Physician Practice Roundtable A Primer on CMS Hierarchical
Physician Practice Roundtable A Primer on CMS’ Hierarchical Condition Category (HCC) Coding How risk adjustment affects our bottom line Board Update from the Physician Practice Roundtable Updated June 2019
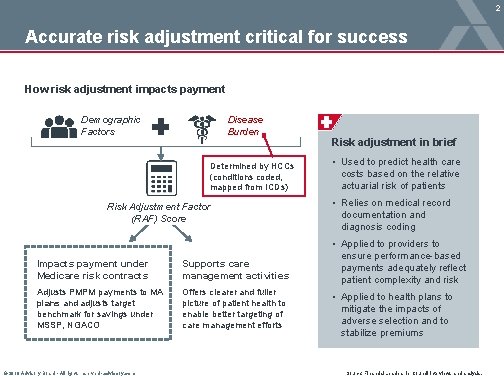
2 Accurate risk adjustment critical for success How risk adjustment impacts payment Demographic Factors Disease Burden Determined by HCCs (conditions coded, mapped from ICDs) Risk Adjustment Factor (RAF) Score Impacts payment under Medicare risk contracts Supports care management activities Adjusts PMPM payments to MA plans and adjusts target benchmark for savings under MSSP, NGACO Offers clearer and fuller picture of patient health to enable better targeting of care management efforts © 2018 Advisory Board • All rights reserved • advisory. com Risk adjustment in brief • Used to predict health care costs based on the relative actuarial risk of patients • Relies on medical record documentation and diagnosis coding • Applied to providers to ensure performance-based payments adequately reflect patient complexity and risk • Applied to health plans to mitigate the impacts of adverse selection and to stabilize premiums Source: Financial Leadership Council interviews and analysis.
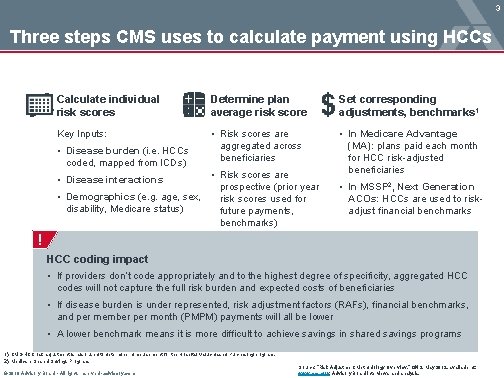
3 Three steps CMS uses to calculate payment using HCCs Calculate individual risk scores Determine plan average risk score Set corresponding adjustments, benchmarks 1 Key Inputs: • Risk scores are aggregated across beneficiaries • In Medicare Advantage (MA): plans paid each month for HCC risk-adjusted beneficiaries • Disease burden (i. e. HCCs coded, mapped from ICDs) • Risk scores are prospective (prior year • Demographics (e. g. age, sex, risk scores used for disability, Medicare status) future payments, benchmarks) • Disease interactions • In MSSP 2, Next Generation ACOs: HCCs are used to riskadjust financial benchmarks ! HCC coding impact • If providers don’t code appropriately and to the highest degree of specificity, aggregated HCC codes will not capture the full risk burden and expected costs of beneficiaries • If disease burden is under represented, risk adjustment factors (RAFs), financial benchmarks, and per member per month (PMPM) payments will all be lower • A lower benchmark means it is more difficult to achieve savings in shared savings programs 1) CMS-HCC risk adjustment is also used to determine reimbursement for the Hospital Value-Based Purchasing program. 2) Medicare Shared Savings Program. © 2018 Advisory Board • All rights reserved • advisory. com Source: “Risk Adjustment Methodology Overview, ” CMS, May 2012, available at: www. cms. gov; Advisory Board interviews and analysis.
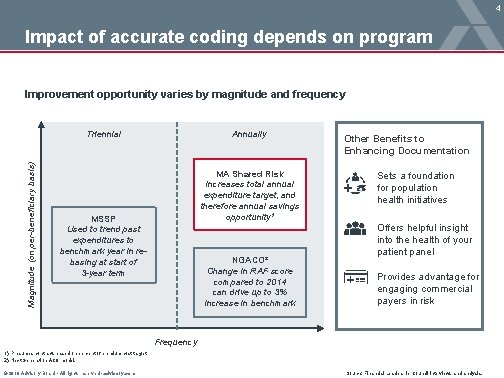
4 Impact of accurate coding depends on program Improvement opportunity varies by magnitude and frequency Magnitude (on per-beneficiary basis) Triennial Annually MA Shared Risk Increases total annual expenditure target, and therefore annual savings opportunity 1 MSSP Used to trend past expenditures to benchmark year in rebasing at start of 3 -year term NGACO² Change in RAF score compared to 2014 can drive up to 3% increase in benchmark Other Benefits to Enhancing Documentation Sets a foundation for population health initiatives Offers helpful insight into the health of your patient panel Provides advantage for engaging commercial payers in risk Frequency 1) Presumes contracts based on percent of premium cost target. 2) Next Generation ACO model. © 2018 Advisory Board • All rights reserved • advisory. com Source: Financial Leadership Council interviews and analysis.
