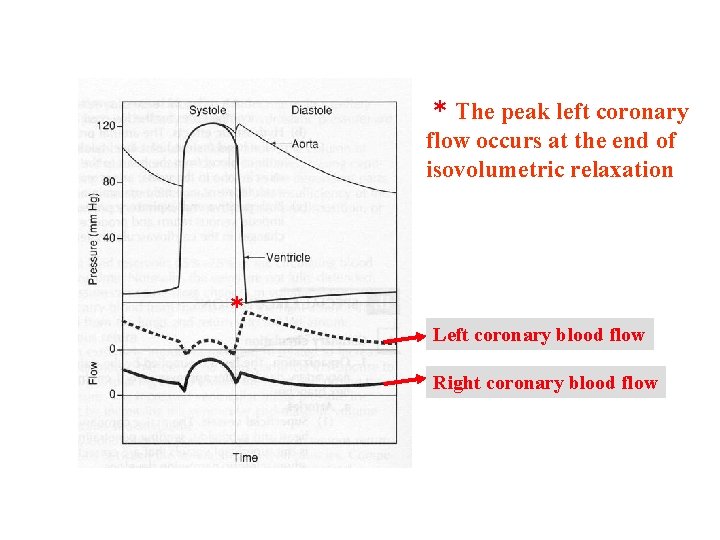
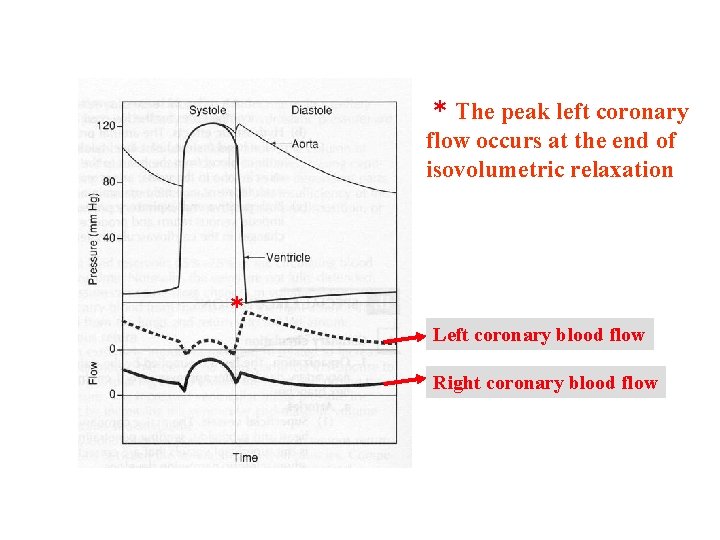
* The peak left coronary flow occurs at the end of isovolumetric relaxation * Left coronary blood flow Right coronary blood flow
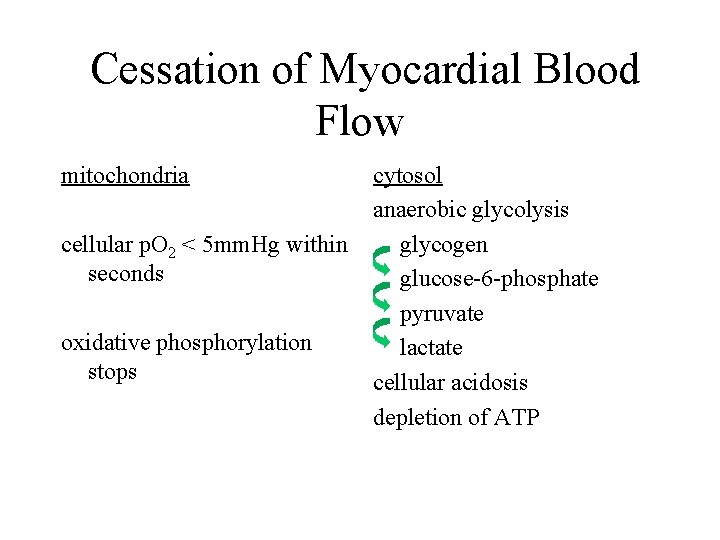
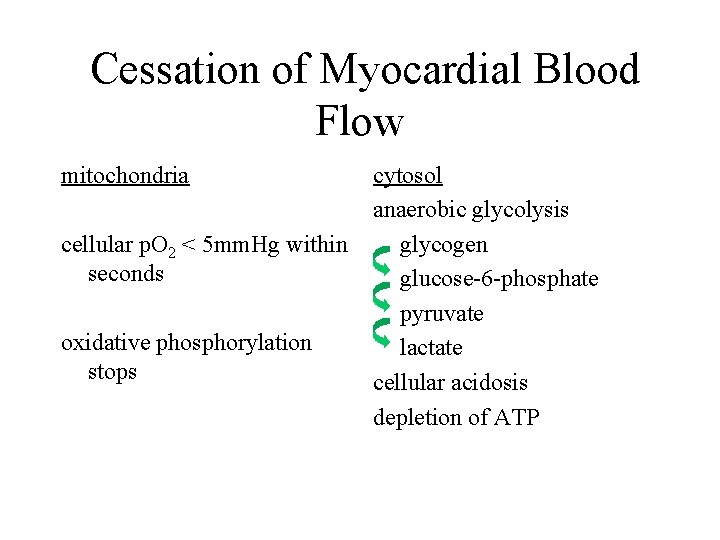
Cessation of Myocardial Blood Flow mitochondria cytosol anaerobic glycolysis cellular p. O 2 < 5 mm. Hg within glycogen seconds glucose-6 -phosphate pyruvate oxidative phosphorylation lactate stops cellular acidosis depletion of ATP
Blood Vessel • Intima primarily the endothelial lining • Media vascular smooth muscle, collagen, elastin • Adventitia connective tissue
