Physical Therapy Clinical Decision Making Interventions and Outcomes
- Slides: 1
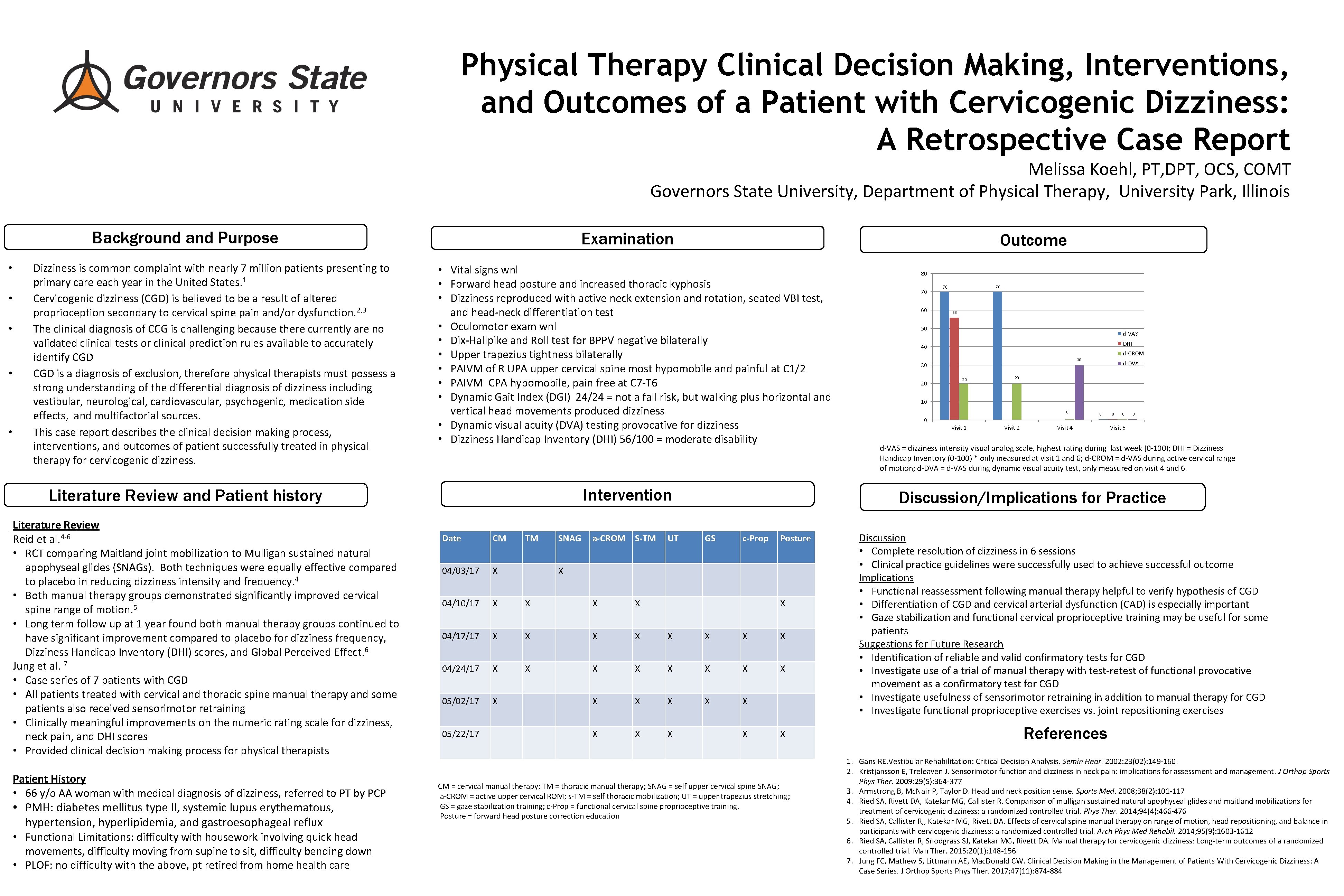
Physical Therapy Clinical Decision Making, Interventions, and Outcomes of a Patient with Cervicogenic Dizziness: A Retrospective Case Report Melissa Koehl, PT, DPT, OCS, COMT Governors State University, Department of Physical Therapy, University Park, Illinois Background and Purpose • • • Dizziness is common complaint with nearly 7 million patients presenting to primary care each year in the United States. 1 Cervicogenic dizziness (CGD) is believed to be a result of altered proprioception secondary to cervical spine pain and/or dysfunction. 2, 3 The clinical diagnosis of CCG is challenging because there currently are no validated clinical tests or clinical prediction rules available to accurately identify CGD is a diagnosis of exclusion, therefore physical therapists must possess a strong understanding of the differential diagnosis of dizziness including vestibular, neurological, cardiovascular, psychogenic, medication side effects, and multifactorial sources. This case report describes the clinical decision making process, interventions, and outcomes of patient successfully treated in physical therapy for cervicogenic dizziness. Examination • Vital signs wnl • Forward head posture and increased thoracic kyphosis • Dizziness reproduced with active neck extension and rotation, seated VBI test, and head-neck differentiation test • Oculomotor exam wnl • Dix-Hallpike and Roll test for BPPV negative bilaterally • Upper trapezius tightness bilaterally • PAIVM of R UPA upper cervical spine most hypomobile and painful at C 1/2 • PAIVM CPA hypomobile, pain free at C 7 -T 6 • Dynamic Gait Index (DGI) 24/24 = not a fall risk, but walking plus horizontal and vertical head movements produced dizziness • Dynamic visual acuity (DVA) testing provocative for dizziness • Dizziness Handicap Inventory (DHI) 56/100 = moderate disability Intervention Literature Review and Patient history • Literature Review Reid et al. 4 -6 • RCT comparing Maitland joint mobilization to Mulligan sustained natural apophyseal glides (SNAGs). Both techniques were equally effective compared to placebo in reducing dizziness intensity and frequency. 4 • Both manual therapy groups demonstrated significantly improved cervical spine range of motion. 5 • Long term follow up at 1 year found both manual therapy groups continued to have significant improvement compared to placebo for dizziness frequency, Dizziness Handicap Inventory (DHI) scores, and Global Perceived Effect. 6 Jung et al. 7 • Case series of 7 patients with CGD • All patients treated with cervical and thoracic spine manual therapy and some patients also received sensorimotor retraining • Clinically meaningful improvements on the numeric rating scale for dizziness, neck pain, and DHI scores • Provided clinical decision making process for physical therapists Patient History • 66 y/o AA woman with medical diagnosis of dizziness, referred to PT by PCP • PMH: diabetes mellitus type II, systemic lupus erythematous, hypertension, hyperlipidemia, and gastroesophageal reflux • Functional Limitations: difficulty with housework involving