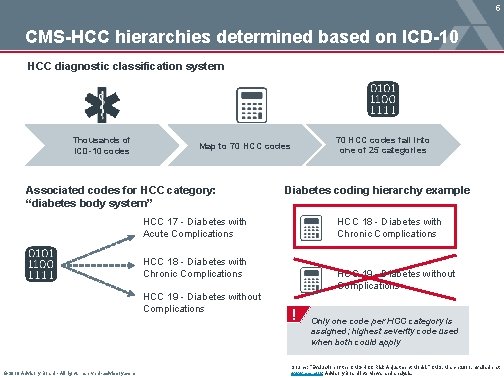
5 CMS-HCC hierarchies determined based on ICD-10 HCC diagnostic classification system Thousands of ICD-10 codes 70 HCC codes fall into one of 25 categories Map to 70 HCC codes Associated codes for HCC category: “diabetes body system” Diabetes coding hierarchy example HCC 18 - Diabetes with Chronic Complications HCC 17 - Diabetes with Acute Complications HCC 18 - Diabetes with Chronic Complications HCC 19 - Diabetes without Complications © 2018 Advisory Board • All rights reserved • advisory. com HCC 19 - Diabetes without Complications ! Only one code per HCC category is assigned; highest severity code used when both could apply Source: “Evaluation of the CMS-HCC Risk Adjustment Model, ” CMS, March 2011, available at: www. cms. gov; Advisory Board interviews and analysis.
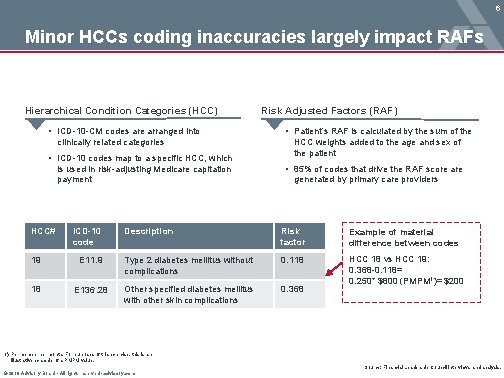
6 Minor HCCs coding inaccuracies largely impact RAFs Hierarchical Condition Categories (HCC) • ICD-10 -CM codes are arranged into clinically related categories • ICD-10 codes map to a specific HCC, which is used in risk-adjusting Medicare capitation payment HCC# ICD-10 code Risk Adjusted Factors (RAF) • Patient’s RAF is calculated by the sum of the HCC weights added to the age and sex of the patient • 85% of codes that drive the RAF score are generated by primary care providers Description Risk factor Example of material difference between codes HCC 18 vs HCC 19: 0. 368 -0. 118= 0. 250* $800 (PMPM 1)= $200 19 E 11. 9 Type 2 diabetes mellitus without complications 0. 118 18 E 136. 28 Other specified diabetes mellitus with other skin complications 0. 368 1) Per member per month. For purposes of this exercise, this is an illustrative example of a PMPM value. Source: Financial Leadership Council interviews and analysis. © 2018 Advisory Board • All rights reserved • advisory. com
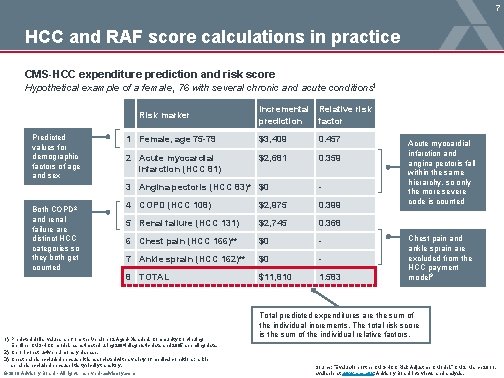
7 HCC and RAF score calculations in practice CMS-HCC expenditure prediction and risk score Hypothetical example of a female, 76 with several chronic and acute conditions 1 Risk marker Predicted values for demographic factors of age and sex Both COPD 2 and renal failure are distinct HCC categories so they both get counted Incremental Relative risk prediction factor 1 Female, age 75 -79 $3, 409 0. 457 2 Acute myocardial infarction (HCC 81) $2, 681 0. 359 3 Angina pectoris (HCC 83)* $0 - 4 COPD (HCC 108) $2, 975 0. 399 5 Renal failure (HCC 131) $2, 745 0. 368 6 Chest pain (HCC 166)** $0 - 7 Ankle sprain (HCC 162)** $0 - 8 TOTAL $11, 810 1. 583 1) Predicted dollar values are from the Version 12 Aged-Disabled, Community Continuing Acute myocardial infarction and angina pectoris fall within the same hierarchy, so only the more severe code is counted Chest pain and ankle sprain are excluded from the HCC payment model 3 Total predicted expenditures are the sum of the individual increments. The total risk score is the sum of the individual relative factors. Enrollee CMS-HCC model, as estimated using 2004 diagnostic data and 2005 spending data. 2) Chronic obstructive pulmonary disease. 3) Chest pain is excluded because it is associated with a variety of medical conditions; ankle sprain is excluded because it is typically transitory. © 2018 Advisory Board • All rights reserved • advisory. com Source: “Evaluation of the CMS-HCC Risk Adjustment Model, ” CMS, March 2011, available at: www. cms. gov; Advisory Board interviews and analysis.