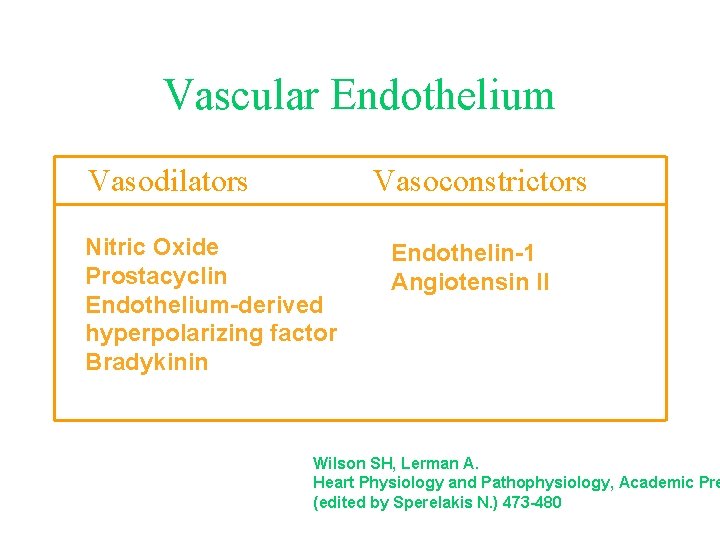
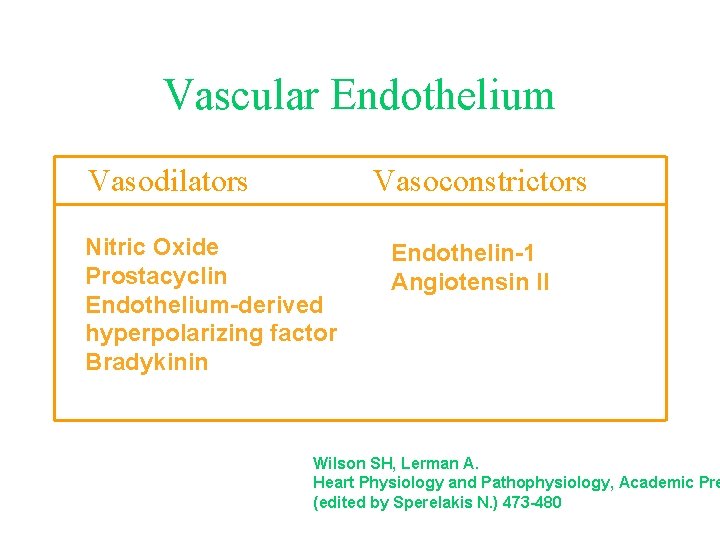
Vascular Endothelium Vasodilators Vasoconstrictors Nitric Oxide Prostacyclin Endothelium-derived hyperpolarizing factor Bradykinin Endothelin-1 Angiotensin II Wilson SH, Lerman A. Heart Physiology and Pathophysiology, Academic Pre (edited by Sperelakis N. ) 473 -480
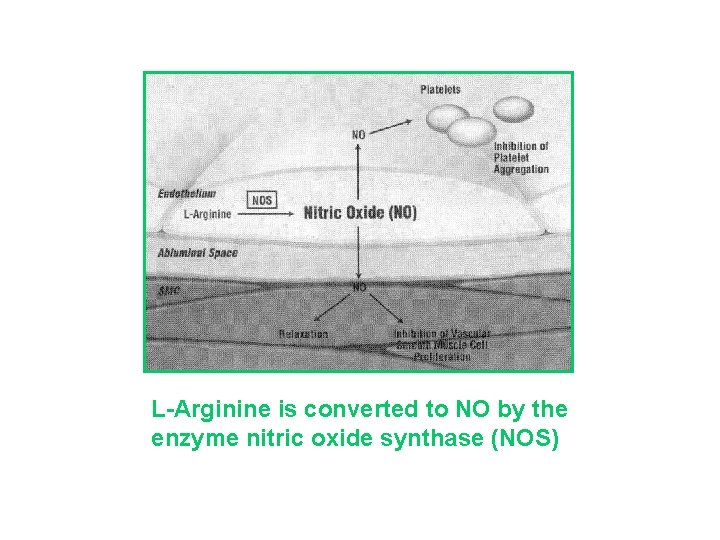
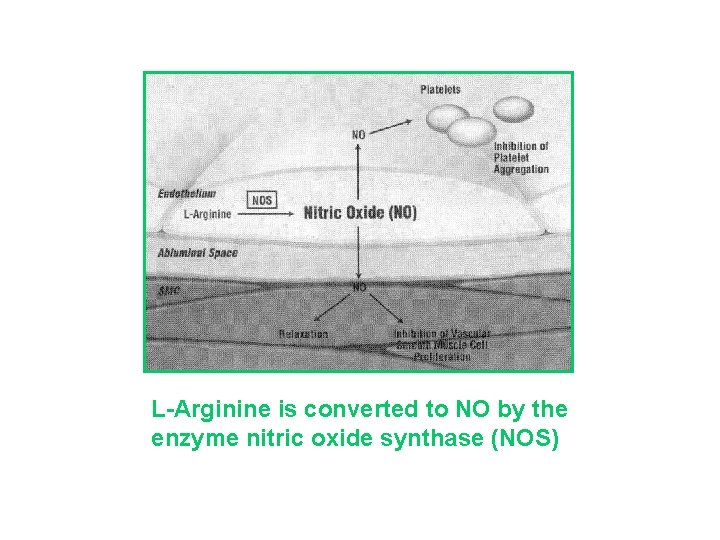
L-Arginine is converted to NO by the enzyme nitric oxide synthase (NOS)