quick head movements, difficulty moving from supine to sit, difficulty bending down • PLOF: no difficulty with the above, pt retired from home health care Outcome SNAG a-CROM S-TM UT 70 60 70 70 56 50 d-VAS DHI 40 d-CROM 30 30 20 20 d-DVA 20 10 0 0 Visit 1 Visit 2 0 Visit 4 0 0 0 Visit 6 d-VAS = dizziness intensity visual analog scale, highest rating during last week (0 -100); DHI = Dizziness Handicap Inventory (0 -100) * only measured at visit 1 and 6; d-CROM = d-VAS during active cervical range of motion; d-DVA = d-VAS during dynamic visual acuity test, only measured on visit 4 and 6. Discussion/Implications for Practice Date CM 04/03/17 X 04/10/17 X X 04/17/17 X X X X 04/24/17 X X X X 05/02/17 X X X X X 05/22/17 TM 80 GS c-Prop Posture X X CM = cervical manual therapy; TM = thoracic manual therapy; SNAG = self upper cervical spine SNAG; a-CROM = active upper cervical ROM; s-TM = self thoracic mobilization; UT = upper trapezius stretching; GS = gaze stabilization training; c-Prop = functional cervical spine proprioceptive training. Posture = forward head posture correction education Discussion • Complete resolution of dizziness in 6 sessions • Clinical practice guidelines were successfully used to achieve successful outcome Implications • Functional reassessment following manual therapy helpful to verify hypothesis of CGD • Differentiation of CGD and cervical arterial dysfunction (CAD) is especially important • Gaze stabilization and functional cervical proprioceptive training may be useful for some patients Suggestions for Future Research • Identification of reliable and valid confirmatory tests for CGD • Investigate use of a trial of manual therapy with test-retest of functional provocative movement as a confirmatory test for CGD • Investigate usefulness of sensorimotor retraining in addition to manual therapy for CGD • Investigate functional proprioceptive exercises vs. joint repositioning exercises References 1. Gans RE. Vestibular Rehabilitation: Critical Decision Analysis. Semin Hear. 2002: 23(02): 149 -160. 2. Kristjansson E, Treleaven J. Sensorimotor function and dizziness in neck pain: implications for assessment and management. J Orthop Sports Phys Ther. 2009; 29(5): 364 -377 3. Armstrong B, Mc. Nair P, Taylor D. Head and neck position sense. Sports Med. 2008; 38(2): 101 -117 4. Ried SA, Rivett DA, Katekar MG, Callister R. Comparison of mulligan sustained natural apophyseal glides and maitland mobilizations for treatment of cervicogenic dizziness: a randomized controlled trial. Phys Ther. 2014; 94(4): 466 -476 5. Ried SA, Callister R, , Katekar MG, Rivett DA. Effects of cervical spine manual therapy on range of motion, head repositioning, and balance in participants with cervicogenic dizziness: a randomized controlled trial. Arch Phys Med Rehabil. 2014; 95(9): 1603 -1612 6. Ried SA, Callister R, Snodgrass SJ, Katekar MG, Rivett DA. Manual therapy for cervicogenic dizziness: Long-term outcomes of a randomized controlled trial. Man Ther. 2015: 20(1): 148 -156 7. Jung FC, Mathew S, Littmann AE, Mac. Donald CW. Clinical Decision Making in the Management of Patients With Cervicogenic Dizziness: A Case Series. J Orthop Sports Phys Ther. 2017; 47(11): 874 -884