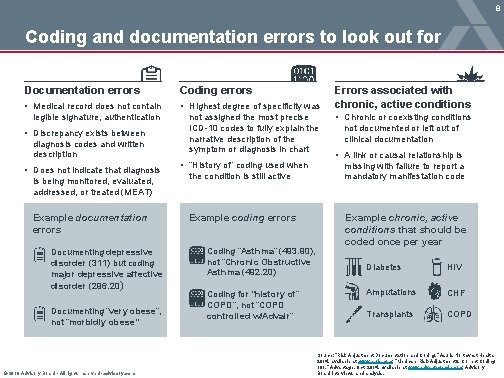
8 Coding and documentation errors to look out for Documentation errors Coding errors • Medical record does not contain • Highest degree of specificity was legible signature, authentication not assigned the most precise ICD-10 codes to fully explain the narrative description of the symptom or diagnosis in chart • Discrepancy exists between diagnosis codes and written description • Does not indicate that diagnosis is being monitored, evaluated, addressed, or treated (MEAT) Example documentation errors Documenting depressive disorder (311) but coding major depressive affective disorder (296. 20) Documenting “very obese”, not “morbidly obese” © 2018 Advisory Board • All rights reserved • advisory. com • “History of” coding used when the condition is still active Example coding errors Coding “Asthma” (493. 90), not “Chronic Obstructive Asthma (492. 20) Coding for “history of” COPD”, not “COPD controlled w/Advair” Errors associated with chronic, active conditions • Chronic or coexisting conditions not documented or left out of clinical documentation • A link or causal relationship is missing with failure to report a mandatory manifestation code Example chronic, active conditions that should be coded once per year Diabetes HIV Amputations CHF Transplants COPD Source: “Risk Adjustment Documentation and Coding, ” Asuris Northwest Health, 2014, available at: www. auris. com; “Medicare Risk-Adjustment & Correct Coding 101. ” Advantage, Oct. 2014, available at: www. advantagecdn. com; Advisory Board interviews and analysis.
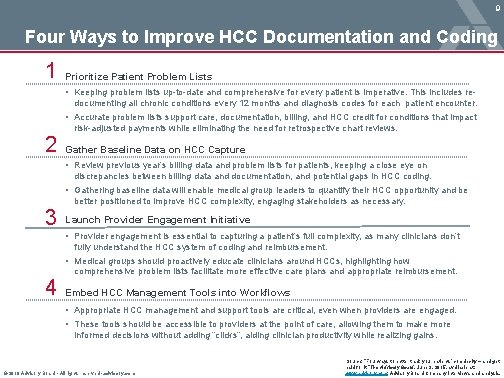
9 Four Ways to Improve HCC Documentation and Coding 1 Prioritize Patient Problem Lists • Keeping problem lists up-to-date and comprehensive for every patient is imperative. This includes redocumenting all chronic conditions every 12 months and diagnosis codes for each patient encounter. • Accurate problem lists support care, documentation, billing, and HCC credit for conditions that impact 2 risk-adjusted payments while eliminating the need for retrospective chart reviews. Gather Baseline Data on HCC Capture • Review previous year’s billing data and problem lists for patients, keeping a close eye on discrepancies between billing data and documentation, and potential gaps in HCC coding. • Gathering baseline data will enable medical group leaders to quantify their HCC opportunity and be 3 better positioned to improve HCC complexity, engaging stakeholders as necessary. Launch Provider Engagement Initiative • Provider engagement is essential to capturing a patient’s full complexity, as many clinicians don’t fully understand the HCC system of coding and reimbursement. • Medical groups should proactively educate clinicians around HCCs, highlighting how 4 comprehensive problem lists facilitate more effective care plans and appropriate reimbursement. Embed HCC Management Tools into Workflows • Appropriate HCC management and support tools are critical, even when providers are engaged. • These tools should be accessible to providers at the point of care, allowing them to make more informed decisions without adding “clicks”, aiding clinician productivity while realizing gains. © 2018 Advisory Board • All rights reserved • advisory. com Source: “Four ways to better track your patients’ complexity – and get paid for it, ” The Advisory Board, June 3, 2015, available at: www. advisory. com; Advisory Board Company interviews and analysis.
- Slides: 9