Nitric Oxide (NO) Function • Vasodilator • Inhibitor of vascular smooth muscle cell proliferation • Inhibitor of platelet adherence/aggregation • Inhibitor of leukocyte/endothelial interactions
Endothelin-1 (ET-1) • Peptide first sequenced in 1988 • Most potent vasoconstrictor in humans • Maintenance of basal arterial vasomotor tone • Strong chemoattractant for circulating monocytes and macrophage activation “proatherogenic”
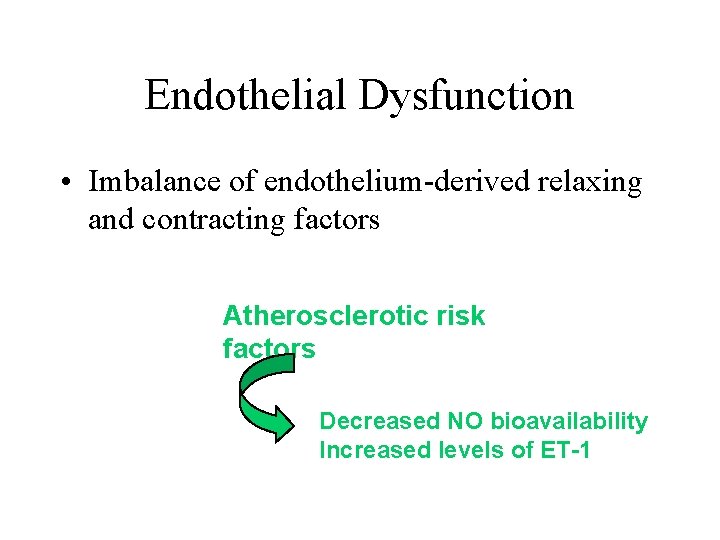
Endothelial Dysfunction • Imbalance of endothelium-derived relaxing and contracting factors Atherosclerotic risk factors Decreased NO bioavailability Increased levels of ET-1